Abstract
Objective:
To determine whether changes in primary attending (PA) doctor coverage frequency caused an increase in orthodontic treatment time or a decrease in the quality of treatment results in a postgraduate orthodontic clinic. The effect of T1 Peer Assessment Rating (PAR) scores on PA doctor coverage frequency, treatment times, and results was also evaluated.
Materials and Methods:
A sample of 191 postorthodontic subjects was divided into three groups based on PA doctor coverage (high, medium, or low). Treatment times, treatment results, and other variables were compared between the three PA coverage groups. Additionally, the sample was divided into three groups based on T1 PAR scores. Attending coverage frequency, treatment times, and results were compared between the T1 PAR groups.
Results:
No statistically significant differences were found in treatment time (P = .128) or results (P = .052). There were no statistically significant differences in the mean scores for T1 PAR (P = .056), T2 PAR (P = .602), patient age at T1 (P = .747), total appointments (P = .128), missed appointments (P = .177), or cancelled appointments (P = .183). Statistically significant differences were found between the low T1 PAR group and the medium and high T1 PAR groups (attending coverage, P = .008; results, P < .001; treatment time, P = .001).
Conclusions:
Under the conditions of this study, variations in PA doctor coverage frequency did not lengthen orthodontic treatment or reduce the quality of treatment results. Low T1 PAR scores were associated with less PA coverage, less change in PAR, and shorter treatment times.
Keywords: Treatment time, Treatment results, Peer Assessment Ratings, Graduate clinic
INTRODUCTION
In some postgraduate orthodontic clinics, routine treatment for a single patient may be directed by a variable number of orthodontic faculty members. Similarly, some private practice arrangements may lead to treatment of individual patients by two or more orthodontic practitioners. Some of these situations might include practice transfer and associate coverage during sickness or vacation. Each orthodontist may have individualized ideas concerning the best management of an individual orthodontic problem. Some of this variation might shift orthodontic treatment along new treatment pathways. It seems intuitive that changes in the supervision of orthodontic cases might, therefore, lead to prolonged orthodontic treatment.
It is important to understand all the variables that influence treatment time, because our patients demand accurate estimates. In a recent study of patients' most common recommendations for orthodontists, “true and accurate timing estimates” ranked second to “reduction in treatment fees.”1 Patients who are given accurate information about predicted treatment times are more likely to be satisfied with treatment overall and will have more realistic expectations about the outcomes of their treatment.2
A generally accepted treatment time for satisfactory completion of normal orthodontic treatment has not been determined. Recently, 15 to 24 months was suggested as a typical fixed appliance treatment time.3 In general, claims that certain types of fixed appliances are superior to others in their ability to expedite treatment or improve results remain unsubstantiated.3,4 Some observations suggest that extraction treatment,4,5 impacted canines,6,7 increased Difficulty Index (American Board of Orthodontics),6 patient compliance,8 and orthognathic surgery9,10 may be factors that lead to prolonged treatment time. Orthodontic cases that involve orthognathic surgery are reported to have treatment times between 27.8 and 30.6 months.9,10
A recent study in a postgraduate orthodontic clinic evaluated the effect of changing orthodontic residents on treatment time and results.11 The study found that treatment by multiple orthodontic residents caused a statistically significant increase in treatment time but had no effect on treatment results.11 The authors did not evaluate the effect of changes in primary attending (PA) doctor coverage frequency.
The main goal of this study was to determine whether variations in the supervision of orthodontic treatment have a deleterious effect on treatment time or results. This study was conducted in a school setting, where variation in case supervision was likely to be elevated vs private practice. The null hypothesis was that changes in PA doctor coverage frequency would have no effect on treatment time or treatment results.
The secondary goal of this study was to determine if variations in T1 Peer Assessment Rating (PAR) scores have an effect on PA doctor coverage frequency, treatment time, or results. The null hypothesis was that variation in T1 PAR scores would have no effect on PA doctor coverage frequency, treatment time, or results.
MATERIALS AND METHODS
Subjects were selected from patients in the retention phase of treatment in a postgraduate orthodontic clinic. In this clinic, most patients who have finished orthodontic treatment are supervised in retention for a period of at least 2 years. Two inclusion criteria were applied to the retention patients: (1) digital study models were available for analysis, and (2) the patient had been approved for appliance removal by the PA doctor and by the patient (or legal guardian). The following types of cases were excluded from the study: (1) phase one or limited phase two cases, (2) complex interdisciplinary patients, (3) orthognathic surgical patients, (4) craniofacial patients, (5) patients who were debonded prior to completing treatment, and (6) patients who were missing any information required in this study. Of the 364 active retention patients that met the inclusion criteria, 191 of these met both the inclusion and exclusion criteria of this study. The study group comprised 118 female and 73 male patients.
Clinical data collected from each chart included: (1) age at the start of treatment (rounded to the nearest tenth of a year), (2) gender, (3) total treatment time from delivery of the first appliances to the debonding appointment, (4) number of appointments, (5) number of missed appointments, (6) number of cancelled appointments, and (7) number of appointments covered by the PA faculty member. The PA faculty was the faculty member who signed the patient's chart most frequently.
In this orthodontic clinic, T1 and T2 stone models are routinely scanned into digital format using an Ortho Insight 3D laser scanner (Motion View Software, Chattanooga, Tenn). The digital model records of the sample group were collected and anonymized. The PAR index at T1 and T2 was evaluated by a single rater who was calibrated in PAR scoring. The United Kingdom PAR scoring system was used. The digital charting systems in use by the orthodontic clinic were Ortho2 (version ViewPoint 9; Ortho2, Ames, Iowa) and Dolphin Imaging (version 11.5 Premium; Patterson Dental, Chatsworth, Calif). Institutional review board approval was obtained before initiation of data collection.
Analysis of the Sample Group
The sample group (n = 191) was divided into three nearly equal-sized groups based on the percentage of PA coverage (low, medium, or high). The low PA coverage group (n = 65) included patients who saw the PA at 18% to 50% of their appointments. The medium PA coverage group (n = 63) included patients who saw the PA at 50% to 65% of their appointments. The high PA coverage group (n = 63) included patients who saw the PA at more than 65% of their appointments.
The three PA coverage groups were compared with respect to: (1) T1 PAR scores, (2) T2 PAR scores, (3) change in PAR scores (PAR Chg), (4) percent change in PAR scores (PAR%Chg), (5) treatment time (Tx Time) in months, (6) age at T1 (T1 Age) in years, (7) total number of appointments (Total Appts), (8) missed appointments (Missed Appts), and (9) cancelled appointments (Cancelled Appts).
The sample group was divided a second time into three groups based on T1 PAR scores (low, medium, high). The low T1 PAR group (n = 66) included patients who had T1 PAR scores of 3–17. The medium T1 PAR group (n = 65) comprised patients who had T1 PAR scores of 18–29. The high T1 PAR group (n = 60) consisted of patients with T1 PAR scores of 30–54. These three T1 PAR groups were compared with respect to: (1) percent change in PAR scores (PAR%Chg), (2) percentage PA appointments (%PA Appts), and (3) treatment time (Tx Time) in months.
Statistical Analysis
One-way analysis of variance was used evaluate the relationships between the variables. Statistical significance was accepted at α = .05. Further analysis of additional questions was done using Pearson correlation tests and comparisons of means. A correlation score of 0 to 0.3 indicated weak correlation, 0.31 to 0.5 indicated moderate correlation, 0.51 to 0.7 indicated strong correlation, and greater than 0.7 indicated very strong correlation.
RESULTS
Average Treatment Time and Appointment Number
The mean treatment time was 24.8 months, with a standard deviation of 8.0 months. The mean number of appointments was 24.9, with a standard deviation of 7.6 appointments.
Analysis of the Sample Group
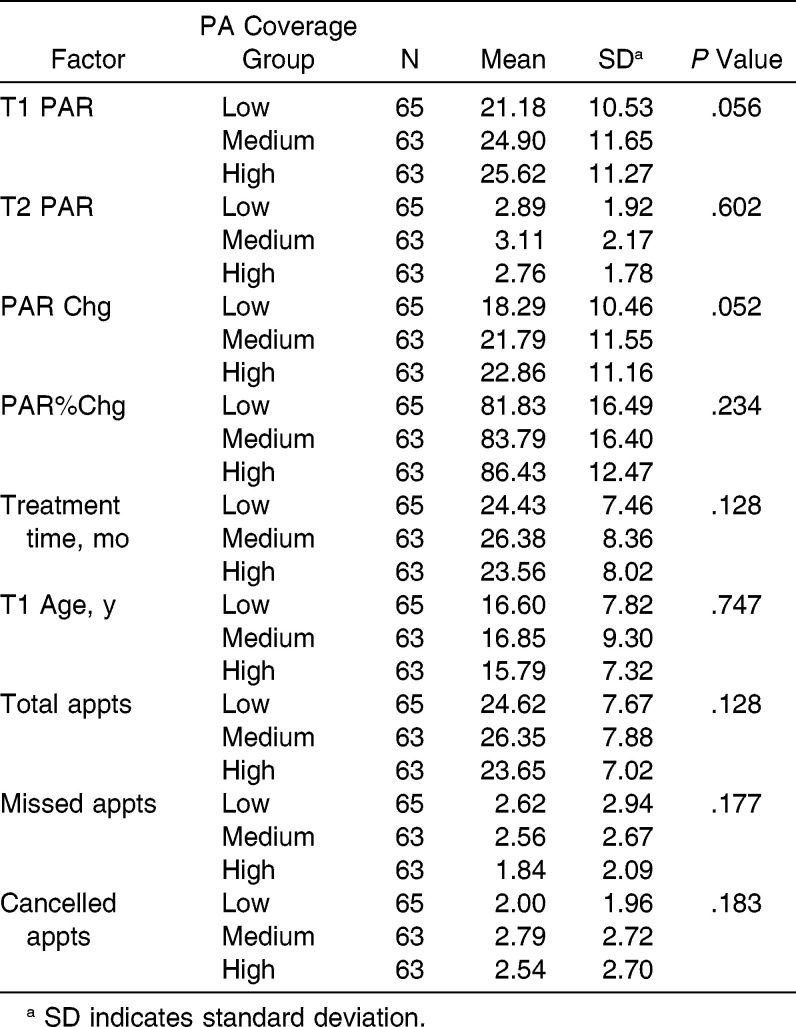
Low, medium, and high PA coverage groups had average treatment times of 24.4, 26.4, and 23.6 months, respectively. Average percent changes in PAR for the three groups were 81.8%, 83.8%, and 86.4%, respectively. There were no statistically significant differences between treatment time (P = .128) and PAR results (P = .234) among the three groups (Table 1).
Table 1.
Summary of Findings for the PA Coverage Groups
There were no statistically significant differences in T1 PAR scores, T2 PAR scores, total number of appointments, missed appointments, cancelled appointments, or patient age at the start of treatment (P > .052) (Table 1).
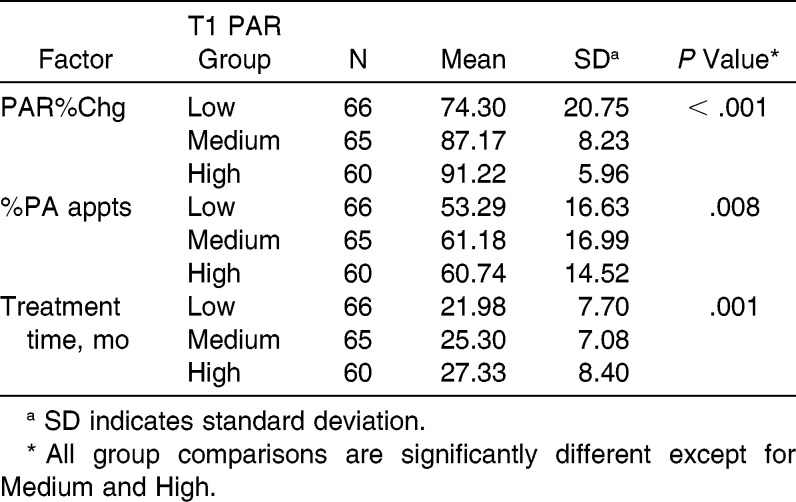
Low, medium, and high T1 PAR groups had average percent changes in PAR score of 74.3%, 87.2%, and 91.2%, respectively. Average percent of appointments covered with the PA doctor were 53.3%, 61.2%, and 60.7%, respectively. Average treatment times were 22.0, 25.3, and 27.3 months, respectively. There were statistically significant differences in percent change in PAR (P < .001), treatment time (P = .008), and percent of PA coverage (P = .001) between the low T1 PAR and the medium T1 PAR groups as well as the low T1 PAR and high T1 PAR groups. The medium and high T1 PAR groups were not statistically significantly different from each other (Table 2).
Table 2.
Summary of Findings for the T1 PAR Groups
Additional Comparisons
Correlations with T1 PAR score
A weak correlation was found between T1 PAR scores and number of total appointments (r = 0.248, P = .001), as well as T1 PAR scores and total treatment time (r = 0.280, P < .001).
Correlations with treatment time
The total number of appointments had a very strong correlation with total treatment time (r = 0.822, P < .001). Missed appointments were moderately correlated with total treatment time (r = 0.333, P < .001). Cancelled appointments were weakly correlated with treatment time (r = 0.119, P = .119).
DISCUSSION
In our orthodontic clinic, 22 orthodontists supervise patient treatment. Two or three faculty members supervise 12 to 18 students during each 4-hour clinic session. Faculty members are assigned to the clinic in 2-week cycles. A single faculty member (the PA) is charged with the supervision of all aspects of a single patient's care (including treatment planning, supervision of adjustment appointments, and the final debonding decision). Ideally, patients are scheduled on days that match the faculty member's schedule; however, there are numerous situations in which this ideal scheduling cannot be accomplished. In these situations, patients may be scheduled with a non-PA faculty member. The non-PA faculty often follows the original written treatment plan but has the authority to evaluate the patient's response to treatment and may recommend changes to the original treatment plan.
The Three PA Coverage Groups
Because treatment duration and treatment results were similar between the three PA coverage groups, it can be concluded that orthodontic treatment time and results were not affected by changes in PA doctor coverage. The following confounding variables were evaluated to make sure that they did not influence these conclusions.
The demographic characteristics of the three PA coverage groups were similar. There were no significant differences between the groups in T1 PAR scores or patient age at the start of treatment. This was expected because incoming orthodontic clinic patients were randomly assigned to the PA doctors. Furthermore, factors related to patient compliance (missed appointments, cancelled appointments) were similar between the three PA coverage groups. Because the variables related to demographics and patient compliance were equal among the three groups, they could not have influenced treatment time or results.
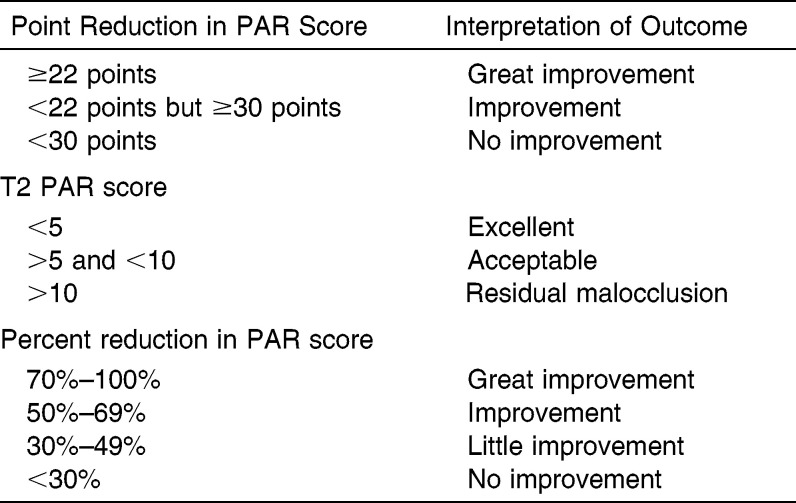
Use of PAR scores to evaluate treatment results
The PAR score assigns numeric values to the traits that comprise a malocclusion. The score increases as the severity of the malocclusion increases. The PAR scoring method has been validated in the United Kingdom11–13 and has been adapted for use in North America.14,15 This scoring method has also been used to evaluate digital models.16,17 The PAR scoring system has been used to measure treatment results in several published ways: (1) point reduction in PAR score, (2) T2 PAR score, and (3) percent reduction in PAR score (see Table 3).18–22 All three methods were applied to the analysis of T2 PAR scores reported in this paper.
Table 3.
Published Methods to Evaluate Case Results Using PAR Scores
Point reduction in PAR score
Previous authors have suggested that a 22-point (or greater) reduction in PAR scores indicates a “great improvement” in the malocclusion. Applying this cutoff to the study sample shows that 46.6% of subjects (89/191 subjects) demonstrated “great improvement.” Furthermore, if all cases with T1 PAR scores under 22 are eliminated from the sample, then 83% of the remaining subjects demonstrated “great improvement.”
T2 PAR score
When only T2 PAR point values were used to assess the outcome of treatment, 90% (172/191 subjects) had T2 PAR scores of 5 or lower and therefore demonstrated “excellent” treatment outcomes. Two subjects had T2 PAR scores of 10 and therefore demonstrated a “residual malocclusion.” The other subjects fell between these two groups.
Percent reduction in PAR score
When percent reduction in PAR score was used to assess treatment outcome, 1.0% (2/191) of the subjects showed “no improvement,” 4.2% (8/191) showed “little improvement,” 8.4% (16/191) showed “improvement,” and 86.4% showed “great improvement.”
The Three T1 PAR Groups
Patients with low T1 PAR scores showed less improvement over the course of treatment than those with medium or high T1 PAR scores. This is a result that could be expected, since a low T1 PAR score means there is less malocclusion to improve.
While the mean percent change for the high T1 PAR group was greater than that in the medium group (91.2% compared to 87.2%), the percentages were not statistically significantly different. Treatment times were also shorter on average for the low T1 PAR group (22.0 months), which was significantly different from the other two groups. The medium and high T1 PAR groups were, again, not significantly different from each other, at 25.3 and 27.3 months, respectively. What was interesting was that the low T1 PAR group had less consistency in PA coverage (53.3%, compared to over 60% in the other two groups), and this difference was statistically significant. One possible explanation for this could be that cases that are less challenging at T1 do not need to be scheduled as rigidly with the same attending doctor.
Correlations with T1 PAR Scores
One might expect that as T1 PAR scores increase (indicating an increase in case difficulty), the treatment time and numbers of appointments would also increase. Analysis of the data confirmed weak correlations between T1 PAR scores and both treatment time (r = 0.280) and total appointments (r = 0.248). This finding is in agreement with Parrish et al., who reported that higher Difficulty Index scores (which also measure complexity in a case at the start of treatment) were predictive of longer treatment times.6
Correlations with Treatment Time
Total appointments and treatment time were strongly correlated (r = 0.822). This is expected to be true in most orthodontic cases, since most patients are seen at regular intervals throughout treatment. Increases in treatment time were moderately correlated with missed appointments (r = 0.333) and weakly correlated with cancelled appointments (r = 0.119). From a patient compliance standpoint, this finding makes sense, since the “cancelled” appointments designated instances in which a patient had called to communicate that they were not coming in (and often to reschedule) and the “missed” appointments indicated that a patient had failed to show (and had not called). These findings support the findings of Beckwith et al., who concluded that poor patient compliance prolongs treatment time.8
CONCLUSIONS
Variation in PA doctor coverage in a postgraduate orthodontic clinic does not lengthen orthodontic treatment or reduce the quality of treatment results.
Average treatment times in the examined postgraduate clinic are within published “normal treatment times,” and treatment results (as measured by PAR scores) meet or exceed what is considered clinically acceptable.18–21
Low-complexity cases (low T1 PAR) were associated with less PA coverage, less change in PAR, and shorter treatment times.
REFERENCES
- 1.O'Connor PJ. Patient's perceptions before, during, and after orthodontic treatment. J Clin Orthod. 2000;34:591–592. [PubMed] [Google Scholar]
- 2.Mavreas D, Athanasiou A. Factors affecting the duration of orthodontic treatment: a systematic review. Eur J Orthod. 2008;30:386–395. doi: 10.1093/ejo/cjn018. [DOI] [PubMed] [Google Scholar]
- 3.Fleming PS, DiBiase AT, Lee RT. Randomized clinical trial of orthodontic treatment efficiency with self-ligating and conventional fixed orthodontic appliances. Am J Orthod Dentofacial Orthop. 2010;137:738–742. doi: 10.1016/j.ajodo.2009.06.023. [DOI] [PubMed] [Google Scholar]
- 4.DiBiase AT, Nasr IH, Scott P, Cobourne MT. Duration of treatment and occlusal outcome using Damon3 self-ligated and conventional orthodontic bracket systems in extraction patients. Am J Orthod Dentofacial Orthop. 2011;139:e111–e116. doi: 10.1016/j.ajodo.2010.07.020. [DOI] [PubMed] [Google Scholar]
- 5.Fisher MA, Wenger RM, Hans MG. Pretreatment characteristics associated with orthodontic treatment duration. Am J Orthod Dentofacial Orthop. 2010;137:178–186. doi: 10.1016/j.ajodo.2008.09.028. [DOI] [PubMed] [Google Scholar]
- 6.Parrish LD, Roberts WE, Maupome G, Stewart KT, Bandy RW, Kula KS. The relationship between ABO discrepancy index and treatment duration in a graduate orthodontic clinic. Angle Orthod. 2011;81:192–197. doi: 10.2319/062210-341.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stewart JA, Heo G, Glover EK, Williamson PC, Lam EN, Major PW. Factors that relate to treatment duration for patients with palatally impacted maxillary canines. Am J Orthod Dentofacial Orthop. 2001;119:216–225. doi: 10.1067/mod.2001.110989. [DOI] [PubMed] [Google Scholar]
- 8.Beckwith FR, Ackerman RJ, Cobb CM, Tira DE. An evaluation of factors affecting duration of orthodontic treatment. Am J Orthod Dentofacial Orthop. 1999;115:439–447. doi: 10.1016/s0889-5406(99)70265-9. [DOI] [PubMed] [Google Scholar]
- 9.Slavnic S, Marcusson A. Duration of orthodontic treatment in conjunction with orthognathic surgery. Swed Dent J. 2010;34:159–166. [PubMed] [Google Scholar]
- 10.Arad I, Jandu J, Bassett P, Fleming PS. Influence of single-jaw surgery vs bimaxillary surgery on outcome and duration of combined orthodontic-surgical treatment. Angle Orthod. 2011;81:983–987. doi: 10.2319/030211-150.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McGuinness NJ, McDonald JP. The influence of operator changes on orthodontic treatment times and results in a postgraduate teaching environment. Eur J Orthod. 1998;20:159–167. doi: 10.1093/ejo/20.2.159. [DOI] [PubMed] [Google Scholar]
- 12.Shaw WC, Richmond S, O'Brien K, Brook P, Stephens CD. Quality control in orthodontics: indices of orthodontic treatment need and treatment standards. Brit Dent J. 1991;170:107–112. doi: 10.1038/sj.bdj.4807429. [DOI] [PubMed] [Google Scholar]
- 13.Richmond S, Shaw WC, O'Brien K, et al. The development of the PAR Index (Peer Assessment Rating): reliability and validity. Eur J Orthod. 1992;14:125–139. doi: 10.1093/ejo/14.2.125. [DOI] [PubMed] [Google Scholar]
- 14.DeGuzman L, Bahiraei BS, Vig KWL, Vig PS, Weyant RJ, O'Brien K. The validation of the Peer Assessment Rating index for malocclusion severity and treatment difficulty. Am J Orthod Dentofacial Orthop. 1995;107:172–176. doi: 10.1016/s0889-5406(95)70133-8. [DOI] [PubMed] [Google Scholar]
- 15.Firestone A, Beck FM, Beglin FM, Vig KWL. Evaluation of the peer assessment rating (PAR) index as an index of orthodontic treatment need. Am J Orthod Dentofacial Orthop. 2002;122:463–469. doi: 10.1067/mod.2002.128465. [DOI] [PubMed] [Google Scholar]
- 16.Mayers M, Firestone A, Rashid R, Vigd KWL. Comparison of peer assessment rating (PAR) index scores of plaster and computer-based digital models. Am J Orthod Dentofacial Orthop. 2005;128:431–434. doi: 10.1016/j.ajodo.2004.04.035. [DOI] [PubMed] [Google Scholar]
- 17.Fleming PS, Marinho V, Johal A. Orthodontic measurements on digital study models compared with plaster models: a systematic review. Orthod Craniofac Res. 2010;14:1–16. doi: 10.1111/j.1601-6343.2010.01503.x. [DOI] [PubMed] [Google Scholar]
- 18.Feghali R, Nelson S, Hans MG. Comparing orthodontic treatment outcome of two geographically different clinic samples [abstract] J Dental Res. 1997;76:1181. [Google Scholar]
- 19.Ngan P, Yiu C. Evaluation of treatment and posttreatment changes of protraction facemask treatment using the PAR index. Am J Orthod Dentofacial Orthop. 2000;118:414–419. doi: 10.1067/mod.2000.108253. [DOI] [PubMed] [Google Scholar]
- 20.Salvatore de Freitas KM, Janson G, Roberto de Freitas M, Pinzan A, Henriques JFC, Pinzan-Vercelinoa CRM. Influence of the quality of the finished occlusion on postretention occlusal relapse. Am J Orthod Dentofacial Orthop. 2007;132:428.e9–e14. doi: 10.1016/j.ajodo.2007.02.051. [DOI] [PubMed] [Google Scholar]
- 21.Richmond S, Shaw WC, Roberts CT, Andrews M. The PAR Index (Peer Assessment Rating): methods to determine outcome of orthodontic treatment in terms of improvement and standards. Eur J Orthod. 1992;14:180–187. doi: 10.1093/ejo/14.3.180. [DOI] [PubMed] [Google Scholar]
- 22.Ahmad N, Fida M. orthodontic treatment outcome assessment using Peer Assessment Rating (PAR) Index. Pak Oral Dent J. 2010;30:380–387. [Google Scholar]