Abstract
Objective:
To investigate changes in maxillary alveolar bone thickness after maxillary incisor proclination and extrusion during anterior crossbite correction in a group of growing patients with Class III malocclusion.
Materials and Methods:
Maxillary incisors of 15 growing patients with anterior crossbite were proclined and extruded with 0.016″ beta-titanium advancing loops and Class III elastics. Lateral cephalograms were recorded before advancement (T0) and 4 months after a normal overjet and overbite were achieved (T1). Changes in alveolar bone thickness surrounding the maxillary incisors at the crestal (S1), midroot (S2), and apical (S3) levels were measured using cone-beam computed tomography (CBCT). Paired t-tests were used to determine the significance of the changes. A Spearman rank correlation analysis was performed to explore the relationship between thickness changes and the rate and amount of incisor movements.
Results:
Although statistically significant decreases were observed in palatal and total bone thickness at the S2 and S3 level (P < .05), the amounts of these changes were clinically insignificant, ranging from 0.34 to 0.59 mm. Changes in labial bone thickness at all levels were not significant. Changes in palatal bone thickness at S3 were negatively correlated with changes in incisor inclination. (r = −0.71; P < .05).
Conclusion:
In a group of growing patients with Class III malocclusion undergoing anterior crossbite correction, controlled tipping mechanics accompanied by extrusive force may produce successful tooth movement with minimal iatrogenic detriment to the alveolar bone.
Keywords: Alveolar bone thickness, CBCT, Light force, Incisor proclination, Incisor extrusion
INTRODUCTION
Patients exhibiting an anterior crossbite can be successfully treated by a maxillary archwire with advancing loops on a partially fixed appliance.1–3 The anterior part of the archwire tips the maxillary incisors forward, resulting in correction of the anterior crossbite. Nevertheless, a loss of maxillary labial alveolar bone is a common complication with incisor proclination.4,5
The use of forces exceeding the optimal level has been suggested to cause loss of the labial alveolar crest and labial gingival recession.6,7 Although approximately 200 g has been suggested as the horizontal force required for proclination of the four maxillary incisors,8 consensus has not yet been reached on the optimal magnitude of the force required.9,10 Recent studies have reported the possibility that teeth may be moved using light forces. Iwasaki et al.11 demonstrated movement of the maxillary canines with forces as light as 18 g. Similarly, Yee et al.12 measured the rate and amount of maxillary canine movement induced by heavy (300 g) and light (50 g) continuous forces; they reported that light forces provided a greater percentage of canine retraction than heavy forces and caused less strain on the anchorage. They suggested that application of light forces to an individual tooth may influence not only the adjacent alveolar bone, but also the neighboring cortical bone of the loaded area resulting in displacement of both tooth and alveolar bone. This principle may be applied to any direction of orthodontic tooth movement. We hypothesized that the alveolar bone thickness around the teeth would be unharmed by the use of light forces to move the maxillary incisors forward.
Yodthong et al.13 studied changes in alveolar bone thickness during maxillary incisor retraction with various mechanics and archwires. They reported that the rate of retraction, change of inclination, and extent of intrusion were positively related to the increase of labial and total alveolar bone thickness of the incisors. It would be interesting to investigate whether such relationships exist when the maxillary incisors are proclined with light forces. Our hypothesis was that when light forces are used to procline maxillary incisors, changes in alveolar thickness are not related to the rate or amount of tooth movement or to changes in inclination.
With the introduction of cone-beam computed tomography (CBCT), the true three-dimensional anatomy of the bone can be visualized and measured. It has been shown that CBCT can be used to quantify buccal bone height and thickness with high precision and accuracy.14 The purposes of this study were therefore to use CBCT to quantify maxillary anterior alveolar bone thickness changes after maxillary incisor proclination and extrusion with light forces in a group of growing patients and to determine the factors related to changes in alveolar bone thickness during incisor proclination.
MATERIALS AND METHODS
Subjects
This prospective study was approved by the Ethics Committee, Faculty of Dentistry, Prince of Songkla University. Sample-size calculation was based on the significant results from a similar study by Sarikaya et al.,15 who studied anterior tooth retraction (the difference of means = 0.78, and the difference of the standard deviations = 0.72). According to the table of sample-size determination for paired t-test,16 with the established significance level and power of the test set at 0.05 and 80% respectively, the sample size would be 11. The following criteria were used for patients: anterior crossbite in maximum intercuspation occlusion, mild skeletal Class III (−2° < ANB < 1°) with a hypodivergent or normodivergent growth pattern (SN-MP < 350), growth status at the prepubertal stage according to the hand and wrist maturation method (PP2–MP3cap),17 good general and oral health, no use of anti-inflammatory drugs for at least 6 months before or during the study, and no history of trauma to the maxillary anterior teeth. Before participating in the study, the parents of all subjects provided written informed consent after receiving a written explanation of the aim of the study.
Treatment Protocol
Fixed appliances were bonded to the molars and incisors (2 × 4 design, Roth System-Slot 0.022″; Ormco Corporation, Glendora, Calif) of both arches. The mandibular incisors were leveled and aligned until a 0.021″ × 0.025″ stainless steel passive utility archwire could be placed. Subjects were excluded if anterior crossbite was spontaneously corrected at this stage. Light-cured compomer was placed on the occlusal surface of the mandibular first molars to eliminate occlusal interference. The maxillary incisors were then leveled and aligned until a 0.021″ × 0.025″ stainless steel sectional wire was passively fitted and overlaid with a 0.016″ titanium-molybdenum archwire (Ormco Corporation) with advancing loops pushing against the buccal tubes of the first molars. Each loop was 5 mm high and 3 mm wide (Figure 1).
Figure 1.

Clinical setup with light force generated by the maxillary archwire with advancing loops and Class III elastics.
Extrusive force was applied to the incisors by having the patients wear bilateral Class III elastics (5/16″ 2 oz, Ormco Corporation). These extended from hooks in the maxillary archwire in the primary first molar or first premolar area to the mandibular lateral incisors. Patients were asked to wear the elastics full-time, except when brushing teeth or eating.
The advancing loops were activated 1 mm every 4 weeks until a 2-mm overjet was achieved. The compomer was then gradually reduced until the posterior teeth were well occluded and a normal overbite was achieved. A passive titanium-molybdenum archwire with stops was placed to maintain the achieved dental position. The advancing loops activation in combination with the Class III elastics resulted in forces averaging 89.6 ± 11.8 g anteriorly and 42.2±9.4 g extrusively. Averaged over the four incisors, each tooth was moved with a force of approximately 22.5 g anteriorly and 10.5 g vertically. These forces are 30% to 40% less than the previously recommended minimum forces for tipping (35 g) and extrusion (15 g) of an individual tooth.18,19
Lateral Cephalogram Analysis
Lateral cephalograms were taken when the maxillary incisors were well aligned and ready to be proclined (T0) and 4 months after achieving normal overjet and overbite (T1), when completion of the bone remodeling process was expected.20 The analysis was based on the method proposed by Pancherz.21 The horizontal reference plane was established from the sella with a 6° downward inclination to the sella-nasion (S-N) line. The vertical reference plane was perpendicular to the horizontal reference plane at the sella (Figure 2). The perpendicular distances from the following seven points were measured to both reference planes: anterior nasal spine (ANS), A-point, incisal edge of the maxillary incisor (M×I), and B-point. The ANB angle, the palatal plane (PP) to the SN plane, and the maxillary incisor inclination to the PP were also measured (Figure 3).The changes of maxillary incisor positions in the horizontal and vertical planes were used to calculate for the rates of maxillary incisor proclination and extrusion.
Figure 2.
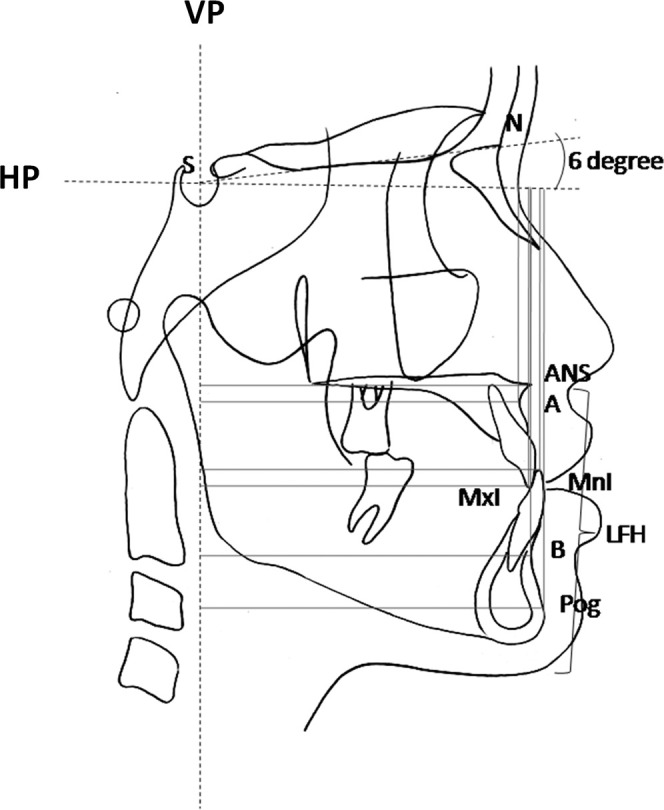
Cephalometric reference planes and points used in this study.
Figure 3.
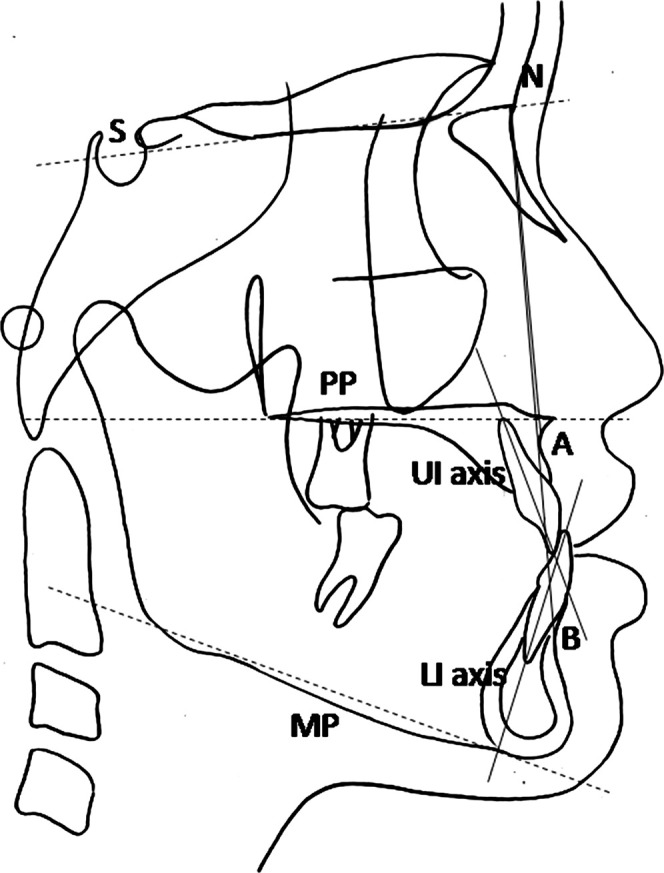
Cephalometric reference points and lines used in this study.
CBCT Analysis
Changes in the maxillary anterior alveolar bone were evaluated using computed tomography scans (80 kV, 5 mA, 7.5 second exposure time, 0.125 mm voxel resolution, and 80 × 40 mm field of view; Veraviewepocs J Morita MPG, Kyoto, Japan). The CBCT data were reconstructed at 0.125-mm increments. The Digital Imaging and Communications in Medicine (DICOM) images were assessed as described by Sarikaya et al.15 The thickness of the labial and palatal alveolar plates of each tooth were determined at the site adjacent to the widest point of the labiopalatal root, in three slices separated by 3 mm (S1, S2, and S3, respectively; Figure 4); these levels were specified along the long axis of the tooth and located every 3 mm above the cementoenamel junction (CEJ) level. Labial, palatal, and total alveolar bone thickness were assessed at the crestal level (S1; L1, P1, and T1), midroot level (S2; L2, P2, and T2) and apical level (S3; L3, P3, and T3) at T0 and T1. The alveolar thickness of each side and level of the four incisors were then averaged to represent mean thickness of the particular side and level.
Figure 4.
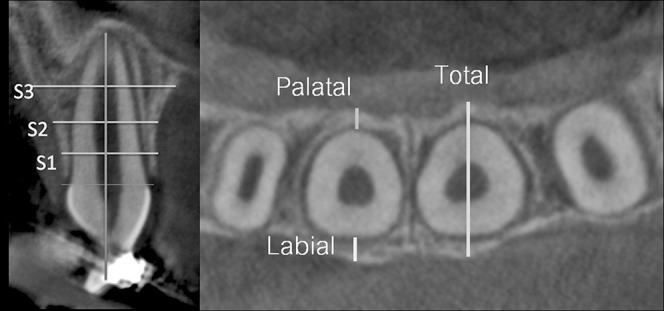
Location of alveolar bone thickness measurements.
The method of alveolar thickness measurement perpendicular to the tooth axis cannot detect thickness changes at the same point because as the tooth axis changes, the measured points on the bone change as well. However, the advantage of this method is that it observes alveolar thickness relative to the root, which is of clinical concern.
Statistical Analysis
Shapiro-Wilk tests demonstrated that all of the tested parameters were normally distributed. Hence, paired t-tests were used to evaluate the changes between T0 and T1. A Spearman rank correlation analysis was used to analyze the relationship between amount and rate of dental movement and changes of alveolar bone thickness. The significance level of all tests was established at .05.
The CBCT and cephalometric measurement error for two sets of measurements for each data point taken 4 weeks apart by the same investigator was assessed using the Dahlberg formula.22 The error for each parameter measured was less than 0.05. Paired t-tests showed no significant differences (P > .05) between the two sets of measurements. The intraclass correlation coefficients for all measurements were higher than 0.9, indicating that the measured data were sufficiently reliable.
RESULTS
Fifteen patients (11 girls and 4 boys; mean age, 9.9 ± 1.0 years) were involved in the study. As skeletal growth does not vary by sex during the prepubertal stage,23 the data from all subjects were pooled for statistical analysis. The average treatment duration was 10.6 ± 0.5 months. Of this time, 5.6 ± 1.7 months were spent on aligning and leveling, and 5.0±3.6 months on incisor proclination.
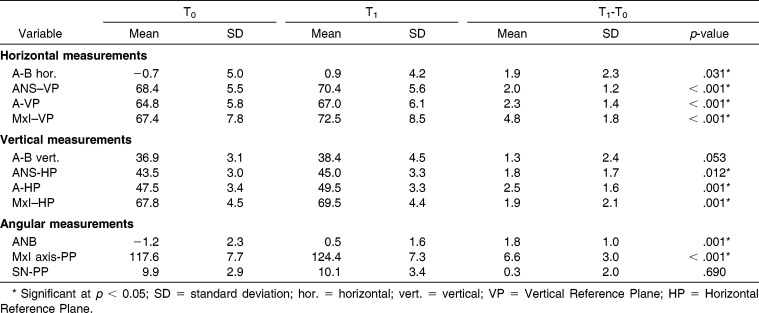
Table 1 shows the mean values and differences in cephalometric measurements at T0 and T1. Dentally, forward movement, labial tipping, and extrusion of the maxillary incisors were significant (ΔMxI-VP = 4.8 ± 1.8 mm; ΔMxI axis-PP = 6.6° ±3.0°; P < .001; ΔMxI-HP = 1.9 ± 2.1 mm; P = .001). Skeletally, the ANB angle improved by 1.8±1.0° (P = .001) due to significant forward movement of the A-point (ΔA-VP = 2.3 ± 1.4 mm; P < .001). The maxillary incisors were proclined and extruded at the rate of 0.8±0.3 mm/month and 0.2 ± 0.3 mm/month respectively.
Table 1.
Mean Cephalometric Values and Differences Before (T0) and 4 Months After (T1) Incisor Advancement
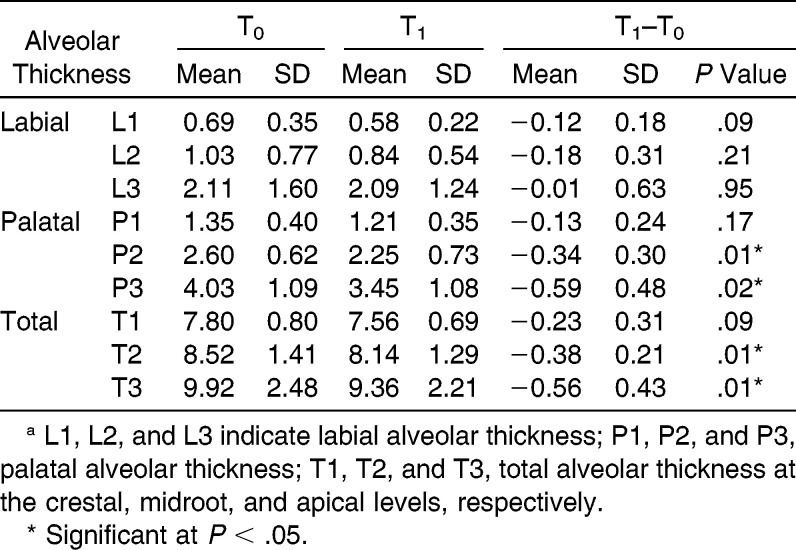
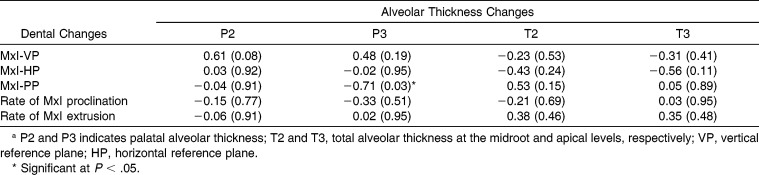
The changes in alveolar bone thickness between T0 and T1 are shown in Table 2. After the proclination and extrusion of maxillary incisors, the alveolar bone thickness at the P2, P3, T2, and T3 areas significantly decreased (P < .05). None of the labial alveolar thickness parameters (L1, L2, L3) changed significantly. Correlation coefficients (r) between significant alveolar thickness changes and dental changes are presented in Table 3. Change in alveolar thickness at P3 was significantly and negatively correlated with MxI-PP (r = −0.71; P = .03). Neither the rate nor the amount of incisor movement was significantly related to alveolar thickness changes.
Table 2.
Comparison of Means and Standard Deviations (SDS) of Alveolar Thickness for Maxillary Incisors Before (T0) and 4 Months After (T1) Incisor Advancementa
Table 3.
Spearman Rank Correlation Coefficients and P Values Between Alveolar Thickness Changes and Dental Changesa
DISCUSSION
The present investigation shows that alveolar bone remodeling may not be consistent with tooth movement. The finding is in agreement with that of previous studies using CBCT to measure bone thickness changes.13,15,24,25 However, although all of those studies, assumed to use optimal force levels, found significant decrease of bone thickness in the direction of tooth movement, our study revealed that as the incisors were moved forward with light forces, the labial alveolar thickness on all levels (L1, L2, L3) remained unchanged.
Alveolar bone may respond to different force magnitudes differently. It has been postulated that light orthodontic forces promote better cellular activity in the surrounding tissues than heavy forces, which subsequently not only improves the frontal resorption process26 but also promotes bone apposition.27 Successful canine movement across a bone-deficient alveolar ridge using light force with subsequent bony apposition to the defect area has been reported.27
Additionally, the ability to maintain labial alveolar bone thickness may be explained by the fact that growing children have a higher bone turnover rate than adults.28 Rapid bone remodeling in children may overtake the bone resorption and apposition processes due to orthodontic tooth movement, and thus maintain the labial alveolar bone thickness.
With light extrusion forces, alveolar bone thicknesses in the crestal level (L1, P1, T1) were maintained. This is consistent with a previous study that showed additional crestal alveolar bone increases in both the vertical and buccolingual dimensions as a result of light-force extrusion.19 However, such favorable bony reactions did not occur in the midroot and apical levels. During extrusion, the tooth entered the narrower part of the alveolar bone housing. If the bone remodeling process could not keep up with the rate of tooth movement, a decrease in total alveolar bone thickness would be observed.
Bony responses to light forces on the labial and palatal sides may be different as we found inconsistent bone thickness changes on the labial and palatal sides. Also, the more the incisors were tipped labially, the more the bone thickness at the apico-palatal area decreased. Research on the effect of different degrees of tip and torque movements with light force may lead to a better understanding of how alveolar bone reacts to light forces in different areas.
In terms of clinical application, we advocate the application of light orthodontic forces to procline and extrude maxillary incisors in children with anterior crossbite. The ability to preserve labial bone thickness indicates that light forces allow orthodontists to move the maxillary incisors labially and vertically with less harm to the alveolar bone. The decrease in palatal bone thickness of approximately 0.5 mm, although statistically significant, may be considered of no clinical consequence.
Apart from the small sample size, some limitations of this study must be considered. First, because of ethical considerations, patients with Class III malocclusion and anterior crossbite should be treated immediately. As a consequence, we were unable to collect data from untreated control subjects to distinguish the changes due to mechanics from the effects of growth. Second, the study was cross-sectional, whereas bone remodeling takes place continuously. Therefore, dynamic changes were not observed. Third, CBCT was performed after the completion of leveling and aligning, so information on the initial bone changes is lacking. The results must be interpreted with caution. Last, long-term changes in bone thickness after orthodontic treatment were not evaluated. A longitudinal observational study beyond treatment completion may provide further insight into the long-term alveolar bone remodeling process.
CONCLUSIONS
With the use of light forces to procline and extrude maxillary incisors
The palatal and total alveolar bone thickness at the midroot and apical levels decreased, but these changes could be considered clinically insignificant.
The change in apico-palatal alveolar bone thickness was negatively related to changes in incisor inclination.
ACNOWLEDGMENTS
We would like to thank the Graduate School and the Faculty of Dentistry, Prince of Songkla University, for grant support and Associate Professor Chidchanok Leethanakul for help preparing the manuscript.
REFERENCES
- 1.Rabie AB, Gu Y. Management of pseudo Class III malocclusion in southern Chinese children. Br Dent J. 1999;186(special no):183–187. doi: 10.1038/sj.bdj.4800058. [DOI] [PubMed] [Google Scholar]
- 2.Gu Y, Rabie AB, Hagg U. Treatment effects of simple fixed appliance and reverse headgear in correction of anterior crossbites. Am J Orthod Dentofacial Orthop. 2000;117:691–699. [PubMed] [Google Scholar]
- 3.Dowsing P, Sandler PJ. How to effectively use a 2 × 4 appliance. J Orthod. 2004;31:248–258. doi: 10.1179/146531204225020541. [DOI] [PubMed] [Google Scholar]
- 4.Sperry TP, Speidel TM, Isaacson RJ, Worms FW. The role of dental compensations in the orthodontic treatment of mandibular prognathism. Angle Orthod. 1977;47:293–299. doi: 10.1043/0003-3219(1977)047<0293:TRODCI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Kornhauser S, Schwartz Z, Bimstein E. Changes in the gingival structure of maxillary permanent teeth related to the orthodontic correction of simple anterior crossbite. Am J Orthod Dentofacial Orthop. 1996;110:263–268. doi: 10.1016/s0889-5406(96)80009-6. [DOI] [PubMed] [Google Scholar]
- 6.Khouw FE, Goldhaber P. Changes in vasculature of the periodontium associated with tooth movement in the rhesus monkey and dog. Arch Oral Biol. 1970;15:1125–1132. doi: 10.1016/0003-9969(70)90003-8. [DOI] [PubMed] [Google Scholar]
- 7.Krishnan V, Davidovitch Z. Cellular, molecular, and tissue-level reactions to orthodontic force. Am J Orthod Dentofacial Orthop. 2006;129:469.e1–e32. doi: 10.1016/j.ajodo.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 8.Quinn RS, Yoshikawa DK. A reassessment of force magnitude in orthodontics. Am J Orthod. 1985;88:252–260. doi: 10.1016/s0002-9416(85)90220-9. [DOI] [PubMed] [Google Scholar]
- 9.Ren Y, Maltha JC, Kuijpers-Jagtman AM. Optimum force magnitude for orthodontic tooth movement: a systematic literature review. Angle Orthod. 2003;73:86–92. doi: 10.1043/0003-3219(2003)073<0086:OFMFOT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Ren Y, Maltha JC, Van't Hof MA, Kuijpers-Jagtman AM. Optimum force magnitude for orthodontic tooth movement: a mathematic model. Am J Orthod Dentofacial Orthop. 2004;125:71–77. doi: 10.1016/j.ajodo.2003.02.005. [DOI] [PubMed] [Google Scholar]
- 11.Iwasaki LR, Haack JE, Nickel JC, Morton J. Human tooth movement in response to continuous stress of low magnitude. Am J Orthod Dentofacial Orthop. 2000;117:175–183. doi: 10.1016/s0889-5406(00)70229-0. [DOI] [PubMed] [Google Scholar]
- 12.Yee JA, Turk T, Elekdag-Turk S, Cheng LL, Darendeliler MA. Rate of tooth movement under heavy and light continuous orthodontic forces. Am J Orthod Dentofacial Orthop. 2009;136:150.e1–e9; discussion 50–51. doi: 10.1016/j.ajodo.2009.03.026. [DOI] [PubMed] [Google Scholar]
- 13.Yodthong N, Charoemratrote C, Leethanakul C. Factors related to alveolar bone thickness during upper incisor retraction. Angle Orthod. 2013;83:394–401. doi: 10.2319/062912-534.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Timock AM, Cook V, McDonald T, et al. Accuracy and reliability of buccal bone height and thickness measurements from cone-beam computed tomography imaging. Am J Orthod Dentofacial Orthop. 2011;140:734–744. doi: 10.1016/j.ajodo.2011.06.021. [DOI] [PubMed] [Google Scholar]
- 15.Sarikaya S, Haydar B, Ciger S, Ariyurek M. Changes in alveolar bone thickness due to retraction of anterior teeth. Am J Orthod Dentofacial Orthop. 2002;122:15–26. doi: 10.1067/mod.2002.119804. [DOI] [PubMed] [Google Scholar]
- 16.Knapp RG, Miller MC. Clinical Epidemiology and Biostatistics. Baltimore, MD: Williams & Wilkins; 1992. [Google Scholar]
- 17.Grave KC, Brown T. Skeletal ossification and the adolescent growth spurt. Am J Orthod. 1976;69:611–619. doi: 10.1016/0002-9416(76)90143-3. [DOI] [PubMed] [Google Scholar]
- 18.Proffit WR, Fields HW, Sarver DM. Contemporary Orthodontics 4th ed. St Louis, MO: Mosby Elsevier; 2007. [Google Scholar]
- 19.Korayem M, Flores-Mir C, Nassar U, Olfert K. Implant site development by orthodontic extrusion. A systematic review. Angle Orthod. 2008;78:752–760. doi: 10.2319/0003-3219(2008)078[0752:ISDBOE]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 20.Wainwright WM. Faciolingual tooth movement: its influence on the root and cortical plate. Am J Orthod. 1973;64:278–302. doi: 10.1016/0002-9416(73)90021-3. [DOI] [PubMed] [Google Scholar]
- 21.Pancherz H. The mechanism of Class II correction in Herbst appliance treatment. A cephalometric investigation. Am J Orthod. 1982;82:104–113. doi: 10.1016/0002-9416(82)90489-4. [DOI] [PubMed] [Google Scholar]
- 22.Dahlberg G. Statistical Methods for Medical and Biological Students. London, UK: G. Allen & Unwin Ltd; 1940. [Google Scholar]
- 23.Alexander AE, McNamara JA, Jr, Franchi L, Baccetti T. Semilongitudinal cephalometric study of craniofacial growth in untreated Class III malocclusion. Am J Orthod Dentofacial Orthop. 2009;135:700.e1–e14; discussion 00-1. doi: 10.1016/j.ajodo.2008.06.025. [DOI] [PubMed] [Google Scholar]
- 24.Ahn HW, Moon SC, Baek SH. Morphometric evaluation of changes in the alveolar bone and roots of the maxillary anterior teeth before and after en masse retraction using cone-beam computed tomography. Angle Orthod. 2013;83:212–221. doi: 10.2319/041812-325.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Picanco PR, Valarelli FP, Cancado RH, Freitas KM, Picanco GV. Comparison of the changes of alveolar bone thickness in maxillary incisor area in extraction and non-extraction cases: Computerized tomography evaluation. Dental Press J Orthod. 2013;18:91–98. doi: 10.1590/s2176-94512013000500016. [DOI] [PubMed] [Google Scholar]
- 26.Tomizuka R, Shimizu Y, Kanetaka H, et al. Histological evaluation of the effects of initially light and gradually increasing force on orthodontic tooth movement. Angle Orthod. 2007;77:410–416. doi: 10.2319/0003-3219(2007)077[0410:HEOTEO]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 27.Hibino K, Wong RW. Orthodontic tooth movement enhancing bony apposition in alveolar bony defect: a case report. Cases J. 2009;2:116. doi: 10.1186/1757-1626-2-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Szulc P, Seeman E, Delmas PD. Biochemical measurements of bone turnover in children and adolescents. Osteoporos Int. 2000;11:281–294. doi: 10.1007/s001980070116. [DOI] [PubMed] [Google Scholar]