PRACTICAL IMPLICATIONS
Nutritional deficiency has to be considered among the main causes of reversible dementia. An adequate dietary supplementation might solve cognitive impairment entirely.
Case
A 49-year-old man was admitted in the psychiatric unit of our hospital because of an acute episode of severe agitation and persecutory ideas, forcing the wife to bring him to the emergency department (ED). His medical history was marked by a couple of similar accesses to the ED with acute agitation in the recent past. In addition, his wife reported, in the past 2 years, an inclination to retirement and depressive mood and a continuous decline in mood with apathy and inertia and deficits in episodic memory, with increasing forgetfulness despite maintaining good work functioning. Quite surprisingly, she added that the patient had started to follow a strict fruitarian diet with a highly predominant consumption of just apples. He did neither smoke nor drink alcohol. Notwithstanding, oral olanzapine (15 mg/d) was started with improvement of agitation; however, the patient showed a gradual cognitive worsening with disorientation and executive dysfunction.
The neurologic examination found no abnormalities in strength, sensation, and cranial nerves. Deep tendon reflexes were normal. Minimental state examination (MMSE) performed at day 5 scored 19 of 30. Deficits were seen primarily in the areas of working memory and immediate attention. Weakness in the executive functioning was also suggested based on his qualitative performance across the copy of the pentagons test. The symptoms worsened within the following days with insomnia, marked fluctuations in alertness, and daytime sleepiness alternating psychomotor agitation. At day 8, a second MMSE scored 15 of 30. Brain MRI, lumbar puncture, serologic testing for syphilis and HIV, and onconeural antibodies were unremarkable. Serial EEG showed a persistent diffuse slow rhythm. A [18F] fluorodeoxyglucose PET showed bilateral frontal, parietal, and temporal hypometabolism with a focal even lower metabolism area on the right temporal region. Blood samples indicated increased mean corpuscular volume of red cells (120 fL, normal range 80–100 fL) and very low levels of vitamin B12 (50 ng/mL, normal range 200–900 ng/mL), whereas folate was in the normal range. Intramuscular supplementation of cyanocobalamin (1 mg/d in the first week) was initiated, together with an appropriate diet that the patient now accepted. After 10 days, initial signs of cognitive improvement were present, and his behaviour now seemed appropriate to the setting. He was discharged to a rehabilitation clinic at day 19. Two months later, he underwent a neuropsychological evaluation that showed an impressive improvement in global cognitive performance—MMSE now scored 27. At the last follow-up evaluation on April 2020, i.e., 4 years after the hospitalization, MMSE was 30.
Discussion
Vitamin B12 deficiency precipitating megaloblastic anemia or glossitis is a common condition, although it is rarer to appreciate its flagrant neuropsychological manifestations. Cyanocobalamin deficit might precipitate many different neurologic manifestations, such as peripheral neuropathy, subacute combined degeneration, autonomic dysfunction, optic atrophy, mood and behavior changes, psychosis, memory impairment, and cognitive decline.1 In the present case, cognitive and psychotic symptoms rapidly resolved after cyanocobalamin replacement, thus demonstrating a linkage between vitamin B12 deficit and patient's cognitive deterioration. Specifically, the subacute fluctuating course of the clinical picture was compatible with delirium so that delirium superimposed on dementia could not be excluded.2
In our case, vitamin B12 defect was caused by the strict fruitarian diet followed voluntarily by the patient, which had caused an insufficient supply of the vitamin. The fruitarian diet is a subset of the vegan one. It is a highly restrictive eating regime. It consists entirely of fruits, nuts, and seeds. The risk of malnutrition is high despite the nutritional quality of most fruits.
The debate between followers of plant-rich vs inflexible plant-only diets dates back to about one century ago when the British Medical Journal berated fruitarians writing: “man can be natural without doing unnatural things.”3
Although evidence from epidemiology studies suggest that most balanced vegetarian diets are associated with a lower risk of ischemic heart disease and cancer,4 the safety of a strict vegan diet remains unproven; in fact, according also to our case, strict veganism and its fruitarian declination could lead to a wide range of severe consequences such as severe ketoacidosis5 or intestinal obstructing fitobezoars forcing to surgical intervention.6
A poll conducted in 2019 by EURISPES reported that in Italy, 5.4% and 1.9% of the population is vegetarian or vegan, respectively.7 Compared with 2018, the number of people following a vegan diet is increased, whereas vegetarian have lost almost one-point percent, probably because of a shift toward stricter vegan regime. Assuming that the Italian trend reflects a global direction, the incidence of dementia associated with B12 deficiency may increase according to the growing number of vegan people worldwide.
Neurologists and, more generally, clinicians should be prepared to recognize it and supplement any deficiency; what is more, they should be prone to educate patients toward more equilibrated diets.
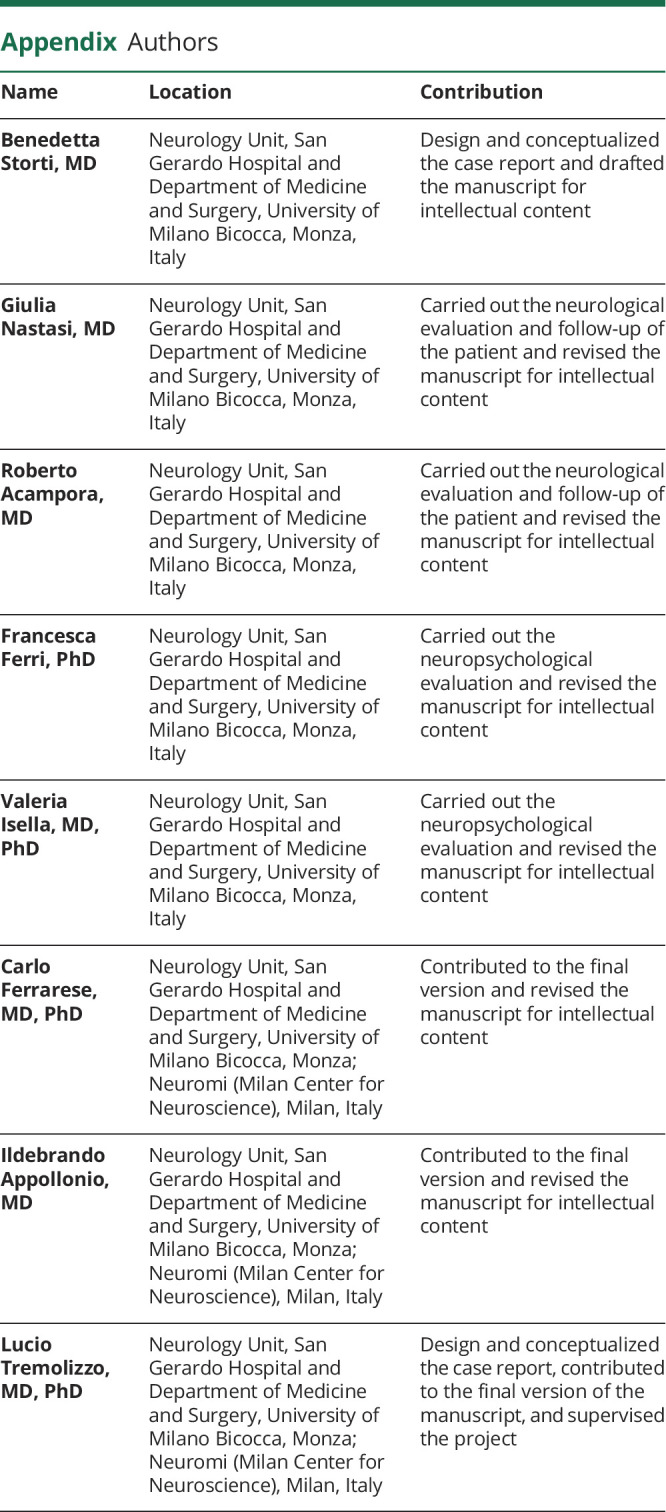
Appendix. Authors
Study Funding
No targeted funding reported.
Disclosure
The authors report no disclosures relevant to the manuscript. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
References
- 1.Reynolds E. Vitamin B12, folic acid, and the nervous system. Lancet Neurol 2006;5:949–960. [DOI] [PubMed] [Google Scholar]
- 2.Morandi A, Bellelli G. Delirium superimposed on dementia. Eur Geriatr Med 2020;11:53–62. [DOI] [PubMed] [Google Scholar]
- 3.A converted “Fruitarian.” BMJ 2000;321:1331E. [PMC free article] [PubMed] [Google Scholar]
- 4.Dinu M, Abbate R, Gensini GC, Casini A, Sofi F. Vegetarian, vegan diets and multiple health outcomes: a systematic review with meta-analysis of observational studies. Crit Rev Food Sci Nutr 2017;57:3640–3649. [DOI] [PubMed] [Google Scholar]
- 5.Causso C, Arrieta F, Hernández J, et al. Severe ketoacidosis secondary to starvation in a frutarian patient. Nutr Hosp 2010;25:1049–1052. [PubMed] [Google Scholar]
- 6.Slavin M, Malinger P, Rudnicki Y, Inbar R, Avital S. Ileo-ileal intussusception of a sutured enterotomy site, 6days after laparotomy due to fetobezoar: a case report. Int J Surg Case Rep 2017;36:136–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.EURISPES. Rapporto Italia 2019. Vegetariani e vegani: le nuove diete si consolidano. Estratto rapporto Italia 2019. Available at: https://eurispes.eu/rapporto-italia-2019-vegetariani-e-vegani-le-nuove-diete-si-consolidano/.


