Abstract
Objective:
To determine in which clinical scenarios digital models are valid as replacements for plaster models during orthodontic treatment decision-making process and treatment planning.
Materials and Methods:
An attempt to identify all pertinent published information was made. Retained articles were those where a decision-making process leading to differential orthodontic treatment plans based on either method were compared. The search was tailored for PubMed and adapted for EMBASE, MEDLINE, the Cochrane Library, LILACS, and Web of Science. A partial grey literature search was conducted through Google Scholar. References lists of the included articles were screened for potential relevant studies. The methodology of selected studies was evaluated using the Quality Assessment Tool for Diagnostic Accuracy Studies (QUADAS).
Results:
Only two studies were finally selected for the qualitative and quantitative synthesis. QUADAS results scores from selected studies ranged from 61% to 83% of 11 items evaluated. In one, the overall treatment plan regarding orthognathic surgery for Class II malocclusion changed in 13% to 22% of the cases. In the other one, 6% of the orthodontic treatment plans changed.
Conclusion:
Digital models could be used to replace plaster models in Class II malocclusion treatment planning.
Keywords: Plaster models, Digital models, Decision making, Orthodontics, Review
INTRODUCTION
In some areas of dentistry, there is a need to record and manipulate three-dimensional (3D) replicas of a patient's occlusion before making treatment decisions.1 Plaster dental models have provided dentists with a diagnosis and treatment planning tool in addition to being a 3D record of a patient's original occlusion.2 Moreover, in the education field, dental plaster models have been considered important for didactic purposes, case progress assessment, and research documentation.3
The dental plaster model is the current gold-standard reference for occlusal assessment in orthodontics3,4 and is considered a cornerstone tool for diagnosis and treatment planning.3 Its advantages range from being easy to manufacture to being inexpensive and accurate. Conversely, dental plaster models have disadvantages such as storage costs and the potential for breakage, loss, and wear.5
Digital models provide multiple advantages, such as durability,6 possibility to share images with other dentists and patients through the Internet,7 monitoring of treatment progress,1 reduced laboratory fees and chairside costs,1 electronic storage of models,8 improved patient education,9 and increased office efficiency and production.10 In contrast, major obstacles to the general use of this technology are related to cost,10 security or privacy,10 time management,10 turnaround time depending on the technology,3 and the potential that electronically stored information could be permanently lost.11
Scientific evidence consistently supports the validity of measurements from digital dental arch models.12 Studies assessing the accuracy of measurements regarding tooth size,13 arch width and length,14,15 space analysis,15,16 reconstruction of the dental cast shape,17 and relationship between arches18,19 have shown that digital dental models are reliable and credible.
Although the validity of digital vs plaster models in terms of accuracy and reliability of specific dental arch measurements has been demonstrated in previous systematic reviews,12,20 a similar critical assessment has not been conducted for overall treatment decisions about malocclusion. When assessing malocclusion, plaster models are used not only to quantify measurable occlusal features but also to observe and manipulate the patient's occlusion in three dimensions. A previous systematic review (SR)21 did investigate the use of records for orthodontic treatment planning decisions, but with a more wide scope. The purpose of this systematic review is therefore to evaluate whether the decision-making process differs when the orthodontic treatment planning is based on either plaster or digital models when the remaining orthodontic records are similar.
MATERIALS AND METHODS
This systematic review follows the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) checklist.22 A systematic review of studies that evaluated the orthodontic diagnosis and treatment planning decisions based on plaster dental models in contrast to digital dental models was undertaken. Study selection was based on the following inclusion criteria:
An orthodontic decision-making diagnosis that led to differential treatment plans based on the same patient records except for use of either plaster dental cast or digital models;
Digital models obtained from physical plaster models.
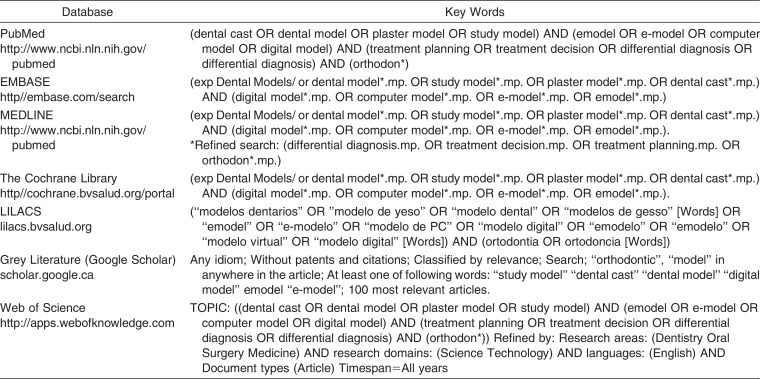
The search was tailored for PubMed and adapted for EMBASE, MEDLINE, the Cochrane Library, LILACS, and Web of Science. A partial grey literature search was conducted through Google Scholar. Searches were inclusive until June 4, 2014. Reference lists of the included articles were screened for potential relevant studies not identified through the electronic databases. Tailored truncation and word combinations were applied and adapted for each database search (Table 1).
Table 1. .
Databases and Search Terms
Two reviewers (CP and GL) independently screened the titles and abstracts identified from the electronic database results. Next, full articles were retrieved to confirm their eligibility. Researchers were not blinded to the authors and results of the study. Two investigators (CP and GL) selected articles for inclusion in the review and performed quality assessment independently. Disagreements were discussed verbally, and a third investigator (CF) was involved when necessary.
Thereafter one author (CP) performed data extraction and a second author (GL) crosschecked all the collected information. Disagreements were again discussed verbally until consensus was achieved. A third investigator was involved when necessary.
Any type of outcome measurement was considered (categoric and continuous variables). When required, authors were contacted to identify unpublished or unclear pertinent information.
Methodologic quality of selected studies was assessed through the Quality Assessment Tool of Diagnostic Accuracy Studies (QUADAS)23 checklist. Two reviewers scored the QUADAS items and assessed, independently, the quality of each included study. A third reviewer (PWM) solved potential disagreements between the two reviewers. A meta-analysis was planned if the data from different studies were relatively homogeneous and appropriate to statistical clustering.
RESULTS
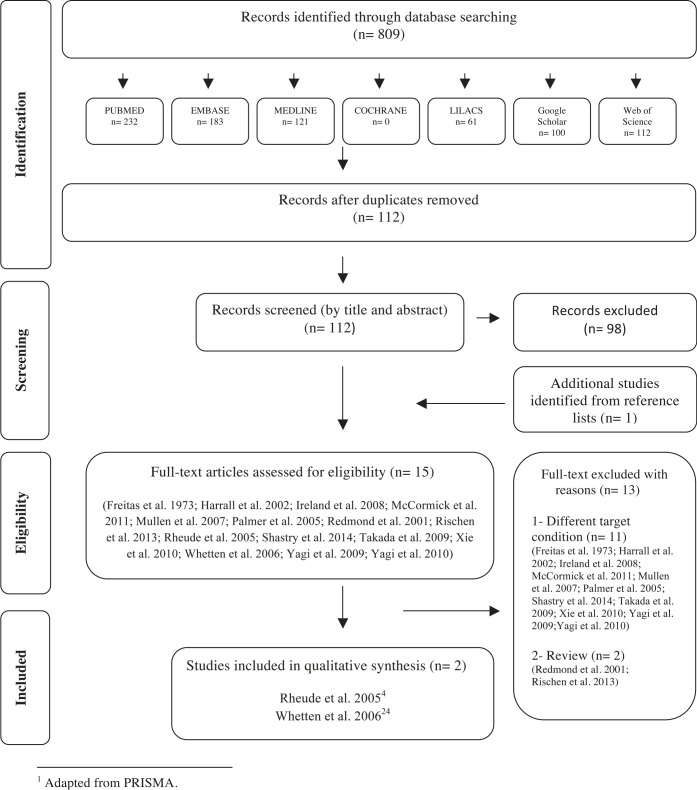
Once the selection process was completed only two articles24 remained for the qualitative and quantitative synthesis. A flow diagram of the selection process is presented in Figure 1, and a list of excluded studies with reasons for the exclusion is outlined in Appendix 1.
Figure 1.
Flow diagram of literature search and selection criteria.
Study Characteristics
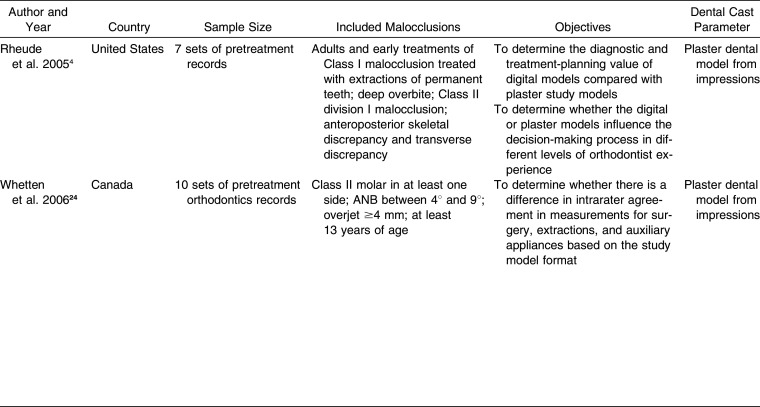
The selected studies were conducted in the United States4 and Canada.24 Both assessment groups were based in dental schools and published in English. Sample size ranged from 7 to 10 sets of records. Age of the patients, as indicated pretreatment records, was at least 13 years in one study24 but not specified in the other.4 Plaster models were made from alginate impressions, and in both studies the digital models were produced by Geodigm Corporation (e-model, Falcon Heights, MN, USA). Two sets of impressions were made for each patient, one for the plaster model and the other for digital model production. Table 2 presents the data extracted from the included studies.
Table 2. .
Summary of Descriptive Characteristics of Included Articles
Table 2. .
Extended
For the first study,4 the assessed outcome was the influence of using plaster or digital models on diagnostic descriptions, treatment plans, and the absolute need for plaster casts to be able to complete a diagnostic decision. The seven cases represented different types of malocclusions, as defined by the American Board of Orthodontics, and encompassed an early treatment case, an adult treatment case, a Class I malocclusion to be treated with extractions, a deep overbite malocclusion, a Class II division 1 malocclusion, an anteroposterior skeletal discrepancy, and a transverse discrepancy.
In the second study,24 a decision flowchart targeted agreements regarding the need for: surgery or not, extraction or not, and adoption of auxiliary appliance or not. They24 blinded the examiners and the records to maintain evaluator blindness and prevent further identification of the case during the second evaluation. Ten sets of Class II malocclusion records were selected to represent a spectrum of severity based on ANB angle between 4° and 9°, overjet ≥4 mm, age 13 years and older, and at least a half-step Class II molar relation in one side.
Significant differences between the numbers of examiners included were detected. In the first study,4 seven examiners were divided in two groups based on their level of clinical orthodontic experience. In the second study,24 31 examiners, divided in two groups, analyzed the records: an experimental group unfamiliar with digital models and a control group composed of 11 orthodontists who used digital models in treatment planning.
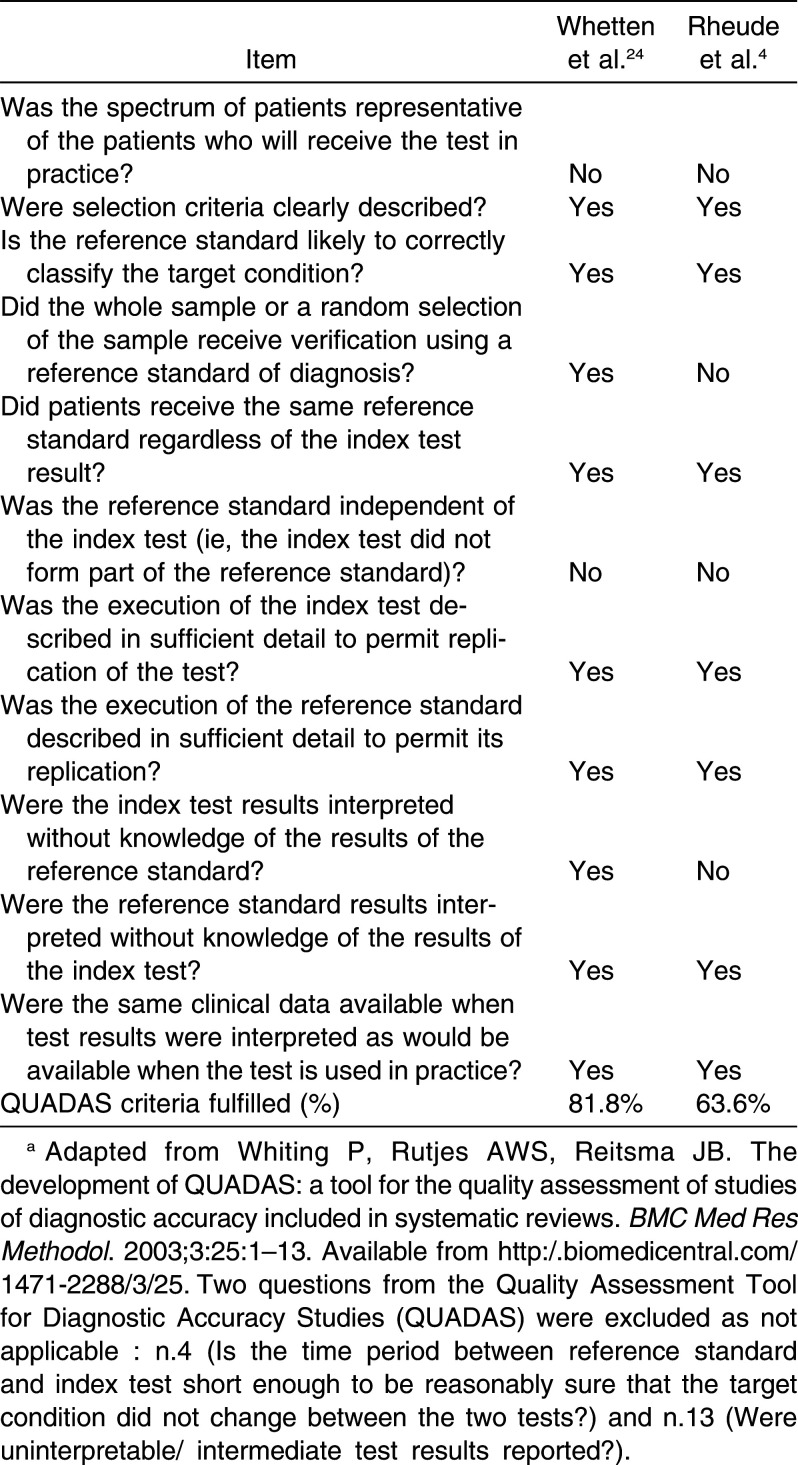
Risk of Bias Within Studies
The overall percentage of the QUADAS criteria for each study is shown in Appendix 2. The QUADAS score was 63% for one study4 and 81% for the other.24 The quality assessment score was based on 11 of the 14 items of the quality assessment. Specifically, 11 items, including patient spectrum, reference standard, verification bias, review bias, clinical review bias, incorporation bias, test execution, and indeterminate results, were analyzed by this systematic review and represent 100% of the score. The QUADAS items 4, 13, and 14 did not apply to this specific diagnostic setup. No study represented the whole spectrum of malocclusion cases properly. As in this case most of the diagnostic available information was similar, so full independence between tests could not be expected. Only 30 minutes passed between evaluations for one study,4 and recall bias could occur in such a short time span.
Synthesis of Results
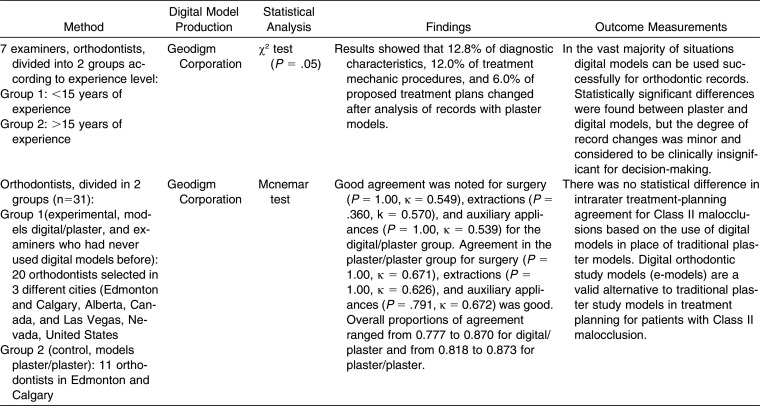
The study of Whetten et al.24 presented decision agreement for surgery, indication of extractions, and adoption of auxiliary appliances when digital models were compared with plaster models and vice versa in a spectrum of Class II malocclusion cases. Overall agreement ranged from 78% to 87% for digital vs plaster and from 82% to 87% for plaster vs plaster.
Rheude et al.4 found a statistically significant disagreement during diagnosis in 13% of the cases. In addition, disagreements were found during treatment of the same patient and during treatment mechanics selection in 6 of 49 mechanical procedures.
Both studies used e-models as digital models, and their examiners received specific training to view and manipulate the digital model's software.
Risk of Bias Across Studies
The selected studies24 used similar diagnostic methods, which reduced the possibility of misdiagnosis. They could be considered homogeneous, but they presented the data in different way. Whetten et al.24 reported only the proportion of agreement whereas Rheude et al.4 reported the number of diagnostic characteristics and treatment-planning changes. Therefore, it was not feasible to conduct a meta-analysis.
DISCUSSION
Orthodontic treatment planning is complex and requires the ability to simultaneously analyze multiple data obtained from different orthodontic diagnostic records. In this context, dental models are essential in providing a 3D record of a patient's occlusion.5 The development of an interactive 3D digital model of a patient's occlusion has been proposed as a way to greatly improve the clinician's ability to determine different treatment options, monitor changes over time, predict and display final treatment results, and measure treatment outcomes more accurately.7 Radiographs, photographs, and superimposition of images are tools that were initially nondigital but nowadays are largely optimized through the use of digital software. This systematic review found that digital dental casts could well replace conventional dental cast models for some clinical decision processes; however, complete equivalency has not been established.
Whetten et al.24 attested that digital models do not affect the treatment-planning decision in Class II malocclusions. Although discrepancies were identified when borderline surgical cases were considered, neither the digital nor the plaster model skewed the frequency of recommendation for surgery. It is noteworthy that discrepancies were also present in treatment planning for borderline surgery cases based on two sessions with plaster models.
The results of the study of Rheude et al.4 should be interpreted with caution. The sample size was small (seven cases) and represented a heterogeneous group of malocclusions. Only one case per malocclusion type was evaluated. The study design was appropriate to evaluate the degree of agreement regarding diagnosis. However, a study design without a spectrum of severity within a particular category of malocclusion does not provide enough information to evaluate equivalency of treatment plan decision-making. It was found that the frequency of variation in diagnosis between digital and plaster models decreased as the evaluator gained experience with digital models; thus, a transition phase is recommended when replacing plaster models with digital models as some software handling and understanding are required. In addition, a component of clinical experience, related to visual adjustment when using digital models and software tools, may initially affect the decision-making process.
The fact that orthodontists do not solely rely on dental models to diagnose patients and do treatment planning cannot be omitted. Therefore, the impact of changing one of the multiple diagnostic tools used during decision-making should not be overemphasized.
Two previous systematic reviews discussed the reliability of measurements from digital models compared with plaster models. Fleming et al.12 and Luu et al.20 concluded that measurements in digital models were reliable and valid. Our conclusions were different from those in the review by Rischen et al.21 The current systematic review focuses exclusively on the diagnostic implications of using either plaster or digital models while keeping the remaining records similar. In contrast to their conclusions, we do not believe that, based on the available evidence of the two included studies, it can be concluded that digital models can be used to replace plaster casts. Digital models should only be used to replace plaster models in Class II malocclusion treatment planning. Unfortunately, the included articles did not provide sufficient evidence to conclude that digital models are a valid replacement for other malocclusion types. In addition, the review by Rischen et al.21 did not analyze treatment-planning implications in depth.
Several authors have stated the benefits of accessing virtual images from patients' records. Among these benefits are easy data transmission during referral processes3,10 and time savings during treatment planning and diagnosis compared with the time required for conventional model setup and reconstruction.25 When considering the usefulness of digital models in addition to other digital orthodontic data, the decision process could be optimized by integrating 3D views of models, patient's photos, and cross-sectional anatomic images extracted from cone-beam computed tomography, thereby reducing the time spent to prepare surgical cases.26,27 It has been argued that the high definition of 3D imaging software benefits the orthodontist's decision process.28 It has not yet been proven, however. Finally, the useful application of digital technology to increase office efficiencies and reduce storage requirements is reported by orthodontists.10 However, current clinicians should enhance their acceptance behavior by adapting to new technology.29 It can be argued that this transition will not be faced by the future generation of orthodontists because they are already being trained with this technology. Several studies from the health sciences and education areas attested to the importance of using virtual patients to teach medical students.29,30 Despite the high costs linked to the implementation of technology, virtual patients are considered an effective teaching methodology.30,31 The benefits of this integrative learning approach range from education training to simulation of the consequences of clinical decision-making.
In summary, the results of this systematic review suggest that digital models are valid in treatment planning for Class II malocclusion. Additional research is needed to demonstrate the validity of digital models in treatment planning for other forms of malocclusion, such as Class III.
Some methodologic limitations of this review should be considered. First, there was no standardization regarding the methodology of the two included articles. Second, there was a significant sample-size difference. These studies do not represent the complete variation of the malocclusions faced by orthodontists. One article assessed seven sets of records4 with different malocclusion types without showcasing the malocclusion spectrum for any of these malocclusion types. The other study24 used 10 sets of records focused exclusively on a spectrum of Class II malocclusions. Future studies should include all types of molar relation and discrepancies. Issues regarding the capability of this technology to properly articulate the occlusion has been noted.3 In one of the studies only 30 minutes passed between the evaluations.4 It could be argued that the evaluators could have easily recalled their previous decision. Furthermore, digital models were assessed first followed by plaster models. The sequence of model analysis could produce a systematic bias. This study included only one case for each malocclusion category. Assessment of decision-making should evaluate multiple cases within each category. It is clear that additional research is needed to properly represent the whole malocclusion spectrum.
CONCLUSIONS
Digital models could be used to replace plaster models in Class II malocclusion treatment planning.
The included articles did not provide sufficient evidence to conclude that digital models could be used to replace plaster models in all other malocclusion types.
ACKNOWLEDGMENT
We thank Dr José Roberto Pereira for his helpful feedback.
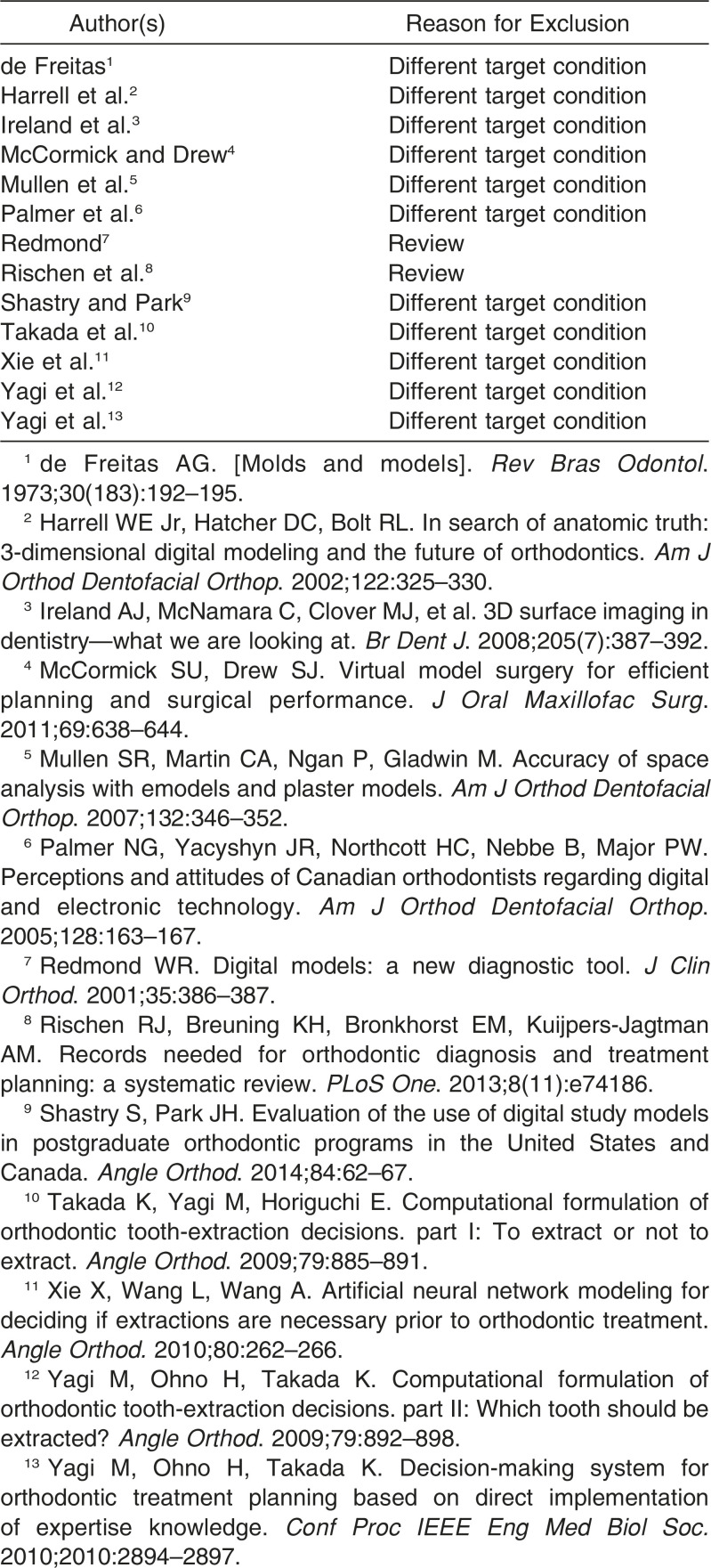
APPENDIX 1
Articles Excluded and Reasons for Exclusion
APPENDIX 2
Quality Assessment of Included Studiesa
REFERENCES
- 1.Ireland AJ, McNamara C, Clover MJ, et al. 3D surface imaging in dentistry—what we are looking at. Br Dent J. 2008;205:387–392. doi: 10.1038/sj.bdj.2008.845. [DOI] [PubMed] [Google Scholar]
- 2.Joffe L. OrthoCAD: digital models for a digital era. J Orthod. 2004;31:344–347. doi: 10.1179/146531204225026679. [DOI] [PubMed] [Google Scholar]
- 3.Shastry S, Park JH. Evaluation of the use of digital study models in postgraduate orthodontic programs in the United States and Canada. Angle Orthod. 2014;84:62–67. doi: 10.2319/030813-197.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rheude B, Sadowsky PL, Ferriera A, Jacobson A. An evaluation of the use of digital study models in orthodontic diagnosis and treatment planning. Angle Orthod. 2005;75:300–304. doi: 10.1043/0003-3219(2005)75[300:AEOTUO]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Abizadeh N, Moles DR, O'Neill J, Noar JH. Digital versus plaster study models: how accurate and reproducible are they. J Orthod. 2012;39:151–159. doi: 10.1179/1465312512Z.00000000023. [DOI] [PubMed] [Google Scholar]
- 6.Horton HM, Miller JR, Gaillard PR, Larson BE. Technique comparison for efficient orthodontic tooth measurements using digital models. Angle Orthod. 2010;80:254–261. doi: 10.2319/041709-219.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harrell WE, Hatcher DC, Bolt RL. In search of anatomic truth: 3-dimensional digital modeling and the future of orthodontics. Am J Orthod Dentofacial Orthop. 2002;122:325–330. doi: 10.1067/mod.2002.126147. [DOI] [PubMed] [Google Scholar]
- 8.Mullen SR, Martin CA, Ngan P, Gladwin M. Accuracy of space analysis with emodels and plaster models. Am J Orthod Dentofacial Orthop. 2007;132:346–352. doi: 10.1016/j.ajodo.2005.08.044. [DOI] [PubMed] [Google Scholar]
- 9.Schleyer TK, Thyvalikakath TP, Spallek H, Dziabiak MP, Johnson LA. From information technology to informatics: the information revolution in dental education. J Dent Educ. 2012;76:142–153. [PMC free article] [PubMed] [Google Scholar]
- 10.Palmer NG, Yacyshyn JR, Northcott HC, Nebbe B, Major PW. Perceptions and attitudes of Canadian orthodontists regarding digital and electronic technology. Am J Orthod Dentofacial Orthop. 2005;128:163–167. doi: 10.1016/j.ajodo.2005.02.015. [DOI] [PubMed] [Google Scholar]
- 11.State FDo. Electronic Records and Records Management Practices. 2010. Available at: http://dlis.dos.state.fl.us/RecordsManagers Accessed Jan 2014. [Google Scholar]
- 12.Fleming PS, Marinho V, Johal A. Orthodontic measurements on digital study models compared with plaster models: a systematic review. Orthod Craniofac Res. 2011;14:1–16. doi: 10.1111/j.1601-6343.2010.01503.x. [DOI] [PubMed] [Google Scholar]
- 13.Bootvong K, Liu Z, McGrath C, et al. Virtual model analysis as an alternative approach to plaster model analysis: reliability and validity. Eur J Orthod. 2010;32:589–595. doi: 10.1093/ejo/cjp159. [DOI] [PubMed] [Google Scholar]
- 14.Keating AP, Knox J, Bibb R, Zhurov AI. A comparison of plaster, digital and reconstructed study model accuracy. J Orthod. 2008;35:191–201; discussion 175. doi: 10.1179/146531207225022626. [DOI] [PubMed] [Google Scholar]
- 15.Goonewardene RW, Goonewardene MS, Razza JM, Murray K. Accuracy and validity of space analysis and irregularity index measurements using digital models. Aust Orthod J. 2008;24:83–90. [PubMed] [Google Scholar]
- 16.Leifert MF, Leifert MM, Efstratiadis SS, Cangialosi TJ. Comparison of space analysis evaluations with digital models and plaster dental casts. Am J Orthod Dentofacial Orthop. 2009;136:16 e11–14; discussion 16. doi: 10.1016/j.ajodo.2008.11.019. [DOI] [PubMed] [Google Scholar]
- 17.Hirogaki Y, Sohmura T, Satoh H, Takahashi J, Takada K. Complete 3-D reconstruction of dental cast shape using perceptual grouping. IEEE Trans Med Imaging. 2001;20:1093–1101. doi: 10.1109/42.959306. [DOI] [PubMed] [Google Scholar]
- 18.Mok CW, Zhou L, McGrath C, Hagg U, Bendeus M. Digital images as an alternative to orthodontic casts in assessing malocclusion and orthodontic treatment need. Acta Odontol Scand. 2007;65:362–368. doi: 10.1080/00016350701771850. [DOI] [PubMed] [Google Scholar]
- 19.Naidu D, Freer TJ. Validity, reliability, and reproducibility of the iOC intraoral scanner: a comparison of tooth widths and Bolton ratios. Am J Orthod Dentofacial Orthop. 2013;144:304–310. doi: 10.1016/j.ajodo.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 20.Luu NS, Nikolcheva LG, Retrouvey JM, et al. Linear measurements using virtual study models. Angle Orthod. 2012;82:1098–1106. doi: 10.2319/110311-681.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rischen RJ, Breuning KH, Bronkhorst EM, Kuijpers-Jagtman AM. Records needed for orthodontic diagnosis and treatment planning: a systematic review. PLoS One. 2013;8(11):e74186. doi: 10.1371/journal.pone.0074186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Open Med. 2009;3:e123–e130. [PMC free article] [PubMed] [Google Scholar]
- 23.Hollingworth W, Medina LS, Lenkinski RE, et al. Interrater reliability in assessing quality of diagnostic accuracy studies using the QUADAS Tool. Acad Radiol. 2006;13:803–810. doi: 10.1016/j.acra.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 24.Whetten JL, Williamson PC, Heo G, Varnhagen C, Major PW. Variations in orthodontic treatment planning decisions of Class II patients between virtual 3-dimensional models and traditional plaster study models. Am J Orthod Dentofacial Orthop. 2006;130:485–491. doi: 10.1016/j.ajodo.2005.02.022. [DOI] [PubMed] [Google Scholar]
- 25.Kuroda T, Motohashi N, Tominaga R, Iwata K. Three-dimensional dental cast analyzing system using laser scanning. Am J Orthod Dentofacial Orthop. 1996;110:365–369. doi: 10.1016/s0889-5406(96)70036-7. [DOI] [PubMed] [Google Scholar]
- 26.Xie X, Wang L, Wang A. Artificial neural network modeling for deciding if extractions are necessary prior to orthodontic treatment. Angle Orthod. 2010;80:262–266. doi: 10.2319/111608-588.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McCormick SU, Drew SJ. Virtual model surgery for efficient planning and surgical performance. J Oral Maxillofac Surg. 2011;69:638–644. doi: 10.1016/j.joms.2010.10.047. [DOI] [PubMed] [Google Scholar]
- 28.Yagi M, Ohno H, Takada K. Computational formulation of orthodontic tooth-extraction decisions. Part II: which tooth should be extracted. Angle Orthod. 2009;79:892–898. doi: 10.2319/081908-439.1. [DOI] [PubMed] [Google Scholar]
- 29.Sambasivan M, Esmaeilzadeh P, Kumar N, Nezakati H. Intention to adopt clinical decision support systems in a developing country: effect of physician's perceived professional autonomy, involvement and belief: a cross-sectional study. BMC Med Inform Dec Mak. 2012;12:142–149. doi: 10.1186/1472-6947-12-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bloice MD, Simonic KM, Holzinger A. On the usage of health records for the design of virtual patients: a systematic review. BMC Med Inform Decis Mak. 2013;13:103–110. doi: 10.1186/1472-6947-13-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huang G, Reynolds R, Candler C. Virtual patient simulation at US and Canadian medical schools. Acad Med. 2007;82:446–451. doi: 10.1097/ACM.0b013e31803e8a0a. [DOI] [PubMed] [Google Scholar]