Abstract
Objective:
To assess oral health–related quality of life (OHRQoL) in young adult patients with malocclusion and to measure the association between orthodontic treatment need and OHRQoL.
Materials and Methods:
The study sample comprised 190 young adults aged 18 to 25 years who were attending orthodontic clinics at the Faculty of Dentistry. The Index of Orthodontic Treatment Need-Dental Health Component was used to measure orthodontic treatment need. Each participant was assessed for OHRQoL before and after treatment by using the Oral Health Impact Profile, Chinese version (OHIP-14).
Results:
Patients who had little or no, borderline, and actual need for orthodontic treatment represented 21.6%, 50.5%, and 27.9% of the total sample, respectively. OHRQoL (total OHIP-14 score and score for each domain) improved after treatment (P < .05). Significant differences in summary OHIP-14 scores were apparent with respect to orthodontic treatment need. Participants with high treatment need reported a significantly greater negative impact on the overall OHRQoL score. The greatest impact was seen in the psychological discomfort domain and the psychological disability domain.
Conclusion:
Malocclusion has a significant negative impact on OHRQoL. This is greatest for the psychological discomfort and psychological disability domains. The orthodontic treatment of malocclusion improves OHRQoL of patients.
Keywords: Oral health–related quality of life, Orthodontic treatment needs, Malocclusion
INTRODUCTION
Malocclusion and dentofacial deformities are highly prevalent and can influence physical, social, and psychological functioning, thus playing an important role in social acceptance and interactions.1,2 The concept of oral health-related quality of life (OHRQoL) corresponds to the impact of oral health or disease on a person's daily functioning, well-being, or overall quality of life.3 Research on the physical, social, and psychological impact of malocclusion on OHRQoL sheds light on the effects of malocclusion on people's lives and provides a greater understanding of the demand for orthodontic treatment beyond the measurement of clinical parameters.4 Because social and psychological effects are often the key motives for seeking orthodontic treatment, OHRQoL can be considered the measurement for orthodontic treatment need and outcome.5
More recently, a number of orthodontic need indices have been developed and used as outcome measures. However, it is questionable whether there is a strong association between orthodontic indices and patients' perception of their oral health status.6 The Index of Orthodontic Treatment Need (IOTN) is a scoring system for malocclusion, which has been used extensively in the literature to evaluate actual and perceptive orthodontic treatment needs.7 However, there is evidence that many people with normative orthodontic treatment need measured by IOTN experience no impacts on their OHRQoL, whereas others with minor irregularity report high negative impacts on quality of life.8 Therefore, the use of IOTN alone to establish orthodontic treatment need may be potentially problematic.
Most of the research has focused on the impact of malocclusion on quality of life in children rather adults. This relates in part to the fact that children make up the majority of orthodontic patients, although it is increasingly recognized that more and more adults are seeking correction of their malocclusion. A systematic review revealed no high-quality studies on the association of malocclusion (longitudinal studies) or its associated treatment (randomized controlled trials). Most evidence is cross-sectional and based on reduced samples of individuals.9 In this study, we aimed to evaluate the impact of oral health–related problems on quality of life in young adults with dentofacial deformities, using the Oral Health Impact Profile, Chinese version (OHIP-14), and to evaluate the relationship between orthodontic treatment need and OHRQoL.
MATERIALS AND METHODS
Participants in the study were young adults aged 18 to 25 years, who were attending orthodontic clinics at Guanghua School of Stomatology, Hospital of Stomatology, Sun Yat-sen University, in China. Ethical approval from the Ethics Committee of the Guanghua Stomatology Institute was obtained at the beginning of the study, and informed consent was obtained before beginning data collection. The participants were informed about the examination procedures and were assured of the confidentiality of the collected information. Only those who gave consent were included in the research. A convenience consecutive sampling approach was used. The participants were recruited at their first visit for orthodontic screening before starting any orthodontic treatment. Exclusion criteria were patients with untreated dental caries (cavitated lesions), periodontal diseases (periodontal pockets >4 mm), missing teeth in need of prosthetic rehabilitation, previous orthodontic treatment, and patients for whom combined orthodontic treatment and orthognathic surgery was proposed or planned. A sample-size calculation was carried out using data from a study investigating the effects of orthodontic treatment on quality of life.10 It was estimated that a sample size of 48 subjects would be needed to demonstrate a significant change in OHRQoL, with an 80% probability power at the 5% level of significance. The sample size was inflated by a 10% margin to allow for loss to follow-up and dropouts; thus, the total sample size was a minimum of 52.
Variables and Their Measurement
For the OHRQoL assessment, a cultural and linguistically valid and reliable version of the OHIP-14, which has shown good psychometric properties, similar to those from the original instrument, was used.11,12 The OHIP-14 assesses the burden of oral health status on life quality across seven domains (two items per domain) by asking subjects to rate the frequency with which a particular problem occurred, as captured by the individual item. The dimensions are functional limitation, physical pain, psychological discomfort, physical disability, psychological disability, social disability, and handicap. Responses are rated on a five-point Likert scale: 0 = never; 1 = hardly ever; 2 = occasionally; 3 = fairly often; 4 = very often/every day. Summary OHIP-14 scores can range from 0 to 56, and domain scores can range from 0 to 8. A higher OHIP-14 score indicates poorer OHRQoL. To assess external reliability, 10% of the sample answered the questionnaire twice and were interviewed on two consecutive days. Test-retest reliability was carried out on all questions of OHRQoL measures. The correlation coefficient used to calculate the correlation between the two sets of observations was 0.85 in OHIP-14. The Cronbach α adopted to assess the internal consistency was 0.86 for the OHIP-14. Ultimately, the OHIP-14 was presented to subjects for a retrospective evaluation of OHRQoL at baseline (T1), and after treatment (T2).
Each patient was examined for orthodontic treatment need with the dental health component (DHC) of the IOTN before starting any orthodontic treatment. This index has gained international acceptance because it is valid, reliable, and easy to use.13 The training and calibration exercise consisted of two steps (theoretical and clinical) according to a study of how oral health conditions affect quality of life.14 Data analysis involved the calculation of the Cohen κ coefficient on a tooth-by-tooth basis (κ = 0.896–0.915 for both inter- and intraexaminer agreement). As the κ coefficients were good, the examiners were considered able to perform the study. The DHC is a five-grade index that categorizes treatment need as little or no treatment need (DHC score = 1 or 2), borderline need (DHC score = 3) and treatment required (DHC score = 4 or 5). The DHC uses a simple ruler and an acronym—MOCDO (missing teeth, overjet, crossbite, displacements of contact points, overbite)—to identify the most severe occlusal trait for each patient. The overall score was given to the patient according to the most severe trait.
Statistical Analysis
Data analysis was performed using the Statistical Package for the Social Science software (SPSS, version 19.0, SPSS Inc, Chicago, Ill), with statistical significance set at P < .05. Changes occurring during follow-up were normally distributed, so statistical significances of the changes were evaluated with paired samples t-tests. One-way analysis of variance (ANOVA) with Bonferroni test was used to assess differences in OHRQoL across groups as defined by the IOTN-DHC.
RESULTS
Of 220 patients invited to participate, only eight refused to take part, giving a 96% response rate, despite no financial or other incentive being offered. Therefore, 212 young adult patients were recruited to the study, all of whom were of Chinese ethnicity. However, a further 22 patients (10.4%) who met exclusion criteria were subsequently removed from further analysis. Thus, the final sample was 190 patients, maintaining the statistical power of the study.
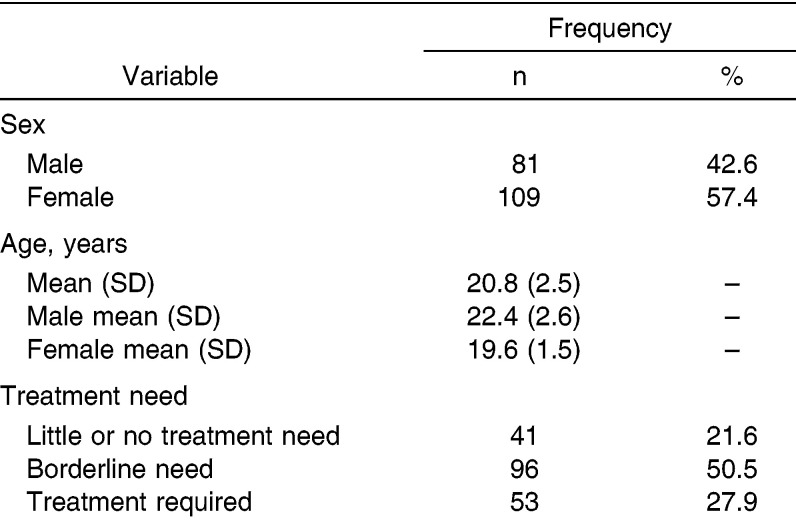
Table 1 shows that male and female subjects made up 42.6% and 57.4% of the sample, respectively. Most patients were female (n = 109). The mean age of the total sample was 20.8 years. In this study, more than half (50.5%; 96 of 190) of the sample had borderline need for orthodontic treatment. Furthermore, 21.6% of the subjects did not have IOTN orthodontic need (grades 1 and 2 of the IOTN) and 27.9% did have orthodontic need (grades 4 and 5 of the IOTN).
Table 1.
Characteristics and Orthodontic Treatment Needs of the Study Sample
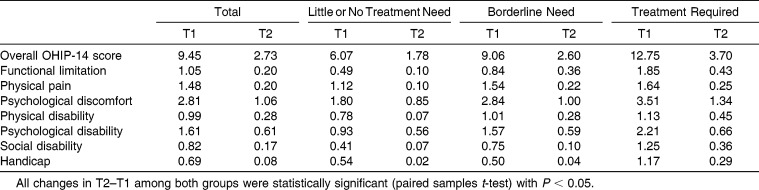
All 190 participants answered the OHRQoL questionnaire completely before and after orthodontic treatment; there were no missing responses. Table 2 displays the mean total OHIP-14 score and the mean score for each domain among different types of IOTN-DHC groups at T1 and T2. Before treatment, the mean overall score for OHIP-14 was 9.45. The mean score (2.81) of the psychological discomfort domain of the OHIP-14 showed the highest impact due to malocclusion in patients, whereas the handicap domain had the lowest reported impact with a mean score of (0.69). Significant difference in overall scores was detected between baseline and end of treatment. Statistically significant changes were observed among all seven domain scores. The paired-samples t-test analysis showed that OHRQoL and its dimensions improved after treatment regardless of the type of treatment need (Table 2).
Table 2.
Mean Scores in Overall and Seven Domains of Oral Health Impact Profile-14 (OHIP-14) OHIP-14 Among Different Types of Index of Orthodontic Treatment Need-Dental Health Component (IOTN-DHC) Groups Before Treatment (T1) and After Treatment (T2)
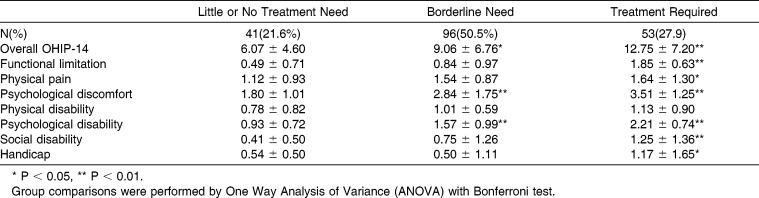
Table 3 shows the results from the one-way ANOVA and Bonferroni test comparing groups defined by IOTN-DHC. Significant differences in summary OHIP-14 scores were apparent with respect to orthodontic treatment need (P < .05). Participants with high treatment need reported a significantly greater negative impact on the overall OHRQoL score and in each domain of the OHIP-14, except the physical disability domain. The greatest impact was seen in the psychological discomfort domain and the psychological disability domain, where even having borderline need was associated with a significant difference in OHIP-14 scores compared with the group needing little or no treatment. Besides, the domains of functional limitation, physical pain, handicap, and social disability all showed a significant difference in OHIP-14 score at the level of the borderline treatment need group.
Table 3.
Mean Scores in Overall and Seven Domains of Oral Health Impact Profile-14 (OHIP-14) OHIP-14 Among Different Types of Index of Orthodontic Treatment Need-Dental Health Component (IOTN-DHC) Groups
DISCUSSION
One of the main findings of this study was that improvement due to orthodontic treatment seems to lead to significant improvement in OHRQoL (Table 2). The positive change in OHRQoL because of orthodontic treatment is in line with findings of earlier studies of children. De Oliveira et al.6 conducted a cross-sectional study with 15- to 16-year-old Brazilian children and concluded that those who had completed orthodontic treatment had a better OHRQoL than those currently undergoing treatment or those who had never been treated. Bernabé et al.15 found that Brazilian adolescents with a history of completed orthodontic treatment experienced fewer condition-specific impacts on their daily lives attributed to malocclusion than did adolescents with no history of treatment. However, studies have not yet provided much evidence showing the effect of conventional orthodontic treatment on quality of life in adults. Palomares et al.16 found that adults who had completed orthodontic treatment and were in the retention phase of treatment were found to have better OHRQoL than nontreated subjects who were waiting for treatment. Johal et al.17 reported that during the first 3 months of fixed orthodontic therapy there appeared to be a negative impact on the overall OHRQoL with a gradual observed return at 6 months and a complete return at the end of treatment where OHRQoL improved to pretreatment scores. Our earlier study, which followed 250 Chinese orthodontic patients, showed that their OHRQoL was better after they completed treatment than before or during treatment.11 It is generally considered that patients benefit psychologically from orthodontic treatment through improved facial and dental appearance and the increased self-confidence that accompanies those changes. Improvement in esthetic satisfaction due to the treatment of severe malocclusion improves OHRQoL, particularly by decreasing psychological discomfort and psychological disability.18 Our study indicates that satisfaction after treatment was generally high, with patients perceiving OHRQoL more positively.
Previous research exploring the relationship between malocclusions and OHRQoL, as well as the impact of orthodontic treatment on OHRQOL has been equivocal. Some authors found a strong relationship between malocclusion or orthodontic treatment need and OHRQoL, but others reported no clear relationship.9,19 The following reasons may account for the different findings: use of different measures; wide age range or different age groups; different cultures, traditions, and social norms across countries; and different races and ethnic groups. In this study, statistical analysis showed that participants with more severe malocclusions reported a greater impact on quality of life (Table 3). The patients who had an orthodontic treatment need, according to the IOTN had poorer OHRQoL (greater OHIP-14 scores) before treatment. Young people with borderline and high orthodontic treatment need scored 3 and 6 points higher, respectively, on the OHIP-14 scale compared with the no treatment need group. This suggests that orthodontic treatment need and poor OHRQoL coexist in the same population. The sociodental approach, which combines normative and psychosocial perception of occlusion, is recommended for routine evaluation of treatment need so that measures of patients' views complement clinical measures.20
In this study, the physiological discomfort domain including tenseness and self-consciousness was significantly correlated to orthodontic treatment needs. The findings of the study suggest that orthodontic patients mainly suffer esthetic and social problems rather than impairment of daily activities, and minor differences in orthodontic treatment needs may have a significant effect on perceived OHRQoL in the physiological discomfort domain. Previous research supports the finding of an association between malocclusion and psychological discomfort.6,21–23 Psychometric scales reveal that questions related to emotional and social domains, including such aspects as shyness, embarrassment, being upset, and avoidance of smiling or laughing, are more relevant to an orthodontic patient.24 Also, Hassan and Amin25 found that in both male and female patients, the need for orthodontic treatment significantly affected self-consciousness and feelings of tension. Besides, orthodontic patients with clinically assessed greater orthodontic needs reported more psychological disability (difficulty relaxing and embarrassment,) than those with no or borderline orthodontic treatment needs. Zhou et al.26,27 found that nearly half of the patients with malocclusion had a nickname related to their dentofacial problems, and 8 of 10 of these patients felt embarrassed or angry about their nickname. In addition, the psychological status (embarrassment, feeling worn out, anger, pressure from friends, and so on) of patients with skeletal malocclusion was closely related to severity of the malocclusion.26,27 Seehra et al.28 also reported that significant relationships exist between bullying and certain occlusal traits, self-esteem, and OHRQoL. Patients with malocclusion can develop feelings of self-consciousness and shame about their dental condition or may feel shy in social contexts, and because of their facial appearance their body self-concept might be negatively affected.24,29 It has been recognized that the most common reason for seeking orthodontic treatment is to correct dental esthetics and improve self-esteem.22 Thus, orthodontists should be aware that young adult patients might expect orthodontic treatment to provide not only improved oral functioning and health but also enhancement of esthetics, self- esteem, and social life.30 The use of the OHRQoL measure as part of the diagnostic procedure may provide information on priorities for treatment in order to maximize patient satisfaction.22,31 However, the OHIP-14 has only four items (of 14) specific to the assessment of psychological status. It could be inferred that an ideal instrument for orthodontic-related quality of life research might need to have more consideration of psychological aspects as they play important roles in determining how malocclusion affects quality of life.32
CONCLUSIONS
Malocclusion has a significant negative impact on OHRQoL and its domains. The greatest impact was seen in the psychological discomfort and psychological disability domains.
Orthodontic treatment clearly improved the OHRQoL among adults. These results highlight the impact of malocclusion on the OHRQOL of young adults and emphasize the importance of patient-based evaluation of oral health status and oral health needs.
ACKNOWLEDGMENTS
The authors would like to thank all reviewers for their thoughtful comments in the manuscript. This work was partially supported by grants from the Project of the National Natural Science Foundation of China (Grant No. 81300862), the Project of Health and Family Planning Commission of Shenzhen Municipality (Grant No. 201302202), and the Project of Science and Technology Innovation Commission of Nanshan Municipality (Grant No. 2012040).
REFERENCES
- 1.Rusanen J, Lahti S, Tolvanen M, Pirttiniemi P. Quality of life in patients with severe malocclusion before treatment. Eur J Orthod. 2010;32:43–48. doi: 10.1093/ejo/cjp065. [DOI] [PubMed] [Google Scholar]
- 2.Silvola AS, Rusanen J, Tolvanen M, Pirttiniemi P, Lahti S. Occlusal characteristics and quality of life before and after treatment of severe malocclusion. Eur J Orthod. 2012;34:704–709. doi: 10.1093/ejo/cjr085. [DOI] [PubMed] [Google Scholar]
- 3.Abanto J, Tello G, Bonini GC, Oliveira LB, Murakami C, Bonecker M. Impact of traumatic dental injuries and malocclusions on quality of life of preschool children: a population-based study. Int J Paediatr Dent. 2014 doi: 10.1111/ipd.12092. [DOI] [PubMed] [Google Scholar]
- 4.Masood Y, Masood M, Zainul NN, Araby NB, Hussain SF, Newton T. Impact of malocclusion on oral health related quality of life in young people. Health Qual Life Outcomes. 2013;11:25. doi: 10.1186/1477-7525-11-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Masood M, Masood Y, Saub R, Newton JT. Need of minimal important difference for oral health-related quality of life measures. J Public Health Dent. 2014;74:13–20. doi: 10.1111/j.1752-7325.2012.00374.x. [DOI] [PubMed] [Google Scholar]
- 6.de Oliveira CM, Sheiham A. Orthodontic treatment and its impact on oral health-related quality of life in Brazilian adolescents. J Orthod. 2004;31:20–27. doi: 10.1179/146531204225011364. [DOI] [PubMed] [Google Scholar]
- 7.Burden DJ, Pine CM, Burnside G. Modified IOTN: an orthodontic treatment need index for use in oral health surveys. Community Dent Oral Epidemiol. 2001;29:220–225. doi: 10.1034/j.1600-0528.2001.290308.x. [DOI] [PubMed] [Google Scholar]
- 8.de Oliveira CM, Sheiham A. The relationship between normative orthodontic treatment need and oral health-related quality of life. Community Dent Oral Epidemiol. 2003;31:426–436. doi: 10.1046/j.1600-0528.2003.00002.x. [DOI] [PubMed] [Google Scholar]
- 9.Andiappan M, Gao W, Bernabé E, Kandala NB, Donaldson AN. Malocclusion, orthodontic treatment, and the Oral Health Impact Profile (OHIP-14) systematic review and meta-analysis. Angle Orthod. 2014 doi: 10.2319/051414-348.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu Z, McGrath C, Hägg U. Changes in oral health-related quality of life during fixed orthodontic appliance therapy: an 18-month prospective longitudinal study. Am J Orthod Dentofacial Orthop. 2011;139:214–219. doi: 10.1016/j.ajodo.2009.08.029. [DOI] [PubMed] [Google Scholar]
- 11.Chen M, Wang DW, Wu LP. Fixed orthodontic appliance therapy and its impact on oral health-related quality of life in Chinese patients. Angle Orthod. 2010;80:49–53. doi: 10.2319/010509-9.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xin WN, Ling JQ. Validation of a Chinese version of the oral health impact profile-14 [in Chinese] Zhonghua Kou Qiang Yi Xue Za Zhi. 2006;41:242–245. [PubMed] [Google Scholar]
- 13.Jarvinen S. Indexes for orthodontic treatment need. Am J Orthod Dentofacial Orthop. 2001;120:237–239. doi: 10.1067/mod.2001.114830. [DOI] [PubMed] [Google Scholar]
- 14.Gomes MC, Pinto-Sarmento TC, Costa EM, Martins CC, Granville-Garcia AF, Paiva SM. Impact of oral health conditions on the quality of life of preschool children and their families: a cross-sectional study. Health Qual Life Outcomes. 2014;12:55. doi: 10.1186/1477-7525-12-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bernabé E, Sheiham A, Tsakos G, Messias DOC. The impact of orthodontic treatment on the quality of life in adolescents: a case-control study. Eur J Orthod. 2008;30:515–520. doi: 10.1093/ejo/cjn026. [DOI] [PubMed] [Google Scholar]
- 16.Palomares NB, Celeste RK, Oliveira BH, Miguel JA. How does orthodontic treatment affect young adults' oral health-related quality of life. Am J Orthod Dentofacial Orthop. 2012;141:751–758. doi: 10.1016/j.ajodo.2012.01.015. [DOI] [PubMed] [Google Scholar]
- 17.Johal A, Alyaqoobi I, Patel R, Cox S. The impact of orthodontic treatment on quality of life and self-esteem in adult patients. Eur J Orthod. 2014 doi: 10.1093/ejo/cju047. [DOI] [PubMed] [Google Scholar]
- 18.Silvola AS, Varimo M, Tolvanen M, Rusanen J, Lahti S, Pirttiniemi P. Dental esthetics and quality of life in adults with severe malocclusion before and after treatment. Angle Orthod. 2014;84:594–599. doi: 10.2319/060213-417.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heravi F, Farzanegan F, Tabatabaee M, Sadeghi M. Do malocclusions affect the oral health-related quality of life. Oral Health Prev Dent. 2011;9:229–233. [PubMed] [Google Scholar]
- 20.Kolawole KA, Agbaje HO, Otuyemi OD. Impact of malocclusion on oral health related quality of life of final year dental students. Odontostomatol Trop. 2014;37:64–74. [PubMed] [Google Scholar]
- 21.O'Brien C, Benson PE, Marshman Z. Evaluation of a quality of life measure for children with malocclusion. J Orthod. 2007;34:185–193, 176. doi: 10.1179/146531207225022185. [DOI] [PubMed] [Google Scholar]
- 22.Feu D, de Oliveira BH, de Oliveira AM, Kiyak HA, Miguel JA. Oral health-related quality of life and orthodontic treatment seeking. Am J Orthod Dentofacial Orthop. 2010;138:152–159. doi: 10.1016/j.ajodo.2008.09.033. [DOI] [PubMed] [Google Scholar]
- 23.Feu D, Miguel JA, Celeste RK, Oliveira BH. Effect of orthodontic treatment on oral health-related quality of life. Angle Orthod. 2013;83:892–898. doi: 10.2319/100412-781.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Paula JD, Santos NC, da Silva ET, Nunes MF, Leles CR. Psychosocial impact of dental esthetics on quality of life in adolescents. Angle Orthod. 2009;79:1188–1193. doi: 10.2319/082608-452R.1. [DOI] [PubMed] [Google Scholar]
- 25.Hassan AH, Amin H. Association of orthodontic treatment needs and oral health-related quality of life in young adults. Am J Orthod Dentofacial Orthop. 2010;137:42–47. doi: 10.1016/j.ajodo.2008.02.024. [DOI] [PubMed] [Google Scholar]
- 26.Zhou YH, Hagg U, Rabie AB. Concerns and motivations of skeletal Class III patients receiving orthodontic-surgical correction. Int J Adult Orthodon Orthognath Surg. 2001;16:7–17. [PubMed] [Google Scholar]
- 27.Zhou Y, Hägg U, Rabie AB. Severity of dentofacial deformity, the motivations and the outcome of surgery in skeletal Class III patients. Chin Med J (Engl) 2002;115:1031–1034. [PubMed] [Google Scholar]
- 28.Seehra J, Fleming PS, Newton T, DiBiase AT. Bullying in orthodontic patients and its relationship to malocclusion, self-esteem and oral health-related quality of life. J Orthod. 2011;38:247–256, 294. doi: 10.1179/14653121141641. [DOI] [PubMed] [Google Scholar]
- 29.Zhang M, McGrath C, Hägg U. The impact of malocclusion and its treatment on quality of life: a literature review. Int J Paediatr Dent. 2006;16:381–387. doi: 10.1111/j.1365-263X.2006.00768.x. [DOI] [PubMed] [Google Scholar]
- 30.Tung AW, Kiyak HA. Psychological influences on the timing of orthodontic treatment. Am J Orthod Dentofacial Orthop. 1998;113:29–39. doi: 10.1016/S0889-5406(98)70274-4. [DOI] [PubMed] [Google Scholar]
- 31.Agou S, Locker D, Muirhead V, Tompson B, Streiner DL. Does psychological well-being influence oral-health-related quality of life reports in children receiving orthodontic treatment. Am J Orthod Dentofacial Orthop. 2011;139:369–377. doi: 10.1016/j.ajodo.2009.05.034. [DOI] [PubMed] [Google Scholar]
- 32.Liu Z, McGrath C, Hägg U. Associations between orthodontic treatment need and oral health-related quality of life among young adults: does it depend on how you assess them. Community Dent Oral Epidemiol. 2011;39:137–144. doi: 10.1111/j.1600-0528.2010.00573.x. [DOI] [PubMed] [Google Scholar]