Abstract
Objective:
To evaluate and compare skeletal effects and the amount of molar distalization in maxilla using modified palatal anchorage plate (MPAP) vs headgear appliances in adolescent patients.
Materials and Methods:
Pre- and posttreatment lateral cephalograms of 45 Class II malocclusion patients were analyzed; 24 were treated with MPAP appliances (age, 12.4 years) and 21 with headgear (age, 12.1 years). Fixed orthodontic treatment started with the distalization process in both groups. Thirty-two variables were measured and compared between both groups using multivariate analysis of covariates.
Results:
There was no significant main effect of the appliance type on the treatment results (P = .063). Also, there was no significant main effect of the appliance type on both pre- and posttreatment comparisons (P = .0198 and .135, respectively). The MPAP and headgear groups showed significant distalization of maxillary first molars (3.06 ± 0.54 mm and 1.8 ± 0.58 mm, respectively; P < .001). Sagittal skeletal maxillomandibular differences were improved after treatment (P < .001), with no significant differences between the two groups. No significant difference in treatment duration was found between the groups.
Conclusions:
The MPAP showed a significant skeletal effect on the maxilla. Both MPAP and headgear resulted in distalization of maxillary first molars. Therefore, it is recommended that clinicians consider the application of MPAP, especially in noncompliant Class II patients.
Keywords: Modified palatal anchorage plate, Maxillary molar distalization, Headgear, Skeletal effect
INTRODUCTION
It is challenging to perform distalization of maxillary molars without tipping and extrusion that could cause relapse. Traditionally, headgear has shown successful results in Class II treatment.1,2 While its effect is a combination of distal movement of molars, inhibition of maxillary growth, and rotation of the palate,3,4 it is dependent on patient cooperation and may cause psychological distress.5,6 Also, it is difficult to achieve bodily tooth movement.
To avoid the negative aspects of headgear, several intraoral appliances such as distal jet, Herbst, and pendulum springs have been developed to distalize molars7–9; however, they have some drawbacks. For instance, the distal jet has been known to lead to mesial rotation of the molars during distalization, and the pendulum appliance has resulted in distal tipping of molars, anchorage loss, and a tendency for reciprocal effects.10–12 In general, the side effects of these appliances are anchorage loss at the reactive part causing flaring of the incisors, distal tipping, and rotation of the distalized molars.
To reduce these shortcomings, several studies have considered the application of temporary anchorage devices (TADs).13,14 TADs have been applied to the buccal plate of bone to achieve molar distalization.15–17 However, the buccal approach poses an increased risk of contact with the roots of adjacent teeth, and the range of action might be limited by the interradicular space in adolescents.
Triaca et al.18 have introduced the palate for skeletal anchorage. The placement of TADs in the palate eliminates the need for reimplanting mini-screws as in the buccal approach. Therefore, palatal bone thickness and density as well as palatal soft tissue thickness have recently been evaluated in adolescents.19–21
Currently, the modified palatal anchorage plate (MPAP) offers a simple and effective nonextraction approach for distalization of the maxillary dentition in adults.22 However, the effect of palatal plates on the growth of the maxilla has not been evaluated. Moreover, no comparison has been made of the treatment effects with MPAP appliances vs headgear.
Therefore, the purpose of this study was to evaluate the amount of molar distalization and skeletal effects in maxilla resulting from molar distalization using MPAPs and to compare these effects with those of headgear appliances in adolescent patients.
MATERIALS AND METHODS
The sample of this retrospective study consisted of lateral cephalograms of 45 Class II division 1 malocclusion patients; 24 were treated with MPAP appliances (age, 12.42 ± 1.69 years; 18 girls) at the Department of Orthodontics, Seoul St. Mary's Hospital, The Catholic University of Korea, and 21 with cervical pull headgear (age, 12.05 ± 1.40 years; 10 girls) at a private practice office. The inclusion criteria were age range from 10 to 16 years, Class II division 1 malocclusion with normal divergent growth pattern, moderate maxillary crowding (<5 mm) and protrusion, nonextraction treatment, molar distalization via either MPAPs or headgear exclusively, and absence of craniofacial syndromes. Approval to conduct this study was granted by the Institutional Review Board (KC11RASI0790).
The MPAP appliance has been described previously.23,24 The MPAPs were installed by a single operator using three 8-mm-length and 2.0-mm-diameter miniscrews (Jeil Corporation, Seoul, Korea) in the paramedinan area to avoid interference with the growth of the suture. A palatal bar with two hooks extending along the gingival margins of the teeth was bonded to the maxillary first molars. Distalization was initiated by engaging elastics or NiTi closed-coil springs between the MPAP arm notches and the hooks on the palatal bar, applying approximately 300 g of force per side (Figure 1).
Figure 1.

The MPAP placed on the palate of a patient with late mixed dentition.
All headgear cases (cervical pull) were treated by one operator. The outer bows of the headgear were adjusted upward to pass close to the center of resistance of the maxillary first molars. Each patient was given a wearing-time recording card for motivation, and most of the patients reported satisfactory records.
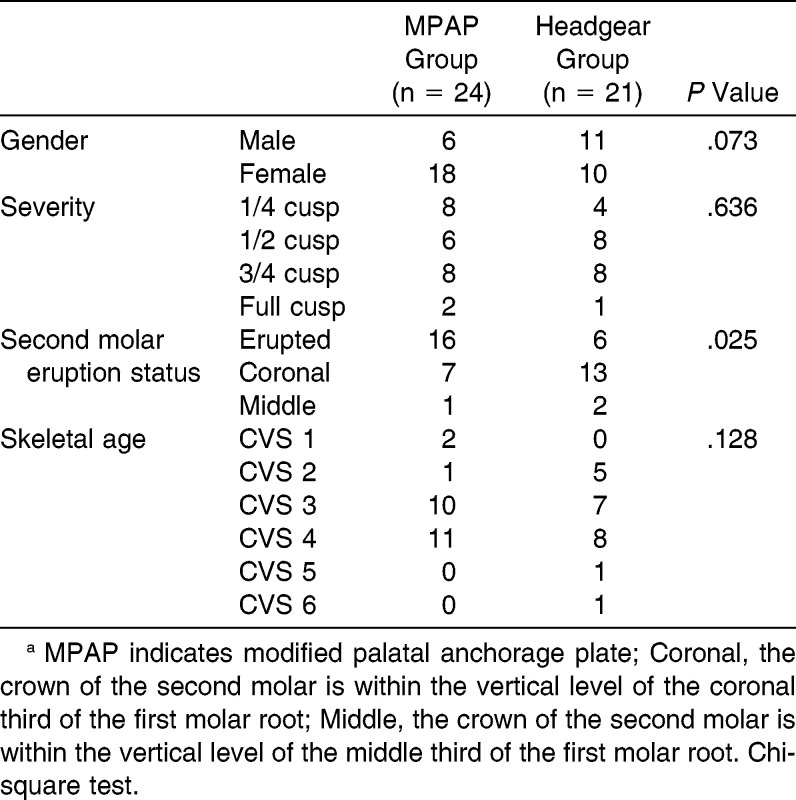
Table 1 shows the demographic data of the two groups including the severity of Class II molar relationship (very mild, 1/4 cusp; mild, 1/2 cusp; moderate, 3/4 cusp; and severe, full cusp), the eruption status of the maxillary second molar, and the skeletal age according to the method of Baccetti et al.25
Table 1.
Demographic Dataa
Cephalometric Measurements
The pre- (T1) and posttreatment (T2) lateral cephalograms were digitized using V-Ceph 5.5 (Cybermed, Seoul, South Korea). The horizontal reference line was the FH plane, and the vertical reference line was a perpendicular line passing through the pterygoid. Thirty-two linear and angular measurements were made by one examiner (Figures 2–4). Differences between T1 and T2 were calculated.
Figure 2.
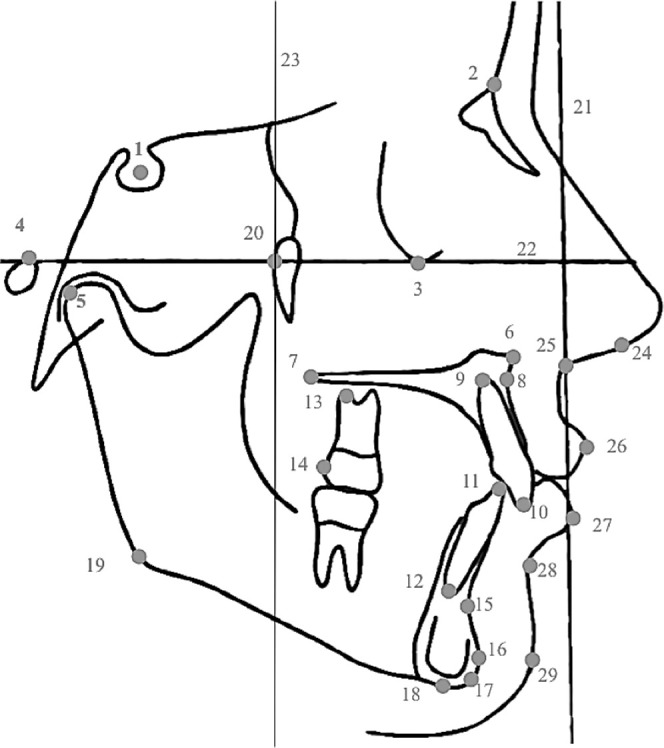
Landmarks and reference lines: 1, sella; 2, nasion; 3, orbitale; 4, porion; 5, condylion; 6, anterior nasal spine (ANS); 7, posterior nasal spine (PNS); 8, a point; 9, maxillary central incisor root apex; 10, maxillary central incisor incisal edge; 11, mandibular central incisor incisal edge; 12, mandibular central incisor root apex; 13, maxillary first molar root apex; 14, maxillary first molar crown; 15, B point; 16, pogonion; 17, gnathion; 18, menton; 19, gonion; 20, pterygoid point; 21, true vertical line; 22, Frankfort horizontal plane; 23, vertical reference line; 24, columella; 25, subnasale; 26,upper lip; 27, lower lip; 28, soft tissue B point; 29, soft tissue pogonion.
Figure 3.
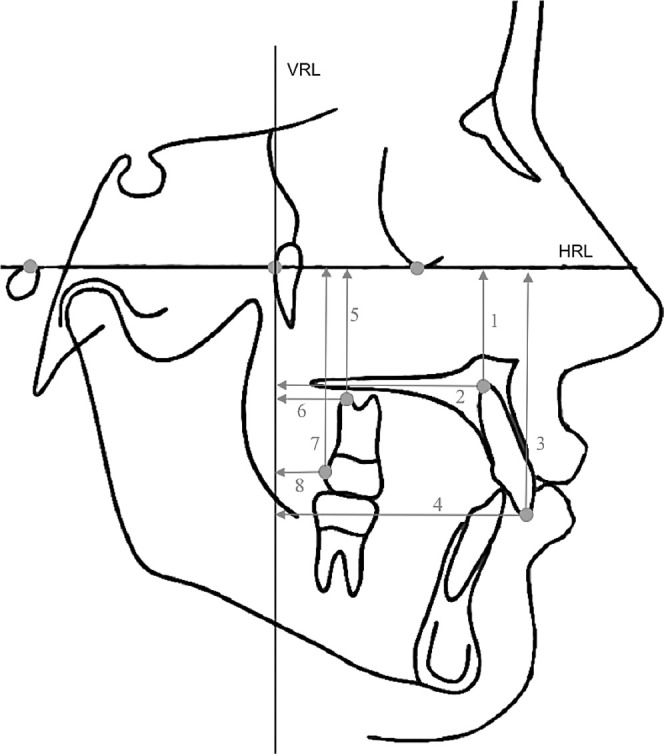
Linear measurements: 1, vertical distance of maxillary central incisor root apex to horizontal reference line (HRL); 2, horizontal distance of maxillary central incisor root apex to vertical reference line (VRL); 3, vertical distance of maxillary central incisor crown to HRL; 4, horizontal distance of maxillary central incisor crown to VRL; 5, vertical distance of maxillary first molar root apex to HRL; 6, horizontal distance of maxillary first molar root apex to VRL; 7, vertical distance of maxillary first molar crown to HRL; 8, horizontal distance of maxillary first molar crown to VRL.
Figure 4.
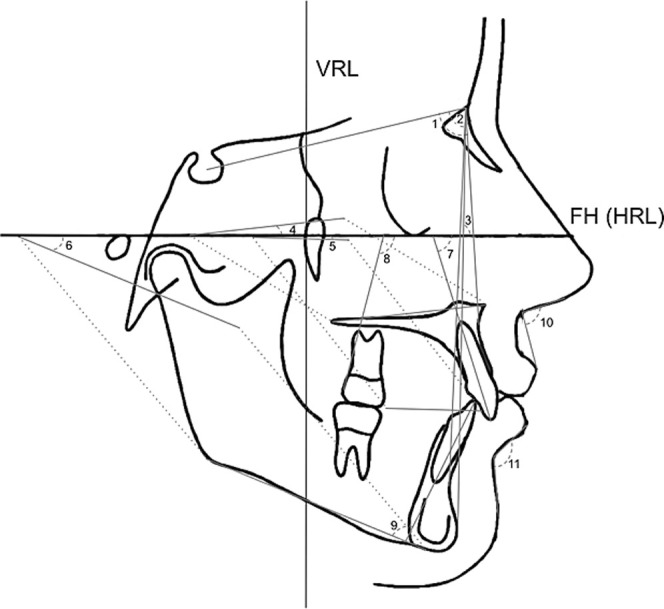
Angular measurements: 1, SNA; 2, SNB; 3, facial angle (FH/N-Pg); 4, palatal plane angle (FH/ANS-PNS); 5, occlusal plane angle (FH/OP); 6, mandibular plane angle (FH/Go-Me); 7, maxillary central incisor inclination; 8, maxillary first molar inclination; 9, incisor mandibular plane angle (IMPA); 10, nasolabial angle; 11, mentolabial fold angle.
Ten randomly selected cases from each group were redigitized and analyzed 2 weeks later by the same examiner. Intraexaminer reliability was evaluated by intraclass correlation coefficient and was >.9.
Statistical Analysis
Statistical evaluation was performed using SPSS 16.0 (SPSS Inc, Chicago, Ill). Paired t-test was used to evaluate the skeletal, dental, and soft tissue changes from T1 to T2 within each group. A multivariate analysis of covariates (MANCOVA) was performed to evaluate the differences pre- and posttreatment and the treatment effects between the groups. An independent-sample t-test showed no significant difference in age (P = .433), and a chi-square test showed no significant differences in frequency distribution of gender (P = .073), severity (P = .636), or skeletal age (P = .128) between the groups. However, a significant difference was found in the second molar eruption status (P = .025; Table 1). Therefore, this variable was used as a covariate in the MANCOVA. Statistical significance was set at .05, and by applying Bonferroni correction, it became .0016.
RESULTS
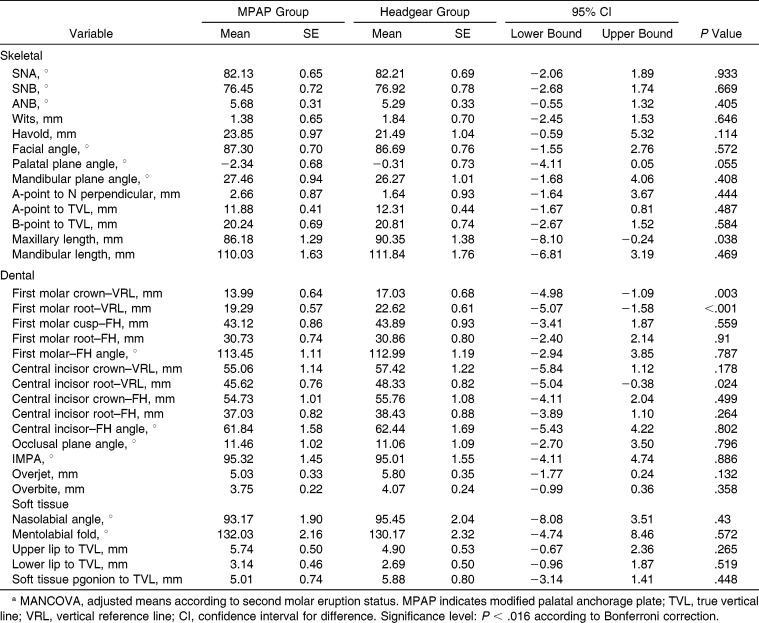
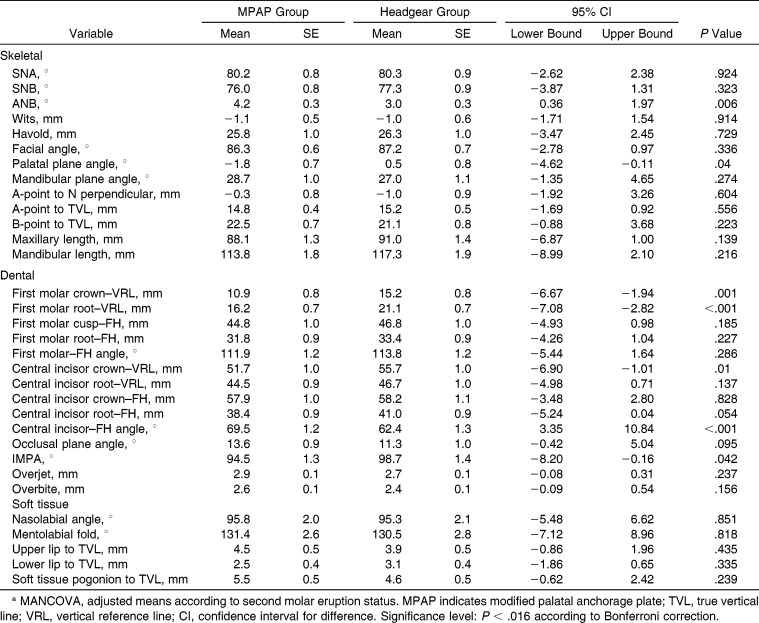
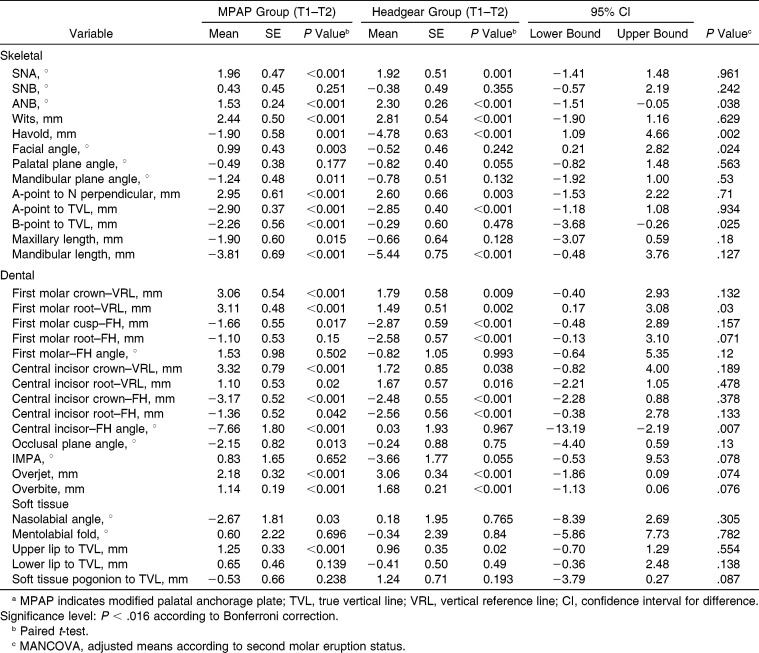
There was no significant main effect of the type of the appliance on the comparison of pre- and posttreatment variables (P = .198 and .135, respectively; Tables 2 and 3). Also, there was no significant effect of the second molar eruption status on both comparisons (P = .384 and .532, respectively). Similarly, there was no significant main effect of the type of the appliance or second molar eruption status on the treatment effects (P = .063 and .396, respectively; Table 4).
Table 2.
Comparison Between Cephalometric Variables of MPAP and Headgear Groups at Pretreatmenta
Table 3.
Comparison Between Cephalometric Variables of MPAP and Headgear Groups at Posttreatmenta
Table 4.
Comparison of Treatment Effects Between MPAP and Headgear Groupsa
Several skeletal variables showed significant changes between pre- and posttreatment values within each group. ANB decreased 1.53° ± 0.24° in the MPAP group and 2.30° ± 0.26° in the headgear group. The Wits also decreased 2.44 ± 0.50 mm and 2.81 ± 0.54 mm, respectively (P < .001; Table 4). Nonetheless, there was no significant difference between the groups regarding all of the skeletal variables based on univariate analysis (Table 4).
Sagittally, the amounts of distal movement of the maxillary first molar crown were 3.06 ± 0.54 mm in the MPAP group and 1.8 ± 0.58 mm in the headgear group. Meanwhile, the first molar root was distalized 3.11 ± 0.48 mm and 1.49 ± 0.51 mm, respectively. Vertically, the MPAP group showed slight extrusion of the maxillary first molar (−1.66 ± 0.55 mm), while the headgear group demonstrated significant extrusion (−2.87 ± 0.59 mm; P < .001). In addition, both groups showed no significant distal tipping of the maxillary first molar (P = .502 and .993, respectively). However, univarate analysis showed no significant difference between the groups regarding dental variables (Table 4).
For the central incisor, the MPAP group showed significant retraction, extrusion, and lingual inclination (P < .001), while the headgear group showed significant extrusion (P < .001). Nevertheless, univariate analysis showed no significant difference between the groups regarding these variables (Table 4).
Regarding soft tissue, in the MPAP group, the upper lip was significantly retracted (1.25 ± 0.33 mm; P < .001), and the nasolabial angle was increased −2.67° ± 1.81°, although not significantly. Likewise, in the headgear group, the change was not significant (0.96 ± 0.35 mm and 0.18° ± 1.95°, respectively). Soft tissue variables demonstrated no significant difference between the groups (Table 4). Treatment duration showed no significant difference between the MPAP (28.0 ± 8.2 months) and headgear groups (28.9 ± 10.5 months).
The survival rate of the miniscrews was 97.2%, with just three cases showing signs of soft tissue inflammation around the MPAP.
DISCUSSION
Distalization of the maxillary molars is often performed to gain space or to correct Class II dental relationships using TADs. MPAPs have been developed to offer a simple and effective nonextraction approach for distalization.23,24
Noncompliance appliances for molar distalization produced about 71% molar distalization and 29% reciprocal anchorage loss.7 However, TAD-anchored molar distalizing appliances showed 3.3–6.4 mm of distalization of the maxillary first molars without flaring of anterior teeth.26 Sar et al.27 demonstrated 2.81 mm of first molar distalization using skeletal anchorage. In agreement, the amount of distalization of the MPAP group in our study was 3.1 mm, with 3.3 mm of incisor retraction.
In addition to the retraction of anteriors in the MPAP group, there was extrusion and lingual inclination, while the headgear group showed only significant extrusion. This might be due to differences between the two treatment strategies. In the MPAP group, the upper lip was more protruded and the nasolabial angle was smaller than that of the headgear group, although this was not statistically significant. Moreover, both groups showed >5-mm overjet. In the MPAP group, the overjet was corrected through retracting and retroclining the upper incisors. On the other hand, the upper lip position was slightly better in the headgear group, which might have been due to a subjective difference in facial profile preference between the two different clinicians. Therefore, the correction of the overjet was accomplished by proclination of the mandibular incisors while maintaining the maxillary incisors in their sagittal position.
Yu et al.28 concluded that MPAP showed bodily molar movement without incisor flaring, while buccally placed mini-implants demonstrated distal tipping and extrusion of molars and flaring and intrusion of incisors. Our study showed 3.06 mm of distalization of the first molars for the MPAP group with 1.5° distal tipping. This bodily movement might have been because of the special design of the MPAP appliance (Figure 1). In the headgear group, the distal movement was 1.8 mm and the tipping was 0.82° mesially. Previous studies showed 6.4 and 3.9 mm of first molar distalization using TAD-anchored appliances, with distal tipping of 10.9° and 8.8°, respectively.13,14 Meanwhile, Burhan29 showed 5.5 mm of molar distalization, 4.9° of distal tipping, and 2.7 mm loss of anchorage with a Frog appliance; however, when combined with headgear, the values were 5.9 mm, 1.25°, and 0.9 mm, respectively, which increased bodily distalization with less anchorage loss.
The MPAP and headgear groups produced similar skeletal effects such as a reduction of ANB and Wits appraisal. In agreement, Kirjavainen et al.30 reported similar results of decreased ANB by 1.3°, using the cervical headgear.
Vertically, the MPAP group showed slight extrusion of maxillary first molars, while the headgear group demonstrated significant extrusion. This might be because the cervical headgear has limited control over the downward growth of the maxilla. Meanwhile, the MPAPs usually result in intrusion of molars.22,28 However, in this study, the intrusion was masked by the downward growth of the maxilla, resulting in extrusion, yet less than in the headgear group.
The effect that the eruption status of second molars has on distalization is still controversial. Several authors have reported minimal or no significant effect on the first molar movement,11,31–33 while others have demonstrated that the second molar eruption status might negatively affect first molar movement.34–36 Moreover, distal tipping of first molars was less in patients with erupted second molars.37 In addition, the first molar movement rate was almost two times greater before the eruption of second molars.34 In our study, the second molar eruption had no significant main effect on the comparisons between the groups; however, its effect on molar distalization was not evaluated. A previous study showed that the tooth bud might act as a fulcrum, resulting in an increased degree of tipping of the molars.37
This study compared fixed and removable appliances to show that MPAP could be considered for treatment of Class II patients. Therefore, it is recommended that clinicians consider the application of MPAP especially in noncompliant Class II patients.
CONCLUSIONS
The modified palatal anchorage plate showed significant skeletal changes on the maxilla. However, this was not significantly different from the headgear group.
Both MPAP and headgear resulted in significant distalization of maxillary first molars with no significant difference between them. In addition, both groups showed minimal distal tipping.
REFERENCES
- 1.Kloehn SJ. Orthodontics—force or persuasion. Angle Orthod. 1953;23:56–65. [Google Scholar]
- 2.Mann KR, Marshall SD, Qian F, Southard KA, Southard TE. Effect of maxillary anteroposterior position on profile esthetics in headgear-treated patients. Am J Orthod Dentofacial Orthop. 2011;139:228–234. doi: 10.1016/j.ajodo.2010.04.031. [DOI] [PubMed] [Google Scholar]
- 3.Osvaldik-Trapl M, Droschl H. Upper headgear versus lower headgear, yokes, and Class III elastics. Angle Orthod. 1978;48:57–61. doi: 10.1043/0003-3219(1978)048<0057:UHVLHY>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Poulton DR. The influence of extraoral traction. Am J Orthod. 1967;53:8–18. doi: 10.1016/0002-9416(67)90135-2. [DOI] [PubMed] [Google Scholar]
- 5.Turbill EA, Richmond S, Wright JL. Social inequality and discontinuation of orthodontic treatment: is there a link. Eur J Orthod. 2003;25:175–183. doi: 10.1093/ejo/25.2.175. [DOI] [PubMed] [Google Scholar]
- 6.Mehra T, Nanda RS, Sinha PK. Orthodontists' assessment and management of patient compliance. Angle Orthod. 1998;68:115–122. doi: 10.1043/0003-3219(1998)068<0115:OAAMOP>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Bolla E, Muratore F, Carano A, Bowman SJ. Evaluation of maxillary molar distalization with the distal jet: a comparison with other contemporary methods. Angle Orthod. 2002;72:481–494. doi: 10.1043/0003-3219(2002)072<0481:EOMMDW>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Chiu PP, McNamara JA, Jr, Franchi L. A comparison of two intraoral molar distalization appliances: distal jet versus pendulum. Am J Orthod Dentofacial Orthop. 2005;128:353–365. doi: 10.1016/j.ajodo.2004.04.031. [DOI] [PubMed] [Google Scholar]
- 9.Baccetti T, Franchi L, Stahl F. Comparison of 2 comprehensive Class II treatment protocols including the bonded Herbst and headgear appliances: a double-blind study of consecutively treated patients at puberty. Am J Orthod Dentofacial Orthop. 2009;135:698e1–10. doi: 10.1016/j.ajodo.2008.03.015. [DOI] [PubMed] [Google Scholar]
- 10.Sfondrini MF, Cacciafesta V, Sfondrini G. Upper molar distalization: a critical analysis. Orthod Craniofac Res. 2002;5:114–126. doi: 10.1034/j.1600-0544.2002.01155.x. [DOI] [PubMed] [Google Scholar]
- 11.Ghosh J, Nanda RS. Evaluation of an intraoral maxillary molar distalization technique. Am J Orthod Dentofacial Orthop. 1996;110:639–646. doi: 10.1016/s0889-5406(96)80041-2. [DOI] [PubMed] [Google Scholar]
- 12.Kinzinger GS, Eren M, Diedrich PR. Treatment effects of intraoral appliances with conventional anchorage designs for non-compliance maxillary molar distalization: a literature review. Eur J Orthod. 2008;30:558–571. doi: 10.1093/ejo/cjn047. [DOI] [PubMed] [Google Scholar]
- 13.Gelgor IE, Buyukyilmaz T, Karaman AI, Dolanmaz D, Kalayci A. Intraosseous screw-supported upper molar distalization. Angle Orthod. 2004;74:838–850. doi: 10.1043/0003-3219(2004)074<0838:ISUMD>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 14.Kircelli BH, Pektas ZO, Kircelli C. Maxillary molar distalization with a bone-anchored pendulum appliance. Angle Orthod. 2006;76:650–659. doi: 10.1043/0003-3219(2006)076[0650:MMDWAB]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 15.Park HS. The skeletal cortical anchorage using titanium microscrew implants. Korean J Orthod. 1999;29:699–706. [Google Scholar]
- 16.Park HS, Bae SM, Kyung HM, Sung JH. Micro-implant anchorage for treatment of skeletal Class I bialveolar protrusion. J Clin Orthod. 2001;35:417–422. [PubMed] [Google Scholar]
- 17.Oh YH, Park HS, Kwon TG. Treatment effects of microimplant-aided sliding mechanics on distal retraction of posterior teeth. Am J Orthod Dentofacial Orthop. 2011;139:470–481. doi: 10.1016/j.ajodo.2009.05.037. [DOI] [PubMed] [Google Scholar]
- 18.Triaca A, Antonini M, Wintermantel E. Ein neues Titan-Flachschrauben-Implantat zur orthodontischen Verankerung am anterioren Gaumen. Inf Orthod Kieferorthop. 1992;24:251–257. [Google Scholar]
- 19.Lee SM, Park JH, Bayome M, Kim HS, Mo SS, Kook YA. Palatal soft tissue thickness at different ages using an ultrasonic device. J Clin Pediatr Dent. 2012;36:405–409. doi: 10.17796/jcpd.36.4.58tm38928v522283. [DOI] [PubMed] [Google Scholar]
- 20.Ryu JH, Park JH, Vu Thi Thu T, Bayome M, Kim Y, Kook YA. Palatal bone thickness compared with cone-beam computed tomography in adolescents and adults for mini-implant placement. Am J Orthod Dentofacial Orthop. 2012;142:207–212. doi: 10.1016/j.ajodo.2012.03.027. [DOI] [PubMed] [Google Scholar]
- 21.Han S, Bayome M, Lee J, Lee YJ, Song HH, Kook YA. Evaluation of palatal bone density in adults and adolescents for application of skeletal anchorage devices. Angle Orthod. 2012;82:625–631. doi: 10.2319/071311-445.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kook YA, Bayome M, Trang VT, et al. Treatment effects of a modified palatal anchorage plate for distalization evaluated with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2014;146:47–54. doi: 10.1016/j.ajodo.2014.03.023. [DOI] [PubMed] [Google Scholar]
- 23.Kook YA, Kim SH, Chung KR. A modified palatal anchorage plate for simple and efficient distalization. J Clin Orthod. 2010;44:719–730. [PubMed] [Google Scholar]
- 24.Kook YA, Lee DH, Kim SH, Chung KR. Design improvements in the modified C-palatal plate for molar distalization. J Clin Orthod. 2013;47:241–248. [PubMed] [Google Scholar]
- 25.Baccetti T, Franchi L, McNamara JA., Jr The cervical vertebral maturation (CVM) method for the assessment of optimal treatment timing in dentofacial orthopedics. Semin Orthod. 2005;11:119–129. [Google Scholar]
- 26.Fudalej P, Antoszewska J. Are orthodontic distalizers reinforced with the temporary skeletal anchorage devices effective. Am J Orthod Dentofacial Orthop. 2011;139:722–729. doi: 10.1016/j.ajodo.2011.01.019. [DOI] [PubMed] [Google Scholar]
- 27.Sar C, Kaya B, Ozsoy O, Ozcirpici AA. Comparison of two implant-supported molar distalization systems. Angle Orthod. 2013;83:460–467. doi: 10.2319/080512-630.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yu IJ, Kook YA, Sung SJ, Lee KJ, Chun YS, Mo SS. Comparison of tooth displacement between buccal mini-implants and palatal plate anchorage for molar distalization: a finite element study. Eur J Orthod. 2014;36:394–402. doi: 10.1093/ejo/cjr130. [DOI] [PubMed] [Google Scholar]
- 29.Burhan AS. Combined treatment with headgear and the Frog appliance for maxillary molar distalization: a randomized controlled trial. Korean J Orthod. 2013;43:101–109. doi: 10.4041/kjod.2013.43.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kirjavainen M, Hurmerinta K, Kirjavainen T. Facial profile changes in early Class II correction with cervical headgear. Angle Orthod. 2007;77:960–967. doi: 10.2319/092106-384. [DOI] [PubMed] [Google Scholar]
- 31.Bussick TJ, McNamara JA., Jr Dentoalveolar and skeletal changes associated with the pendulum appliance. Am J Orthod Dentofacial Orthop. 2000;117:333–343. doi: 10.1016/s0889-5406(00)70238-1. [DOI] [PubMed] [Google Scholar]
- 32.Flores-Mir C, McGrath L, Heo G, Major PW. Efficiency of molar distalization associated with second and third molar eruption stage. Angle Orthod. 2013;83:735–742. doi: 10.2319/081612-658.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nienkemper M, Wilmes B, Pauls A, Yamaguchi S, Ludwig B, Drescher D. Treatment efficiency of mini-implant-borne distalization depending on age and second-molar eruption. J Orofac Orthop. 2014;75:118–132. doi: 10.1007/s00056-013-0199-z. [DOI] [PubMed] [Google Scholar]
- 34.Karlsson I, Bondemark L. Intraoral maxillary molar distalization. Angle Orthod. 2006;76:923–929. doi: 10.2319/110805-390. [DOI] [PubMed] [Google Scholar]
- 35.Gianelly AA. Distal movement of the maxillary molars. Am J Orthod Dentofacial Orthop. 1998;114:66–72. doi: 10.1016/s0889-5406(98)70240-9. [DOI] [PubMed] [Google Scholar]
- 36.Jeckel N, Rakosi T. Molar distalization by intra-oral force application. Eur J Orthod. 1991;13:43–46. doi: 10.1093/ejo/13.1.43. [DOI] [PubMed] [Google Scholar]
- 37.Kinzinger GS, Fritz UB, Sander FG, Diedrich PR. Efficiency of a pendulum appliance for molar distalization related to second and third molar eruption stage. Am J Orthod Dentofacial Orthop. 2004;125:8–23. doi: 10.1016/j.ajodo.2003.02.002. [DOI] [PubMed] [Google Scholar]