Abstract
Objective:
To evaluate skeletal and dental changes after intrusion of the maxillary molars in subjects with anterior open bite.
Materials and Methods:
This retrospective cephalometric study evaluated skeletal and dental changes resulting from the use of maxillary orthodontic mini-implants in 31 consecutively treated patients. Radiographs were taken at the start and end of maxillary molar intrusion to evaluate the associated changes. Statistical analysis was performed using a one-sample t-test.
Results:
The mean treatment observation time was 1.31 years (SD = 2.03). The maxillary first molars (P = 0.0026) and second molars (P = 0.039) were intruded. However, the mandibular first molars (P = 0.0004) and second molars (P = 0.003) erupted in adolescent patients. Both the maxillary and mandibular first molars inclined distally (P = 0.025 and P = 0.044, respectively). The mandibular plane angle decreased (P = 0.036), lower facial height decreased (P = 0.002), and the occlusal plane angle increased (P = 0.009). The overbite increased (P < .0001). The ANB angle decreased (P < .0001). Mandibular dental and skeletal changes were more apparent in adolescents, while adults tended toward maxillary changes.
Conclusions:
Vertical traction from orthodontic mini-implants reduces the maxillary posterior dentoalveolar height, thereby assisting orthodontic closure of anterior open bite. However, simultaneous eruption or extrusion of the mandibular molars should be controlled. Adolescent patients tend to demonstrate more favorable effects of mandibular autorotation than do adults.
Keywords: Mini-implant, Anterior open bite, Molar intrusion
INTRODUCTION
Anterior open bite (AOB) is widely regarded as one of the more difficult malocclusions to correct, especially when associated with an increased maxillomandibular plane angle (MMPA). Full correction often requires a maxillary impaction osteotomy to indirectly reduce the MMPA and lower anterior face height (LAFH). However, it is possible to successfully correct AOB with the adjunctive use of temporary skeletal anchorage.1–8
It has been suggested that palatal alveolar mini-implants, coupled with a customized rigid transpalatal arch provides optimal chances for mini-implant stability and molar intrusion, especially in patients with high-arched palates.9,10
Several studies have investigated the total effects of molar intrusion, but the results have included additional mandibular molar intrusion and vertical maxillary and mandibular molar (occlusal) settling following both the intrusion phase and treatment completion.1,2,8,11 As a result, the principal maxillary molar movements and any associated mandibular changes may be difficult to discern. In addition, there has not been an analysis of age effects (growing vs nongrowing cases) in the literature. Therefore, this study aimed to analyze the dental and skeletal effects of maxillary molar intrusion using orthodontic mini-implants at the end of the intrusion phase in both adolescent and adult patients.
MATERIALS AND METHODS
The Research Subjects Review Board of the University of Rochester approved this study. The records of 31 consecutively treated cases were collected retrospectively for the study. Patient ages ranged from 11.6 years to 55.5 years (mean, 20.7 years). Twenty-one patients were female and 10 were male.
Inclusion criteria were as follows:
Pretreatment AOB
Maxillary molars had been intruded with mini-implant traction as the principal treatment for AOB
Exclusion criteria were as follows:
previous digit-sucking habit within 2 years prior to treatment,
bite-closing biomechanics such as multiloop edgewise archwire and/or intermaxillary elastic traction used,
orthodontic space closure in the maxillary arch during intrusion phase,
orthognathic or TMJ surgery during intrusion phase.
Variations in individual growth patterns, fixed appliance prescription, and Angle's molar classification were not considered criteria for exclusion. Nor were type, commercial brand, and exact locations of the mini-implants considered within these criteria.
Twenty-five of the patients (group A) were treated by a single orthodontist (R.C.) using a standardized method that gained anchorage from bilateral perimolar orthodontic mini-implants.9,10 Infinitas mini-implants (DB Orthodontics Ltd, UK; www.infinitas-miniimplant.com) with a 1.5-mm diameter and 9-mm body length were used in all cases. For 19 of the 25 patients, a single mini-implant was inserted in bilateral palatal alveolar sites between the first and second molars. For one adult patient, they were inserted mesial to the first molar because of limited intraoral access caused by trismus. Insertion sites mesial to the first molars were utilized in the remaining five adolescent patients because of incomplete eruption of the second molars. Only one of these five patients had the mini-implants on the buccal side of the alveolus.
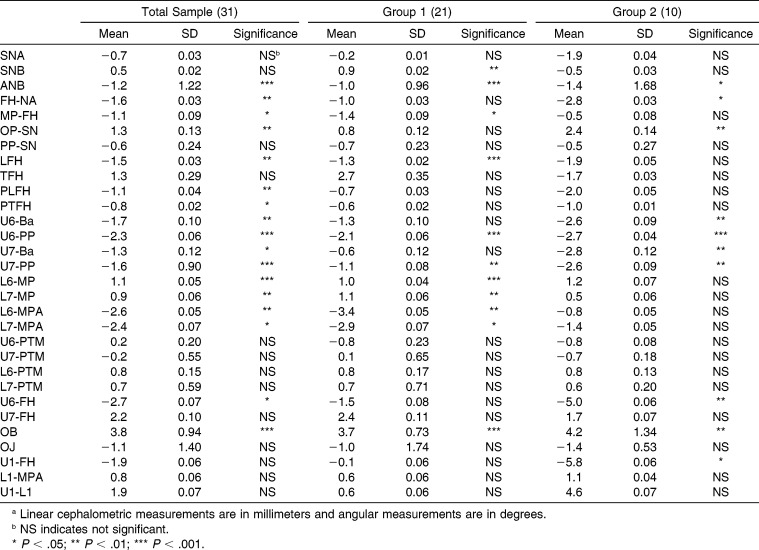
Either a modified transpalatal arch or quad helix expansion appliance was fitted on the maxillary first molars during the intrusion phase in order to maintain or increase intermolar width (Figure 1).9,10
Figure 1.
Elastomeric traction applied from bilateral palatal (alveolar) mini-implants to a quad helix appliance. The maxillary second molars have been bonded as part of bilateral sectional fixed appliances.
The remaining six patients (group B) were treated by a different orthodontist using a method that gained anchorage from a single, midpalatal mini-implant. One Tomas mini-implant (Dentaurum GmbH & Co KG, Ispringen, Germany; www.dentaurum.de) with a 1.5-mm diameter and 6-mm body length was used in all cases. The mini-implant was placed near the midpalatal raphe under local anesthesia and was attached to a dumbbell-type transpalatal arch (Rocky Mountain Orthodontics, Denver, Colo; www.rmortho.com). Traction was applied with elastomeric chain from the dumbbell to lingual buttons on the maxillary first and second molars (Figure 2).
Figure 2.

Elastomeric traction applied from a single midpalatal mini-implant with a dumbbell attachment to a transpalatal arch and second molars.
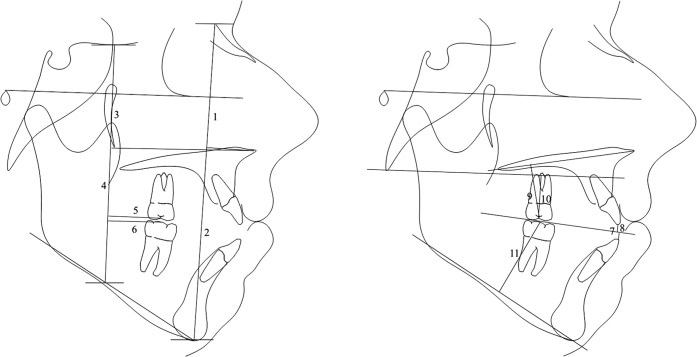
Two lateral cephalometric radiographs were collected for each patient. One radiograph was taken before intrusion, and one was taken after the end of the intrusion phase or full treatment. The lateral cephalometric radiographs were calibrated to actual size using Dolphin software and traced manually. They were then measured independently three times by one investigator to minimize any errors. Twelve of the measurements were derived from conventional cephalometric analyses. The other 18 were linear and angular measurements and were related to horizontal and vertical reference lines (Figures 3, 4). The basion horizontal plane, which is parallel to FH and palatal plane were used to evaluate vertical changes. Decreasing vertical values represent superior dental movements. The reference line to assess horizontal changes was constructed perpendicular to Frankfort horizontal (FH), intersecting the anterior curvature of the pterygomaxillary fissure (PTM). This was used because of the horizontal stability of the PTM during growth.12 An increase in horizontal values represents anterior movement.
Figure 3.
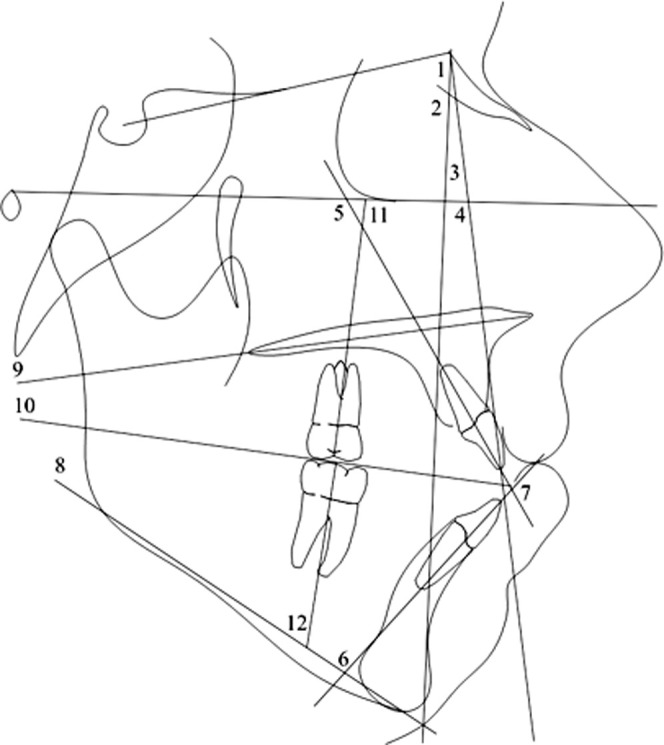
Angular cephalometric measurements (degrees): 1 = SNA, 2 = SNB, 3 = ANB, 4 = FH-NA, 5 = U1-FH, 6 = L1-MP, 7 = U1-L1, 8 = MP-FH, 9 = PP-SN, 10 = OP-SN, 11 = U6-FH, 12 = L6-MP. Not shown: U7-FH, L7-MP.
Figure 4.
Linear cephalometric measurements (mm): 1 = LFH (ANS-Me), 2 = TFH (N-Me), 3 = PLFH (ANS-MP), 4 = PTFH (SES-MP), 5 = U6-PTM, 6 = L6-PTM, 7 = OB, 8 = OJ, 9 = U6-PP, 10 = U6-Ba, 11 = L6-MP. Not shown: U7-PTM, L7-PTM, U7-PP, U7-Ba, L7-MP.
All statistical analyses were conducted using Version 9.3 of the SAS System for Windows (SAS Institute Inc, Cary, NC). One sample statistical t-test was used to evaluate whether any of the changes were significantly different in terms of both the whole sample and for two age subgroups. Twenty-one of the patients (group 1) were age 18 years or less before treatment was initiated, and were compared with 10 patients (Group 2) age 19 years or more. The estimated mean differences and associated 95% confidence intervals were calculated. Pearson correlation coefficients were calculated relative to cephalometric changes and chronological age. Intrarater reliability was calculated from the three sets of cephalometric measurements.
RESULTS
Intrarater reliability was 98.2% for all measurements.
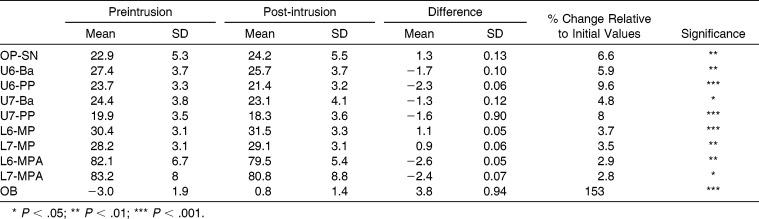
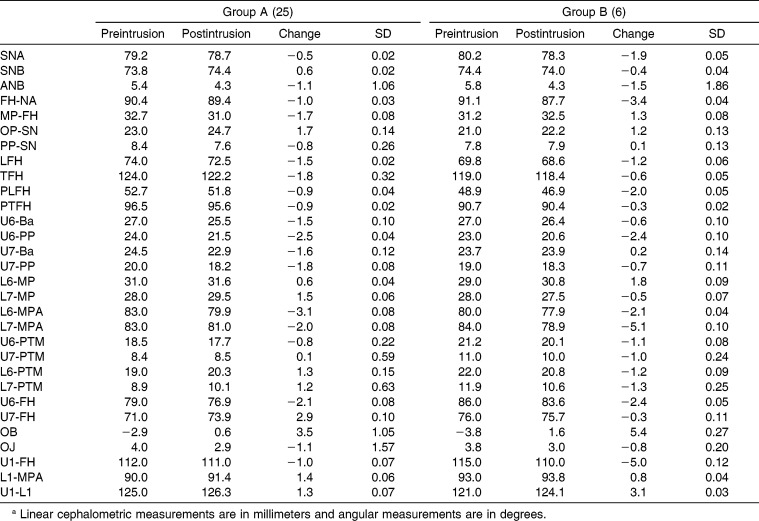
Vertical Dental Changes (Table 1)
Table 1.
Preintrusion and Postintrusion Vertical Dental Measurements (mm)
The maxillary first and second molars were intruded in 90% (28/31) and 74% (23/31) of the cases, respectively. The average intrusion relative to the palatal plane was 2.3 mm for the first molars and 1.6 mm for the second molars. The vertical molar changes ranged from −5 mm to 1 mm for the first molars and −5 mm to 2.5 mm for the second molars.
The mandibular first and second molars erupted in 77% (24/31) and 65% (20/31) of the cases, respectively. The average increase in distance from the mandibular plane was 1.1 mm for the first molars and 0.9 mm for the second molars. The changes ranged from −2 mm to 6 mm for both the first and second molars.
The vertical incisor relationship, as represented by the overbite (OB), improved in 97% (30/31) of the cases. The average amount of bite closure was 3.9 mm, with a range of 0 mm to 8.5 mm. The vertical incisor changes are not reported separately since they were also influenced by orthodontic alignment.
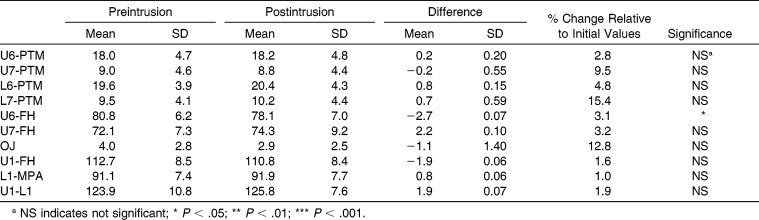
Horizontal Dental Changes (Table 2)
Table 2.
Preintrusion and Postintrusion Horizontal Dental Measurements (mm)
The overjet (OJ) decreased in 65% (20/31) of the cases. The average amount of OJ reduction was 1.1 mm, with a range of −3 mm to 6 mm. Changes in OJ were not statistically significant.
The maxillary and mandibular first molars demonstrated more anteroposterior tipping than did the second molars. The maxillary first molars tipped distally in 74% (23/31) of the cases, by an average of 2.6°, with a range from −15° to 16°. The mandibular first molars tipped distally in 58% (18/31) of the cases by an average of 2.5°, with a range from −6° to 11°.
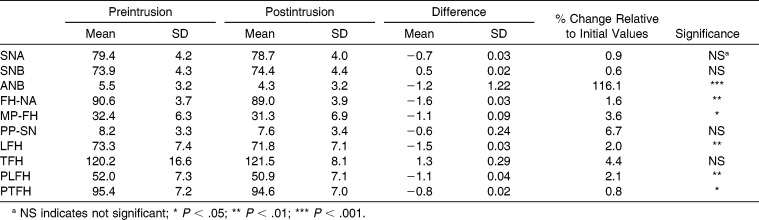
Skeletal Changes (Table 3)
Table 3.
Preintrusion and Postintrusion Skeletal Measurements (°)
SNA decreased in 55% (17/31) of the cases by an average of 0.7°, with a range from −10.5° to 3°. SNB increased in 58% (18/31) of the cases by an average of 0.5°, with a range from 4° to −6.5°. ANB decreased in 81% (25/31) of the cases by an average of 1.2°, with a range from −4° to 1°. Lande's Angle (FH-NA) decreased in 68% (21/31) of the cases by an average of 1.5°, with a range from −11° to 3°.
Both anterior and posterior facial height decreased. Lower anterior facial height (ANS-Me) decreased in 71% (22/31) of the cases by an average of 1.5 mm, with a range from −7 mm to 6 mm. Total facial height (Na-Me) decreased in 74% (23/31) of the cases by an average of 1.4 mm, with a range from −6 mm to 7 mm. Posterior lower facial height (ANS-MP) decreased in 55% (17/31) of the cases by an average of 1.2 mm, with a range from −7 mm to 3 mm. Posterior total facial height (SES-MP) decreased in 55% (17/31) of the cases by an average of 0.7 mm, with a range from −6 mm to 4 mm.
The mandibular plane angle (MP-FH) decreased in 61% (19/31) of the cases by an average of 1.1°, with a range from −7° to 5.5°. Inclination of the occlusal plane (OP) increased in 58% (18/31) of the cases by an average of 1.3°, with a range from −4° to 6°.
Age-Related Changes (Table 4)
Table 4.
Treatment Changes According to Age Subgroups: Group 1 (≤18 y); Group 2 (≥19)a
Chronological age was negatively correlated with OB (r = −0.51, P = 0.0047) and SNB (r = −0.36, P = 0.046) changes but positively correlated with OP-SN (r = 0.38, P = 0.0336) changes. In group 1 (patients ≤ 18 years of age) the OB increased in 100% (21/21) of the cases by an average of 3.7 mm, with a range from 0.5 mm to 8.5 mm. SNB increased in 67% (14/21) of the cases by an average of 0.9°, with a range from −1° to 4°. ANB decreased in 81% (17/21) of the cases by an average of 1.0°, with a range from −3° to 0.5°. MP-FH decreased in 62% (13/21) of the cases by an average of 1.5°, with a range from −7° to 3°. TFH decreased in 67% (14/21) of the cases by an average of 1.3 mm, with a range from −6 mm to 1 mm.
Maxillary first and second molars intruded in 86% (18/21) and 71% (15/21) of the cases, respectively. The average intrusion was 2.1 mm for the first molars and 1.1 mm for the second molars. Vertical molar changes ranged from −5 mm to 1 mm and −3 mm to 2.5 mm, respectively. The mandibular first and second molars moved superiorly (erupted) in 86% (18/21) and 62% (13/21) of the cases, respectively. The average vertical movement was 1.1 mm for both first and second molars. The ranges varied from −2 mm to 4 mm and −1 mm to 6 mm, respectively. They also tipped distally in 67% (14/21) and 62% (13/21) of the cases, respectively. The average amount of tipping was 3.4° and 2.7°, and the ranges varied from −6° to 11° and −7° to 21°, respectively.
Results for group 2 (patients ≥ 19 years of age) showed that the OB increased in 90% (9/10) of the cases by an average of 4.3 mm, with a range from 0 mm to 8 mm. SNA decreased by 1.9° and SNB was reduced by 0.4°, causing a reduction of ANB in 80% (8/10) of the cases by an average of 1.5°, with a range from −4° to 1°. FH-NA decreased in 90% (9/10) of the cases by an average of 2.7°, with a range from 0° to 11°. OP inclination increased in 80% (8/10) of the cases by an average of 2.4°, with a range of −2° to 5°. Lower facial height (LFH) was reduced by 1.9 mm. Maxillary first and second molars intruded in 100% (10/10) and 80% (8/10) of the cases, respectively. The average intrusion was 2.7 mm for the first molars and 2.6 mm for the second molars. Vertical molar movements ranged from −1 mm to −4.5 mm and −6 mm to 2 mm, respectively. The maxillary first molars tipped distally in 80% (8/10) of the cases by an average of 4.8°, with a range from −3° to 13°. The maxillary incisors retroclined in 70% (7/10) of the cases by an average of 5.7°, with a range from −5° to 14°.
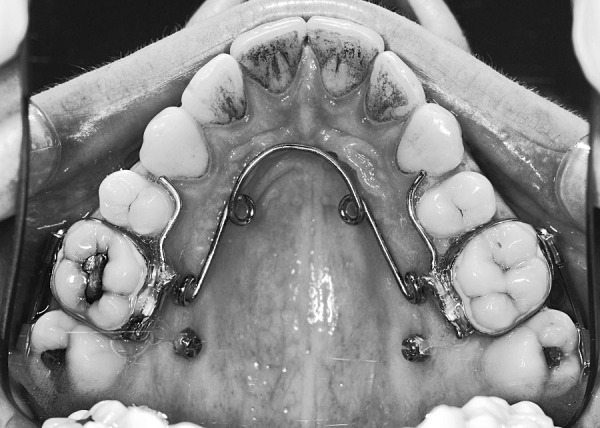
DISCUSSION
The retrospective sample studied here was heterogeneous in terms of patient age, severity of AOB, incisor relationship and inclinations, and treatment biomechanics. There are inherent weaknesses in retrospective studies, and these factors probably account for the wide ranges in cephalometric changes (Table 5). For example, while the mean maxillary first molar intrusion was 2.3 mm, the maximum achieved was 5 mm, to the extent that some of these patients had vertical molar changes such as expected only with orthognathic surgery. The mean molar intrusion and AOB correction demonstrated here is similar to those of other studies of adult subjects.1,2,6,8,13
Table 5.
Treatment Changes Relative to Mini-Implant Biomechanicsa
As in previous studies,1,2,8,11 mandibular plane angulation, OB, and maxillary first molar height (relative to the palatal plane) all demonstrated significant changes after molar intrusion. These published studies also demonstrated decreases in skeletal Class II features, as represented by the ANB angle, except that of Deguchi et al.2 Total facial height (TFH), LFH, and mandibular first molar height reductions were also significant in the current study, in agreement with the study by Xun et al.11 It seems that a combination of changes causes the overall clinical changes of relevance, especially the increase in OB, reduction in the Class II relationship, and long-face features.
In the current study, both the maxillary and mandibular molars moved in an anterosuperior direction parallel to the PTM line. They also demonstrated distal tipping. This may be explained by a posterosuperior direction of traction on the maxillary first molar in many of these patients (where the mini-implants were inserted distal to that tooth). The statistically insignificant results of the changes in OJ were initially surprising compared with findings in other studies.2,11 As the mandible moves anteriorly and superiorly with closure of the AOB, it appears logical that the OJ would decrease. However, such decrease was demonstrated in only 65% of the cases. This lack of significance is possibly due to considerable variations (large standard deviations) in pretreatment incisal inclination and whether the incisors were aligned during the observation period. In particular, those patients with full fixed appliances for alignment of a Class II division 2 incisor relationship would tend toward a reduction in OB at the same time that molar intrusion was causing an OB increase.
Chronological age was not a consideration in the exclusion criteria, and our results suggest that the relative effects of molar intrusion may differ according to whether the patient is growing. Buschang et al. (2011)5 reported a pilot study of nine adolescent patients, but ours is the first paper to report both skeletal and dental changes resulting from molar intrusion in adolescent patients.
Treatment at an earlier chronological age, coincident with adolescent growth, showed statistically significant correlations with the changes in OB, OP-SN, and SNB. Adult patients (group 2) demonstrated greater dental changes in terms of maxillary molar intrusion and OB closure. This was associated with greater steepening of the occlusal plane and a tendency to more reduction in SNA and less anterior displacement of the mandible (SNB increase) than in the adolescents (group 1) (Table 4). In contrast, the adolescent group had more favorable mandibular autorotation as demonstrated by a mean increase in SNB and a significant reduction in MP-FH. Both age groups had a mean reduction in the LFH, but this was at odds with an overall 2.7-mm mean increase in TFH in adolescents. This may be interpreted as an indication that the intrusion-related changes in mandibular position (reductions in LFH and MP-FH) offset the underlying pattern of vertical facial growth in growing individuals. The adult cases had a similar reduction in both LFH and TFH.
While the subgroup numbers are too small for meaningful statistical analysis, our results also indicate that adult patients demonstrated more maxillary second molar intrusion than did the adolescents. This might be because most adult AOB occlusions are “propped” open on the second molar occlusal contacts while in adolescents these teeth would still be erupting. Both age groups exhibited at least some vertical mandibular molar changes, representing continued eruption or overeruption of the mandibular molars. However, these changes were not significant in the adult subgroup. Since uncontrolled eruption of the mandibular molars could mitigate the beneficial effects of the maxillary molar intrusion, the authors recommend that mandibular molar positions be controlled from the start of maxillary molar intrusion, especially in adolescent patients whose second molars are still erupting. This could be achieved using either occlusal coverage of these molars with a vacuum-formed appliance (retainer), full fixed appliance engagement of all erupted molar teeth, or another reliable form of mandibular second molar anchorage.
Future studies should include standardization of the clinical intrusion technique including mini-implant location, amount and vector of traction, transpalatal fixtures, and mandibular molar anchorage, particularly for adolescent subjects. Larger age subgroups in a prospective study compared with controls would offer more meaningful statistical analysis of changes in growing and nongrowing patients.
CONCLUSIONS
Orthodontic mini-implants provide adequate skeletal anchorage for maxillary molar intrusion in patients with anterior open bites.
Therefore, this treatment modality can be considered a reasonable alternative to orthognathic surgery for AOB correction in appropriate cases wherein the malocclusion—rather than facial esthetics—is the primary issue.
While maxillary molar intrusion aids in the correction of AOB irrespective of age, adolescent patients tend to demonstrate more favorable mandibular autorotation changes (Class II correction). In contrast, more changes occur in the occlusal plane angle and maxillary parameters in adults.
ACKNOWLEDGMENT
Dr. Richard Cousley has a financial interest in the Infinitas mini-implant system, as sold by DB Orthodontics Ltd. No other relationships, conditions, or circumstances present a conflict of interest for Dr. Cousley or any of the other three authors involved in the preparation of this manuscript.
REFERENCES
- 1.Baek MS, Choi YJ, Yu HS, Lee KJ, Kwak J, Park YC. Long-term stability of anterior open-bite treatment by intrusion of maxillary posterior teeth. Am J Orthod Dentofacial Orthop. 2010;138:396.e1–e9. doi: 10.1016/j.ajodo.2010.04.023. discussion, 396–398. [DOI] [PubMed] [Google Scholar]
- 2.Deguchi T, Kurosaka H, Oikawa H, et al. Comparison of orthodontic treatment outcomes in adults with skeletal open bite between conventional edgewise treatment and implant-anchored orthodontics. Am J Orthod Dentofacial Orthop. 2011;139(Suppl):S60–S68. doi: 10.1016/j.ajodo.2009.04.029. [DOI] [PubMed] [Google Scholar]
- 3.Kravitz ND, Kusnoto B, Tsay TP, Hohlt WF. The use of temporary anchorage devices for molar intrusion. J Am Dent Assoc. 2007;138:56–64. doi: 10.14219/jada.archive.2007.0021. [DOI] [PubMed] [Google Scholar]
- 4.Park HS, Kwon TG, Kwon OW. Treatment of open bite with microscrew implant anchorage. Am J Orthod Dentofacial Orthop. 2004;126:627–636. doi: 10.1016/j.ajodo.2003.07.019. [DOI] [PubMed] [Google Scholar]
- 5.Buschang PH, Carrillo R, Rossouw PE. Orthopedic correction of growing hyperdivergent, retrognathic patients with miniscrew implants. J Oral Maxillofac Surg. 2011;69:754–762. doi: 10.1016/j.joms.2010.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akan S, Kocadereli I, Aktas A, Tasar F. Effects of maxillary molar intrusion with zygomatic anchorage on the stomatognathic system in anterior open bite patients. Eur J Orthod. 2013;35:93–102. doi: 10.1093/ejo/cjr081. [DOI] [PubMed] [Google Scholar]
- 7.Kuroda S, Sakai Y, Tamamura N, Deguchi T, Takano-Yamamoto T. Treatment of severe anterior open bite with skeletal anchorage in adults: comparison with orthognathic surgery outcomes. Am J Orthod Dentofacial Orthop. 2007;132:599–605. doi: 10.1016/j.ajodo.2005.11.046. [DOI] [PubMed] [Google Scholar]
- 8.Lee H, Park Y. Treatment and posttreatment changes following intrusion of maxillary posterior teeth with miniscrew implants for open bite correction. Korean J Orthod. 2008;38:31–40. [Google Scholar]
- 9.Cousley RR. The Orthodontic MiniImplant Clinical Handbook. 1st ed. Wiley-Blackwell; 2013. p. 184. [Google Scholar]
- 10.Cousley RR. A clinical strategy for maxillary molar intrusion using orthodontic mini-implants and a customized palatal arch. J Orthod. 2010;37:202–208. doi: 10.1179/14653121043101. [DOI] [PubMed] [Google Scholar]
- 11.Xun C, Zeng X, Wang X. Microscrew anchorage in skeletal anterior open-bite treatment. Angle Orthod. 2007;77:47–56. doi: 10.2319/010906-14R.1. [DOI] [PubMed] [Google Scholar]
- 12.King EW. A roentgenographic study of pharyngeal growth 1. Angle Orthod. 1952;22:23–37. [Google Scholar]
- 13.Erverdi N, Keles A, Nanda R. The use of skeletal anchorage in open bite treatment: a cephalometric evaluation. Angle Orthod. 2004;74:381–390. doi: 10.1043/0003-3219(2004)074<0381:TUOSAI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]