Abstract
Objective:
To synthesize evidence on the impact of malocclusion and its associated treatment on people's quality of life across studies that used the Oral Health Impact Profile (OHIP-14) questionnaire in the adult population.
Materials and Methods:
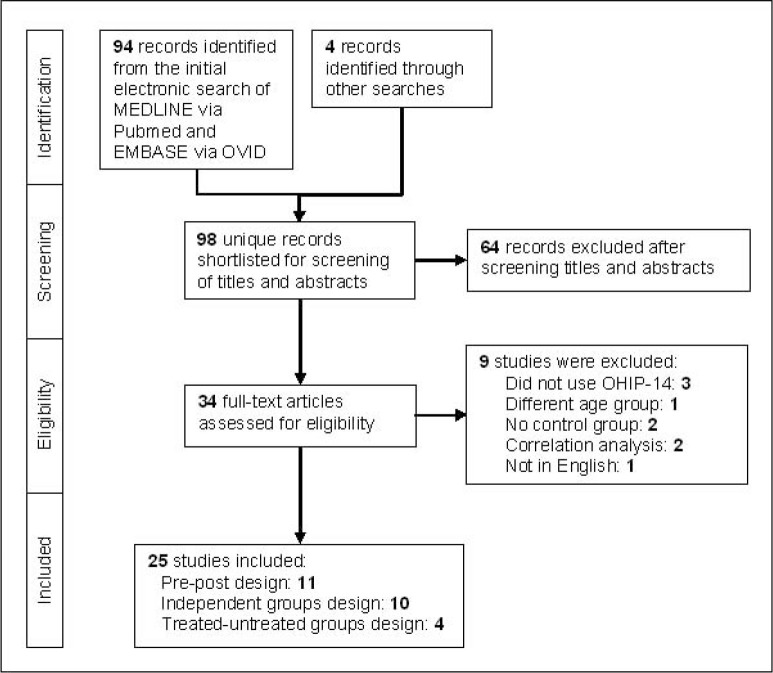
A systematic search of the English literature using Medline, PubMed, and EMBASE yielded 98 unique citations. Studies using OHIP-14 with individuals 15 years of age and older were included. After initial screening, 64 citations were excluded and another 9 were excluded after reading full text reports; the remaining 25 were included in the review. All studies were observational and used one of three study designs: 11 compared the same group before and after treatment (pre-post design), 10 compared groups with and without malocclusion (independent groups design) and four compared an orthodontically treated group with an independent group requiring treatment (treated-untreated groups design). Only three studies using the pre-post design and four using the independent groups design reported comparable OHIP-14 data and were combined in separate meta-analyses. Meta-analysis was carried out using metan command in Stata.
Results:
The standardized mean difference (SMD) in OHIP-14 total score was 1.29 (95% CI: 0.67 to 1.92) for the three studies using the pre-post design. Similarly, the SMD score was 0.84 (95% CI: 0.25 to 1.43) for the four studies using the independent groups design. There was evidence of high heterogeneity and publication bias among the studies included.
Conclusions:
This meta-analysis revealed that OHIP-14 scores were significantly lower after receiving treatment for malocclusion and in individuals without malocclusion/orthodontic treatment need compared to those with such condition (independent groups).
Keywords: Malocclusion, Orthodontic treatment, Oral health related quality of life, Review
INTRODUCTION
Evidence on the physical, psychological, and social consequences of malocclusion and its associated treatment as they relate to quality of life is still conflicting.1–3 Although studies generally report an association between malocclusion/orthodontic treatment need and oral health–related quality of life (OHRQoL) scores, the strength of evidence is relatively low, and there is a need for using standardized methods to enhance comparability.1,3 Focusing on studies that used the same OHRQoL instrument may help in comparing findings across studies and even synthesizing the evidence quantitatively.
Though various instruments are available to measure people's OHRQoL, the Oral Health Impact Profile (OHIP) has been widely used due to its good psychometric properties.4 As the original version of the OHIP questionnaire has 49 questions (OHIP-49), it was later considered time-consuming to complete. To overcome this shortcoming, a shorter version with 14 items was derived from the original questionnaire (OHIP-14).5 The OHIP-14 is considered a more practical instrument in clinical practice and epidemiological surveys and has also shown good reliability and validity.6 Each of the 14 items contained in the instrument can be scored with the scale of 0 to 5. The score 0 refers to good quality of life and 5 refers to worst. Hence, the total score ranges from 0 to 70.
The aim of this study was to synthesize the evidence on the impact of malocclusion and its associated treatment on people's quality of life using studies that used the OHIP-14 questionnaire among the individuals of 15 years of age and above.
MATERIALS AND METHODS
Search Strategy for Identification of Studies
We sought to identify all studies exploring the impact of malocclusion and its associated treatment on people's quality of life, published until November 2013. To identify relevant English studies, MEDLINE and EMBASE via OVID and PubMed were electronically searched. The search strategies included a combination of medical subject heading (MeSH) terms and text words around two main subjects: the exposure (malocclusion or its associated treatment) and outcome (OHRQoL). The MeSH terms were “Malocclusion,” “Orthodontics,” “Orthognathic Surgery,” and “quality of life” and the keywords were orthod*, orthogn*, malocclus*, Oral Health Impact Profile, OHIP, and quality of life. Electronic search strategies were supplemented by hand search of the reference lists of all relevant publications and the most recent related review articles in order to identify additional undetected published studies.
Criteria for Inclusion of Studies
Predefined criteria were applied to select the final list of intervention and/or observational studies to be included in the review. The inclusion criteria used for this review were:
population: individuals aged 15 years and above;
intervention/exposure: either malocclusion (determined via clinical examination) or its associated treatment (ie, orthodontic therapy or orthognathic surgery);
comparison: a control group of individuals without malocclusion (for assessing the impact of malocclusion) or a control group of individuals requiring either orthodontic treatment or orthognathic surgery (for assessing the impact of the treatment of malocclusion, before and after treatment); and
outcome: OHRQoL measured using the short-version of the OHIP, OHIP-14.
The exclusion criteria were:
studies carried out with children or adolescents (below the age of 15);
letters to editors, unpublished articles, case reports, case series, and reviews;
studies published in languages other than English;
duplicate studies (studies originating from the same subjects by the same investigators but published in different journals); and
articles providing no information on sample size, mean, or standard deviation for the OHIP-14 total score, or insufficient information for their calculation.
Data Extraction and Validity Assessment Procedure
Two reviewers performed independent searches, assessed the quality of the included studies, and extracted the data in duplicate. Records of all references were combined in EndNote X4 (Thomas Reuters, Philadelphia, Pa). Differences were resolved by discussion and/or rereading. The titles and abstracts obtained from initial electronic searches were screened for relevance. For studies meeting the inclusion criteria, or for which there was insufficient data in the title and abstract to make a clear decision, the full report was obtained and assessed to establish whether they met the inclusion criteria. Studies rejected at this or subsequent stages were recorded in the table of excluded studies, and reasons for exclusion were noted. The full text of all topic-related studies was assessed for methodologic quality using the STROBE checklists.7,8
General bibliographic information as well as key methodologic characteristics (author, year of publication, study design, and methods used) and relevant results (number of samples used, mean score, and standard deviation for the two groups—with and without malocclusion or with and without treatment) were extracted from all included studies.
Statistical Methods
Descriptive statistics were used to summarize the study characteristics. A meta-analysis was performed using the metan command in Stata version 11.2 (StataCorp, College Station, Tex). As the studies selected in this analysis were carried out in different countries and populations, between-study variations were assumed a priori. Hence, random effect models were used in the meta-analysis, which takes into account both within- and between-study variations in effect sizes. To test whether there was more heterogeneity in the data than the chance, Q test was used. The heterogeneity measure I2 was also calculated to measure the percentage of heterogeneity in the data. Both the Begg and Egger tests were used to measure the bias due to small study effects in our data. Funnel plots were used to assess the publication bias visually.
RESULTS
Study Characteristics
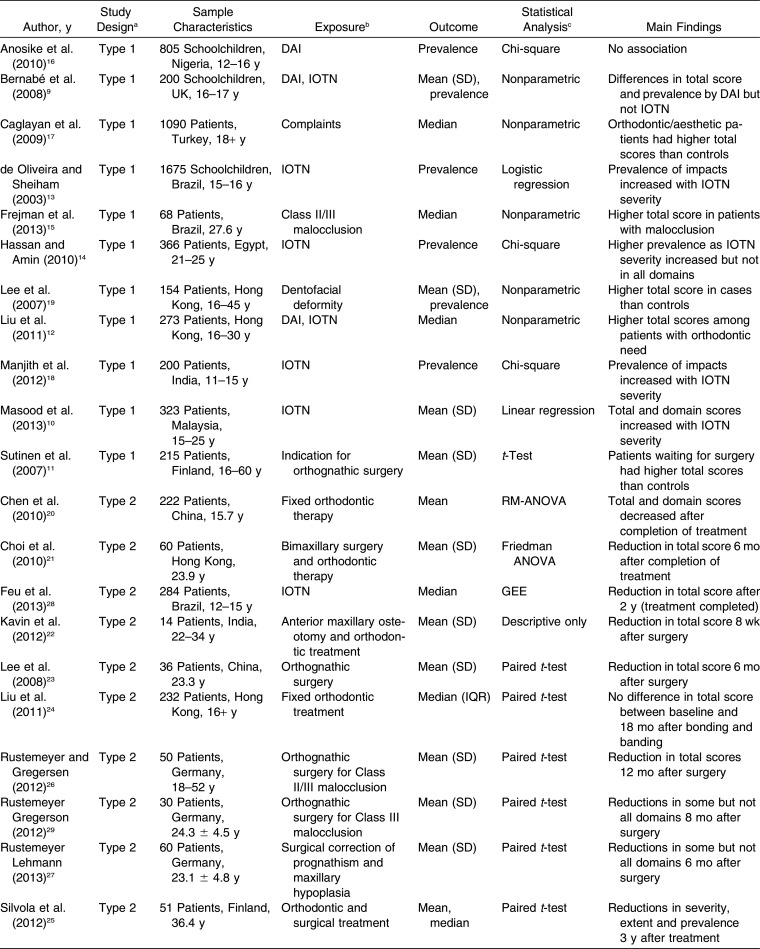
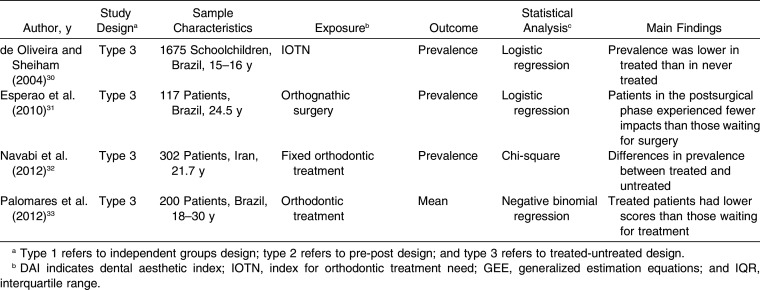
A flowchart describing the systematic review search results is presented in Figure 1. The search yielded 98 unique citations. After screening titles and abstracts, 64 citations were excluded as clearly not relevant to this systematic review, leaving 34 for full-text review. Nine studies were further excluded after reading their full text reports; the remaining 25 were assessed for their methodologic quality. Table 1 summarizes the key methodological aspects and findings of the 25 studies included in this review. All 25 studies were observational and were organized into three groups according to the type of comparisons made: (1) 11 studies9–19 comparing groups with and without malocclusion/orthodontic treatment need (independent groups design), (2) 10 studies20–29 comparing the same group of individuals before and after treatment (labelled as pre-post design), and (3) four studies30–33 comparing an orthodontically treated group with an independent group requiring treatment (treated-untreated groups design).
Figure 1.
Flowchart of the selection of studies for the review.
Table 1. .
Characteristics of the Studies on the Association of Malocclusion and Its Associated Treatment With OHIP-14a,b
Table 1. .
Continued
Findings From Meta-analysis
Among the studies that used OHIP-14, only a few used the same type and details of reporting. Only eight of the 25 studies included in the review (32%) provided information on the OHIP-14 mean and standard deviation as well as the sample size of the groups compared, namely three of the 11 using the pre-post design, four of the 10 using the independent groups design, and one of the four using the treated-untreated groups design (Table 1). The three and four studies in the first and second study designs were amenable to meta-analysis. The remaining 18 studies were excluded from the meta-analysis. Figure 2 depicts the results of the two meta-analyses. The contribution of each study to the meta-analysis is given as a percentage of weight. For the four studies that used the pre-post study design, the standardized mean difference (SMD) was 1.29 (95% CI: 0.67 to 1.92), indicating that the OHIP-14 score decreased after treatment. Similarly, for the three studies that used the independent groups study design, the SMD was 0.84 (95% CI: 0.25 to 1.43), indicating that people without malocclusion had lower OHIP-14 scores compared with their counterparts. The mean SMD score was significantly different from 0 in both cases (P < .001 and .005, respectively). The studies involved in each meta-analysis were heterogeneous and the heterogeneity was statistically significant (P = .047 and <.001 for the first and second meta-analysis, respectively). The variations in SMD measured as a percentage (I2) were 67.2% (pre-post study design) and 91.6% (independent group study design). The between-study variance was 0.20 and 0.34 for the pre-post and independent-group study designs, respectively.
Figure 2.
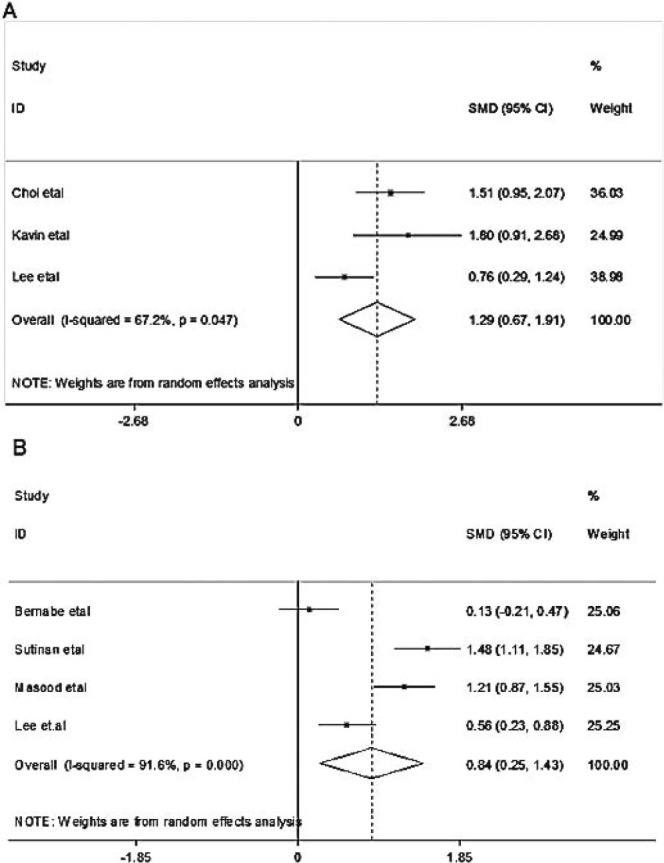
Forest plot depicting the standardized mean difference (SMD) and its 95% confidence interval for (A) studies comparing the same group before and after treatment (pre-post study design) and (B) studies comparing groups with and without malocclusion (independent group study design).
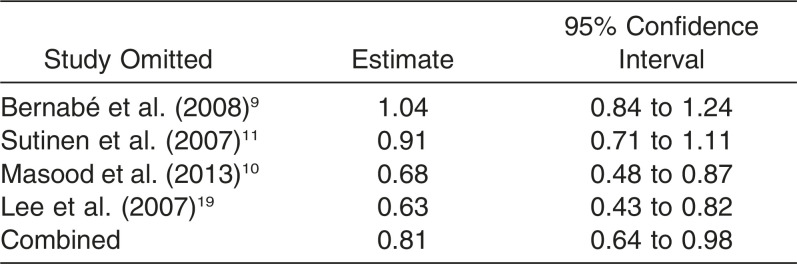
Bias due to small study effect was tested using Begg's test and Egger's test. The two tests showed no evidence of bias (P = .30 and .43 for the pre-post study design and 0.31 and 0.32 for the independent group study design, respectively). Publication bias was assessed using funnel plots with 95% pseudo CI (Figure 3). There was no evidence of publication bias in the first meta-analysis, whereas there was evidence of publication bias in the second meta-analysis. Hence, further trimming was performed for the independent-group study design to adjust for publication bias (Table 2). The sensitivity analysis indicated that the omission of any of the studies led to a new estimate of 0.81 (95% CI: 0.25 to 1.43).
Figure 3.
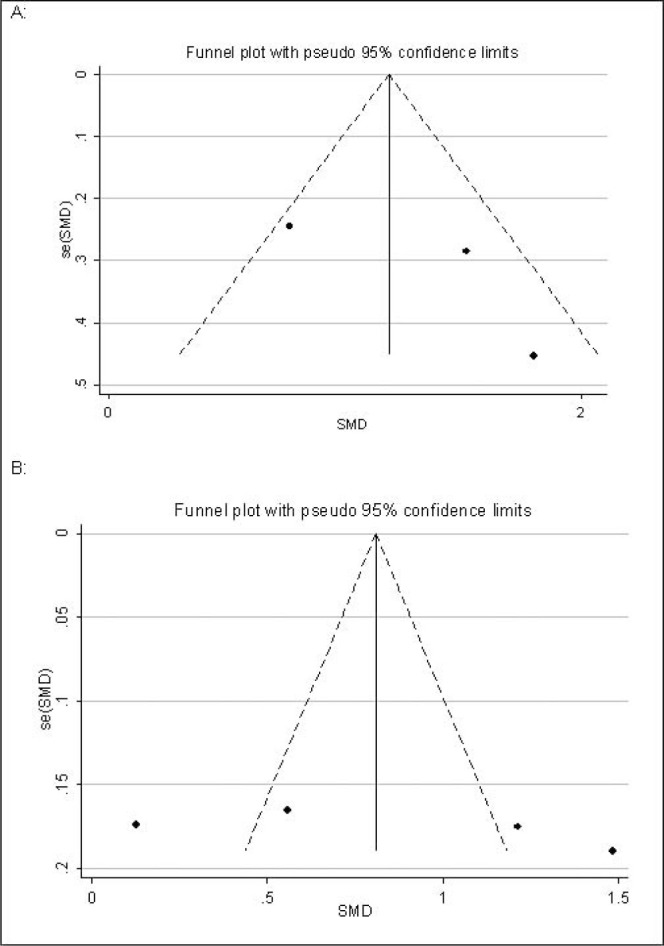
Funnel plot for evaluation of publication bias for (A) studies comparing the same group before and after treatment (pre-post study design) and (B) studies comparing groups with and without malocclusion (independent group study design).
Table 2. .
Sensitivity Analysis for the Meta-Analysis of Studies Comparing Groups With and Without Malocclusion (Independent Groups Study Design)
DISCUSSION
Our review revealed no high-quality studies on the association of malocclusion (longitudinal studies) or its associated treatment (randomized controlled trials) with OHIP-14 scores. Most evidence is cross-sectional and based on reduced samples of individuals. However, evidence from these studies suggests that OHIP-14 scores were significantly lower after receiving treatment for malocclusion (pre-post design), indicating that the quality of life has improved and in individuals without malocclusion/orthodontic treatment need compared to those with such condition (independent groups design). The pooled SMD from the three studies that used the pre-post design was 1.29 (95% CI: 0.67 to 1.92,) whereas the pooled SMD from the four studies that used the independent groups design was 0.84 (95% CI: 0.25 to 1.43). The two values indicate large effects according to the Cohen (1988) benchmark values of small (0.20), moderate (0.50), and large (0.80) effects.34 However, they should be taken with certain caution as they came from studies with no parallel control group or follow-up assessment (ie, for the pre-post and independent groups design, respectively).
Furthermore, our two meta-analyses revealed high levels of heterogeneity among the studies, meaning that findings varied widely between the populations and countries where the primary studies were conducted. The meta-analyses also revealed the presence of publication bias in these published papers, which needs to be addressed. All studies but one9 included in the meta-analyses reported significant differences in OHIP-14 total scores between groups, but previous reviews (not focusing exclusively on the above instrument) have found conflicting results.1–3
Our review highlights some areas for further improvement in this research field. First, despite identifying 25 studies for this review, none used the best study design (either a randomized controlled trial for the impact of orthodontic/orthognathic treatment or a longitudinal study for the impact of malocclusion). Researchers have used three main types of study designs to assess the impact of malocclusion and its associated treatment on OHIP-14 total scores. Sadly, those choices will not provide the best evidence on this topic. There is, therefore, the necessity for more studies using appropriate designs to be carried out in this field in the future. Second, different studies follow different approaches when reporting OHRQoL using the OHIP-14 instrument. Seven studies using the pre-post design and four in the independent groups design did not report mean and standard deviation for the OHIP-14 total score and could not be used in the corresponding meta-analyses. As meta-analysis requires the summary statistics for each group considered in the study, lack of these statistics restricts the application of a meta-analysis in achieving its objectives.
Some limitations of this review need to be addressed. First, the results of any meta-analysis are highly reliable only if it is based on a large number of studies. However, the results of the present meta-analyses were based on three studies for the pre-post design and four studies for the independent groups design. This review and meta-analysis will need to be updated once more studies have been conducted. Second, our search was restricted to studies published in English only, and as such, some relevant evidence could have been omitted (language bias). Third, although we only combined findings from studies with the two strongest study designs among those available, they are not the best possible designs to assess the impact of malocclusion and its associated treatment on quality of life. Also, as the impact of malocclusion on quality of life may differ between children and adults as adults look this in context with aesthetics apart from functional, comparison between these two populations will help the policy makers for better planning. However, the strength of this review is that it is the first attempt to use meta-analysis to elucidate the effect of treatment on oral health–related quality of life of patients of different groups by combining studies carried out across the world. The precision of the meta-analysis results could have been improved if the analysis included properly designed studies like clinical trials for the impact of orthodontic treatment and longitudinal studies for the impact of malocclusion.
CONCLUSIONS
This meta-analysis revealed that:
OHIP-14 scores were significantly lower after receiving treatment (indicating improvement in quality of life) for malocclusion (pre-post study design) and in individuals without malocclusion/orthodontic treatment need compared to those with such condition (independent groups study design).
There is a lack of standardization among studies in terms of study designs and reporting of OHIP-14 scores; hence, there is poor evidence on this topic.
REFERENCES
- 1.Zhang M, McGrath C, Hagg U. The impact of malocclusion and its treatment on quality of life: a literature review. Int J Paediatr Dent. 2006;16:381–387. doi: 10.1111/j.1365-263X.2006.00768.x. [DOI] [PubMed] [Google Scholar]
- 2.Kiyak HA. Does orthodontic treatment affect patients' quality of life. J Dent Educ. 2008;72:886–894. [PubMed] [Google Scholar]
- 3.Liu Z, McGrath C, Hägg U. The impact of malocclusion/ orthodontic treatment need on the quality of life. A systematic review. Angle Orthod. 2009;79:585–591. doi: 10.2319/042108-224.1. [DOI] [PubMed] [Google Scholar]
- 4.Slade GD, Spencer AJ. Development and evaluation of the impact profile oral health. Community Dent Health. 1994;11:3–11. [PubMed] [Google Scholar]
- 5.Slade GD. Derivation and validation of a shot-form oral heal impact profile. Community Dent Oral Epidemiol. 1997;25:284–290. doi: 10.1111/j.1600-0528.1997.tb00941.x. [DOI] [PubMed] [Google Scholar]
- 6.Locker D, Allen F. What do measures of ‘oral health-related quality of life’ measure. Community Dent Oral Epidemiol. 2007;35:401–411. doi: 10.1111/j.1600-0528.2007.00418.x. [DOI] [PubMed] [Google Scholar]
- 7.Mohr D, Hopewell S, Schulz KF, et al. CONSORT 2010 Explanation and Elaboration: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol. 2010;63:e1–37. doi: 10.1016/j.jclinepi.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 8.Vandenbroucke JP, Von Elm E, Altman DG, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Ann Intern Med. 2007;147:W163–194. doi: 10.7326/0003-4819-147-8-200710160-00010-w1. [DOI] [PubMed] [Google Scholar]
- 9.Bernabe E, Oliveira C, Sheiham A. Comparison of the discriminative ability of a generic and a condition-specific OHRQoL measure in adolescents with and without normative need for orthodontic treatment. Health Qual Life Outcomes. 2008;6:64. doi: 10.1186/1477-7525-6-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Masood Y, Masood M, Zainul NN, Araby NBAA, Hussain SF, Newton T. Impact of malocclusion on oral health related quality of life in young people. Health Qual Life Outcomes. 2013;11:25. doi: 10.1186/1477-7525-11-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sutinen S, Lahti S, Nuttall NM, et al. Effect of a 1-month vs. a 12-month reference period on responses to the 14-item Oral Health Impact Profile. Eur J Oral Sci. 2007;115:246–249. doi: 10.1111/j.1600-0722.2007.00442.x. [DOI] [PubMed] [Google Scholar]
- 12.Liu Z, McGrath C, Hägg U. Associations between orthodontic treatment need and oral health-related quality of life among young adults: does it depend on how you assess them. Community Dent Oral Epidemiol. 2011;39:137–144. doi: 10.1111/j.1600-0528.2010.00573.x. [DOI] [PubMed] [Google Scholar]
- 13.de Oliveira CM, Sheiham A. The relationship between normative orthodontic treatment need and oral health-related quality of life. Community Dent Oral Epidemiol. 2003;31:426–436. doi: 10.1046/j.1600-0528.2003.00002.x. [DOI] [PubMed] [Google Scholar]
- 14.Hassan AH, Amin Hel S. Association of orthodontic treatment needs and oral health-related quality of life in young adults. Am J Orthod Dentofacial Orthop. 2010;137:42–47. doi: 10.1016/j.ajodo.2008.02.024. [DOI] [PubMed] [Google Scholar]
- 15.Frejman MW, Vargas IA, Rosing CK, Closs LQ. Dentofacial deformities are associated with lower degrees of self-esteem and higher impact on oral health-related quality of life: results from an observational study involving adults. J Oral Maxillofac Surg. 2013;71:763–767. doi: 10.1016/j.joms.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 16.Anosike AN, Sanu OO, da Costa OO. Malocclusion and its impact on quality of life of school children in Nigeria. West Afr J Med. 2010;29:417–424. doi: 10.4314/wajm.v29i6.68298. [DOI] [PubMed] [Google Scholar]
- 17.Caglayan F, Altun O, Miloglu O, Kaya MD, Yilmaz AB. Correlation between oral health-related quality of life (OHQoL) and oral disorders in a Turkish patient population. Med Oral Patol Oral Cir Bucal. 2009;14:e573–578. doi: 10.4317/medoral.14.e573. [DOI] [PubMed] [Google Scholar]
- 18.Manjith CM, Karnam SK, Manglam S, Praveen MN, Mathur A. Oral Health-Related Quality of Life (OHQoL) among adolescents seeking orthodontic treatment. J Contemp Dent Pract. 2012;13:294–298. doi: 10.5005/jp-journals-10024-1140. [DOI] [PubMed] [Google Scholar]
- 19.Lee S, McGrath C, Samman N. Quality of life in patients with dentofacial deformity: a comparison of measurement approaches. Int J Oral Maxillofac Surg. 2007;36:488–492. doi: 10.1016/j.ijom.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 20.Chen M, Wang DW, Wu LP. Fixed orthodontic appliance therapy and its impact on oral health-related quality of life in Chinese patients. Angle Orthod. 2010;80:49–53. doi: 10.2319/010509-9.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Choi WS, Lee S, McGrath C, Samman N. Change in quality of life after combined orthodontic-surgical treatment of dentofacial deformities. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:46–51. doi: 10.1016/j.tripleo.2009.08.019. [DOI] [PubMed] [Google Scholar]
- 22.Kavin T, Jagadesan AGP, Venkataraman SS. Changes in quality of life and impact on patients' perception of esthetics after orthognathic surgery. J Pharm Bioallied Sci. 2012;4(suppl 2):S290–293. doi: 10.4103/0975-7406.100276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee S, McGrath C, Samman N. Impact of orthognathic surgery on quality of life. J Oral Maxillofac Surg. 2008;66:1194–1199. doi: 10.1016/j.joms.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 24.Liu Z, McGrath C, Hägg U. Changes in oral health-related quality of life during fixed orthodontic appliance therapy: an 18-month prospective longitudinal study. Am J Orthod Dentofacial Orthop. 2011;139:214–219. doi: 10.1016/j.ajodo.2009.08.029. [DOI] [PubMed] [Google Scholar]
- 25.Silvola AS, Rusanen J, Tolvanen M, Pirttiniemi P, Lahti S. Occlusal characteristics and quality of life before and after treatment of severe malocclusion. Eur J Orthod. 2012;34:704–709. doi: 10.1093/ejo/cjr085. [DOI] [PubMed] [Google Scholar]
- 26.Rustemeyer J, Gregersen J. Quality of life in orthognathic surgery patients: post-surgical improvements in aesthetics and self-confidence. J Craniomaxillofac Surg. 2012;40:400–404. doi: 10.1016/j.jcms.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 27.Rustemeyer J, Lehmann A. Reduction genioplasty enhances quality of life in female patients with prognathism and maxillary hypoplasia undergoing bimaxillary osteotomy. Int J Oral Maxillofac Surg. 2013;42:1083–1092. doi: 10.1016/j.ijom.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 28.Feu D, Miguel JAM, Celeste RK, Oliveira BH. Effect of orthodontic treatment on oral health-related quality of life. Angle Orthod. 2013;83:892–898. doi: 10.2319/100412-781.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rustemeyer J, Martin A, Gregersen J. Changes in quality of life and their relation to cephalometric changes in orthognathic surgery patients. Angle Orthod. 2012;82:235–241. doi: 10.2319/042211-285.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.De Oliveira CM, Sheiham A. Orthodontic treatment and its impact on oral health-related quality of life in Brazilian adolescents. J Orthod. 2004;31:20–27. doi: 10.1179/146531204225011364. discussion 15. [DOI] [PubMed] [Google Scholar]
- 31.Esperao PTG, Oliveira BH, Almeida MAO, Kiyak HA, Miguel JAM. Oral health-related quality of life in orthognathic surgery patients. Am J Orthod Dentofacial Orthop. 2010;137:790–795. doi: 10.1016/j.ajodo.2008.08.031. [DOI] [PubMed] [Google Scholar]
- 32.Navabi N, Farnudi H, Rafiei H, Tahmasbi Arashlow M. Orthodontic treatment and the oral health-related quality of life of patients. J Dent (Tehran) 2012;9:247–254. [PMC free article] [PubMed] [Google Scholar]
- 33.Palomares NB, Celeste RK, de Oliveira BH, Migueld JAM. How does orthodontic treatment affect young adults' oral health-related quality of life. Am J Orthod Dentofacial Orthop. 2012;141:751–758. doi: 10.1016/j.ajodo.2012.01.015. [DOI] [PubMed] [Google Scholar]
- 34.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]