Abstract
Objective:
To assess camouflage effects by concealment of postorthodontic white-spot lesions (WSLs) to sound adjacent enamel (SAE) achieved over 12 months with resin infiltration (Icon, DMG, Hamburg, Germany).
Methods:
Twenty subjects (trial teeth nteeth = 111) who had received resin infiltration treatment of noncavitated postorthodontic WSLs were contacted for a 1-year follow-up assessment of CIE-L*a*b* colors (T12). Color and lightness (CIE-L*a*b*) data for WSLs and SAE were compared to baseline data assessed before infiltration (T0) and those assessed after 6 months (T6), using a spectrophotometer. The target parameter was the difference between the summarized color and lightness values (ΔEWSL/SAE). Intergroup (WSL, SAE) and intertime comparisons (T0 vs T6, T12) were performed using paired t-tests at a significance level of α = 5%.
Results:
Nine subjects (trial teeth nteeth = 49; male/female ratio 5/4; age range 13–19 years) were available at T12. After the highly significant reduction of ΔEWSL/SAE discrepancies between T0 and T6, analysis of 12-month records revealed color and lightness discrepancy of WSL vs SAE that was significantly decreased compared with baseline, indicating an assimilation of WSL color to SAE appearance after infiltration, while an additional reduction of discrepancies between T6 and T12 was not significant.
Conclusion:
As color and lightness characteristics of the Icon infiltrant as well as the esthetic camouflage effects achieved by WSL infiltration were not altered significantly or clinically relevant after 12 months, the method of resin infiltration can be recommended for an enduring esthetic improvement of postorthodontic WSL. (Angle Orthod. 2015;85:374–380.)
Keywords: White spot lesion, Resin infiltration, Icon, Durability of camouflage effect, CIE-L*a*b*, in vivo
INTRODUCTION
Formation of white spot lesions (WSLs) and incipient caries has been described as typical unwanted side-effects of fixed orthodontic therapy. Risk factors include insufficient oral hygiene,1,2 individual salivary buffering capacity and saliva flow rate,3 presence or absence of local fluoridation,4 and inattentive surplus etching of enamel surfaces that are not covered by bracket bases or sealants.5 Recent research found the incidence for at least one WSL to be between 46% and 73% of patients treated with fixed appliances.6,7 As orthodontic therapy includes the use of fixed buccal appliances in most patients, the handling of WSLs is a matter that concerns almost every orthodontist. It is accepted as good clinical practice that cavitated lesions require restoration, whereas noncavitated lesions should be arrested and/or remineralized by preventive therapy.8
Preventive WSL therapy basically consists of combinations of local fluoridation and tooth brushing abrasion,9–11 with or without an esthetic concealment by external bleaching12 or by resin infiltration in order to stop the progression of demineralization.13 Remineralization and abrasion by unimpeded tooth brushing after bracket removal create a pseudo-intact WSL surface layer that is smoother and harder than fresh, active WSLs.9–11,14–18 A side effect of this is a slight optical abatement of WSLs within the first 12 months after debracketing; however, this rarely occurs to an extent that results in an esthetically acceptable dentofacial appearance.17,19 Other than inhibiting lesion progression, treatment with resin infiltrants has been proven to have the positive side-effect of improving the appearance of WSLs, an effect that is due to the similar refractive index of infiltrated and sound adjacent enamel areas.13,20,21 A recent 6-month randomized controlled trial on the durability of this effect found that there was a significant and clinically relevant abatement of color and lightness differences between infiltrated WSLs and sound adjacent enamel; there were no significant changes in untreated control WSLs at the same time.19
There is still a lack of information on the long-term behavior of camouflage effects by lesion infiltration in vivo. However, this information is needed, as patients who are eligible for this kind of treatment need a valid estimate of the durability of potential masking effects.
The aim of this study was to extend available knowledge on the longevity of achieved color and lightness assimilation between WSLs and sound adjacent enamel (SAE) areas after resin infiltration in vivo by reassessing previously infiltrated WSLs after 12 months and compared the findings to baseline and 6-month records.19
We tested the null hypothesis that there would be no significantly different CIE-Lab ΔE-values between WSL and SAE areas of assessments after 12 months (T12) compared with those at baseline and after 6 months (T6).
SUBJECTS AND METHODS
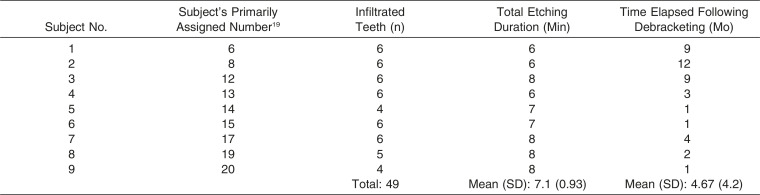
This study is a follow-up of patients treated with WSL infiltration during a single-center, split-mouth controlled simple-randomized trial. Full ethical approval was obtained from the University of Göttingen Ethics Committee, and all patients and their guardians gave informed consent before the start of the trial. In those patients, postorthodontic WSLs in the treatment quadrants were infiltrated according to the producer's instruction sheet (Icon, DMG, Hamburg, Germany). Conditioning of WSL and SAE surfaces was by 15% HCL gel (Icon-Etch, DNG) and subsequent application of the drying solution (Icon-Dry, DMG), and has been iterated in cases of engrained lesions and those with hardened surface layers. Numbers of additional etching intervals have been determined by visual assessment after each of the etch/dry intervals to achieve individual, customized intensities of WSL surface conditioning (Table 1).19
Table 1. .
Time Points and Intensity of Etching and Infiltration Treatment
As part of the agreement made with the patients before starting the trial, the original control quadrants were also infiltrated after the first 6 months. Therefore, CIE-Lab values after 12 months (T12) were compared with baseline assessments (T0) and 6-month results (T6).
Original inclusion criteria for subject recruitment included multibracket induced WSLs and completed debracketing; exclusion criteria were cavitated lesions as well as filled, restored, and deciduous teeth. During the trial, participants were given the same type of toothbrushes (Oral-B Classic Care, Procter & Gamble, Cincinnati, Ohio) and dentifrices (elmex, GABA, Lörrach, Germany) for oral hygiene home care.
Subjects
Of 20 contacted subjects (10 boys, 11 girls; mean age 15.5 years; n = 231 teeth; 114 control/117 treatment teeth) who received resin infiltration treatment of nteeth = 111 nonrestored, noncavitated (postorthodontic) WSLs after multibracket treatment at the Department of Orthodontics, University of Göttingen (Germany), nine subjects (trial teeth nteeth = 49; male/female ratio 5/4; age range, 13–19 years; mean age, 5.89 years; response rate, 45%) were available for a 12-month follow-up (T12). Table I gives specific details on the subjects' treatment and the time lapse between debracketing and infiltration.
Method
Extent and longevity of assimilation of WSLs and SAE have been assessed by comparing CIE (L*a*b*) enamel color and lightness data recorded before infiltration (baseline, T0), directly after infiltration (T1a), and after 6 months (T6);19 those assessments were compared with WSL and SAE records taken after 12 months (T12). The experimental setup was identical to that at previous assessment times. The same intraoral spectrophotometer (ShadePilot, Degudent, Hanau-Wolfgang, Germany) was used by the same operator as before at the Department of Orthodontics, University of Göttingen. In order to achieve the highest possible level of standardization during this in vivo trial, measurements were performed with the patient's lips closed to exclude the distortive variation of ambient light. We used the system-immanent target caption to retrieve the exact locations of infiltrated WSLs and previously used SAE control areas. As a positive side-effect, variation in the patient's head position during CIE-(L*a*b*) assessments was compensated for and did not negatively affect the measurements.22
Statistical Analysis
Means and 95% confidence intervals were calculated for lightness color parameters L*, a*, and b* separately for WSL and sound enamel. The target parameter was the difference between the summarized color and lightness values (ΔE of WSL vs. SAE). The WSL and SAE color and lightness characteristics (CIE-L*a*b*) were each summarized by ΔE-values for both an intragroup/intertime area comparison at different time points and an intergroup area comparison:
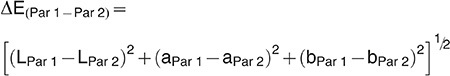 |
All intergroup (WSL and sound enamel) and intertime comparisons (T0 vs T6 and T12) were performed using paired t-tests, and the significance level was set at α = 5%. Statistical analyses were performed with Statistica 10 (StatSoft, Tulsa, Okla).
Method Error Assessment
The accuracy of the spectrophotometer in recording CIE-L*a*b* values has been determined by 10-time repeated pretrial assessments by two assessors. Variance in measurements and the results of intra- and interoperator method error have been published19 and ranged from 0.16 units (L* value, upper incisor) to 0.82 units (a* value, upper incisor), corroborating previous assessments of the accuracy of the same type of spectrophotometer.23 Furthermore, the CIE-a*/b* color value correlations at T0, T6, and T12 were computed for all trial participants who stayed in the study until T12 for testing the veridicality of assessed color values. 24 At T0, a*/b* correlations were r = 0.283 (P = .049) for WSL and r = 0.504 (P < .001) for SAE. At T6, the correlation structure was nearly identical with r = 0.289 (P = .044) and r = .64 (P < .001) for SAE. At T12, a*/b* correlations were r = 0.13 (P = .385) for WSL and r = 0.638 (P < .0001) for SAE.
RESULTS
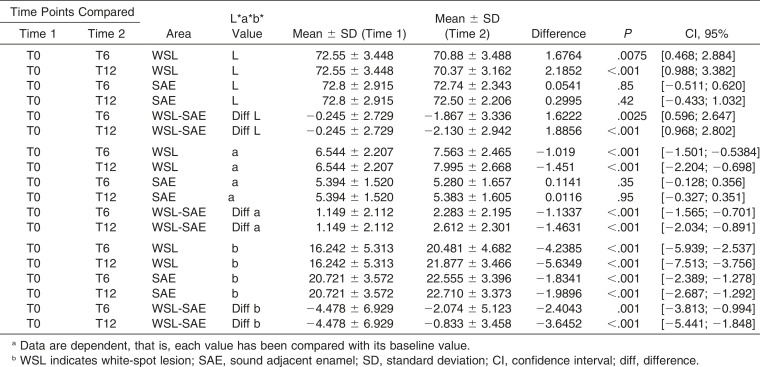
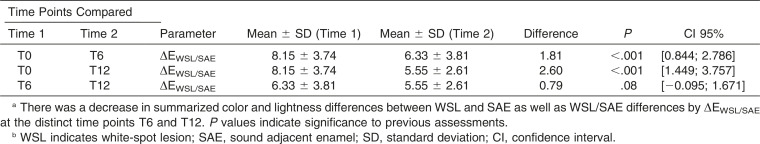
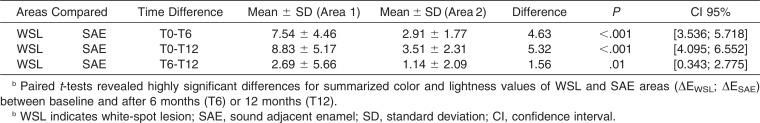
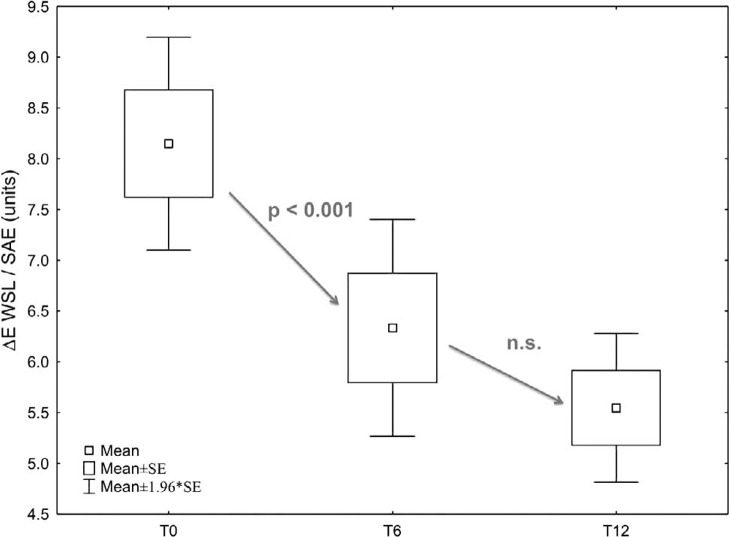
Development and comparisons of segregated CIE-L*a*b* values of infiltrated WSL and SAE areas at the distinct time points are shown in Table 2. Analysis of the nine available subjects (trial teeth nteeth = 49; nsites = 96) at T12 revealed a decrease in summarized color and lightness WSL/SAE discrepancy by ΔE (WSL/SAE) after 12 months (T12, 5.546 units) compared with the baseline data (T0, 8.149), and to the 6-month follow up assessments (T6, 6.33 units), indicating an assimilation of WSL color to SAE appearance after infiltration that is even slightly increased after 12 months (Tables 3 and 4; Figures 1 and 2). The reduction of the ΔEWSL/SAE discrepancy between T6 and T12, however, was not significant.
Table 2. .
Descriptive Statistics: CIE-L*-, a*, and b* Values of infiltrated WSLs, SAE Values, and WSL/SAE Differences at Distinct Time Pointsa,b
Table 3. .
Intergroup Comparison of Summarized Mean Color Differences (ΔE Between WSL and SAE) Between Different Assessments (T0, T6, T12)a,b
Table 4. .
Intragroup/Intertime Comparisons of Mean Color Change (ΔE Between Different Time Points) Between WSLs and SAEa,b
Figure 1.
Color difference between white-spot lesions (WSLs) and sound adjacent enamel (SAE) at various assessment time points.The t-tests detected highly significant differences for summarized color and lightness values (ΔE CIE-L*a*b* b) of the WSL vs SAE areas between baseline measurements and measures taken 6 months (T6) or 12 months (T12) after infiltration. A further reduction of ΔE values between T6 and T12 was not found to be significant.
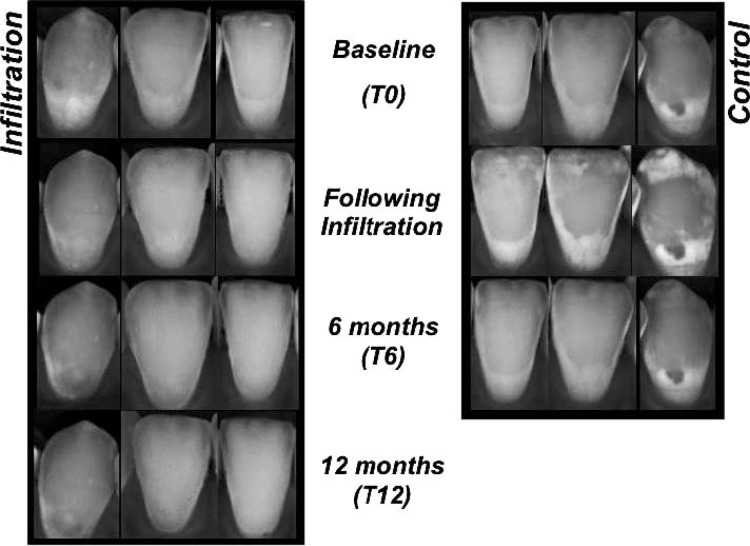
Figure 2.
An example of spectrophotometric recordings of one subject. Nontreated control teeth were also infiltrated after 6 months as part of an agreement with the patients. There was a typical temporary increase in lightness of control teeth after the infiltration appointment, which is an effect of desiccation. Overall, esthetic concealment of white-spot lesions worked out better in more superficial lesions, though the appearance of deeper lesions also benefits from resin infiltration, as evident from the depicted lower canine.
The null hypothesis was rejected: Highly significant color differences that were achieved by infiltration and persisted for 6 months (T0 and T6 assessments, [[19]]) persisted after 12 months as confirmed by analysis of T0-T12 assessments (P < .0001) (Table 3).
DISCUSSION
The Icon resin infiltrant's capability in concealing postorthodontic caries lesions has recently been the subject of short-term studies, case reports, and in vitro research,20,21,25–27 and those studies indicate a clinically relevant optical harmonization of infiltrated WSL with adjacent enamel. A recent 6-month randomized controlled trial on the longevity of this effect reported a stability of the infiltrants and achieved esthetic assimilation of color and lightness differences between infiltrated WSL and SAE, but no significant changes in untreated control WSL at the same time.19 The current follow-up assessment of the lesions infiltrated in the previous randomized controlled trial was conducted as there are currently no other long-term data on the color stability of the resin infiltrant in vivo available. Also, against the background of the known potential risks of excessive surplus etching during orthodontic bonding,5 there is currently no information on the long-term integrity and potential color changes of the SAEs available, which are likewise etched with the HCl-gel as the adjacent WSL.
It has been shown that the surface hardness and smoothness, as well as dimensions and depths, of WSL are decisive factors for success or failure in concealing postorthodontic lesions. In general, lesions of smaller dimensions with surface structures that are less smoothed and remineralized after bracket removal require fewer etching intervals and allow for a deeper penetration of the infiltrant, yielding treatment results that are esthetically more appealing.19 In the subjects available for this follow-up, infiltration was carried out at a mean time of 4.7 months after debonding. In order to remove the hard pseudo-intact surface layer of the lesions, etching intervals of up to 8 minutes were necessary, each at 1- or 2-minute intervals. Previous investigations have reported a penetration depth of approximately 30 µm per 2-minute etching interval.28 The subjects that were available for this follow-up had a total mean etching duration of 7.1 minutes.
Twelve-Month Changes of Segregated Color or Lightness Values
At T12, the WSL's lightness value L* was significantly decreased by a mean of about 0.5 units compared with the baseline, in contrast to the records taken at T6 (Table 1). The SAE areas did not change significantly at the same time. That is, in terms of lightness, the infiltrated WSLs approximate adjacent enamel areas even more; however, it is doubtful that an improvement of an average of 0.5 units on the lightness scale is more than meets the eye.29 Also, no further significant changes in the color (a*, b*) values of the also etched and treated SAE areas were observed after 12 months, other than the change of b* value in both areas that had already been detected before the 6-month trial. Though statistically significant, this change on the axis from blue to yellow is also not considered clinically relevant as the absolute mean changes in b* value are smaller than the threshold value needed for detection by the naked eye.29 Beyond that, the patients reported no important adverse events or side-effects during the 12-month period after infiltration.
Total Effect on Summarized Color and Lightness Development After 12 Months
Despite a further reduction of 1.81 in the summarized color and lightness discrepancy between WSL and SAE areas after T6 (mean ΔEWSL/SAE discrepancy was lowered from 6.3 units at T6 to 5.5 units at T12), this decrease of the ΔEWSL/SAE discrepancy between T6 and T12 was found to be neither statistically significant nor clinically relevant.29 That is, WSL camouflage effects achieved by resin infiltration were found to be stable in color with no significant changes over 12 months, and the null hypothesis of no significant color and lightness changes of infiltrated WSL after 12 months in vivo was rejected. Therefore, on the basis of assessed color and lightness discrepancies between WSL and SAE, the method of resin infiltration can be recommended as an enduring improvement of postorthodontic WSL. Future research will be concerned with follow-up assessments of the teeth investigated in this trial.
Beyond the ambit of postorthodontic WSL, the technique of resin infiltration has been shown to be have abilities not only for inhibiting the progression of caries lesions and concealing WSL but also for improving the appearance of dental fluorosis30,31 or penetrating enamel affected by molar-incisor hypomineralization.32 It may be expected that infiltration will be an established treatment option for these indications in a few years. However, despite the excellent short-term reports provided, there is still a paucity of available information on the long-term durability of those camouflage effects in vivo.
CONCLUSIONS
The optical appearance of WSL was improved by lesion infiltration.
The infiltrant material and the achieved concealment of WSL with SAE were stable over a period of 12 months in vivo; no statistically significant or clinically relevant additional color or lightness alterations were noted between 6 and 12 months after infiltration, allowing for a valid estimate of the durability of esthetic effects.
The patients reported no important adverse events or side-effects during the 12-month period following infiltration.
ACKNOWLEDGMENT
This study was financially supported by DMG, Hamburg, Germany. We also thank Degudent, Hanau-Wolfgang, Germany for donating the spectrophotometer for use in this trial. There were no restrictions with respect to the publication of the results.
REFERENCES
- 1.Øgaard B, Rolla G, Arends J. Orthodontic appliances and enamel demineralization. Part 1. Lesion development. Am J Orthod Dentofacial Orthop. 1988;94:68–73. doi: 10.1016/0889-5406(88)90453-2. [DOI] [PubMed] [Google Scholar]
- 2.Bishara SE, Ostby AW. White spot lesions: formation, prevention, and treatment. Semin Orthod. 2008;14:174–182. [Google Scholar]
- 3.Bardow A, Nyvad B, Nauntofte B. Relationships between medication intake, complaints of dry mouth, salivary flow rate and composition, and the rate of tooth demineralization in situ. Arch Oral Biol. 2001;46:413–423. doi: 10.1016/s0003-9969(01)00003-6. [DOI] [PubMed] [Google Scholar]
- 4.Featherstone JDB. Prevention and reversal of dental caries: role of low level fluoride. Community Dent Oral Epidemiol. 1999;27:31–40. doi: 10.1111/j.1600-0528.1999.tb01989.x. [DOI] [PubMed] [Google Scholar]
- 5.Knösel M, Bojes M, Jung K, Ziebolz D. Increased susceptibility for white spot lesions by surplus orthodontic etching exceeding bracket base area. Am J Orthod Dentofacial Orthop. 2012;141:574–582. doi: 10.1016/j.ajodo.2011.11.017. [DOI] [PubMed] [Google Scholar]
- 6.Richter AE, Arruda AO, Peters MC, Sohn W. Incidence of caries lesions among patients treated with comprehensive orthodontics. Am J Orthod Dentofacial Orthop. 2011;139:657–664. doi: 10.1016/j.ajodo.2009.06.037. [DOI] [PubMed] [Google Scholar]
- 7.Tufekci E, Dixon JS, Gunsolley JC, Lindauer SJ. Prevalence of white spot lesions during orthodontic treatment with fixed appliances. Angle Orthod. 2011;81:206–210. doi: 10.2319/051710-262.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stahl J, Zandona AF. Rationale and protocol for the treatment of non-cavitated smooth surface carious lesions. Gen Dent. 2007;55:105–111. [PubMed] [Google Scholar]
- 9.Al-Khateeb S, Forsberg CM, de Josselin de Jong E, Angmar-Mansson B. A longitudinal laser fluorescence study of white spot lesions in orthodontic patients. Am J Orthod Dentofacial Orthop. 1998;113:595–602. doi: 10.1016/s0889-5406(98)70218-5. [DOI] [PubMed] [Google Scholar]
- 10.Fejerskov O, Nyvad B, Kidd EAM. Dental Caries—The Disease and Its Clinical Management. Ames, IA: Blackwell Munksgaard; 2003. Clinical and histological manifestations of dental caries; pp. 72–97. [Google Scholar]
- 11.Willmot DR. White lesions after orthodontic treatment: does low fluoride make a difference. J Orthod. 2004;31:235–242. doi: 10.1179/146531204225022443. [DOI] [PubMed] [Google Scholar]
- 12.Knösel M, Attin R, Becker K, Attin T. External bleaching effect on the color and luminosity of inactive white-spot lesions after fixed orthodontic appliances. Angle Orthod. 2007;77:646–652. doi: 10.2319/060106-224. [DOI] [PubMed] [Google Scholar]
- 13.Paris S, Hopfenmuller W, Meyer-Lueckel H. Resin infiltration of caries lesions: an efficacy randomized trial. J Dent Res. 2010;89:823–826. doi: 10.1177/0022034510369289. [DOI] [PubMed] [Google Scholar]
- 14.Backer Dirks O. The clinical testing of agents for the prevention of dental caries. Adv Fluorine Res. 1966;4:1–2. [PubMed] [Google Scholar]
- 15.Palamara J, Phakey PP, Rachinger WA, Orams HJ. Ultrastructure of the intact surface zone of white spot and brown spot carious lesions in human enamel. J Oral Pathol. 1986;15:28–35. doi: 10.1111/j.1600-0714.1986.tb00560.x. [DOI] [PubMed] [Google Scholar]
- 16.Holmen L, Thylstrup A, Artun J. Surface changes during the arrest of active enamel carious lesions in vivo. A scanning electron microscope study. Acta Odontol Scand. 1987;45:383–390. doi: 10.3109/00016358709096362. [DOI] [PubMed] [Google Scholar]
- 17.Øgaard B, Ten Bosch JJ. Regression of white spot enamel lesions. A new optical method for quantitative longitudinal evaluation in vivo. Am J Orthod Dentofacial Orthop. 1994;106:238–242. doi: 10.1016/S0889-5406(94)70042-7. [DOI] [PubMed] [Google Scholar]
- 18.Wiegand A, Köwing L, Attin T. Impact of brushing force on abrasion of acid-softened and sound enamel. Arch Oral Biol. 2007;52:1043–1047. doi: 10.1016/j.archoralbio.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 19.Knösel M, Eckstein A, Helms HJ. Durability of esthetic improvement following Icon resin infiltration of multibracket-induced white spot lesions compared with no therapy over 6 months: a single-center, split-mouth, randomized clinical trial. Am J Orthod Dentofacial Orthop. 2013;144:86–96. doi: 10.1016/j.ajodo.2013.02.029. [DOI] [PubMed] [Google Scholar]
- 20.Paris S, Meyer-Lueckel H. Masking of labial enamel white spot lesions by resin infiltration—a clinical report. Quintessence Int. 2009;40:713–718. [PubMed] [Google Scholar]
- 21.Rocha Gomes Torres C, Borges AB, Torres LM, Gomes IS, de Oliveira RS. Effect of caries infiltration technique and fluoride therapy on the colour masking of white spot lesions. J Dent. 2011;39:202–207. doi: 10.1016/j.jdent.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 22.Knösel M, Attin R, Jung K, Brunner E, Kubein-Meesenburg D, Attin T. Digital image color analysis compared to direct dental CIE colorimeter assessment under different ambient Conditions. Am J Dent. 2009;22:67–72. [PubMed] [Google Scholar]
- 23.Sluzker A, Knösel M, Athanasiou AE. Sensitivity of digital dental photo CIE L*a*b* analysis compared to spectrophotometer clinical assessments over 6 months. Am J Dent. 2011;24:300–304. [PubMed] [Google Scholar]
- 24.Knösel M, Reus M, Rosenberger A, Ziebolz D. A novel method for testing the veridicality of dental colour assessments. Eur J Orthod. 2012;34:19–24. doi: 10.1093/ejo/cjq142. [DOI] [PubMed] [Google Scholar]
- 25.Neuhaus KW, Graf M, Lussi A, Katsaros C. Late infiltration of post-orthodontic white spot lesions. J Orofac Orthop. 2010;71:442–447. doi: 10.1007/s00056-010-1038-0. [DOI] [PubMed] [Google Scholar]
- 26.Hammad SM, El Banna M, El Zayat I, Mohsen MA. Effect of resin infiltration on white spot lesions after debonding orthodontic brackets. Am J Dent. 2012;25:3–8. [PubMed] [Google Scholar]
- 27.Senestraro SV, Crowe JJ, Wang M, et al. Minimally invasive resin infiltration of arrested white-spot lesions: a randomized clinical trial. J Am Dent Assoc. 2013;144:997–1005. doi: 10.14219/jada.archive.2013.0225. [DOI] [PubMed] [Google Scholar]
- 28.Meyer-Lueckel H, Paris S, Kielbassa AM. Surface layer erosion of natural caries lesions with phosphoric and hydrochloric acid gels in preparation for resin infiltration. Caries Res. 2007;41:223–230. doi: 10.1159/000099323. [DOI] [PubMed] [Google Scholar]
- 29.Johnston WM, Kao EC. Assessments of appearance match by visual observation and clinical colorimetry. J Dent Res. 1989;68:819–822. doi: 10.1177/00220345890680051301. [DOI] [PubMed] [Google Scholar]
- 30.Munoz MA, Arana-Gordillo LA, Gomes GM, et al. Alternative esthetic management of fluorosis and hypoplasia stains: blending effect obtained with resin infiltration techniques. J Esthet Restor Dent. 2013;25:32–39. doi: 10.1111/j.1708-8240.2012.00527.x. doi: 10.1111/j.1708-8240.2012.00527.x. [DOI] [PubMed] [Google Scholar]
- 31.Tirlet G, Chabouis HF, Attal JP. Infiltration, a new therapy for masking enamel white spots: a 19-month follow-up case series. Eur J Esthet Dent. 2013;8:180–190. [PubMed] [Google Scholar]
- 32.Crombie F, Manton D, Palamara J, Reynolds E. Resin infiltration of developmentally hypomineralised enamel. Int J Paediatr Dent. 2013 Feb 15;2014;24:51–55. doi: 10.1111/ipd.12025. doi: 10.1111/ipd.12025. [DOI] [PubMed] [Google Scholar]