Abstract
Objective:
To evaluate if the improved accelerated osteogenic orthodontics (IAOO) procedure could speed Class III surgical patients' preoperative orthodontic treatment duration and, if yes, to what extent. This study was also designed to determine whether or not an IAOO procedure affects the tooth-moving pattern during extraction space closure.
Materials and Methods:
The samples in this study consisted of 24 Class III surgical patients. Twelve skeletal Class III surgery patients served as an experimental group (group 1) and the others as a control group (group 2). Before treatment, the maxillary first premolars were removed. For group 1, after the maxillary dental arch was aligned and leveled (T2), IAOO procedures were performed in the maxillary alveolar bone. Except for this IAOO procedure in group 1, all 24 patients experienced similar combined orthodontic and orthognathic treatment. Study casts of the maxillary dentitions were made before orthodontic treatment (T1) and after extraction space closure (T3). All of the casts were laser scanned, and the amount of movement of the maxillary central incisor, canine, and first molar, as well as arch widths, were digitally measured and analyzed by using the three-dimensional model superimposition method.
Results:
The time durations T3–T2 were significantly reduced in group 1 by 8.65 ± 2.67 months and for T3–T1 were reduced by 6.39 ± 2.00 months (P < .001). Meanwhile, the tooth movement rates were all higher in group 1 (P < .05). There were no significant differences in the amount of teeth movement in the sagittal, vertical, and transverse dimensions between the two groups (P > .05).
Conclusion:
The IAOO can reduce the surgical orthodontic treatment time for the skeletal Class III surgical patient by more than half a year on average. The IAOO procedures do not save anchorage.
Keywords: Corticotomy, Class III surgical patients, Preoperative orthodontic treatment duration, Three-dimensional measurement, Tooth movement pattern, Improved accelerated osteogenic orthodontics
INTRODUCTION
Young adult patients who have a skeletal facial discrepancy such as a skeletal Class III malocclusion must seek interdisciplinary treatment. A combination of surgical and orthodontic therapy is chosen for most of these patients. They also care very much about the treatment duration.1 In general, the presurgical orthodontic treatment for these patients takes 1.5 or even 2 years,2 and the postoperative orthodontic treatment takes about 6 months to 1 year.3 The overall treatment time, therefore, for these patients usually takes about 3 years, sometimes even longer. To shorten the treatment time and still meet the facial esthetic requirements of these patients is an important goal.
A corticotomy that can facilitate the speed of orthodontic treatment may be one solution that will meet the needs of these young adult patients. Corticotomy-facilitated tooth movement was first described by Bryan in 1893.4,5 A surgical procedure that involved both osteotomy and corticotomy was first described by Kole in 1959.6 Accelerated osteogenic orthodontics (AOO), or Wilckodontics, was demonstrated by Wilcko et al. in 2001.7 This technique includes selective alveolar decortification, alveolar augmentation, and orthodontic treatment. In 2009, Dibart et al.8 used the piezocision technique to achieve rapid orthodontic tooth movement. To reduce surgical injury, we combined two kinds of operative methods proposed by Wilcko and Dibart, respectively, improving the AOO procedure. A piezoelectric method has been used in our study to replace the traditional slow-speed drills. We named this procedure the improved accelerated osteogenic orthodontics (IAOO).
Wilcko reported that orthodontic treatment could be completed in one-third to one-fourth of the time required by traditional orthodontic treatment.4,9 In 2007, Fischer10 reported that a corticotomy-assisted surgical technique helps reduce orthodontic treatment time for palatally impacted canines, and in 2011, Aboul-Ela et al.11 described that the average daily rate of canine retraction was two times more rapid on the corticotomy side of a sample than on the control side during the first 2 months after the corticotomy surgery. Most clinical articles are case studies and nonextraction cases.12 For surgical patients, AOO has also been used to reshape and increase the buccolingual thickness of the supporting alveolar bone during and after orthodontic treatment.13–15
There were three objectives for this pilot clinical study. The first was to find out whether or not the IAOO procedure could reduce the duration of preoperative orthodontic treatment. The second objective was to determine to what extent IAOO could reduce the preoperative orthodontic treatment time. The third objective was to find out whether or not the IAOO procedure affects the tooth-moving pattern during extraction space closure or, in other words, whether or not the IAOO procedure saves molar anchorage when it is applied to the anterior dental area.
MATERIALS AND METHODS
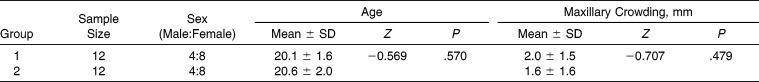
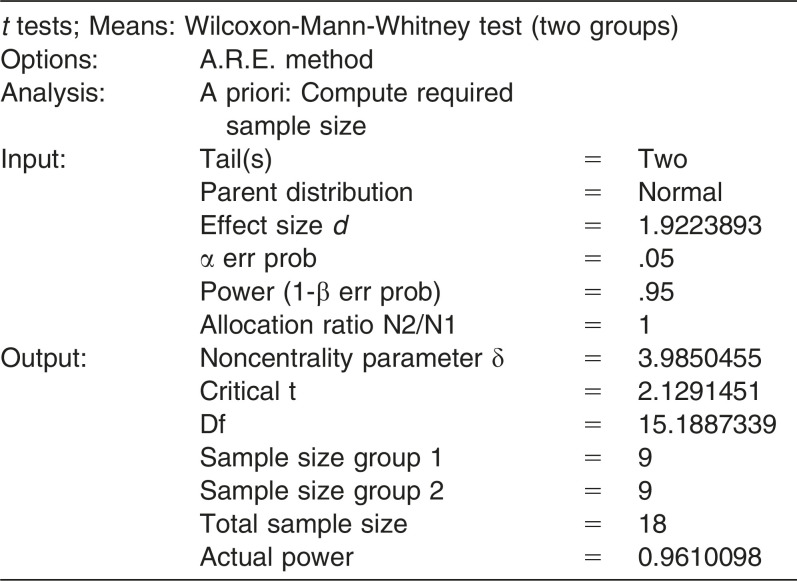
The University Ethics Committee and Competent Authority approved this clinical trial protocol before it started and has been supervising the process. All patients were provided information about the proposed treatment and signed consent forms. The samples in this study consisted of 24 Class III surgical patients. Twelve of them agreed to have the IAOO procedures. These patients served as the experimental group (group 1). Another 12 patients, matched according to age, gender, diagnosis, extraction pattern, and crowding, served as the control group (group 2; Table 1). The screening criteria for all patients were as follows: (1) 18 to 30 years of age; (2) Class III anterior, canine, and molar relationships, ANB <−4° or Wits <−6 mm; (3) bilateral extraction of maxillary first premolars and nonextraction in the mandibular arches; and (4) mild crowding in the maxillary arch (≤3 mm; Table 1). Exclusion criteria were patients with active periodontal disease, supernumerary teeth, and craniofacial syndromes. The cephalometric analyses for the two groups were compared and are shown in Table 2.
Table 1.
Demographic Information for Samples in Group 1 and Group 2
Table 2.
Cephalometric Measurements of the Sample
Treatment Progress
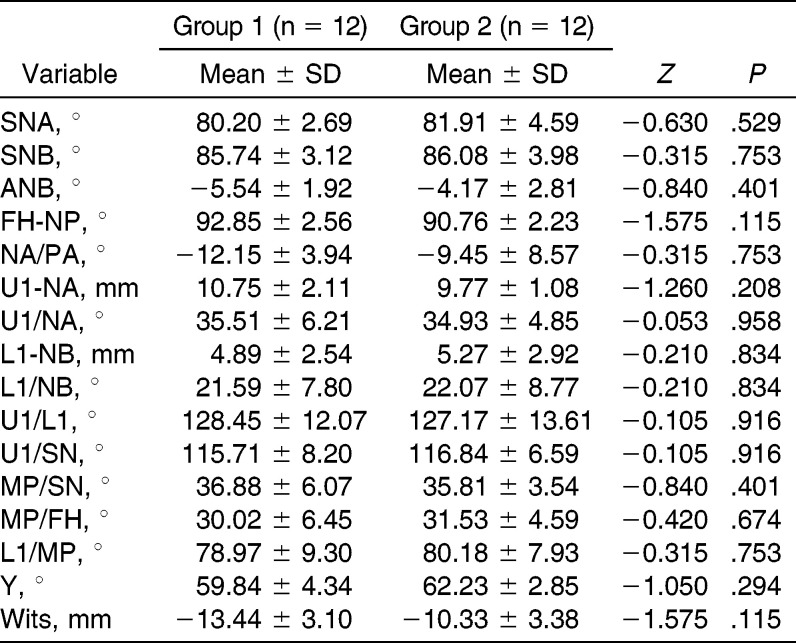
After the extraction of maxillary first premolars, patients were bonded with preadjusted edgewise 0.022-inch fixed appliances. For group 1, after aligning and leveling the maxillary arch, a 0.019× 0.025-inch stainless-steel archwire was ligated into the maxillary brackets; corticotomies were performed only on the buccal side of the alveolar bone with a piezo ultrasonic surgery unit (Piezotome made in France by SATELEC). During the procedure, a full-thickness mucoperiosteum flap was reflected. Parallel vertical incisions were then made in the interradicular spaces from the mesial area of the right second premolar to the mesial area of the left second premolar. These incisions cut through the entire thickness of the cortical plate. No horizontal corticotomy cuts were made. Bone grafting material (Cerasorb, 50∼500 µm, 0.5 g, Curasan AG, Germany) was applied to cover the selective decortification areas. The flaps were carefully repositioned and sutured (Figure 1). Two weeks later, the patients were examined for the first orthodontic adjustment after the IAOO procedure. En masse retraction of the anterior teeth was completed. Group 2 had no IAOO procedure, but the same orthodontics and subsequent orthognathic surgery were done. The intervals for orthodontic adjustments averaged 4 weeks for both groups.
Figure 1.
(a) Sulcular incision performed on the anterior teeth area. (b) Reflection of full-thickness flap. (c, d) Interradicular alveolar corticotomy grooves with piezosurgery. (e) Bone graft material filled the corticotomy area. (f) Flap was sutured.
Measurements and Statistical Method
Treatment time before orthognathic surgery
Time points included the following:
T1: The date when brackets and bands were placed on the maxillary dentition.
T2: The date when the upper teeth were aligned and leveled.
T3: The date when the maxillary dentition spaces were closed.
Measurements
Measurements included the time duration for (1) maxillary dentition leveling and alignment (T2–T1), (2) extraction space closure (T3–T2), and (3) preoperative orthodontic treatment for leveling, alignment, and extraction space closure (T3–T1). Independent samples nonparametric tests (Mann-Whitney test) were applied to compare the two groups.
Measurements of the Three-Dimensional Virtual Maxillary Models
Maxillary digital dental model creation
Maxillary dental models of T1 and T3 were scanned by a three-dimensional (3D) laser scanner (R700 laser scanner, 3 Shape, ±0.02 mm, Denmark), and the digital models were named T1 scan and T3 scan, respectively. Reconstruction and analyses of 3D images were performed using reverse engineering software (Rapidform2006; INUS Technology Inc, Seoul, Korea).
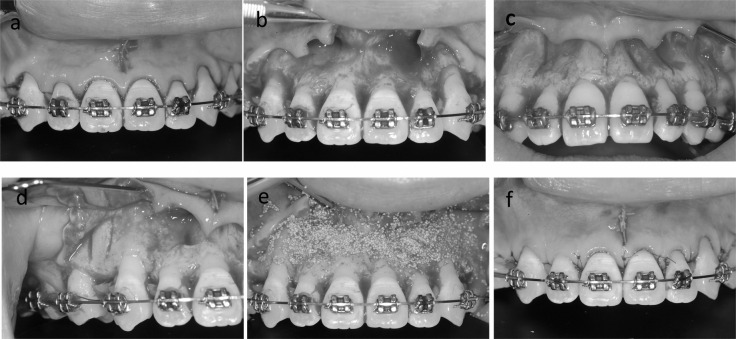
Establishment of the 3D coordinates
A coordinate system modified from the proposal of Cha et al.16 and Chen et al.17 was established on the T1 scan. The junction of the incisive papilla and the palatine raphe served as the origin (0, 0, 0), resulting in an x-, y-, and z-axis and three planes (Figure 2).16,17
Figure 2.
The coordinate system. (a) The x-z horizontal plane is the section that includes the junction of inclusive papilla and palatine raphe (PMRJ) and parallel to the occlusal plane constructed by connecting the mesio-buccal cusp tips of the right and left maxillary first molars and the midpoints of the central incisor edges using the best-fitting process. (b) The x-y sagittal plane is the section inclusive of one arbitrary point on the midpalatal suture and the PMRJ and perpendicular to the x-z horizontal plane. (c) The x-z frontal plane is the section inclusive of the PMRJ and perpendicular to both the horizontal and sagittal planes.
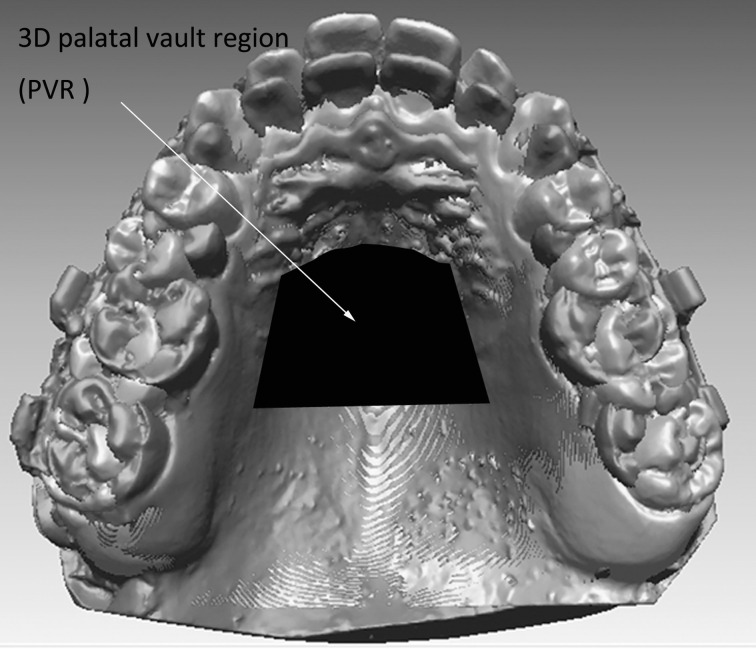
Three-dimensional model superimposition
To measure orthodontic tooth movement, digital maxillary casts T1 and T3 were registered using the iterative closest point (ICP) method,18 in which initial rotation and translation scans are estimated using the 3D palatal vault region (PVR). This 3D cast superimposition method was performed on the 3D PVR and included the medial two-thirds of the palatal vault between the third rugae and a line in contact with the distal surface of the left and right maxillary first molars (Figure 3).17
Figure 3.
Superimposition of maxillary digital casts of T1 (in blue; please see the online version for color) and T3 (in red) on the three-dimensional palatal vault region.
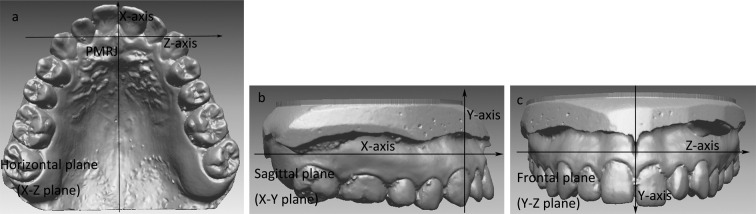
Measuring and Statistics Analysis
Using the coordinate system of the superimposed 3D models, the measuring points were fixed on the T1 scan. The points were the midpoint on the edge of the maxillary right central incisor (UR1) and the maxillary left central incisor (UL1), the tip of the maxillary right canine (UR3) and maxillary left canine (UL3), and the fovea of the maxillary right (UR6) and maxillary left first molars (UL6; Figure 4a). With a 3D image registration technique using the ICP method, these points on the T1 scan were transferred onto the corresponding teeth on the T3 scan (Figure 4).19 These superimposed digital casts described the maxillary first molar, canine, and central incisor movement. The widths of the arch forms were measured (Figure 4a,d). The mean sagittal, vertical, and total tooth movement along with widths of arch form for group 1 were compared with those of group 2.
Figure 4.
(a) The measuring points on T1 scan (in blue; please see the online version for color). UR1 indicates the midpoint on the edge of maxillary right central incisor; UL1, midpoint on the edge of maxillary left central incisor; UR3, tip of maxillary right canine; UL3, tip of maxillary left canine; UR6, fovea of right maxillary first molar; UL6, fovea of maxillary left first molar; intercanine width, distance between UR3 and UL3; intermolar width, distance between UR6 and UL6. (b) The maxillary right central incisor was detached from the T1 scan. (c) UR1 fixed on the maxillary right central incisor on the T1 scan was transferred into the maxillary right central incisor on the T3 scan (in red) with the three-dimensional image registration technique. (d) The measuring points on the T1 scan were transferred into the corresponding teeth on the T3 scan, respectively.
The Mann-Whitney tests were performed to determine whether significant differences existed between the two groups. Two operators measured digital casts twice and compared their findings. The intraclass correlation coefficient (>0.8) exhibited high reliability between operators. The definitive values were defined as the average values from two examiners.
RESULTS
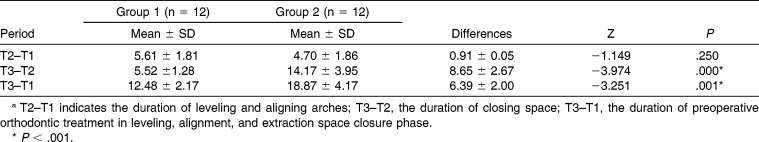
Treatment Time Before Orthognathic Surgery
There was no statistically significant difference for T2–T1 between the two groups (P = .250; Table 3). The T3–T2 and T3–T1 times were significantly shorter for group 1 than for group 2 (P < .001).
Table 3.
Comparison of the Treatment Duration Between Group 1 and Group 2a
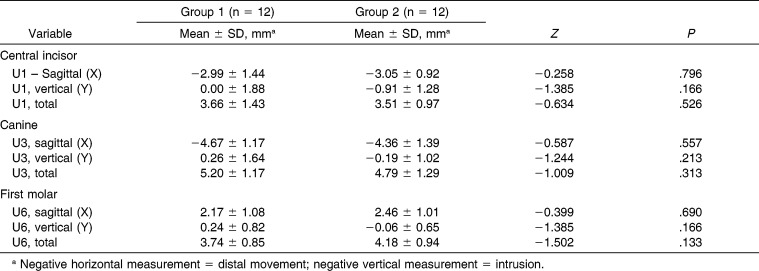
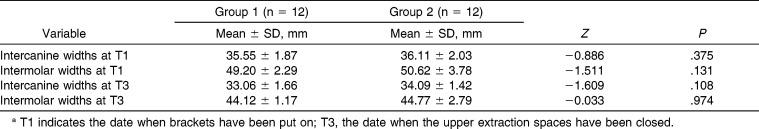
Measurements of the 3D Virtual Maxillary Models
The sagittal, vertical, and total amount of movement of maxillary central incisor, maxillary canine, and maxillary first molar indicated no statistical differences between the two groups (P > .05; Table 4). Similarly, the intercanine widths and intermolar widths showed no significant differences between the two groups (P > .05; Table 5).
Table 4.
Mann-Whitney Test Comparing Central Incisor, Canine, and First Molar Movement Measured From Group 1 and Group 2 Digital Models
Table 5.
Comparison of Intercanine Widths and Intermolar Widths Between Group 1 and Group 2 Measured at T1 and T3a
Tooth Movement Rate During the Preoperative Orthodontic Treatment in Leveling, Alignment, and Extraction Space Closure Phase
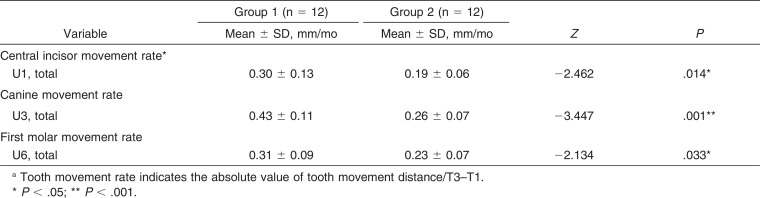
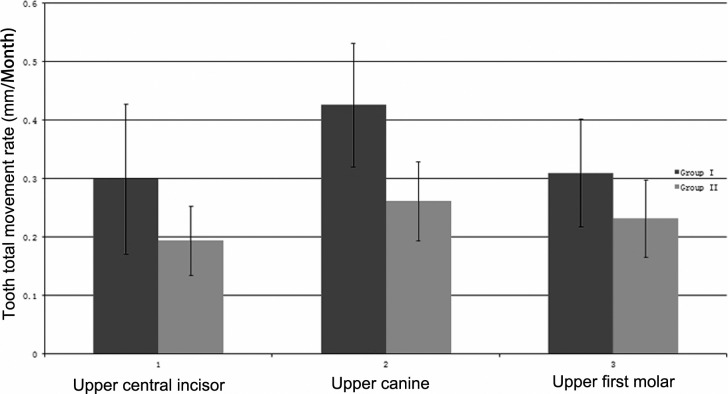
Rates of maxillary central incisor, canine, and first molar total movement were significantly higher in group 1 than in group 2 (P < .05; Table 6; Figure 5).
Table 6.
Comparison of Upper Central Incisor, Canine, and First Molar Sagittal and Total Movement Ratesa
Figure 5.
Graphic presentation of total tooth movement rate of group 1 and group 2 from T1 to T3.
DISCUSSION
The length of treatment time is a major concern for the young adult patient, especially for those who have a combination of orthodontics and surgical therapy. Luther et al.2 reported that the median duration of the presurgical phase of orthodontic treatment for Class III patients was 18 months. Many factors such as extraction or nonextraction, malocclusion classification, sex, age, and so forth influence preoperative orthodontic treatment duration. Dowling et al.20 found that the median duration of preoperative orthodontics was 15.4 months. They found that extractions added 5 more months to the median preoperative duration (P < .001).
Some research studies claim that corticotomy induces a localized increase in turnover of alveolar spongiosa and the acceleration of a physiologic demineralization and remineralization process (reversible osteopenia).7,21 A recent study confirmed that the basic mechanism underlying corticotomy is the coupling between osteoblasts and osteoclasts initiated at the same time after a mechanical injury.22
The T3–T2 and T3–T1 times were significantly shortened after the IAOO procedures for group 1. The treatment time was reduced by 8.65 ± 2.67 months and 6.39 ± 2.00 months, respectively. This finding suggests that preoperative orthodontic treatment time in the leveling, alignment, and extraction space closure phase (T3–T1) can be shortened at least half a year by utilization of the IAOO procedure. If the time duration for extraction space closure (T3–T2) is considered, nearly 9 months has been saved for the patient. The rates of tooth movement further confirmed this result.
In this study, a piezoelectric surgical device replaced the slow-speed hand piece that is commonly used during the IAOO procedure. In previous reports, slow-speed drills showed signs of thermal damage and bone fragments.23 Piezosurgery was claimed as ideal to perform osteotomies in thin and fragile bones. The ultrasound appliance is precise and easily handled, and the microvibrations allow a selective cut of only mineralized structures, thereby creating minimal damage to adjacent tissue. In addition, in this study, only buccal-side corticotomy incisions were performed; there was no horizontal subapical cut. Sebaoun et al.21 reported that cuts on only the buccal side were enough for inducing reversible osteopenia. For the patients in group 1, little discomfort was reported during and after the IAOO procedure.
Laser scanning was introduced to digitize the dental casts and enhance the 3D measurement and analysis of study casts.24 Compared with plaster dental casts, 3D digital dental casts proved to be more accurate and reliable.25,26 In previous studies, pretreatment and posttreatment maxillary digital dental casts were superimposed to analyze tooth movement patterns in extraction patients.16,17 In this study, similar methods were used to superimpose and analyze the T1 and T3 scans.
Wilcko and Wilcko27 mentioned that the AOO procedure increased rates of movement differentially between decorticated and nondecorticated teeth and thus created the ability to alter the relative anchorage between teeth. Therefore, the anchorage teeth should be more effective anchors if not decorticated; conversely, decorticated teeth moved with greater ease. In this study, the maxillary first premolars were removed to allow the retraction of the maxillary anterior teeth. An assumption had been made that the amount of the incisor retraction in group 1 would be greater than that in group 2. However, the results indicated that this was not the case: there were no significant differences between two groups, no differences in the amount of movement of anterior teeth and molars in the sagittal, vertical, and transverse dimensions. In another animal study, two groups, selective alveolar decortications + tooth movement and tooth movement alone, demonstrated that the cumulative tooth movement amount was the same.22 The total amount of tooth movement was not changed by the IAOO procedure, but the tooth movement rates were increased. Molar anchorage loss was similar between the two groups, so corticotomy cuts performed in the anterior area did not affect the pattern of tooth movement or relatively increase molar anchorage. If patients need more anterior teeth retraction, extra posterior anchorage devices should be applied during the treatment.
To explore whether there was a selection bias, the baseline data that might influence the results between two groups were compared. First, patient age, gender, and extraction patterns were matched in the two groups (Table 1). Second, the detailed skeletal and dental analysis of the two groups at baseline (T1) was done, and the statistical analysis showed that the two groups had no significant differences in measurable parameters (P > .05; Table 2). In addition, the amount of crowding and incisor angulation indicated no statistical differences between the two groups (P > .05; Tables 1 and 2). In conclusion, the only difference between the two groups was the corticotomy intervention.
This was a preliminary clinical research trial. This study should be extended further to increase the sample size and the follow-up period.
CONCLUSIONS
The IAOO can reduce the preoperative orthodontic treatment time in leveling, alignment, and extraction space closure phase for the skeletal Class III surgical patients by an average of more than half a year.
The IAOO procedures do not save anchorage.
ACKNOWLEDGMENTS
This study was supported by the National Natural Science Foundation of China (No. 81171006) and also by the Beijing Science and Technology Committee (No. Z121107001012024).
APPENDIX
REFERENCES
- 1.Phillips C, Proffit WR. Contemporary Treatment of Dentofacial Deformity. St Louis, Mo: Mosby; 2003. Psychosocial aspects of dentofacial deformity and its treatment; p. 69. [Google Scholar]
- 2.Luther F, Morris DO, Hart C. Orthodontic preparation for orthognathic surgery: how long does it take and why? A retrospective study. Br J Oral Maxillofac Surg. 2003;41:401–406. doi: 10.1016/s0266-4356(03)00163-3. [DOI] [PubMed] [Google Scholar]
- 3.Luther F, Morris DO, Karnezi K. Orthodontic treatment following orthognathic surgery: how long does it take and why? A retrospective study. J Oral Maxillofac Surg. 2007;65:1969–1976. doi: 10.1016/j.joms.2007.05.026. [DOI] [PubMed] [Google Scholar]
- 4.Wilcko TM, William MW, Bissada NF. An evidence-based analysis of periodontally accelerated orthodontic and osteogenic techniques: a synthesis of scientific perspectives. Semin Orthod. 2008;14:305–316. [Google Scholar]
- 5.Hassan AH, Al-Fraidi AA, Al-Saeed SH. Corticotomy-assisted orthodontic treatment: review. Open Dent J. 2010;4:159–164. doi: 10.2174/1874210601004010159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kole H. Surgical operations on the alveolar ridge to correct occlusal abnormalities. Oral Surg. 1959;12:515–529. doi: 10.1016/0030-4220(59)90153-7. [DOI] [PubMed] [Google Scholar]
- 7.Wilcko MW, Wilcko MT, Bouquot JE, Ferguson DJ. Rapid orthodontics with alveolar reshaping: two case reports of de-crowding. Int J Periodont Restor Dent. 2001;21:9–19. [PubMed] [Google Scholar]
- 8.Dibart S, Sebaoun JD, Surmenian J. Piezocision: a minimally invasive, periodontally accelerated orthodontic tooth movement procedure. Compend Conti Educ Dent. 2009;30:342–344, 346, 348–350. [PubMed] [Google Scholar]
- 9.Wilcko WM, Ferguson DJ, Bouquot JE, Wilcko MT. Rapid orthodontic decrowding with alveolar augmentation: case report, with alveolar augmentation. World J Orthod. 2003;4:197–205. [Google Scholar]
- 10.Fischer TJ. Orthodontic treatment acceleration with corticotomy-assisted exposure of palatally impacted canines. Angle Orthod. 2007;77:417–420. doi: 10.2319/0003-3219(2007)077[0417:OTAWCE]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Aboul-Ela SM, El-Beialy AR, El-Sayed KM, Selim EM, El-Mangoury NH, Mostafa YA. Miniscrew implant-supported maxillary canine retraction with and without corticotomy-facilitated orthodontics. Am J Orthod Dentofacial Orthop. 2011;139:252–259. doi: 10.1016/j.ajodo.2009.04.028. [DOI] [PubMed] [Google Scholar]
- 12.Mathews DP, Kokich VG. Accelerating tooth movement: the case against corticotomy-induced orthodontics. Am J Orthod Dentofacial Orthop. 2013;144:5–13. doi: 10.1016/j.ajodo.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 13.Kim SH, Kim I, Jeong DM, Chung KR, Zadeh H. Corticotomy-assisted decompensation for augmentation of the mandibular anterior ridge. Am J Orthod Dentofacial Orthop. 2011;140:720–731. doi: 10.1016/j.ajodo.2009.12.040. [DOI] [PubMed] [Google Scholar]
- 14.Hyo-Won Ahn, Dong-Yeol Lee, Young-Guk Park, et al. Accelerated decompensation of mandibular incisors in surgical skeletal Class III patients by using augmented corticotomy: a preliminary study. Am J Orthod Dentofacial Orthop. 2012;142:199–206. doi: 10.1016/j.ajodo.2012.03.028. [DOI] [PubMed] [Google Scholar]
- 15.Coscia G, Coscia V, Peluso V, Addabbo F. Augmented corticotomy combined with accelerated orthodontic forces in class III orthognathic patients: morphologic aspects of the mandibular anterior ridge with cone-beam computed tomography. J Oral Maxillofac Surg. 2013;71:1760.e1–1760.e9. doi: 10.1016/j.joms.2013.04.022. [DOI] [PubMed] [Google Scholar]
- 16.Cha BK, Lee JY, Jost-Brinkmann PG, Yoshida N. Analysis of tooth movement in extraction cases using three-dimensional reverse engineering technology. Eur J Orthod. 2007;29:325–331. doi: 10.1093/ejo/cjm019. [DOI] [PubMed] [Google Scholar]
- 17.Chen G, Chen S, Zhang XY, et al. Stable region for maxillary dental cast superimposition in adults, studied with the aid of stable miniscrews. Orthod Craniofac Res. 2011;14:70–79. doi: 10.1111/j.1601-6343.2011.01510.x. [DOI] [PubMed] [Google Scholar]
- 18.Besl P, McKay N. A method for registration of 3-D shapes. IEEE Trans Pattern Anal Mach Intell. 1992;14:239–256. [Google Scholar]
- 19.Chen G, Qin YF, Xu TM. Tip and torque changes in maxillary buccal segment after orthodontic treatment: a three-dimensional study. Zhonghua Kou Qiang Yi Xue Za Zhi. 2010;45:650–654. [PubMed] [Google Scholar]
- 20.Dowling PA, Espeland L, Krogstad O, Stenvik A, Kelly A. Duration of orthodontic treatment involving orthognathic surgery. Int J Adult Orthod Orthognath Surg. 1999;14:146–152. [PubMed] [Google Scholar]
- 21.Sebaoun JD, Kantarci A, Turner JW, Carvalho RS, Van Dyke TE, Ferguson DJ. Modeling of trabecular bone and lamina dura following selective alveolar decortication in rats. J Periodontol. 2008;79:1679–1688. doi: 10.1902/jop.2008.080024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baloul SS, Gerstenfeld LC, Morgan EF, Carvalho RS, Van Dyke TE, Kantarci A. Mechanism of action and morphologic changes in the alveolar bone in response to selective alveolar decortication-facilitated tooth movement. Am J Orthod Dentofacial Orthop. 2011;139:S83–S101. doi: 10.1016/j.ajodo.2010.09.026. [DOI] [PubMed] [Google Scholar]
- 23.Romeo U, Del VA, Palaia G, Tenore G, Visca P, Maggiore C. Bone damage induced by different cutting instruments—an in vitro study. Braz Dent J. 2009;20:162–168. doi: 10.1590/s0103-64402009000200013. [DOI] [PubMed] [Google Scholar]
- 24.Joffe L. OrthoCAD: digital models for a digital era. J Orthod. 2004;31:344–347. doi: 10.1179/146531204225026679. [DOI] [PubMed] [Google Scholar]
- 25.Zilberman O, Huggare JA, Parikakis KA. Evaluation of the validity of tooth size and arch width measurements using conventional and three-dimensional virtual orthodontic models. Angle Orthod. 2003;73:301–306. doi: 10.1043/0003-3219(2003)073<0301:EOTVOT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 26.Quimby M, Vig K, Rashid R, Firestone A. The accuracy and reliability of measurements made on computer-based digital models. Angle Orthod. 2004;74:298–303. doi: 10.1043/0003-3219(2004)074<0298:TAAROM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 27.Wilcko W, Wilcko MT. Accelerating tooth movement: the case for corticotomy-induced orthodontics. Am J Orthod Dentofacial Orthop. 2013;144:4–12. doi: 10.1016/j.ajodo.2013.04.009. [DOI] [PubMed] [Google Scholar]