Abstract
Background
Determinants of COVID-19 vaccine acceptance are complex; how perceptions of the effectiveness of science, healthcare and government impact personal COVID-19 vaccine acceptance is unclear, despite all three domains providing critical roles in development, funding and provision, and distribution of COVID-19 vaccine.
Objective
To estimate impact of perception of science, healthcare systems, and government along with sociodemographic, psychosocial, and cultural characteristics on vaccine acceptance.
Design
We conducted a global nested analytical cross-sectional study of how the perceptions of healthcare, government and science systems have impacted COVID-19 on vaccine acceptance.
Setting
Global Facebook, Instagram and Amazon Mechanical Turk (mTurk) users from 173 countries.
Participants
7411 people aged 18 years or over, and able to read English, Spanish, Italian, or French.
Measurements
We used Χ2 analysis and logistic regression-derived adjusted Odds Ratios (aORs) and 95% CIs to evaluate the relationship between effectiveness perceptions and vaccine acceptance controlling for other factors. We used natural language processing and thematic analysis to analyse the role of vaccine-related narratives in open-ended explanations of effectiveness.
Results
After controlling for confounding, attitude toward science was a strong predictor of vaccine acceptance, more so than other attitudes, demographic, psychosocial or COVID-19-related variables (aOR: 2.1; 95% CI: 1.8 to 2.5). The rationale for science effectiveness was dominated by vaccine narratives, which were uncommon in other domains.
Limitations
This study did not include participants from countries where Facebook and Amazon mTurk are not available, and vaccine acceptance reflected intention rather than actual behaviour.
Conclusions
As our findings show, vaccine-related issues dominate public perception of science’s impact around COVID-19, and this perception of science relates strongly to the decision to obtain vaccination once available.
Keywords: COVID-19, public health, international health services
Strengths and limitations of this study.
Large sample size (n=7411) with significant global coverage (173 countries).
Study conducted in four languages (English, Italian, Spanish, French) where SARS-CoV-2 dominated at the time of data collection.
Qualitative and quantitative data integrate to generate key findings.
Recruitment for participation was through social media, which would under-represent people without internet or without social media presence.
Study was limited to the languages indicated.
Background
Implementation of a vaccination for COVID-19 is a core, essential component of the strategic plan in reducing the future burden of morbidity and mortality due to SARS-CoV-2 infection.1 Whether or not people are vaccinated is a complex intersection of personal factors that relate to interest and ability to obtain a vaccine, and to structural-systemic factors that govern access and availability.2 Public trust underlies much of the personal decision-making in accepting a vaccine. Confidence in accepting vaccination relies on community knowledge and expectation in science to develop and offer a safe and effective vaccine, along with the conviction that the healthcare system will successfully deliver the vaccine. Trust in science, government, and public health structures to support and promote vaccines encourages access and confidence.3
Trust in these systems, however, has proven challenging for many communities, and the WHO has registered ‘vaccine hesitancy’ as one of the main risks to global health.4 During outbreaks, many people are willing to receive a vaccine but not all do. Community resistance to vaccination does not necessarily revolve solely around biomedical considerations, as people express social, economic, religious or moral concerns that might overshadow the risk of acquiring the disease. Hence, the public confidence in vaccination programmes depends on healthcare, public health and in community governance.5 Trust in science, for example, is complex, given that the conduct of science inherently takes time, can generate a range of findings that reflect methodology and limitations of study design, and often requires complicated constructs and investigations.6 7 Science-informed policy can be vulnerable to politicisation as public communications and communities may not reflect the same understanding of the process as scientists themselves.8 9 Overcoming resistance to COVID-19 vaccination relies on enhancing communication to better explain science and policy options for disparate public audiences.10
An Italian survey regarding public response to COVID-19 found that trust in authorities was necessary to combat COVID-1911 and that, over time, trust in public authorities polarised. A survey from France found that 26% of respondents (n=1012) distrusted government and would not accept a vaccine against SARS-CoV-2 if available.12 The most reluctant to receive the vaccine were low-income people (37%), women 18–35 years old (36%) and people older than 75 years (22%).12 Often, under-represented communities distrust pharmaceutical and clinical trials, stemming from historical and systemic legacies of mistreatment, potentially leading to vaccine scepticism.13 Political disregard for scientific expertise only amplifies the vaccine-sceptic positions, recently highlighted as resistance to government-mandated immunisation requirements and the rise of conspiracy theories around COVID-19, sometimes perpetuated by celebrities.14 A 2019 study focused on 14 Western European countries suggested an association between the political populism and vaccine hesitance, showing a strong correlation between those who voted for populist parties and those who distrust and dismiss the vaccines as not important and not effective.15 Indeed, political polarisation is an important factor in vaccine acceptance, with the far left and far right voters stating they would refuse a vaccine if available.16 These findings show the importance of monitoring vaccine confidence and also the need to rebuild population’s trust in public health.
The influence of personal perceptions of effectiveness toward the impact of different systems (healthcare, science, government) on individual preference toward obtaining a COVID-19 vaccination is unknown, yet crucially important. If these perceptions were better understood, then public entities could incorporate those views in their promotion and implementation of COVID-19 vaccination to communities. Additionally, the relative importance of these influences (perception of healthcare, science and government system’s effectiveness) compared with other demographic and psychosocial determinants of vaccine acceptance is unknown, and could guide social marketing strategies to reduce vaccine hesitancy and increase COVID-19 vaccine uptake.
Methods
Study design
We conducted an analytical cross-sectional study17 of attitudes toward institutional effectiveness in addressing COVID-19 and intentions for accepting a COVID-19 vaccine if one was available. This analysis was nested within a wider mixed-methods study of COVID-19 lived experience18 around the world. Specifically, we aimed to examine associations between attitudes toward the effectiveness of healthcare systems, science, and of governments in acting against COVID-19 and participant acceptance for COVID-19 vaccine. The study’s overall design was guided by the Critical Medical Ecology theoretical framework that prioritises understanding context in analysing health, including systems and power relationships.19 The results presented are consistent with the Reporting of Studies Conducted using Observational Routinely-collected Data guidelines20 and we used the Strengthening the Reporting of Observational Studies in Epidemiology cross-sectional checklist when writing this report.21
Setting and participants
This study recruited participants from around the world through two social media channels to complete a REDCap (V.9.9.2, Vanderbilt University)-based online survey in one of four languages (English, French, Spanish and Italian). Potential respondents were reached using purchased ads in the four languages through Facebook, Instagram and the Facebook Audience Network, which has been shown to be an effective mechanism for reaching a worldwide population.22 23 We also recruited participants from Amazon’s Mechanical Turk (mTurk) digital workforce which complements the scope of Facebook-based recruitment.24 The survey was deployed between 6 April and 29 May 2020. During this period, the COVID-19 pandemic centred in English, French, Spanish and Italian-speaking countries around the world,25 hence the use of those four languages for the survey. The survey was developed and pretested in English, then translated into French, Spanish and Italian by professional translators who were native speakers. Potential participants were asked to confirm that they were 18 years or older, and could read the survey in one of the four languages offered. In total, 7411 participants were included in the final sample, the disposition of which is reported elsewhere.26
Survey
Once potential participants were routed from the social media site where they were recruited to the survey portal, they were presented with an informed consent document, asked to confirm they were 18 years or older and if they wanted to proceed. Participants continuing past consent were required to provide their country of residence, the only required variable in the survey. The survey ascertained a range of psychosocial indices and variables, including sets of questions specific to COVID-19 experience, attitudes and actions. Most COVID-19-related questions arose from the Kaiser Family Foundation Coronavirus Poll27 or were developed and pretested by the project team. The survey also provided opportunities for participants to explain their responses and perceptions in several open-ended questions. mTurk participants took an average of 36 min to complete the survey (completion time not available for Facebook participants). The surveys in English, Spanish, French and Italian are available as online supplemental materials 1–4.
bmjopen-2021-049716supp001.pdf (4.7MB, pdf)
bmjopen-2021-049716supp002.pdf (4.6MB, pdf)
bmjopen-2021-049716supp003.pdf (9.4MB, pdf)
bmjopen-2021-049716supp004.pdf (9.3MB, pdf)
Primary exposure
We ascertained participant perception of effectiveness of selected institutions and sectors regarding COVID-19 through a 4-point Likert scale applied to the following question (English/Spanish/French/Italian):
How effective do you feel each of the following groups have been in taking action against coronavirus and COVID-19?/¿Qué tan efectivo cree que fue cada uno de los siguientes grupos en tomar medidas en contra del coronavirus y COVID-19?/Dans quelle mesure estimez-vous que chacun des groupes suivants se montre efficace dans la lutte contre le coronavirus et le COVID-19 ?/In che misura ritieni che ciascuna delle seguenti categorie sia intervenuta efficacemente contro il coronavirus e il COVID-19?
The healthcare system (including hospitals, clinics, doctors, nurses and other health providers)/El sistema de salud (incluyendo hospitales, clínicas, médicos, enfermeros y otros proveedores de la salud)/Le système des soins de santé (y compris les hôpitaux, cliniques, médecins, infirmiers et autres prestataires de soins de santé)/Il sistema sanitario (compresi ospedali, ambulatori, medici, infermieri e altri operatori sanitari).
Science (including researchers and analysts)/La ciencia (incluyendo investigadores y analistas)/Le monde de la science (y compris les chercheurs et analystes)/La comunità scientifica (compresi ricercatori e analisti).
The government (including local and national governments)/El gobierno (incluyendo el gobierno local y nacional)/Le gouvernement (y compris les gouvernements locaux et nationaux)/Il governo (comprese le autorità locali e regionali).
For analysis, we collapsed the first two categories of the Likert scale and the last two categories of the Likert scale into a binary variable of effectiveness perception for each of the three domains (healthcare, science, government) into two categories for each (English or English equivalents: ‘very/somewhat effective’ vs ‘not very/not at all effective’).
Additionally, participants were asked in an open-ended question to explain their perception toward effectiveness. Those responses were captured as written and form unstructured data that supplemented the quantitative data.
Outcome measure
The primary outcome variable ascertained participants’ interest in receiving COVID-19 vaccine, if available, specifically worded as (English/Spanish/French/Italian):
If there was a vaccine that prevented people from getting sick from coronavirus, would you get the vaccine?/Si hubiera una vacuna para evitar que las personas contraigan coronavirus, ¿se pondría la vacuna?/S'il existait un vaccin qui empêche de contracter le coronavirus, vous feriez-vous vacciner?/Se esistesse un vaccino per impedire che le persone si ammalassero a causa del coronavirus, ti faresti vaccinare?
Participants could select three choices (‘yes’, ‘no’ and ‘don’t know’) which were reduced to two categories for analysis (‘yes’ vs ‘no/don’t know’).
Other measures
As the Critical Medical Ecology model19 was the framework used to design this entire study, other variables considered as potential confounders, effect modifiers or covariates between the relationship of institutional effectiveness perception and COVID-19 vaccine acceptance include a range of variables reflecting biological, sociocultural, healthcare and abiotic measures. Sociodemographic measures include country of residence (recoded into United Nations region), age, gender, education, material assets (home and car ownership); sociocultural measures include child or elder care responsibilities and religion; psychosocial measures include perceived social support, Multidimensional Health Locus of Control (MHLC), COVID-19-specific measures (COVID-19 knowledge, worry, personal impact, and family/personal COVID-19 infection, morbidity, and mortality), COVID-19 prevention strategies (mask procurement and use, social distancing and stayed home), and health measures (general health (Health-related Quality of Life (HRQOL‐14)), difficulty accessing healthcare, work in healthcare environment or have a chronic illness).
Sample size
Sample size for the parent project was computed (JMP Pro V.14.1.0 (SAS Institute, Cary, North Carolina, USA)) a priori based on the standardised T-scores of a non-medical COVID-19-related personal impact index, with the ability to detect a mean difference of 3 points from the standard mean of 50 (SD=10). With 99.9% confidence and 80.0% power, we estimated 380 participants were required per geographical region inflated by 50% to 570 to account for multivariate analysis, missing data and planned subanalyses. Recruitment occurred for the period of the survey until all regions exceeded the targeted sample size of 570.
For this specific analysis, we conducted a post hoc power computation of this study’s ability to detect a significant difference in vaccine acceptance by effectiveness perception. With an estimated two-sided confidence of 99%, our sample size exceeded 90% power to detect an effect size of at least 15% with normal approximation and continuity correction (JMP Pro V.15.0.0 (SAS Institute, Cary, North Carolina, USA)).
Statistical analysis
We used both Χ2 analysis and ORs with 95% CIs to assess the bivariate relationship between all study variables against the binary effectiveness perception variables for each domain (healthcare, science, government) and with vaccine acceptance. Logistic regression was conducted first entering the three effectiveness domains into single model (model 2) with vaccine acceptance, and following Hosmer-Lemeshow’s approach,28 then adding the other variables statistically or marginally associated (p<0.10) with both the effectiveness perception variables and the vaccine interest variable (model 3). To be included in the multivariate model, variables had to be associated with vaccine acceptance with p<0.10 and with at least two of the domains (p<0.10). All explanatory variables with a variance inflation factor value <0.05 and demonstrating linearity were retained in the model. We used multiple imputation to account for missing data,29 using the iterative Markov chain Monte Carlo method and logistic regression as the univariate model. Because the imputed results showed no significant variation from the observed results, we report only the observed multivariate summary measures (adjusted ORs and 95% CIs). Statistical significance was set at p<0.05 and IBM SPSS Statistics (V.27) was used for all analyses. The Hosmer-Lemeshow test for goodness of fit was used to assess the degree to which the data fit the final models.
Analysis of unstructured data
Participants were asked to explain the ratings they applied to their assessment of the effectiveness of science, healthcare and government. We used natural language processing (NLP) to ascertain frequency of words and phrases participants provided in their responses. We used the Text Explorer command in JMP Pro V.15.0.0 (2019 SAS Institute) with stemming and regular expression (regex) functions to quantify key terms and phrases. We present the magnitude and ranking of key words by each domain of effectiveness (science, healthcare and government) along with ranking the most common verb phrases with excerpts for each. Second, we had two analysts review the original responses and assemble thematic groupings based on content. The analyst-driven groupings supplemented the NLP-generated word and phrase frequencies with meaningful outliers and categories with semantic divergence from the NLP results. For the analysis of unstructured data, all phrases were translated to English with the analysis completed on the English words and phrases.
Public involvement
We iteratively pretested the instrument with a non-random selection of public participants, incorporating their feedback into the final version. Public comments were allowed on social media recruitment materials and advertisements about the topic, the study and participation. This study’s publications are widely disseminated through social media channels, and publications are made available through open access. Finally, we assessed participant experience and opinion of completing the survey with closed and open questions, enabling communication about their participation, the survey quality and others issues of importance. We considered public input in the construction of results and data interpretations from this project.
Results
Vaccination acceptance
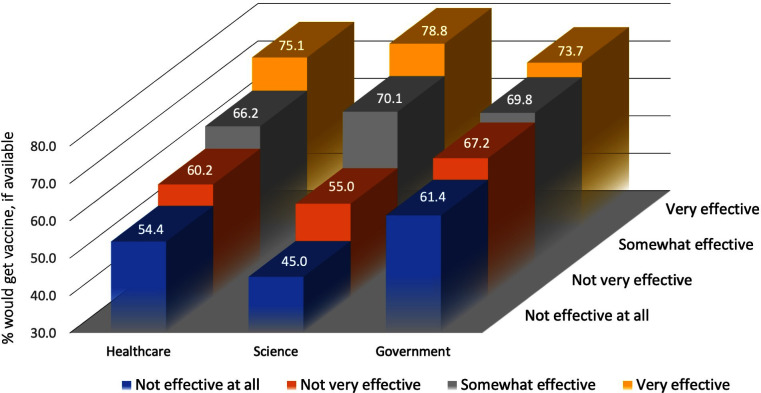
Overall, 68.7% of participants indicated they would accept the COVID-19 vaccine if it was available (table 1). Shown in figure 1, the vaccine acceptance rate increased with each rise in effectiveness ranking (not effective at all, not very effective, somewhat effective, very effective) across all three domains (healthcare, science and government). A statistically significant difference in vaccine acceptance rates was noted for all three domains (table 1) when reduced to ‘effective’ versus ‘not effective’ with ‘science’ noting the largest gap in vaccine acceptance: 73.8% of participants considering that science has been effective at taking action against COVID-19 indicated acceptance for a potential vaccine, while 52.1% of people who responded that science was not effective at taking action would accept the vaccine (p<0.001).
Table 1.
Association of selected demographic, psychosocial, COVID-19, and household characteristics and vaccine acceptance, perceived healthcare/science/government effectiveness
| Variable | If there was a vaccine that prevented people from getting sick from coronavirus, would you get the vaccine? | How effective do you feel the healthcare system (including hospitals, clinics, doctors, nurses and other health providers) has been in taking action against coronavirus and COVID-19? | How effective do you feel science (including researchers and analysts) has been in taking action against coronavirus and COVID-19? | How effective do you feel the government (including local and national governments) has been in taking action against coronavirus and COVID-19? | ||||
| Yes # (%) |
No/don’t know # (%) |
Effective # (%) |
Not effective # (%) |
Effective # (%) |
Not effective # (%) |
Effective # (%) |
Not effective # (%) |
|
| Total | 4729 (68.7) | 2154 (31.3) | 5954 (81.4) | 1358 (18.6) | 5577 (76.6) | 1700 (23.4) | 4456 (61.2) | 2824 (38.8) |
| Healthcare (effective) | 3989 (71.1)**** | 1623 (28.9) | – | – | 4961 (83.8)**** | 957 (16.2) | 4113 (69.5)**** | 1806 (30.5) |
| Healthcare (not effective) | 734 (58.4) | 523 (41.6) | – | – | 610 (45.2) | 740 (54.8) | 333 (24.7) | 1014 (75.3) |
| Science (effective) | 3878 (73.8)**** | 1377 (26.2) | 4961 (89.1)**** | 610 (10.9) | – | – | 3785 (68.2)**** | 1764 (31.8) |
| Science (not effective) | 826 (52.1) | 759 (47.9) | 957 (56.4) | 740 (43.6) | – | – | 642 (38.0) | 1047 (62.0) |
| Government (effective) | 2985 (71.4)**** | 1197 (28.6) | 4113 (92.5)**** | 333 (7.5) | 3785 (85.5)**** | 642 (14.5) | – | – |
| Government (not effective) | 1722 (64.6) | 942 (35.4) | 1806 (64.0) | 1014 (36.0) | 1764 (62.8) | 1047 (37.2) | – | – |
| Age <32 | 1443 (72.3)*** | 554 (27.7) | 1710 (85.0)*** | 301 (15.0) | 1615 (80.4)*** | 393 (19.6) | 1247 (62.3) | 756 (37.7) |
| Age 32+ | 2800 (68.1) | 1312 (31.9) | 3365 (81.6) | 760 (18.4) | 3140 (76.5) | 964 (23.5) | 2501 (60.8) | 1615 (39.2) |
| Gender male | 2214 (69.3) | 983 (30.7) | 2605 (81.2)** | 602 (18.8) | 2391 (74.8)**** | 806 (25.2) | 1937 (60.7)* | 1256 (39.3) |
| Gender female | 1946 (69.2) | 866 (30.8) | 2372 (84.0) | 453 (16.0) | 2276 (81.0) | 534 (19.0) | 1745 (61.9) | 1076 (38.1) |
| Gender other | 26 (72.2) |
10 (27.8) |
30 (83.3) | 6 (16.7) | 26 (72.2) | 10 (27.8) | 16 (44.4) | 20 (55.6) |
| Education HS or less | 609 (64.2)**** | 339 (35.8) | 781 (82.1) | 170 (17.9) | 700 (74.2)*** | 243 (25.8) | 579 (60.9) | 371 (29.1) |
| Education over HS | 3495 (70.5) | 1463 (29.5) | 4131 (83.0) | 847 (17.0) | 3906 (78.7) | 1057 (21.3) | 3044 (61.3) | 1919 (38.7) |
| Own home | 2906 (69.2) | 1291 (30.8) | 3482 (82.6)** | 733 (17.4) | 3238 (77.2) | 959 (22.8) | 2644 (63.0)**** | 1556 (37.0) |
| Do not own home | 1728 (67.8) | 821 (32.2) | 2056 (80.3) | 503 (19.7) | 1943 (76.3) | 603 (23.7) | 1486 (58.3) | 1065 (41.7) |
| Own car | 2924 (69.1) | 1306 (30.9) | 3528 (83.1)*** | 720 (16.9) | 3272 (77.3) | 960 (22.7) | 2587 (61.1) | 1650 (38.9) |
| Do not own car | 1718 (68.0) | 808 (32.0) | 2021 (79.7) | 514 (20.3) | 1915 (76.0) | 606 (24.0) | 1552 (61.5) | 972 (38.5) |
| Religion—not stated | 1632 (70.1)* | 697 (29.9) | 2220 (81.1) | 517 (18.9) | 2086 (76.6) | 637 (23.4) | 1587 (58.3)**** | 1134 (41.7) |
| Religion—stated | 3097 (68.0) | 1457 (32.0) | 3734 (81.6) | 841 (18.4) | 3491 (76.7) | 1063 (23.3) | 2869 (62.9) | 1690 (37.1) |
| Region | ||||||||
| Africa | 284 (58.6)**** | 201 (41.4) | 427 (74.8)**** | 144 (25.2) | 381 (67.1)**** | 187 (32.9) | 330 (58.5)**** | 234 (41.5) |
| Latin America and the Caribbean | 1164 (76.6) | 355 (23.4) | 1104 (67.7) | 526 (32.3) | 1214 (74.9) | 407 (25.1) | 777 (47.8) | 848 (52.2) |
| Europe | 1071 (71.8) | 421 (28.2) | 1333 (87.0) | 200 (13.0) | 1170 (76.6) | 358 (23.4) | 873 (57.0) | 659 (43.0) |
| Asia | 924 (68.8) | 419 (31.2) | 1213 (84.4) | 225 (15.6) | 1122 (78.5) | 307 (21.5) | 1094 (76.7) | 333 (23.3) |
| Oceania | 300 (65.1) | 161 (34.9) | 419 (87.7) | 59 (12.3) | 390 (81.6) | 88 (18.4) | 386 (80.6) | 93 (19.4) |
| Northern America | 986 (62.3) | 597 (37.7) | 1458 (87.7) | 204 (12.3) | 1300 (78.6) | 353 (21.4) | 996 (60.3) | 657 (39.7) |
| Reside in other than Africa | 4445 (69.5)**** | 1953 (30.5) | 5527 (82.0)**** | 1214 (18.0) | 5196 (77.4)**** | 1513 (22.6) | 4126 (61.4) | 2590 (38.6) |
| Reside in Africa region | 284 (58.6) | 201 (41.1) | 427 (74.8) | 144 (25.2) | 381 (67.1) | 187 (32.9) | 330 (58.5) | 234 (41.5) |
| COVID-19 knowledge high | 2913 (73.4)**** | 1054 (26.6) | 3532 (85.2)**** | 613 (14.8) | 3323 (80.3)**** | 814 (19.7) | 2462 (59.5)**** | 1677 (40.5) |
| COVID-19 knowledge low | 1808 (62.7) | 1076 (37.3) | 2405 (76.8) | 727 (23.2) | 2236 (71.9) | 872 (28.1) | 1980 (63.7) | 1128 (36.3) |
| COVID-19 worry low | 2346 (65.0)**** | 1264 (35.0) | 3141 (83.5)**** | 621 (16.5) | 2868 (76.5) | 883 (23.5) | 2354 (62.6)*** | 1404 (37.4) |
| COVID-19 worry high | 2382 (72.9) | 887 (27.1) | 2796 (79.3) | 732 (20.7) | 2698 (76.9) | 811 (23.1) | 2091 (59.7) | 1414 (40.3) |
| COVID-19 impact score low | 2375 (67.1)*** | 1162 (32.9) | 3042 (83.9)**** | 583 (16.1) | 2745 (76.1) | 860 (23.9) | 2254 (62.3)** | 1364 (37.7) |
| COVID-19 impact score high | 2345 (70.7) | 970 (29.3) | 2755 (79.1) | 728 (20.9) | 2690 (77.4) | 784 (22.6) | 2079 (60.0) | 1388 (40.0) |
| No family/friend has COVID-19 | 3606 (68.0)** | 1697 (32.0) | 4709 (82.3)**** | 1014 (17.7) | 4388 (77.1) | 1306 (22.9) | 3589 (63.0)**** | 2108 (37.0) |
| Family/friend has COVID-19 | 1123 (71.1) | 457 (28.9) | 1245 (78.4) | 344 (21.6) | 1189 (75.1) | 394 (24.9) | 867 (54.8) | 716 (45.2) |
| No family/friend died COVID-19 | 4277 (69.3)*** | 1896 (30.7) | 5471 (82.9)**** | 1125 (17.1) | 5096 (77.6)**** | 1472 (22.4) | 4062 (61.9)*** | 2504 (38.1) |
| Family/friend died COVID-19 | 452 (63.7) | 258 (36.3) | 483 (67.5) | 233 (32.5) | 481 (67.8) | 228 (32.2) | 394 (55.2) | 320 (44.8) |
| Do not believe have had COVID-19 | 4311 (69.0)* | 1935 (31.0) | 5179 (82.7)**** | 1083 (17.3) | 4838 (77.5)**** | 1401 (22.5) | 3872 (62.0)**** | 2369 (38.0) |
| Believe have had COVID-19 | 399 (65.3) | 212 (34.7) | 435 (71.0) | 178 (29.0) | 415 (68.4) | 192 (31.6) | 312 (50.9) | 301 (49.1) |
| Bought/used mask | 3905 (72.3)**** | 1493 (27.7) | 4610 (82.1)** | 1003 (17.9) | 4395 (78.7)**** | 1193 (21.3) | 3439 (61.5) | 2149 (38.5) |
| Did not buy/use mask | 782 (55.7) | 622 (44.3) | 1151 (79.5) | 297 (20.5) | 1018 (70.4) | 428 (29.6) | 868 (59.9) | 582 (40.1) |
| Social distancing observed | 4389 (71.8)**** | 1723 (28.2) | 5085 (83.0)**** | 1045 (17.0) | 4800 (78.6)**** | 1306 (21.4) | 3780 (61.8)*** | 2339 (38.2) |
| Social distancing not observed | 334 (43.9) | 426 (56.1) | 542 (71.1) | 220 (28.9) | 469 (62.0) | 287 (38.0) | 419 (55.8) | 332 (44.2) |
| Stayed home | 4080 (71.6)**** | 1620 (28.4) | 4898 (83.0)**** | 1005 (17.0) | 4636 (78.8)**** | 1247 (21.2) | 3639 (61.9)*** | 2243 (38.1) |
| Did not stay home | 577 (55.1) | 471 (44.9) | 818 (74.8) | 276 (25.2) | 737 (67.7) | 351 (32.3) | 627 (57.4) | 466 (42.6) |
| No childcare responsibilities | 2833 (71.0)**** | 1158 (29.0) | 3357 (83.9)**** | 642 (16.1) | 3153 (79.2)**** | 829 (20.8) | 2382 (59.7)*** | 1607 (40.3) |
| Childcare responsibilities | 1718 (65.7) | 897 (34.3) | 2077 (79.0) | 553 (21.0) | 1926 (73.5) | 693 (26.5) | 1673 (63.9) | 947 (36.1) |
| No elder care responsibilities | 3082 (70.2)*** | 1311 (29.8) | 3676 (83.5)**** | 726 (16.5) | 3419 (77.9)*** | 969 (22.1) | 2626 (59.8)*** | 1766 (40.2) |
| Elder care responsibilities | 1519 (66.4) | 770 (33.6) | 1814 (78.7) | 490 (21.3) | 1712 (74.8) | 576 (25.2) | 1468 (64.1) | 823 (35.9) |
| General health excellent/good | 4339 (77.5) | 1262 (22.5) | 4654 (82.8)** | 969 (17.2) | 4339 (77.5) | 1262 (22.5) | 3485 (62.2)**** | 2121 (37.8) |
| General health fair/poor | 555 (76.8) | 168 (23.2) | 577 (79.4) | 150 (20.6) | 555 (76.8) | 168 (23.2) | 396 (54.6) | 329 (45.4) |
| No difficulty accessing care | 3391 (69.8)* | 1468 (30.2) | 4112 (84.3)**** | 764 (15.7) | 3831 (78.9)**** | 1023 (21.1) | 3039 (62.5)**** | 1823 (37.5) |
| Difficulty accessing care | 959 (67.4) | 463 (32.6) | 1080 (75.6) | 348 (24.4) | 1038 (72.9) | 385 (27.1) | 810 (56.9) | 613 (43.1) |
| Work in healthcare | 588 (70.9) | 241 (29.1) | 653 (78.1)*** | 183 (21.9) | 638 (77.1) | 190 (22.9) | 505 (60.8) | 326 (39.2) |
| Do not work in healthcare | 4141 (68.4) | 1913 (31.6) | 5301 (81.9) | 1135 (18.1) | 4939 (76.6) | 1510 (23.4) | 3951 (61.3) | 2498 (38.7) |
| Have chronic disease | 1082 (72.3)**** | 414 (27.7) | 1209 (80.5) | 292 (19.5) | 1117 (75.1) | 371 (24.9) | 903 (60.3) | 595 (39.7) |
| Do not have chronic disease | 3647 (67.7) | 1740 (32.3) | 4745 (81.7) | 1066 (18.3) | 4460 (77.0) | 1329 (23.0) | 3553 (61.4) | 2229 (38.6) |
| High level of Perceived Social Support (PSS) | 2319 (74.5)**** | 792 (25.5) | 2692 (86.3)**** | 429 (13.7) | 2551 (82.1)**** | 557 (17.9) | 2009 (64.4)**** | 1111 (35.6) |
| PSS Social Support low | 1878 (63.7) | 1069 (36.3) | 2317 (78.3) | 642 (21.7) | 2142 (72.6) | 807 (27.4) | 1697 (57.6) | 1249 (42.4) |
| Multidimensional Health Locus of Control (MHLC) internal health locus low | 2111 (69.9) | 907 (30.1) | 2602 (82.3) | 561 (17.7) | 2419 (76.7) | 734 (23.3) | 1860 (58.9)**** | 1300 (41.1) |
| MHLC internal health locus high | 2454 (68.1) | 1147 (31.9) | 3128 (81.0) | 734 (19.0) | 2957 (77.0) | 884 (23.0) | 2420 (63.1) | 1414 (36.9) |
| MHLC chance health locus low | 2412 (73.7)**** | 862 (26.3) | 2824 (81.8) | 629 (18.2) | 2734 (79.4)**** | 710 (20.6) | 2062 (59.9)** | 1379 (40.1) |
| MHLC chance health locus high | 2153 (64.1) | 1208 (35.9) | 2922 (81.5) | 663 (18.5) | 2647 (74.2) | 922 (25.8) | 2239 (62.7) | 1332 (37.3) |
| MHLC powerful others locus high | 2226 (72.3)**** | 852 (27.7) | 2706 (81.7) | 608 (18.3) | 2541 (77.1) | 754 (22.9) | 2167 (65.8)**** | 1126 (34.2) |
| MHLC powerful others locus low | 2360 (65.8) | 1226 (34.2) | 3057 (81.3) | 702 (18.7) | 2872 (76.6) | 877 (23.4) | 2150 (57.3) | 1601 (42.7) |
*P<0.10; **p<0.05; ***p<0.01; ****p<0.001.
HS, high school; MHLC, Multidimensional Health Locus of Control.
Figure 1.
COVID-19 vaccination acceptance rates by effectiveness rating and domain.
Vaccine acceptance was significantly higher (p<0.001) among younger (age <32 years) participants and among those with more education (>high school). Participants residing in Africa were significantly less likely than all other regions to accept a potential vaccine (58.6% vs 69.5%, respectively), with Latin America and the Caribbean residents most likely (76.6%) to accept a vaccine.
Participants with higher COVID-19-related knowledge were more likely to accept a vaccine than those with lower levels of COVID-19-related knowledge (p<0.001). While those participants with more COVID-19-related worry and higher levels of COVID-19-related non-medical impact were also more likely to indicate vaccine acceptance (p<0.001), those participants with direct COVID-19-related experience (had a family or friend die from COVID-19, or believed they have COVID-19 themselves) were less likely to indicate vaccine acceptance. Participants demonstrating adherence to COVID-19 prevention strategies (masking, social–physical distancing and staying home) were significantly more likely (p<0.001) to indicate vaccine acceptance. While vaccine acceptance did not vary by general health status nor healthcare-related employment (table 1), vaccine acceptance was significantly higher among participants with a chronic disease (p<0.001).
Participants reporting higher levels of social support were more likely to indicate vaccine acceptance (p<0.001) as were participants who felt their health was less likely to be a function of chance (ie, lower levels on the ‘chance’ subscale of the MHLC). Participants who scored higher on the ‘powerful others’ subscale (ie, one’s health is controlled by powerful external entities, like doctors or government) of the MHLC were more likely to indicate vaccine acceptance (p<0.001).
Domain effectiveness
Overall, participants who indicated the highest level of perceived effectiveness (table 1) in addressing COVID-19 was in the healthcare system (81.4%), followed by science (76.6%) and government (61.2%). Younger people (<age 32 years) and women were significantly more likely to consider healthcare systems and science effective at addressing COVID-19 than their older counterparts aged 32 years or older, or males/other genders. Participants with more than high school education were more likely to believe that science (not healthcare nor government) was effective at addressing COVID-19. Identifying with a religion was not related to perceptions of healthcare effectiveness nor science effectiveness, but was significantly associated with perceptions of government effectiveness: participants identifying with a religion were significantly (p<0.001) more likely to consider governments effective at addressing COVID-19 than participants not identifying with religion.
Material assets were inconsistently associated with perceptions of domain effectiveness. Homeowners were significantly more likely to feel that healthcare and government were more effective at addressing COVID-19 than non-homeowners, and car owners were more likely to feel healthcare was effective than non-car owners. Neither home nor car ownership was associated with perception of science. Participants with childcare or elder care responsibilities were significantly more likely to consider governments as effective at addressing COVID-19—and significantly less likely to consider healthcare or science effective—than participants without those responsibilities.
Residents of Latin America and the Caribbean (LAC) were significantly (p<0.001) the least likely to consider healthcare systems effective at addressing COVID-19, followed by residents of Africa, and then residents from other parts of the world. LAC residents were also least likely to consider governments effective at addressing COVID-19, followed by residents of Africa, Europe and Northern America. Residents of Asia and Oceania were significantly more likely to consider governments effective at addressing COVID-19 than residents of other parts of the world. Residents of Africa were least likely to believe science was effective at addressing COVID-19 compared with residents from other parts of the world.
Higher COVID-19-related knowledge was positively associated with healthcare and science effectiveness perceptions: participants with higher COVID-19-related knowledge were more likely to perceive healthcare and science systems as effective in addressing COVID-19. In contrast, higher COVID-19-related knowledge was inversely associated with perception of government effectiveness, with participants with higher levels of COVID-19-related knowledge perceiving governments as less effective than did those with lower levels of COVID-19-related knowledge. Participants with higher levels of COVID-19-related worry and higher levels of non-medical COVID-19-related impact were less likely to consider healthcare systems or government effective. Effectiveness perception of science was unrelated to COVID-19-related worry or impact.
Personal experience with COVID-19 was significantly and consistently associated with domain effectiveness perceptions: participants indicating they themselves, or a family member or friend, had COVID-19 or that a family member or friend had died from COVID-19 were less likely to consider all three systems effective at addressing COVID-19. Similarly, domain effectiveness perception was significantly and consistently positively associated with adherence to COVID-19-related prevention behaviours: participants reporting masking, social–physical distancing or staying home.
Participants indicating difficulties with accessing healthcare were significantly less likely to consider any of the domains (healthcare, science, government) effective in addressing COVID-19 when compared with participants not experiencing difficulties accessing healthcare. Participants with higher levels of all three domains of the MHLC (internal, chance, powerful others) were more likely to consider government as effective in addressing COVID-19.
Participants with higher levels of social support were significantly more likely to consider all domains as effective at addressing COVID-19 than were participants with lower levels of social support. Additionally, participants who considered that their health was largely up to chance were significantly less likely to consider science as effective at addressing COVID-19.
Multivariate results
Shown in table 2, science effectiveness perception is the domain most strongly associated with positive vaccine acceptance (model 1). Once adjusting for each domain (model 2), science effectiveness perception remains most strongly associated with positive vaccine acceptance, followed by perceived effectiveness of the healthcare system. Perception of government effectiveness did not remain a significant predictor of positive vaccine acceptance. After controlling for confounders (model 3), science effectiveness perception remains a significant predictor of positive vaccine acceptance, second in point estimate magnitude only to (though not significantly different from) social–physical distancing (data not shown). Once controlling for confounders in this model, healthcare effectiveness perception does not remain a significant predictor of positive vaccine acceptance. The Hosmer-Lemeshow goodness-of-fit test statistic remained non-significant, indicating the data fit the final model well.
Table 2.
Positive vaccine acceptance by domain effectiveness perception
| Perception of domain effectiveness in taking action against COVID-19 (effective vs not effective) | OR (with 95% CI) | ||
| Model 1 | Model 2 | Model 3 | |
| Healthcare | 1.8 (1.5 to 2.0) | 1.2 (1.1 to 1.4) | 1.0 (0.9 to 1.2) |
| Science | 2.6 (2.3 to 2.9) | 2.4 (2.1 to 2.7) | 2.1 (1.8 to 2.5) |
| Government | 1.4 (1.2 to 1.5) | 1.0 (0.9 to 1.2) | – |
Model 1: unadjusted, each domain with outcome alone.
Model 2: domains together.
Model 3: significant domains and potential confounders (stayed home,* social–physical distancing,* childcare responsibilities, COVID-19 knowledge,* social support,* procured/wore mask, age <32 years,* resident of Africa, elder care responsibilities, friend/family has/had COVID-19,* friend/family died from COVID-19, believe have had COVID-19, difficulties accessing care); *=remained in model.
Qualitative analysis
‘Vaccine’ was the most commonly mentioned word provided by participants when describing the rationale for their effectiveness rating of the science domain’s impact on COVID-19 (table 3). ‘Vaccine’ was not a prominent nor common feature, however, of participant rationale for their effectiveness ratings of healthcare system or government. For example, some of the most commonly polarised constructs surrounded beliefs that reflect uncertainty about COVID-19 and conflicts embedded within the research enterprise:
Table 3.
Most common words and phrases in describing effectiveness perception rationale, with excerpts
| Science (including researchers and analysts) | Healthcare system (including hospitals, clinics, doctors, nurses and other health providers) | Government (including local and national governments) |
| Science word count (#) | Healthcare word count (#) | Government word count (#) |
| 1. Vaccine (1128) | 1. Health providers/healthcare (561) | 1. Political (eg, govt, Trump, China) (1142) |
| 2. Virus (628) | 2. Virus (346) | 2. Virus (302) |
| 3. Cure (296) | 4. Treatments (341) | 3. Sceptical (eg, fake, lies, corruption) (90) |
| 5. Treatments (236) | 6. Political (eg, govt, Trump, China) (119) | 4. Health providers/healthcare (56) |
| 7. Political (eg, govt, Trump, China) (105) | 8. Fight (103) | 5. Fight (50) |
| 9. Hope (57) | 10. Cure (70) | 6. Treatments (39) |
| 11. Fight (53) | 12. Sceptical (eg, fake, lies, corruption) (66) | 7. Cure (19) |
| 13. Health providers/healthcare (18) |
14. Vaccine (27) | 8. Vaccine (13) |
| 15. Sceptical (eg, fake, lies, corruption) (15) | 16. Hope (6) | 9. Hope (10) |
|
Most common verb phrases (science) ‘find a vaccine’ (99) They're trying to find ways to get through this, prevent the spread, and find a vaccine. (Northern America) ‘working hard’ (90) Working hard to understand the virus, advise governments (who unfortunately don't always listen/react in time)… Working round the clock to find effective treatments and vaccines (Northern Europe) ‘trying to find’ (74) They are trying to find a cure or vaccine but there is so much conflict about how to do this and human trials are happening too quickly. (Northern America) ‘find a cure’ (59) We are knowing more about the virus because of their research. They are also trying to find a cure and vaccine… (Northern America) ‘develop a vaccine’ (35) Science cannot be rush to get a miracle cure. It needs time to develop a vaccine or cure and then test it. (Caribbean) |
Most common verb phrases (healthcare) ‘taking care’ (54) Only can speak of the area I'm in. But the medical system here has been performing admirably. Getting out needed information and taking care of the afflicted well. (Northern America) ‘working hard’ (49) The health providers, doctors and nurses of this country are acting selflessly and working hard to protect the nation from the threat. (South Asia) ‘risking their lives’ (25) They are the more affected by this crisis. They are risking their lives as treating people in health system that is not prepared for a pandemic. (Northern Europe) ‘trying their best’ (25) They are trying their best to cope with limited resources. (Southeast Asia) ‘save lives’ (24) Ils gèrent très bien cette crise à mon avis et se donne tout les moyen pour sauver des vies. (They are managing this crisis very well in my opinion and are doing everything they can to save lives.) (Western Europe) |
Most common verb phrases (government) ‘spread of the virus’ (44) Delayed response to the virus/pandemic. The government could have mitigated the spread of the virus if they acted fast and didn't downplay it. (Southeast Asia) ‘stop the spread’ (20) I think the [country] government have done an excellent job. After seeing what happened in [another country] I was relieved when our government took such drastic measures so quickly to stop the spread and give the hospitals a fighting chance at treating people. (Northern Europe) ‘measures taken’ (18) Political decisions have not taken into account the huge ethical, social, economical, and sanitary implications of extreme public health measures taken such as national lockdowns and measured them against the risk posed by the epidemic. (Southwestern Europe) ‘done a good job’ (16) Some governments such as in [names three countries], have done a good job containing the virus. Others have used it to benefit themselves ->turned it into a political game. (Western Europe) ‘mixed messages’ (14) Very high rates in [country]. Strong lockdown which has been effectively enforced. However there has been a lot of confusion about testing, payments to people in need and general mixed messages. (Southwestern Europe) |
| (Vaccine-related: Scientists are trying to get rid of this pandemic and work in to find new vaccine or medicine. (Oceania) For the scientists looking for a vaccine, I haven't heard much from them on their progress. (Oceania) Even though people are doubting science and scientists, I think they have been working hard to find a vaccine and how to treat those with Coronavirus. (Northern America) Hanno svolto un lavoro di ricerca molto utile, anche se per trovare vaccino ci vuole un altro po' di tempo. (They have done some very useful research work, although it takes a little longer to find the vaccine.) (Southern Europe) Thousands of people dying, no vaccine yet, come on people! (Northern America) |
Vaccine-related: Massiccio intervento da parte loro per contrastare la malattia. Conoscenze mediche e ricerca fondamentali allo sviluppo di un vaccine. Massive intervention on their part to counter the disease. (Medical knowledge and fundamental research for the development of a vaccine.) (Southern Europe) It’s because the healthcare system is just gambling around with the vaccine and research shows that they provide alkaline foods to infected persons because the virus survives in acidic conditions. (East Africa) A causa della mancanza di un vaccino, il sistema sanitario fa del suo meglio per prendersi cura dei pazienti, ma non sempre efficace. (Due to the lack of a vaccine, the health system does its best to take care of patients, but not always effective.) (South America) Everything they can do is in place except the vaccine. (South Asia) Etant donné l'absence de vaccin/remède, le personnel médical fait ce qu'il peut avec ce qu'il a. (Since there is no vaccine/cure, the medical staff do what they can with what they have.) (Western Europe) |
Vaccine-related: Supporting the healthcare system while supporting the research for a vaccine. (Northern America) The government has not created a vaccine or helped those who are out of work efficiently. (Northern America) Only taking advice from vaccine schills and ineffective global agencies. (Northern America) Contributing financially to get the vaccine and provision of free treatment to people tested positive. (Northern America) Could have (h)astened the vaccine discovery process. (South Asia) |
Still no vaccine has been invented. Not yet found from where this virus has come and what is the reason behind this. (Southern Europe)
E' stata trovato una cura per i malati tramite il plasma super immune, manca solo il vaccine. (A cure for the sick has been found through super immune plasma, only the vaccine is missing.) (Southern Europe)
Trop de limitations des chercheurs dues au carcan de la science empirique au lobby pharmaceutique au désir incontrole de faire paraitre des études… (Too many limitations of researchers, due to the shackles of empirical science and the pharmaceutical lobby, to the uncontrolled desire to publish studies…) (Western Europe)
Pienso que aun no se ha tomado muy enserio con la vacuna a las personas entendemos que es un proceso largo pero creo que se deber’a realizar algo mas rápido ya que la economía mundial esta afectando a los ciudadanos. (I think that people have not yet been taken very seriously with the vaccine, we understand that it is a long process but I believe that something should be done faster since the world economy is affecting citizens.) (Southwestern Europe)
Independent scientists who do not work for government or furthering political agendas are very thin on the ground and have very little airing of their work in the media. (Northern Europe)
With that said, much of the response to the effectiveness of science in responding to COVID-19 is related to the effort of science workers, with scientists viewed as responsible for the development (or lack thereof) of a vaccine:
Most trustworthy, reliable, objective. Working on the vaccine. (Northern Europe)
Science has helped in locating the vector for this disease (humans) and describing the DNA of the virus. But so far there’s no treatment nor a vaccine… (South America)
Avec les chercheurs qui trouveront les remedes. ([It is] with the researchers who will find the cures.) (Southern Africa)
Hacen lo que pueden para encontrar una vacuna, tengo confianza en la ciencia. (They do what they can to find a vaccine, I have confidence in science.) (Southwestern Europe)
La comunità scientifica è attualmente a pieno regime al lavoro sul vaccino e gli scienziati collaborano a stretto contatto con il governo per prendere le giuste decisioni per quanto riguarda il lockdown e le procedure sociali da rispettare per contenere il contagio (The scientific community currently at full capacity working on the vaccine and scientists collaborate closely with the government to make the right decisions regarding the lockdown and the social procedures to be followed to contain the contagion.) (Southern Europe)
I think scientists are working 24/7 to find a vaccine and have given their best advice to the Government. (Northern Europe)
They can make cars fly and change your heart and brain and eye color but somehow they can’t make an antivirus for a measly flu virus… (Northern America)
I am confident and hopeful that the all hands on deck approach will find a vaccine and or effective treatments for the illness quickly. (Northern America)
Too slow. We should improve our emergency science with less heavy protocol. (Western Europe)
Takes too long to get vaccine. (Northern America)
While mentioning vaccine-related issues was uncommon in participant rationale for effectiveness ratings of the healthcare system, several participants did mention similarly themed vaccine-related issues (impact of lack of vaccine on healthcare, conspiracy):
A causa della mancanza di un vaccino, il sistema sanitario fa del suo meglio per prendersi cura dei pazienti, ma non sempre efficace. (Due to the lack of a vaccine, the health system does its best to take care of patients, but not always effective.) (South America)
They are doing the best they can despite not having a vaccine, and there are cases of recovered patients (especially those with no underlying issues). (Northern America)
No estoy muy enterada de este tema, pero hay tantas teorías e información de gente diferente que ya no sabemos ni que es cierto y que no. (I am not very aware of this topic, but there are so many theories and information from different people that we no longer know what is true and what is not.) (Central America)
They won’t acknowledge cures that don’t make them money. Seem to be pushing the vaccine agenda for money and control. Are killing people because they won’t treat them properly… (Northern America)
Similarly, participants uncommonly mentioned vaccine-related issues in their rationale for their ratings of government effectiveness, but echoed the sentiments from the science and healthcare domains:
Contributing financially to get the vaccine and provision of free treatment to people tested positive. (Northern America)
The government has not created a vaccine or helped those who are out of work efficiently. (Northern America)
They aren’t giving any answers to how we will start to exit lockdown. We can’t stay locked up until a treatment or vaccine is found that could be 18 months from now. The country can’t afford to furlough people for that long. People will end up dying through starvation, abusive parents/partner, suicides will rise. (Northern Europe)
Discussion
Attitude toward the effectiveness of the science domain’s ability to impact COVID-19 was a strong predictor of vaccine acceptance, more so than attitudes toward healthcare or government effectiveness, or other demographic, psychosocial, or COVID-19-related variables. People with more positive attitudes toward science’s impact on COVID-19 were more likely to indicate acceptance for a COVID-19 vaccine than people with a negative attitude toward science’s impact, even after controlling for a wide range of confounding variables.
Our rate of COVID-19 vaccine acceptance (68.7%) was similar to the rates found by other studies from around the world. In a global survey conducted in June 2020 with 13 426 people in 19 countries, 71.5% of people said they would be very or somewhat likely to accept COVID-19 vaccine.30 Similarly, a study conducted in France found that 26% of participants would not take the vaccine.12 Moreover, in a study conducted in the UK, distrust was associated with unwillingness to get vaccinated against COVID-19.31 These attitudes were higher between ethnic minority groups. Italian studies also found that 44% of participants would not get vaccinated; in particular, older adults were less likely to get vaccinated than younger adults.32 This finding is worrisome because these groups are some of the societal groups that present a greater risk for clinical complications.33 In contrast, in a wide European study, 74% of participants expressed willingness to get vaccinated.34 Studies conducted in North America suggest that most participants between the USA and Canada expressed willingness to get vaccinated against COVID-19. For example, in a study conducted by Fisher et al, 58% of participants favoured the vaccine; however, 32% were uncertain about getting immunised against COVID-19.35 In addition, Reiter et al found that 69% of their participants were willing to receive the vaccine.36 This inclination toward vaccination was associated with participants’ healthcare provider’s recommendations. That said, vaccine acceptance has lagged in some areas of the world related to a range of factors.37 Overall, the main reasons in these studies against accepting a COVID-19 vaccine were related to efficacy, safety, mistrust against biomedical research and potential side effects.31 32 34
Trust is crucial for the success of public health policies. Governments can respond efficiently if their citizens feel confident in the public institutions looking out for their well-being and social cohesion.38 If too few people are willing to receive the COVID-19 vaccine when available, then the impact will be incomplete in halting the spread of disease, thus requiring a multilevel engagement and dialogue between the scientific community, government and population.32 As shown in our study, COVID-19 vaccine-related issues dominated participant attitudes around the effectiveness of science, even more so than treatments or cures. While effectiveness attitudes in all three domains (science, healthcare and government) and several important key variables were associated with vaccine acceptance initially (in particular, geographical residence in Africa, personal experience with COVID-19 as being personally infected, having family/friends infected or died), these variables did not remain significant in the multivariate model. The global conversation around COVID-19 vaccination dominates thoughts around science effectiveness, logically leading to these perceptions impacting willingness to obtain a vaccine when available. How science communicates in particular around vaccination is crucial in shaping this trust.8
While less strongly associated with COVID-19 vaccine acceptance than perceptions of science effectiveness, adherence to prevention behaviours (social–physical distancing, masking, staying home) was also strongly and significantly related to vaccine acceptance and remained in the model after controlling for other significant variables. As a result, positive COVID-19 vaccine acceptance may fit well with the recommended set of public health prevention strategies. Despite the effect of positive attitudes toward science on vaccine acceptance, however, some participants clearly held negative perceptions, mostly around existential beliefs about the COVID-19 pandemic itself and in viewing the scientific enterprise as collaborating with other entities with ulterior motives, or to deny populations the benefit of vaccines and treatment. Clearly, recognising efficient approaches, for example, knowledge sharing, to restore population trust in vaccination, is an essential issue that must be prioritised by governments and public health officials in order to counterbalance negative COVID-19 vaccination perceptions.39
Vaccine-related rationales were uncommon in justifying effectiveness rankings in the healthcare and government domains, despite the widespread belief that vaccines have been politicised. The few times vaccine-related issues arose in rationales around healthcare, they were viewed as absent from the sets of treatments available to the healthcare workforce. Vaccine-related issues mentioned in government effectiveness rationales often surrounded the role of government in supporting and distributing vaccines.
Our study is limited by its reliance on social media outlets to recruit participants. While these platforms provided access to much of the world and exceeded sample size requirements, participants in key countries (for example, China) without access to the platforms we used are not included in this analysis. Also, vaccine acceptance is hypothetical since COVID-19 vaccine was not available at the time of this analysis; participants could make different decisions when actually facing the opportunity to obtain vaccine. Finally, we did not consider higher levels of determinants of vaccine availability in this analysis at the country or wider levels. Our focus was on participant preference and perception of these additional multilevel determinants could, perhaps, temper our results.
Our findings contribute to better understanding of vaccine hesitancy, in that the primacy of belief in science’s effectiveness in addressing COVID-19—more so than the role of healthcare or government, or of direct COVID-19-related experiences, knowledge, and beliefs, or sociodemographic characteristics—on vaccine acceptance has not been previously described. Vaccine hesitancy needs to be examined in a multidimensional, sociocultural context as it challenges trust in the healthcare system, the healthcare workers who administer the vaccines, the policymakers who implement the vaccinations, the media communication surrounding vaccines, individual’s past experiences and individual’s knowledge.40 Vaccine hesitancy has been increasing due to social media disinformation campaigns that cast public doubt about their safety.38 Helping to communicate and improve the public’s understanding of science could help improve attitudes toward—and potentially uptake of—COVID-19 vaccine once available.
Conclusions
People’s confidence in accepting vaccination primarily depends on their knowledge and trust in science. In order to realise the full public health impact of COVID-19 vaccination, a call for equity-focused coordinated global response is warranted to halt the pandemic. Community-based groups and non-governmental organisations, such as the Red Cross, could be considered essential to build public trust in accepting COVID-19 vaccine.30 Public trust is fragile at best and emphasising any uncertainty regarding COVID-19 can erode public confidence; thus, clear and careful scientific communication is paramount in relaying support for scientific-based policies.8 As our findings show, vaccine-related issues dominate public perception of science’s impact around COVID-19, and this perception relates strongly to the decision to obtain vaccination once available.
Supplementary Material
Acknowledgments
We are grateful for the assistance of Connor DeAndrea-Lazarus, Kathleen Buckwell, Cody Gardner and Carrie Dykes for logistical assistance with developing and implementing aspects of this project. We appreciate the feedback of participants, the public and reviewers of our work.
Footnotes
Twitter: @GlobalHealthNow, @Jprglobalhealth
Contributors: TDD is the guarantor of this paper, and accepts full responsibility for the work and the conduct of the study, had access to the data, and controlled the decision to publish. TDD, EP, SS, JGPR and MB conceptualised this study and developed the methodology. TDD, HM and LA implemented analyses. TDD and EP obtained funding. TDD led the writing of this manuscript, and SS, HM, JP, MB and LA contributed to writing the original draft. TDD, SS, HM, JGPR, MB, LA and EP approved the final submitted version.
Funding: This work was funded by the Richard W and Mae Stone Goode Foundation (award # 057843-002). LA is a trainee in the University of Rochester’s Translational Biomedical Science PhD Program, which is supported by grant 2TL1TR002000-05 from the National Center For Advancing Translational Sciences, National Institutes of Health. LA is additionally funded by grant #BWF1014095 from the Burroughs Wellcome Fund. SS is supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number K12GM106997. We also accessed the recruitment and REDCap resources of the University of Rochester CTSA (award number UL1 TR002001) from the National Center for Advancing Translational Sciences of the National Institutes of Health.
Disclaimer: The funders had no role in the study design, data collection and analysis, decision to publish or preparation of this manuscript.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Given the identifying and potentially stigmatising nature of the data in this study, analyses are provided in this paper to support its conclusions, although datasets are not publicly available. Interested investigators can request data from the corresponding author.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study was performed in accordance with the ethical standards established by the 1964 Declaration of Helsinki and its later amendments. The University of Rochester’s Research Subjects Review Board determined that this study met federal and university criteria for exemption (Study #00004825). Participants consented to engage in this research after a review of a detailed information sheet presented in English, French, Spanish or Italian at the beginning of the REDCap survey. Participants could skip any question in the survey except the age screen and country of residence. All researchers and analysts involved in this study completed research, ethics and compliance training from the Collaborative Institutional Training Initiative (CITI Programme).
References
- 1.World Health Organization . COVID-19 strategy update. Geneva, Switzerland: World Health Organization Printing Office, 2020. [Google Scholar]
- 2.Access to Medicine Foundation . Access to vaccines index 2017: how vaccine companies are responding to calls for greater immunisation coverage. Amsterdam, The Netherlands: Access to Medicine Foundation, 2017. [Google Scholar]
- 3.Miton H, Mercier H. Cognitive obstacles to pro-vaccination beliefs. Trends Cogn Sci 2015;19:633–6. 10.1016/j.tics.2015.08.007 [DOI] [PubMed] [Google Scholar]
- 4.Hickler B, Guirguis S, Obregon R. Vaccine special issue on vaccine hesitancy. Vaccine 2015;33:4155–6. 10.1016/j.vaccine.2015.04.034 [DOI] [PubMed] [Google Scholar]
- 5.Harrison EA, Wu JW,. Vaccine confidence in the time of COVID-19. Eur J Epidemiol 2020;35:325–30. 10.1007/s10654-020-00634-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maher PJ, MacCarron P, Quayle M. Mapping public health responses with attitude networks: the emergence of opinion‐based groups in the UK’s early COVID‐19 response phase. Br J Soc Psychol 2020;59:641–52. 10.1111/bjso.12396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pechar E, Bernauer T, Mayer F. Beyond political ideology: the impact of attitudes towards government and corporations on trust in science. Sci Commun 2018;40:291–313. 10.1177/1075547018763970 [DOI] [Google Scholar]
- 8.Kreps SE, Kriner DL. Model uncertainty, political contestation, and public trust in science: evidence from the COVID-19 pandemic. Sci Adv 2020;6:eabd4563. 10.1126/sciadv.abd4563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goldenberg MJ. Antivaccination movement exploits public's distrust in scientific authority. BMJ 2019;367:l6960. 10.1136/bmj.l6960 [DOI] [PubMed] [Google Scholar]
- 10.Newhagen JE, Bucy EP. Overcoming resistance to COVID-19 vaccine adoption: how affective dispositions shape views of science and medicine. Harv Kennedy Sch Misinformation Rev 2020. 10.37016/mr-2020-44 [DOI] [Google Scholar]
- 11.Falcone R, Colì E, Felletti S, et al. All we need is trust: how the COVID-19 outbreak reconfigured trust in Italian public institutions. Front Psychol 2020;11:561747. 10.3389/fpsyg.2020.561747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peretti-Watel P, Seror V, Cortaredona S, et al. A future vaccination campaign against COVID-19 at risk of vaccine hesitancy and politicisation. Lancet Infect Dis 2020;20:769–70. 10.1016/S1473-3099(20)30426-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gamble VN. A legacy of distrust: African Americans and medical research. Am J Prev Med 1993;9:35–8. 10.1016/S0749-3797(18)30664-0 [DOI] [PubMed] [Google Scholar]
- 14.Hoffman J. Mistrust of a coronavirus vaccine could imperil widespread immunity, 2020. The New York times. Available: https://www.nytimes.com/2020/07/18/health/coronavirus-anti-vaccine.html
- 15.Kennedy J. Populist politics and vaccine hesitancy in Western Europe: an analysis of national-level data. Eur J Public Health 2019;29:512–6. 10.1093/eurpub/ckz004 [DOI] [PubMed] [Google Scholar]
- 16.COCONEL Group . A future vaccination campaign against COVID-19 at risk of vaccine hesitancy and politicisation. Lancet Infect Dis 2020;20:769–70. 10.1016/S1473-3099(20)30426-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang X, Cheng Z. Cross-sectional studies: strengths, weaknesses, and recommendations. Chest 2020;158:S65–71. 10.1016/j.chest.2020.03.012 [DOI] [PubMed] [Google Scholar]
- 18.Dye T, Levandowski B, Li D, et al. Multilevel analysis of personal, non-medical COVID-19-related impact worldwide. Ann Epidemiol 2020;52:116. 10.1016/j.annepidem.2020.08.060 [DOI] [Google Scholar]
- 19.De Ver Dye T, Muir E, Farovitch L, et al. Critical medical ecology and SARS-COV-2 in the urban environment: a pragmatic, dynamic approach to explaining and planning for research and practice. Infect Dis Poverty 2020;9:1–7. 10.1186/s40249-020-00694-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Benchimol EI, Smeeth L, Guttmann A, et al. The reporting of studies conducted using observational Routinely-collected health data (record) statement. PLoS Med 2015;12:e1001885. 10.1371/journal.pmed.1001885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Elm E, Altman DG, Egger M. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008;61. 10.1016/j.jclinepi.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 22.Kayrouz R, Dear BF, Karin E, et al. Facebook as an effective recruitment strategy for mental health research of hard to reach populations. Internet Interv 2016;4:1–10. 10.1016/j.invent.2016.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nelson EJ, Hughes J, Oakes JM, et al. Estimation of geographic variation in human papillomavirus vaccine uptake in men and women: an online survey using facebook recruitment. J Med Internet Res 2014;16:e198. 10.2196/jmir.3506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boas TC, Christenson DP, Glick DM. Recruiting large online samples in the United States and India: facebook, mechanical Turk, and Qualtrics. Political Sci Res Methods 2020;8:232–50. 10.1017/psrm.2018.28 [DOI] [Google Scholar]
- 25.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis 2020;20:533–4. 10.1016/S1473-3099(20)30120-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dye T, Levandowski B, Siddiqi S. Non-medical COVID-19-related personal impact in medical ecological perspective: a global multileveled, mixed method study. medRxiv 2020;12. 10.1101/2020.12.26.20248865 [DOI] [Google Scholar]
- 27.Hamel L, Lopez L, Muñana C. KFF health tracking poll March 2020, 2020. Available: https://www.kff.org/coronavirus-covid-19/poll-finding/kff-coronavirus-poll-march-2020/;
- 28.Hosmer Jr DW, Lemeshow S. Applied logistic regression. John Wiley & Sons, 2004. [Google Scholar]
- 29.Enders CK. Multiple imputation as a flexible tool for missing data handling in clinical research. Behav Res Ther 2017;98:4–18. 10.1016/j.brat.2016.11.008 [DOI] [PubMed] [Google Scholar]
- 30.Lazarus JV, Ratzan SC, Palayew A. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med 2021;27. 10.1038/s41591-020-1124-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Paul E, Steptoe A, Fancourt D. Anti-vaccine attitudes and risk factors for not agreeing to vaccination against COVID-19 amongst 32,361 UK adults: implications for public health communications. medRxiv 2020;10. 10.2139/ssrn.3716874 [DOI] [Google Scholar]
- 32.Palamenghi L, Barello S, Boccia S, et al. Mistrust in biomedical research and vaccine hesitancy: the forefront challenge in the battle against COVID-19 in Italy. Eur J Epidemiol 2020;35:785–8. 10.1007/s10654-020-00675-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Garnier-Crussard A, Forestier E, Gilbert T, et al. Novel coronavirus (COVID-19) epidemic: what are the risks for older patients? J Am Geriatr Soc 2020;68:939–40. 10.1111/jgs.16407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Neumann-Böhme S, Varghese NE, Sabat I. Once we have it will we use it? a European survey on willingness to be vaccinated against COVID-19. Springer, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fisher KA, Bloomstone SJ, Walder J. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of US adults. Ann Intern Med 2020;173. 10.7326/M20-3569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Reiter PL, Pennell ML, Katz ML. Acceptability of a COVID-19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine 2020;38:6500–7. 10.1016/j.vaccine.2020.08.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Al-Qerem WA, Jarab AS. COVID-19 vaccination acceptance and its associated factors among a middle Eastern population. Front Public Health 2021;9:34. 10.3389/fpubh.2021.632914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wilson SL, Wiysonge C. Social media and vaccine hesitancy. BMJ Glob Health 2020;5:e004206. 10.1136/bmjgh-2020-004206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Verger P, Dubé E. Restoring confidence in vaccines in the COVID-19 era. Expert Rev Vaccines 2020;19:991–3. 10.1080/14760584.2020.1825945 [DOI] [PubMed] [Google Scholar]
- 40.Dubé E, Laberge C, Guay M, et al. Vaccine hesitancy: an overview. Hum Vaccin Immunother 2013;9:1763–73. 10.4161/hv.24657 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-049716supp001.pdf (4.7MB, pdf)
bmjopen-2021-049716supp002.pdf (4.6MB, pdf)
bmjopen-2021-049716supp003.pdf (9.4MB, pdf)
bmjopen-2021-049716supp004.pdf (9.3MB, pdf)
Data Availability Statement
Data are available upon reasonable request. Given the identifying and potentially stigmatising nature of the data in this study, analyses are provided in this paper to support its conclusions, although datasets are not publicly available. Interested investigators can request data from the corresponding author.