Abstract
Purpose
The COVID-19 pandemic affects students in a myriad of different ways. Our prospective, longitudinal study in a cohort of students in Hannover, Germany explores behavioral patterns during escalating COVID-19 restrictions.
Methods
In total, 777 students between the age of 9 and 20 were assessed for their activity engagement, travel patterns, and self-assessed compliance with protective recommendations at six time points between June 2020 and June 2021 (3,564 observations) and were monitored for severe acute respiratory syndrome coronavirus 2 infection by nasal swab polymerase chain reaction and serum antibody titers.
Results
Activity engagement decreased, but self-assessed compliance with measures such as mask wearing and social distancing was stable during escalating restrictions. Although we found no sex difference during the summer break, when incidence was lowest, females engaged in a higher variety of activities than males for all other time points. Older students engaged in more activities and self-assigned themselves lower compliance values than younger ones. Greater involvement in different activities was seen in households which traveled more frequently. Infection rate in our cohort was low (0.03% acute infections, 1.94% positive seroprevalence).
Discussion
Our study supports the view that, overall, students show high compliance with COVID-19 recommendations and restrictions. The identification of subsets, such as female and older students, with higher risk behavioral patterns should be considered when implementing public information campaigns. In light of the low infection rate in our cohort, we conclude that in-person learning can occur safely if extensive protective measures are in place and the incidence in the general population remains moderate.
Keywords: Adolescents, COVID-19, Behavior, School, Infections
Graphical abstract
Implications and Contribution.
In this study, we longitudinally assessed students’ behavior regarding activities, travel, and compliance with protective measures. Children and adolescents modify their behavior in response to pandemic-related restrictions in an age- and sex-dependent manner. These patterns are highly relevant for the implementation of effective infection control measures, including public information campaigns.
Germany introduced a series of restrictions in March and April of 2020 to combat the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1]. Restrictions were de-escalated in May and June of 2020, but reinstated in November [2]. Children and adolescents were affected by limitations regarding in-person learning, sports and leisure activities, and restrictions on social contacts [3]. The burden of COVID-19 pandemic on young people’s mental and physical health has been the subject of intense study, yet the full impact remains uncertain [4,5].
Much debate surrounds the dilemma that children are potential drivers of the pandemic, but restrictions and school closures have a significant impact on their wellbeing [6,7]. Children overwhelmingly experience mild or asymptomatic disease and are unlikely to be index cases in household transmission [8,9]. Whether this is due to intrinsic biological mechanisms, behavioral patterns, or a combination of both remains unclear [8,10]. Adolescent behavior and alleged noncompliance have been discussed as drivers of viral spread [11] and the role of in-person learning in transmitting infection remains controversial [[12], [13], [14]].
To explore children’s and adolescents’ behavioral patterns and their determinants during escalating COVID-19 restrictions, we conducted a longitudinal observational study in a cohort of students attending in-person schooling in Hannover, Germany.
Methods
Study design
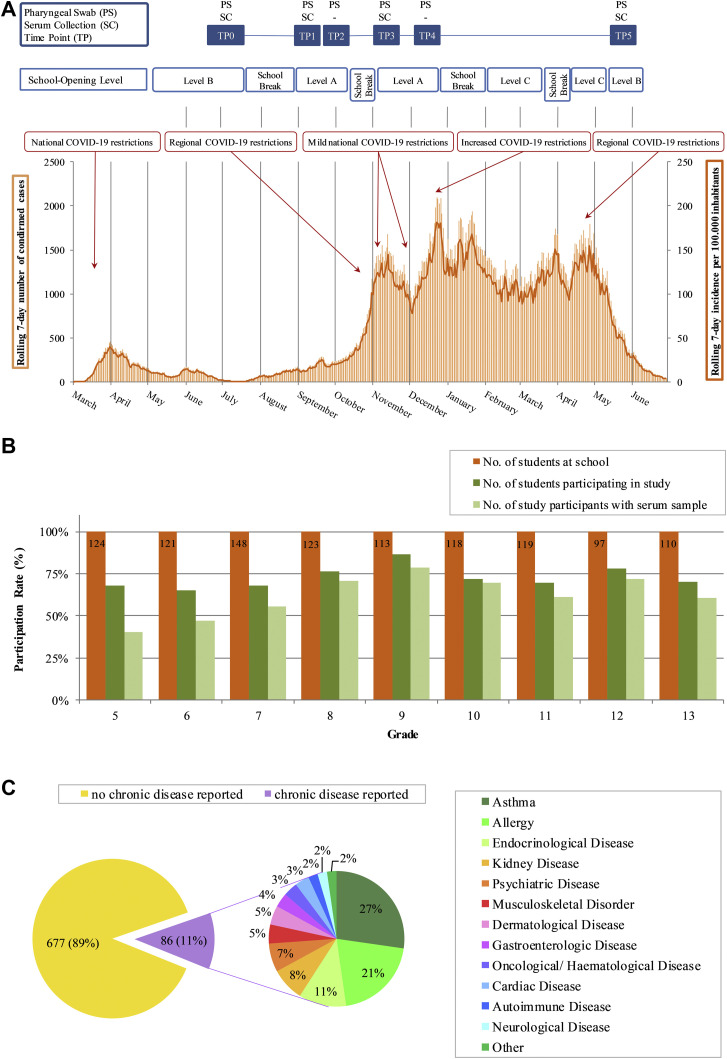
This prospective, longitudinal cohort study was open to all students (grades 5–13) attending a secondary school in Hannover, Germany. Data were collected at six time points (TP) over the course of 1 year (June 2020 to June 2021), with the initial TP before the summer break (TP0) and five follow-up TP (TP1-5) in September, October, November, December, and June (Figure 1 A). Detailed information about state-mandated COVID-19 restrictions and school opening levels are given in Figure A1. Participants were tested on-site during school hours and were asymptomatic at the time of testing. Students with symptoms of a respiratory tract infection or with a “high risk contact” were not permitted on school grounds due to the Department of Education regulations.
Figure 1.
Study design. Testing time points (TP0–TP4) in relation to regional infection rate shown as number of confirmed cases (orange bars) and rolling 7-day average per 100,000 inhabitants [15] (orange line). Serum collection (SC) and pharyngeal swap (PS) sampling are indicated. School-opening levels (A–C) (Figure A1), school breaks, and national restrictions are displayed (A). Percentage of students participating in this study per grade including subject that consented to serum collection (B). Proportion of chronic disease reported by participants. Chronic diseases were summarized in organ related groups (C).
The study was approved by the Institutional Review Board (No. 9085_BO_S_2020) and complies with the Declaration of Helsinki. Study participation was voluntary and informed consent was obtained from participants and, in case of minors, their legal guardians. Study entry or opt-out was possible at any time.
Data and sample collection
Pharyngeal swabs were collected at each TP; serum samples were collected at TP0, TP1, TP3, and TP5.
A questionnaire assessing age, sex, history of COVID-19 infection, smoking behavior, health status, and household size was handed out at study inclusion. At every follow-up TP, we distributed a second, shorter questionnaire on everyday activities, travel, and compliance with COVID-19 prevention recommendations. Participants were asked whether in the previous 30 days they had engaged in 23 predefined activities. Travel was defined as at least one overnight stay outside a participant’s primary residence. Adherence to hand hygiene, social distancing, and mask usage were reported by the participants on a visual analog scale between 0 (low) and 10 (high) compliance. Participants ranked both their own and their families’ compliance.
Laboratory testing
Polymerase chain reaction (PCR) tests for samples at TP0, TP1, TP2, TP3, and TP5 were performed using the protocol of Corman et al. [16]. RNA was isolated immediately on-site in a mobile laboratory, and transported for further processing off-site. The samples of TP4 and TP5 were processed using reverse transcriptase PCR Allplex 2019-nCoV assay (Seegene Inc., Seoul, South Korea) according to manufacturer’s instructions. A cycle threshold of 40 or below was considered positive.
Serum samples were aliquoted and stored by Hannover Unified Biobank within 3 hours of collection. Sera were tested using the Elecsys Anti-SARS-CoV-2 (Diagnostics International Ltd., Rotkreuz, Switzerland) assay following the manufacturer’s instruction. A cut-off index ≥1.0 was considered reactive.
In a second step, positive antibody samples were tested with a neutralization assay. The samples were diluted at 1:25, 1:100, 1:400, and 1:600. To this end, we used the vesicular stomatitis virus–based SARS-CoV-2 spike pseudotyping system recently described [17].
Statistical analysis
Data are given as mean and standard deviation (SD), numbers (n) and percentages (%) or interquartile range. Paired t-test was performed for self-assessed compliance and self-assessed family member compliance. Multivariable linear mixed regression models were employed for activity engagement, travel patterns, and self-assessed compliance with protective measures, adjusted for TP of testing, age group, and sex as fixed effects, including participant ID as random effect to account for the intersubject variation [18]. For dichotomous endpoints, i.e., the types of activity such as meeting friends (yes/no), we performed a logistic regression for repeated measures including sex as fixed effect [19]. Corrected means and confidence interval for the endpoints were obtained from the least-square-means adjusted to the models. Multiple comparisons were adjusted with Sidak correction. p-values <.05 were considered significant. Statistical analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC).
Results
Study population
A total of 779 students agreed to participate (Table A1). Two students were excluded because the collection of pharyngeal swabs failed due to excessive gagging. About 72.3% (777 of 1,074) of students at the school participated in at least one TP, and 61.2% (657 of 1,074) gave at least one serum sample (Table A2, Figure 1B). Female students accounted for 46.5% (n = 361) of the study population. The mean age was 14.55 (SD 2.57) years. Nine percent reported active smoking within the last 3 months, mainly older students. Detailed demographical data are shown in Table A2. Eleven percent reported having a chronic disease, most commonly asthma and allergies (48.8%) (Figure 1C). Sixty percent (n = 473) of students had at least one college-educated adult in the household.
Severe acute respiratory syndrome coronavirus 2 infection rates and seroprevalence
In June 2020 (TP0), COVID-19 incidence in the region was low, with a 7-day rolling incidence of ∼10/100,000. Incidence rose over the course of the study, reaching ∼130/100,000 by TP4. Following an extensive period of lockdown with no in-person schooling in the winter of 2020/2021 and the introduction of vaccines, incidence decreased, and had reached ∼40/100,000 by TP5 (Figure 1A). In response to infection rates, state mandated restrictions changed multiple times (Figure A1). From April 2020 until the summer break, school restarted with a combination of in-person and virtual learning. When school resumed after the summer break, classes were in-person. From the beginning of 2021, all lessons took place virtually until May 2021, when falling infection rates precipitated a return to an in-person/virtual hybrid model. Whenever in-person schooling took place, mask wearing and handwashing were implemented as well as measures to reduce the number of personal contacts (fixed cohorts, staggered breaks) and frequent ventilation of class rooms (but no air filtering) (Figure A1). Under these conditions, of 3,564 collected pharyngeal swaps, only 1 student tested positive (0.03%). This occurred at TP3 (Table A1).
We identified six students with a positive antibody titer at TP0, reflecting the first wave of infections in Germany (Tables A1 and A3). Neutralizing antibodies were detected in five of six cases. There was no further seroconversion at TP1 or TP3 despite extensive travel over the summer and in-person schooling in autumn. In TP5, after a long period of homeschooling and lockdown, 7 students had seroconverted with neutralizing antibodies in 6 of 7 cases, reflecting the third wave of infections in Germany. The overall seroprevalence was therefore 1.94% (13 of 667).
Student behavior during COVID-19 restrictions
We investigated the changes in behavioral patterns under varying levels of COVID-19 restrictions by assessing the level of activity, travel patterns, and self-assessed compliance with protective recommendations.
Activity engagement
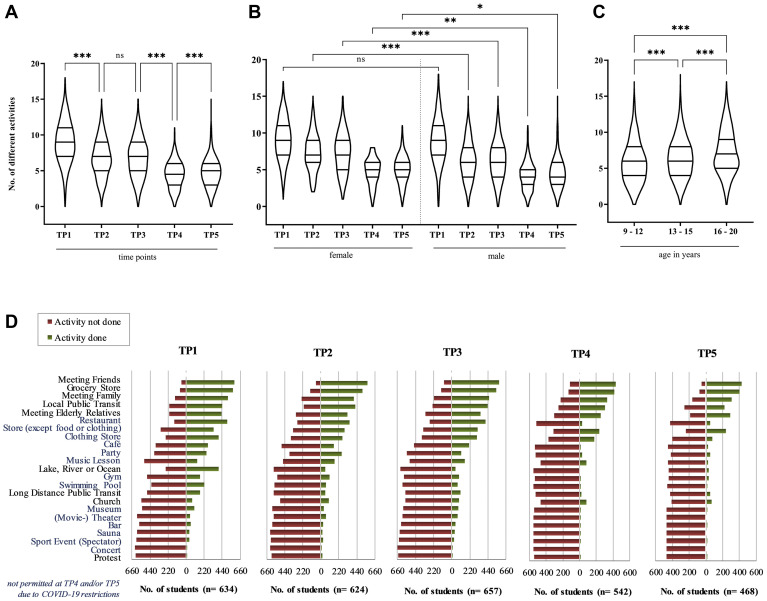
The number of different activities performed by the students decreased with escalating restrictions (Table 1 , Figure 2 A). The lowest level of engagement was seen at TP4, during lockdown, with a decrease in average five activities from TP1 (Table 1: linear mixed regression model, ß(TP4) = −4.7; p < .001). Female students engaged in a higher variety of activities than males, except at TP1 (Table 1, Figure 2B); this was confirmed in a mixed model using an interaction term between sex and TP (data not shown). Adolescents showed a significantly higher number of different activities when compared to younger students (age group 9–12 years) (Table 1, Figure 2C). Escalating state-mandated restrictions from December 2020 on prohibited most leisure activities (e.g., sports, music lessons) and restaurants, retail stores, and cultural institutions stayed closed for several months (Figure A1). For activities which were not permitted at TP4 and/or TP5 due to stricter state-mandated restrictions, the age and sex differences disappeared. It is important to note that significant reductions occurred even in activities that continued to be permitted under the stricter COVID-19 measures at TP4 and TP5, such as grocery shopping, the use of public transit, and (limited) private gatherings, reflecting voluntary behavior (Figure 2D). Meeting other people, e.g., friends and family, was common at all TPs, with adolescents seeing friends more frequently than younger children. Notably, private gatherings were limited by law as infection rates rose; in summer 2020 gatherings of two households were allowed, but this was reduced to one household plus one person in January/February 2021 (Figure A1). Furthermore, shopping of any kind was more common in female and older students (Table A4). Females were more likely to go to a café or (movie-) theater and use local public transit, whereas males were more likely to have visited the gym, a lake, or a professional sporting event. For most individual categories, adolescents engaged in more activities than children; only “going to the swimming pool” and “attending music lessons” were more common in the younger age group (Table A4). The proportion of indoor activity increased continuously from TP0 48.9% (n = 2,778) to TP4 68.0% (n = 1,628) while activities that were exclusively outdoors decreased from 24.2% (n = 1,375) to 7.3% (n = 174). Between TP4 and TP5, as spring approached, this trend was reversed.
Table 1.
Linear mixed regression model for number of different activities
| Covariate | ß | SE | p-value |
|---|---|---|---|
| Intercept | 7.94 | 0.14 | <.001 |
| Time point 2 | −2.30 | 0.095 | < .001 |
| Time point 3 | −2.15 | 0.10 | <.001 |
| Time point 4 | −4.68 | 0.11 | <.001 |
| Time point 5 | −4.23 | 0.11 | <.001 |
| Time point 1 | Reference | ||
| Sex (female) | 0.63 | 0.14 | <.001 |
| Sex (male) | Reference | ||
| Age (13–15 years) | 0.78 | 0.15 | <.001 |
| Age (16–20 years) | 1.51 | 0.17 | <.001 |
| Age (9–12 years) | Reference |
ß, regression coefficient; SE, standard error.
Figure 2.
Activity engagement over time during COVID-19 restrictions. The number of different activities students engaged in shown by time point (TP) (A), sex (B), and age group (C). ∗p < .05, ∗∗p < .01, ∗∗∗p < .001, ns p > .05. Activity engagement by type of activity over time (D). ns, not significant.
Travel patterns
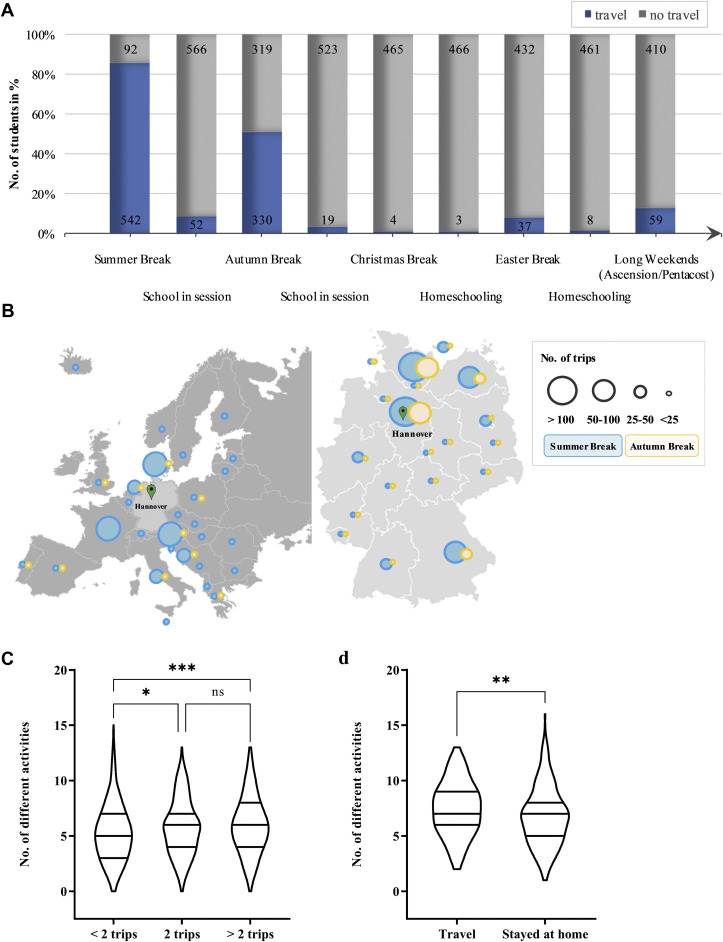
Fewer students travelled during the autumn break than during the summer break (50.8% vs. 85.5%). During both these periods, touristic overnight stays were permitted without restrictions (Figure 3 A, Figure A1). Travelling was rare for Christmas break (0.9%) and Easter break (7.9%), when touristic overnight stays were forbidden due to high COVID-19 incidence (Figure 3A, Figure A1). The average number of trips per student also decreased. In summer, 52.4% (n = 285) of travelers took two trips or more versus 16.1% (n = 54) in autumn. During the summer break, 39.4% (n = 213) of traveling students remained within Germany, 29.5% (n = 159) traveled outside of Germany but within Europe, 29.6% (n = 160) both in Europe and Germany, and 1.5% (n = 8) outside Europe. During the autumn break, fewer students traveled and those who did overwhelmingly remained within Germany (83.1%, n = 271). Notably, most trips were local, with 12.3% (n = 131) of all trips in summer and 21.7% (n = 107) in autumn within Northern Germany (Figure 3B). Most trips were undertaken by car, and holiday rentals were the most popular accommodation during school breaks, both for trips inside and outside Germany (Figure A2). Students who travelled regularly had higher everyday activity levels both during school breaks and when school was in session. Students who travelled more than twice or travelled during autumn break, when the incidence was already rising, also displayed a higher activity engagement while at home, possibly indicating a higher risk tolerance overall (Figure 3C,D).
Figure 3.
Travel patterns. Travel frequencies during school breaks or while school was in session (A). Total number of trips by travel destination for summer and autumn break (B). Number of activities for different travel frequencies (C) and for students either traveled or stayed home in autumn break (D). ∗p < .05, ∗∗p < .01, ∗∗∗p < .001, p > .05. ns, not significant.
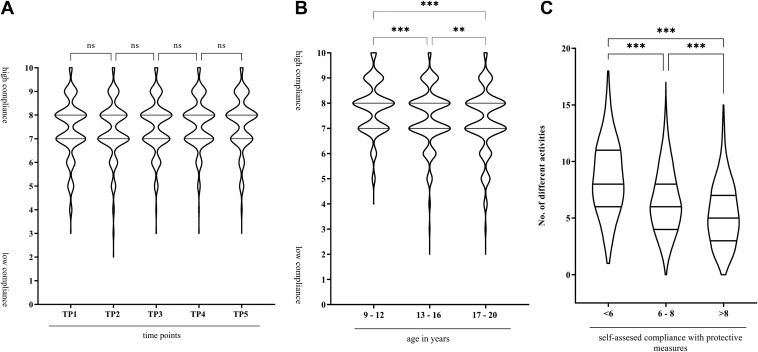
Compliance with protective recommendations
We measured the self-assessed compliance with COVID-19 protective recommendations including social distancing, mask wearing, and hand hygiene on a visual analog scale between 0 and 10. The interquartile range was between seven and eight for all TPs (Figure 4 A). There was no sex difference, but adolescents assigned themselves lower values for compliance than children (Figure 4B). Students assessed their families with higher compliance levels than they awarded themselves (mean difference 0.6, 95% confidence interval 0.5–0.70). Students who assessed their own compliance with lower values were more likely to display higher activity levels (Figure 4C).
Figure 4.
Self-assessment of compliance with COVID-19 measures. Assessment of compliance with protective measures of students by time point (TP) (A) and age groups (B). Correlation of number of activities with different self-assessment in groups (C). ∗∗p < .01, ∗∗∗p < .001, ns p > .05. ns, not significant.
Factors influencing behavior
We performed a mixed model analysis comprising activity engagement, travel, and self-assessed compliance to identify factors that influence students’ behavioral patterns, or predispose certain groups to more cautious behavior (Table A5). Presence or absence of a chronic disease did not influence any of the behavioral parameters we measured, nor did we find differences for specific illnesses such as asthma (Figure A3). To explore the influence of parental education on students’ behavior, we analyzed the profession of adults living in the same household, presumably parents or guardians. Households with two or more college-educated adults travelled more frequently, but did slightly less activities than those with one or no college-educated adult. However, we observed no further association between adults’ profession or educational level and students’ everyday activities or self-assessed compliance (Figure A4). Our cohort included a large proportion of households with adults working in the healthcare industry (16.5% one adult and 6.8% two adults in the household). Interestingly, the healthcare worker status of adults did not affect students’ behavior in any of the examined metrics (Figure A4). Similarly, household size, which ranged from 1 to 10 persons (mean 4.06, SD 1.07) did not affect behavioral patterns.
Discussion
This longitudinal study examined activity engagement, travel patterns, and self-assessed compliance with protective measures in students under escalating, state-mandated COVID-19 restrictions. In the first 7-month period (June to December 2020) in-person schooling was possible, while instruction occurred purely online for 4 1/2 months between January and May 2021. Behavioral patterns, including leisure activities, protective measures, and travel are known to be important factors in determining viral spread [[20], [21], [22]]. Notably, we found significant voluntary behavioral changes in our cohort: even activities that were permitted under stricter COVID-19 measures underwent a significant reduction. Although overall activity engagement decreased, individual behavioral patterns remained consistent under increasing restrictions. For example, while all groups reduced their activity level significantly under restrictions, students with higher activity levels under loose restrictions continued to belong to the higher activity group under lockdown. Our study supports the view that most students are compliant with restrictions [11,23,24], but identifies subsets with higher risk behavioral patterns regarding COVID-19.
Behavioral patterns differed by sex and age. Although self-assessed compliance did not differ between the sexes, females overall engaged in a larger number of different activities than males. Our study did not investigate the underlying causes of behavior. However, we speculate that several factors could be responsible for the observed sex difference in activity engagement. First, societal gender norms may cause female adolescents to help with household tasks such as grocery shopping more often than their male counterparts. Alternatively, a higher index of social interaction and reliance on social support while under stress may cause woman and girls to maintain contact with their social groups more than men and boys [25]. It is relevant to note that the selection of activities was based on the risk of transmission and is skewed toward activities with higher levels of social interaction. These differences may therefore partly reflect that adolescent males engage in more solitary leisure time [26]. Moreover, activities predominantly performed by male students, such as visiting the gym or professional sporting events, were prohibited by the COVID-19 measures (Figure A1), whereas activities that female students reported engaging in (shopping, use of local public transit) were restricted, but not forbidden (Figure A1). Another possibility is differential risk awareness regarding COVID-19, as previous studies highlight the importance of self-perceived risk and the desire to protect others as important motivational factors for compliance [27,28]. Further research exploring the psychological and societal phenomena underlying sex differences in activity engagement by adolescents is merited.
In addition to sex, behavioral patterns differed by age group. Older students engaged in a wider variety of activities than younger ones, and self-assigned themselves lower compliance values. This is consistent with Hommes et al. [29], who report that infection precautions were followed more frequently by primary school students than adolescents, despite higher risk perception in the latter group. Surprisingly, we did not find any differences for factors commonly associated with a higher risk perception. Presence or absence of chronic disease did not correlate with a particular behavior in our cohort. Similarly, students living with an adult healthcare worker did not behave differently from those without family members in a healthcare profession.
Although we identified isolated cases of restriction-flaunting behavior, including 65 individuals (out of 777) who reported attending a party after restrictions forbidding such gatherings were implemented, overall behavior modification in response to restrictions was high. This suggests that escalating restrictions effectively modified the behavior of children and adolescents, refuting claims that adolescents engage in widespread noncompliance with COVID-19 restrictions [30].
The role of in-person schooling in driving viral spread remains controversial [6,7,20]. Contrary to our expectations, infection rates in our cohort were low. We detected only one asymptomatically positive student during in-person instruction. It is interesting to note that 7 of the 13 students who seroconverted during the course of our study did so between TP4 and TP5, a period during which no in-person schooling took place, but community incidence was high. This is consistent with previous German reports showing that in-school transmission is limited, more common in older children, and correlates closely with overall community transmission [31]. School-specific measures such as half-sized classes, fixed cohorts, and staggered breaks to reduce contacts as well as frequent ventilation of classrooms (Figure A1), may explain the low infection rate we observed. The one PCR positive student’s case occurred during a period of increased community infections, underlining the relationship between school and community in viral spread. In England, the risk of an outbreak in an educational setting grew by 72% for every 5 cases per 100,000 increase in the community incidence [32]. At the start of our study period, community transmission was very low, with an average 7-day rolling incidence of 9 cases per 100,000 inhabitants. Not a single participant in our cohort seroconverted over the summer holidays even though 85.4% reported taking at least one trip, amounting to more than 930 trips taken overall. Although traveling was permitted in Europe during the summer due to low infection rates, some evidence suggests that this extensive travel may have driven the second wave of infections in autumn [33]. As testing rates increased simultaneously with the increase in travel activity, the effect of these disparate factors on the rising infection rate remains uncertain [34]. Notably, many participants of our study travelled by car, stayed in holiday rentals, and remained relatively close to home. These travel choices were likely associated with a lower rate of social contacts and therefore lower infection risk and may explain the lack of seroconversion [35,36]. We do not have data on the prepandemic travel behavior of our study participants. However, studies on tourism from before the pandemic indicate higher rates of air travel and hotel usage, suggesting that families adjusted their plans in context of the pandemic [37,38].
Certain limitations must be considered when interpreting our data. First, participation in our study was voluntary, and participants received the results of their tests, potentially skewing our cohort toward those with more concern about COVID-19. Second, factors besides the pandemic influenced student behavior: cold weather in Northern Europe during the autumn and winter months largely preclude certain outdoor activities (e.g., “swimming in a lake, sea, or ocean”). Third, our study focused on a single, large school in a relatively affluent neighborhood, potentially limiting the transferability of our conclusions to other regions and socioeconomic settings. Overall, it is difficult to gauge the generalizability of our findings in Germany to the behavior of teenagers in other countries, as cultural norms and the politicization of pandemic-related protective measures may significantly affect behavioral patterns. Notably, only the final time point (TP5), in June 2021, occurred after the delta variant gained predominance in Germany. The most recent data from Germany’s national Public Health Institute (Robert Koch Institute) show higher in-school transmission rates in the summer of 2021 than in the summer of 2020, likely reflecting the predominance of this highly contagious variant [39]. However, we observed consistent sex and age differences in student behavior over the entire study period, independent of the community incidence or predominant variant of the virus.
Conclusion
Behavioral patterns remained consistent under increasing restrictions with female students engaging in a wider variety of activities than males (except for the first TP, with the lowest community-wide incidence) and older students displaying higher activity levels and lower self-assed compliance values than younger ones. This should be taken into account when implementing infection control measures in schools. Overall, we found a low rate of infection both by pharyngeal swap and antibody test, supporting the view of high compliance with COVID-19 restrictions and protective measures in our cohort. We also demonstrate that state-mandated restrictions result in effective behavior modification in children and adolescents, even in subsets previously displaying higher risk behavior such as frequent travel, high activity levels, and low self-assessed compliance scores. Taken together, our data suggest that in-person learning can occur safely if extensive protective measures are in place and the incidence in the general population remains moderate.
Acknowledgments
The authors gratefully acknowledge the contributions of Beate Günther, Philipp Tups, Katharina Kalinowski, Rita Wonik-Schmidt, Brigitte Naber, and Frank Weinberg for their organizational support at the school.
The authors would like to thank all study participants, including the students, teachers, and staff at the Schillerschule and IGS Roderbruch for their support of the TRAC-19 Study.
The authors also thank Thorsten Saenger, Maxine Swallow, and Andreas Winkel for their logistical support as well as all study personal for their contributions in collecting data and samples.
The study is funded by the Ministry of Science and Culture of Lower Saxony, Germany, refrence number 14-76103-184. The Ministry of Science and Culture had no role in the design and conduct of the study; data collection, management, analysis, or interpretation; or writing of the report.
Footnotes
Conflict of interest: The authors have no conflicts of interest to disclose.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jadohealth.2021.11.021.
Supplementary Data
References
- 1.Measures by the Federal Government to contain the spread of the COVID-19 pandemic and address its impacts. The Federal Government; Berlin, Germany: 2020. [Google Scholar]
- 2.Schilling J., Buda S., Fischer M., et al. [Retrospective classification of distint phases of the COVID-19 pandemic in Germany from the start of the outbreak to Febuary 2021] Epidemiol Bull. 2021;15:3–12. [Google Scholar]
- 3.Langmeyer A., Guglhör-Rudan A., Naab T., et al. Deutsches Jugendinstitut e.V./German Youth Institute; München, Germany: 2020. [Childhood in the Corona Era: Report on the Effect of the Spring 2020 Lockdown on Children] [Google Scholar]
- 4.Nearchou F., Flinn C., Niland R., et al. Exploring the impact of COVID-19 on mental health outcomes in children and adolescents: A Systematic review. Int J Environ Res Public Health. 2020;17:8479. doi: 10.3390/ijerph17228479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ezeoke O., Kanaley M., Brown D., et al. The impact of COVID-19 on adolescent Wellness. Pediatrics. 2021;147:224–225. [Google Scholar]
- 6.Balancing the risks of Pupils returning to schools: DELVE Report No. 4. The DELVE Initiative; London, UK: 2020. [Google Scholar]
- 7.Fantini M.P., Reno C., Biserni G.B., et al. COVID-19 and the re-opening of schools: A policy maker's dilemma. Ital J Pediatr. 2020;46:79. doi: 10.1186/s13052-020-00844-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Felsenstein S., Hedrich C.M. SARS-CoV-2 infections in children and young people. Clin Immunol. 2020;220:108588. doi: 10.1016/j.clim.2020.108588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhu Y., Bloxham C.J., Hulme K.D., et al. A meta-analysis on the role of children in SARS-CoV-2 in household transmission clusters. Clin Infect Dis. 2021;72:e1146–e1153. doi: 10.1093/cid/ciaa1825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mossong J., Hens N., Jit M., et al. Social contacts and mixing patterns relevant to the spread of infectious diseases. Plos Med. 2008;5:e74. doi: 10.1371/journal.pmed.0050074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nivette A., Ribeaud D., Murray A., et al. Non-compliance with COVID-19-related public health measures among young adults in Switzerland: Insights from a longitudinal cohort study. Soc Sci Med. 2021;268:113370. doi: 10.1016/j.socscimed.2020.113370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Macartney K., Quinn H.E., Pillsbury A.J., et al. Transmission of SARS-CoV-2 in Australian educational settings: A prospective cohort study. Lancet Child Adolesc Health. 2020;4:807–816. doi: 10.1016/S2352-4642(20)30251-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Varma J.K., Thamkittikasem J., Whittemore K., et al. COVID-19 infections among students and staff in New York City public schools. Pediatrics. 2021;147 doi: 10.1542/peds.2021-050605. e2021050605. [DOI] [PubMed] [Google Scholar]
- 14.Yung C.F., Kam K.Q., Nadua K.D., et al. Novel coronavirus 2019 transmission risk in educational settings. Clin Infect Dis. 2021;72:1055–1058. doi: 10.1093/cid/ciaa794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.State of lower Saxony – Current case numbers. https://www.niedersachsen.de/Coronavirus/Niedersachsen_Aktuelle_Fallzahlen Available at:
- 16.Corman V.M., Landt O., Kaiser M., et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25:2000045. doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoffmann M., Kleine-Weber H., Schroeder S., et al. SARS-CoV-2 Cell entry Depends on ACE2 and TMPRSS2 and is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020;181:271–280.e278. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu C., Cao D., Chen P., Zagar T. Eli Lilly & Company; Indianapolis, IN: 2007. RANDOM and REPEATED statements - How to Use Them to model the Covariance Structure in Proc mixed. [Google Scholar]
- 19.Sheu C-f. Regression analysis of correlated binary outcomes. Behav Res Methods Instrum Comput. 2000;32:269–273. doi: 10.3758/bf03207794. [DOI] [PubMed] [Google Scholar]
- 20.COVID-19 in children and the role of school settings in transmission - first update. European Centre for Disease Prevention and Control (ECDC); Stockholm, Sweden: 2020. [Google Scholar]
- 21.Hobbs C.V., Martin L.M., Kim S.S., et al. Factors associated with positive SARS-CoV-2 test results in Outpatient health Facilities and Emergency Departments among children and adolescents aged <18 Years - Mississippi, September-November 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1925–1929. doi: 10.15585/mmwr.mm6950e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Burns J., Movsisyan A., Stratil J.M., et al. Travel-related control measures to contain the COVID-19 pandemic: A rapid review. Cochrane Database Syst Rev. 2020;10:CD013717. doi: 10.1002/14651858.CD013717. [DOI] [PubMed] [Google Scholar]
- 23.Soest T.V., Pedersen W., Bakken A., Sletten M.A. Compliance with infection control rules among adolescents in Oslo during the COVID-19 pandemic. Tidsskr Nor Laegeforen. 2020;140 doi: 10.4045/tidsskr.20.0449. [DOI] [PubMed] [Google Scholar]
- 24.Dardas L.A., Khalaf I., Nabolsi M., et al. Developing an Understanding of adolescents' Knowledge, Attitudes, and Practices toward COVID-19. J Sch Nurs. 2020;36:430–441. doi: 10.1177/1059840520957069. [DOI] [PubMed] [Google Scholar]
- 25.Buhrke R.A., Fuqua D.R. Sex differences in same- and cross-sex supportive relationships. Sex Roles. 1987;17:339–352. [Google Scholar]
- 26.Bradley G.L., Inglis B.C. Adolescent leisure dimensions, psychosocial adjustment, and gender effects. J Adolesc. 2012;35:1167–1176. doi: 10.1016/j.adolescence.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 27.Oosterhoff B., Palmer C.A., Wilson J., Shook N. Adolescents' Motivations to engage in social distancing during the COVID-19 pandemic: Associations with mental and social health. J Adolesc Health. 2020;67:179–185. doi: 10.1016/j.jadohealth.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang X.Y., Gong R.N., Sassine S., et al. Risk perception of COVID-19 infection and Adherence to preventive measures among adolescents and young adults. Children (Basel) 2020;7:311. doi: 10.3390/children7120311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hommes F., Wv Loon, Thielecke M., et al. SARS-CoV-2 infection, risk perception, behaviour, and preventive measures at schools in Berlin, Germany, during the early post-lockdown phase: A cross-sectional study. Int J Environ Res Public Health (Online) 2020;18:2739. doi: 10.3390/ijerph18052739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Press Conference by Chancellor Merkel, Berlin mayor Müller and Minister of Bavaria Söder after the Conference between the Chancellors and the state Govenors on October 14th. 2020. https://www.bundeskanzlerin.de/bkin-de/aktuelles/pressekonferenz-von-bundeskanzlerin-merkel-dem-regierenden-buergermeister-mueller-und-ministerpraesident-soeder-nach-der-besprechung-der-bundeskanzlerin-mit-den-regierungschefinnen-und-regierungschefs-der-laende Available at:
- 31.Buchholz U., Lehfeld A., Otte im Kampe E., et al. [Epidemiology of COVID-19 in a school setting] Epidemiol Bull. 2021;13:23–36. [Google Scholar]
- 32.Ismail S.A., Saliba V., Lopez Bernal J., et al. SARS-CoV-2 infection and transmission in educational settings: A prospective, cross-sectional analysis of infection clusters and outbreaks in England. Lancet Infect Dis. 2021;21:344–353. doi: 10.1016/S1473-3099(20)30882-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Plümper T., Neumayer E. Summer school holidays and the Growth rate in Sars-CoV-2 infections across German Districts. medRxiv. 2020 doi: 10.1101/2020.10.11.20210773. [DOI] [Google Scholar]
- 34.Frank C., Hellenbrand W., Sievers C. [Report on travel-associated COVID-19 cases in the summer of 2020 in the context of school breaks, trips and testing capacity] Epidemiol Bull. 2021;8:10–23. [Google Scholar]
- 35.Barbieri D.M., Lou B., Passavanti M., et al. Impact of COVID-19 pandemic on mobility in ten countries and associated perceived risk for all transport modes. PLoS One. 2021;16:e0245886. doi: 10.1371/journal.pone.0245886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shi P., Keskinocak P., Swann J.L., Lee B.Y. The impact of mass gatherings and holiday traveling on the course of an influenza pandemic: A computational model. BMC Public Health. 2010;10:778. doi: 10.1186/1471-2458-10-778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Domestic Travel Patterns in Germany. Deutsche Zentrale für Tourismus e.V. (DZT))/German Center for Tourism; Comissioned by the Federal Ministry for Economic Affairs and Energy; Frankfurt a.M./Berlin: 2013. [Google Scholar]
- 38.[Analysis 2021 by the Foundation for Future studies – Travel Report 2020] http://www.tourismusanalyse.de/zahlen/daten/statistik/tourismus-urlaub-reisen/2021/reisebilanz-2020/ Available at:
- 39.[Weekly status report of the RKI to coronavirus disease-2019 (COVID-19) 07.10.2021] https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/Wochenbericht/Wochenbericht_2021-10-07.pdf?__blob=publicationFile Available at:
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.