Abstract
Objective:
To evaluate and compare intrapulpal temperature rise with three different light-curing units by using a study model simulating pulpal blood microcirculation.
Materials and Methods:
The roots of 10 extracted intact maxillary central incisors were separated approximately 2 mm below the cement-enamel junction. The crowns of these teeth were fixed on an apparatus for the simulation of blood microcirculation in pulp. A J-type thermocouple wire was inserted into the pulp chamber through a drilled access on the palatal surfaces of the teeth. Four measurements were made using each tooth for four different modes: group 1, 1000 mW/cm2 for 15 seconds; group 2, 1200 mW/cm2 for 10 seconds; group 3, 1400 mW/cm2 for 8 seconds; and group 4, 3200 mW/cm2 for 3 seconds. The tip of the light source was positioned at 2 mm to the incisor's labial surface.
Results:
The highest temperature rise was recorded in group 1 (2.6°C ± 0.54°C), followed by group 2 (2.57°C ± 0.62°C) and group 3 (2.35°C ± 0.61°C). The lowest temperature rise value was found in group 4 (1.74°C ± 0.52°C); this value represented significantly lower ΔT values when compared to group 1 and group 2 (P = .01 and P = .013, respectively).
Conclusions:
The lowest intrapulpal temperature rise was induced by 3200 mW/cm2 for 3 seconds of irradiation. Despite the significant differences among the groups, the temperature increases recorded for all groups were below the critical value of 5.6°C.
Keywords: Temperature rise, Microcirculation, Light-curing units, Bonding
INTRODUCTION
The use of light-curing (LC) resin adhesives for orthodontic bracket bonding was first described in 1979.1 These resins have advantages, such as offering an extended working time to place the attachments properly on the tooth surface or a shortened working time when a quick set is required—for example, in a case involving bonding an attachment onto an impacted tooth after surgical uncovering, with the attendant risks of bleeding and contamination.2
Polymerization of these resins can be accomplished by using different light sources. Initially, a halogen light source with a light intensity of approximately 400mW/cm2 was commonly used. Then higher intensity light sources have been developed in an attempt to achieve a deeper and more effective cure and to reduce chair time both for patients and clinicians.3 Recently, Cerekja and Cakirer4 reported that curing for 10 seconds with high-intensity LED (1200 ± 10 mW/cm2) and for 6 seconds with high-power halogen light (3000 mW/cm2) does not compromise the shear bond strength of metal brackets in vitro.
During the light-activated polymerization process of resin composites temperature increases as a result of the exothermic reaction process and energy absorption during irradiation.5 It has been proved that the pulp chamber is sensitive to physical, chemical, biological, and thermal changes. According to the findings of a study6 on rhesus monkeys, a 5.6°C temperature rise in the pulp chamber caused irreversible pulp damage in 15% of the monkeys, while 11°C and 16.6°C increases caused irreversible pulp damage, respectively, in 60% and 100% of the monkeys.
Pulp microcirculation is one of the important factors to consider in the regulation of intrapulpal temperature when heat is transferred by external thermal stimuli to the dentine-pulp complex.7,8 Therefore, lack of microcirculation may cause higher values in studies evaluating intrapulpal temperature changes. Kodonas et al.9 evaluated the rise in intrapulpal temperature induced by the application of various curing units ex vivo; in this study the authors tried to achieve water circulation inside the pulp chamber by injection of water into the chamber using a standard injector to evaluate the effect of fluid circulation in the chamber during curing light irradiation. The temperature rises produced by all curing units except the conventional halogen lamp were found to be high enough to be potentially harmful to the pulp when the simulated pulpal circulation was absent.
The aim of this in vitro study was to evaluate and compare intrapulpal temperature rise with four different light-curing modes using a study model simulating pulpal blood microcirculation.
MATERIALS AND METHODS
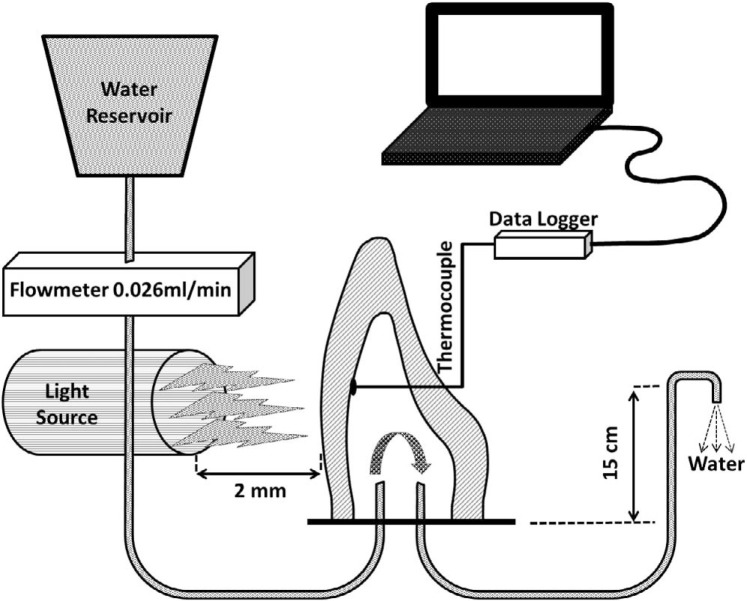
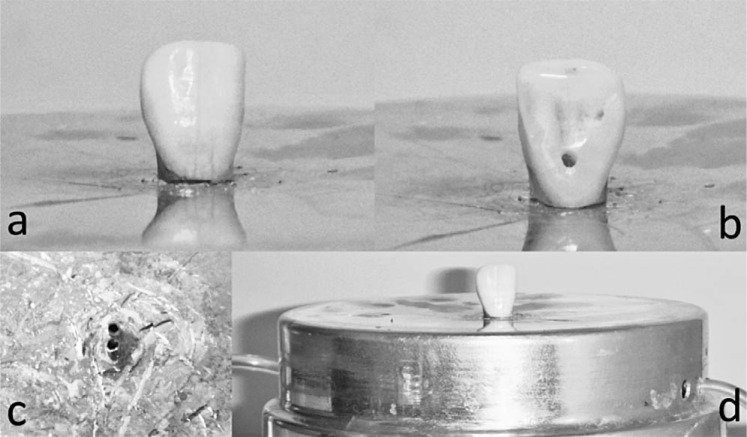
In this in vitro study, 10 extracted intact maxillary central incisors were used. The teeth were selected so that they had similar size and shape in order to provide homogeneity of enamel and dentin thickness among the group. The roots were separated approximately 2 mm below the cement-enamel junction perpendicular to the long axis of the teeth. The opening into the pulp chamber was enlarged and the pulp chamber was cleaned of remnant pulpal tissues with a spoon excavator. Pulpal blood microcirculation was simulated with an apparatus described in a previous study10 (Figure 1). This apparatus allows distilled water (at room temperature) to flow through the pulp chamber with a defined flow rate (0.026 mL/min) to simulate the pulpal vascular fluid flow. A digital infusion flowmeter (SK-600II infusion pump, SK Medical, Shenzhen, China) was integrated into the system for controlling flow rate. An access was drilled into the pulp chambers on the palatal surface of the crowns with a diamond bur. A 0.36-mm-diameter J-type thermocouple wire (Omega Engineering, Stamford, Conn) was inserted into the pulp chamber to contact the buccal wall of the pulp chamber. A silicone heat-transfer compound (ILC P/N 213414; Wakefield Engineering, Beverly, Mass) was applied to the tip of the thermocouple wire. To fix the thermocouple wire in the predrilled cavity, in order to maintain contact with the buccal wall of the pulp chamber and to seal the area for water leakage, a light-curing calcium hydroxide cement (Calcimol LC; Voco 158 GmbH, Cuxhaven, Germany) was applied. The thermocouple wire was connected a data logger (XR440-M Pocket Logger; Pace Scientific, Mooresville, NC), which is connected to a computer so that the temperature increase (ΔT °C) data from inside the pulp were recorded.10 The tip of the light source was positioned at 2 mm to the incisor's labial surface during the polymerization process. The study model is shown schematically in Figure 2.
Figure 1. .
Schematic drawing of temperature measurement apparatus.11
Figure 2. .
A sample incisor positioned on the temperature measurement apparatus (d); the buccal side of the incisor (a); the palatal side of the incisor, drilled to place the thermocouple (b); and the tips of the water circulation pipes on the apparatus (c).
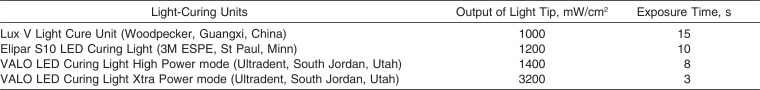
The same group of teeth (n = 10) was used to determine the temperature changes, and four measurements were made using each tooth. Four different curing modes of three different light-curing units were tested. The light sources and respective study groups were as follows: group 1, Lux V (Woodpecker, Guangxi, China) (1000 mW/cm2) for 15 seconds; group 2, Elipar S10 (3M ESPE, St Paul, Minn) (1200 mW/cm2) for 10 seconds; group 3, Valo (Ultradent, South Jordan, Utah) high-power mode (1400 mW/cm2) for 8 seconds; and group 4, Valo Xtra power mode (3200 mW/cm2) for 3 seconds (Table 1).
Table 1. .
The Light-Curing Units Used in the Present Study
Statistical Analysis
Descriptive statistics, including means, standard deviations, and minimum and maximum values, were calculated for each of the four groups. Analysis of variance (ANOVA) and the Tukey's honestly significant differences (HSD) tests (version 10.0, SPSS, Chicago, Ill) were used to analyze temperature changes between the groups at a significance level of P < .05.
RESULTS
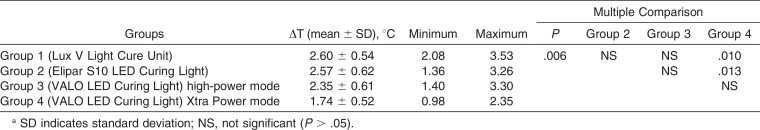
The mean pulp temperature change values (ΔT) and standard deviations are shown in Table 2. The highest temperature rise was recorded in group 1 (2.6°C ± 0.54°C), followed by group 2 (2.57°C ± 0.62°C) and group 3 (2.35°C ± 0.61°C). The lowest temperature rise value was found in group 4 (1.74°C ± 0.52°C).
Table 2. .
Descriptive Statistics and Multiple Comparisons of Groupsa
One-way ANOVA analysis showed that there is significant difference among the groups (P = .006) (Table 2).
According to the Tukey's HSD tests, group 4 presented significantly lower ΔT values compared to group 1 and group 2 (P = .01 and P = .013, respectively). There were no other significant differences in the pairwise comparisons (P > .05).
DISCUSSION
When the scientific breakthrough combined with innovation, various new high-intensity curing units and lasers were brought to market. Under certain circumstances, high-intensity units should be used with extreme care to avoid harm to the dentine-pulp complex.9 Thermal changes during the light-curing of composites are well documented in previous studies, but without taking the pulpal blood flow into consideration. Therefore, in this in vitro study intrapulpal temperature rise during polymerization of orthodontic bonding systems was evaluated for three commercially available light-curing units' four different modes by incorporation of pulpal blood flow simulation. All units and curing modes tested in this study caused a temperature increase, but not beyond the critical value of 5.6°C.
The thermal response of the dentine-pulp complex in vivo may depend on the intensity and duration of the applied thermal stimulus caused by the light-curing unit, the fluid motion in the dentinal tubules, the pulp microcirculation, and the pulpal blood flow alterations as a result of the stimulated pulpal nervous system.8 In previous studies the tested teeth were placed inside a tank containing standing water at a constant temperature of 37°C, which may have resulted in more accurate results that reflect clinical situations when compared to those studies performed without water or fluid flow, in which the absence of flow reduces the possibility of heat conduction.9 The calculated amount of blood circulating inside the pulp is an average of 40 mL/min per 100 g of tissue.11,12 According to Baik et al.,13 blood circulation in the pulp of the upper central incisor measures 0.026 mL/min. In the current study, to simulate in vivo conditions, a previously introduced system10 was used for water circulation in the pulp chamber at a rate of 0.026 mL/min. This was also one of the reasons for choosing the upper central incisors. On the other hand, future improvements are needed in the circulation apparatus to fix the temperature of water circulated within the pulp chamber to the body temperature of 37°C for a literal simulation. This was not performed in this study to avoid possible temperature fluctuations related to the heating/cooling apparatus. The bracket and bonding resin combination was not used in this study in order to reduce the number of parameters that could affect the treatment results.
The conduction of temperature changes from the enamel surface to the pulp chamber is affected by the thickness of the enamel and dentine of the tooth.14,15 Mizrahi et al.15 reported that the temperature within the lower incisors and maxillary laterals with thin walls will rise significantly more rapidly and to higher levels than in the other teeth with thicker walls. However, Jost-Brinkmann et al.14 mentioned that the most pronounced temperature rise was measured for the maxillary lateral incisors. According to Malkoç et al.,16 upper central incisors have a high risk of thermal damage because they have thinner enamel and because of the dentinal structure characteristics on the labial side. In addition, maxillary central incisors are the most noticeable teeth in the dentition, and the color change following pulpal damage will have negative effects on esthetics.16 In the present study, upper central incisors were used for the following reasons: previously a constant blood circulation level was reported for these teeth; they are at risk because of their relatively thinner enamel dentin thickness; and the sizes of the pulp chamber are more suitable for placing the water circulation system, when compared to those of the lower central and upper lateral incisors. However, further studies may be beneficial to evaluate the temperature rise inside the pulp chamber of various types of teeth and to confirm the results of the current study.
In previous studies, various light sources were compared. Some of the authors reported that light-curing units with low energy output (Halogen and LED) caused lower temperature changes when compared to high-energy output (Plasma Arc Light) light sources under dentin disks.17,18 Santini et al.3 also reported significantly less temperature rise for a traditional halogen lamp than for high-intensity light sources within the pulp. However, there are contradictory findings in the literature too. Rajesh Ebenezar et al.19 reported that the quartz-tungsten-halogen units caused significantly greater temperature rise than did LED light-cure units. Malkoç et al.16 reported significantly higher intrapulpal temperature changes for high- and low-intensity halogen light units than for the LED and plasma arc curing light, which is in accordance with the findings of Ulusoy et al.20 and Uzel et al.21 Similarly, in the present study, the minimum temperature change was found to be 1.74°C ± 0.52°C for the most powerful curing mode, Valo Xtra power mode (3200 mW/cm2 for 3 seconds), which was significantly lower than changes recorded for Lux V (1000 mW/cm2 for 15 seconds) and Elipar S10 (1200 mW/cm2 for 10 seconds) (P < .05). As the powers of the light-curing units are decreased the curing times are extended. This might be a possible reason for increased temperature rise recorded for a lower irradiation level, as a certain amount of time is required for thermal energy to be transferred to the pulp tissue through enamel and dentin, respectively. It seems that high-power units create significant temperature increases on the surface, which cannot be transferred as a result of short curing times (ie, 3–8 seconds). Rajesh Ebenezar et al.19 similarly reported that the fast mode produces significantly less temperature rise than do the ramp and pulse-cure modes in LED units.
Regarding the possible adverse effect of recorded temperature changes on the pulpal tissue, Zach and Cohen6 reported that a 5.6°C temperature rise caused irreversible pulp damage in 15% of the rhesus monkeys. The duration of this temperature increase was similarly evaluated by Eriksson et al.,22 who reported that a temperature increase of 5°C for 1 minute is critical for the health of vital pulp. This study focuses on the temperature changes rather than their histological effects, and temperature changes for all light-curing units and curing modes were under the critical levels reported previously.
CONCLUSIONS
The lowest intrapulpal temperature rise was induced by Valo Xtra power mode (3200 mW/cm2) for 3 seconds of irradiation, which has the highest power and the shortest curing time among the test groups.
All light-curing units and modes evaluated in this study generated temperature rises within the safe range for the health of the vital pulp.
REFERENCES
- 1.Tavas MA, Watts DC. Bonding of orthodontic brackets by transillumination of a light activated composite: an in vitro study. Br J Orthod. 1979;6:207–208. doi: 10.1179/bjo.6.4.207. [DOI] [PubMed] [Google Scholar]
- 2.Zachrisson BU, Buyukyilmaz T. Bonding in orthodontics. In: Graber TM, Vanarsdall RL Jr, Vig KW, editors. Orthodontics Current Principles and Techniques. 4th. St Louis, Mo: Elsevier; 2005. pp. 579–659. [Google Scholar]
- 3.Santini A, Watterson C, Miletic V. Temperature rise within the pulp chamber during composite resin polymerisation using three different light sources. Open Dent J. 2008;2:137–141. doi: 10.2174/1874210600802010137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cerekja E, Cakirer B. Effect of short curing times with a high-intensity light-emitting diode or high-power halogen on shear bond strength of metal brackets before and after thermocycling. Angle Orthod. 2011;81:510–516. doi: 10.2319/071810-412.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hannig M, Bott B. In-vitro pulp chamber temperature rise during composite resin polymerization with various light-curing sources. Dent Mater J. 1997;15:275–281. doi: 10.1016/s0109-5641(99)00047-0. [DOI] [PubMed] [Google Scholar]
- 6.Zach L, Cohen G. Pulp response to externally applied heat. Oral Surg Oral Med Oral Pathol. 1965;19:515–530. doi: 10.1016/0030-4220(65)90015-0. [DOI] [PubMed] [Google Scholar]
- 7.Kodonas K, Gogos C, Tziafas D. Effect of simulated pulpal microcirculation on intrapulpal temperature changes following application of heat on tooth surface. Int Endod J. 2009;42:247–252. doi: 10.1111/j.1365-2591.2008.01508.x. [DOI] [PubMed] [Google Scholar]
- 8.Raab WH. Temperature related changes in pulpal microcirculation. Proc Finn Dent Soc. 1992;88:469–479. [PubMed] [Google Scholar]
- 9.Kodonas K, Gogos C, Tziafa C. Effect of simulated pulpal microcirculation on intrachamber temperature changes following application of various curing units on tooth surface. J Dent. 2009;37:485–490. doi: 10.1016/j.jdent.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 10.Sari T, Celik G, Usumez A. Temperature rise in pulp and gel during laser-activated bleaching: in vitro. Lasers Med Sci. 2013 Jun 21; doi: 10.1007/s10103-013-1375-5. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 11.Meyer MW. Pulpal blood flow: use of radio-labelled microspheres. Int Endod J. 1993;26:6–7. doi: 10.1111/j.1365-2591.1993.tb00527.x. [DOI] [PubMed] [Google Scholar]
- 12.Matthews B, Andrew D. Microvascular architecture and exchange in teeth. Microcirculation. 1995;2:305–313. doi: 10.3109/10739689509148275. [DOI] [PubMed] [Google Scholar]
- 13.Baik JW, Rueggeberg FA, Liewehr FR. Effect of light enhanced bleaching on in vitro surface and intrapulpal temperature rise. J Esthet Restor Dent. 2001;13:370–378. doi: 10.1111/j.1708-8240.2001.tb01022.x. [DOI] [PubMed] [Google Scholar]
- 14.Jost-Brinkmann P-G, Stein H, Miethke R-R, Nakata M. Histologic investigation of the human pulp after thermobonding of metal and ceramic brackets. Am J Orthod Dentofacial Orthop. 1992;102:410–417. doi: 10.1016/s0889-5406(05)81187-4. [DOI] [PubMed] [Google Scholar]
- 15.Mizrahi E, Cleaton-Jones P, Landy C. Tooth surface and pulp chamber temperatures developed during electrothermal bonding. Am J Orthod Dentofacial Orthop. 1996;109:506–514. doi: 10.1016/s0889-5406(96)70135-x. [DOI] [PubMed] [Google Scholar]
- 16.Malkoç S, Uysal T, Uşümez S, Işman E, Baysal A. In-vitro assessment of temperature rise in the pulp during orthodontic bonding. Am J Orthod Dentofacial Orthop. 2010;137:379–383. doi: 10.1016/j.ajodo.2008.02.028. [DOI] [PubMed] [Google Scholar]
- 17.Usumez A, Ozturk N. Temperature increase during resin cement polymerization under a ceramic restoration: effect of type of curing unit. Int J Prosthodont. 2004;17:200–204. [PubMed] [Google Scholar]
- 18.Ozturk B, Ozturk AN, Usumez A, Usumez S, Ozer F. Temperature rise during adhesive and resin composite polymerization with various light curing sources. Oper Dent. 2004;29:325–332. [PubMed] [Google Scholar]
- 19.Rajesh Ebenezar AV, Anilkumar R, Indira R, Ramachandran S, Srinivasan MR. Comparison of temperature rise in the pulp chamber with different light curing units: an in-vitro study. J Conserv Dent. 2010;13:132–135. doi: 10.4103/0972-0707.71644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ulusoy C, Irmak O, Bagis YH, Ulusoy OI. Temperature rise and shear bond strength of bondable buccal tubes bonded by various light sources. Eur J Orthod. 2008;30:413–417. doi: 10.1093/ejo/cjn013. [DOI] [PubMed] [Google Scholar]
- 21.Uzel A, Buyukyilmaz T, Kayalioglu M, Uzel I. Temperature rise during orthodontic bonding with various light-curing units—an in vitro study. Angle Orthod. 2006;76:330–334. doi: 10.1043/0003-3219(2006)076[0330:TRDOBW]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 22.Eriksson A, Albrektsson T, Grane B, McQueen D. Thermal injury to bone. A vital-microscopic description of heat effects. Int J Oral Surg. 1982;11:115–121. doi: 10.1016/s0300-9785(82)80020-3. [DOI] [PubMed] [Google Scholar]