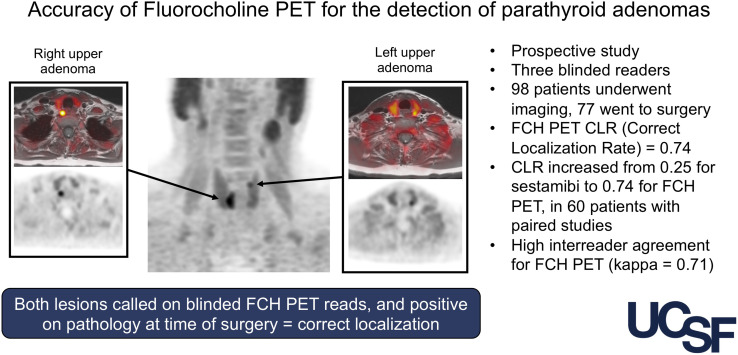
Visual Abstract
Keywords: endocrine, PET, fluorocholine, hyperparathyroidism, PET, parathyroid adenomas
Abstract
The purpose of this prospective study was to determine the correct localization rate (CLR) of 18F-fluorocholine PET for the detection of parathyroid adenomas in comparison to 99mTc-sestamibi imaging. Methods: This was a single-arm prospective trial. Ninety-eight patients with biochemical evidence of primary hyperparathyroidism were imaged before parathyroidectomy using 18F-fluorocholine PET/MRI. 99mTc-sestamibi imaging performed separately from the study was evaluated for comparison. The primary endpoint of the study was the CLR on a patient level. Each imaging study was interpreted by 3 masked readers on a per-region basis. Lesions were validated by histopathologic analysis of surgical specimens. Results: Of the 98 patients who underwent 18F-fluorocholine PET, 77 subsequently underwent parathyroidectomy and 60 of those had 99mTc-sestamibi imaging. For 18F-fluorocholine PET in patients who underwent parathyroidectomy, the CLR based on the masked reader consensus was 75% (95% CI, 0.63–0.82). In patients who underwent surgery and had an available 99mTc-sestamibi study, the CLR increased from 17% (95% CI, 0.10–0.27) for 99mTc-sestamibi imaging to 70% (95% CI, 0.59–0.79) for 18F-fluorocholine PET. Conclusion: In this prospective study using masked readers, the CLR for 18F-fluorocholine PET was 75%. In patients with a paired 99mTc-sestamibi study, the use of 18F-fluorocholine PET increased the CLR from 17% to 70%. 18F-fluorocholine PET is a superior imaging modality for the localization of parathyroid adenomas.
Primary hyperparathyroidism (PHPT) is a common endocrine disorder caused by a hyperfunctioning parathyroid adenoma in over 85% of cases. Surgery is the only curative therapy for PHPT and is associated with a decreased risk of fractures and nephrolithiasis and with a long-term improvement in quality of life (1–4). A minimally invasive unilateral surgical approach is preferred to lessen the morbidity associated with bilateral neck exploration while providing similar cure rates and long-term benefits (5). This less invasive approach is possible only when preoperative imaging studies can correctly localize the culprit parathyroid adenomas (6). These studies include 99mTc-sestamibi scintigraphy and neck ultrasound, which are traditionally the most commonly used first-line imaging options for PHPT, as well as newer modalities such as 4-dimensional CT.
Although most commonly reported for use in prostate cancer, 18F-fluorocholine PET has been studied extensively for the detection of parathyroid adenomas (7). It has been hypothesized that parathyroid adenomas have increased uptake of 18F-fluorocholine due to upregulation of phospholipid/calcium2+-dependent choline kinase (8). European centers have shown 18F-fluorocholine PET to be highly accurate in the detection of parathyroid adenomas (9), particularly among patients with negative, discordant, or inconclusive results on conventional imaging, as well as among reoperative patients (10,11). Though most reports of 18F-fluorocholine PET pair it with low-dose CT for anatomic mapping, our institution performs simultaneous MRI to avoid excess ionizing radiation. We have previously reported a 90% sensitivity and 100% positive predictive value for correct localization of parathyroid adenomas using 18F-fluorocholine PET/MRI in a pilot study of 10 patients with PHPT and inconclusive results on ultrasound and 99mTc-sestamibi imaging (12).
In this study, we aimed to prospectively evaluate the ability of 18F-fluorocholine PET to correctly localize parathyroid adenomas, and we compared the correct localization rate (CLR) of 18F-fluorocholine PET with that of 99mTc-sestamibi imaging.
MATERIALS AND METHODS
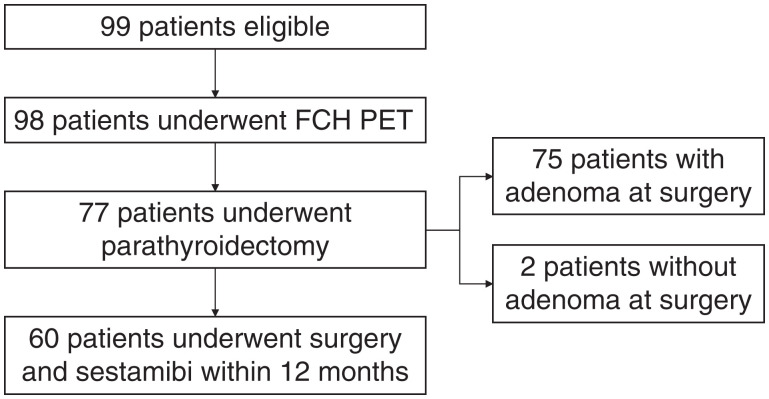
This study was approved by the local institutional review board, and written informed consent was obtained from all subjects. Between September 2016 and July 2019, 98 patients were consecutively enrolled in this prospective study evaluating the use of 18F-fluorocholine PET in patients with PHPT at the University of California, San Francisco (NCT03764007). This study was performed under a cost-recovery investigational-new-drug approval from the Food and Drug Administration. Inclusion criteria included biochemically proven PHPT, intention to treat with surgery, and a age of more than 13 y. Prior 99mTc-sestamibi imaging was not a requirement for enrollment. The Standards for Reporting of Diagnostic Accuracy (STARD) flow diagram is shown in Figure 1. The study was initiated, planned, conducted, analyzed, and published by the investigators. No financial support was received from commercial entities. The full protocol is available as supplemental material (available at http://jnm.snmjournals.org).
FIGURE 1.
STARD flow diagram for efficacy cohort.
18F-Fluorocholine Synthesis
18F-fluorocholine was synthesized using the ORA Neptis Perform synthesizer (Optimized Radiochemical Applications) as previously described, using a nucleophilic substitution reaction (13). Dibromomethane (primary precursor) and N,N-dimethylethanolamine (secondary precursor) were obtained from Abx GmbH.
Imaging Protocol
All imaging was performed on a 3.0-T time-of-flight PET/MRI scanner (Signa; GE Healthcare). Patients were injected with a mean (±SD) of 222 ± 26 MBq (6.0 ± 0.7 mCi) of 18F-fluorocholine, and imaging was performed 31 ± 16 min after injection (the protocol window for uptake time was 20–60 min after injection). Two PET bed positions were acquired, the first centered over the thyroid, and the second more inferiorly, to catch any mediastinal adenomas. The first bed position, over the neck, was acquired for 20 min, and the second, over the chest, was acquired for 8 min. PET datasets were reconstructed using a time-of-flight algorithm with ordered-subset expectation maximization using 2 iterations and 28 subsets and a matrix size of 256 × 256. Axial sections were reconstructed at a thickness of 2.78 mm. In the neck, the MRI acquisition included axial T1-weighted spin-echo and axial T2-weighted spin-echo imaging with IDEAL fat saturation (iterative decomposition of water and fat with echo asymmetry and least-squares estimation). In the chest, the MRI acquisition included a T2-weighted spin-echo sequence with 2-point Dixon fat saturation, as well as a T1-weighted spoiled gradient-echo sequence with 2-point Dixon fat saturation.
Image Analysis
All 18F-fluorocholine PET studies were reviewed by 3 nuclear medicine physicians not involved in the study and from different institutions. The 3 readers had no prior experience interpreting 18F-fluorocholine PET parathyroid studies, and each reviewed a 10-patient training dataset before performing the masked readings for this study. The central readers were masked to all aspects of the subject’s history, and interpretation was performed using OsiriX (14). Image interpretations were recorded in a centralized REDcap database for analysis. The location of the most likely parathyroid adenoma was recorded. For patients in whom multiple adenomas were visualized, all abnormal regions were recorded.
Two months separate from the 18F-fluorocholine PET readings, the same 3 readers interpreted the 99mTc-sestamibi studies in the subset of patients for whom 99mTc-sestamibi imaging was performed. The 99mTc-sestamibi studies were not performed as part of this protocol, and interpretation was based on the images available in the PACS. The 99mTc-sestamibi technique was not harmonized across all patients. Analysis also was performed using local readings, as bias may exist among the 3 masked readers.
Surgical Management
Patients who subsequently had surgery underwent either focused unilateral parathyroidectomy or bilateral neck exploration at our institution per the surgeon’s judgment, with the standard practice being to offer focused parathyroidectomy with intraoperative parathyroid hormone monitoring in cases with localizing preoperative imaging. The surgeon designated the adenoma location as anatomic or embryologic, and histopathologic analysis confirmed whether the adenoma was enlarged or hypercellular. For this study, the definition of surgical success was based on normalization of serum calcium and parathyroid hormone levels 6 h after parathyroidectomy, as well as on serum calcium levels from blood drawn at approximately 2 wk after surgery.
Statistical Analysis
The primary endpoint of this prospective study was a comparison of the CLR of 18F-fluorocholine PET with that of 99mTc-sestamibi imaging for the detection of parathyroid adenomas. Our analysis focused on CLR, which was chosen on the basis of guidance to the investigators by the Food and Drug Administration during a preliminary new-drug-application meeting. The use of CLR helps to minimize the benefit of overcalling lesions and more accurately reflects the ability of the imaging study to guide a focused surgical approach. Correct localization was defined as positive on a patient level if at least 1 anatomic region (categorized into 3 groups—left neck, right neck, and other) was correctly characterized as a true-positive signal and no other regions were characterized as false-positive; the denominator for CLR is all patients available for analysis. True-negative patients were defined as patients in whom all regions were called negative and no parathyroid adenoma was found at the time of surgery. False-positive and false-negative patients were defined as patients in whom 1 region was determined to be either false-positive or false-negative, respectively, independent of whether a separate region was determined to be true-positive. For presentation purposes, the consensus reading of the 3 masked readers is used when the consensus was determined by the majority reading from the initial assessment. Our predetermined statistical plan estimated that we needed 67 patients with pathologic analysis and 99mTc-sestamibi imaging to demonstrate a difference in sensitivity of 70% for 99mTc-sestamibi imaging and 85% for 18F-fluorocholine PET, with a power of 87, allowing for a drop of 10 patients. Interreader variability was calculated for the location of the parathyroid adenoma (left neck vs. right neck vs. other) using a Fleiss κ and for all regions together for both 18F-fluorocholine PET and 99mTc-sestamibi interpretations, and strength of agreement was determined according to the definition described by Landis and Koch (15). Statistical analysis was performed in R statistical software (version 3.3.3; R Foundation).
The safety of 18F-fluorocholine PET imaging was assessed by regular monitoring for adverse events during and immediately after study acquisition and was measured as a secondary endpoint by the rate of reported adverse events.
RESULTS
In total, of the 99 patients who enrolled in the study, 98 were ultimately imaged using 18F-fluorocholine PET/MRI, 72 of whom were female (Table 1). Forty-one patients (42%) had prior parathyroidectomy, a disproportionate number reflecting the higher frequency of more complex clinical cases evaluated at a tertiary-care referral center.
TABLE 1.
Characteristics of Patients at Baseline
| Characteristic | All patients (n = 98) | Efficacy cohort | |
|---|---|---|---|
| Surgery cohort (n = 77) | 99mTc-sestamibi cohort (n = 60) | ||
| Median age (y) | 64 (range, 17–90) | 66 (range, 17–86) | 65 (range, 17–85) |
| Sex | |||
| Male | 26 (27) | 18 (23) | 13 (22) |
| Female | 72 (73) | 59 (77) | 47 (78) |
| Prior parathyroidectomy | 41 (42) | 26 (34) | 24 (40) |
| Prior imaging with 99mTc-sestamibi | |||
| Total | 92 (94) | 73 (95) | n/ |
| Within 12 mo | 77 (79) | 62 (81) | n/ |
| Number positive | 44 (57) | 43 (59) | n/ |
| Ultrasound | |||
| Total | 94 (96) | 76 (99) | 59 (98) |
| Number positive | 45 (48) | 41 (54) | 33 (56) |
| Baseline laboratory values (mean ± SD) | |||
| Calcium | 10.6 ± 0.6 | 10.7 ± 0.6 | 10.7 ± 0.5 |
| Parathyroid hormone | 116 ± 119 | 122 ± 132 | 125 ± 143 |
| 18F-fluorocholine–positive for adenoma* | 94 (96) | 75 (97) | 58 (97) |
| Surgical results | |||
| Adenoma found at surgery | NA | 75 (97) | 58 (97) |
| Biochemical cure after surgery | NA | 63 (85)† | 48 (84)† |
Positive determined by consensus of masked readers.
3 patients had no follow-up laboratory values available for review.
NA = not applicable.
Data are number followed by percentage in parentheses unless otherwise noted.
18F-Fluorocholine PET Accuracy Compared with Pathologic Analysis
Seventy-seven of the 98 patients (79%) subsequently underwent parathyroidectomy an average of 85 ± 66 d after 18F-fluorocholine PET imaging. At surgery, 75 patients had an adenoma removed, and 65 patients (87%) had biochemical cure after surgery. During surgery, 56 patients underwent targeted unilateral minimally invasive surgery based on the findings from 18F-fluorocholine PET. Of the 21 patients who underwent bilateral neck exploration, 14 were due to bilateral lesions seen on 18F-fluorocholine PET, 3 were unplanned and due to an insufficient drop in parathyroid hormone when the adenoma visualized on the 18F-fluorocholine PET was removed, 2 were planned because of negative 18F-fluorocholine PET findings, and 2 were for removal of goiter.
Of the 12 patients who did not have evidence of biochemical cure, 5 had persistently elevated laboratory values after surgery, 4 had no laboratory follow-up, and 3 were found to have parathyromatosis. In the first patient who had no cure, 2 hypercellular adenomas were removed at the time of surgery, but a known mediastinal adenoma was knowingly left in place. In the second patient without cure, a hypercellular adenoma seen on 18F-fluorocholine PET was removed, but the hypercalcemia persisted and a repeat surgery removed a second adenoma also seen on the original 18F-fluorocholine PET study. In the third patient without cure, the adenoma on 18F-fluorocholine PET was determined histopathologically to be hypercellular but the hypercalcemia persisted. In the fourth patient without cure, the adenoma seen on 18F-fluorocholine PET was determined histopathologically to be normal, and a hypercellular adenoma on the opposite side was removed at surgery, but again the hypercalcemia persisted. In the fifth patient without cure, no adenoma was removed at surgery, and the adenoma seen on 18F-fluorocholine PET was believed to have been missed and was subsequently successfully removed at repeat surgery. Separately, 1 additional patient had no adenoma found on pathologic analysis although a lesion was seen on 18F-fluorocholine PET, and laboratory values had normalized by the time of follow-up.
Ninety-seven percent (75/77) of the imaging studies were read as positive by consensus masked readings. On the basis of local readings, the adenomas were correctly localized in 52 patients, with 20 false-positive and 5 false-negative patients, resulting in a CLR of 68% (95% CI, 57%–77%). On the basis of the consensus of the 3 masked readers, the adenomas were correctly localized in 56 patients, with 16 false-positive and 4 false-negative patients, resulting in a CLR of 74% (95% CI, 63%–82%). The CLRs of the 3 readers were 74% (95% CI, 63%–82%), 64% (95% CI, 53%–74%), and 64% (95% CI, 53%–74%). Of 20 false-positives based on local readings, 5 were true-positive in 1 region and false-positive in a separate region.
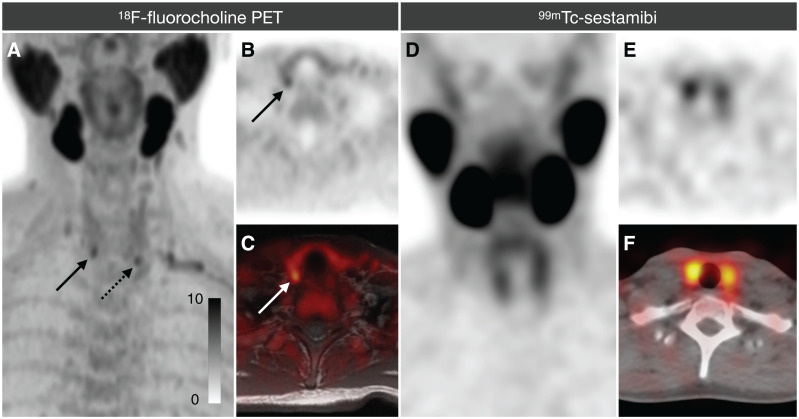
18F-Fluorocholine PET Compared with 99mTc-Sestamibi Imaging
Seventy-three patients also underwent 99mTc-sestamibi imaging; of these, 60 underwent both 99mTc-sestamibi imaging and 18F-fluorocholine PET within 12 mo of one another and subsequently underwent parathyroidectomy. 18F-fluorocholine PET outperformed 99mTc-sestamibi imaging for the detection of parathyroid adenomas (Table 2; Fig. 2). On the basis of local readings, the CLR increased from 25% (95% CI, 17%–36%) with 99mTc-sestamibi imaging to 75% (95% CI, 64%–83%) with 18F-fluorocholine PET. On the basis of the 3 masked readings, the CLR increased from 17% (95% CI, 10%–27%) with 99mTc-sestamibi imaging to 70% (95% CI, 59%–79%) with 18F-fluorocholine PET (Table 2).
TABLE 2.
Comparison of PET Results in Patients Who Underwent Both 99mTc-Sestamibi Imaging and 18F-Fluorocholine PET as Well as Surgery
| Finding | 99mTc-sestamibi | 18F-fluorocholine | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Local | R1 | R2 | R3 | Cons | Local | R1 | R2 | R3 | Cons | |
| Correct localization | 15 | 8 | 10 | 15 | 10 | 52 | 44 | 37 | 40 | 42 |
| False-positive | 8 | 1 | 3 | 6 | 3 | 13 | 13 | 19 | 15 | 15 |
| False-negative | 36 | 49 | 46 | 38 | 46 | 4 | 3 | 4 | 5 | 3 |
| True-negative | 1 | 2 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |
| CLR | 25% | 14% | 17% | 25% | 17% | 75% | 73% | 62% | 67% | 70% |
R1 = reader 1; R2 = reader 2; R3 = reader 3; Cons = consensus interpretation.
In local readings, CLR increased from 25% to 75%, and in 3 masked readings, CLR increased from 17% to 70%.
FIGURE 2.
Example patient who underwent both 18F-fluorocholine PET and 99mTc-sestamibi imaging. (A–C) 18F-fluorocholine PET was correctly localized by all 3 readers as positive on both right (solid arrows) and left (dotted arrow). (D–F) 99mTc-sestamibi imaging study (which included immediate and 2-h SPECT, although only 2-h is shown) was called negative by all 3 readers. At parathyroidectomy, both lesions seen on 18F-fluorocholine PET were confirmed to be parathyroid adenomas. A = PET maximum-intensity projection (MIP); B = PET axial; C = PET fused; D = SPECT MIP; E = SPECT axial; F = fused SPECT.
Reader Agreement
For 18F-fluorocholine PET, the interreader agreement was substantial for the left neck (κ = 0.75; 95% CI, 0.66–0.83) and right neck (κ = 0.64; 95% CI, 0.54–0.73) and was moderate for other locations (κ = 0.50; 95% CI, 0.40–0.60). Across all 3 regions, the interreader agreement for 18F-fluorocholine PET was substantial, with a κ of 0.71 (95% CI, 0.66–0.76). For 99mTc-sestamibi imaging, the interreader agreement was moderate for the left neck (κ = 0.47; 95% CI, 0.37–0.58) and right neck (κ = 0.47; 95% CI, 0.36–0.57) and was fair for other locations (κ = 0.32; 95% CI, 0.22–0.42). Across all 3 regions, the interreader agreement for 99mTc-sestamibi imaging was moderate, with a κ of 0.47 (95% CI, 0.41–0.53).
Safety
All patients were evaluated for potential adverse events. There were no reported adverse events from any patient.
DISCUSSION
In this prospective study of the largest cohort of PHPT patients in the United States to undergo 18F-fluorocholine PET for preoperative localization, the CLR for the detection of parathyroid adenomas was higher for 18F-fluorocholine PET than for 99mTc-sestamibi imaging. This result supports the use of 18F-fluorocholine PET for the localization of parathyroid adenomas in patients with PHPT.
Published studies on 18F-fluorocholine PET report sensitivities ranging from 81% to 100% and specificities of 95%–100% (16). Our analysis focused on the CLR, which is more stringent than patient-level sensitivity—an index for which identification of any true-positive region would convert a study to true-positive. Using conventional sensitivity analysis, 18F-fluorocholine PET in this study would have had a sensitivity of 98%, 98%, and 95% for each of the 3 readers for the 60 patients who underwent 99mTc-sestamibi imaging and 18F-fluorocholine PET. The CLR approach minimizes the benefit of overcalling lesions during interpretation, providing a better representation of the ability of the study to direct minimally invasive surgery.
Better preoperative localization is likely to increase the number of PHPT patients definitively treated with surgery. Patients with negative imaging results are less likely to be referred to a surgeon and, even when referred, remain less likely to undergo parathyroidectomy (17). The benefits of parathyroidectomy are well established, including decreased risk of bone fracture and kidney stones (2,3) and better quality of life (18). Parathyroidectomy is more cost-effective than medical management (19), even in mild or asymptomatic PHPT.
This study was performed using imaging with PET/MRI rather than PET/CT. MRI has a role in diagnosing parathyroid adenomas, and in particular, dynamic images of the neck after contrast administration can be helpful to characterize parathyroid adenomas because of the early, brisk enhancement (20). The use of MRI for this study was applied only for anatomic localization, and dynamic contrast-enhanced images were not acquired. In our first work using PET/MRI in this setting, we used contrast medium and did not find that it added significantly to the 18F-fluorocholine PET results (21); we therefore limited our MRI protocol to unenhanced T1- and T2-weighted imaging.
One of the strengths of our study was that the imaging studies were interpreted using both local and 3 masked readings, which limits the bias present in many retrospective studies that use single readers at the same institution as where the imaging studies were performed. Although none of the 3 masked readers had experience interpretating 18F-fluorocholine PET studies at their individual institutions, the interreader agreement was substantial for 18F-fluorocholine PET interpretation. Nonetheless, there is a small learning curve required, particularly in regard to the low level of uptake seen in cervical lymph nodes. Additionally, our study was prospective and included sequential patients. This was the first study to examine 18F-fluorocholine PET for PHPT on a large scale in North America.
Our study had several limitations. First, the 99mTc-sestamibi studies were not all performed on site and had heterogeneous techniques. Of the 77 99mTc-sestamibi studies evaluated, 63 were performed with SPECT/CT, 8 with SPECT, and 6 with planar imaging.
Second, our study did not compare the performance of 18F-fluorocholine PET with all other parathyroid imaging modalities, such as ultrasound and 4-dimensional CT; instead, we chose 99mTc-sestamibi imaging as the most appropriate comparator because of its widespread use and its commonality with 18F-fluorocholine PET as a nuclear medicine–based imaging tool. We anticipate that future studies will examine in greater detail the relative accuracy and role of 18F-fluorocholine PET in the current armamentarium of parathyroid imaging options.
Third, 21 patients in our cohort did not undergo surgical parathyroidectomy after imaging with 18F-fluorocholine PET. There are many reasons, including patient preference, but there is concern that a reason for forgoing surgery was a negative 18F-fluorocholine PET result. The rate of positive 18F-fluorocholine PET results was lower in the nonsurgery group (81% vs. 97%), although that only represents 4 patients with negative 18F-fluorocholine PET results who did not undergo surgery.
Fourth, long-term biochemical cure of PHPT is traditionally assessed by measuring serum calcium and parathyroid hormone levels at 6 mo after surgery, an interval that was beyond the time scope of our current study (we are accruing these long-term data for a future report). However, we believe the postoperative biochemical data we obtained, when interpreted together with the pathology results, provide robust evidence of the efficacy of 18F-fluorocholine PET in the localization of parathyroid tumors that can be targeted for subsequent surgical removal.
Fifth, our study evaluated a large number of patients without localization on ultrasound or 99mTc-sestamibi imaging—patients who do not reflect the overall population with PHPT. There were several sources for this bias. First, our institution serves as a referral center for parathyroidectomies, and our population reflects a cohort in which localization is more difficult. Second, patients without localization on 99mTc-sestamibi imaging or ultrasound were preferentially sent for advanced imaging using 18F-fluorocholine PET. Third, 42% of our study population had undergone a previous parathyroidectomy, and both ultrasound and 99mTc-sestamibi imaging are less accurate in the reoperative setting than in primary disease (22). Our complex cohort likely resulted in the unusually low (significantly lower than in previous studies) CLR for 99mTc-sestamibi imaging (25%, based on local readings). Considering that our study population in whom 18F-fluorocholine PET demonstrated excellent accuracy was highly enriched for those with more complex clinical scenarios, we hypothesize that 18F-fluorocholine PET performed in the broader population of PHPT patients would localize at an even higher rate.
CONCLUSION
Our study demonstrated that in a cohort of PHPT patients, 18F-fluorocholine PET outperformed 99mTc-sestamibi imaging. In a consensus interpretation by centrally masked readers, the CLR increased from 17% for 99mTc-sestamibi imaging to 70% for 18F-fluorocholine PET. These results support the use of 18F-fluorocholine PET for the localization of parathyroid adenomas in patients with PHPT.
DISCLOSURE
Thomas Hope receives institutional research funding from Advanced Accelerator Applications and Philips and is a consultant for Curium. Julie Sosa is a member of the Data Monitoring Committee of the Medullary Thyroid Cancer Consortium Registry supported by GlaxoSmithKline, Novo Nordisk, Astra Zeneca, and Eli Lilly. She receives institutional research funding from Exelixis and Eli Lilly. Insoo Suh is a consultant for Prescient Surgical, Medtronic, and Gerson Lehman Group. Thomas Hope is supported by the National Cancer Institute (R01CA212148, R01CA229354, and R01CA235741). Carolyn Seib (R03AG060097) and Insoo Suh (R43AG066230) are supported by the National Institute on Aging. No other potential conflict of interest relevant to this article was reported.
KEY POINTS
QUESTION: Is 18F-fluorocholine PET superior to 99mTc-sestamibi imaging for the localization of parathyroid adenomas?
PERTINENT FINDINGS: In this prospective study using 3 masked readers, 18F-fluorocholine PET had a 70% CLR, compared with 17% for 99mTc-sestamibi imaging.
IMPLICATIONS FOR PATIENT CARE: 18F-fluorocholine PET is superior to 99mTc-sestamibi imaging for the localization of parathyroid adenomas.
REFERENCES
- 1. VanderWalde LH, Liu I-LA, O’Connell TX, Haigh PI. The effect of parathyroidectomy on bone fracture risk in patients with primary hyperparathyroidism. Arch Surg. 2006;141:885–889. [DOI] [PubMed] [Google Scholar]
- 2. Yeh MW, Zhou H, Adams AL, et al. The relationship of parathyroidectomy and bisphosphonates with fracture risk in primary hyperparathyroidism: an observational study. Ann Intern Med. 2016;164:715–723. [DOI] [PubMed] [Google Scholar]
- 3. Mollerup CL, Vestergaard P, Frøkjaer VG, Mosekilde L, Christiansen P, Blichert-Toft M. Risk of renal stone events in primary hyperparathyroidism before and after parathyroid surgery: controlled retrospective follow up study. BMJ. 2002;325:807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pasieka JL, Parsons L, Jones J. The long-term benefit of parathyroidectomy in primary hyperparathyroidism: a 10-year prospective surgical outcome study. Surgery. 2009;146:1006–1013. [DOI] [PubMed] [Google Scholar]
- 5. Westerdahl J, Bergenfelz A. Unilateral versus bilateral neck exploration for primary hyperparathyroidism: five-year follow-up of a randomized controlled trial. Ann Surg. 2007;246:976–980. [DOI] [PubMed] [Google Scholar]
- 6. Sackett WR, Barraclough B, Reeve TS, Delbridge LW. Worldwide trends in the surgical treatment of primary hyperparathyroidism in the era of minimally invasive parathyroidectomy. Arch Surg. 2002;137:1055–1059. [DOI] [PubMed] [Google Scholar]
- 7. Kim S-J, Lee S-W, Jeong S-Y, Pak K, Kim K. Diagnostic performance of F-18 fluorocholine PET/CT for parathyroid localization in hyperparathyroidism: a systematic review and meta-analysis. Horm Cancer. 2018;9:440–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ishizuka T, Kajita K, Kamikubo K, et al. Phospholipid/Ca2+-dependent protein kinase activity in human parathyroid adenoma. Endocrinol Jpn. 1987;34:965–968. [DOI] [PubMed] [Google Scholar]
- 9. Lezaic L, Rep S, Sever MJ, Kocjan T, Hocevar M, Fettich J. 18F-fluorocholine PET/CT for localization of hyperfunctioning parathyroid tissue in primary hyperparathyroidism: a pilot study. Eur J Nucl Med Mol Imaging. 2014;41:2083–2089. [DOI] [PubMed] [Google Scholar]
- 10. Quak E, Blanchard D, Houdu B, et al. F18-choline PET/CT guided surgery in primary hyperparathyroidism when ultrasound and MIBI SPECT/CT are negative or inconclusive: the APACH1 study. Eur J Nucl Med Mol Imaging. 2018;45:658–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Christakis I, Khan S, Sadler GP, Gleeson FV, Bradley KM, Mihai R. 18Fluorocholine PET/CT scanning with arterial phase-enhanced CT is useful for persistent/recurrent primary hyperparathyroidism: first UK case series results. Ann R Coll Surg Engl. 2019;101:501–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kluijfhout WP, Pasternak JD, Gosnell JE, et al. 18F fluorocholine PET/MR imaging in patients with primary hyperparathyroidism and inconclusive conventional imaging: a prospective pilot study. Radiology. 2017;284:460–467. [DOI] [PubMed] [Google Scholar]
- 13. DeGrado TR, Baldwin SW, Wang S, et al. Synthesis and evaluation of 18F-labeled choline analogs as oncologic PET tracers. J Nucl Med. 2001;42:1805–1814. [PubMed] [Google Scholar]
- 14. Rosset A, Spadola L, Ratib O, Osiri X. An open-source software for navigating in multidimensional DICOM images. J Digit Imaging. 2004;17:205–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Landis JR, Koch GG. An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics. 1977;33:363–374. [PubMed] [Google Scholar]
- 16. Boccalatte LA, Higuera F, Gómez NL, et al. Usefulness of 18F-fluorocholine positron emission tomography-computed tomography in locating lesions in hyperparathyroidism: a systematic review. JAMA Otolaryngol Head Neck Surg. 2019;145:743–750. [DOI] [PubMed] [Google Scholar]
- 17. Wu S, Hwang SS, Haigh PI. Influence of a negative sestamibi scan on the decision for parathyroid operation by the endocrinologist and surgeon. Surgery. 2017;161:35–43. [DOI] [PubMed] [Google Scholar]
- 18. Ambrogini E, Cetani F, Cianferotti L, et al. Surgery or surveillance for mild asymptomatic primary hyperparathyroidism: a prospective, randomized clinical trial. J Clin Endocrinol Metab. 2007;92:3114–3121. [DOI] [PubMed] [Google Scholar]
- 19. Zanocco KA, Wu JX, Yeh MW. Parathyroidectomy for asymptomatic primary hyperparathyroidism: a revised cost-effectiveness analysis incorporating fracture risk reduction. Surgery. 2017;161:16–24. [DOI] [PubMed] [Google Scholar]
- 20. Kluijfhout WP, Venkatesh S, Beninato T, et al. Performance of magnetic resonance imaging in the evaluation of first-time and reoperative primary hyperparathyroidism. Surgery. 2016;160:747–754. [DOI] [PubMed] [Google Scholar]
- 21. Kluijfhout WP, Pasternak JD, Gosnell JE, et al. 18F fluorocholine PET/MR imaging in patients with primary hyperparathyroidism and inconclusive conventional imaging: a prospective pilot study. Radiology. 2017;284:460–467. [DOI] [PubMed] [Google Scholar]
- 22. Parikh AM, Grogan RH, Morón FE. Localization of parathyroid disease in reoperative patients with primary hyperparathyroidism. Int J Endocrinol. 2020;2020:9649564. [DOI] [PMC free article] [PubMed] [Google Scholar]