Abstract
Objective:
To compare the initial failure rate (≤4 months) for extra-alveolar mandibular buccal shelf (MBS) miniscrews placed in movable mucosa (MM) or attached gingiva (AG).
Materials and Methods:
A total of 1680 consecutive stainless steel (SS) 2 × 12-mm MBS miniscrews were placed in 840 patients (405 males and 435 females; mean age, 16 ± 5 years). All screws were placed lateral to the alveolar process and buccal to the lower first and second molar roots. The screw heads were at least 5 mm superior to the soft tissue. Loads from 8 oz–14 oz (227 g–397 g, 231–405 cN) were used to retract the mandibular buccal segments for at least 4 months.
Results:
Overall, 121 miniscrews out of 1680 (7.2%) failed: 7.31% were in MM and 6.85% were in AG (statistically insignificant difference). Failures were unilateral in 89 patients and bilateral in 16. Left side (9.29%) failures was significantly greater (P < .001) compared with those on the right (5.12%). Average age for failure patients was 14 ± 3 years.
Conclusion:
MBS miniscrews were highly successful (approximately 93%), but there was no significant difference between placement in MM or AG. Failures were more common on the patient's left side and in younger adolescent patients. Having 16 patients with bilateral failures suggests that a small fraction of patients (1.9%) are predisposed to failure with this method.
Keywords: Mandibular buccal shelf, Miniscrews, Skeletal anchorage, Attached gingiva, Alveolar mucosa, Extra-alveolar orthodontic anchorage
INTRODUCTION
Skeletal anchorage is a broad-based experimental and clinical concept.1–7 Kanomi8 introduced surgical miniscrews for orthodontic anchorage, and more specific devices soon followed.9,10 Currently there is a large range of miniscrews varying in diameter from 1.0 mm–2.3 mm and in length from 4 mm–21 mm.11–19 Interradicular (I-R) miniscrews are the most common application, but they are often problematic in the posterior mandible.11,12,15,17–26 Miniscrews in the mandibular buccal shelf (MBS) are proposed as a reliable source of extra-alveolar (E-A) anchorage for retracting the entire mandibular arch to correct severe crowding, protrusion, and skeletal malocclusion, without extractions or orthognathic surgery.1,2
Success rates for I-R miniscrews range from 57%–95%, with a mean of approximately 84%.26–28 Failure is common in the posterior mandible, typically occurring in the first few weeks, so primary stability is the critical factor for clinical success.29–31 Attempts to improve primary stability include smaller diameter pilot holes,23 sites with increased cortical bone thickness and density,29–32 and a self-drilling protocol.33,34 Bone quality is particularly important for orthodontic miniscrews because they are retained by mechanical locking rather than osseointegration.35,36 Screw design studies show a >70% success rate for I-R miniscrews with a diameter of ≥1.2 mm, and multiple studies show success is directly related to screw length.17–21 However, increased screw size increases the probability of root damage,21 and a recent review suggests that cortical bone thickness may be the most important stability factor overall.20 Placement technique focuses on minimal root damage during screw placement. Park et al.15,17 suggested placing the screws at an obtuse angle to the bone surface to increase bone contact and lower the risk of root damage. Placing the devices in an E-A site like the MBS permits the use of larger-diameter screws that can be inserted parallel to the axial inclination of molars and not interfere with tooth roots.1,2
A pull-out study on both arches of dogs showed greater strength for miniscrews placed in the mandible30 but in human studies, maxillary sites were more successful than those in the mandible in all26,37–40 but one study.23 More recent research confirmed the maxilla as a superior site for miniscrews,12,17,24 but inadequate AG continues to be a concern.1,2 These results suggest there may be a problem if E-A miniscrews are inserted in MM, but soft tissue considerations have not been specifically addressed.41–44
The hypothesis tested is that MBS miniscrews are less successful short-term (<4 months) if they are placed in MM.
MATERIALS AND METHODS
MBS miniscrews were installed in a consecutive series of 840 patients (405 males, 435 females; age 16 ± 5 years), inserted in private practice by the same orthodontist (senior author) from 2009 to 2012. A total of 1680 SS miniscrews (2 × 12-mm, Newton's A, Hsinchu City, Taiwan) (Figure 1) were placed without flap elevation under local anesthesia (Figures 2 and 3); 1286 were in MM and 394 penetrated the AG (Figures 4 and 5). All miniscrews were placed as nearly parallel as possible to the mandibular first and second molar roots (extra-alveolar approach). The surgical procedure began with a sharp dental explorer sounding through the soft tissue to bone at the desired skeletal site (Figures 2 and 3). The most anatomically favorable site for the miniscrew is usually at or near the mucogingival junction (Figure 4). A self-drilling bone screw was inserted and screwed into the bone perpendicular to the occlusal plane (Figures 5 and 6).43–46 After installation, the screw head was at least 5 mm above the level of the soft tissue (Figure 5) and the endosseous portion had approximately 5 mm of bone engagement (contact) (Figure 6).46 All miniscrews were immediately loaded using prestretched elastomeric modules (power chains) to deliver a relatively uniform force.45–50 The mandibular retraction force varied from 8 oz–14 oz (227 g–397 g, 231–405 cN), being proportional to the perceived density of the bone when screwing in the miniscrew. The patients were instructed in oral hygiene procedures to control inflammation. The prestretched power chains47–49 were replaced every 4 weeks. The stability of the buccal shelf screws was tested at every appointment for 4 months. Percent failure data was tested by chi-square. The Indiana University Institutional Review Board approved the protocol, assigning the number 1408974880.
Figure 1.
A 2 × 12-mm stainless steel bone screw is designed to be inserted in the mandibular buccal shelf as a self-drilling fixture.
Figure 2.
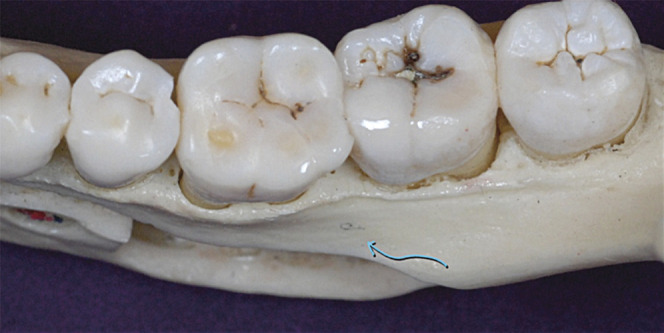
An occlusal view of a human mandible shows the available bone in the buccal shelf area (arrow).
Figure 3.
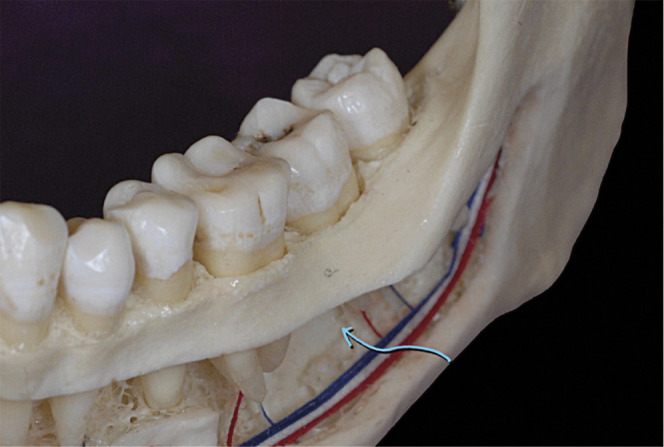
A lateral cutaway view of a human mandible shows the area of available bone (arrow) for placing a buccal shelf bone screw.
Figure 4.
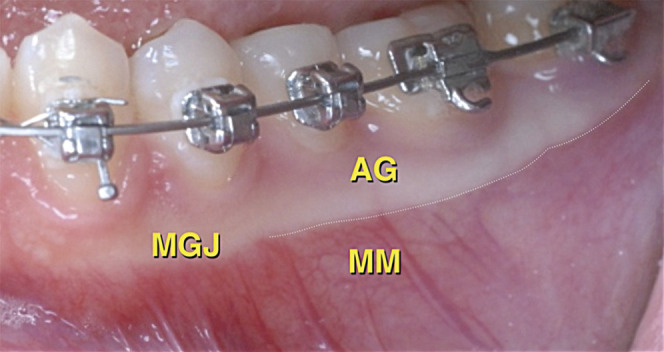
The mucogingival junction (MGJ) separates the attached gingiva (AG) from the movable mucosa (MM).
Figure 5.
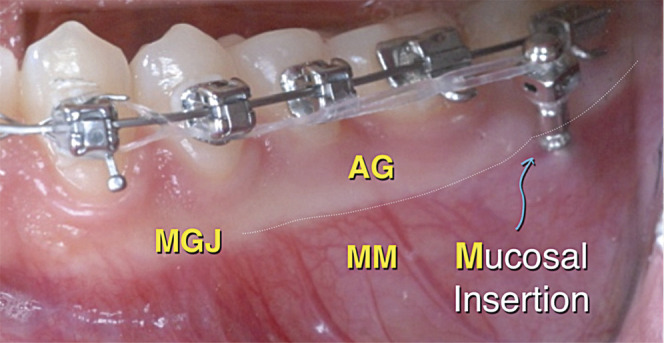
Screw insertion point may penetrate AG or MM but the head of the screw must be at least 5 mm above the level of the soft tissue.
Figure 6.
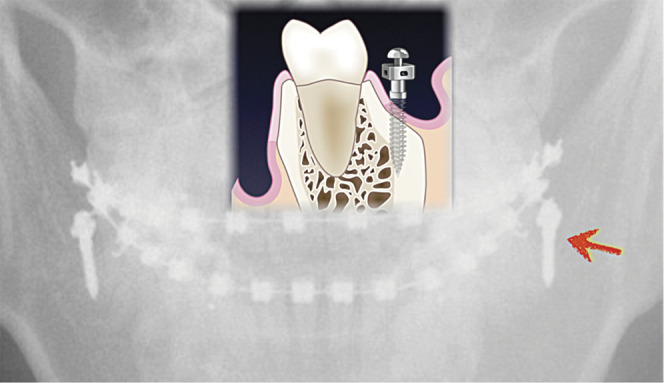
A drawing superimposed on a radiograph shows that a properly positioned screw is buccal to the molars roots.
RESULTS
Retrospective analysis of the 1680 miniscrews revealed that 1286 (76.5%) were placed in MM and 394 (23.5%) were in AG. Overall, 121 of 1680 (7.2%) miniscrews failed within 4 months, and the average time of failure was 3.3 months. In the MM group, 94 out of 1286 (7.31%) failed, and 27 out of 394 (6.85%) failed in AG (Figure 7). A chi-square test failed to show a statistical significance (P > .05) between the groups, so the hypothesis was rejected.
Figure 7.
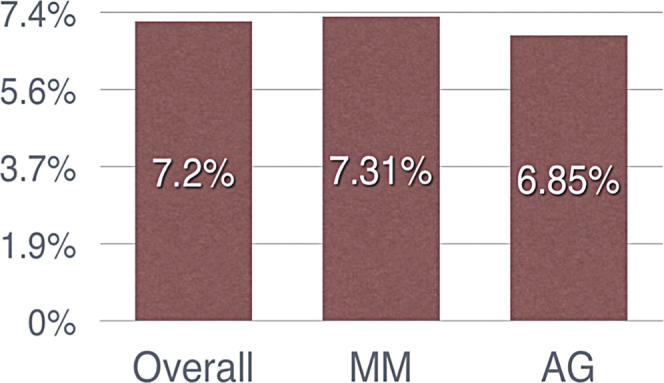
There was a slight tendency for more failures when screws were in MM rather than AG, but the difference was not statistically significant.
On the other hand, there were interesting failure relationships among other variables: age, side (right vs left), and predisposition. The average age of the 121 failure patients was 14 ± 3 years, which is considerably lower than the average age of all patients (16 ± 5 years). These data suggest that the failures were more common among the younger patients who tended to have less dense cortical bone in the MBS. Regarding side of patient, 78/121 (64.5%) of the failures were on the left side and 43/121 (35.5%) were on the right (Figure 8). Overall, the failure rate on the right (9.29%), compared with the left (5.12%) side, was statistically significant (P < .001). The 121 failed screws involved only 105 patients: 89 patients had single-screw failure and the other 16 lost screws on both sides. The bilateral failures suggest a predisposition to failure in a small portion of the patients (16/840 = 1.9%).
Figure 8.
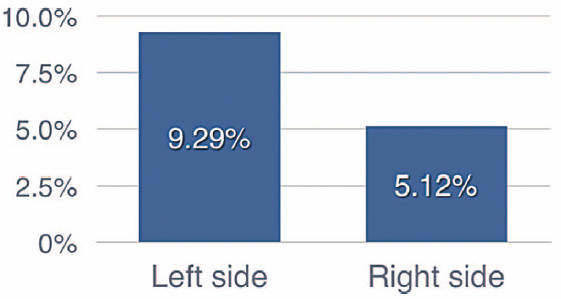
For the right-handed surgeon in this study, the failure rate for buccal shelf miniscrews was significantly greater (P < .001) on the patient's left than on the right.
DISCUSSION
Within the restraints of this study, placing MBS miniscrews in MM is an acceptable clinical procedure. The 4-month assessment interval was selected because all patients in the study required at least 4 months of mandibular buccal segment retraction. Additional study of the sample is indicated to determine the long-term failure rate relative to the anchorage needs of each patient.
Most studies of I-R miniscrews have shown a higher failure rate in the mandible (19.3%) than in the maxilla (12.0%).24,51,53 Furthermore, the physical stability of miniscrews tends to decrease for the first 3 weeks.31 With a primary failure rate of approximately 7%, MBS miniscrews are an attractive option for retraction of the mandibular buccal segments or the entire lower arch. Furthermore, the risk of root damage is remote when buccal shelf miniscrews are applied as described Figures 2–6.
Many patients have a minimal width of attached gingiva buccal to the molars, so >75% of optimally positioned buccal shelf screws penetrated MM.43 Attached gingiva can be moved to the buccal shelf site with an apically repositioned flap, but the present data suggest that the expense and discomfort associated with that additional surgical procedure is unnecessary. However, the elevated position of the screw head is probably an important factor in successfully maintaining the screws in MM, because oral hygiene is facilitated to control peri-screw inflammation.
The significant difference in primary failures on the left side (9.29%) vs the right (5.12%) reflects the technical sensitivity of the procedure and possibly other uncontrolled biological factors such as chewing and brushing habits. It is more difficult for a right-handed clinician to ideally position buccal shelf miniscrews on the opposite side. Additional refinement of the clinical technique is indicated to help control this variable.
Predisposition to MBS miniscrew failures is an important area for future research. Miniscrew studies of other sites have found no significant relationship between failure rate and age.11,16,17,21 However, in the current study, younger patients tended to have a higher failure rate, suggesting that a more mature skeleton may be advantageous for buccal shelf miniscrews.52 In addition, there were 16 patients who had bilateral failures, suggesting a predisposition to failure in some patients. This result is not surprising because “clustered failures” are well known both for dental implants53 and orthodontic miniscrews.54 A follow-up study of all failures in the sample is indicated to investigate predisposition based on patient age, genetic factors, and bone characteristics. Some patients may have an enhanced regional acceleratory phenomenon55 when bone is wounded with a miniscrew. This exaggerated hyperinflammatory response may be genetic, such as homozygosity for allele 2 of interleukins 1-beta, predisposing a patient to periodontitis.56
CONCLUSIONS
To provide optimal anchorage for retracting the mandibular arch, MBS miniscrews must be positioned precisely relative to tooth roots, soft tissue, and available bone.
Assuming adequate soft tissue clearance (approximately 5 mm), screws can be positioned in attached or movable mucosa.
Overall, the method is highly successful for most (93%) patients, but a small fraction of patients (1.9%) appears to be predisposed to failure.
ACKNOWLEDGMENT
This article is a research study presented to the Midwest Component of the Edward H. Angle Society of Orthodontists in partial fulfillment of the requirements for active membership.
REFERENCES
- 1.Chang C, Roberts WE. Orthodontics. Taipei: Yong Chieh; 2012. pp. 285–298. [Google Scholar]
- 2.Lin J, Liaw J, Chang C, Roberts WE. Orthodontics Class III Correction. Taipei: Yong Chieh; 2013. [Google Scholar]
- 3.Creekmore TD, Eklund MK. The possibility of skeletal anchorage. J Clin Orthod. 1983;17:266–269. [PubMed] [Google Scholar]
- 4.Roberts WE, Smith RK, Zilberman Y, Mozsary PG, Smith RS. Osseous adaptation to continuous loading of rigid endosseous implants. Am J Orthod. 1984;86:95–111. doi: 10.1016/0002-9416(84)90301-4. [DOI] [PubMed] [Google Scholar]
- 5.Roberts WE, Helm RF, Marshall JK, Gongloff RK. Rigid endosseous implants for orthodontic and orthopedic anchorage. Angle Orthod. 1989;59:247–256. doi: 10.1043/0003-3219(1989)059<0247:REIFOA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Roberts WE, Marshall KJ, Mozsary PG. Rigid endosseous implant utilized as anchorage to protract molars and close an atrophic extraction site. Angle Orthod. 1990;60:135–152. doi: 10.1043/0003-3219(1990)060<0135:REIUAA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Lee KJ, Park YC, Hwang CJ, et al. Displacement pattern of the maxillary arch depending on miniscrew position in sliding mechanics. Am J Orthod Dentofacial Orthop. 2011;140:224–232. doi: 10.1016/j.ajodo.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 8.Kanomi R. Mini-implant for orthodontic anchorage. J Clin Orthod. 1997;31:763–767. [PubMed] [Google Scholar]
- 9.Costa A, Raffainl M, Melsen B. Miniscrews as orthodontic anchorage: a preliminary report. Int J Adult Orthod Orthognath Surg. 1998;13:201–209. [PubMed] [Google Scholar]
- 10.Bechtold TE, Kim JW, Choi TH, Park YC, Lee KJ. Distalization pattern of the maxillary arch depending on the number of orthodontic miniscrews. Angle Orthod. 2013;83:266–273. doi: 10.2319/032212-123.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miyawaki S, Koyama I, Inoue M, Mishima K, Sugahara T, Takano-Yamamoto T. Factors associated with the stability of titanium screws placed in the posterior region for orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2003;124:373–378. doi: 10.1016/s0889-5406(03)00565-1. [DOI] [PubMed] [Google Scholar]
- 12.Cheng SJ, Tseng IY, Lee JJ, Kok SH. A prospective study of the risk factors associated with failure of mini implants used for orthodontic anchorage. Int J Oral Maxillofac Implants. 2004;19:100–106. [PubMed] [Google Scholar]
- 13.Liou EJ, Pai BC, Lin JC. Do miniscrews remain stationary under orthodontic forces. Am J Orthod Dentofacial Orthop. 2004;126:42–47. doi: 10.1016/j.ajodo.2003.06.018. [DOI] [PubMed] [Google Scholar]
- 14.Fritz U, Ehmer A, Diedrich P. Clinical suitability of titanium microscrews for orthodontic anchorage—preliminary experiences. J Orofac Orthop. 2004;65:410–418. doi: 10.1007/s00056-004-0408-x. [DOI] [PubMed] [Google Scholar]
- 15.Park HS, Lee SK, Kwon OW. Group distal movement of teeth using microscrew implant anchorage. Angle Orthod. 2005;75:602–609. doi: 10.1043/0003-3219(2005)75[602:GDMOTU]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 16.Motoyoshi M, Hirabayashi M, Uemura M, Shimizu N. Recommended placement torque when tightening an orthodontic mini-implant. Clin Oral Implants Res. 2006;17:109–114. doi: 10.1111/j.1600-0501.2005.01211.x. [DOI] [PubMed] [Google Scholar]
- 17.Park HS, Jeong SH, Kwon OW. Factors affecting the clinical success of screw implants used as orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2006;130:18–25. doi: 10.1016/j.ajodo.2004.11.032. [DOI] [PubMed] [Google Scholar]
- 18.Chen CH, Chang CS, Hsieh CH, Tseng YC, Shen YS, Huang IY, et al. The use of microimplants in orthodontic anchorage. J Oral Maxillofac Surg. 2006;64:1209–1213. doi: 10.1016/j.joms.2006.04.016. [DOI] [PubMed] [Google Scholar]
- 19.Tseng YC, Hsieh CH, Chen CH, Shen YS, Huang IY, Chen CM. The application of mini-implants for orthodontic anchorage. Int J Oral Maxillofac Surg. 2006;35:704–707. doi: 10.1016/j.ijom.2006.02.018. [DOI] [PubMed] [Google Scholar]
- 20.Marquezan M, Mattos CT, Sant'Anna EF, de Souza MM, Maia LC. Does cortical thickness influence the primary stability of miniscrews? A systematic review and meta-analysis. Angle Orthod. 2014;84(6):1093–1103. doi: 10.2319/093013-716.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kuroda S, Sugawara Y, Deguchi T, Kyung HM, Takano-Yamamoto T. Clinical use of miniscrew implants as orthodontic anchorage: success rates and postoperative discomfort. Am J Orthod Dentofacial Orthop. 2007;131:9–15. doi: 10.1016/j.ajodo.2005.02.032. [DOI] [PubMed] [Google Scholar]
- 22.Wiechmann D, Meyer U, Buchter A. Success rate of mini-and micro-implants used for orthodontic anchorage: a prospective clinical study. Clin Oral Implants Res. 2007;18:263–267. doi: 10.1111/j.1600-0501.2006.01325.x. [DOI] [PubMed] [Google Scholar]
- 23.Motoyoshi M, Matsuoka M, Shimizu N. Application of orthodontic mini-implants in adolescents. Int J Oral Maxillofac Surg. 2007;36:695–699. doi: 10.1016/j.ijom.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 24.Chen YJ, Chang HH, Huang CY, Hung HC, Lai EHH, Yao CCJ. A retrospective analysis of the failure rate of three different orthodontic skeletal anchorage systems. Clin Oral Implants Res. 2007;18:768–775. doi: 10.1111/j.1600-0501.2007.01405.x. [DOI] [PubMed] [Google Scholar]
- 25.Keim RG. Answering the questions about mini-screws. J Clin Orthod. 2005;39:7–9. [PubMed] [Google Scholar]
- 26.Berens A, Wiechmann D, Dempf R. Mini- and micro-screws for temporary skeletal anchorage in orthodontic therapy. J Orofac Orthop. 2006;67:450–458. doi: 10.1007/s00056-006-0601-1. [DOI] [PubMed] [Google Scholar]
- 27.Viwattanatipa N, Thanakitcharu S, Uttraravichien A, Pitiphat W. Survival analyses of surgical miniscrews as orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2009;136:29–36. doi: 10.1016/j.ajodo.2007.06.018. [DOI] [PubMed] [Google Scholar]
- 28.Schatzle M, Mannchen R, Zwahlen M, Lang NP. Survival and failure rates of orthodontic temporary anchorage devices: a systemic review. Clin Oral Implants Res. 2009;20:1351–1359. doi: 10.1111/j.1600-0501.2009.01754.x. [DOI] [PubMed] [Google Scholar]
- 29.Wilmes B, Rademacher C, Olthoff G, Drescher D. Parameters affecting primary stability of orthodontic mini-implants. J Orofac Orthop. 2006;67:162–174. doi: 10.1007/s00056-006-0611-z. [DOI] [PubMed] [Google Scholar]
- 30.Huja SS, Litsky AS, Beck FM, Johnson KA, Larsen PE. Pull-out strength of monocortical screws placed in the maxillae and mandibles of dogs. Am J Orthod Dentofacial Orthop. 2005;127:307–313. doi: 10.1016/j.ajodo.2003.12.023. [DOI] [PubMed] [Google Scholar]
- 31.Ure DS, Oliver DR, Kim KB, Melo AC, Buchang PH. Stability changes of miniscrew implants over time: a pilot resonance frequency analysis. Angle Orthod. 2011;81:994–1000. doi: 10.2319/120810-711.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shank SB, Beck FM, D'Atri AM, Huja SS. Bone damage associated with orthodontic placement of miniscrew implants in an animal model. Am J Orthod Dentofacial Orthop. 2012;141:412–418. doi: 10.1016/j.ajodo.2011.10.021. [DOI] [PubMed] [Google Scholar]
- 33.Florvaag B, Kneuertz P, Lazar F, Koebke J, Zoller JE, Braumann B, et al. Biomechanical properties of orthodontic mini-screws: an in-vitro study. J Orofac Orthop. 2010;71:53–67. doi: 10.1007/s00056-010-9933-y. [DOI] [PubMed] [Google Scholar]
- 34.Chen Y, Shin HI, Kyung HM. Biomechanical and histological comparison of self-drilling and self-tapping orthodontic micro-implants in dogs. Am J Orthod Dentofacial Orthop. 2008;133:44–50. doi: 10.1016/j.ajodo.2007.01.023. [DOI] [PubMed] [Google Scholar]
- 35.Crismani AG, Bertl MH, Celar AG, Bantleon HP, Burstone CJ. Miniscrews in orthodontic treatment: review and analysis of published clinical trials. Am J Orthod Dentofacial Orthop. 2010;137:108–113. doi: 10.1016/j.ajodo.2008.01.027. [DOI] [PubMed] [Google Scholar]
- 36.Chung KR, Kim SH, Choo HR, Kook YA, Cope JB. Distalization of the mandibular dentition with mini-implants to correct a Class III malocclusion with a midline deviation. Am J Orthod Dentofacial Orthod. 2010;137:135–146. doi: 10.1016/j.ajodo.2007.06.023. [DOI] [PubMed] [Google Scholar]
- 37.Cha JK, Kil JK, Yoon TM, Hwang CJ. Mini-screw stability evaluated with computerized tomography scanning. Am J Orthod Dentofacial Orthop. 2010;137:73–79. doi: 10.1016/j.ajodo.2008.03.024. [DOI] [PubMed] [Google Scholar]
- 38.Tseng YC, Hsieh CH, Chen CH, Shen YS, Huang IY, Chen CM. The application of mini-implants for orthodontic anchorage. Int J Oral Maxillofac Surg. 2006;35:704–707. doi: 10.1016/j.ijom.2006.02.018. [DOI] [PubMed] [Google Scholar]
- 39.Wiechmann D, Meyer U, Buchter A. Success rate of mini- and micro-implants used for orthodontic anchorage: a prospective clinical study. Clin Oral Implants Res. 2007;18:263–267. doi: 10.1111/j.1600-0501.2006.01325.x. [DOI] [PubMed] [Google Scholar]
- 40.Chen YJ, Chang HH, Lin HY, Lai EH, Hung HC, Yao CC. Stability of miniplates and miniscrews used for orthodontic anchorage: experience with 492 temporary anchorage devices. Clin Oral Impl Res. 2008;19:1188–1196. doi: 10.1111/j.1600-0501.2008.01571.x. [DOI] [PubMed] [Google Scholar]
- 41.Lim HJ, Eun CS, Cho JH, Lee KH, Hwang HS. Factors associated with initial stability of miniscrews for orthodontic treatment. Am J Orthod Dentofacial Orthop. 2009;136:236–242. doi: 10.1016/j.ajodo.2007.07.030. [DOI] [PubMed] [Google Scholar]
- 42.Hsu YL, Chang C, Roberts WE. The 12 applications of OrthoBoneScrew on impacted teeth. Int J Orthod Implantol. 2011;23:34–49. [Google Scholar]
- 43.Chang C. Clinical applications of Orthodontic Bone Screw in Beethoven Orthodontic Center. Int J Orthod Implantol. 2011;23:50–51. [Google Scholar]
- 44.Huang S, Chang C, Roberts WE. A severe skeletal Class III open bite malocclusion treated with non-surgical approach. Int J Orthod Implantol. 2011;24:28–39. [Google Scholar]
- 45.Su B, Chang C, Roberts WE. Conservative management of a severe Class III open bite malocclusion. Int J Orthod Implantol. 2013;30:40–60. [Google Scholar]
- 46.Chang C, Roberts WE. Analysis of cortical bone engagement by using CBCT: a retrospective study of the extra-alveolar miniscrew insertion on buccal shelves. Int J Orthod Implantol. 2015 (in press) [Google Scholar]
- 47.Ash JL, Nikolai RJ. Relaxation of orthodontic elastomeric chains and modules in vitro and in vivo. J Dent Res. 1978;57:685–690. doi: 10.1177/00220345780570050301. [DOI] [PubMed] [Google Scholar]
- 48.Baty DL, Storie DJ, von Fraunhofer JA. Synthetic elastomeric chains: a literature review. Am J Orthod Dentofacial Orthop. 1994;105:536–542. doi: 10.1016/S0889-5406(94)70137-7. [DOI] [PubMed] [Google Scholar]
- 49.Kin KH, Chung CH, Choy K, Lee JS, Vanarsdall RL. Effects of prestrectching on force degradation of synthetic elastomeric chains. Am J Orthod Dentofacial Orthop. 2005;128:477–482. doi: 10.1016/j.ajodo.2004.04.027. [DOI] [PubMed] [Google Scholar]
- 50.Manni A, Cozzani M, Tamborrino F, Rinaldis S, Menini A. Factors influencing the stability of miniscrews: a retrospective study on 300 miniscrews. Eur J Orthod. 2010;33:388–395. doi: 10.1093/ejo/cjq090. [DOI] [PubMed] [Google Scholar]
- 51.Moon CH, Lee DG, Lee HS, Im JS, Baek SH. Factors associated with the success rate of orthodontic miniscrews placed in the upper and lower posterior buccal region. Angle Orthod. 2008;78:101–106. doi: 10.2319/121706-515.1. [DOI] [PubMed] [Google Scholar]
- 52.Hsu YL, Chang C, Roberts WE. Early intervention of Class III malocclusion and impacted cuspids in late mixed dentition. Int J Orthod Implantol. 2013;28:66–79. [Google Scholar]
- 53.Ekfeldt A, Christiansson U, Eriksson, et al. A retrospective analysis of factors associated with multiple implant failures in the maxilla. Clin Oral Implants Res. 2001;12:462–467. doi: 10.1034/j.1600-0501.2001.120505.x. [DOI] [PubMed] [Google Scholar]
- 54.Melsen B, Graham J, Baccetti T, et al. Factors contributing to the success or failure of skeletal anchorage devices, an informal JCO survey. J Clin Orthod. 2010;44:714–718. [PubMed] [Google Scholar]
- 55.Frost HM. The biology of fracture healing: an overview for clinicians. Part II. Clin Orthop Relat Res. 1989;248:294–309. [PubMed] [Google Scholar]
- 56.Ianni M, Bruzzesi G, Pugliese D, Porcellini E, Carbone I, Schiavone A, Licastro F. Variations in inflammatory genes are associated with periodontitis. Immun Ageing. 2013;10(1):10–39. doi: 10.1186/1742-4933-10-39. [DOI] [PMC free article] [PubMed] [Google Scholar]



