Abstract
Objective:
To assess maxilla and mandibular arch widths' response to Haas-type rapid maxillary expansion (RME) anchored to deciduous vs permanent molars on children with unilateral posterior crossbite.
Materials and Methods:
Seventy patients with unilateral posterior crossbite recruited at the Universities of Genova, Siena, and Insubria (Varese) were randomly located into GrE (RME on second deciduous molars) or Gr6 (RME on first permanent molars) and compared.
Results:
Upper intermolar distance and permanent molar angulation increased significantly in Gr6 vs GrE at T1. Upper intercanine distance increased significantly in GrE vs Gr6 at T1 and T2. GrE showed significant increases for upper intermolar and upper intercanine widths. Gr6 showed statistically significant increases for upper intermolar widths, for upper and lower intercanine widths, and for increases of angulation of upper and lower permanent molars.
Conclusions:
GrE showed reduced molar angulation increases at T1 and reduced molar angulation decreases at T2 when compared with Gr6. At T2, the net increase of the upper intercanine distance in GrE was still significant compared with Gr6, indicating a more stable expansion in the anterior area.
Keywords: Rapid maxillary expansion, Multicentric randomized trial, Three-dimensional, Deciduous vs permanent molars
INTRODUCTION
Posterior crossbite is a common clinical condition often associated with transverse maxillary deficiency and functional mandibular shift. This frequent malocclusion is not self-correcting and can lead to the development of craniofacial asymmetries and mandibular dysfunction.1–3
The effects of rapid maxillary expansion (RME) on the maxillary complex have been highly investigated,4 reporting a maximum maxillary intermolar and intercanine width increase of 6.7 mm and 5.3 mm,5 respectively, when RME is banded on upper first permanent molars.
Literature6 also reported cases of periodontal and endodontic damage on RME anchoring teeth; therefore, some authors7–10 have suggested banding RME on primary teeth and reporting also different mean intermolar (3.6–4.1 mm)8,10 and intercanine width increases (5–5.9 mm).8,10
Few studies have investigated the changes in molar dental tipping and inclinations (on average from 3° up to 16.7°)9,11 following RME but comprised difficult (ie, barium sulfate solution)12 and more invasive examinations such as computed tomography and cone beam computed tomography (CBCT).13,14 Few articles8,15–17 concerning the indirect effects on mandibular arch following RME11,18–20 reported a low but statistically significant increase of lower intermolar (0.6621–0.97 mm)20 and intercanine width (0.9 mm).8,20 Since no studies in the literature have analyzed the differences in permanent vs primary molars as anchoring teeth for RME, the decision to band the permanent deciduous molars did not follow a clinical protocol, but an individual decision was made for each patient based on clinician experience.
The aim of the current study was to evaluate maxillary and mandibular arch widths' response to RME when it is anchored to the upper second deciduous molars or to the upper first permanent molars and to create a decision-making protocol for RME therapy in mixed-dentition patients.
MATERIALS AND METHODS
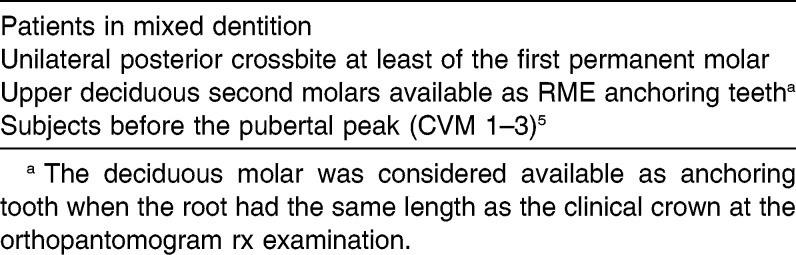
The design of this study was first approved by the Institutional Ethical Review Board of the Universities of Genova, Siena, and Insubria (Varese), Italy. Eighty-eight consecutive children presenting unilateral posterior crossbite were recruited in the corresponding three departments of orthodontics. The inclusion and primary and secondary exclusion criteria are shown in Tables 1 and 2. The final sample of patients comprised 70 subjects (31 boys and 39 girls; mean age, 8.4 ± 1.1 years) in Class I or Class II dental malocclusion with ANB <5°.
Table 1.
Inclusion Criteria
Table 2.
Exclusion Criteria and Number of Patients
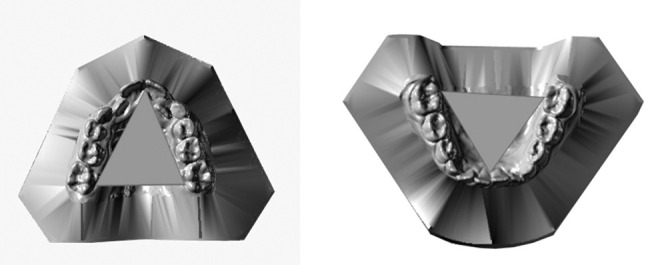
Subjects were randomly assigned to group GrE (RME on second deciduous molars; Figure 1a) or Gr6 (RME on first permanent molars; Figure 1b) by using a stratified blocked randomization with random block sizes performed by an electronic computer program. Patients were also stratified according to age and gender. The treating clinician was blinded from the randomization procedure, but because of clear differences in appliance design, blinding was not possible during the treatment period. The cast examiner was also blinded from the treatment protocol.
Figure 1.

(a) Haas-type RME banded on upper second deciduous molars. (b) Haas-type RME banded on upper first permanent molars.
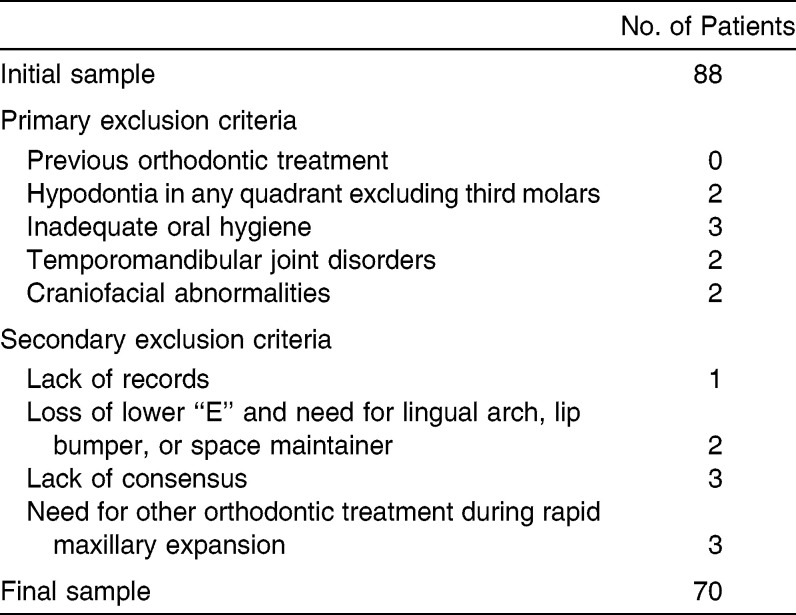
In GrE or Gr6, when RME was in situ, patients started the screw activation (Snap-lock expander screw, Forestadent, Pforzheim, Germany) of one-quarter turn a day (0.22 mm) until overcorrection was achieved (ie, the occlusal surface of the first maxillary palatal cusp contacted the occlusal surface of the mandibular first molar facial cusp), and the RME remained in place for 10 months. The screw was turned for 41 ± 8 days for GrE and for 35 ± 6 days for Gr6, and the average treatment time was 12 ± 1.3 months. Dental casts were taken at T0 (before the treatment) and at T1 (5 months after the end of the active treatment, with RME in situ in GrE to avoid second deciduous molar exfoliation and with RME temporarily removed for the impression in Gr6) and at T2 (5 months after T1), according to the protocol by Cozzani et al.8 The mean age of the patients at T0, T1 and T2 is reported in Table 3.
Table 3.
Patient Ages in the Two Analyzed Study Groups
Measurements on 3D Dental Casts
The maxillary and mandibular casts were processed by a three-dimensional (3D) scanner (NextEngine, Inc, Santa Monica, Calif), and landmarks were traced by means of Geomagic 3D Software (Research Triangle Park, Durham, NC). Measurements were subsequently calculated directly on scanned dental casts by means of ad hoc software. If cusp tips were worn, the centers of the resulting facets were used as landmarks.
Palatal and lingual measurements for maxillary and mandibular intermolar width were made at the point of intersection of the palatal or lingual groove with the cervical gingival margin (Figure 2a,b, line 1) according to McDougall et al.21
Figure 2.
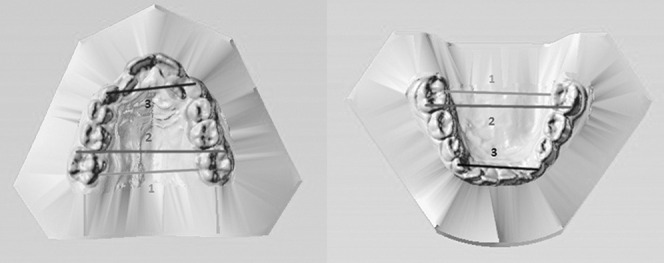
(a) Maxillary 3D dental cast. (b) Mandibular 3D dental cast. Line 1 = palatal maxillary and lingual mandibular intermolar width; line 2 = maxillary and mandibular vestibular intermolar width; line 3 = maxillary and mandibular intercanine width.
The upper and lower occlusal vestibular intermolar width was measured as the distance between mesiobuccal cusps tips of the first permanent molars bilaterally and the upper and lower intercanine width as the distance between cusp tips bilaterally (Figure 2a, b, lines 2 and 3). Two points per teeth were allowed to trace the facial axis of the clinical crown (FACC) of the first molars and deciduous canines at T0, T1, and T2 (Figure 3).
Figure 3.
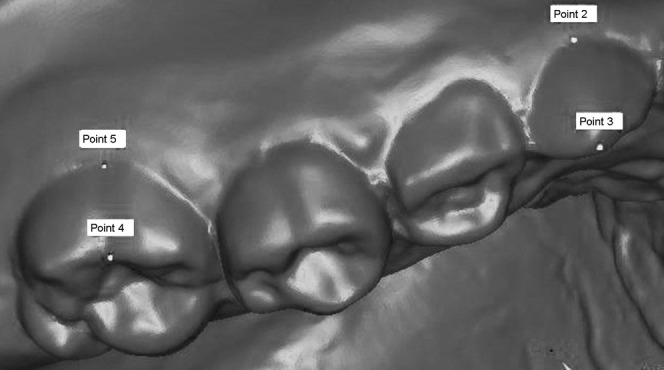
FACC of the upper right first permanent molar and upper right deciduous canine.
Also, three lingual or palatal points (interincisal papilla; right and left molar points at the intersection of the tooth and gingival margin between the two cusps) were used as a reference to trace a plane22 (Figure 4a,b). The angles between FACC and this reference plane were then measured. These angles corresponded to crown angulation on a reference plane (Figure 5a,b), and their clinical equivalent was the torque of the crown.23
Figure 4.
(a) Triangular reference plane for crown angulation in maxillary 3D dental cast. (b) Triangular reference plane for crown angulation in mandibular 3D dental cast.
Figure 5.
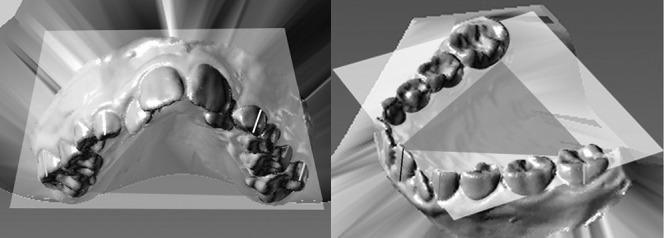
(a) Crown angulations of 1.6, 2.6, 5.3, and 6.3 in the maxillary 3D dental casts. (b) Crown angulations of 3.6, 4.6, 7.3. and 8.3 in the mandibular 3D dental casts.
Statistical Analysis
Method error
To standardize measurements, data were collected by the principal investigator and checked by another senior clinician. Measurements and landmark location were repeated (3 days after the first measurement) on 25 randomly selected casts to determine the error of method.
Dahlberg's values method error24 (inter- and intraoperator) was performed and ranged from 0.17 to 0.53 mm (not significant). Also, intraclass correlation coefficients25 were calculated, and all values were larger than .95. Standard deviations between repeated measurements were found to be in the range of 0.08 to 0.17 mm for all measurements and of 0.09° to 0.2° for angular measurement. Overall, the method error was considered negligible.
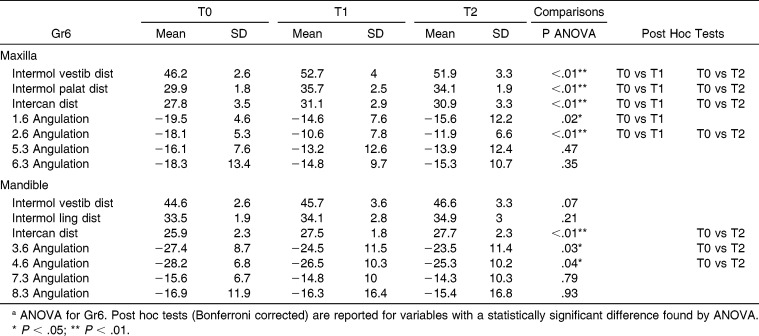
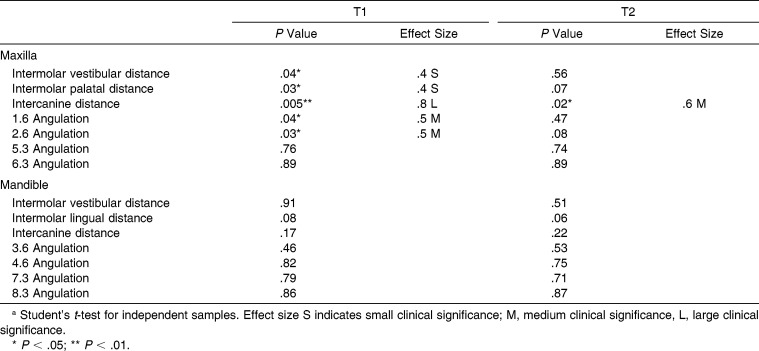
Descriptive statistics were computed for all analyzed variables (Tables 3, 4 and 5). Shapiro-Wilks test showed that data were normally distributed (W = 0.93 in Tables 4 and 5). A one-way repeated-measures analysis of variance (ANOVA; T0, T1, and T2 were the independent variables) was used to find statistically significant differences for the variables analyzed in the same group (widths and angulations). When a statistically significant difference was found, a post hoc test (Bonferroni corrected) was performed. In Table 6, GrE and Gr6 changes at T1 and at T2 were compared using Student's t-tests. Probabilities of less than .05 were accepted as significant in all statistical analyses (P < .05).
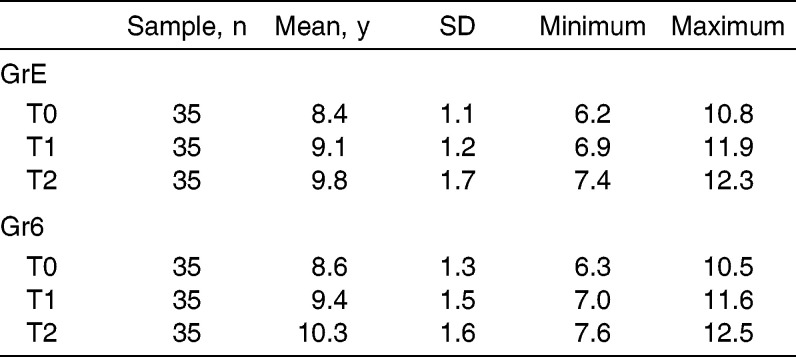
Table 4.
Dental Arch Distances (Unit: mm) and Crown Angulations (Unit: °) in GrE Patientsa
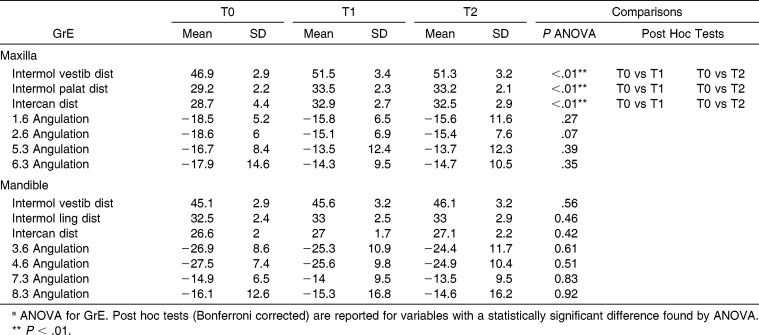
Table 5.
Dental Arch Distances (Unit: mm) and Crown Angulations (Unit: °) in Gr6 Patientsa
Table 6.
Comparison of Dental Arch Distances and Crown Angulations in Gr6 vs GrE Patients in the Two Analyzed Time Pointsa
Sample size was calculated a priori based on a primary outcome (molar expansion, as continuous outcome) to obtain a statistical power of the study greater than 0.85, using the mean values and standard deviations of maxillary molar expansion after RME therapy found by Cozzani et al.,8 at α = .05 and β = .2). Based on these parameters, to have an 85% chance of detecting as significant (at the two-sided 5% level) a five-point difference between the two groups, with an assumed standard deviation of 20 and a loss to follow-up of 20%, the sample size required was 30 patients in each group.
The effect size (ES) coefficient (d)26 was also calculated. An ES of .2 to .3 might be a “small” effect and thus a small clinically significant difference, about .5 a “medium” effect, and 0.8 to infinity a “large” effect.
RESULTS
Clinical crossbites were entirely corrected in 100% of the cases at T1 and at T2. At T2 in GrE, during the appliance debonding, 6 (8%) second deciduous molars were lost (removed with the RME).
No differences between GrE and Gr6 were found at T0 for age, sex distribution, or for the variables regarding dental measurements. At T1, there were no statistical differences (P = .4) for the screw activation between the groups.
Both ANOVA for GrE (Table 4) and ANOVA for Gr6 (Table 5) showed a statistically significant increase between T0–T1 and T0–T2 for upper intermolar vestibular and palatal widths and for upper intercanine width. Moreover, a statistically significant increase of the angulation of the upper right and left first permanent molars, of the lower intercanine distance, and of 3.6 and 4.6 angulations was also found in Gr6. When GrE was compared with Gr6 (Table 6), at T1, there were statistically significant larger increments of upper intermolar vestibular and palatal distances as well as of upper first right and left molar angulations in GR6 than GrE. The ES was small for upper intermolar vestibular and palatal distance and medium for 1.6 and 2.6 angulation. There was also a statistically significant larger increase of upper intercanine distance of 1.8 mm (P = .005) in GrE compared with Gr6. The ES was large.
At T2, GrE showed a statistically significant larger increase of upper intercanine distance of 1.6 mm (P = .02) in comparison with Gr6 patients. The ES result was medium.
DISCUSSION
All subjects were selected before the pubertal peak (CVM 1–3). In these three stages, RME patients exhibit significant and more effective long-term changes at the skeletal level in both maxillary and circummaxillary structures.27
Between T0 and T1, there was a significant larger increase of upper intermolar vestibular and palatal width together with a larger increase of 1.6 and 2.6 angulation in Gr6 vs GrE patients. Patients in GrE showed instead a trend of reduced angulation increases of 1.6 and 2.6 at T1 and reduced angulation decreases of the same teeth at T2. This is in accordance with Asanza et al.,28 who assessed that banded RME will produce tipping of the anchor tooth (an average of 3°) instead of true skeletal expansion, although this tipping is not considered clinically significant. Ferrario et al.11 found 17.6° of molar vestibular inclination increase, but that was due to the use of the less rigid NiTi palatal expander. In our study, we found also a small ES and thus a small clinical significance. Moreover, at T2, the significant difference for the increase of 1.6 and 2.6 angulation between Gr6 and GrE disappeared, thus indicating the same expansion conditions for both groups at the end of treatment. In GrE, the molar width increase is mainly related to the actual molar expansion (85%), and only a minor percentage was related to the angulation increase (15%). On the opposite, in Gr6, angulation produced 45% of the molar expansion.
At T1 and T2, we also found a significant larger increase of upper intercanine width in GrE vs Gr6 patients, which was not associated with differences in the increase of upper canine angulation. These results suggest a better and more stable expansion in the anterior area in GrE, probably due to a more anterior position of the screw. Regarding the lower arch, between T0 and T2, for both groups there was a general tendency of increase of lower molar and canine values together with increase of lower intermolar and intercanine widths, but no statistically significant differences between GrE and Gr6 were found, in accordance with Cozzani et al.8 Between T0–T1 and T0–T2, GrE patients showed a statistically significant increase of upper intermolar vestibular and lingual widths together with intercanine width. There was no statistically significant increase of the angulation of 1.6, 2.6, 5.3, or 6.3, thus indicating no dental tipping and dentoalveolar compensation. Although there was a general tendency of expansion of the lower arch, no statistically significant differences were found regarding the variables for the lower arch in GrE. In Gr6 patients, statistically significant increases of upper intermolar vestibular and lingual widths together with intercanine width were observed between T0–T1 and T0–T2. In this case, there was also a significant increase of the angulation of 1.6 and 2.6, indicating dental tipping and dentoalveolar compensation.11,29
In contrast with previous investigations,15–17 the present study did not find any statistically significant increase of lower intermolar width but rather a significant increase of lower 3.6 and 4.6 angulation (+6.8°, 2.9° right and 3.9° left) in Gr6 between T0 and T2 (Figure 6). This change was probably due to occlusal changes following 1.6–2.6 angulation increase so that the resultant force vector acting on the mandibular teeth (especially molars) was more vestibular directed, because the occlusal aspect of the lingual cusp of upper first molars contacted the occlusal aspect of the facial cusp of the lower first molars, as stated by Haas.18 Haas18 also associated these changes to the “lip bumper effect”; that is, the lateral movement of the maxillae widened the area of attachment of the buccal musculature.
Figure 6.
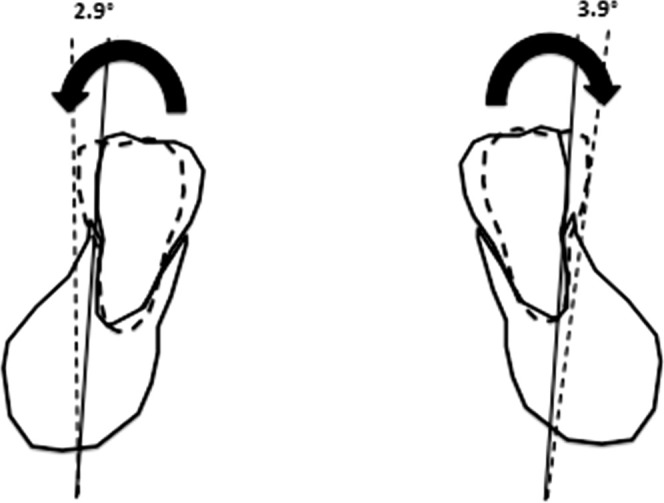
Lower increase molar angulation between T0 and T2.
In Gr6, a significant increase of lower intercanine width (mean of 1.8 mm) between T0 and T2 was also found, in accordance with previous studies.8,17,18
Two long-term retrospective trials reported the changes in untreated (Class I or Class II malocclusion but not crossbite) control groups.29,30 They found a reduction in mandibular arch perimeter, mainly related to the exfoliation of the mandibular second deciduous molars; a slight decrease in intercanine width; and very little or no increase in molar width. For ethical reasons, it was not possible to assemble a control group, since the crossbite is not a self-correcting situation. Moreover, emphasis was given to two different clinical procedures, and this was made with a longitudinal design, in which each patient was his or her own control.
In our study, a custom-designed digital procedure was used to evaluate tooth angulation measurements. Based on our previous investigation,23 this procedure showed good results in terms of reproducibility and reliability of the method, compared with other questionable methods to measure angulation of the crowns (eg, manual protractor, trimming models) Nevertheless, further comparisons between this method and new modern (but more invasive) measurement methods, such as CBCT, may help to confirm the effective reproducibility and reliability of the custom-designed digital procedure.
Although the literature considers a retention period of 6 months sufficient for patients undergoing RME treatment during their CVM 1–3,31,32 our procedure revealed interesting clinical aspects such as the stability of upper second deciduous molars in GrE: at T1, no anchoring teeth were lost, and at T2, only a small percentage (8%) of the anchoring deciduous molars remained attached to the bands of RME. Therefore, our inclusion criteria of availability of the second deciduous molars through orthopantomogram examination could be taken as a clinical reference in the evaluation of anchoring RME on deciduous teeth for an RME treatment of unilateral posterior crossbite.
CONCLUSIONS
GrE patients show reduced molar angulation increases at T1 and reduced molar angulation decreases at T2 (ie, less dental compensation) when compared with Gr6 patients. Moreover, at T2, the net increase of maxillary intercanine distance in GrE is still significant compared with Gr6, indicating a more stable expansion on the anterior region of the arch.
Transverse maxillary deficiency can be successfully corrected with RME on upper second deciduous molars, avoiding undesirable periodontal effects on permanent teeth when RME is anchored on the upper first permanent molars.
RME anchored on second deciduous molars was clinically efficient when the root of the anchoring tooth had at least the same length of the clinical crown at the orthopantomogram rx examination.
REFERENCES
- 1.McNamara J., Jr Maxillary transverse deficiency. Am J Orthod Dentofacial Orthop. 2000;117:567–570. doi: 10.1016/s0889-5406(00)70202-2. [DOI] [PubMed] [Google Scholar]
- 2.Thilander B, Wahlund S, Lennartsson B. The effect of early interceptive treatment in children with posterior cross-bite. Eur J Orthod. 1984;6:25–34. doi: 10.1093/ejo/6.1.25. [DOI] [PubMed] [Google Scholar]
- 3.Santos Pinto A, Buschang PH, Throckmorton GS, Chen P. Morphological and positional asymmetries of young children with functional unilateral posterior crossbite. Am J Orthod Dentofacial Orthop. 2001;120:513–520. doi: 10.1067/mod.2001.118627a. [DOI] [PubMed] [Google Scholar]
- 4.Petrén S, Bondemark L, Soderfeldt B. A systematic review concerning early orthodontic treatment of unilateral posterior crossbite. Angle Orthod. 2003;73:588–596. doi: 10.1043/0003-3219(2003)073<0588:ASRCEO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Lagravere MO, Heo G, Major PW, Flores-Mir C. Meta-analysis of immediate changes with rapid maxillary expansion treatment. J Am Dental Assoc. 2006;13:44–53. doi: 10.14219/jada.archive.2006.0020. [DOI] [PubMed] [Google Scholar]
- 6.Vanarsdall RL Transverse dimension and long-term stability. Semin Orthod. 1999;5:177–180. doi: 10.1016/s1073-8746(99)80008-5. [DOI] [PubMed] [Google Scholar]
- 7.Cozzani M, Rosa M, Cozzani P, Siciliani G. Deciduous dentition-anchored rapid maxillary expansion in cross-bite and non-cross-bite mixed dentition patients: reaction of the permanent first molar. Prog Orthod. 2003;4:15–22. doi: 10.1034/j.1600-9975.2002.02034.x. [DOI] [PubMed] [Google Scholar]
- 8.Cozzani M, Guiducci A, Mirenghi S, Mutinelli S, Siciliani G. Arch width changes with a rapid maxillary expansion appliance anchored to the primary teeth. Angle Orthod. 2007;77:296–302. doi: 10.2319/0003-3219(2007)077[0296:AWCWAR]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Rosa M, Lucchi P, Mariani L, Caprioglio A. Spontaneous correction of anterior crossbite by RPE anchored on deciduous teeth in the early mixed dentition. Eur J Paediatr Dent. 2012;13:176–180. [PubMed] [Google Scholar]
- 10.Mutinelli S, Cozzani M, Manfredi M, Bee M, Siciliani G. Dental arch changes following rapid maxillary expansion. Eur J Orthod. 2008;30:469–476. doi: 10.1093/ejo/cjn045. [DOI] [PubMed] [Google Scholar]
- 11.Ferrario VF, Garattini G, Colombo A, Filippi V, Pozzoli S, Sforza C. Quantitative effects of a nickel-titanium palatal expander on skeletal ad dental structures in the primary and mixed dentition: a preliminary study. Eur J Orthod. 2003;25:401–410. doi: 10.1093/ejo/25.4.401. [DOI] [PubMed] [Google Scholar]
- 12.Kilik N, Kiki A, Oktay H. A comparison of dentoalveolar inclination treated by two palatal expanders. Eur J Orthod. 2008;30:67–72. doi: 10.1093/ejo/cjm099. [DOI] [PubMed] [Google Scholar]
- 13.Bazargani F, Feldmann I, Bondemark L. Three-dimensional analysis of effect of rapid maxillary expansion on facial sutures and bone. Angle Orthod. 2013;83:1074–1082. doi: 10.2319/020413-103.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rungcharassaeng K, Caruso JM, Kan JY, Kim J, Taylor G. Factors affecting buccal bone changes of maxillary posterior teeth after rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2007;132:428.e1–8. doi: 10.1016/j.ajodo.2007.02.052. [DOI] [PubMed] [Google Scholar]
- 15.Gryson JA. Changes in mandibular interdental distance concurrent with rapid maxillary expansion. Angle Orthod. 1977;47:187–192. doi: 10.1043/0003-3219(1977)047<0186:CIMIDC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 16.Cross DL, McDonald JP. Effect of rapid maxillary expansion on skeletal, dental, and nasal structures: a postero-anterior cephalometric study. Eur J Orthod. 2000;22:519–528. doi: 10.1093/ejo/22.5.519. [DOI] [PubMed] [Google Scholar]
- 17.Lima AC, Lima AL, Lima Filho RMA, Oyen OJ. Spontaneous mandibular arch response after rapid palatal expansion: a long-term study on class I malocclusion. Am J Orthod Dentofacial Orthop. 2004;126:576–582. doi: 10.1016/j.ajodo.2004.06.011. [DOI] [PubMed] [Google Scholar]
- 18.Haas AJ. Rapid expansion of the maxillary dental arch and nasal cavity by opening the midpalatal suture. Angle Orthod. 1961;31:73–90. [Google Scholar]
- 19.Wertz RA. Skeletal and dental changes accompanying rapid midpalatal suture opening. Am J Orthod. 1970;58:41–66. doi: 10.1016/0002-9416(70)90127-2. [DOI] [PubMed] [Google Scholar]
- 20.Wertz RA, Dreskin M. Midpalatal suture opening: a normative study. Am J Orthod. 1977;71:367–381. doi: 10.1016/0002-9416(77)90241-x. [DOI] [PubMed] [Google Scholar]
- 21.McDougall PD, McNamara JA, Jr, Dierkes MJ. Arch width development in class II patients treated with the Frankel appliance. Am J Orthod. 1982;82:10–22. doi: 10.1016/0002-9416(82)90541-3. [DOI] [PubMed] [Google Scholar]
- 22.Ferrario VF, Sforza C, Colombo A, Ciusa V, Serrao G. Three-dimensional inclination of the dental axes in healthy permanent dentition: a cross-sectional study in a normal population. Angle Orthod. 2001;71:257–264. doi: 10.1043/0003-3219(2001)071<0257:TDIOTD>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 23.Huanca Ghislanzoni LT, Lineberger M, Cevidanes L, Mapelli A, Sforza C, McNamara JA., Jr Evaluation of tip and torque on virtual study models: a validation study. Prog Orthod. 2013;14:19. doi: 10.1186/2196-1042-14-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dahlberg G. Statistical Methods for Medical and Biological Students. London, UK: Allen and Unwin; 1940. [Google Scholar]
- 25.Harris EF, Smith RN. Accounting for measurements error: a critical but often overlooked process. Arch Oral Biol. 2009;54S:107–117. doi: 10.1016/j.archoralbio.2008.04.010. [DOI] [PubMed] [Google Scholar]
- 26.Cohen J. A power primer. Psychol Bull. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 27.Baccetti T, Franchi L, McNamara JA., Jr An improved version of the cervical vertebral maturation (CVM) method for the assessment of mandibular growth. Angle Orthod. 2002;72:316–323. doi: 10.1043/0003-3219(2002)072<0316:AIVOTC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 28.Asanza S, Cisneros GJ, Nieberg LG. Comparison of Hyrax and bonded expansion appliances. Angle Orthod. 1997;67:15–22. doi: 10.1043/0003-3219(1997)067<0015:COHABE>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 29.Geran RG, McNamara JA, Jr, Baccetti T, Franchi L, Shapiro LM. A prospective long-term study on the effects of rapid maxillary expansion in the early mixed dentition. Am J Orthod Dentofacial Orthop. 2006;129:621–640. doi: 10.1016/j.ajodo.2005.01.020. [DOI] [PubMed] [Google Scholar]
- 30.O'Grady, McNamara JA, Jr, Baccetti T, Franchi L. A long-term evaluation of the mandibular Schwarz appliance and the acrylic splint expander in early mixed dentition patients. Am J Orthod Dentofacial Orthop. 2006;130:202–213. doi: 10.1016/j.ajodo.2004.12.023. [DOI] [PubMed] [Google Scholar]
- 31.Ballanti F, Lione R, Baccetti T, Franchi L, Cozza P. Treatment and posttreatment skeletal effects of rapid maxillary expansion investigated with low-dose computed tomography in growing subjects. Am J Orthod Dentofacial Orthop. 2010;138:311–317. doi: 10.1016/j.ajodo.2008.10.022. [DOI] [PubMed] [Google Scholar]
- 32.Agostino P, Ugolini A, Signori A, Silvestrini-Biavati A, Harrison JE, Riley P. Orthodontic treatment for posterior crossbites. Cochrane Database Syst Rev. 2014 Aug 8; doi: 10.1002/14651858. 8CD000979. doi. CD000979.pub2. [DOI] [PubMed] [Google Scholar]