Abstract
Objective:
To assess skeletal and dentoalveolar effects of fixed functional appliances, alone or in combination with multibracket appliances (comprehensive treatment), on Class II malocclusion in pubertal and postpubertal patients.
Materials and Methods:
Literature survey was conducted using the Medline, SCOPUS, LILACS, and SciELO databases and The Cochrane Library, and through a manual search. The studies retrieved had to have a matched untreated control group. No restrictions were set regarding the type of fixed appliance, treatment length, or to the cephalometric analysis used. Data extraction was mostly predefined at the protocol stage by two authors. Supplementary mandibular elongation was used for the meta-analysis.
Results:
Twelve articles qualified for the final analysis of which eight articles were on pubertal patients and four were on postpubertal patients. Overall supplementary total mandibular elongations as mean (95% confidence interval) were 1.95 mm (1.47 to 2.44) and 2.22 mm (1.63 to 2.82) among pubertal patients and −1.73 mm (−2.60 to −0.86) and 0.44 mm (−0.78 to 1.66) among postpubertal patients, for the functional and comprehensive treatments, respectively. For pubertal subjects, maxillary growth restraint was also reported. Nevertheless, skeletal effects alone would not account for the whole Class II correction even in pubertal subjects with dentoalveolar effects always present.
Conclusions:
Fixed functional treatment is effective in treating Class II malocclusion with skeletal effects when performed during the pubertal growth phase, very few data are available on postpubertal patients.
Keywords: Class II, Functional treatment, Timing, Growth phase, Systematic review
INTRODUCTION
Skeletal Class II malocclusion occurs in 25%–30% of the general population, is one of the most prevalent malocclusions,1 and is mainly a consequence of mandibular retrusion.2 Therefore, removable or fixed functional appliances were designed to increase mandibular growth by forward positioning of the mandible.2 Previous systematic reviews of the literature3–5 on the outcomes of functional treatment for Class II malocclusion, mainly through removable appliances, have shown substantial variability of reported results. These differences have to be ascribed mainly to the type of appliance used or duration of active treatment needed to achieve Class II correction. However, none of these reviews have focused attention on the timing of intervention, ie, the growth phase during which treatment was performed.6 Indeed, timing has been reported as one of the key factors for successful treatment outcome with the pubertal growth phase as the optimal period for the achievement of skeletal effects.6,7 Moreover, patient compliance is another important issue when dealing with functional treatment, which can be overcome by the use of fixed functional appliances.
Therefore, the aim of the present review and meta-analysis was to assess main skeletal and dentoalveolar effects of fixed functional appliances, alone or in combination with multibracket appliances (MBA), in the treatment of Class II malocclusion. This was done according to the pubertal or postpubertal growth phase in growing patients as compared with matched untreated controls.
MATERIALS AND METHODS
Search Strategy
The present meta-analysis follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement,8 and it has been registered at the PROSPERO database (http://www.crd.york.ac.uk/PROSPERO, CRD42014009769). Articles were identified through a literature survey carried out through the following databases: (1) PubMed, (2) SCOPUS, (3) Latin American and Caribbean Health Sciences (LILACS), (4) Scientific Electronic Library Online (SciELO), and (5) The Cochrane Library. The survey covered the period from inception to the last access on July 2, 2014, without language restrictions. The search algorithms used in each database are given in Appendix 1. Finally, a manual search was also performed by scoring the references within the studies examined and the titles of the papers published over the last 20 years in the main orthodontic journals. The eligibility assessment and data collection processes were performed independently by two blinded authors. Conflicts were resolved by discussion of each article, until consensus was reached.
Eligibility Criteria
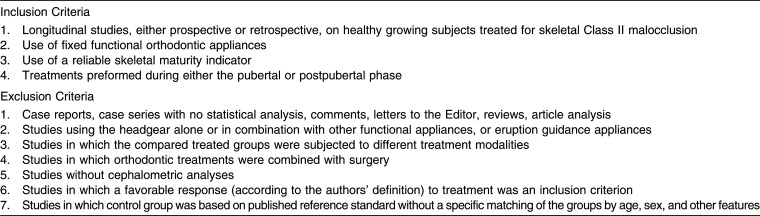
The studies retrieved had to be either randomized controlled trials (RCTs) or either prospective or retrospective controlled clinical trials (CCTs). They had to include healthy patients treated during either the pubertal or postpubertal growth phases. These studies had to investigate the skeletal and dentoalveolar effects with no restriction as to the type of parameters collected. Also, no restrictions were set regarding the type of fixed appliance used alone or in combination with MBA (comprehensive treatment), treatment length, or to the cephalometric analysis used. Studies were also excluded if a reliable indicator of the growth phase (hand-and-wrist maturation [HWM] method or cervical vertebral maturation [CVM] method) was not used. Further details are listed in Table 1.
Table 1. .
Inclusion and Exclusion Criteria Used in the Present Review
Data Items
The following data were extracted independently by two authors: study design, enrollment of the treated group, sample size, sex distribution, age, treatment, Class II diagnosis, indicators of skeletal maturity, and distribution of subjects according to growth phase, prognostic or other features, full observational term, functional and/or comprehensive treatment length, mandibular advancement, and when treatment was stopped. Regarding the treatment effects, the following items were also collected: success rate (as defined in the different studies); skeletal, dentoalveolar, and soft tissue effects; and clinical implications with regard to the growth phase at which treatment was performed. Forms used for the data extraction were mostly predefined at the protocol stage by two authors.
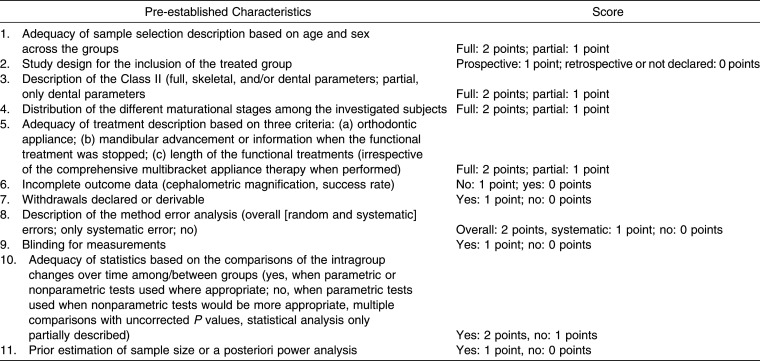
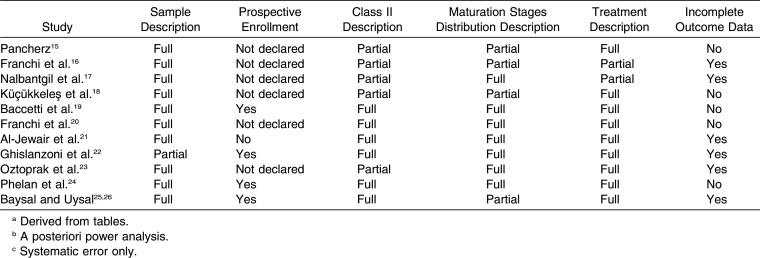
Assessment of Risk of Bias in Individual Studies and Across Studies
As no single approach in assessing methodologic soundness may be appropriate for all systematic reviews,9 a dedicated evaluation risk of bias in individual studies (performed independently by two expert authors) was used that followed pre-established characteristics, along with the systematic scores that were assigned to the individual retrieved articles detailed in Table 2. The quality of the studies, with a maximum possible score of 17, was considered as follows:
Table 2. .
Assessment of Risk of Bias
low: total score ≤7 points;
medium: total score >7 and ≤10 points;
medium/high: total score >10 and ≤14 points; and
high: total score >14 points.
Heterogeneity was assessed using the χ2-based Q-statistic method and I2 Index; however, because of the moderate insensitivity of the Q statistic,10 only an I2 Index ≥50% was considered associated with a substantial heterogeneity among the studies.11 The tau2 was also calculated for the heterogeneity assessment. Egger test was employed to assess publication bias12 for those parameters that showed acceptable heterogeneity (I2 Index generally below 50%). Calculations were performed by using the Comprehensive Meta-Analysis software (Biostat Inc, Englewood, NJ).
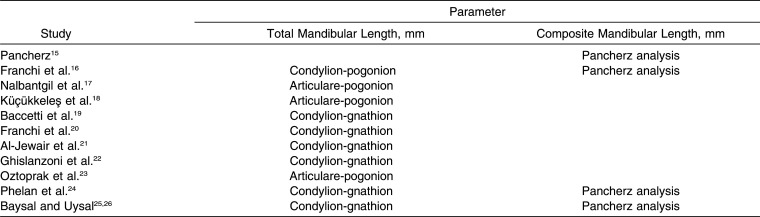
Primary and Secondary Outcomes
Supplementary mandibular growth with respect to the untreated control group was considered as the primary outcome. This outcome was defined either as total or composite mandibular length change. The total mandibular length was derived from the following cephalometric measurements: condylion-gnathion, condylion-pogonion, and articulare-pogonion; unit of measure was expressed in millimeters. Composite mandibular length, also expressed in millimeters, was obtained by the Pancherz analysis.13 Analyses were performed separately for the two parameters. Secondary outcomes were: SNA, SNB, and ANB angles, total facial divergence (angle between mandibular plane and S-N line or Frankfort horizontal plane), maxillary incisors inclination (relative to the S-N line or Frankfort horizontal plane), and mandibular incisors inclination (relative to the mandibular plane).
Meta-analysis
For meta-analysis, data were combined using the Review Manager software 5.2 (http://www.cochrane.org). The mean difference was used for statistical pooling of data, and results were expressed as mean and 95% confidence intervals (CIs). Although the measures of total mandibular length differed slightly among the studies, these measurements were combined in the overall effects according to the concept that the differences in the intragroup changes would be poorly sensitive to the absolute measures from which they are derived. Subgroup analyses were performed whenever possible according to the growth phase (pubertal or postpubertal) during which the treatment was performed. Moreover, to account for the heterogeneity of the treatments (ie, differences among appliance used), treatment length, and cephalometric analysis, a random effect model was used for the overall effects calculations.14 Finally, these analyses were reported according to the type of treatment (functional or comprehensive) and shown through forest plots. In studies including two or more treated groups compared to a single control group, data from treated groups were pooled according to the Cochrane Handbook indications (http://handbook.cochrane.org).
RESULTS
Study Search
The results of the electronic and manual searches are summarized in Figure 1. According to the electronic search, 2611 articles were retrieved. Among these, 12 studies15–26 were judged to be relevant to the present study according to the inclusion/exclusion criteria. However, two articles were clearly derived from the same study sample reporting either the results about soft tissues and SNA, SNB, and ANB angles25 or other dentoskeletal effects,26 and may be considered as a single study. A further article27 could not be retrieved upon Internet search, through the local library facility, and after having contacted the authors. For one study pooling pubertal and postpubertal subjects,20 data regarding the pubertal subjects could be extracted only from the whole sample. The full details of the 12 included studies are summarized in Tables 3 and 4.
Figure 1.
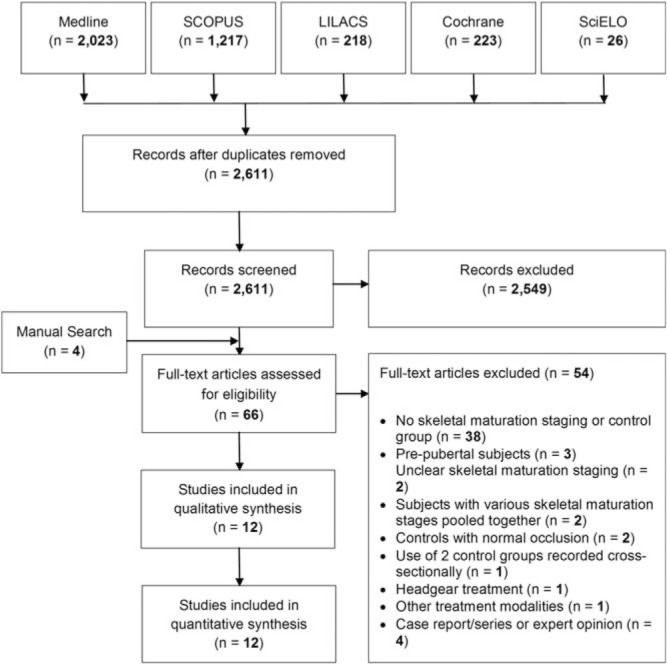
Flow diagram of the search strategy.
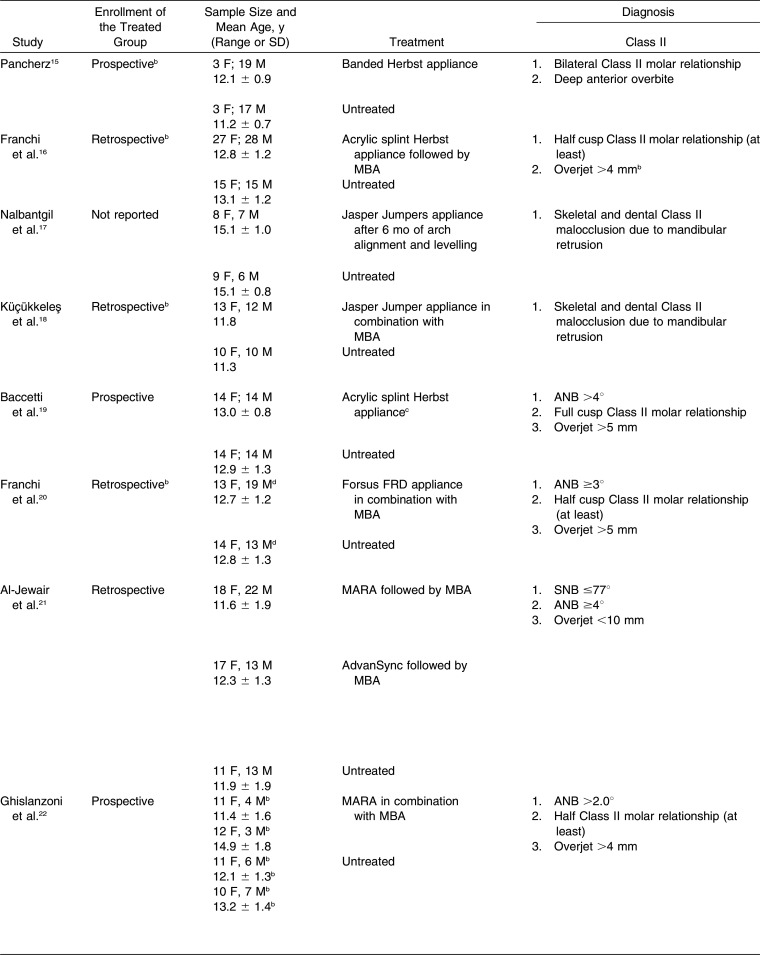
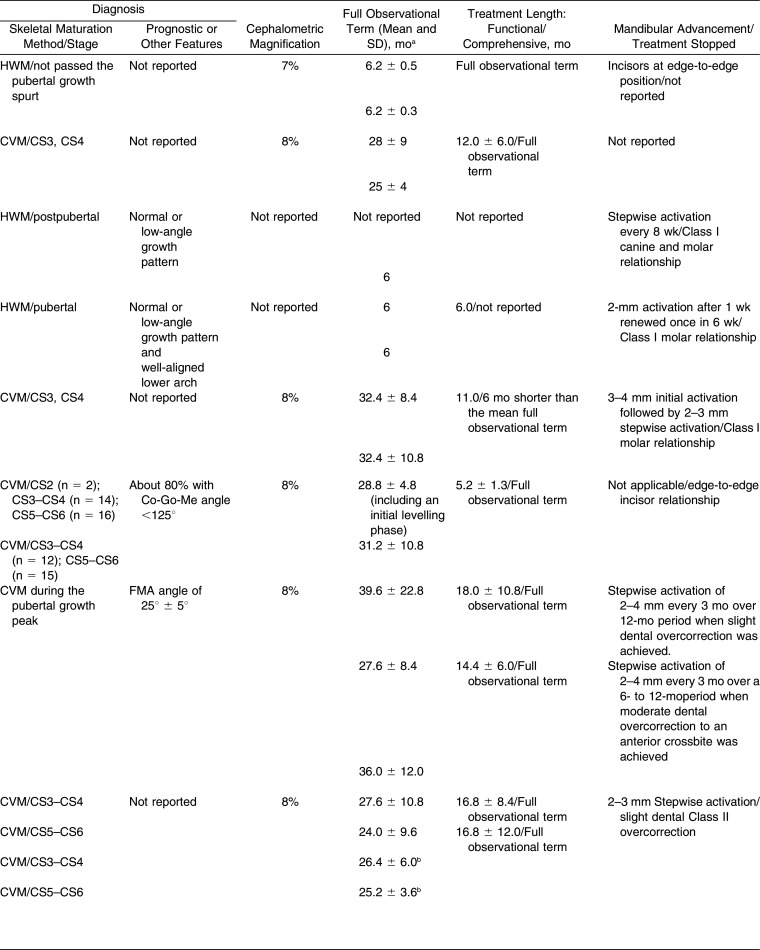
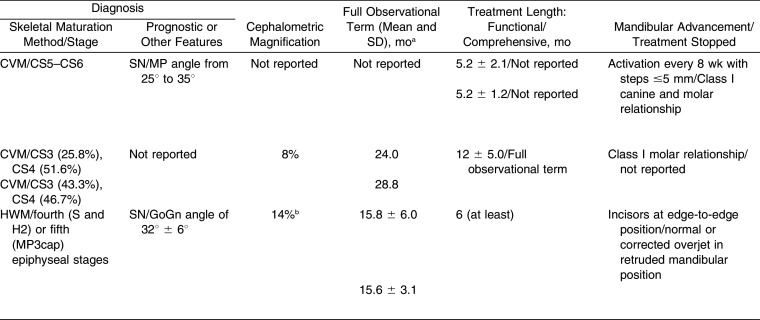
Table 3. .
Summarized Protocols of the 11 Studies (12 Articles) Included in the Present Systematic Review*
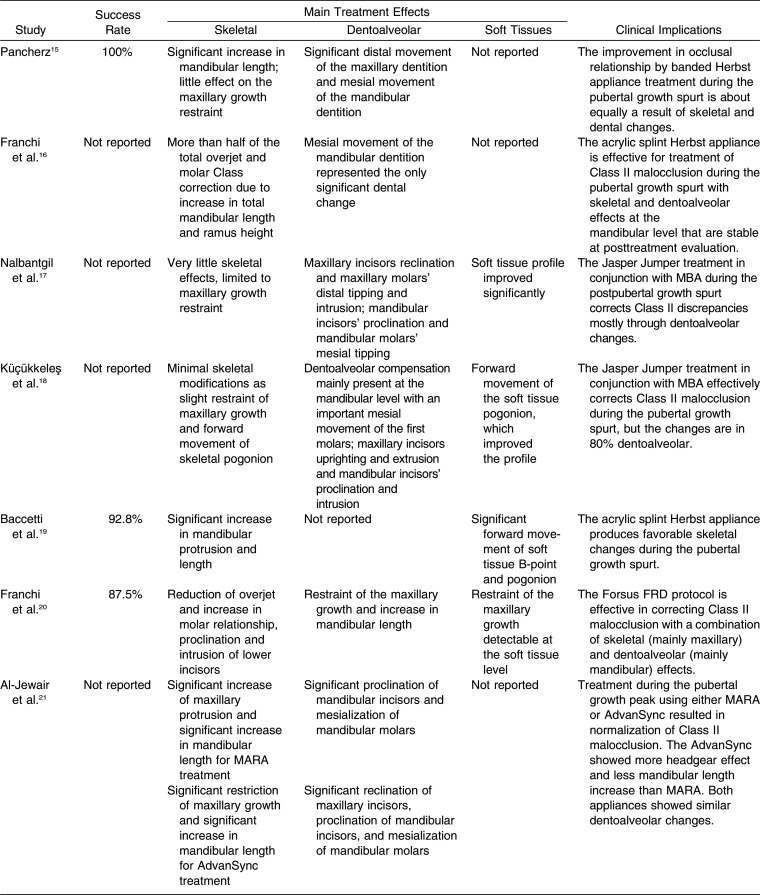
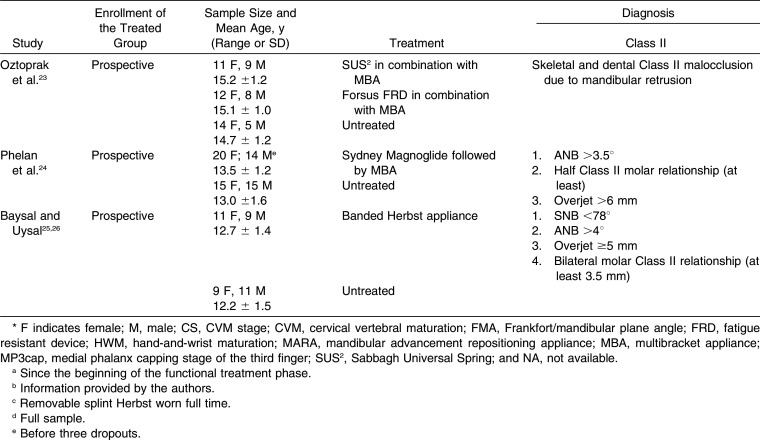
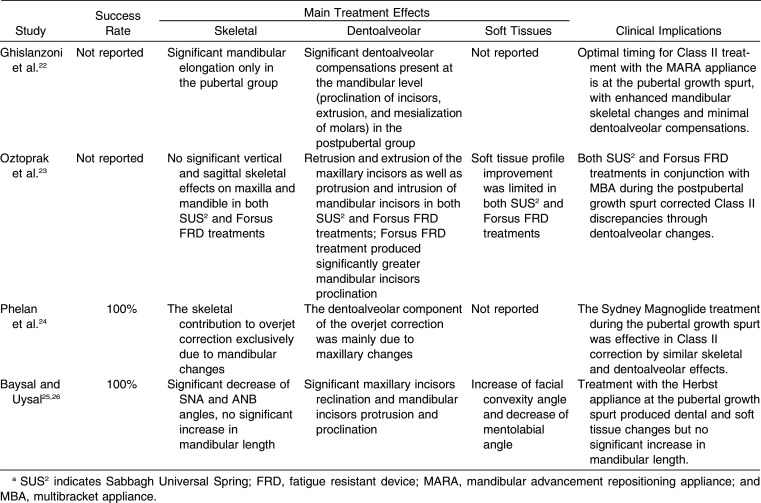
Table 4. .
Summarized Treatment Effects in the 11 Studies (12 Articles) Included in the Present Systematic Review*
Table 3. .
Extended
Table 3. .
Continued
Table 3. .
Extended Continued
Table 4. .
Continued
Study Designs and Treatment Interventions
Of the 12 studies included, the enrollment of the treated group was prospective in six of them15,19,22–26 and retrospective in four16,18,20,21; in one study the enrollment protocol was not reported or retrieved after contacting the authors. The sample sizes ranged from a minimum of 15 subjects17,22 to a maximum of 55 subjects,16 and all the studies included both male and female subjects.
The fixed functional appliances used were either a banded Herbst appliance,15,25,26 an acrylic splint Herbst19 followed by MBA,16 a Jasper Jumper mounted after dental arch alignment17 or in combination with MBA,18 Forsus fatigue resistant device (FRD) in combination with MBA,20,23 mandibular repositioning appliance (MARA) followed by MBA,21,22 AdvanSync followed by MBA,21 Sabbagh Universal Spring (SUS2) in combination with MBA,23 and the magnetic Sydney Magnoglide followed by MBA.24
To assess the growth phase, seven studies16,19–24 used the CVM method, while the other investigations15,17,18,25,26 used the HWM method. Accordingly, treatments were performed during the pubertal growth phase in all the studies, except for three investigations that included also22 or only17,23 postpubertal subjects.
The mean treatment duration with a fixed functional appliance (with or without MBA) performed during the pubertal growth phase ranged from 5.2 (Forsus FRD)20 to 18.0 (MARA)21 months. In the postpubertal patients, the mean treatment duration ranged from 5.2 (SUS2)23 to 16.8 (MARA)22 months. Comprehensive treatments lasted from 24.0 (MARA and MBA, postpubertal)22 to 39.6 months (MARA and MBA, pubertal).21
A stepwise mandibular advancement of 2 to 4 mm was performed in most of the studies.17–19,21–24 In two investigations, a mandibular advancement to an incisor edge-to-edge relationship was used,15,26 while in one study24 mandibular advancement to a Class I molar relationship was performed. Two studies did not report the amount of mandibular advancement during treatment.16,20 In most of the studies, treatment was performed until a Class I molar relationship17–19,23 or a slight overcorrection20–22 was achieved. In one study, treatment was stopped when a normal or corrected overjet was achieved in a mandibular retruded position,26 while three studies did not report when treatment was stopped.15,16,24
Main Results
Three studies reported 100% success rate.15,24–26 Two studies reported success rates of 87.5%20 and 92.8%,19 while in the rest of the studies the success rate was not reported.
Regardless of the treatment timing, dentoalveolar effects were generally seen. At the mandibular level, these effects were reported as mesial movement of the mandibular dentition,15,16 mesial movement18,21,22 or tipping17 of lower first molars, and proclination of lower incisors.17,18,20–23,25,26 Dentoalveolar treatment effects at the maxillary level were reported in seven studies as distal movement of the maxillary dentition,15,24 distal tipping of upper first molars,17 and/or retroclination of upper incisors.17,18,21–23,25,26 One study19 did not report any dentoalveolar treatment effects.
Significant skeletal effects were reported mainly in the studies including pubertal patients. In two investigations including pubertal25,26 and postpubertal17 patients, very little skeletal effects limited to maxillary growth restraint were observed. On the contrary, eight studies on pubertal patients reported a significant increase of mandibular length,15,16,19–22,24 with forward movement of the pogonion,18 or restraint of the maxillary growth from minimal18 to significant.20,21 Finally, two studies22,23 including postpubertal patients reported no skeletal effects. Modifications of the soft tissue profile were described in only six studies17–20,23,25 as improvement of the profile, mainly due to soft tissue pogonion/B-point advancement.
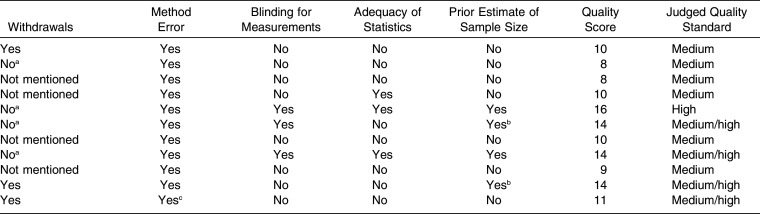
Risk of Bias in Individual Studies
The overall quality level of the studies included was medium for six studies,15–18,21,23 medium/high for four studies20,22,24–26 and high for only one study19 (Table 5). Sample description was partial in only one study.22 Prospective enrollment was clearly reported in four studies.19,22,24–26 For diagnosis, Class II description and maturational stage distribution were full in six19–22,24–26 and seven17,19–24 studies, respectively. For treatment, description was partial in only two studies.16,17 Withdrawals were declared in three studies15,24–26 and not mentioned in four studies17,18,21,23; in four studies16,19,20,22 withdrawals were not declared but were excluded according to data reported in the tables. Incomplete data outcome was seen in six studies.16,17,21–23,25,26 Method error analysis was included in all of the studies, even though one study25,26 was limited to systematic error. Blinding of measurements was followed in three studies.19,20,22 Inferential statistical analysis related to the comparisons in dental/skeletal changes between groups was judged to be adequate in three studies.18,19,22 Finally, in two studies19,22 a previous estimate of sample size was followed, while two more studies19,23 reported a posteriori power analysis.20,24
Table 5. .
Risk of Bias of the 11 Studies (12 Articles) Included in the Present Review
Table 5. .
Extended
Risk of Bias Across Studies
Among the cephalometric parameters included in the analyses, only the total and composite mandibular length changes yielded an acceptable level of heterogeneity (I2 Indexes generally below 50%). On the contrary, all of the other parameters yielded noteworthy heterogeneity (I2 Indexes generally above 60%). Therefore, meta-analysis was limited to the total and composite mandibular length changes. Results on the publication bias analyses when applicable to these parameters were nonsignificant (P > .2, at least).
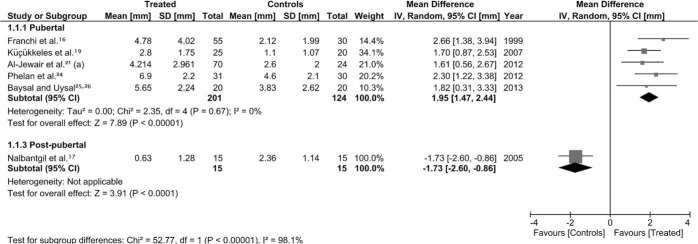
Meta-analysis
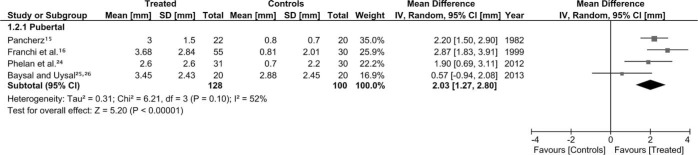
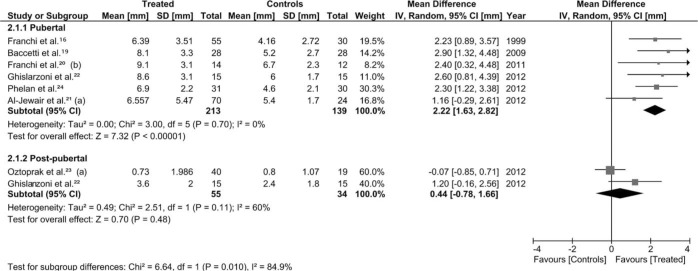
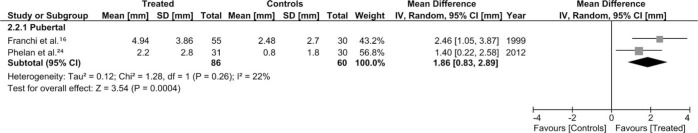
The cephalometric measurements used in each study and pooled herein for the meta-analysis are reported in Table 6, with detailed results for the meta-analysis shown in Figures 2 through 5. For the functional treatment alone, the overall total mandibular length change in pubertal patients as mean (95% CI) was 1.95 mm (1.47 to 2.44). Only one study17 on postpubertal patients treated by functional treatment alone reported a negative total mandibular length increase for the treated group of −1.73 mm (−2.60 to −0.86) (Figure 2). Regarding the composite mandibular length changes, the overall change was 2.03 mm (1.27 to 2.80) for the pubertal patients (Figure 3). For the comprehensive treatment, the overall total mandibular length changes were 2.22 mm (1.63 to 2.82) and 0.44 mm (−0.78 to 1.66) for the pubertal and postpubertal patients, respectively (Figure 4). Finally, the composite mandibular length change for the postpubertal patients was 1.86 mm (0.83 to 2.89) (Figure 5). The subgroup analysis for the total mandibular length revealed a statistically significant greater effect for the pubertal patients as compared to the postpubertal patients for the functional treatment alone (P < .001; Figure 2) but not for the comprehensive treatment (P = .10; Figure 4).
Table 6. .
The Cephalometric Measurements for Total and Composite Mandibular Length Used in Each Study and Pooled Herein for the Meta-analyses
Figure 2.
Forest plot (mean difference and 95% CI) for the total mandibular length changes (in mm) for pubertal and postpubertal subjects. (a) Pooled means and SDs from two groups compared to a single control group.
Figure 3.
Forest plot (mean difference and 95% CI) for the composite mandibular length changes (in mm) for pubertal and postpubertal subjects.
Figure 4.
Forest plot (mean difference and 95% CI) for the total mandibular length changes (in mm) for pubertal and postpubertal subjects. (a) Pooled means and SDs from two groups compared to a single control group. (b) Only pubertal subjects of the sample.
Figure 5.
Forest plot (mean difference and 95% CI) for the composite mandibular length changes (in mm) for pubertal and postpubertal subjects.
DISCUSSION
The present review is the first using the growth phase as a main selection criterion, thus allowing a comparison of the pubertal and postpubertal patients undergoing functional treatment for skeletal Class II malocclusion with fixed appliances. Moreover, only studies with matched untreated control groups were considered. However, this often implies the use of historical Class II controls mainly due to ethical issues involved in leaving patients with relevant malocclusions without orthodontic treatment during the pubertal and postpubertal growth phases. For this reason, the inclusion of CCTs has been advocated in systematic reviews.4 Thus, the retrieved studies were only CCTs without any RCTs (Table 3). Selective reporting of data was seen, as for instance success rate (Table 4), or cephalometric magnifications used reported in only seven studies.15,16,19–22,24 Therefore, studies with an improved level of quality are necessary, in terms of prospective enrollment, full description of Class II features, adequate statistical analysis, and other information on treatment and data recording (Table 5).
Heterogeneity of the selected studies was mainly seen in the treatment interventions within pubertal and postpubertal patients (treatment duration, type of appliance; Table 3). Such differences could hardly be avoided, even though the effects of fixed functional appliances alone or in combination with MBAs were analyzed separately, and random models were used herein for meta-analysis. However, studies with more homogeneity in the interventions and data reporting are necessary.
Generally, irrespective of treatment modalities, the studies that included patients treated during the pubertal growth phase indicated that this timing would be suited for functional treatment (Table 4), whereas studies with postpubertal patients clearly reported that dentoalveolar effects were responsible for the Class II correction. However, when considering the meta-analysis on the mandibular length, the subgroup comparisons between the pubertal and postpubertal patients were significant only for the functional treatment alone (P < .001; Figure 2), and close to significance for the comprehensive treatment (P = .10; Figure 4). Therefore, while skeletal effects may be expected by functional treatment in pubertal patients, more studies are necessary to fully elucidate whether these effects are significantly greater than those achievable in patients treated post puberty.
Limitation of the Review
Several studies included herein followed a retrospective enrollment for the treated groups and/or used historical control groups. The differences in functional treatment lengths, from 6 months15,18 to 18 months,21 or in the cephalometric magnifications, and the pooling of slightly different parameters expressing the total mandibular length need also to be taken into account for a critical interpretation of the meta-analysis. Therefore, while a clinically relevant mandibular elongation has been shown in pubertal patients, a precise quantification of the efficiency of such treatment with fixed functional appliances remains undetermined. The risk of bias followed herein has not been validated. Moreover, only three studies17,22,23 on postpubertal patients were retrieved; therefore, conclusions about inducible mandibular elongation at this stage should be interpreted with caution. Finally, long-term treatment stability, irrespective of the modalities followed, has yet to be evaluated.
Clinical Implications
Skeletal effects provided by fixed functional appliances in the correction of Class II malocclusion appear to be related to treatment timing. Skeletal corrections, including mandibular elongation, may be achieved if treatment is performed during the pubertal growth phase. Therefore, the use of a reliable skeletal maturity indicator would be advisable in everyday clinical practice in order to perform treatment during the pubertal growth phase, thus pursuing more skeletal effects. However, pure skeletal effects could not be expected even during puberty, as dentoalveolar effects, such as maxillary incisors retroclination and mandibular incisors proclination, are often present. Even though no significant effect in terms of mandibular elongation was seen herein for the postpubertal patients, this does not deny the existence of such effects due to the still limited data available in the literature.
CONCLUSIONS
Fixed functional treatment is effective in treating Class II malocclusion with skeletal effects when performed during the pubertal growth phase.
Both mandibular elongation and maxillary growth restraint are seen.
Skeletal effects alone would not account for the whole Class II correction, with dentoalveolar effects always present, even in patients treated during puberty.
REFERENCES
- 1.Proffit WR, Fields HW, Jr, Moray LJ. Prevalence of malocclusion and orthodontic treatment need in the United States: estimates from the NHANES III survey. Int J Adult Orthodon Orthognath Surg. 1998;13:97–106. [PubMed] [Google Scholar]
- 2.McNamara JA, Jr, Brudon WL. Ann Arbor, Mich: Needham Press; 2001. Orthodontics and dentofacial orthopedics. [Google Scholar]
- 3.Chen JY, Will LA, Niederman R. Analysis of efficacy of functional appliances on mandibular growth. Am J Orthod Dentofacial Orthop. 2002;122:470–476. doi: 10.1067/mod.2002.126730. [DOI] [PubMed] [Google Scholar]
- 4.Cozza P, Baccetti T, Franchi L, De Toffol L, McNamara JA., Jr Mandibular changes produced by functional appliances in Class II malocclusion: a systematic review. Am J Orthod Dentofacial Orthop. 2006;129:599 e1–12. doi: 10.1016/j.ajodo.2005.11.010. [DOI] [PubMed] [Google Scholar]
- 5.Marsico E, Gatto E, Burrascano M, Matarese G, Cordasco G. Effectiveness of orthodontic treatment with functional appliances on mandibular growth in the short term. Am J Orthod Dentofacial Orthop. 2011;139:24–36. doi: 10.1016/j.ajodo.2010.04.028. [DOI] [PubMed] [Google Scholar]
- 6.Baccetti T, Franchi L, McNamara JA., Jr The cervical vertebral maturation (CVM) method for the assessment of optimal treatment timing in dentofacial orthopedics. Semin Orthod. 2005;11:119–129. [Google Scholar]
- 7.Petrovic A, Stutzmann J, Lavergne J. Mechanism of craniofacial growth and modus operandi of functional appliances: a cell-level and cybernetic approach to orthodontic decision making. In: Carlson DS, editor. Craniofacial Growth Theory and Orthodontic Treatment Monograph 23 Craniofacial Growth Series. Ann Arbor, Mich: Center for Human Growth and Development, University of Michigan; 1990. pp. 13–74. [Google Scholar]
- 8.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1–34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 9.Centre for Reviews and Dissemination. Systematic Reviews CRD's Guidance for Undertaking Reviews in Healthcare. York, UK: University of York NHS Centre for Reviews & Dissemination; 2009. [Google Scholar]
- 10.Lau J, Ioannidis JP, Schmid CH. Quantitative synthesis in systematic reviews. Ann Intern Med. 1997;127:820–826. doi: 10.7326/0003-4819-127-9-199711010-00008. [DOI] [PubMed] [Google Scholar]
- 11.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 12.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pancherz H. A cephalometric analysis of skeletal and dental changes contributing to Class II correction in activator treatment. Am J Orthod. 1984;85:125–134. doi: 10.1016/0002-9416(84)90004-6. [DOI] [PubMed] [Google Scholar]
- 14.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to MetaAnalysis. Chichester, UK: John Wiley & Sons; 2009. [Google Scholar]
- 15.Pancherz H. The mechanism of Class II correction in Herbst appliance treatment. A cephalometric investigation. Am J Orthod. 1982;82:104–113. doi: 10.1016/0002-9416(82)90489-4. [DOI] [PubMed] [Google Scholar]
- 16.Franchi L, Baccetti T, McNamara JA., Jr Treatment and posttreatment effects of acrylic splint Herbst appliance therapy. Am J Orthod Dentofacial Orthop. 1999;115:429–438. doi: 10.1016/s0889-5406(99)70264-7. [DOI] [PubMed] [Google Scholar]
- 17.Nalbantgil D, Arun T, Sayinsu K, Fulya I. Skeletal, dental and soft-tissue changes induced by the Jasper Jumper appliance in late adolescence. Angle Orthod. 2005;75:426–436. doi: 10.1043/0003-3219(2005)75[426:SDASCI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.Küçükkeleş N, Ilhan I, Orgun IA. Treatment efficiency in skeletal Class II patients treated with the jasper jumper. Angle Orthod. 2007;77:449–456. doi: 10.2319/0003-3219(2007)077[0449:TEISCI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 19.Baccetti T, Franchi L, Stahl F. Comparison of 2 comprehensive Class II treatment protocols including the bonded Herbst and headgear appliances: a double-blind study of consecutively treated patients at puberty. Am J Orthod Dentofacial Orthop. 2009;135:698.e1–10; discussion 98–99. doi: 10.1016/j.ajodo.2008.03.015. [DOI] [PubMed] [Google Scholar]
- 20.Franchi L, Alvetro L, Giuntini V, Masucci C, Defraia E, Baccetti T. Effectiveness of comprehensive fixed appliance treatment used with the Forsus Fatigue Resistant Device in Class II patients. Angle Orthod. 2011;81:678–683. doi: 10.2319/102710-629.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al-Jewair TS, Preston CB, Moll EM, Dischinger T. A comparison of the MARA and the AdvanSync functional appliances in the treatment of Class II malocclusion. Angle Orthod. 2012;82:907–914. doi: 10.2319/090411-569.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ghislanzoni LT, Baccetti T, Toll D, Defraia E, McNamara JA, Jr, Franchi L. Treatment timing of MARA and fixed appliance therapy of Class II malocclusion. Eur J Orthod. 2012;35:394–400. doi: 10.1093/ejo/cjs023. [DOI] [PubMed] [Google Scholar]
- 23.Oztoprak MO, Nalbantgil D, Uyanlar A, Arun T. A cephalometric comparative study of class II correction with Sabbagh Universal Spring (SUS(2)) and Forsus FRD appliances. Eur J Dent. 2012;6:302–310. [PMC free article] [PubMed] [Google Scholar]
- 24.Phelan A, Tarraf NE, Taylor P, et al. Skeletal and dental outcomes of a new magnetic functional appliance, the Sydney Magnoglide, in Class II correction. Am J Orthod Dentofacial Orthop. 2012;141:759–772. doi: 10.1016/j.ajodo.2012.01.014. [DOI] [PubMed] [Google Scholar]
- 25.Baysal A, Uysal T. Soft tissue effects of Twin Block and Herbst appliances in patients with Class II division 1 mandibular retrognathy. Eur J Orthod. 2013;35:71–81. doi: 10.1093/ejo/cjq187. [DOI] [PubMed] [Google Scholar]
- 26.Baysal A, Uysal T. Dentoskeletal effects of Twin Block and Herbst appliances in patients with Class II division 1 mandibular retrognathy. Eur J Orthod. 2014;36:164–172. doi: 10.1093/ejo/cjt013. [DOI] [PubMed] [Google Scholar]
- 27.Küçükkeleş N, Sandalli T. Cephalometric evaluation of the therapeutic effects of the Herbst appliance in the treatment of Class II. Div I. malocclusion. J Marmara Univ Dent Fac. 1992;1:230–236. [PubMed] [Google Scholar]