Abstract
Background
The IMPPAC cohort (Implications of the COVID-19 pandemic on psychosocial aspects and work ability among Brazilian workers) seeks to understand the impact of the pandemic on Brazilian workers. This article describes the occupational profile, psychosocial aspects, and work ability determined during the baseline and follow-up measurements of the cohort.
Methods
Workers were invited to participate through media advertisements, social networks, and e-mails. From June to September 2020, 1211 workers were included in the cohort. Follow-up measurements finished on October 2021 with 633 workers. Data were collected through standardized questionnaires using Google Forms. Psychosocial aspects were assessed using the COPSOQ II-Br. Work ability was assessed using the Work Ability Index (WAI).
Results
At baseline and follow-up, high proportion of workers were in the risk zone with regard to work pace, emotional work demands, influence on work, work–family conflict, burnout, and stress. Approximately 75% of the workers reported good to excellent work ability at baseline and follow-up.
Conclusion
The occupational profile, psychosocial aspects, and work ability of Brazilian workers from the IMPPAC cohort were described. Psychosocial aspects and WAI were similar at baseline and follow-up.
Keywords: COPSOQ II, Mental health, Occupational health, SARS-CoV-2
1. Introduction
Workers around the world have experienced drastic changes in work conditions because of the COVID-19 pandemic. In Brazil, work sectors were split into essential and nonessential. Essential work sectors were those considered fundamental for survival, such as health care, food and drug trade, policing, supply chains, and the maintenance of electricity, gas, telephone, and sanitation; these sectors continued operating during the pandemic [1].
All essential workers have been under pressure to follow all sanitary regulations and occupational hygiene measures to reduce the biological hazard of COVID-19 contamination [2,3]. Among essential workers, healthcare providers have received special attention, as these individuals are on the forefront of the combat with the pandemic [3]. Because of the uncertainty of the prognosis and treatment for patients, especially those who develop the long COVID-19 syndrome [4], symptoms of anxiety, depression, and post-traumatic stress in healthcare providers were aggravated [5].
Workers considered nonessential were oriented to perform work activities from home. However, these individuals are more exposed to mental stressors and the imminent risk of the loss of work [6]. Increased workload and work intensity, the loss of social life, communication difficulties, reduced physical activity, care for dependents (animals, elderly or children), and a lack of breaks are some of the factors reported by workers as exerting a negative influence on mental health [7].
Pandemic coping strategies with alternating periods of greater and lesser restrictions also have affected worker health. Economic difficulties and uncertainty regarding the duration of these measures generate insecurity, anxiety, and stress during the prolonged period of isolation [8]. The loss of stability, the imminent threat of unemployment, and reduced income are also associated with a greater risk and severity of mental health symptoms [9].
Specific factors of the pandemic, such as the fear of becoming infected and the difficulty in adapting to social isolation, can provoke and aggravate mental health symptoms [10]. A study conducted in China between January and February 2020 found that 54% of workers rated the psychological impact of COVID-19 as moderate or severe, 29% reported symptoms of anxiety, and 17% reported depressive symptoms [11]. Frontline workers in Pakistan added other factors that affect mental health, such as the risk of family contamination, the fear of death from the disease, and an urgent health situation that makes it impossible to perform religious funeral rites and has altered the experience of grief [12].
Even 1 year after the onset of the pandemic, its consequences on occupational health remain uncertain. Economic effects are being observed, such as income reduction, with a consequent reduction in purchasing power and increase in poverty and hunger throughout the country [13]. Another important factor is the understanding of how changes in relationships and work can impact work ability in the face of these sudden drastic changes in the way tasks are performed [14]. Thus, the monitoring of psychosocial aspects and work ability is of considerable importance to identifying how such changes at work may affect worker health over time [4,15].
In Brazil, the first case of COVID-19 was registered on February 26, 2020, and the first death on March 17, 2020. By October 29, 2021, there were 21,793,401 confirmed cases, with 607,462 deaths. The national immunization plan began on January 17, 2021, and approximately 54% of the population was completely immunized by October 29, 2021 [16]. Thus, Brazil stands out on the world stage as one of the most impacted countries in terms of the number of people infected and killed by the disease. The direct and indirect impacts have been devastating for some sectors [17]. Delayed health effects, such as depression and anxiety, have also been identified among Brazilian women [18].
Many systematic reviews with meta-analyses about the mental health consequences of the pandemic, particularly of frontline health professionals, are available [[19], [20], [21], [22]]. However, we did not find any longitudinal study that carried out a long-term follow-up on psychosocial aspects and work ability among essential and nonessential workers.
As the pandemic continues to impact Brazil, the long-term effects of the COVID-19 outbreak on mental health and work ability should be evaluated. The IMPPAC cohort (Implications of the COVID-19 pandemic on psychosocial aspects and work ability among Brazilian workers) seeks to understand how this historically unique situation may interfere with psychosocial aspects and work ability among Brazilian workers in a 12-month follow-up. Therefore, the aim of the present paper was to describe the occupational profile of Brazilian workers as well as psychosocial aspects and work ability among the baseline and follow-up participants of the cohort from June to September 2020 (first wave) until October 2021 (end of the second wave).
2. Material and methods
2.1. Study design
A cohort study was conducted with a prospective 12-month follow-up. In this article, we present the data obtained at baseline and follow-up. The preparation of this article followed the checklist of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE statement) [23] and the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) [24].
2.2. Recruitment process
Individuals were invited to participate in the study through advertisements in the local press, social media, and invitations sent by email. Thus, the sample was selected by convenience based on the voluntary response of the participants. The intended sample size was approximately 1000 workers, based on a previous study that evaluated pain trajectories over a 12-month period [25].
The IMPPAC cohort included workers who agreed to participate in the study aged 18 years or older residing in Brazil and working in any economic sector. Students, interns, retirees, and individuals who presented inconsistent data and repeated data were excluded from the sample.
2.3. Ethical aspects
This study received approval from the Brazilian Research Ethics Committee (certificate number: 4.166.321) and was conducted in accordance with current ethical standards and resolutions.
2.4. Participants
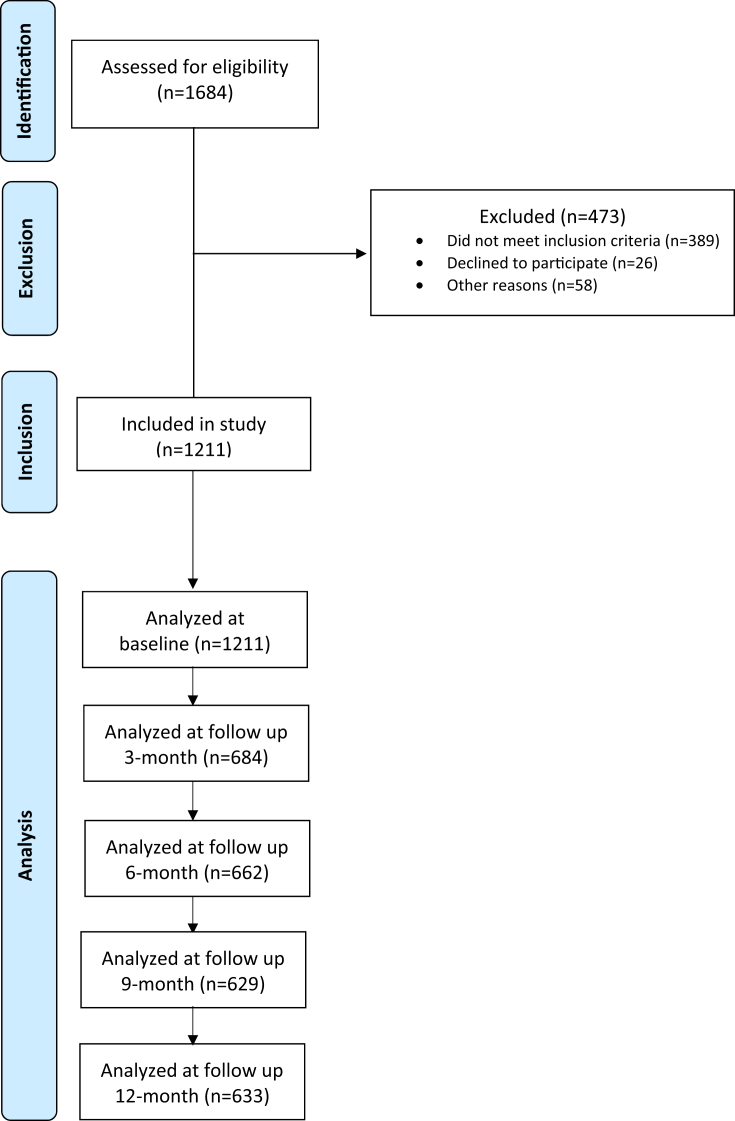
Data were collected from 1684 workers at baseline. After applying the eligibility criteria, 1211 workers were included in the cohort. The following were the reasons for exclusion: seven participants were aged <18 years; 346 were not working at the time; 34 were interns or students; two were retired; 26 declined to participate; one lived abroad; one had inconsistent data; and 56 were repeated data (Fig. 1). Most participants were from São Paulo (SP: 33.6%) and Goiás (GO: 17.3%) states. Participation from the northern and northeastern regions of the country was low (Fig. S1). At follow-up, there was a 43.5%, 45.3%, 48.1%, and 47.7% dropout rate in the 3, 6, 9, and 12 months, respectively.
Fig. 1.
Strengthening the reporting of observational studies in Epidemiology (STROBE) flow chart of study participants.
2.5. Data collection
2.5.1. Baseline
Workers answered a questionnaire addressing sociodemographic and occupational characteristics, the short version of the Copenhagen Psychosocial Questionnaire (COPSOQ II-Br) and the Work Ability Index (WAI).
The sociodemographic and occupational questionnaire was used to collect data on sex, age, marital status, education, type of employment, occupation, work sector, telework, the occurrence of coronavirus infection, among others. The questions were objective to facilitate the understanding and obtain quick answers.
The short version of COPSOQ II-Br, which has been translated and adapted to Brazilian Portuguese, was used to assess psychosocial aspects. The psychometric properties of the COPSOQ II-Br were tested, and the results revealed that the questionnaire is suitable for use on the population of Brazilian workers [26]. COPSOQ II-Br contains 40 questions addressing the following aspects: quantitative work demands, work pace, emotional work demands, influence on work, new skill development, meaningful work, commitment to the workplace, predictability, appreciation and recognition, role clarity, leadership quality, social support from superiors, job satisfaction, work–family conflict, management/worker trust, justice and respect, self-rated health, burnout, stress, unwanted sexual attention, threats of violence, physical violence, and bullying. The score is determined by the sum of the items in each of the domains, which are scored on a Likert scale, except for the offensive behavior domain. For each dimension, the score is classified as safe (green), requires attention (yellow), or health risk (red) [27].
The WAI is composed of seven items that correspond to one or more questions: (1) current ability to work with the best in life (work ability score), (2) ability to work in relation to job requirements, (3) number of current illnesses diagnosed by a physician, (3) estimated work loss because of illness, (5) absence from work in the previous year, (6) self-prognosis of work ability in 2 years, and (7) mental resources. The index is calculated by the sum of the points on each item, and the total ranges from 7 and 49 points. Work ability is then classified as low (7 to 27 points), moderate (28 to 36 points), good (37 to 43 points), or excellent (44 to 49 points) [28].
2.5.2. Follow-up
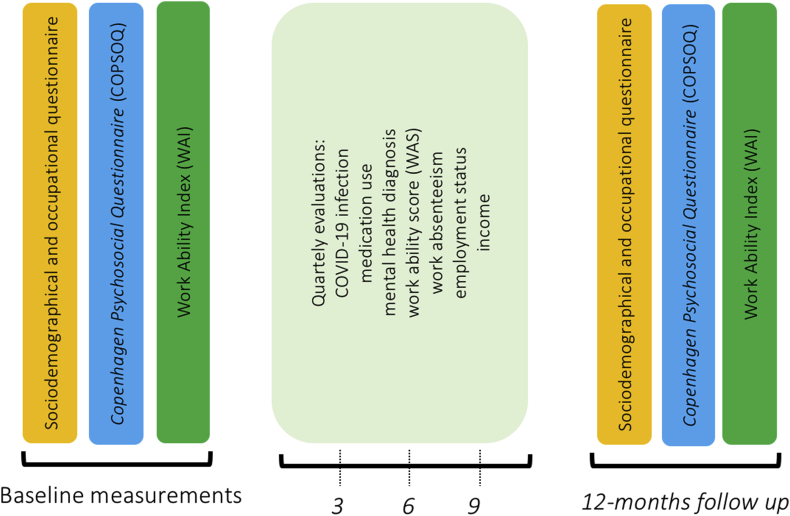
The IMPPAC cohort is composed of five assessment time points over 12 months: baseline as well as 3, 6, 9, and 12 months after the initial assessment (Fig. 2). The quarterly follow-up consists of questions related to COVID-19 infection in the participant and family, whether the worker was hospitalized and intubated; job change due to the pandemic and current income; diagnosis of psychological/psychiatric disorder, use of medications, absenteeism in the previous 3 months for any health reason, and work ability score. The last follow-up (12 months) involved the same instruments used at baseline.
Fig. 2.
Timeline for data collection and design of study.
2.6. Procedures
The questionnaires were made available using the free online software for Google accounts: Google Forms. Before starting the data collection, tests were carried out to verify the time required to answer the questionnaire and correct typographical errors. After this stage, the link to access the forms was widely publicized through social media (Facebook, Instagram, LinkedIn, and WhatsApp), email, television media, and local websites. A website was also developed, on which the participant could ask questions by email and receive informative news (https://sites.google.com/view/imppac-work/).
The forms were electronically registered and open to anyone interested in responding. There was no incentive or remuneration to participate in the study. Baseline data collection started on June 29 and ended on September 29, 2020. Follow-up data collection started on September 30, 2020, and ended on October 29, 2021.
There was no randomization or adaptation of the questions. We used standardized, validated questionnaires. The forms consisted of 17 pages of questions with 12 questions per page. An option to mark “not applicable” was included on all items, which enabled the respondent not to answer the item and pass to the next. A progress bar was included for workers to keep track of their responses.
The inclusion and exclusion criteria were applied after the questionnaires were answered. There were no incomplete questionnaires. No cookies or internet protocol (IP) collections were used, and repeated forms were excluded. The statement of informed consent was inserted in the forms using a link. A copy signed by the researcher was available for download by the participant.
2.7. Data analysis
The answers were saved on spreadsheets. Identifying information was replaced with an identification number in ascending order according to the order of responses received. Participants who answered the form more than once were identified. The time taken for the responses was not measured.
Variables from the sociodemographic and occupational questionnaire, COPSOQ II-Br, and WAI were analyzed with the aid of the SPSS software (version 26.0). Descriptive statistics (absolute [n] and relative [%] frequencies, mean and standard deviation [SD]) were performed. Stratified analysis according to COVID-19 infection status is also presented.
3. Results
3.1. Sociodemographic and occupational characteristics at baseline
Among the participants, 51.9% were women and 48.1% men. The mean age was 37.7 years (SD = 10.5), with a minimum of 18 and maximum of 75 years. Approximately 54.7% were married; 43.4% had children, and 83.1% had a higher education degree. The mean body mass index was 26.8 kg/m2 (SD = 5.0), 23.6% were obese, 5.8% reported being smokers, and 40.4% took medications. Regarding the occupational profile, 44% reported a work regimen in accordance with the Brazilian Consolidation of Labor Laws, and 41% were public servants. Most participants (41.2%) had more than 10 years in the profession. Approximately 37% worked in education, 18% worked in the healthcare field, and 7% worked in industry. Approximately 46% of the sample reported a family income of up to six times the monthly minimum wage ( US$ 1200). Approximately 56% of workers maintained their workload, 74% reported no income reduction, 74% worked from home, and 72% were afraid of becoming infected with the coronavirus. Approximately 5% reported being infected, and 21% had a family member infected with the coronavirus (see Table 1).
Table 1.
Characteristics of participants in IMPPAC cohort (n = 1211)
| Characteristics | n | % |
|---|---|---|
| Sex female | 629 | 51.9 |
| Age | ||
| 18–29 years | 280 | 23.1 |
| 30–39 years | 470 | 38.8 |
| 40–49 years | 269 | 22.2 |
| 50–59 years | 153 | 12.6 |
| 60–75 years | 39 | 3.2 |
| Marital status | ||
| Single | 475 | 39.2 |
| Married | 663 | 54.7 |
| Widower/divorced | 73 | 6.0 |
| Has children | 526 | 43.4 |
| Educational level | ||
| Low (primary education) | 18 | 1.5 |
| Middle (secondary education) | 186 | 15.4 |
| High (university degree) | 1007 | 83.1 |
| Body mass index | ||
| Underweight | 18 | 1.5 |
| Normal weight | 475 | 39.2 |
| Overweight | 432 | 35.7 |
| Obese | 286 | 23.6 |
| Smoker | 70 | 5.8 |
| Medication use | 489 | 40.4 |
| Work contract | ||
| Public servant | 496 | 41.0 |
| Self-employed | 160 | 13.2 |
| Formal contract in private sector | 533 | 44.0 |
| Informal/outsourced/owner | 21 | 1.7 |
| Job seniority | ||
| <1 year | 17 | 1.5 |
| 1–5 years | 347 | 30.9 |
| 6–10 years | 296 | 26.4 |
| ≥11 years | 462 | 41.2 |
| Work sector | ||
| Education | 450 | 37.2 |
| Health | 219 | 18.1 |
| Industry | 82 | 6.8 |
| Information technology | 77 | 6.4 |
| Nonessential trade and services | 71 | 5.9 |
| Public services | 64 | 5.3 |
| Administrative and logistic services | 48 | 4.0 |
| Attorney services | 43 | 3.6 |
| Essential trade and services | 40 | 3.3 |
| Construction | 26 | 2.1 |
| Communication and entertainment services | 22 | 1.8 |
| Bank services | 18 | 1.5 |
| Public security | 16 | 1.3 |
| Agriculture | 15 | 1.2 |
| Tourism and hospitality services | 5 | 0.4 |
| Private transportation (taxi, Uber) | 4 | 0.3 |
| Public transportation | 4 | 0.3 |
| Nongovernmental organizations | 4 | 0.3 |
| Delivery | 2 | 0.2 |
| Cleaning | 1 | 0.1 |
| Family income (US$) | ||
| Up to MMW | 20 | 1.7 |
| >1 to 3 × MMW | 218 | 18.0 |
| >3 to 6 × MMW | 322 | 26.6 |
| >6 to 9 × MMW | 194 | 16.0 |
| >9 to 12 × MMW | 174 | 14.4 |
| >12 × MMW | 223 | 18.4 |
| Not declared | 60 | 5.0 |
| Workload | ||
| Decreased | 229 | 18.9 |
| Maintained | 676 | 55.8 |
| Increased | 306 | 25.3 |
| Income | ||
| Decreased | 316 | 26.1 |
| Maintained | 895 | 73.9 |
| Work from home | 897 | 74.1 |
MMW: monthly minimum wage = R$ 1045 US$ 200.
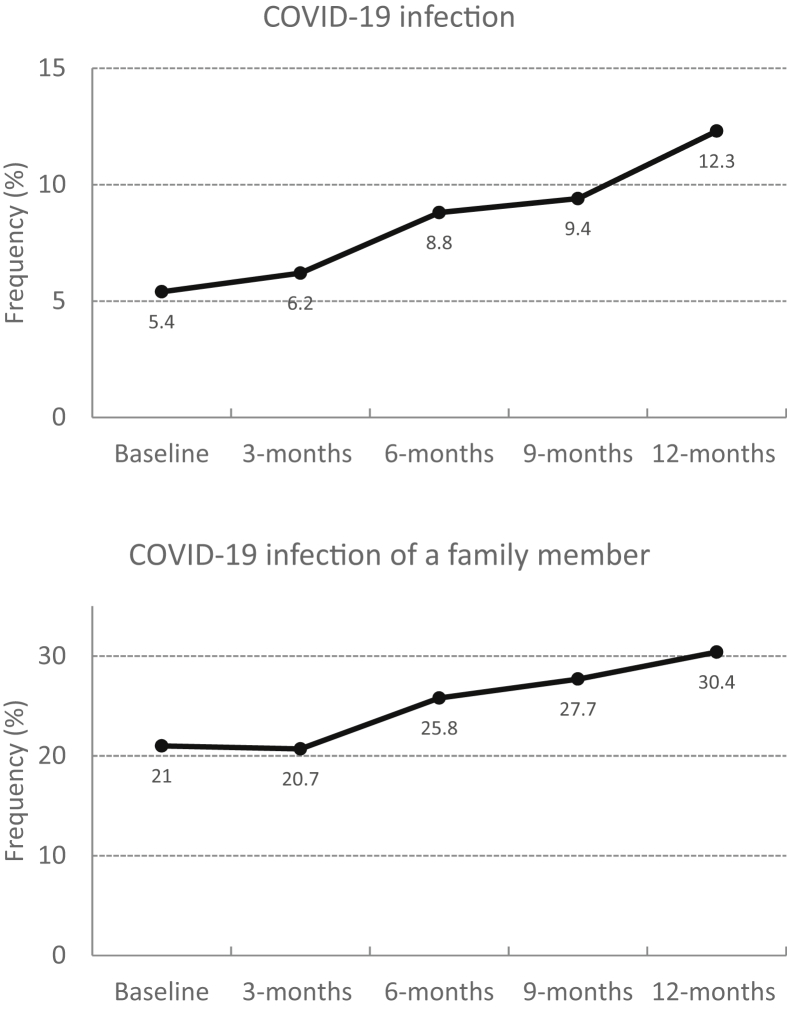
COVID-19-related variables at baseline and quarterly follow-ups are shown in Fig. 3. The infection rate increased from 5.4% at baseline to 12.3% at the 12-month follow-up. Family member infection also increased, from 21.0% to 30.4% at the same period.
Fig. 3.
COVID-19 infection and family member infection at baseline and follow-up.
3.2. Copenhagen psychosocial questionnaire
Psychosocial aspects are displayed in Table 2. At baseline, more than 75% of the workers were in the safe zone with regard to quantitative work demands, new skill development, meaningful work, commitment to the workplace, job satisfaction, management/worker trust, unwanted sexual attention, threats of violence, physical violence, and bullying. In contrast, a high proportion of workers were in the risk zone with regard to work pace, emotional work demands, influence on work, work–family conflict, burnout, and stress. These proportions were similar between infected and noninfected groups. At the 12-month follow-up, more than 75% of the workers were in the safe zone with regard to new skill development, meaningful work, commitment to the workplace, job satisfaction, management/worker trust, unwanted sexual attention, threats of violence, physical violence, and bullying. In contrast, a high proportion of workers were in the risk zone with regard to work pace, emotional work demands, influence on work, work–family conflict, burnout, and stress. These proportions were also similar between infected and noninfected groups.
Table 2.
Percentage of psychosocial risks according to COPSOQ II-Br dimensions at baseline and follow-up
| Psychosocial dimension | Safe |
Attention |
Risk |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline |
Follow-up |
Baseline |
Follow-up |
Baseline |
Follow-up |
|||||||
| - | + | - | + | - | + | - | + | - | + | - | + | |
| Quantitative work demands | 76.1 | 78.5 | 66.5 | 70.5 | 14.4 | 9.2 | 21.1 | 18.1 | 9.5 | 12.3 | 12.4 | 11.4 |
| Work pace | 17.5 | 7.7 | 17.1 | 16.1 | 33.8 | 35.4 | 36.6 | 33.6 | 48.7 | 56.9 | 46.3 | 50.3 |
| Emotional work demands | 27.2 | 23.1 | 30.8 | 25.5 | 19.7 | 12.3 | 22.5 | 20.8 | 53.1 | 64.6 | 46.7 | 53.7 |
| Influence on work | 44.4 | 41.5 | 46.7 | 40.3 | 21.2 | 27.7 | 21.5 | 26.2 | 34.4 | 30.8 | 31.8 | 33.6 |
| New skill development | 85.8 | 89.2 | 87.2 | 81.2 | 6.5 | 9.2 | 7.0 | 10.1 | 7.8 | 1.5 | 5.8 | 8.7 |
| Meaningful work | 82.4 | 89.2 | 78.5 | 80.5 | 6.1 | 4.6 | 6.0 | 5.4 | 11.5 | 6.2 | 15.5 | 14.1 |
| Commitment to the workplace | 78.5 | 86.2 | 77.1 | 79.9 | 10.2 | 3.1 | 10.7 | 6.0 | 11.3 | 10.8 | 12.2 | 14.1 |
| Predictability | 60.1 | 66.2 | 57.0 | 55.0 | 13.9 | 10.8 | 16.9 | 16.1 | 26.0 | 23.1 | 26.0 | 28.9 |
| Appreciation and recognition | 70.2 | 66.2 | 73.6 | 65.1 | 11.8 | 12.3 | 10.5 | 15.4 | 18.0 | 21.5 | 15.9 | 19.5 |
| Role clarity | 66.7 | 63.1 | 65.1 | 60.4 | 22.7 | 24.6 | 23.1 | 25.5 | 10.6 | 12.3 | 11.8 | 14.1 |
| Leadership quality | 58.2 | 72.3 | 63.4 | 55.7 | 14.7 | 9.2 | 13.4 | 19.5 | 27.1 | 18.5 | 23.1 | 24.8 |
| Social support from superiors | 49.9 | 56.9 | 52.1 | 49.0 | 28.6 | 33.8 | 30.4 | 30.2 | 21.5 | 9.2 | 17.6 | 20.8 |
| Job satisfaction | 82.0 | 84.6 | 82.0 | 83.2 | 0.0 | 0.0 | 0.0 | 0.0 | 18.0 | 15.4 | 18.0 | 16.8 |
| Work–family conflict | 42.4 | 40.0 | 38.2 | 47.7 | 11.4 | 12.3 | 12.8 | 12.8 | 46.2 | 47.7 | 49.0 | 39.6 |
| Management/worker trust | 79.9 | 84.6 | 83.3 | 81.2 | 10.6 | 4.6 | 10.7 | 6.0 | 9.4 | 10.8 | 6.0 | 12.8 |
| Justice and respect | 64.5 | 67.7 | 64.0 | 59.7 | 15.1 | 13.8 | 17.8 | 18.1 | 20.4 | 18.5 | 18.2 | 22.1 |
| Self-rated health | 53.6 | 53.8 | 50.0 | 48.3 | 35.8 | 35.4 | 37.0 | 40.3 | 10.6 | 10.8 | 13.0 | 11.4 |
| Burnout | 12.8 | 7.7 | 12.4 | 8.1 | 11.1 | 15.4 | 12.6 | 16.1 | 76.1 | 76.9 | 75.0 | 75.8 |
| Stress | 11.3 | 13.8 | 11.0 | 9.4 | 9.7 | 9.2 | 11.2 | 8.7 | 79.0 | 76.9 | 77.9 | 81.9 |
| Unwanted sexual attention | 93.5 | 86.2 | 95.7 | 91.9 | 0.0 | 0.0 | 0.0 | 0.0 | 6.5 | 13.8 | 4.3 | 8.1 |
| Threats of violence | 89.8 | 75.4 | 93.2 | 88.6 | 0.0 | 0.0 | 0.0 | 0.0 | 10.2 | 24.6 | 6.8 | 11.4 |
| Physical violence | 98.3 | 96.9 | 99.8 | 96.6 | 0.0 | 0.0 | 0.0 | 0.0 | 1.7 | 3.1 | 0.2 | 3.4 |
| Bullying | 84.7 | 75.4 | 86.6 | 89.3 | 0.0 | 0.0 | 0.0 | 0.0 | 15.3 | 24.6 | 13.4 | 10.7 |
COPSOQ, Copenhagen Psychosocial Questionnaire; −, COVID-19 negative; +, COVID-19 positive.
3.3. Work ability index
The WAI and dimensions are displayed in Table 3. At baseline and follow-up, the work ability score (WAS) was between 7.7 and 8.3 points. Work demands were also high (7.6–7.8 points). The number of diagnosed diseases was higher at baseline in comparison with the follow-up for both groups. Work loss, self-prognosis, and mental resources showed no variation between baseline and follow-up and between groups. The infected group showed a higher proportion of absenteeism, mainly between 9 and 24 days. Approximately 70–75% and of workers reported a good to excellent WAI at baseline and follow-up for both groups.
Table 3.
Work ability dimensions at baseline and follow-up
| Work ability dimensions | Baseline |
Follow-up |
||
|---|---|---|---|---|
| - | + | - | + | |
| Work Ability Score (0–10 points) | 7.8 (1.6) | 8.3 (1.3) | 7.7 (1.7) | 7.7 (1.5) |
| Work demands (1–10 points) | 7.8 (1.5) | 7.8 (1.4) | 7.6 (1.6) | 7.6 (1.5) |
| Diagnosed diseases | 1.7 (2.3) | 2.0 (3.2) | 1.2 (1.9) | 1.4 (2.5) |
| 0, n (%) | 489 (42.7) | 32 (49.2) | 273 (56.4) | 86 (57.7) |
| 1, n (%) | 211 (18.4) | 13 (20.0) | 68 (14.0) | 20 (13.4) |
| 2, n (%) | 153 (13.4) | 3 (4.6) | 48 (9.9) | 13 (8.7) |
| 3, n (%) | 122 (10.6) | 3 (4.6) | 42 (8.7) | 8 (5.4) |
| 4, n (%) | 56 (4.9) | 3 (4.6) | 13 (2.7) | 10 (6.7) |
| ≥5 | 115 (10.0) | 11 (16.9) | 40 (8.3) | 12 (8.1) |
| Work loss (1–6 points) | 5.2 (0.9) | 5.2 (0.9) | 5.2 (1.0) | 5.2 (1.0) |
| Work absenteeism | ||||
| None, n (%) | 679 (59.2) | 19 (29.2) | 300 (62.0) | 53 (35.6) |
| Up to 9 days, n (%) | 368 (32.1) | 17 (26.2) | 141 (29.1) | 49 (32.9) |
| 10–24 days, n (%) | 72 (6.3) | 23 (35.4) | 34 (7.0) | 33 (22.1) |
| 25–99 days, n (%) | 20 (1.7) | 6 (9.2) | 6 (1.2) | 11 (7.4) |
| 100–365 days, n (%) | 7 (0.6) | 0 (0.0) | 3 (0.6) | 3 (2.0) |
| Self-prognosis | ||||
| Likely, n (%) | 982 (85.7) | 54 (83.1) | 414 (85.5) | 125 (83.9) |
| Not sure, n (%) | 122 (10.6) | 8 (12.3) | 56 (11.6) | 15 (10.1) |
| Unlikely, n (%) | 42 (3.7) | 3 (4.6) | 14 (2.9) | 9 (6.0) |
| Mental resources (1–4 points) | 2.8 (0.8) | 2.9 (0.9) | 2.8 (0.9) | 2.8 (0.8) |
| Work Ability Index | 39.6 (5.5) | 39.2 (5.5) | 39.7 (5.7) | 39.0 (5.5) |
| Poor, n (%) | 28 (2.4) | 3 (4.6) | 16 (3.3) | 4 (2.7) |
| Moderate, n (%) | 264 (23.0) | 15 (23.1) | 103 (21.3) | 36 (24.2) |
| Good, n (%) | 561 (49.0) | 31 (47.7) | 219 (45.2) | 80 (53.7) |
| Excellent, n (%) | 293 (25.6) | 16 (24.6) | 146 (30.2) | 29 (19.5) |
Data are shown as mean (SD) unless otherwise specified
−, COVID-19 negative; +, COVID-19 positive.
4. Discussion
The present paper describes sociodemographic and occupational data from the IMPPAC cohort. The cohort is composed of women (52%) and men (48%), between 18 and 75 years, married (55%) and single (39%), with children (43%), a high educational level (83%), and predominantly residing in the state of São Paulo (34%). The most frequent work sector was education (37%).
The results suggest that the workers who took part in this survey were mainly young adults with a high level of education and working in the field of education. One of the factors that may explain this profile is the fact that these workers have greater digital literacy and more access to the internet. The choice of a completely online collection method is justified by the pandemic itself, which makes face-to-face contact with the participants restricted and, therefore, may have interfered with the characteristics of the cohort.
In Brazil, approximately 79% of households have internet access, and the most widely used internet access equipment is a cell phone, which is found in 99% of households with internet service [29]. As most workers have access to the internet, one may assume that those with less education were less interested in contributing to the study or had difficulties related to time and literacy that impeded answering the instruments. On the other hand, workers with more education may have a better understanding of the importance of such studies and may be more willing to contribute.
Workers with a formal contract were the majority in the sample (44% with a formal contract in the private sector and 41% with a formal contract in the public sector), which may explain the low rate of income reduction (26%). Most workers had their work routine changed to a home-office scheme, which may be associated with high levels of stress (79%) and burnout (76%). A study conducted with Canadian workers found a relationship between home office and anxiety [30]. Another study found that occupation and the change to remote work exert an influence on psychological distress [31].
Analyzing the COPSOQ results, the most affected aspects were stress, burnout, work–family conflict, emotional demands, and work pace. These findings were similar to the study of McKee [32] and indicate that workers were impacted by the COVID-19 pandemic, which may have caused an increase in work demands by increasing time spent working because of the lack of a distinction between the work and family environment, which may also explain work–family conflict. Emotional demands may be related to suffering caused by the pandemic in the case of healthcare workers or difficulties in adapting to distance learning in the case of the teachers.
A study by Wotto [33] points to social distancing as the main factor of change in learning and that the distance-education market, which requires the development of new skills, was not prepared to absorb the urgent demand. Teachers follow traditional education methods because of lack of training and practice in using technology as a teaching strategy. School closures have disproportionately harmed the most disadvantaged students, who depend on schools for a variety of social services, including health and nutrition. Furthermore, teachers needed to develop new skills, such as resilience, emotional intelligence, empathy, and collaboration despite the work overload and insecurity regarding the effectiveness of the teaching–learning process [34].
Work ability was apparently not affected by the pandemic among 75% of the workers. The 12-month follow-up also showed no difference for the WAI, for contaminated and noncontaminated workers. We did not expect to find these results, as our initial hypothesis was that the pandemic would have a negative impact on work ability. A possible explanation for these findings is the fact that most of our sample is composed of public servants with job stability and working from home. These protective factors may have contributed to the maintenance of work capacity over the 12-month follow-up.
4.1. Limitations and perspectives
The results of this cohort are important to demonstrate the effects of the COVID-19 pandemic on the health, psychosocial aspects, and work ability among workers in Brazil. We believe that this study will make contributions to the scientific community regarding knowledge of health problems caused by the COVID-19 pandemic. The study is expected to analyze the indirect effects of the pandemic and thus enable an understanding on how worker health will be impacted because of the consequences of changes in the performance of activities, job and income instability, the fear of becoming ill, overwork or loss of work, and how workers deal with these adverse situations.
A limitation of this study was the low participation of workers from informal sectors of the economy, which represent more than 40% of the economically active population in Brazil. There was also a low response rate from workers residing in the northern and northeastern regions of the country, which respectively represent around 8% and 30% of the country's population.
5. Conclusion
The IMPPAC cohort was obtained through a prospective longitudinal study design to understand the implications of the COVID-19 pandemic on the mental and physical health of Brazilian workers. A total of 1211 workers from public administration, commerce and services, education, industry, healthcare, and public services were included in the cohort. The sample was diverse in terms of sex, age, and work sector. The change in labor relations was noticeable, and it will be possible to understand the impacts of these changes on worker health and work ability over time.
Funding
This study was financed in part by the Brazilian fostering agency Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) – Finance Code 001.
Conflicts of interest
The authors declare that (1) this work was not published or submitted anywhere; (2) they do not have any conflict of interest related to this article; (3) the final version of this manuscript has been read by all authors, the requirements for authorship have been met, and each author believes that the manuscript represents honest work; (4) the authors encourage collaboration and the use of the data by other researchers. Researchers interested in using the data for scientific purposes should contact the authors.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.shaw.2021.11.004.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Brasil . Edição Extra G; 20 mar. 2020. Medida Provisória nº 926, de 20 de março de 2020.Diário Oficial [da] República Federativa do Brasil, Poder Executivo, Brasília, DF. [Google Scholar]
- 2.Agius R. COVID-19 and health at work. Occup Med. 2020;70(5):349–351. doi: 10.1093/occmed/kqaa075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burdorf A., Porru F., Rugulies R. The COVID-19 (Coronavirus) pandemic: consequences for occupational health. Scand J Work Environ Health. 2020;46(3):229–230. doi: 10.5271/sjweh.3893. [DOI] [PubMed] [Google Scholar]
- 4.Godeau D., Petit A., Richard I., Roquelaure Y. Descatha A Return-to-work, disabilities and occupational health in the age of COVID-19. Scand J Work Environ Health. 2021;47(5):408–409. doi: 10.5271/sjweh.3960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burdorf A., Porru F., Rugulies R. The COVID-19 pandemic: one year later - an occupational perspective. Scand J Work Environ Health. 2021;47(4):245–247. doi: 10.5271/sjweh.3956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Faghri P.D., Dobson M., Landsbergis P., Schnall P.L. COVID-19 pandemic what has got to do with it? J Occup Environ Med. 2021;63(4):245–247. doi: 10.1097/JOM.0000000000002154. [DOI] [PubMed] [Google Scholar]
- 7.Xiao Y., Becerik-Gerber B., Lucas G., Roll S.C. Impacts of working from home during COVID-19 pandemic on physical and mental well-being of office workstation users. J Occup Environ Med. 2020;63(3):181–190. doi: 10.1097/JOM.0000000000002097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sasangohar F., Moats J., Mehta R., Peres S.C. Disaster ergonomics: human factors in COVID-19 pandemic emergency management. Hum Factor. 2020;7(62):1061–1068. doi: 10.1177/0018720820939428. [DOI] [PubMed] [Google Scholar]
- 9.Coulombe S., Pacheco T., Cox E., Khalil C., Doucerain M.M., Auger E., Meunier S. Risk and resilience factors during the COVID-19 pandemic: a snapshot of the experiences of Canadian workers early on in the crisis. Front Psychol. 2020;11:580702. doi: 10.3389/fpsyg.2020.580702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ornell F., Schuch J.B., Sordi A.O., Kessler F.H. “Pandemic fear” and COVID-19: mental health burden and strategies. Braz J Psych. 2020;42(3):232–235. doi: 10.1590/1516-4446-2020-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nawaz M.W., Imtiaz S., Kausar E. Self-care of frontline health care workers: during COVID-19 pandemic. Psych Danubina. 2020;32(3–4):557–562. doi: 10.24869/psyd.2020.557. [DOI] [PubMed] [Google Scholar]
- 13.Ribeiro-Silva R.C., Pereira M., Campello T., Aragão E., Guimarães J.M.M., Ferreira A.J.F., Barreto M.L., Santos S.M.C. COVID-19 pandemic implications for food and nutrition security in Brazil. Cienc Saúde Coletiva. 2020;25(9):3421–3430. doi: 10.1590/1413-81232020259.22152020. [DOI] [PubMed] [Google Scholar]
- 14.Truxillo D.M., Cadiz D.M., Brady G.M. COVID-19 and its implications for research on work ability. Work Aging Retirement. 2020;6(4):242–245. doi: 10.1093/workar/waaa016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hasad I., Nurka P. Predictors of changing level of work ability index among employees of public and industrial sector. Maced J Med Sci. 2020;8(E):367–372. [Google Scholar]
- 16.World Health Organization WHO coronavirus (COVID-19) dashboard/overview/Brazil. https://covid19.who.int/region/amro/country/br Available at:
- 17.Silva-Sobrinho R.A., Zilly A., Silva R.M.M., Arcoverde M.A.M., Deschutter E.J., Palha P.F., Bernardi A.S. Coping with COVID-19 in an international border region: health and economy. Rev Latino-Am Enfermagem. 2021;29:e3398. doi: 10.1590/1518-8345.4659.3398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Feter N., Caputo E.L., Doring I.R., Leite J.S., Cassuriaga J., Reichert F.F., Silva M.C., Coombes J.S., Rombaldi A.J. Sharp increase in depression and anxiety among Brazilian adults during the COVID-19 pandemic: findings from the PAMPA cohort. Public Health. 2021;190:101–107. doi: 10.1016/j.puhe.2020.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Salari N., Khazaie H., Hosseinian-Far A., et al. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum Resour Health. 2020;18(1):100. doi: 10.1186/s12960-020-00544-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Santabárbara J., Bueno-Notivol J., Lipnicki D.M., et al. Prevalence of anxiety in health care professionals during the COVID-19 pandemic: a rapid systematic review (on published articles in Medline) with meta-analysis. Prog Neuropsychopharmacol Biol Psychiatr. 2021;107:110244. doi: 10.1016/j.pnpbp.2021.110244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bareeqa S.B., Ahmed S.I., Samar S.S., et al. Prevalence of depression, anxiety and stress in China during COVID-19 pandemic: a systematic review with meta-analysis. Int J Psychiatr Med. 2021;56(4):210–227. doi: 10.1177/0091217420978005. [DOI] [PubMed] [Google Scholar]
- 22.Busch I.M., Moretti F., Mazzi M., Wu A.W., Rimondini M. What we have learned from two decades of epidemics and pandemics: a systematic review and meta-analysis of the psychological burden of frontline healthcare workers. Psychother Psychosom. 2021;90(3):178–190. doi: 10.1159/000513733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P., STROBE Initiative The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 24.Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet e-surveys (CHERRIES) J Med Internet Res. 2004;6(3):e34. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hallman D.M., Holtermann A., Björklund G.N., Rasmussen C.D.N. Sick leave due to musculoskeletal pain: determinants of distinct trajectories over 1 year. Int Arch Occup Environ Health. 2019;92(8):1099–1108. doi: 10.1007/s00420-019-01447-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gonçalves J.S., Moriguchi C.S., Chaves T.C., Sato T.O. Cross-cultural adaptation and psychometric properties of the short version of COPSOQ II-Brazil. Rev Saude Publica. 2021;55:69. doi: 10.11606/s1518-8787.2021055003123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Silva C, Amaral V, Pereira AC, Bem-Haja P, Pereira A, Rodrigues V, Cotrim T, Silvério J, Nossa P. Copenhagen Psychosocial Questionnaire: Portugal e Países Africanos de Língua oficial Portuguesa. Aveiro: departamento de Educação, Universidade de Aveiro.
- 28.Tuomi K., Ilmarinen J., Jahkola A., Katajarinne L., Tulkki A. EdUFSCar; São Carlos: 2010. Work ability index. Translated by frida marina fischer (coord) [Google Scholar]
- 29.Brazil. Brazilian Institute of Geography and Statistics. Social Statistics . 2018. PNAD Continuous ICT 2017: internet reaches three out of four households in the country.https://agenciadenoticias.ibge.gov.br/agenciasaladeimprensa/noticias/releases/2563pnad-continua-tic-2017-internet-chega-a-tres-em-cada-quatro-domicilios-do-parents Available at: [Google Scholar]
- 30.Chee M.J., Ly N.K.K., Anisman H., Matheson K. Piece of cake: coping with COVID-19. Nutrients. 2020;12(12):3803–3823. doi: 10.3390/nu12123803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ruiz-Frutos C., Ortega-Moreno M., Allande-Cussó R., Ayuso-Murillo D., Domínguez-Salas S., Gómez-Salgado J. Sense of coherence, engagement, and work environment as precursors of psychological distress among non-health workers during the COVID-19 pandemic in Spain. Saf Sci. 2021;133:105033–105053. doi: 10.1016/j.ssci.2020.105033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McKee H., Gohar B., Appleby R., Nowrouzi-Kia B., Hagen B.N.M., Jones-Bitton A. High psychosocial work demands, decreased well-being, and perceived well-being needs within veterinary academia during the COVID-19 pandemic. Front Vet Sci. 2021;8:746716. doi: 10.3389/fvets.2021.746716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wotto M. The future high education distance learning in Canada, the United States, and France: insights from before COVID-19 secondary data analysis. J Educ Technol Syst. 2020;49(2):262–281. [Google Scholar]
- 34.D’Orville H. COVID-19 causes unprecedented educational disruption: is there a road towards a new normal? Prospects. 2020;49:11–15. doi: 10.1007/s11125-020-09475-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.