Abstract
Introduction
Depression and anxiety are common among people with rosacea. However, the exact magnitude of the prevalence rate and odds ratios (ORs) for depression and anxiety, respectively, in rosacea patients is unclear, and no systematic review or meta-analysis of published data has yet been performed. We therefore performed as systematic review and meta-analysis to determine the prevalence rates and ORs for depression and anxiety in rosacea patients.
Methods
We performed a systematic search of the PubMed, Embase and Medline databases for all observational studies published up to October 2020 that reported the prevalence rates and ORs for depression and anxiety in patients with rosacea. The primary outcome measures were prevalence rates and ORs for depression and anxiety in patients with rosacea. Heterogeneity across studies was assessed with the I2 statistic. Sources of heterogeneity were explored through subgroup and meta-regression analyses.
Results
A total of 14 studies involving 14,134,021 patients with rosacea were included in the systematic review and meta-analysis. The pooled prevalence of depression was 19.6% (95% confidence interval [CI] 15.0–24.3%) and that of anxiety was 15.6% (95% CI 11.8–19.3%). The prevalence of depression and anxiety was significantly lower in studies using clinical criteria to diagnose depression and anxiety (9.2 and 10.2%, respectively) than in those studies using screening tools (26.2% [P < 0.01] and 22.7% [P = 0.03], respectively). The methodological quality of the included studies greatly contributed to the heterogeneity. Patients with rosacea were more likely to experience depression (OR 2.21, 95% CI 1.79–2.72) and anxiety (OR 2.31, 95% CI 1.56–3.44) than healthy controls.
Conclusions
This systematic review and meta-analysis indicates that patients with rosacea are at a higher risk of experiencing depression and anxiety. More efforts are warranted to recognize and manage depression and anxiety in patients with rosacea.
Supplementary Information
The online version contains supplementary material available at 10.1007/s13555-021-00613-w.
Keywords: Rosacea, Depression, Anxiety, Prevalence
Key Summary Points
| Why carry out this study? |
| The reported prevalence of depression and anxiety in patients with rosacea varies substantially. The exact prevalence rate and odds ratio for depression and anxiety in this patient population remains unknown. |
| We performed a systematic review and meta-analysis of all published literature to determine the association between rosacea, depression and anxiety. |
| What was learned from the study? |
| The overall prevalence of depression and anxiety in rosacea patients was 19.0 and 15.6% respectively. The odds ratio for depression and anxiety was 2.21 (95% confidence interval [CI] 1.79–2.72) and 2.31 (95% CI 1.56–3.44) in patients with rosacea compared with the healthy controls. |
| Patients with rosacea are at a higher risk of depression and anxiety. |
Introduction
Rosacea is a chronic recurrent inflammatory skin disorder that primarily affects the central area of the face [1]. The global prevalence of rosacea is 5.46% among the general population, with its prevalence according to geographic area ranging from 1 to 22% [2–4]. While rosacea affects both women and men, women aged ≥ 30 years represent the majority of patients, although men with rosacea may suffer more psychologically in comparison with women [5, 6]. The exact etiology of rosacea is unknown, but a genetic component, dysregulation of the immune response, deviant neurovascular signaling and microorganisms may play a role in its pathogenesis [1]. In addition, many extrinsic triggers seem to exacerbate rosacea, including sun exposure, cold, heat, alcohol and physical activity [1].
The symptoms of rosacea include flushing, redness, pustules and telangiectasia on the face. These unpleasant symptoms may lead to physical discomfort (e.g. burning and stinging) and cause psychological distress [7, 8]. Multiple comorbidities have been found to be associated with rosacea [9], including cardiovascular disease [10], gastrointestinal disorders [11], neurologic disorders [12], autoimmune condition [13], malignancies [14] and psychiatric disorders [15]. Bewley et al. reported that the erythema of rosacea can impair health-related quality of life (HRQoL) in most patients, which in turn is closely related to depression, anxiety and even suicide [16]. The prevalence of depression and anxiety among individuals with rosacea has been reported to vary from 0.68 to 58%, with the prevalences depending on the different study methodologies [17, 18]. This vast range in these outcomes may be attributed to moderating variables, such study setting, diagnostic criteria, geographic area/region, gender balance and demographic data. Although the authors of some previous studies concluded there is an association between rosacea and depression and anxiety [18, 19], the discrepant findings on this topic have not been systematically reviewed.
In this systematic review and meta-analysis, we sought to analyze the pooled estimate of prevalence rate and odds for depression and anxiety disorders in patients with rosacea. In addition, since many aspects may impact on outcomes, such as study methodology, we also aimed to examine potential sources of heterogeneity across studies.
Methods
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Literature Search
This systematic review and meta-analysis was performed in accordance with PRISMA guidelines [20]. Eligible studies reporting the prevalence rates or/and odds ratios (ORs) were identified by searching the PubMed, Embase and Medline databases using various forms and combinations of search terms, including “rosacea,” “depressive disorder,” “depression,” “anxiety,” “anxiety disorders,” “psychiatric disorders,” “mental disorder,” “phobia” and “suicide.” No language limitation was imposed. The search included all articles available in the databases from database inception to 5 October 2020. Reference lists of relevant publications were screened manually for potential eligibility. Two investigators (SLX and RD) performed independent screenings of literature.
Inclusion and Exclusion Criteria
No restrictions were made on study designs with the aim to increase the number of relevant publications. The inclusion criteria were: (1) original study; (2) study assessed the prevalence rates or the relationship of depression or anxiety in rosacea patients; (3) Study was conducted in adults aged > 18 years; (4) study included at least 20 subjects with rosacea. People with rosacea or depression or anxiety were diagnosed by physicians, on the basis of International Classification of Disease (ICD) codes or by self-reported diagnoses from physicians (patient reported that he or she has been diagnosed by a physician as having rosacea). No restriction was made to rosacea subtypes. We also included studies using screening questionnaires to indicate the possible occurrence of depression and anxiety. In present study, we used physically-diagnosed, self-reported and screening questionnaire methods to diagnose study variables. Studies without sufficient data to calculate prevalence or ORs were excluded. When data were duplicated in multiple publications, the most informative article was included in the analysis.
Data Extraction and Quality Assessment
The following data were extracted from each article: first author, year of publication, geographic region of study, study design, study setting, study size, mean age of patients, distribution by sex, methods used to diagnose rosacea, depression and anxiety, prevalence of depression or anxiety, crude and/or adjusted OR estimates with corresponding 95% confidence intervals (CIs). Since the number of studies that stratified rosacea by clinical subtypes was insufficient, we excluded these data. If a study did not provide ORs directly, we calculated this parameter based on raw data extracted from the study. Any disagreement on data was resolved with consensus among all authors. If certain data were unavailable or unclear in published form, the authors of the study were contacted by email and asked to provide the original information.
The quality of each included study was assessed using the Newcastle–Ottawa Scale (NOS), in which studies are judged on eight items regarding representatives of study population, comparability and ascertainment of exposure or outcome of interest [21]. An adapted version was used for cross-sectional studies (Electronic Supplementary Material [ESM] File S1). Higher scores in the NOS indicate better methodical quality, and studies that met ≥ 5 of the NOS items were considered to be of high quality.
Statistical Analysis
The prevalence rates of rosacea patients with depression and anxiety were calculated in both controlled and uncontrolled studies. In controlled studies, ORs and 95% CI for depression and anxiety between rosacea patients and healthy controls were analyzed. If some study did not provide overall ORs for depression risk but presented separate ORs for different exposure levels of rosacea, we combined the corresponding odds estimates on the basis of Hamling’s method [22]. The pooled prevalence and ORs with 95% CIs obtained from included studies were estimated by random-effects models because of significant heterogeneity (I2 > 50% for all analyses) [23]. Heterogeneity across studies was assessed by I2 statistics, which represents the percentage of total variation contributed by a cross-study variation [24]. A study was defined to be heterogeneous if the P < 0.1 or I2 > 50%.
Potential sources of heterogeneity were explored using subgroup and random-effect meta-regression analyses. Subgroup analyses were conducted on study setting, methods used to assess rosacea, depression and anxiety and geographic areas. Meta-regression analyses were conducted only when there were data from > 5 independent datasets. For the meta-regression analyses, we took mean age, percentage of female subjects and NOS scores into consideration. In studies assessing the ORs for depression and anxiety, sensitivity analyses were performed to investigate the influence of the individual study on the pooled estimate by subsequent omitting studies and determining the potential weighted outliers. When > 10 studies were available, we used Egger' regression and Begg rank to assess the publication bias. The trim-and-fill method was used to determine the effect size when publication bias was noted.
All statistical analyses were performed with Stata software version 13.0 (Stata Corp., College Station, TX, USA). The significance level was set to P < 0.05.
Results
Study Characteristics
The initial comprehensive search yielded a total of 164 articles. The title and abstract of each of these articles were then screened to determine potential eligibility, yielding 37 articles for full-text assessment. Combined with the additional two articles identified from relevant references, 14 articles were ultimately included in the systematic review and meta-analysis. The search strategy is illustrated in the PRISMA flow diagram shown in Fig. 1.
Fig. 1.
PRISM flow diagram of study inclusion
In this meta-analysis of the 14 studies [17, 18, 25–36], we pooled data on 14,134,021 patients with rosacea and 686,447,139 controls (Table 1). Only one study included > 100,000 patients and three studies included > 10,000 patients. Five studies were conducted on the general population, and nine studies were conducted on a hospital-based population. In most studies, rosacea was diagnosed by a physician or using an ICD code. Only two studies defined rosacea through self-report. All included studies ascertained outcomes of depression or anxiety using screening questionnaires, with the exception of five studies which evaluated depressive symptoms by ICD codes. In all, 14 studies examined the association between rosacea and depression, and seven studies examined the association between rosacea and anxiety.
Table 1.
Summary of included studies
| First author of study [reference] | Country | Study design | Setting | Rosacea patients (n) | Female patients, n (%) | Mean age (years) | Rosacea assessment | Assessment of psychological disorders | Prevalence, % (95% CI) | Control group size (n) | OR (95% CI) | NOS score | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Crude | Adjusted | ||||||||||||
| Lukaviciute et al. [36] | Lithuania | Case–control | Hospital-based | 120 | 107 (89.2%) | 42.3 | Physician diagnosis | HADS |
Depression: 30.0 (21.8–38.2) Anxiety: 36.7 (28.1–45.3) |
497 |
Depression: 5.84 (3.46–9.85) Anxiety: 3.31 (2.12–5.17) |
Depression: 7.22 (4.12–12.63) Anxiety: 3.40 (2.16–5.36) |
7 |
| Uysal et al. [27] | Turkey | Case–ontrol | Hospital-based | 194 | 147 (75%) | 47 | Physician diagnosis | GAD-7 |
Depression: 12.9 (9.0–18.8) Anxiety: 10.8 (6.4–15.2) |
194 |
Depression: 3.32 (2.72–3.38) Anxiety: 4.59 (3.61–5.83) |
NA | 7 |
| Alinia et al. [26] | USA | Cross-sectional | Hospital-based | 183 | NA | NA | ICD-9 | PHQ-9 | Depression: 31.2 (24.4–37.9) | NA | NA | NA | 5 |
| Hung et al. [29] | Taiwan, China | Retrospective cohort | General population-based | 7881 | 5336 (67.7%) | 40.6 | ICD-9 | ICD-9 |
Depression: 4.6 (4.1–5.0) Anxiety: 10.8 (10.1–11.5) |
31,524 |
Depression: 1.47 (1.45–1.49) Anxiety: 1.13 (1.12–1.13) |
NA | 9 |
| Singam et al. [30] | USA | Retrospective cohort | Hospital-based | 35,446 | 19,772 (55.8%) | 63.7 | ICD-9 | ICD-9 |
Depression: 14.4 (14.1–14.8) Anxiety: 6.5 (6.2–6.8) |
87,017,709 |
Depression: 2.28 (2.20–2.37) Anxiety: 2.32 (2.21–2.44) |
Depression: 1.83 (1.76–1.91) Anxiety: 1.86 (1.76–1.96) |
8 |
| Wu et al. [28] | China | Cross-sectional | Hospital-based | 201 | 137 (68.2%) | 38.8 | Physician diagnosis | HADS |
Depression: 16.4 (11.3–21.5) Anxiety: 20.4 (14.8–26.0) |
196 |
Depression: 2.21 (1.92–2,54) Anxiety: 1.93 (1.70–2.19) |
NA | 7 |
| Egeberg et al. 2016 | Denmark | Prospective-cohort | General population-based | 55,437 | 36,673 (66.2%) | 39.9 | ICD-8/10 | ICD-8/10 |
Depression: 10.0 (9.7–10.2) Anxiety: 13.4 (13.1–13.7) |
4,576,904 |
Depression: 2.20 (2.14–2.26) Anxiety: 2.21 (2.15–2.26) |
Depression: 1.96 (1.90–2.01) Anxiety: 1.87 (1.83–1.9) |
9 |
| Halioua et al. [33] | UK, France, Germany, USA | Cross-sectional | General population-based | 629 | 362 (57.6%) | 31.3 | Self-report | Questionnaire | Depression: 28.0 (24.5–31.5) | NA | NA | NA | 7 |
| Dirschka et al. [35] | Germany, UK, Ireland, Sweden, Denmark, France, Italy, Mexico | Cross-sectional | Online general population-based | 820 | NA | NA | Self-report | Emotix questionnaire | Depression: 22.0 (19.1–24.8) | NA | NA | NA | 7 |
| Böhm et al. [32] | Germany | Cross-sectional | Hospital-based | 168 | 88 (52.4%) | 56 | Physician diagnosis | HADS |
Depression: 20.2 (14.2–26.3) Anxiety: 25 (18.5–31.5) |
NA | NA | NA | 4 |
| Spoendlin et al. [31] | UK | Case–control | General population-based | 53,927 | 33,879 (62.8%) | NA | ICD-10 | ICD-10 | Depression: 16.5 (16.2–16.8) | 53,927 | Depression: 1.16 (1.12–1.20) |
Depression: 1.20 (1.16–1.24) |
8 |
| Beaulieu et al. [18] | France | Cross-sectional | Hospital-based | 185 | 129 (69.7%) | NA | Physician diagnosis | Questionnaire | Depression: 58.4 (51.3–65.5) | NA | NA | NA | 5 |
| Abram et al. [34] | Estonia | Case–control | Hospital-based | 126 | 78 (61.9%) | 46.7 | Physician diagnosis | EMS questionnaire | Depression: 19.1 (12.2–25.9) | 167 | Depression: 1.95 (1.64, 2.32) | NA | 6 |
| Gupta et al. [17] | USA | Retrospective cohort | Hospital-based | 13,978,704 | 9,757,135 (69.8%) | 50.8 | ICD-9 | ICD-9 | Depression: 0.7 (0.7–0.7) | 594,766,021 | Depression: 4.81 (1.39–16.62) | NA | 8 |
CI Confidence interval, EMS Estonian Mood Scale, GAD-7 Anxiety Disorder 7-item scale, HADS Hospital Anxiety and Depression Scale, ICD International Classification of Diseases, NA not available, NOS Newcastle–Ottawa-Scale, OR odds ratio, PHQ-9 Patient Health Questionnaire 9
According to the NOS system, 13 of the 14 included studies can be considered to be of high quality. The remaining study met only four of the nine NOS items. Information on the NOS scores is presented in more detail in ESM Table S1.
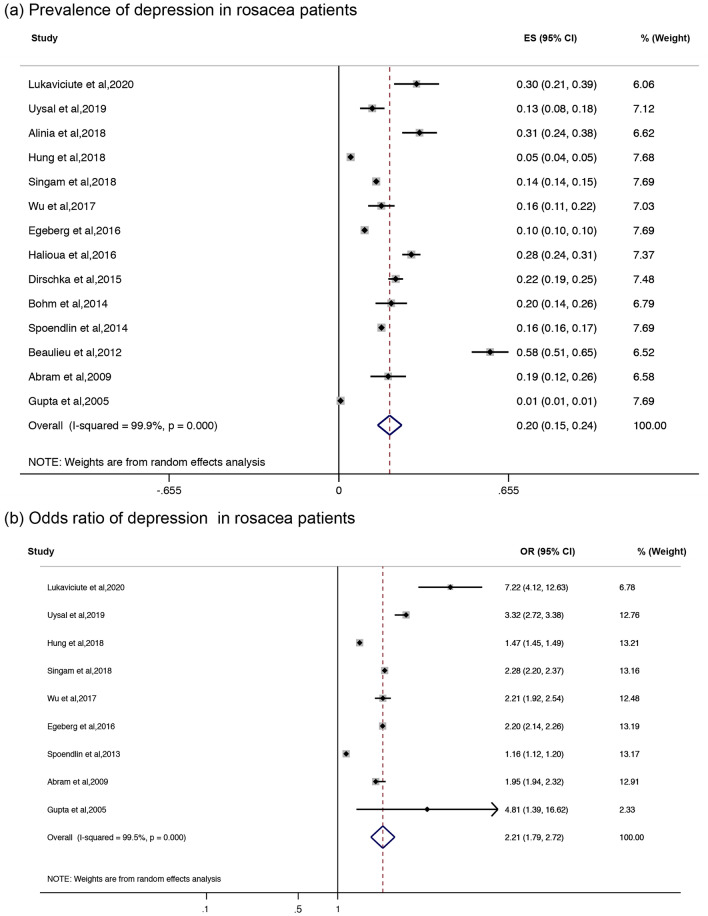
Association of Depression and Rosacea
A total of 14 studies reported the prevalence of depression in patients with rosacea (Fig. 2a; Table 2). The pooled random-effects prevalence of any type of depression was 19.6% (95% CI 15.0–24.3%). Heterogeneity was significant (I2 = 99.9%, P < 0.01). There was publication bias according to the Egger regression (P = 0.012), but no publication bias was found based on the Begg rank (P = 0.23). The trim-and-fill method showed no study was filled up at final analysis. In the subgroup analysis, the prevalence of depression among the general population was 15.9% (95% CI 11.1–20.7%), whereas in studies in a hospital-based population, the prevalence of depression was 22.0% (95% CI 15.2–28.8%). When depression was stratified by the method used to diagnose rosacea, the prevalence of depression in rosacea patients determined using screening questionnaires was 26.2% (95% CI 19.3–33.2%); however, the proportion of depressed patients decreased when outcomes were measured by ICD codes (9.2%, 95% CI 1.9–16.6%). A significant difference in the prevalence of depression was detected in subgroups diagnosed with depression using different methods (P < 0.01). In rosacea patients diagnosed by physicians or ICD codes, the pooled prevalence of depression was 18.7% (95% CI 13.7–23.7%), while in those diagnosed through self-reported records from physicians (only 2 studies), it was 24.9% (95% CI 19.0–30.8%). Seven studies were performed in Europe, with a pooled proportion of depression of 23.4% (95% CI 19.2–27.5%); three studies were performed in North America, with a pooled prevalence of 14.8% (95% CI 3.6–26.1%); the pooled prevalence of depression in Asia was 11% (95% CI 2.9–19.2%). The prevalence of depression was significantly different between these three continents (P = 0.02). According to random-effect meta-regression analyses, the percentage of women with rosacea (coefficient of variance [CV] 0.18, adjusted [adj.] R2 = − 8.9%, τ2 = 0.02, P = 0.71) and the mean age (CV − 0.002, adj. R2 = − 6.71%, τ2 = 0.01, P = 0.50) did not moderate the rate of depression in rosacea patients. However, the NOS scores of included studies explained 41.4% of the variability between studies (CV − 0.06, adj R2 = 41.4%, τ2 = 0.01, P = 0.01). Therefore, the methodological quality of included studies may be a possible source of heterogeneity.
Fig. 2.
Forest plots of depression in rosacea patients. a Prevalence of depression. ES Effect size, CI confidence interval. b Association of depression in rosacea patients versus healthy controls. OR Odds ratios
Table 2.
Depression and anxiety outcomes in rosacea patients: subgroup analysis and meta-regression
| Subgroup | No. of records | Pooled rate (95% CI) | I2 | P | Meta-regression | |||
|---|---|---|---|---|---|---|---|---|
| Proportion of between-study variance explained (adj. R2) (%) | Estimate of between-study variance (τ2) | Coefficient | P | |||||
| Depression | ||||||||
| Stratified by population | 51.9% | 0.15 | − 3.73 | 0.02 | 0.06 | 0.45 | ||
| General population-based | 5 | 0.16 (0.11–0.21) | 99.8% | |||||
| Hospital-based | 9 | 0.22 (0.15–0.29) | 99.9% | |||||
| Stratified by diagnostic method of depression | 90.8% | 0.001* | 35.10 | 0.01 | − 0.17 | 0.02* | ||
| ICD codes | 5 | 0.09 (0.02, 0.17) | 100% | |||||
| Screening questionnaires | 9 | 0.26 (0.19, 0.33) | 94.1% | |||||
| Stratified by diagnostic method of rosacea | 59.2% | 0.12 | − 6.02 | 0.02 | 0.06 | 0.61 | ||
| Physician diagnosis/ICD codes | 12 | 0.19 (0.14, 0.24) | 99.9% | |||||
| Self-report | 2 | 0.25 (0.19, 0.31) | 85.4% | |||||
| Geographic area | 74.9% | 0.02* | 10.95 | 0.02 | − 0.07 | 0.15 | ||
| Europe | 7 | 0.23 (0.19, 0.28) | 99.5% | |||||
| Northern America | 3 | 0.15 (0.04, 0.26) | 100% | |||||
| Asia | 3 | 0.11 (0.03, 0.19) | 93.8% | |||||
| Continuous variables | ||||||||
| Female percentage | 12 | / | / | / | − 8.9 | 0.02 | 0.18 | 0.71 |
| Mean age | 10 | / | / | / | − 6.71 | 0.01 | − 0.002 | 0.50 |
| NOS scores | 14 | / | / | / | 41.4 | 0.01 | − 0.06 | 0.01* |
| Anxiety | ||||||||
| Stratified by population | 51.8% | 0.15 | − 9.41 | 0.010 | − 0.07 | 0.45 | ||
| General population-based | 2 | 0.12 (0.10, 0.15) | 97.9% | |||||
| Hospital-based | 5 | 0.19 (0.10, 0.29) | 96.0% | |||||
| Stratified by diagnostic method of anxiety | 79.5% | 0.03* | 38.27 | 0.006 | 0.12 | 0.1 | ||
| ICD codes | 3 | 0.10 (0.05, 0.15) | 99.8% | |||||
| Screening questionnaires | 4 | 0.23 (0.13, 0.33) | 90.4% | |||||
| Geographic area | / | / | 7.86 | 0.008 | − 0.05 | 0.26 | ||
| Europe | 3 | 0.24 (0.11 0.38) | 94.6% | |||||
| North America | 1 | 0.06 (0.06, 0.07) | / | |||||
| Asia | 3 | 0.13 (0.09, 0.18) | 82.2% | |||||
| Continuous variables | ||||||||
| Female percentage | 7 | / | / | / | 7.38 | 0.008 | − 0.41 | 0.28 |
| Mean age | 7 | / | / | / | − 14.53 | 0.005 | − 0.003 | 0.56 |
| NOS | 7 | / | / | / | 19.99 | 0.007 | − 0.03 | 0.22 |
| Stratified by population | 51.8% | 0.15 | − 9.41 | 0.010 | − 0.07 | 0.45 | ||
* P < 0.05
From the nine studies that included controls, the pooled rate of depression was higher in patients with rosacea than in the control group (OR 2.21, 95% CI 1.79–2.72) (Fig. 2b). When recalculating the pooled estimate by omitting one study each time, sensitivity analysis showed that the ORs for depression remained significant, which indicated that the summary estimates were sufficiently robust to exclude studies with different assessment criteria (ESM Fig. S1a).
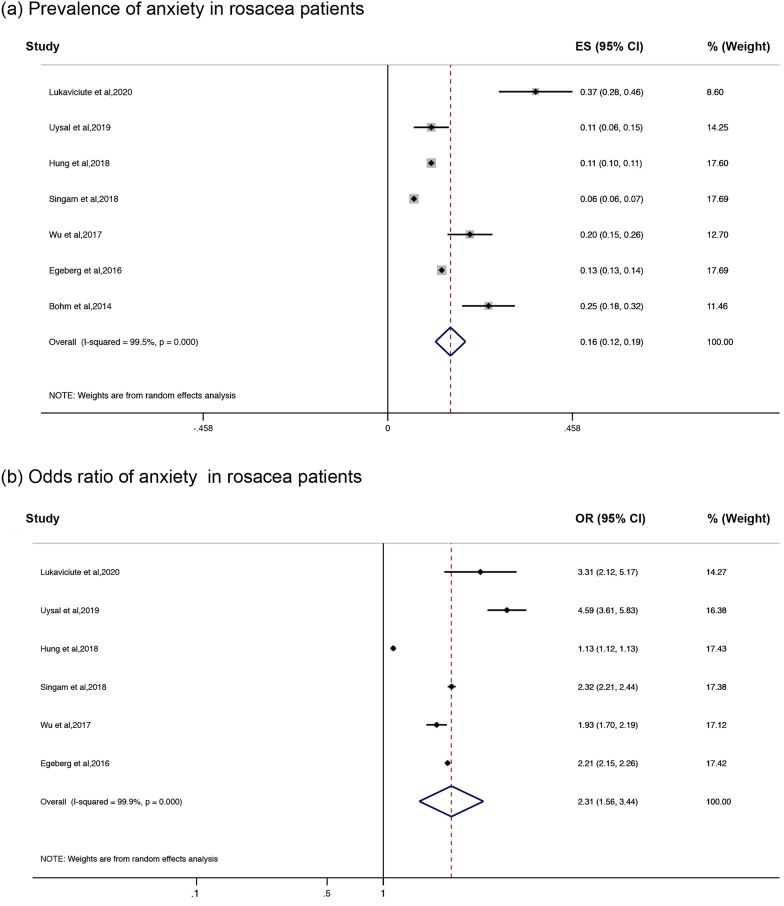
Association of Anxiety and Rosacea
A total of seven studies examined the prevalence of anxiety in patients with rosacea (Fig. 3a, Table 2). The pooled random-effects prevalence of any anxiety was 15.6% (95% CI 11.8–19.3%). Heterogeneity across studies was evident (I2 = 99.5%, P < 0.01). A further subgroup analysis revealed that the prevalence of anxiety was 12.1% (95% CI 9.6–14.7%) in the general populations, whereas in hospital-based populations, the prevalence was 19.2% (95% CI 9.9–28.6%). When stratified by different methods to assess anxiety, the prevalence of anxiety in patients determined using screening questionnaires was 22.7% (95% CI 12.9–32.5%), and the prevalence of anxoius patients when measuring outcomes by ICD codes was 10.2% (95% CI 5.2–15.3%); these parameters were significantly different (P = 0.03). All rosacea patients in the seven studies were diagnosed by physicians or on the basis of ICD codes; therefore, no relevant subgroups analyses were performed. Three studies were conducted in Asia, and the overall prevalence was 13.4% (95% CI 8.5–18.3%); three were conducted in Europe, with a pooled prevalence of 24.4% (95% CI 11.1–37.8%). Only one study reported the anxiety percentage of rosacea patients in North America: 6.5% (95% CI 6.2–6.8%). In addition, the percentage of women (CV − 0.41, adj. R2 = 7.38%, τ2 = 0.008, P = 0.28), mean age (CV − 0.003, adj. R2 = − 14.53%, τ2 = 0.005, P = 0.56) and NOS scores (CV 0.03, adj. R2 = 19.99%, τ2 = 0.0027, P = 0.22) did not moderate the rate of anxiety in rosacea patients.
Fig. 3.
Forest plots of anxiety in rosacea patients. a Prevalence of anxiety. b Association of anxiety in rosacea patients versus healthy controls
Patients with rosacea were significantly more likely to have anxiety (6 out of 7 studies) with a pooled OR of 2.31 (95% CI 1.56–3.44; Fig. 3b). When recalculating the pooled estimate by omitting one study each time, the sensitivity analysis showed that the ORs for anxiety remained significant, which indicated that the summary estimates were sufficiently robust to exclude studies with different assessment criteria (ESM Fig. S1b).
Discussion
To our knowledge, our study is the first systematic review and meta-analysis to assess the prevalence rates and relative odds for depression and anxiety in patients with rosacea. In the present study, we found that 19.6% of rosacea patients were affected by depression and 15.6% had anxiety. The method by which depression and anxiety were diagnosed strongly influenced the proportion of patients with each condition. Persons with rosacea were at least twofold more likely to manifest signs of depression and anxiety compared with their healthy controls.
Five studies were conducted in a general population; these studies showed 16% of the general population were affected by depression and that 12% had anxiety. Nine studies were conducted in a hospital-based population, and the overall prevalence of depression and anxiety was 22 and 19%, respectively. Although the differences between these two populations were not significant either depression or anxiety, they may reflect differences in the occurrence of psychiatric disorders in the general rosacea population compared with rosacea patient populations selected from hospitals. One possible explanation could be the severity of rosacea between two populations. Egeberg et al. reported that the risk of patients with rosacea developing depression was positively associated with increasing rosacea severity [25]. Individuals with mild or moderate rosacea may not seek medical treatment, and thus the general population-based studies may better capture this group of patients, while the hospital-based population may be likely to include patients with severe symptoms who require medical treatment.
Notably, the methods used to diagnose depression and anxiety significantly influenced the reported prevalence of depression and anxiety (P < 0.05). Those studies which ascertained the outcomes of depression or anxiety using screening questionnaires tended to assess only depressive or anxious symptoms, and were more likely to overestimate the prevalence of both [37]. As a result, the pooled prevalence estimates of depression and anxiety defined by questionnaires were higher than those defined by ICD codes. Questionnaires are subjective, and responses may be interpreted as symptoms that are not necessarily indicative of clinical depression and anxiety [38]. A previous study found that the method by which rosacea was diagnosed also impacted the prevalence of rosacea [2]. However, in our study, there was no significant difference between the prevalence of depression among rosacea patients defined by the different methods, although the prevalence of depression was higher in self-reported rosacea patients, possibly due to the relatively low number of available studies (n = 2), potentially increasing the risk of random error. For anxiety disorders, all rosacea patients were defined by physicians or ICD codes, thus a subgroup analysis could not be conducted.
Generally, individuals with lightly pigmented skin (Fitzpatrick skin type I and II) are more likely to develop rosacea [39], and people with a Celtic and northern Europe background have a higher risk for this disease [5]. In the current study, we found that there was no significant difference in estimates of depression prevalence in the Europen, North American and Asian studies, despite the overall prevalence of depression being higher in Europe and North America than in Asia. One possible explanation is that the risk factor for rosacea may not be the same as that for depression. However, there were only three studies from North America and Asia, and thus the risk of random error may exist.
We found the that prevalence of depression and anxiety was independent of the mean age and gender distribution, although depression or anxiety was reported to be more prevalent among younger [15] and male [40] rosacea patients. A Danish nationwide cohort study showed that younger patients were at increased risk of developing depression [25]. One obvious explanation could be that younger people were more concerned about their facial appearance and hence more likely to feel depressed or anxious. In another online survey of representative subjects from the UK, France, Germany and USA, men reported feelings of stigmatization due to rosacea more frequently than women [33]. One possible explanation was that men suffered from more severe forms of rosacea.
Depression and anxiety disorders are common comorbidities in a range of skin disorders, including psoriasis [41], atopic dermatitis [42] and hidradenitis suppurativa [43]. In our study, we found rosacea also affected the psychological health of patients. Therefore, treatments for depression and anxiety among patients with rosacea are warranted. The effects of rosacea on facial appearance has been found to greatly impaired patients’ body image and self-esteem, which may result in psychosocial stress and psychiatric emergencies. The quality of life in rosacea patients has decreases; a meta-analysis using the Dermatology Life Quality Index (DLQI) showed that subjects with severe rosacea had worse mean DLQI scores than those with a moderate condition [16]. Adequate treatments of rosacea results in improved quality of life [44]. Psychological factors of depression and anxiety may physiologically exacerbate rosacea due to the release of inflammatory agents [45, 46]. It is reported that rosacea and depression share certain overlaps in terms of their inflammatory pathways [47–49] and that both cause increased levels of matrix metalloproteinase in serum [25, 50]. However, future prospective studies are needed to elucidate the mechanisms underlying the association between rosacea, depression and anxiety.
Certain limitations to our meta-analysis should be considered. First, heterogeneity was evident in our study, suggesting that differences in prevalence estimates between studies cannot be explained by random chance alone, but rather by factors such as study design, study quality and baseline characteristics. Meta-regression and subgroup analyses were conducted to attempt and explain this heterogeneity. The study quality represented by NOS scores contributed substantially to the heterogeneity, explaining 41.4% of the variability between studies, which indicated further investigations on studies with higher quality may reflect more reliable results. Second, our meta-analysis included nine studies that used screening instruments, such as HADS, for assessing mental disorders, and the subgroup analyses revealed a higher prevalence of depression or anxiety in studies using questionnaires than in those defined by a clinical criteria-based diagnosis. Thus, screening tools may overestimate the prevalence of rosacea in certain cases. Third, due to the small number of eligible studies, further investigations on publication bias among subsets were not possible. Another limitation of this review was that we were unable to provide adjusted data for confounders and data on rosacea phenotypes. It should also be noted that only three of included studies provided adjusted association metrics. Hence, more studies with potential confounding variables are required.
Conclusions
In conclusion, our study showed that patients with rosacea are at a higher risk for depression and anxiety. Our findings also highlight the great need for more efforts toward the awareness and management of depression and anxiety among rosacea patients. However, our results should be interpreted with caution since heterogeneity is evident in our study. Further large-scale studies of high quality are warranted to determine the complex relation of rosacea and psychiatric disorders, underlying mechanisms between them and optimal strategies for their management.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
Funding
This work was supported by the Science Foundation of Zhejiang province (LQ20H110002), Major Science and Technology Program for Medicine and Health in Zhejiang Province (WKJ-ZJ-2012) and Public Welfare Projects of Ningbo (202002N3190). The Journal's Rapid Service Fee is supported by Major Science and Technology Program for Medicine and Health in Zhejiang Province (WKJ-ZJ-2012).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
RD was involved in study conception and design. SLX, RD, BJL XTZ and YCL were involved in data acquisition. BJL and SlX performed the statistical analysis. SlX, RD and BJL were involved in the analysis and interpretation of the data. RD and SlX were responsible for manuscript preparation and approved the final version of the manuscript.
Disclosures
Ru Dai, BingJiang, Xuetong Zhang, Yuchen Lou and Suling Xu have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Footnotes
R. Dai and BJ. Lin contributed equally to this study.
References
- 1.Two AM, Wu W, Gallo RL, Hata TR. Rosacea: part I. Introduction, categorization, histology, pathogenesis, and risk factors. J Am Acad Dermatol. 2015;72(5):749–760. doi: 10.1016/j.jaad.2014.08.028. [DOI] [PubMed] [Google Scholar]
- 2.Gether L, Overgaard LK, Egeberg A, Thyssen JP. Incidence and prevalence of rosacea: a systematic review and meta-analysis. Br J Dermatol. 2018;179(2):282–289. doi: 10.1111/bjd.16481. [DOI] [PubMed] [Google Scholar]
- 3.Tan J, Berg M. Rosacea: current state of epidemiology. J Am Acad Dermatol. 2013;69(6 Suppl 1):S27–S35. doi: 10.1016/j.jaad.2013.04.043. [DOI] [PubMed] [Google Scholar]
- 4.Anzengruber F, Czernielewski J, Conrad C, et al. Swiss S1 guideline for the treatment of rosacea. J Eur Acad Dermatol Venereol. 2017;31(11):1775–1791. doi: 10.1111/jdv.14349. [DOI] [PubMed] [Google Scholar]
- 5.Elewski BE, Draelos Z, Dréno B, Jansen T, Layton A, Picardo M. Rosacea—global diversity and optimized outcome: proposed international consensus from the Rosacea International Expert Group. J Eur Acad Dermatol Venereol. 2011;25(2):188–200. doi: 10.1111/j.1468-3083.2010.03751.x. [DOI] [PubMed] [Google Scholar]
- 6.Abram K, Silm H, Maaroos HI, Oona M. Risk factors associated with rosacea. J Eur Acad Dermatol Venereol. 2010;24(5):565–571. doi: 10.1111/j.1468-3083.2009.03472.x. [DOI] [PubMed] [Google Scholar]
- 7.Wollina U. Is rosacea a systemic disease? Clin Dermatol. 2019;37(6):629–635. doi: 10.1016/j.clindermatol.2019.07.032. [DOI] [PubMed] [Google Scholar]
- 8.Vera N, Patel NU, Seminario-Vidal L. Rosacea comorbidities. Dermatol Clin. 2018;36(2):115–122. doi: 10.1016/j.det.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 9.Haber R, El Gemayel M. Comorbidities in rosacea: a systematic review and update. J Am Acad Dermatol. 2018;78(4):786–792.e8. doi: 10.1016/j.jaad.2017.09.016. [DOI] [PubMed] [Google Scholar]
- 10.Hua TC, Chung PI, Chen YJ, et al. Cardiovascular comorbidities in patients with rosacea: a nationwide case-control study from Taiwan. J Am Acad Dermatol. 2015;73(2):249–254. doi: 10.1016/j.jaad.2015.04.028. [DOI] [PubMed] [Google Scholar]
- 11.Egeberg A, Fowler JF, Jr, Gislason GH, Thyssen JP. Nationwide assessment of cause-specific mortality in patients with rosacea: a cohort study in Denmark. Am J Clin Dermatol. 2016;17(6):673–679. doi: 10.1007/s40257-016-0217-1. [DOI] [PubMed] [Google Scholar]
- 12.Spoendlin J, Voegel JJ, Jick SS, Meier CR. Migraine, triptans, and the risk of developing rosacea: a population-based study within the United Kingdom. J Am Acad Dermatol. 2013;69(3):399–406. doi: 10.1016/j.jaad.2013.03.027. [DOI] [PubMed] [Google Scholar]
- 13.Egeberg A, Hansen PR, Gislason GH, Thyssen JP. Clustering of autoimmune diseases in patients with rosacea. J Am Acad Dermatol. 2016;74(4):667–72.e1. doi: 10.1016/j.jaad.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 14.Egeberg A, Fowler JF, Jr, Gislason GH, Thyssen JP. Rosacea and risk of cancer in Denmark. Cancer Epidemiol. 2017;47:76–80. doi: 10.1016/j.canep.2017.01.006. [DOI] [PubMed] [Google Scholar]
- 15.Oussedik E, Bourcier M, Tan J. Psychosocial burden and other impacts of rosacea on patients' quality of life. Dermatol Clin. 2018;36(2):103–113. doi: 10.1016/j.det.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 16.Bewley A, Fowler J, Schöfer H, Kerrouche N, Rives V. Erythema of rosacea impairs health-related quality of life: results of a meta-analysis. Dermatol Ther (Heidelb) 2016;6(2):237–247. doi: 10.1007/s13555-016-0106-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gupta MA, Gupta AK, Chen SJ, Johnson AM. Comorbidity of rosacea and depression: an analysis of the National Ambulatory Medical Care Survey and National Hospital Ambulatory Care Survey-Outpatient Department data collected by the US National Center for Health Statistics from 1995 to 2002. Br J Dermatol. 2005;153(6):1176–1181. doi: 10.1111/j.1365-2133.2005.06895.x. [DOI] [PubMed] [Google Scholar]
- 18.Beaulieu P, Varlet JL, Savary J. The impact of rosacea on patients' daily life: a transverse observational study among private dermatologists. Ann Dermatol Venereol. 2012;139(3):222–224. doi: 10.1016/j.annder.2011.11.013. [DOI] [PubMed] [Google Scholar]
- 19.Su D, Drummond PD. Blushing propensity and psychological distress in people with rosacea. Clin Psychol Psychother. 2012;19(6):488–495. doi: 10.1002/cpp.763. [DOI] [PubMed] [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, PRISMA Group Altman DG preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 2 March 2020
- 22.Hamling J, Lee P, Weitkunat R, Ambühl M. Facilitating meta-analyses by deriving relative effect and precision estimates for alternative comparisons from a set of estimates presented by exposure level or disease category. Stat Med. 2008;27(7):954–970. doi: 10.1002/sim.3013. [DOI] [PubMed] [Google Scholar]
- 23.Furlan AD, Malmivaara A, Chou R, et al. 2015 updated method guideline for systematic reviews in the cochrane back and neck group. Spine (Phila Pa 1976) 2015;40(21):1660–1673. doi: 10.1097/BRS.0000000000001061. [DOI] [PubMed] [Google Scholar]
- 24.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 25.Egeberg A, Hansen PR, Gislason GH, Thyssen JP. Patients with rosacea have increased risk of depression and anxiety disorders: a Danish nationwide cohort study. Dermatology. 2016;232(2):208–213. doi: 10.1159/000444082. [DOI] [PubMed] [Google Scholar]
- 26.Alinia H, Cardwell LA, Tuchayi SM, et al. Screening for depression in rosacea patients. Cutis. 2018;102(1):36–38. [PubMed] [Google Scholar]
- 27.Incel Uysal P, Akdogan N, Hayran Y, Oktem A, Yalcin B. Rosacea associated with increased risk of generalized anxiety disorder: a case-control study of prevalence and risk of anxiety in patients with rosacea. An Bras Dermatol. 2019;94(6):704–709. doi: 10.1016/j.abd.2019.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wu Y, Fu C, Zhang W, Li C, Zhang J. The dermatology life quality index (DLQI) and the hospital anxiety and depression (HADS) in Chinese rosacea patients. Psychol Health Med. 2018;23(4):369–374. doi: 10.1080/13548506.2017.1361540. [DOI] [PubMed] [Google Scholar]
- 29.Hung CT, Chiang CP, Chung CH, Tsao CH, Chien WC, Wang WM. Risk of psychiatric disorders in rosacea: a nationwide, population-based, cohort study in Taiwan. J Dermatol. 2019;46(2):110–116. doi: 10.1111/1346-8138.14705. [DOI] [PubMed] [Google Scholar]
- 30.Singam V, Rastogi S, Patel KR, Lee HH, Silverberg JI. The mental health burden in acne vulgaris and rosacea: an analysis of the US National Inpatient Sample. Clin Exp Dermatol. 2019;44(7):766–772. doi: 10.1111/ced.13919. [DOI] [PubMed] [Google Scholar]
- 31.Spoendlin J, Bichsel F, Voegel JJ, Jick SS, Meier CR. The association between psychiatric diseases, psychotropic drugs and the risk of incident rosacea. Br J Dermatol. 2014;170(4):878–883. doi: 10.1111/bjd.12734. [DOI] [PubMed] [Google Scholar]
- 32.Böhm D, Schwanitz P, Stock Gissendanner S, Schmid-Ott G, Schulz W. Symptom severity and psychological sequelae in rosacea: results of a survey. Psychol Health Med. 2014;19(5):586–591. doi: 10.1080/13548506.2013.841968. [DOI] [PubMed] [Google Scholar]
- 33.Halioua B, Cribier B, Frey M, Tan J. Feelings of stigmatization in patients with rosacea. J Eur Acad Dermatol Venereol. 2017;31(1):163–168. doi: 10.1111/jdv.13748. [DOI] [PubMed] [Google Scholar]
- 34.Abram K, Silm H, Maaroos HI, Oona M. Subjective disease perception and symptoms of depression in relation to healthcare-seeking behaviour in patients with rosacea. Acta Derm Venereol. 2009;89(5):488–491. doi: 10.2340/00015555-0716. [DOI] [PubMed] [Google Scholar]
- 35.Dirschka T, Micali G, Papadopoulos L, Tan J, Layton A, Moore S. Perceptions on the psychological impact of facial erythema associated with rosacea: results of international survey. Dermatol Ther (Heidelb) 2015;5(2):117–127. doi: 10.1007/s13555-015-0077-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lukaviciute L, Ganceviciene R, Navickas P, Navickas A, Grigaitiene J, Zouboulis CC. Anxiety, depression, and suicidal ideation amongst patients with facial dermatoses (acne, rosacea, perioral dermatitis, and folliculitis) in Lithuania. Dermatology. 2020;236(4):314–322. doi: 10.1159/000506627. [DOI] [PubMed] [Google Scholar]
- 37.Pignone MP, Gaynes BN, Rushton JL, et al. Screening for depression in adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2002;136(10):765–776. doi: 10.7326/0003-4819-136-10-200205210-00013. [DOI] [PubMed] [Google Scholar]
- 38.Gilbody S, Sheldon T, House A. Screening and case-finding instruments for depression: a meta-analysis. CMAJ. 2008;178(8):997–1003. doi: 10.1503/cmaj.070281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang H, Liao W, Chao W, et al. Risk factors for sebaceous gland diseases and their relationship to gastrointestinal dysfunction in Han adolescents. J Dermatol. 2008;35(9):555–561. doi: 10.1111/j.1346-8138.2008.00523.x. [DOI] [PubMed] [Google Scholar]
- 40.Heisig M, Reich A. Psychosocial aspects of rosacea with a focus on anxiety and depression. Clin Cosmet Investig Dermatol. 2018;11:103–107. doi: 10.2147/CCID.S126850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dowlatshahi EA, Wakkee M, Arends LR, Nijsten T. The prevalence and odds of depressive symptoms and clinical depression in psoriasis patients: a systematic review and meta-analysis. J Invest Dermatol. 2014;134(6):1542–1551. doi: 10.1038/jid.2013.508. [DOI] [PubMed] [Google Scholar]
- 42.Patel KR, Immaneni S, Singam V, Rastogi S, Silverberg JI. Association between atopic dermatitis, depression, and suicidal ideation: a systematic review and meta-analysis. J Am Acad Dermatol. 2019;80(2):402–410. doi: 10.1016/j.jaad.2018.08.063. [DOI] [PubMed] [Google Scholar]
- 43.Machado MO, Stergiopoulos V, Maes M, et al. Depression and anxiety in adults with Hidradenitis Suppurativa: a systematic review and meta-analysis. JAMA Dermatol. 2019;155(8):939–945. doi: 10.1001/jamadermatol.2019.0759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Moustafa F, Lewallen RS, Feldman SR. The psychological impact of rosacea and the influence of current management options. J Am Acad Dermatol. 2014;71(5):973–980. doi: 10.1016/j.jaad.2014.05.036. [DOI] [PubMed] [Google Scholar]
- 45.Klaber R, Wittkower E. The pathogenesis of rosacea: a review with special reference to emotional factors. Br J Dermatol. 1939;51(12):501–524. [Google Scholar]
- 46.Reich A, Wójcik-Maciejewicz A, Slominski AT. Stress and the skin. G Ital Dermatol Venereol. 2010;145(2):213–219. [PubMed] [Google Scholar]
- 47.Maes M. Depression is an inflammatory disease, but cell-mediated immune activation is the key component of depression. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(3):664–675. doi: 10.1016/j.pnpbp.2010.06.014. [DOI] [PubMed] [Google Scholar]
- 48.Gerber PA, Buhren BA, Steinhoff M, Homey B. Rosacea: the cytokine and chemokine network. J Investig Dermatol Symp Proc. 2011;15(1):40–47. doi: 10.1038/jidsymp.2011.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sutcigil L, Oktenli C, Musabak U, et al. Pro- and anti-inflammatory cytokine balance in major depression: effect of sertraline therapy. Clin Dev Immunol. 2007;2007:76396. doi: 10.1155/2007/76396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Garvin P, Nilsson L, Carstensen J, Jonasson L, Kristenson M. Plasma levels of matrix metalloproteinase-9 are independently associated with psychosocial factors in a middle-aged normal population. Psychosom Med. 2009;71(3):292–300. doi: 10.1097/PSY.0b013e3181960e7f. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.