Abstract
Depression is a prevalent psychiatric disorder that often leads to poor quality of life and impaired functioning. Treatment during the acute phase of a major depressive episode aims to help the patient reach a remission state and eventually return to their baseline level of functioning. Pharmacotherapy, especially selective serotonin reuptake inhibitors antidepressants, remains the most frequent option for treating depression during the acute phase, while other promising pharmacological options are still competing for the attention of practitioners. Depression-focused psychotherapy is the second most common option for helping patients overcome the acute phase, maintain remission, and prevent relapses. Electroconvulsive therapy is the most effective somatic therapy for depression in some specific situations; meanwhile, other methods have limits, and their specific indications are still being studied. Combining medications, psychotherapy, and somatic therapies remains the most effective way to manage resistant forms of depression.
Keywords: Depression, Treatment, Antidepressants, Psychotherapy, Cognitive-behavioral therapy, Somatic therapies, Electroconvulsive therapy
Core Tip: Depression is a persistent public health problem for which treatments must be codified and simplified to enhance current practice. Several therapies have been suggested worldwide, with varying levels of validity. This article explores effective and valid therapies for treating depression by addressing current and future research topics for different treatment categories.
INTRODUCTION
Depression is a common psychiatric disorder and a major contributor to the global burden of diseases. According to the World Health Organization, depression is the second-leading cause of disability in the world and is projected to rank first by 2030[1]. Depression is also associated with high rates of suicidal behavior and mortality[2].
Treatments administered during the acute phase of a major depressive episode aim to help the patient reach a remission state and eventually return to their baseline level of functioning[3]. Acute-phase treatment options include pharmacotherapy, depression-focused psychotherapy, combinations of medications and psychotherapy, and somatic therapies such as electroconvulsive therapy (ECT). Nevertheless, managing the acute phase of depression is only the first step in a long therapy process that aims to maintain remission and prevent relapses. In this article, we discuss various treatment options implemented by clinicians, highlighting the role that each option plays in actual psychiatric practice.
PHARMACOTHERAPY
While selective serotonin reuptake inhibitors (SSRIs) remain the gold-standard treatment for depression, new antidepressants are always being developed and tested. The ultimate goal is to discover a molecule that exhibits quick effectiveness with as few side effects as possible.
Daniel Bovet studied the structure of histamine (the causative agent in allergic responses) to find an antagonist, which was finally synthesized in 1937[4]. Since then, many researchers have studied the link between the structures and activities of different antihistaminic agents, contributing to the discovery of almost all antidepressants[5].
In the following subsections, we list the main classes of antidepressants in chronological order of apparition, highlighting the most widely used molecules in daily psychiatric practice.
Monoamine oxidase inhibitors
Iproniazid was the first drug defined as an antidepressant; it was later classified as a monoamine oxidase inhibitor (MAOI)[6,7]. Several other MAOIs have been introduced since 1957[8]. Due to their irreversible inhibition of monoamine oxidase, MOAIs have numerous side effects, such as hepatotoxicity and hypertensive crises, that can lead to lethal intracranial hemorrhages. Consequently, MAOIs have become less commonly used over time[9].
Trials have demonstrated that MAOIs’ efficacy is comparable to that of tricyclic antidepressants (TCAs)[10,11]. However, considering MAOIs’ drug interactions, dietary restrictions, and potentially dangerous side effects, they are now almost exclusively prescribed for patients who have not responded to several other pharmacotherapies, including TCAs[9]. Furthermore, MAOIs have demonstrated specific efficacy in treating depression with atypical features, such as reactive moods, reverse neuro-vegetative symptoms, and sensitivity to rejection[12].
MAOIs are also a potential therapeutic option when ECT is contraindicated[13]. MAOIs’ effectiveness is still unclear for treating depression in patients who are resistant to multiple sequential trials with SSRIs and serotonin-norepinephrine reuptake inhibitors (SNRIs)[14]. Nevertheless, psychiatrists’ use of MAOIs has declined over the years[15,16]. The use of MAOIs is generally restricted to patients who do not respond to other treatments.
TCAs
The first TCA was discovered and released for clinical use in 1957 under the brand name Tofranil[5,17]. Since then, TCAs have remained among the most frequently prescribed drugs worldwide[9]. TCAs-such as amitriptyline, nortriptyline, protriptyline, imipramine, desipramine, doxepin, and trimipramine-are about as effective as other classes of antidepressants-including SSRIs, SNRIs, and MAOIs-in treating major depression[18,19].
However, some TCAs can be more effective than SSRIs when used to treat hospitalized patients[20]. This efficacy can be explained by the superiority of TCAs over SSRIs for patients with severe major depressive disorder (MDD) symptoms who require hospitalization[21-24]. However, no differences have been detected in outpatients who are considered less severely ill[18,20]. In most cases, TCAs should generally be reserved for situations when first-line drug treatments have failed[25].
SSRIs
In December 1987, a series of clinical studies confirmed that an SSRI called fluoxetine was as effective as TCAs for treating depression while causing fewer adverse effects[26]. After being released onto the market, its use expanded more quickly than that of any other psychotropic in history. In 1994, it was the second-best-selling drug in the world[7].
Currently available SSRIs include fluoxetine, sertraline, paroxetine, fluvoxamine, citalopram, and escitalopram. They have elicited different tolerance rates and side effects-mostly sexual and digestive (nausea and loss of appetite), as well as irritability, anxiety, insomnia, and headaches[27]. Nevertheless, SSRIs have a good tolerability profile[28].
In most systematic reviews and meta-analyses, SSRIs have demonstrated comparable efficacy to TCAs[18,19,29], and there is no significant evidence indicating the superiority of any other class or agent over SSRIs[29-31]. Furthermore, studies show no differences in efficacy among individual SSRIs[29,31-34]. Therefore, most guidelines currently recommend SSRIs as the first-line treatment for patients with major depression[25].
Norepinephrine reuptake inhibitors
Other monoamine (norepinephrine, serotonin, and dopamine) neurotransmitter reuptake inhibitors called SNRIs emerged during the 1990s to protect patients against the adverse effects of SSRIs[35]. Currently available SNRIs are venlafaxine, desvenlafaxine (the principal metabolite of venlafaxine), and duloxetine. The extended-release form of venlafaxine is the most commonly used drug in this class. Clinical guidelines commonly recommend prescribing SNRI to patients who do not respond to SSRIs[25].
In individual studies, venlafaxine and duloxetine are generally considered effective as SSRIs[36]. Also, venlafaxine’s efficacy is comparable to that of TCAs[37,38].
According to some meta-analyses, reboxetine (a selective noradrenaline reuptake inhibitor) seems less efficacious than SSRIs[39]. However, these findings could be due to the relatively poor tolerance of reboxetine[40].
Other antidepressants
Trazodone is the oldest medication of the so-called “other antidepressants” group that is still in wide use[41,42]. It has been shown to be an effective antidepressant in placebo-controlled research. However, in contemporary practice, it is much more likely to be used in low doses as a sedative-hypnotic than as an antidepressant[41,42].
Nefazodone’s structure is analogous to that of trazodone, though it has different pharmacological properties[43]. Its efficacy and overall tolerability are comparable to those of SSRIs, as indicated by comparative trials[43]. However, its use is associated with rare (but fatal) cases of clinical idiosyncratic hepatotoxicity[44].
Bupropion’s mechanism of action remains unclear, though it is classified as a norepinephrine and dopamine reuptake inhibitor[45]. It appears to have a more activating profile than SSRIs that are modestly superior to bupropion in patients with MDD[46]. However, for individuals with low to moderate levels of anxiety, the efficacy of bupropion in treating MDD is comparable to that of SSRIs[46]. Moreover, bupropion has a better tolerability profile than SSRIs, with minimal weight gain (or even leading to weight loss)[46]. In addition, bupropion is more likely than some SSRIs to improve symptoms of fatigue and sleepiness[47].
Mirtazapine and mianserin are tetracyclic compounds believed to increase the availability of serotonin or norepinephrine (or both), at least initially. Mirtazapine’s ability to antagonize serotoninergic subtypes receptors, <5-HT2A> and <5-HT2C>, could also increase norepinephrine and dopamine release in cortical regions[25]. Mirtazapine is about as effective as SSRIs[48].
Recently, drugs have been developed that block serotonin reuptake while affecting a variety of 5-HT receptor subtypes. The advantages of these agents (e.g., vilazodone and vortioxetine) over SSRIs are not fully clear. However, they appear to produce less sexual dysfunction and, in the specific case of vortioxetine, have particular benefits in depression-related cognitive impairment[49]. Indeed, vortioxetine is a very recent antidepressant with a multimodal mechanism that is thought to have a high affinity for serotonin transporters and 5-HT3, 5HT1A, 5HT7 receptors. Such a specific profile seems to indicate a level of efficacy to other antidepressants with a specific action on cognitive impairments[50,51].
In conclusion, no significant differences have been found between different classes of antidepressants in terms of their efficacy[52], though some drugs show some weak-to-moderate evidence indicating they are more effective than some other drugs[53]. Concerning the acceptability of these drugs, citalopram, escitalopram, fluoxetine, sertraline, and vortioxetine have been deemed more tolerable than other antidepressants, whereas amitriptyline, clomipramine, duloxetine, fluvoxamine, trazodone, and venlafaxine had the highest dropout rates[53] because of their more frequent and severe side effects. Nausea and vomiting were the most common reasons for treatment discontinuation; sexual dysfunction, sedation, priapism, and cardiotoxicity were also reported[31,41].
Ketamine and related molecules
In intravenous sub-anesthetic doses, ketamine has very quick effects on resistant unipolar (and, possibly, bipolar) depression and acute suicidal ideation[54,55]. The antidepressant effect of ketamine can persist for several days but eventually wanes. A few reports are have cited oral and intranasal formulations of ketamine for treatment-resistant depression[56,57], but there is still no data about the potential link between the onset of action and the route of administration.
Common adverse effects of ketamine include dizziness, neurotoxicity, cognitive dysfunction, blurred vision, psychosis, dissociation, urological dysfunction, restlessness, headache, nausea, vomiting, and cardiovascular symptoms[58]. Such adverse effects tend to be brief in acute, low-dose treatments[36], whereas prolonged exposure may predispose patients to neurotoxicity and drug dependence[56]. Lastly, since ketamine is associated with a higher risk of drug abuse and addiction, it cannot be recommended in daily clinical practice[59,60].
Ketamine is not a miracle drug, and many important factors still need to be defined, such as the most effective dose and the optimal administration route[61,62]. The current lack of guidelines about the therapeutic monitoring of ketamine treatment for depression further complicates the expanding use of this treatment[56]. Even though ketamine might never reach the market, it has stimulated research in the neurobiology of depression, including studies on potential fast and long-lasting antidepressants.
Ketamine has an active metabolite (hydroxynorketamine) that can produce rapid and sustained glutamatergic stimulation. It also seems to be free of many of the safety problems associated with ketamine and, thus, should be studied.
Research on the S-enantiomer of ketamine (S-ketamine, or esketamine, especially intranasal) could also be valuable, as it has a 3 to 4 times greater affinity than ketamine for the N-methyl-D-aspartate (NMDA) receptor[40]. It was approved by the United States Food and Drug Administration in March 2019 for treatment-resistant depression. However, current knowledge about the effects of prolonged esketamine therapy is still preliminary. In addition, regarding the potential risk of abuse, esketamine use must be carefully monitored[63-65].
Other glutamate receptor modulators have been evaluated in small studies as monotherapy agents or as adjuncts to other antidepressants. Examples include noncompetitive NMDA receptor antagonists (memantine, dextromethorphan/quinidi-ne, dextromethorphan/bupropion, and lanicemine), NR2B subunit-specific NMDA receptor antagonists (traxoprodil), NMDA receptor glycine site partial agonists (D-cycloserine, rapastinel), and metabotropic glutamate receptor antagonists (basimglurant, declogurant)[66-68] (Table 1).
Table 1.
Main classes of antidepressants with their date of approval, contributions, and disadvantages
|
Product
|
Date of FDA1 approval
|
Contributions
|
Disadvantages
|
|
| MAOI 2 | Iproniazid | 1958 | Confirmed the role of monoaminergic transmission in depression | Drug interactions, dietary restrictions |
| Led to a new search methodologies to develop new antidepressants | Hepatotoxicity and hypertensive crises | |||
| TC 3 | Imipramine | 1959 | Efficacy in patients with more severe symptoms of MDD | Cardiovascular toxicity and anticholinergic side effects. Risk of lethal toxicity from overdoses |
| Desipramine | ||||
| Nortriptyline | 1992 | |||
| Amitriptyline | 1961 | |||
| Clomipramine | Not approved | |||
| First tetracyclicmaprotiline | ||||
| SSRI 4 | Fluoxetine | 1987 | Improved tolerability | Several minor side effects (sexual dysfunction, loss of appetite, vomiting, nausea, irritability, anxiety, insomnia, and headache). Paroxetine had the highest rate of sexual dysfunction. Fluvoxamine is associated with the most overall adverse events |
| Citalopram | 1998 | |||
| Fluvoxamine | 2007 | |||
| Paroxetine | 1992 | |||
| Escitalopram | 2002 | |||
| Sertraline | 1999 | |||
| SNRI 5 | Venlafaxine | 2008 | Commonly recommended for patients who do not respond to SSRIs | No improvement in efficacy. Lower tolerability (highest rates of nausea, vomiting, and sexual dysfunction) |
| Duloxetine | 2004 | |||
| Reboxetine | Not approved | |||
| Other antidepressants | Trazodone | 1981 | Comparable efficacy to SSRIs | High rate of somnolence |
| Nefazodone | 2003 | Rare but fatal hepatotoxicity | ||
| Bupropion | 2003 | A better tolerability profile (minimal weight gain or even weight loss). Likely to improve symptoms of fatigue and sleepiness | May increase risk for seizures (low evidence) | |
| Vortioxetine | 2013 | Efficacy in elderly patients. Supposed cognitive-enhancing properties. Safety profile is similar to SSRIs | The most commonly reported adverse effect was nausea | |
| Vilazodone | 2011 | Less sexual dysfunction (low evidence). Safety profile is similar to SSRIs | The most commonly reported adverse effects were diarrhea and nausea | |
| Mirtazapine | 1997 | Comparable efficacy to SSRIs. Low risk of sexual dysfunction | Weight gain | |
| Ketamine and related drugs | Ketamine | Not approved | Rapid effects on resistant depression and acute suicidal ideation | Short antidepressant effect. Possible neurotoxicity and drug dependence |
| Esketamine | 2019 | Treatment-resistant depression. Greater affinity for NMDA receptor than ketamine | Potential risk of abuse. Lack of hindsight | |
United States Food and Drug Administration.
Monoamine oxidase inhibitors.
Tricyclic antidepressant.
Selective serotonin reuptake inhibitors.
Serotonin-norepinephrine reuptake inhibitors.
NMDA: N-methyl-D-aspartate; SSRI: DSelective serotonin reuptake inhibitors; MDD: Major depressive disorder; MAOI: Monoamine oxidase inhibitor.
Perspectives
A purely neurotransmitter-based explanation for antidepressant drug action-especially serotonin-inhibiting drugs-is challenged by the significant percentage of patients who never achieve full remission[6] and the delayed clinical onset, which varies from two to four weeks. Moreover, studies show an acute increase in monoamines in the synaptic cleft immediately following treatment[69], even when the depletion of tryptophan (serotonin’s precursor) does not induce depressive-like behavior in healthy humans[70,71].
This finding shows that research on the pharmacological options for treating depression must go beyond monoaminergic neurotransmission systems. Research on the development of new antidepressants should explore several mechanisms of action on several types of receptors: Antagonism, inhibition of the reuptake of neurotransmitters, and modulators of glutamate receptors, as well as interactions with α-amino-3-acid receptors, hydroxy-5-methyl-4-isoxazolepropionic, brain-derived neurotrophic factor, tyrosine kinase B receptor (the mechanistic target of rapamycin), and glycogen synthase kinase-3[72].
Identifying the cellular targets of rapid-acting agents like ketamine could help practitioners develop more effective antidepressant molecules by revealing other receptors involved in gamma-aminobutyric acid regulation and glutamate transmission[73].
PSYCHOTHERAPY
Psychotherapeutic interventions are widely used to treat and prevent most psychiatric disorders. Such interventions are common in cases of depression, psychosocial difficulties, interpersonal problems, and intra-psychic conflicts. The specific psychotherapy approach chosen for any given case depends on the patient’s preference, as well as on the clinician’s background and availability[74]. Psychotherapy for patients with depression strengthens the therapeutic alliance and enables the patient to monitor their mood, improve their functioning, understand their symptoms better, and master the practical tools they need to cope with stressful events[75]. The following subsections briefly describe psychotherapeutic interventions that have been designed specifically for patients with depression.
Overview of psychotherapy in depression
Depression-focused psychotherapy is typically considered the initial treatment method for mild to moderate MDD. Based on significant clinical evidence, two specific psychotherapeutic methods are recommended: Cognitive-behavioral therapy (CBT) and interpersonal therapy (IPT). Supportive therapy (ST) and psychoeducational intervention (PEI) have also been recommended, those the evidence supporting these methods s not as strong. In more cases of severe depression, ST and PEI are used only to augment pharmacological treatments.
After remission, CBT, PEI, and mindfulness-based cognitive therapy (MBCT) are proposed to maintain and prevent depression. However, when psychotherapy has been effective during the initial phases of a depressive episode, it should be continued to maintain remission and prevent relapses while reducing the frequency of sessions[25,75,76].
Specific and intensive psychotherapeutic support is recommended for patients with chronic depression because of high rates of comorbidity with personality disorders, early trauma, and attachment deficits. The European Psychiatric Association recommends using the Cognitive Behavioral Analysis System of Psychotherapy (CBASP) for treating chronic depression and utilizing specific approaches suited to each patient’s preferences[77]. All these therapeutic options are summarized in Figure 1.
Figure 1.
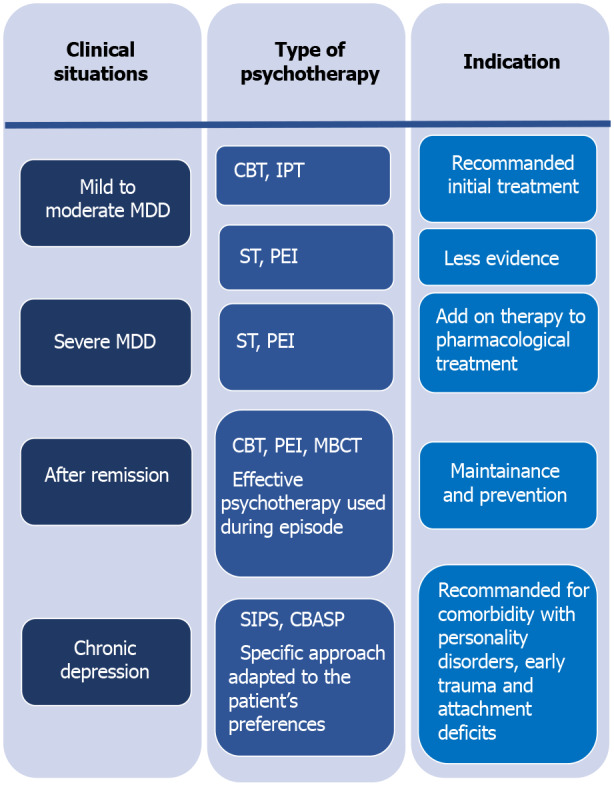
Overview of psychotherapy in different clinical situations of depression. MDD: Major depressive disorder; CBT: Cognitive-behavioral therapy; IPT: Interpersonal therapy; ST: Supportive therapy; PEI: Psycho-educational intervention; MBCT: Mindfulness based cognitive therapy; SIPS: Specific and intensive psychotherapeutic support; CBASP: Cognitive Behavioral Analysis System of Psychotherapy.
Structured psychotherapies
Cognitive and behavioral therapies: Based on robust evidence, CBT is one of the most well-documented and validated psychotherapeutic methods available. Interventional strategies are based on modifying dysfunctional behaviors and cognitions[77]. CBT targets depressed patients’ irrational beliefs and distorted cognitions that perpetuate depressive symptoms by challenging and reversing them[3]. Thus, CBT is a well-known effective treatment method for MDD[78] and has been recommended in most guidelines as a first-line treatment[79-81].
However, the effectiveness of CBT depends on patient’s capacity to observe and change their own beliefs and behaviors. Some simple techniques were developed to overcome this issue, especially in primary care management. Behavioral activation is one such technique, consisting of integrating pleasant activities into daily life to increase the number and intensity of the positive interactions that the patient has with their environment[82,83].
Acceptance and commitment therapy is another form of CBT. This type of therapy, which is based on functional contextualism, can help patients accept and adjusting to persistent problems. It appears to be effective in reducing depressive symptoms and preventing relapses[77,84].
Another form of CBT is computerized CBT (CCBT), implemented via a computer with a CD-ROM, DVD, or online CCBT, allowing patients to benefit from this therapy under conditions of reduced mobility, remoteness, confinement, or quarantine[79].
CCBT and guided bibliotherapy based on CBT could be considered for self-motivated patients with mild to moderate major depression or as a complementary treatment to pharmacotherapy[25]. CBT is also recommended for patients with resistant depression in combination with antidepressants[85].
Schema therapy is another CBT-derived therapy that can be used in patients who have failed classical CBT, like patients with personality disorder comorbidity. Schema therapy is about as effective as CBT for treating depression[86]. In adolescent patients with depression, CBT is also a recommended option with plenty of evidence from multiple trials. Meanwhile, it remains the first-line treatment in children despite mixed findings across trials[87]. CBT is also a promising option for elderly depressed patients, though substantial evidence is still lacking because of the limited data on the subject[88].
IPT: The goal of IPT is to identify the triggers of depressive symptoms or episodes. These triggers may include losses, social isolation, or difficulties in social interactions. The role of the intervention is to facilitate mourning (in the case of bereavement), help the patient recognize their own affect, and resolve social interaction dysfunction by building their social skills and social supports[89]. IPT, like CBT, is a first-line treatment for mild to moderate major depressive episodes in adults; it is also a well-established intervention for adolescents with depression[25].
Problem-solving therapy: The problem-solving therapy (PST) approach combines cognitive and interpersonal elements, focusing on negative assessments of situations and problem-solving strategies. PST has been used in different clinical situations, like preventing depression among the elderly and treating patients with mild depressive symptoms, especially in primary care. Despite its small effect sizes, PST is comparable to other psychotherapeutic methods used to treat depression[88,90].
Marital and family therapy: Marital and family therapy (MFT) is effective in treating some aspects of depression. Family therapy has also been used to treat severe forms of depression associated with medications and hospitalization[91]. Marital and family problems can make people more vulnerable to depression, and MFT addresses these issues[92]. Marital therapy includes both members of the couple, as depression is considered in an interpersonal context in such cases. Some of the goals of this therapy are to facilitate communication and resolve different types of marital conflict. Family therapy uses similar principles as other forms of therapy while involving all family members and considering depression within the context of pathological family dynamics[93].
ST: Although ST is not as well-structured or well-evaluated as CBT or IPT, it is still commonly used to support depressed patients. In addition to sympathetic listening and expressing concern for the patient’s problems, ST requires emotionally attuned listening, empathic paraphrasing, explaining the nature of the patient’s suffering, and reassuring and encouraging them. These practices allow the patient to ventilate and accept their feelings, increase their self-esteem, and enhance their adaptive coping skills[94].
Psychodynamic therapy: Psychodynamic therapy encompasses a range of brief to long-term psychological interventions derived from psychoanalytic theories. This type of therapy focuses on intrapsychic conflicts related to shame, repressed impulses, problems in early childhood with one’s emotional caretakers that lead to low self-esteem and poor emotional self-regulation[93,95]. Psychodynamic therapy’s efficacy in the acute phase of MDD is well-established compared to other forms of psychotherapy.
Group therapy: The application of group therapy (GT) to MDD remains limited. Some data support the efficacy of specific types of GT inspired by CBT and IPT[96-98]. Group CBT for patients with subthreshold depression is an effective post-depressive-symptomatology treatment but not during the follow-up period[99]. Supportive GT and group CBT reduce depressive symptoms[96], especially in patients with common comorbid conditions[100]. However, studies are still lacking in this domain.
MBCT: MBCT is a relatively recent technique that combines elements of CBT with mindfulness-based stress reduction[101]. Studies have shown that eight weeks of MBCT treatment during remission reduces relapse. Thus, it is a potential alternative to reduce, or even stop, antidepressant treatment without increasing the risk of depressive recurrence, especially for patients at a high risk of relapse (i.e., patients with more than two previous episodes and patients who have experienced childhood abuse or trauma)[102].
Other psycho-interventions
Psycho-education: This type of intervention educates depressed patients and (with their permission) family members involved in the patient’s life about depression symptoms and management. This education should be provided in a language that the patient understands. Issues such as misperceptions about medication, treatment duration, the risk of relapse, and prodromes of depression should be addressed. Moreover, patients should be encouraged to maintain healthy lifestyles and enhance their social skills to prevent depression and boost their overall mental health. Many studies have highlighted the role of psycho-education in improving the clinical course, treatment adherence, and psychosocial functioning in patients with depression[103].
Physical exercise: Most guidelines for treating depression, including the National Institute for Health and Care Excellence, the American Psychiatric Association, and the Royal Australian and New Zealand College of Psychiatrists, recommend that depressed patients perform regular physical activity to alleviate symptoms and prevent relapses[104]. Exercise also promotes improvements in one’s quality of life in general[105]. However, exercise is considered an adjunct to other anti-depressive treatments[25].
Although psychotherapy is effective for treating depression and improving patients’ quality of life, its direct actions against depressive symptoms are not fully understood[106]. Identifying factors (e.g., interpersonal variables) linked to treatment responses can help therapists choose the right therapeutic strategy for each patient and guide research to modify existing therapies and develop new ones[107].
Since depression is a primary care problematic, simplifying psychotherapy procedures will increase the use of psychological interventions for depression, especially in general practice. Brief forms (six to eight sessions) of CBT and PST have already shown their effectiveness for treating depression[108]. Nevertheless, simpler solutions must be made available to practitioners to help them manage and prevent depression.
SOMATIC TREATMENTS
In many situations, depression can also be managed via somatic treatments. ECT is the most well-known treatment for resistant depression, and solid evidence supports its effectiveness and safety. In recent decades, various innovative techniques have been proposed, such as repetitive transcranial magnetic stimulation (rTMS), transcranial direct current stimulation (tDCS), vagus nerve stimulation (VNS), deep brain stimulation (DBS), and magnetic seizure therapy, with varying efficiency levels[109].
ECT
ECT is arguably the most effective treatment modality in psychiatry, and its superiority over pharmacotherapy for major unipolar depression is widely supported[110]. ECT reduces the number of hospital readmissions and lightens the burden of depression, leading to a better quality of life[111,112].
Moreover, ECT is considered safe[113]. Advances in anesthesia and ECT techniques have decreased complications related to ECT while also improving cognitive outcomes and patient satisfaction.
However, the stigma surrounding ECT limits its use. Most misconceptions date back to early ECT techniques (when it was performed without muscle relaxants or anesthesia). Nevertheless, some people still consider ECT as the last option for treating depression, even though most studies indicate that ECT is more beneficial in patients with fewer pharmacological treatments[114-116].
ECT is typically recommended for patients with severe and psychotic depression, a high risk of suicide, or Parkinson’s disease, as well as pregnant patients[117-119]. The maintenance ECT also appears to prevent relapses[120]. The current practice of ECT continues to improve as protocols become more advanced, mainly owing to bioinformatics, and as more research is carried out in this domain[121-125].
rTMS
This method, which is a type of biological stimulation that affects brain metabolism and neuronal electrical activity, has been widely used in research on depression[126]. Recent literature shows a significant difference between rTMS and fictitious stimulation regarding its improvements in depressive symptoms[127]. Preliminary research has revealed synergistic (e.g., rTMS/quetiapine) and antagonizing (e.g., rTMS/cannabinoid receptor (CB1) antagonist) interactions between neuro-modulation and pharmacotherapy[128]. Treatments combining rTMS and antidepressants are significantly more effective than placebo conditions, with mild side effects and good acceptability[129]. Although these results are encouraging, they remain inconsistent due to differences in rTMS treatment frequencies, parameters, and stimulation sites[129]. Therefore, clinical trials with large sample sizes are needed to specify which factors promote favorable therapeutic responses. Also, additional preclinical research should investigate the synergistic effects of other pharmacological molecules and guide integrated approaches (rTMS plus pharmacotherapy).
tDCS
This technique delivers weak currents to the brain via electrodes placed on the scalp[130]. It is easy to use, safe, and tolerable[131]. The tDCS technique significantly outperforms the simulator in terms of the rate of response and remission[132]. However, its effect remains lower than that of antidepressants[133] and rTMS[134]. It can be used as a complementary intervention or as monotherapy to reduce depressive symptoms in unipolar or bipolar depression patients[135]. The antidepressant effects of tDCS may involve long-term neuroplastic changes that continue to occur even after the acute phase of treatment, which explains its delayed efficacy[135].
Recently, neurophysiological studies have shown that the clinical effects of tDCS do not have a direct linear relationship with the dose of stimulation[136]. tDCS, as a relatively simple and portable technology, is well-suited for remote supervised treatment and assessment at home, thus facilitating long treatment durations[136].
Since the optimal clinical effects of tDCS are delayed, future clinical trials should use longer evaluation periods and aim to identify responsive patients using algorithms[137].
VNS
VNS is a therapeutic method that has been used for the last sixteen years to treat resistant unilateral or bipolar depression. However, despite several clinical studies attesting to its favorable benefit-risk ratio and its approval by the Food Drug Administration in 2005, it is not used very often[138].
VNS involves the implantation of a pacemaker under the collarbone that is connected to an electrode surrounding the left vagus nerve. The left vagus nerve is preferred because it exposes the patient to fewer potential adverse cardiac effects. Indeed, most cardiac afferent fibers originate from the right vagus nerve[139]. Since the turn of the century, numerous studies have demonstrated the efficacy of VNS in resistant depression[140-142].
However, only one randomized, double-blind, controlled trial comparing VNS with usual medical treatment has been conducted over a short period of 10 wk[141]. Moreover, the results of this study did not indicate that the combination of VNS with typical medical treatments was better than the typical medical treatment on its own.
However, VNS has demonstrated progressively increasing improvements in depressive symptoms, with significant positive outcomes observed after six to 12 mo; these benefits can last for up to two years[143].
More long-term studies are needed to fully determine the predictors of the correct response.
DBS
According to the literature, DBS of the subgenual cingulate white matter (Brodmann area = BA 25) elicited a clinical response in 60% of resistant depression patients after six months and clinical remission in 35% of patients, with benefits maintained for over 12 mo[144]. The stimulation of other targets, in particular the nucleus accumbens, to treat resistant depression has gained interest recently. Behavioral effects indicate the quick and favorable impact of stimulation on anhedonia, with significant effects on mood appearing as early as week one after treatment begins[145].
Magnetic seizure therapy
Magnetic seizure therapy involves inducing a therapeutic seizure by applying magnetic stimulation to the brain while the patient is under anesthesia. This technique is still being investigated as a viable alternative to ECT to treat many psychiatric disorders. Evidence supporting its effectiveness on depressive symptoms continues to grow, and it appears to induce fewer neurocognitive effects than ECT[146,147].
Luxtherapy (phototherapy)
The first description of reduced depression symptoms due to intense light exposure was presented in 1984[148]. Optimal improvements were obtained with bright light exposure of 2500 Lux for two hours per day, with morning exposure shown to be superior to evening exposure[149].
A review and meta-analysis[150] showed that more intense (but shorter) exposures (10000 Lux for half an hour per day or 6000 Lux for 1.5 h per day) have the same efficacy. Importantly, this treatment method is effective both for those with seasonal and non-seasonal depression. Benefits of phototherapy related to sleep deprivation and drug treatments have also been reported[151].
Neuro-modulation treatments offer a range of treatment options for patients with depression. ECT remains the most documented and effective method in this category[151]. rTMS is an interesting technique as well, as it offers a well-tolerated profile[85], while tDCS offers encouraging but varying results that depend on the study’s design and the techniques used[130].
More investigations are needed to specify which indications are the best for each method according to the clinical and biological profiles of patients. The uses of such methods are expanding, probably, with their efficiency increasing when they are tailored to the patient. Furthermore, somatic interventions for depression need to be regularly assessed and integrated into psychiatrists’ therapeutic arsenals.
CONCLUSION
Treating depression is still a significant challenge. Finding the best option for each patient is the best way to obtaining short- and long-term effectiveness. The three principal methods available to caregivers are antidepressants, specifically structured psychotherapies, and somatic approaches. Research on depression pharmacotherapy continues to examine new molecules implicated in gamma-aminobutyric acid regulation and glutamate transmission. Also, efforts to personalize and simplify psychotherapeutic interventions are ongoing. Protocols using somatic interventions need to be studied in more depth, and their indications must be specified. ECT is the only somatic treatment with confirmed indications for certain forms of depression. Combinations of medications, psychotherapy, and somatic therapies remain the most effective ways to manage resistant forms of depression.
Footnotes
Conflict-of-interest statement: All authors declare that they have no conflict of interest related to this article.
Manuscript source: Invited manuscript
Peer-review started: March 31, 2021
First decision: June 5, 2021
Article in press: October 11, 2021
Specialty type: Medicine, research and experimental
Country/Territory of origin: Morocco
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Narumiya K S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
Contributor Information
Rabie Karrouri, Department of Psychiatry, Moulay Ismaïl Military Hospital, Faculty of Medicine and Pharmacy, Sidi Mohamed Ben Abdellah University, Fez 30070, Morocco.
Zakaria Hammani, Department of Psychiatry, Moulay Ismaïl Military Hospital, Faculty of Medicine and Pharmacy, Sidi Mohamed Ben Abdellah University, Fez 30070, Morocco.
Roukaya Benjelloun, Department of Psychiatry, Faculty of Medicine, Mohammed VI University of Health Sciences, Casablanca 20000, Morocco.
Yassine Otheman, Department of Psychiatry, Moulay Ismaïl Military Hospital, Faculty of Medicine and Pharmacy, Sidi Mohamed Ben Abdellah University, Fez 30070, Morocco. yassine.othemane@usmba.ac.ma.
References
- 1.WHO The global burden of disease: 2004 update [Internet]. [cited 29 March 2021]. Available from: https://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/
- 2.Lépine JP, Briley M. The increasing burden of depression. Neuropsychiatr Dis Treat. 2011;7:3–7. doi: 10.2147/NDT.S19617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Allen NB. Cognitive therapy of depression. Aaron T Beck, A John Rush, Brian F Shaw, Gary Emery. New York: Guilford Press, 1979. Aust N Z J Psychiatry. 2002;36:275–278. doi: 10.1046/j.1440-1614.2002.t01-5-01015.x. [DOI] [PubMed] [Google Scholar]
- 4.Cozanitis DA. Daniel Bovet, Nobelist: muscle relaxants in anaesthesia : The role played by two neglected protagonists. Wien Med Wochenschr. 2016;166:487–499. doi: 10.1007/s10354-016-0481-y. [DOI] [PubMed] [Google Scholar]
- 5.Domino EF. History of modern psychopharmacology: a personal view with an emphasis on antidepressants. Psychosom Med. 1999;61:591–598. doi: 10.1097/00006842-199909000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Pereira VS, Hiroaki-Sato VA. A brief history of antidepressant drug development: from tricyclics to beyond ketamine. Acta Neuropsychiatr. 2018;30:307–322. doi: 10.1017/neu.2017.39. [DOI] [PubMed] [Google Scholar]
- 7.López-Muñoz F, Alamo C. Monoaminergic neurotransmission: the history of the discovery of antidepressants from 1950s until today. Curr Pharm Des. 2009;15:1563–1586. doi: 10.2174/138161209788168001. [DOI] [PubMed] [Google Scholar]
- 8.Ban TA. Pharmacotherapy of depression: a historical analysis. J Neural Transm (Vienna) 2001;108:707–716. doi: 10.1007/s007020170047. [DOI] [PubMed] [Google Scholar]
- 9.López-Muñoz F, Alamo C, Juckel G, Assion HJ. Half a century of antidepressant drugs: on the clinical introduction of monoamine oxidase inhibitors, tricyclics, and tetracyclics. Part I: monoamine oxidase inhibitors. J Clin Psychopharmacol. 2007;27:555–559. doi: 10.1097/jcp.0b013e3181bb617. [DOI] [PubMed] [Google Scholar]
- 10.White K, Razani J, Cadow B, Gelfand R, Palmer R, Simpson G, Sloane RB. Tranylcypromine vs nortriptyline vs placebo in depressed outpatients: a controlled trial. Psychopharmacology (Berl) 1984;82:258–262. doi: 10.1007/BF00427786. [DOI] [PubMed] [Google Scholar]
- 11.McGrath PJ, Stewart JW, Harrison W, Wager S, Quitkin FM. Phenelzine treatment of melancholia. J Clin Psychiatry. 1986;47:420–422. [PubMed] [Google Scholar]
- 12.Henkel V, Mergl R, Allgaier AK, Kohnen R, Möller HJ, Hegerl U. Treatment of depression with atypical features: a meta-analytic approach. Psychiatry Res. 2006;141:89–101. doi: 10.1016/j.psychres.2005.07.012. [DOI] [PubMed] [Google Scholar]
- 13.Culpepper L, Kovalick LJ. A review of the literature on the selegiline transdermal system: an effective and well-tolerated monoamine oxidase inhibitor for the treatment of depression. Prim Care Companion J Clin Psychiatry. 2008;10:25–30. doi: 10.4088/pcc.v10n0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McGrath PJ, Stewart JW, Fava M, Trivedi MH, Wisniewski SR, Nierenberg AA, Thase ME, Davis L, Biggs MM, Shores-Wilson K, Luther JF, Niederehe G, Warden D, Rush AJ. Tranylcypromine vs venlafaxine plus mirtazapine following three failed antidepressant medication trials for depression: a STAR*D report. Am J Psychiatry. 2006;163:1531–41; quiz 1666. doi: 10.1176/ajp.2006.163.9.1531. [DOI] [PubMed] [Google Scholar]
- 15.Fiedorowicz JG, Swartz KL. The role of monoamine oxidase inhibitors in current psychiatric practice. J Psychiatr Pract. 2004;10:239–248. doi: 10.1097/00131746-200407000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ban TA. In memory of three pioneers. Int J Neuropsychopharmacol. 2006;9:475–477. doi: 10.1017/S1461145706006870. [DOI] [PubMed] [Google Scholar]
- 17.Abbing-Karahagopian V, Huerta C, Souverein PC, de Abajo F, Leufkens HG, Slattery J, Alvarez Y, Miret M, Gil M, Oliva B, Hesse U, Requena G, de Vries F, Rottenkolber M, Schmiedl S, Reynolds R, Schlienger RG, de Groot MC, Klungel OH, van Staa TP, van Dijk L, Egberts AC, Gardarsdottir H, De Bruin ML. Antidepressant prescribing in five European countries: application of common definitions to assess the prevalence, clinical observations, and methodological implications. Eur J Clin Pharmacol. 2014;70:849–857. doi: 10.1007/s00228-014-1676-z. [DOI] [PubMed] [Google Scholar]
- 18.MacGillivray S, Arroll B, Hatcher S, Ogston S, Reid I, Sullivan F, Williams B, Crombie I. Efficacy and tolerability of selective serotonin reuptake inhibitors compared with tricyclic antidepressants in depression treated in primary care: systematic review and meta-analysis. BMJ. 2003;326:1014. doi: 10.1136/bmj.326.7397.1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barbui C, Guaiana G, Hotopf M. Amitriptyline for inpatients and SSRIs for outpatients with depression? Pharmacopsychiatry. 2004;37:93–97. doi: 10.1055/s-2004-818985. [DOI] [PubMed] [Google Scholar]
- 20.Anderson IM. SSRIS vs tricyclic antidepressants in depressed inpatients: a meta-analysis of efficacy and tolerability. Depress Anxiety. 1998;7 Suppl 1:11–17. [PubMed] [Google Scholar]
- 21.Fairchild CJ, Rush AJ, Vasavada N, Giles DE, Khatami M. Which depressions respond to placebo? Psychiatry Res. 1986;18:217–226. doi: 10.1016/0165-1781(86)90109-5. [DOI] [PubMed] [Google Scholar]
- 22.Raskin A, Crook TH. The endogenous--neurotic distinction as a predictor of response to antidepressant drugs. Psychol Med. 1976;6:59–70. doi: 10.1017/s0033291700007509. [DOI] [PubMed] [Google Scholar]
- 23.Paykel ES. Depressive typologies and response to amitriptyline. Br J Psychiatry. 1972;120:147–156. doi: 10.1192/bjp.120.555.147. [DOI] [PubMed] [Google Scholar]
- 24.Cleare A, Pariante CM, Young AH, Anderson IM, Christmas D, Cowen PJ, Dickens C, Ferrier IN, Geddes J, Gilbody S, Haddad PM, Katona C, Lewis G, Malizia A, McAllister-Williams RH, Ramchandani P, Scott J, Taylor D, Uher R Members of the Consensus Meeting. Evidence-based guidelines for treating depressive disorders with antidepressants: A revision of the 2008 British Association for Psychopharmacology guidelines. J Psychopharmacol. 2015;29:459–525. doi: 10.1177/0269881115581093. [DOI] [PubMed] [Google Scholar]
- 25.Montgomery SA. The efficacy of fluoxetine as an antidepressant in the short and long term. Int Clin Psychopharmacol. 1989;4 Suppl 1:113–119. [PubMed] [Google Scholar]
- 26.Millan MJ. Multi-target strategies for the improved treatment of depressive states: Conceptual foundations and neuronal substrates, drug discovery and therapeutic application. Pharmacol Ther. 2006;110:135–370. doi: 10.1016/j.pharmthera.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 27.Amick HR, Gartlehner G, Gaynes BN, Forneris C, Asher GN, Morgan LC, Coker-Schwimmer E, Boland E, Lux LJ, Gaylord S, Bann C, Pierl CB, Lohr KN. Comparative benefits and harms of second generation antidepressants and cognitive behavioral therapies in initial treatment of major depressive disorder: systematic review and meta-analysis. BMJ. 2015;351:h6019. doi: 10.1136/bmj.h6019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Magni LR, Purgato M, Gastaldon C, Papola D, Furukawa TA, Cipriani A, Barbui C. Fluoxetine vs other types of pharmacotherapy for depression. Cochrane Database Syst Rev. 2013:CD004185. doi: 10.1002/14651858.CD004185.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Montgomery SA. A meta-analysis of the efficacy and tolerability of paroxetine vs tricyclic antidepressants in the treatment of major depression. Int Clin Psychopharmacol . 2001;16:169–178. doi: 10.1097/00004850-200105000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Gartlehner G, Gaynes BN, Hansen RA, Thieda P, DeVeaugh-Geiss A, Krebs EE, Moore CG, Morgan L, Lohr KN. Comparative benefits and harms of second-generation antidepressants: background paper for the American College of Physicians. Ann Intern Med. 2008;149:734–750. doi: 10.7326/0003-4819-149-10-200811180-00008. [DOI] [PubMed] [Google Scholar]
- 31.Kennedy SH, Andersen HF, Lam RW. Efficacy of escitalopram in the treatment of major depressive disorder compared with conventional selective serotonin reuptake inhibitors and venlafaxine XR: a meta-analysis. J Psychiatry Neurosci. 2006;31:122–131. [PMC free article] [PubMed] [Google Scholar]
- 32.Garnock-Jones KP, McCormack PL. Escitalopram: a review of its use in the management of major depressive disorder in adults. CNS Drugs. 2010;24:769–796. doi: 10.2165/11204760-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 33.Edwards JG, Anderson I. Systematic review and guide to selection of selective serotonin reuptake inhibitors. Drugs. 1999;57:507–533. doi: 10.2165/00003495-199957040-00005. [DOI] [PubMed] [Google Scholar]
- 34.Bauer M, Bschor T, Pfennig A, Whybrow PC, Angst J, Versiani M, Möller HJ WFSBP Task Force on Unipolar Depressive Disorders. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for Biological Treatment of Unipolar Depressive Disorders in Primary Care. World J Biol Psychiatry. 2007;8:67–104. doi: 10.1080/15622970701227829. [DOI] [PubMed] [Google Scholar]
- 35.Nemeroff CB, Entsuah R, Benattia I, Demitrack M, Sloan DM, Thase ME. Comprehensive analysis of remission (COMPARE) with venlafaxine vs SSRIs. Biol Psychiatry . 2008;63:424–434. doi: 10.1016/j.biopsych.2007.06.027. [DOI] [PubMed] [Google Scholar]
- 36.Thase ME, Pritchett YL, Ossanna MJ, Swindle RW, Xu J, Detke MJ. Efficacy of duloxetine and selective serotonin reuptake inhibitors: comparisons as assessed by remission rates in patients with major depressive disorder. J Clin Psychopharmacol. 2007;27:672–676. doi: 10.1097/jcp.0b013e31815a4412. [DOI] [PubMed] [Google Scholar]
- 37.Bauer M, Tharmanathan P, Volz HP, Moeller HJ, Freemantle N. The effect of venlafaxine compared with other antidepressants and placebo in the treatment of major depression: a meta-analysis. Eur Arch Psychiatry Clin Neurosci. 2009;259:172–185. doi: 10.1007/s00406-008-0849-0. [DOI] [PubMed] [Google Scholar]
- 38.Cipriani A, Furukawa TA, Salanti G, Geddes JR, Higgins JP, Churchill R, Watanabe N, Nakagawa A, Omori IM, McGuire H, Tansella M, Barbui C. Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet. 2009;373:746–758. doi: 10.1016/S0140-6736(09)60046-5. [DOI] [PubMed] [Google Scholar]
- 39.Wiles NJ, Fischer K, Cowen P, Nutt D, Peters TJ, Lewis G, White IR. Allowing for non-adherence to treatment in a randomized controlled trial of two antidepressants (citalopram vs reboxetine): an example from the GENPOD trial. Psychol Med . 2014;44:2855–2866. doi: 10.1017/S0033291714000221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fava M, Rush AJ, Thase ME, Clayton A, Stahl SM, Pradko JF, Johnston JA. 15 years of clinical experience with bupropion HCl: from bupropion to bupropion SR to bupropion XL. Prim Care Companion J Clin Psychiatry. 2005;7:106–113. doi: 10.4088/pcc.v07n0305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cunningham LA, Borison RL, Carman JS, Chouinard G, Crowder JE, Diamond BI, Fischer DE, Hearst E. A comparison of venlafaxine, trazodone, and placebo in major depression. J Clin Psychopharmacol. 1994;14:99–106. [PubMed] [Google Scholar]
- 42.Papakostas GI, Fava M. A meta-analysis of clinical trials comparing the serotonin (5HT)-2 receptor antagonists trazodone and nefazodone with selective serotonin reuptake inhibitors for the treatment of major depressive disorder. Eur Psychiatry. 2007;22:444–447. doi: 10.1016/j.eurpsy.2007.01.1220. [DOI] [PubMed] [Google Scholar]
- 43.Kostrubsky SE, Strom SC, Kalgutkar AS, Kulkarni S, Atherton J, Mireles R, Feng B, Kubik R, Hanson J, Urda E, Mutlib AE. Inhibition of hepatobiliary transport as a predictive method for clinical hepatotoxicity of nefazodone. Toxicol Sci. 2006;90:451–459. doi: 10.1093/toxsci/kfj095. [DOI] [PubMed] [Google Scholar]
- 44.Gonda X, Sharma SR, Tarazi FI. Vortioxetine: a novel antidepressant for the treatment of major depressive disorder. Expert Opin Drug Discov. 2019;14:81–89. doi: 10.1080/17460441.2019.1546691. [DOI] [PubMed] [Google Scholar]
- 45.Papakostas GI, Stahl SM, Krishen A, Seifert CA, Tucker VL, Goodale EP, Fava M. Efficacy of bupropion and the selective serotonin reuptake inhibitors in the treatment of major depressive disorder with high levels of anxiety (anxious depression): a pooled analysis of 10 studies. J Clin Psychiatry. 2008;69:1287–1292. doi: 10.4088/jcp.v69n0812. [DOI] [PubMed] [Google Scholar]
- 46.Li Z, Maglione M, Tu W, Mojica W, Arterburn D, Shugarman LR, Hilton L, Suttorp M, Solomon V, Shekelle PG, Morton SC. Meta-analysis: pharmacologic treatment of obesity. Ann Intern Med. 2005;142:532–546. doi: 10.7326/0003-4819-142-7-200504050-00012. [DOI] [PubMed] [Google Scholar]
- 47.Papakostas GI, Homberger CH, Fava M. A meta-analysis of clinical trials comparing mirtazapine with selective serotonin reuptake inhibitors for the treatment of major depressive disorder. J Psychopharmacol. 2008;22:843–848. doi: 10.1177/0269881107083808. [DOI] [PubMed] [Google Scholar]
- 48.Deardorff WJ, Grossberg GT. A review of the clinical efficacy, safety and tolerability of the antidepressants vilazodone, levomilnacipran and vortioxetine. Expert Opin Pharmacother. 2014;15:2525–2542. doi: 10.1517/14656566.2014.960842. [DOI] [PubMed] [Google Scholar]
- 49.Schatzberg AF. Trazodone: a 5-year review of antidepressant efficacy. Psychopathology. 1987;20 Suppl 1:48–56. doi: 10.1159/000284523. [DOI] [PubMed] [Google Scholar]
- 50.Orsolini L, Tomasetti C, Valchera A, Iasevoli F, Buonaguro EF, Fornaro M, Fiengo ALC, Martinotti G, Vellante F, Matarazzo I, Vecchiotti R, Perna G, Di Nicola M, Carano A, Di Bartolomeis A, De Giannantonio M, De Berardis D. Current and Future Perspectives on the Major Depressive Disorder: Focus on the New Multimodal Antidepressant Vortioxetine. CNS Neurol Disord Drug Targets. 2017;16:65–92. doi: 10.2174/1871527315666161025140111. [DOI] [PubMed] [Google Scholar]
- 51.Freemantle N, Anderson IM, Young P. Predictive value of pharmacological activity for the relative efficacy of antidepressant drugs. Meta-regression analysis. Br J Psychiatry. 2000;177:292–302. doi: 10.1192/bjp.177.4.292. [DOI] [PubMed] [Google Scholar]
- 52.Cipriani A, Furukawa TA, Salanti G, Chaimani A, Atkinson LZ, Ogawa Y, Leucht S, Ruhe HG, Turner EH, Higgins JPT, Egger M, Takeshima N, Hayasaka Y, Imai H, Shinohara K, Tajika A, Ioannidis JPA, Geddes JR. Comparative Efficacy and Acceptability of 21 Antidepressant Drugs for the Acute Treatment of Adults With Major Depressive Disorder: A Systematic Review and Network Meta-Analysis. Focus (Am Psychiatr Publ) 2018;16:420–429. doi: 10.1176/appi.focus.16407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Schwartz J, Murrough JW, Iosifescu DV. Ketamine for treatment-resistant depression: recent developments and clinical applications. Evid Based Ment Health. 2016;19:35–38. doi: 10.1136/eb-2016-102355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bobo WV, Vande Voort JL, Croarkin PE, Leung JG, Tye SJ, Frye MA. KETAMINE FOR TREATMENT-RESISTANT UNIPOLAR AND BIPOLAR MAJOR DEPRESSION: CRITICAL REVIEW AND IMPLICATIONS FOR CLINICAL PRACTICE. Depress Anxiety. 2016;33:698–710. doi: 10.1002/da.22505. [DOI] [PubMed] [Google Scholar]
- 55.Martin GI. The apgar score ... revisited. J Perinatol. 1989;9:338–346. [PubMed] [Google Scholar]
- 56.Swiatek KM, Jordan K, Coffman J. New use for an old drug: oral ketamine for treatment-resistant depression. BMJ Case Rep. 2016;2016 doi: 10.1136/bcr-2016-216088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhu W, Ding Z, Zhang Y, Shi J, Hashimoto K, Lu L. Risks Associated with Misuse of Ketamine as a Rapid-Acting Antidepressant. Neurosci Bull. 2016;32:557–564. doi: 10.1007/s12264-016-0081-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Liu Y, Lin D, Wu B, Zhou W. Ketamine abuse potential and use disorder. Brain Res Bull. 2016;126:68–73. doi: 10.1016/j.brainresbull.2016.05.016. [DOI] [PubMed] [Google Scholar]
- 59.Caddy C, Giaroli G, White TP, Shergill SS, Tracy DK. Ketamine as the prototype glutamatergic antidepressant: pharmacodynamic actions, and a systematic review and meta-analysis of efficacy. Ther Adv Psychopharmacol. 2014;4:75–99. doi: 10.1177/2045125313507739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sanacora G, Frye MA, McDonald W, Mathew SJ, Turner MS, Schatzberg AF, Summergrad P, Nemeroff CB American Psychiatric Association (APA) Council of Research Task Force on Novel Biomarkers and Treatments. A Consensus Statement on the Use of Ketamine in the Treatment of Mood Disorders. JAMA Psychiatry. 2017;74:399–405. doi: 10.1001/jamapsychiatry.2017.0080. [DOI] [PubMed] [Google Scholar]
- 61.Lee RJ, Hong JS, McGinty JF, Lomax P. Increased enkephalin and dynorphin immunoreactivity in the hippocampus of seizure sensitive Mongolian gerbils. Brain Res. 1987;401:353–358. doi: 10.1016/0006-8993(87)91420-x. [DOI] [PubMed] [Google Scholar]
- 62.Kryst J, Kawalec P, Pilc A. Efficacy and safety of intranasal esketamine for the treatment of major depressive disorder. Expert Opin Pharmacother. 2020;21:9–20. doi: 10.1080/14656566.2019.1683161. [DOI] [PubMed] [Google Scholar]
- 63.Khorassani F, Talreja O. Intranasal esketamine: A novel drug for treatment-resistant depression. Am J Health Syst Pharm. 2020;77:1382–1388. doi: 10.1093/ajhp/zxaa191. [DOI] [PubMed] [Google Scholar]
- 64.Sanders B, Brula AQ. Intranasal esketamine: From origins to future implications in treatment-resistant depression. J Psychiatr Res. 2021;137:29–35. doi: 10.1016/j.jpsychires.2021.02.020. [DOI] [PubMed] [Google Scholar]
- 65.Ionescu DF, Papakostas GI. Experimental medication treatment approaches for depression. Transl Psychiatry. 2017;7:e1068. doi: 10.1038/tp.2017.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lener MS, Kadriu B, Zarate CA Jr. Ketamine and Beyond: Investigations into the Potential of Glutamatergic Agents to Treat Depression. Drugs. 2017;77:381–401. doi: 10.1007/s40265-017-0702-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jaso BA, Niciu MJ, Iadarola ND, Lally N, Richards EM, Park M, Ballard ED, Nugent AC, Machado-Vieira R, Zarate CA. Therapeutic Modulation of Glutamate Receptors in Major Depressive Disorder. Curr Neuropharmacol. 2017;15:57–70. doi: 10.2174/1570159X14666160321123221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Salardini E, Zeinoddini A, Mohammadinejad P, Khodaie-Ardakani MR, Zahraei N, Akhondzadeh S. Riluzole combination therapy for moderate-to-severe major depressive disorder: A randomized, double-blind, placebo-controlled trial. J Psychiatr Res. 2016;75:24–30. doi: 10.1016/j.jpsychires.2016.01.003. [DOI] [PubMed] [Google Scholar]
- 69.Booij L, Van der Does AJ, Riedel WJ. Monoamine depletion in psychiatric and healthy populations: review. Mol Psychiatry. 2003;8:951–973. doi: 10.1038/sj.mp.4001423. [DOI] [PubMed] [Google Scholar]
- 70.Moreno FA, Parkinson D, Palmer C, Castro WL, Misiaszek J, El Khoury A, Mathé AA, Wright R, Delgado PL. CSF neurochemicals during tryptophan depletion in individuals with remitted depression and healthy controls. Eur Neuropsychopharmacol. 2010;20:18–24. doi: 10.1016/j.euroneuro.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wohleb ES, Gerhard D, Thomas A, Duman RS. Molecular and Cellular Mechanisms of Rapid-Acting Antidepressants Ketamine and Scopolamine. Curr Neuropharmacol. 2017;15:11–20. doi: 10.2174/1570159X14666160309114549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gerhard DM, Wohleb ES, Duman RS. Emerging treatment mechanisms for depression: focus on glutamate and synaptic plasticity. Drug Discov Today. 2016;21:454–464. doi: 10.1016/j.drudis.2016.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Practice guideline for the treatment of patients with major depressive disorder (revision). American Psychiatric Association. Am J Psychiatry. 2000;157:1–45. [PubMed] [Google Scholar]
- 74.Bennabi D, Charpeaud T, Yrondi A, Genty JB, Destouches S, Lancrenon S, Alaïli N, Bellivier F, Bougerol T, Camus V, Dorey JM, Doumy O, Haesebaert F, Holtzmann J, Lançon C, Lefebvre M, Moliere F, Nieto I, Rabu C, Richieri R, Schmitt L, Stephan F, Vaiva G, Walter M, Leboyer M, El-Hage W, Llorca PM, Courtet P, Aouizerate B, Haffen E. Clinical guidelines for the management of treatment-resistant depression: French recommendations from experts, the French Association for Biological Psychiatry and Neuropsychopharmacology and the fondation FondaMental. BMC Psychiatry. 2019;19:262. doi: 10.1186/s12888-019-2237-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Malhi GS, Bassett D, Boyce P, Bryant R, Fitzgerald PB, Fritz K, Hopwood M, Lyndon B, Mulder R, Murray G, Porter R, Singh AB. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders. Aust N Z J Psychiatry. 2015;49:1087–1206. doi: 10.1177/0004867415617657. [DOI] [PubMed] [Google Scholar]
- 76.Qaseem A, Barry MJ, Kansagara D Clinical Guidelines Committee of the American College of Physicians. Nonpharmacologic Versus Pharmacologic Treatment of Adult Patients With Major Depressive Disorder: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2016;164:350–359. doi: 10.7326/M15-2570. [DOI] [PubMed] [Google Scholar]
- 77.Lepping P, Whittington R, Sambhi RS, Lane S, Poole R, Leucht S, Cuijpers P, McCabe R, Waheed W. Clinical relevance of findings in trials of CBT for depression. Eur Psychiatry. 2017;45:207–211. doi: 10.1016/j.eurpsy.2017.07.003. [DOI] [PubMed] [Google Scholar]
- 78.National Collaborating Centre for Mental Health (UK) Depression: The Treatment and Management of Depression in Adults (Updated Edition). Leicester (UK): British Psychological Society; 2010. [PubMed] [Google Scholar]
- 79.Gelenberg AJ, Freeman MP, Markowitz JC, Rosenbaum JF, Thase ME, Trivedi MH, Van Rhoads RS, Depaulo JR, Schneck CD. Work group on major depressive disorder, 2010: 152. [cited 208 March 2021]. Available from: https://www.researchgate.net/directory/publications .
- 80.Clinical Practice Guideline. Clinical Practice Guideline for the Treatment of Depression Across Three Age Cohorts. [cited 208 March 2021]. Available from: https://www.apa.org/depression-guideline .
- 81.Cuijpers P, Quero S, Dowrick C, Arroll B. Psychological Treatment of Depression in Primary Care: Recent Developments. Curr Psychiatry Rep. 2019;21:129. doi: 10.1007/s11920-019-1117-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Dimidjian S, Barrera M Jr, Martell C, Muñoz RF, Lewinsohn PM. The origins and current status of behavioral activation treatments for depression. Annu Rev Clin Psychol. 2011;7:1–38. doi: 10.1146/annurev-clinpsy-032210-104535. [DOI] [PubMed] [Google Scholar]
- 83.Twohig MP, Levin ME. Acceptance and Commitment Therapy as a Treatment for Anxiety and Depression: A Review. Psychiatr Clin North Am. 2017;40:751–770. doi: 10.1016/j.psc.2017.08.009. [DOI] [PubMed] [Google Scholar]
- 84.Kennedy SH, Lam RW, McIntyre RS, Tourjman SV, Bhat V, Blier P, Hasnain M, Jollant F, Levitt AJ, MacQueen GM, McInerney SJ, McIntosh D, Milev RV, Müller DJ, Parikh SV, Pearson NL, Ravindran AV, Uher R CANMAT Depression Work Group. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 Clinical Guidelines for the Management of Adults with Major Depressive Disorder: Section 3. Pharmacological Treatments. Can J Psychiatry. 2016;61:540–560. doi: 10.1177/0706743716659417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Carter JD, McIntosh VV, Jordan J, Porter RJ, Frampton CM, Joyce PR. Psychotherapy for depression: a randomized clinical trial comparing schema therapy and cognitive behavior therapy. J Affect Disord. 2013;151:500–505. doi: 10.1016/j.jad.2013.06.034. [DOI] [PubMed] [Google Scholar]
- 86.Weersing VR, Jeffreys M, Do MT, Schwartz KT, Bolano C. Evidence Base Update of Psychosocial Treatments for Child and Adolescent Depression. J Clin Child Adolesc Psychol. 2017;46:11–43. doi: 10.1080/15374416.2016.1220310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Jonsson U, Bertilsson G, Allard P, Gyllensvärd H, Söderlund A, Tham A, Andersson G. Psychological Treatment of Depression in People Aged 65 Years and Over: A Systematic Review of Efficacy, Safety, and Cost-Effectiveness. PLoS One. 2016;11:e0160859. doi: 10.1371/journal.pone.0160859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Nightingale A. Clinician’s Quick Guide to Interpersonal Psychotherapy. Psychiatr Bull. 2008;32:279–279. doi: 10.1176/appi.ajp.2007.07101543. [DOI] [PubMed] [Google Scholar]
- 89.Arean P, Hegel M, Vannoy S, Fan MY, Unuzter J. Effectiveness of problem-solving therapy for older, primary care patients with depression: results from the IMPACT project. Gerontologist. 2008;48:311–323. doi: 10.1093/geront/48.3.311. [DOI] [PubMed] [Google Scholar]
- 90.Alexopoulos GS, Raue P, Areán P. Problem-solving therapy vs supportive therapy in geriatric major depression with executive dysfunction. Am J Geriatr Psychiatry . 2003;11:46–52. [PubMed] [Google Scholar]
- 91.Sargeant JK, Bruce ML, Florio LP, Weissman MM. Factors associated with 1-year outcome of major depression in the community. Arch Gen Psychiatry. 1990;47:519–526. doi: 10.1001/archpsyc.1990.01810180019004. [DOI] [PubMed] [Google Scholar]
- 92.Gautam S, Jain A, Gautam M, Vahia VN, Grover S. Clinical Practice Guidelines for the management of Depression. Indian J Psychiatry. 2017;59:S34–S50. doi: 10.4103/0019-5545.196973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Health Quality Ontario. Psychotherapy for Major Depressive Disorder and Generalized Anxiety Disorder: A Health Technology Assessment. Ont Health Technol Assess Ser. 2017;17:1–167. [PMC free article] [PubMed] [Google Scholar]
- 94.Karasu TB. Developmentalist metatheory of depression and psychotherapy. Am J Psychother. 1992;46:37–49. doi: 10.1176/appi.psychotherapy.1992.46.1.37. [DOI] [PubMed] [Google Scholar]
- 95.Bright JI, Baker KD, Neimeyer RA. Professional and paraprofessional group treatments for depression: a comparison of cognitive-behavioral and mutual support interventions. J Consult Clin Psychol. 1999;67:491–501. doi: 10.1037//0022-006x.67.4.491. [DOI] [PubMed] [Google Scholar]
- 96.Klier CM, Muzik M, Rosenblum KL, Lenz G. Interpersonal psychotherapy adapted for the group setting in the treatment of postpartum depression. J Psychother Pract Res. 2001;10:124–131. [PMC free article] [PubMed] [Google Scholar]
- 97.Bolton P, Bass J, Neugebauer R, Verdeli H, Clougherty KF, Wickramaratne P, Speelman L, Ndogoni L, Weissman M. Group interpersonal psychotherapy for depression in rural Uganda: a randomized controlled trial. JAMA. 2003;289:3117–3124. doi: 10.1001/jama.289.23.3117. [DOI] [PubMed] [Google Scholar]
- 98.Krishna M, Lepping P, Jones S, Lane S. Systematic review and meta-analysis of group cognitive behavioural psychotherapy treatment for sub-clinical depression. Asian J Psychiatr. 2015;16:7–16. doi: 10.1016/j.ajp.2015.05.043. [DOI] [PubMed] [Google Scholar]
- 99.Honagodu AR, Krishna M, Sundarachar R, Lepping P. Group psychotherapies for depression in persons with HIV: A systematic review. Indian J Psychiatry. 2013;55:323–330. doi: 10.4103/0019-5545.120541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sipe WE, Eisendrath SJ. Mindfulness-based cognitive therapy: theory and practice. Can J Psychiatry. 2012;57:63–69. doi: 10.1177/070674371205700202. [DOI] [PubMed] [Google Scholar]
- 101.Cladder-Micus MB, Speckens AEM, Vrijsen JN, T Donders AR, Becker ES, Spijker J. Mindfulness-based cognitive therapy for patients with chronic, treatment-resistant depression: A pragmatic randomized controlled trial. Depress Anxiety. 2018;35:914–924. doi: 10.1002/da.22788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Tursi MF, Baes Cv, Camacho FR, Tofoli SM, Juruena MF. Effectiveness of psychoeducation for depression: a systematic review. Aust N Z J Psychiatry. 2013;47:1019–1031. doi: 10.1177/0004867413491154. [DOI] [PubMed] [Google Scholar]
- 103.Carneiro LF, Mota MP, Schuch F, Deslandes A, Vasconcelos-Raposo J. Portuguese and Brazilian guidelines for the treatment of depression: exercise as medicine. Braz J Psychiatry. 2018;40:210–211. doi: 10.1590/1516-4446-2017-2272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Schuch FB, Vasconcelos-Moreno MP, Borowsky C, Zimmermann AB, Rocha NS, Fleck MP. Exercise and severe major depression: effect on symptom severity and quality of life at discharge in an inpatient cohort. J Psychiatr Res. 2015;61:25–32. doi: 10.1016/j.jpsychires.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 105.Kolovos S, Kleiboer A, Cuijpers P. Effect of psychotherapy for depression on quality of life: meta-analysis. Br J Psychiatry. 2016;209:460–468. doi: 10.1192/bjp.bp.115.175059. [DOI] [PubMed] [Google Scholar]
- 106.Chen CK, Nehrig N, Chou LJ, McGowan R, Guyton AF, Mustafiz F, Bailey RW. Patient Extratherapeutic Interpersonal Problems and Response to Psychotherapy for Depression. Am J Psychother. 2019;72:101–122. doi: 10.1176/appi.psychotherapy.20190005. [DOI] [PubMed] [Google Scholar]
- 107.Nieuwsma JA, Trivedi RB, McDuffie J, Kronish I, Benjamin D, Williams JW. Brief psychotherapy for depression: a systematic review and meta-analysis. Int J Psychiatry Med. 2012;43:129–151. doi: 10.2190/PM.43.2.c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Szekely D, Polosan M. Les thérapeutiques non médicamenteuses en psychiatrie. Ann Méd-Psychol Rev Psychiatr. 2010;168:546–551. [Google Scholar]
- 109.UK ECT Review Group. Efficacy and safety of electroconvulsive therapy in depressive disorders: a systematic review and meta-analysis. Lancet. 2003;361:799–808. doi: 10.1016/S0140-6736(03)12705-5. [DOI] [PubMed] [Google Scholar]
- 110.Slade EP, Jahn DR, Regenold WT, Case BG. Association of Electroconvulsive Therapy With Psychiatric Readmissions in US Hospitals. JAMA Psychiatry. 2017;74:798–804. doi: 10.1001/jamapsychiatry.2017.1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.McCall WV, Rosenquist PB, Kimball J, Haskett R, Isenberg K, Prudic J, Lasater B, Sackeim HA. Health-related quality of life in a clinical trial of ECT followed by continuation pharmacotherapy: effects immediately after ECT and at 24 weeks. J ECT . 2011;27:97–102. doi: 10.1097/YCT.0b013e318205c7d7. [DOI] [PubMed] [Google Scholar]
- 112.Tørring N, Sanghani SN, Petrides G, Kellner CH, Østergaard SD. The mortality rate of electroconvulsive therapy: a systematic review and pooled analysis. Acta Psychiatr Scand. 2017;135:388–397. doi: 10.1111/acps.12721. [DOI] [PubMed] [Google Scholar]
- 113.Liang CS, Chung CH, Tsai CK, Chien WC. In-hospital mortality among electroconvulsive therapy recipients: A 17-year nationwide population-based retrospective study. Eur Psychiatry. 2017;42:29–35. doi: 10.1016/j.eurpsy.2016.12.005. [DOI] [PubMed] [Google Scholar]
- 114.Prudic J, Sackeim HA, Devanand DP. Medication resistance and clinical response to electroconvulsive therapy. Psychiatry Res. 1990;31:287–296. doi: 10.1016/0165-1781(90)90098-p. [DOI] [PubMed] [Google Scholar]
- 115.Chu CW, Chien WC, Chung CH, Chao PC, Chang HA, Kao YC, Chou YC, Tzeng NS. Electroconvulsive Therapy and Risk of Dementia-A Nationwide Cohort Study in Taiwan. Front Psychiatry. 2018;9:397. doi: 10.3389/fpsyt.2018.00397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Anderson EL, Reti IM. ECT in pregnancy: a review of the literature from 1941 to 2007. Psychosom Med. 2009;71:235–242. doi: 10.1097/PSY.0b013e318190d7ca. [DOI] [PubMed] [Google Scholar]
- 117.Fink M, Kellner CH, McCall WV. The role of ECT in suicide prevention. J ECT. 2014;30:5–9. doi: 10.1097/YCT.0b013e3182a6ad0d. [DOI] [PubMed] [Google Scholar]
- 118.Kennedy R, Mittal D, O'Jile J. Electroconvulsive therapy in movement disorders: an update. J Neuropsychiatry Clin Neurosci. 2003;15:407–421. doi: 10.1176/jnp.15.4.407. [DOI] [PubMed] [Google Scholar]
- 119.Saatcioglu O, Tomruk NB. The use of electroconvulsive therapy in pregnancy: a review. Isr J Psychiatry Relat Sci. 2011;48:6–11. [PubMed] [Google Scholar]
- 120.Birkenhager TK, Roos J, Kamperman AM. Improvement after two sessions of electroconvulsive therapy predicts final remission in in-patients with major depression. Acta Psychiatr Scand. 2019;140:189–195. doi: 10.1111/acps.13054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Foo JC, Streit F, Frank J, Witt SH, Treutlein J Major Depressive Disorder Working Group of the Psychiatric Genomics Consortium, Baune BT, Moebus S, Jöckel KH, Forstner AJ, Nöthen MM, Rietschel M, Sartorius A, Kranaster L. Evidence for increased genetic risk load for major depression in patients assigned to electroconvulsive therapy. Am J Med Genet B Neuropsychiatr Genet. 2019;180:35–45. doi: 10.1002/ajmg.b.32700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Nuninga JO, Mandl RCW, Boks MP, Bakker S, Somers M, Heringa SM, Nieuwdorp W, Hoogduin H, Kahn RS, Luijten P, Sommer IEC. Volume increase in the dentate gyrus after electroconvulsive therapy in depressed patients as measured with 7T. Mol Psychiatry. 2020;25:1559–1568. doi: 10.1038/s41380-019-0392-6. [DOI] [PubMed] [Google Scholar]
- 123.Omori W, Itagaki K, Kajitani N, Abe H, Okada-Tsuchioka M, Okamoto Y, Takebayashi M. Shared preventive factors associated with relapse after a response to electroconvulsive therapy in four major psychiatric disorders. Psychiatry Clin Neurosci. 2019;73:494–500. doi: 10.1111/pcn.12859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Li M, Yao X, Sun L, Zhao L, Xu W, Zhao H, Zhao F, Zou X, Cheng Z, Li B, Yang W, Cui R. Effects of Electroconvulsive Therapy on Depression and Its Potential Mechanism. Front Psychol. 2020;11:80. doi: 10.3389/fpsyg.2020.00080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Fregni F, Pascual-Leone A. Technology insight: noninvasive brain stimulation in neurology-perspectives on the therapeutic potential of rTMS and tDCS. Nat Clin Pract Neurol. 2007;3:383–393. doi: 10.1038/ncpneuro0530. [DOI] [PubMed] [Google Scholar]
- 126.De Risio L, Borgi M, Pettorruso M, Miuli A, Ottomana AM, Sociali A, Martinotti G, Nicolò G, Macrì S, di Giannantonio M, Zoratto F. Recovering from depression with repetitive transcranial magnetic stimulation (rTMS): a systematic review and meta-analysis of preclinical studies. Transl Psychiatry. 2020;10:393. doi: 10.1038/s41398-020-01055-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Martinotti G, Montemitro C, Pettorruso M, Viceconte D, Alessi MC, Di Carlo F, Lucidi L, Picutti E, Santacroce R, Di Giannantonio M. Augmenting pharmacotherapy with neuromodulation techniques for the treatment of bipolar disorder: a focus on the effects of mood stabilizers on cortical excitability. Expert Opin Pharmacother. 2019;20:1575–1588. doi: 10.1080/14656566.2019.1622092. [DOI] [PubMed] [Google Scholar]
- 128.Wei Y, Zhu J, Pan S, Su H, Li H, Wang J. Meta-analysis of the Efficacy and Safety of Repetitive Transcranial Magnetic Stimulation (rTMS) in the Treatment of Depression. Shanghai Arch Psychiatry. 2017;29:328–342. doi: 10.11919/j.issn.1002-0829.217106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Brunoni AR, Nitsche MA, Bolognini N, Bikson M, Wagner T, Merabet L, Edwards DJ, Valero-Cabre A, Rotenberg A, Pascual-Leone A, Ferrucci R, Priori A, Boggio PS, Fregni F. Clinical research with transcranial direct current stimulation (tDCS): challenges and future directions. Brain Stimul. 2012;5:175–195. doi: 10.1016/j.brs.2011.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Antal A, Alekseichuk I, Bikson M, Brockmöller J, Brunoni AR, Chen R, Cohen LG, Dowthwaite G, Ellrich J, Flöel A, Fregni F, George MS, Hamilton R, Haueisen J, Herrmann CS, Hummel FC, Lefaucheur JP, Liebetanz D, Loo CK, McCaig CD, Miniussi C, Miranda PC, Moliadze V, Nitsche MA, Nowak R, Padberg F, Pascual-Leone A, Poppendieck W, Priori A, Rossi S, Rossini PM, Rothwell J, Rueger MA, Ruffini G, Schellhorn K, Siebner HR, Ugawa Y, Wexler A, Ziemann U, Hallett M, Paulus W. Low intensity transcranial electric stimulation: Safety, ethical, legal regulatory and application guidelines. Clin Neurophysiol. 2017;128:1774–1809. doi: 10.1016/j.clinph.2017.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Bikson M, Brunoni AR, Charvet LE, Clark VP, Cohen LG, Deng ZD, Dmochowski J, Edwards DJ, Frohlich F, Kappenman ES, Lim KO, Loo C, Mantovani A, McMullen DP, Parra LC, Pearson M, Richardson JD, Rumsey JM, Sehatpour P, Sommers D, Unal G, Wassermann EM, Woods AJ, Lisanby SH. Rigor and reproducibility in research with transcranial electrical stimulation: An NIMH-sponsored workshop. Brain Stimul. 2018;11:465–480. doi: 10.1016/j.brs.2017.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Undurraga J, Baldessarini RJ. Randomized, placebo-controlled trials of antidepressants for acute major depression: thirty-year meta-analytic review. Neuropsychopharmacology. 2012;37:851–864. doi: 10.1038/npp.2011.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Mutz J, Vipulananthan V, Carter B, Hurlemann R, Fu CHY, Young AH. Comparative efficacy and acceptability of non-surgical brain stimulation for the acute treatment of major depressive episodes in adults: systematic review and network meta-analysis. BMJ. 2019;364:l1079. doi: 10.1136/bmj.l1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Moffa AH, Martin D, Alonzo A, Bennabi D, Blumberger DM, Benseñor IM, Daskalakis Z, Fregni F, Haffen E, Lisanby SH, Padberg F, Palm U, Razza LB, Sampaio-Jr B, Loo C, Brunoni AR. Efficacy and acceptability of transcranial direct current stimulation (tDCS) for major depressive disorder: An individual patient data meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2020;99:109836. doi: 10.1016/j.pnpbp.2019.109836. [DOI] [PubMed] [Google Scholar]
- 135.Stagg CJ, Antal A, Nitsche MA. Physiology of Transcranial Direct Current Stimulation. J ECT. 2018;34:144–152. doi: 10.1097/YCT.0000000000000510. [DOI] [PubMed] [Google Scholar]
- 136.Alonzo A, Fong J, Ball N, Martin D, Chand N, Loo C. Pilot trial of home-administered transcranial direct current stimulation for the treatment of depression. J Affect Disord. 2019;252:475–483. doi: 10.1016/j.jad.2019.04.041. [DOI] [PubMed] [Google Scholar]
- 137.Senova S, Rabu C, Beaumont S, Michel V, Palfi S, Mallet L, Domenech P. Stimulation du nerf vague dans le traitement de la dépression [Vagus nerve stimulation and depression] Presse Med. 2019;48:1507–1519. doi: 10.1016/j.lpm.2019.10.019. [DOI] [PubMed] [Google Scholar]
- 138.Shah A, Carreno FR, Frazer A. Therapeutic modalities for treatment resistant depression: focus on vagal nerve stimulation and ketamine. Clin Psychopharmacol Neurosci. 2014;12:83–93. doi: 10.9758/cpn.2014.12.2.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Aaronson ST, Carpenter LL, Conway CR, Reimherr FW, Lisanby SH, Schwartz TL, Moreno FA, Dunner DL, Lesem MD, Thompson PM, Husain M, Vine CJ, Banov MD, Bernstein LP, Lehman RB, Brannon GE, Keepers GA, O'Reardon JP, Rudolph RL, Bunker M. Vagus nerve stimulation therapy randomized to different amounts of electrical charge for treatment-resistant depression: acute and chronic effects. Brain Stimul. 2013;6:631–640. doi: 10.1016/j.brs.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 140.Cristancho P, Cristancho MA, Baltuch GH, Thase ME, O'Reardon JP. Effectiveness and safety of vagus nerve stimulation for severe treatment-resistant major depression in clinical practice after FDA approval: outcomes at 1 year. J Clin Psychiatry. 2011;72:1376–1382. doi: 10.4088/JCP.09m05888blu. [DOI] [PubMed] [Google Scholar]
- 141.Rush AJ, Marangell LB, Sackeim HA, George MS, Brannan SK, Davis SM, Howland R, Kling MA, Rittberg BR, Burke WJ, Rapaport MH, Zajecka J, Nierenberg AA, Husain MM, Ginsberg D, Cooke RG. Vagus nerve stimulation for treatment-resistant depression: a randomized, controlled acute phase trial. Biol Psychiatry. 2005;58:347–354. doi: 10.1016/j.biopsych.2005.05.025. [DOI] [PubMed] [Google Scholar]
- 142.Schlaepfer TE, Frick C, Zobel A, Maier W, Heuser I, Bajbouj M, O'Keane V, Corcoran C, Adolfsson R, Trimble M, Rau H, Hoff HJ, Padberg F, Müller-Siecheneder F, Audenaert K, Van den Abbeele D, Stanga Z, Hasdemir M. Vagus nerve stimulation for depression: efficacy and safety in a European study. Psychol Med. 2008;38:651–661. doi: 10.1017/S0033291707001924. [DOI] [PubMed] [Google Scholar]
- 143.Lozano AM, Mayberg HS, Giacobbe P, Hamani C, Craddock RC, Kennedy SH. Subcallosal cingulate gyrus deep brain stimulation for treatment-resistant depression. Biol Psychiatry. 2008;64:461–467. doi: 10.1016/j.biopsych.2008.05.034. [DOI] [PubMed] [Google Scholar]
- 144.Mayberg HS, Lozano AM, Voon V, McNeely HE, Seminowicz D, Hamani C, Schwalb JM, Kennedy SH. Deep brain stimulation for treatment-resistant depression. Neuron. 2005;45:651–660. doi: 10.1016/j.neuron.2005.02.014. [DOI] [PubMed] [Google Scholar]
- 145.Kosel M, Frick C, Lisanby SH, Fisch HU, Schlaepfer TE. Magnetic seizure therapy improves mood in refractory major depression. Neuropsychopharmacology. 2003;28:2045–2048. doi: 10.1038/sj.npp.1300293. [DOI] [PubMed] [Google Scholar]
- 146.Kallioniemi E, McClintock SM, Deng ZD, Husain MM, Lisanby SH. Magnetic Seizure Therapy: Towards Personalized Seizure Therapy for Major Depression. Pers Med Psychiatry. 2019;17-18:37–42. doi: 10.1016/j.pmip.2019.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Bottai T. Traitement non médicamenteux de la dépression. Presse Méd. 2008;37(5, Part 2):877–882. doi: 10.1016/j.lpm.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 148.Sack RL, Lewy AJ, White DM, Singer CM, Fireman MJ, Vandiver R. Morning vs evening light treatment for winter depression. Evidence that the therapeutic effects of light are mediated by circadian phase shifts. Arch Gen Psychiatry. 1990;47:343–351. doi: 10.1001/archpsyc.1990.01810160043008. [DOI] [PubMed] [Google Scholar]
- 149.Golden RN, Gaynes BN, Ekstrom RD, Hamer RM, Jacobsen FM, Suppes T, Wisner KL, Nemeroff CB. The efficacy of light therapy in the treatment of mood disorders: a review and meta-analysis of the evidence. Am J Psychiatry. 2005;162:656–662. doi: 10.1176/appi.ajp.162.4.656. [DOI] [PubMed] [Google Scholar]
- 150.Benedetti F, Bernasconi A, Blasi V, Cadioli M, Colombo C, Falini A, Lorenzi C, Radaelli D, Scotti G, Smeraldi E. Neural and genetic correlates of antidepressant response to sleep deprivation: a functional magnetic resonance imaging study of moral valence decision in bipolar depression. Arch Gen Psychiatry. 2007;64:179–187. doi: 10.1001/archpsyc.64.2.179. [DOI] [PubMed] [Google Scholar]
- 151.Merkl A, Heuser I, Bajbouj M. Antidepressant electroconvulsive therapy: mechanism of action, recent advances and limitations. Exp Neurol. 2009;219:20–26. doi: 10.1016/j.expneurol.2009.04.027. [DOI] [PubMed] [Google Scholar]


