Abstract
Objectives
The aim of this study was to assess the prevalence and factors associated with COVID-19 vaccine hesitancy among health professionals (HPs) in Togo.
Study design
Cross-sectional study.
Methods
The study was conducted between 24 February and 3 March 2021 among HPs in Togo. Data on sociodemographic characteristics and intention of vaccination were collected using an online questionnaire. Willingness to get vaccinated against COVID-19 was assessed using a single item: “Would you be willing to be vaccinated against COVID-19?“. Responses were grouped into three categories: acceptance (Yes, I will get vaccinated), hesitancy (Not decided yet) and refusal (No). Multinomial regression analyses were performed to assess factors associated with vaccine hesitancy or refusal.
Results
A total of 1115 HPs (79.1% male) with a median age of 35 years were enrolled in the study. Vaccine acceptance, hesitancy and refusal were 44.1%, 32.2% and 23.7%, respectively. Female gender was associated with an increased risk of hesitancy (adjusted odds ratio [aOR] = 1.93; p = 0.005) and refusal (aOR = 1.77; p = 0.005). Participant age 50 years, having a personal history of COVID-19 infection and a good knowledge of COVID-19 vaccination were factors that reduced the risk of refusal [(aOR = 0.30; p < 0.001), (aOR = 0.43; p = 0.031) and (aOR = 0.62; p = 0.020)] or hesitancy [(aOR = 0.53; p = 0.005), (aOR = 0.13; p < 0.001) and (aOR = 0.35; p < 0.001)] of the vaccine.
Conclusions
Acceptance of the COVID-19 vaccine before the vaccination campaign was mixed among HPs, especially young HPs. Sensitisation and information campaigns should be reinforced to combat misinformation and increase COVID-19 vaccination acceptance in the context of the ongoing global pandemic.
Keywords: Vaccine hesitancy, COVID-19, Health professionals, Prevalence, Togo
1. Introduction
COVID-19, caused by SARS-CoV-2, was first identified in China in December 2019 and subsequently declared a public health emergency of international concern on 30 January 2020 [1] and later a pandemic on 11 March 2020 [2]. As of 14 February 2021, >108 million confirmed cases and >2.3 million deaths as a result of COVID-19 have been reported worldwide [3].
Until December 2020, no effective treatment or vaccine was available. Thus, in response to the pandemic, many countries implemented public health and social measures to limit the transmission of SARS-CoV-2. These measures included personal measures (e.g. frequent hand hygiene, use of face masks), physical and social distancing measures in public spaces (e.g. physical distancing of ≥1 m, reduction or cancellation of mass gatherings, avoiding crowded spaces, working from home, staying at home) and movement measures (e.g. quarantine, curfew, lockdown, cordon sanitaire) [4]. Finally, 1 year after the start of the pandemic, in December 2020, the first COVID-19 vaccines received the Emergency Use Listing from the World Health Organization (WHO) [5]. As of 18 February 2021, at least seven different vaccines have been rolled out in different countries [6]; namely, vaccines available through the following manufacturers: Moderna Biotech (Covid-19 Vaccine Moderna®), Pfizer/Biontech (Comirnaty®), Serum Institute of India (CovishieldTM), AstraZeneca (Vaxzevria®), Sinovac (COVID-19 Vaccine [Vero Cell], Inactivated/CoronavacTM), The Gamaleya National Center (Sputnik VTM) and Janssen Pharmaceuticals Companies of Johnson & Jonhson (Janssen Covid-19 vaccineTM). However, with growing vaccine hesitancy worldwide, turning these vaccines into vaccinations became a challenging public health problem.
Vaccine hesitancy is defined as the delay in acceptance or refusal of vaccination despite availability of vaccination services [7]. According to the WHO Strategic Advisory Group of Experts Working Group on vaccine hesitancy (WHO SAGE Working Group), high levels of vaccine hesitancy may lead to low vaccine demand [7], thereby jeopardising global efforts to control the pandemic. Indeed, immunisation of a critical mass of the population is crucial to curb the pandemic. In terms of COVID-19, it is estimated that the incidence of infection will start to decline when ≥67% of the population acquire immunity to SARS-CoV-2 [8]. In a systematic review published in February 2021, COVID-19 vaccine acceptance rates in the general population were highest in Ecuador (97.0%), Malaysia (94.3%), Indonesia (93.3%), China (91.3%) and South Africa (81.6%), while the lowest rates were reported in Kuwait (23.6%), Jordan (28.4%), Italy (53.7%), Russia (54.9%), the US (56.9%), France (58.9%) and Nigeria (65.2%) [9]. In healthcare settings, COVID-19 vaccine acceptance rates were 78.1% among doctors in Israel and 27.7% among doctors/nurses in the Democratic Republic of the Congo (DRC) [9].
In Togo, the first confirmed case of COVID-19 was notified on 6 March 2020 [10] and as of 14 February 2021, 5874 cases and 81 deaths had been reported [11]. Like many African countries, Togo has joined the COVAX facility and participated in the COVID-19 vaccine procurement process [12]. Vaccine from the Serum Institute of India (CovishieldTM) was the first vaccine to be made available in Togo through the COVAX facility. The campaign was launched on 10 March 2021 in Togo and the priority target for the first round of vaccination was 35,119 health professionals (HPs), followed by individuals aged ≥50 years and those living with at least one comorbidity (e.g. hypertension, diabetes, heart disease) [13].
Prior to launching the vaccination campaign, an understanding of COVID-19 vaccine hesitancy among HPs was necessary in order to prepare effective promotion strategies. Thus, the objective of this study was to assess the prevalence and factors associated with COVID-19 vaccine hesitancy among HPs in Togo.
2. Methods
2.1. Study design and setting
A cross-sectional study was conducted between 24 February and 3 March 2021 in Togo. Togo is a West African country covering a 56,800 km2 area, with an average density of 145 inhabitants per km2 [14]. In 2019, the population was 8.08 million, of which 50.2% were women [15]. Most of the population (60%) are aged ≤25 years of age and live in rural areas (62%) [15]. Togo's healthcare system has a pyramidal structure, with three levels (both for administration and healthcare delivery): central, intermediate and peripheral.
2.2. Study population and sample size
The target population included all HPs; this group were identified as a priority target group for the first round of vaccination according to the WHO recommendations. For the purpose of this study, a HP was defined as a professional who works or is affiliated with the health sector, including workers in health administration and logistics, workers in clinical settings and community health workers. All HPs aged 18 years were eligible to participate in the study.
The sample size was calculated using a single proportion population formula with a 95% confidence level (CI). Previous studies have shown that the proportion of COVID-19 vaccine refusal or hesitancy varied between 16.4% [16] and 28.8% [17]. We hypothesised that 50% of study participants would refuse or be hesitant to receive the COVID-19 vaccine, with a 3% margin error and a 10% nonresponse rate. The minimum number of participants was calculated to be 1067.
2.3. Data collection
This study developed a multiple-choice questionnaire with the following two main sections: (i) sociodemographic and professional characteristics (age, sex, working place); and (ii) intention of vaccination (willingness to get vaccinated against COVID-19, reasons of refusal or hesitancy, knowledge on COVID-19 vaccines). The questionnaire was initially pretested in 15 HPs who did not took part in the final survey. The questionnaire was self-administered and made available using an online platform through the internal communication networks of the Ministry of Health. The data collection process started 2 weeks prior to the first round of the vaccination campaign in Togo, which targeted HPs.
2.4. Definition of the outcome variable
The main outcome was the willingness to get vaccinated against COVID-19, which was assessed using a single item: “Would you be willing to be vaccinated against COVID-19?“. This item corresponds to a categorical nominal variable, with three modalities (Yes, No, Not decided yet). For the purpose of the present study, participants who answered ‘No’ were categorised as ‘vaccine refusal’ and those who answered ‘Not decided yet’ were categorised as ‘vaccine hesitancy’.
In addition, participants' knowledge on COVID-19 vaccination was ascertained using a single choice item: “On a scale of 1–10, how much would you say you know about COVID-19 vaccination?“. HPs who responded 6–10 were defined as having a ‘good level of knowledge’ (≥50% knowledge) about COVID-19 vaccination.
2.5. Data management and statistical analyses
Descriptive statistics were performed and the results are presented using frequency tabulations and percentages for categorical variables. Quantitative variables were presented as medians with their interquartile range (IQR). Chi-square test, Fisher's exact test, Kruskal-Wallis rank sum test or Wilcoxon test were used for comparison when appropriate. The proportion of participants who reported COVID-19 vaccine refusal and hesitancy were calculated with their 95% CIs.
A multinomial logistic regression model was performed to assess factors associated with COVID-19 vaccine refusal and COVID-19 vaccine hesitancy. Data analyses were performed using R© version 4.0.1 software and the level of significance was set at 5%.
3. Results
A total of 1115 HPs participated in the study.
3.1. Sociodemographic characteristics
The median age of respondents was 35 years (IQR 30–43 years) and 79.1% were male. The majority (72.6%) of HPs worked in public healthcare settings. Physicians and nurses were the most represented HP qualification groups, with 29.5% and 26.8%, respectively (Table 1).
Table 1.
Sociodemographic characteristics of health professionals in Togo (N = 1115)a.
| Characteristic | Male (n = 882) | Female (n = 233) | Overall (N = 1115) | p-Value |
|---|---|---|---|---|
| Age in years, median (IQR) | 36 (30–43) | 34 (27–42) | 35 (30–43) | 0.019d |
| Marital status | <0.001e | |||
| Living aloneb | 239 (27.1) | 100 (42.9) | 339 (30.4) | |
| Married | 643 (72.9) | 133 (57.1) | 776 (69.6) | |
| Education level | 0.150e | |||
| Less than university | 59 (6.7) | 22 (9.4) | 81 (7.3) | |
| University | 823 (93.3) | 211 (90.6) | 1034 (92.7) | |
| Region | <0.001e | |||
| Grand Lomé | 292 (33.1) | 106 (45.5) | 398 (35.7) | |
| Maritime | 140 (15.9) | 60 (25.7) | 200 (17.9) | |
| Plateaux | 157 (17.8) | 19 (8.2) | 176 (15.8) | |
| Centrale | 73 (8.3) | 10 (4.3) | 83 (7.4) | |
| Kara | 123 (13.9) | 28 (12.0) | 151 (13.6) | |
| Savanes | 97 (11.0) | 10 (4.3) | 107 (9.6) | |
| Type of healthcare setting | 0.004e | |||
| Private | 224 (25.4) | 81 (34.8) | 305 (27.4) | |
| Public | 658 (74.6) | 152 (65.2) | 810 (72.6) | |
| Qualification | 0.789f | |||
| Physician/Pharmacist/Resident | 249 (28.2) | 80 (34.3) | 329 (29.5) | |
| Nurse | 266 (30.2) | 33 (14.2) | 299 (26.8) | |
| Medical Assistant | 103 (11.7) | 15 (6.4) | 118 (10.6) | |
| Technician | 68 (7.7) | 6 (2.6) | 74 (6.6) | |
| Midwife | 1 (0.1) | 55 (23.6) | 56 (5.0) | |
| Otherc | 195 (22.1) | 44 (18.9) | 239 (21.5) | |
| Management of patients | 0.159e | |||
| Yes | 558 (63.3) | 159 (68.2) | 717 (64.3) | |
| No | 324 (36.7) | 74 (31.8) | 398 (35.7) |
IQR: interquartile range.
Data presented as n (%) unless stated otherwise.
Single/divorced/widowed.
Birth attendant/midwife, biologist, administration, physiotherapist.
Wilcoxon test.
Chi-square test.
Fisher test.
3.2. Vaccine acceptance, hesitancy and refusal
COVID-19 vaccine acceptance, hesitancy and refusal was 44.1%, 32.2% and 23.7%, respectively, in the study participants (Table 2).
Table 2.
COVID-19 vaccine acceptance, hesitancy and refusal among health professionals in Togo (N = 1115)a.
| Characteristic | Acceptance (n = 492) | Refusal (n = 264) | Hesitancy (n = 359) | Overall (N = 1115) | p-Value |
|---|---|---|---|---|---|
| Age in years, median (IQR) | 38 (32–46) | 33 (29–40) | 34 (28–41) | 35 (30–43) | <0.001f |
| Sex | <0.001d | ||||
| Male | 423 (47.9) | 199 (22.6) | 260 (29.5) | 882 | |
| Female | 69 (29.6) | 65 (27.9) | 99 (42.5) | 233 | |
| Marital status | 0.008d | ||||
| Living aloneb | 128 (37.7) | 82 (24.2) | 129 (38.1) | 339 | |
| Married | 364 (46.9) | 182 (23.5) | 230 (29.6) | 776 | |
| Education level | 0.543d | ||||
| Less than university | 35 (43.2) | 16 (19.8) | 30 (37.0) | 81 | |
| University | 457 (44.2) | 248 (24.0) | 329 (31.8) | 1034 | |
| Health region | 0.014d | ||||
| Grand Lomé | 181 (45.5) | 98 (24.6) | 119 (29.9) | 398 | |
| Maritime | 67 (33.5) | 65 (32.5) | 68 (34.0) | 200 | |
| Plateaux | 77 (43.7) | 38 (21.6) | 61 (34.7) | 176 | |
| Centrale | 46 (55.4) | 15 (18.1) | 22 (26.5) | 83 | |
| Kara | 74 (49.0) | 27 (17.9) | 50 (33.1) | 151 | |
| Savanes | 47 (43.9) | 21 (19.6) | 39 (36.5) | 107 | |
| Type of healthcare setting | 0.074d | ||||
| Private | 118 (38.7) | 77 (25.2) | 110 (36.1) | 305 | |
| Public | 374 (46.2) | 187 (23.1) | 249 (30.7) | 810 | |
| History of COVID-19 infection | <0.001d | ||||
| Not available | 53 (34.6) | 34 (22.2) | 66 (43.2) | 153 | |
| No | 390 (43.7) | 217 (24.3) | 285 (32.0) | 892 | |
| Yes | 49 (70.0) | 13 (18.6) | 8 (11.4) | 70 | |
| Family history of COVID-19 infection | 0.027d | ||||
| Don't know | 52 (36.9) | 28 (19.8) | 61 (43.3) | 141 | |
| No | 388 (45.2) | 203 (23.6) | 268 (31.2) | 859 | |
| Yes | 52 (45.2) | 33 (28.7) | 30 (26.1) | 115 | |
| Vaccination campaignc | 0.316e | ||||
| Not informed | 5 (27.8) | 6 (33.3) | 7 (38.9) | 18 | |
| Informed | 487 (44.4) | 258 (23.5) | 352 (32.1) | 1097 | |
| Level of knowledge of COVID-19 vaccination | <0.001d | ||||
| <50% | 71 (27.3) | 61 (23.5) | 128 (49.2) | 260 | |
| ≥50% | 421 (49.2) | 203 (23.8) | 231 (27.0) | 855 | |
| Management of patients | 0.112d | ||||
| Yes | 308 (43.0) | 184 (25.7) | 225 (31.4) | 717 | |
| No | 184 (46.2) | 80 (20.1) | 134 (33.7) | 398 |
IQR: interquartile range.
Data presented as n (%) unless stated otherwise.
Single/divorced/widowed.
Togolese government's vaccination campaign for health professionals against COVID-19.
Chi-square test.
Fisher test.
Kruskal-Wallis rank sum test.
Vaccine hesitancy was more frequent among women (42.5%), HPs living alone (38.1%), the Maritime region (34.0%) and HPs without a family history of COVID-19 infection (31.2%) (p < 0.05).
In terms of HPs who had been infected with COVID-19, 11.4% were hesitant to be vaccinated, while 70.0% were in favour of vaccination. For participants with no history of COVID-19 infection, 32.0% were hesitant to be vaccinated and 43.7% were likely to get vaccinated (p < 0.001).
3.3. Reasons for vaccine acceptance, hesitancy and refusal
HPs agreed to be vaccinated to protect themselves against severe forms of COVID-19 (80.7%), to contribute to herd immunity (72.0%) and to prevent transmission of the virus (54.7%). Participants who refused to be vaccinated reported that they were not confident in the vaccine (59.8%), they were not sure of its effectiveness (43.9%) and they were afraid of vaccine adverse effects (40.5%). The main reasons for vaccine hesitancy were the need to obtain more knowledge about the effectiveness of the vaccine (46.0%) and the lack of information on the vaccine (32.0%). In terms of the type of vaccine (i.e. the method the vaccine uses to create immunity), 51.0% of respondents had no preference. Preferences were for the vaccine from Germany (55.1%) and the US (47.4%), while 17.1% and 2.8% of HPs were happy to be vaccinated with vaccines from China and India, respectively.
3.4. Factors associated with COVID-19 vaccine refusal and COVID-19 vaccine hesitancy
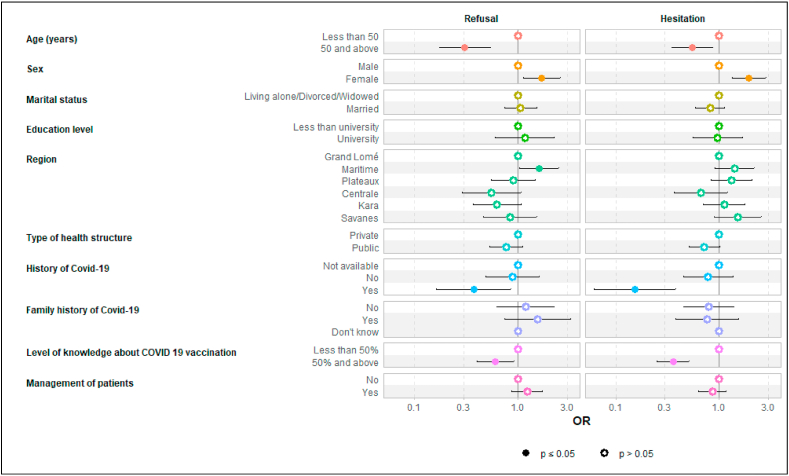
HPs aged 50 years (adjusted odds ratio [aOR] = 0.30; p < 0.001), those with a history of COVID-19 infection (aOR = 0.43; p = 0.031) and with a good knowledge of COVID-19 vaccination (≥50% level of knowledge) (aOR = 0.62; p = 0.020) were less likely to refuse COVID-19 vaccination. In contrast, female HPs (aOR = 1.77; p = 0.005) and those from the Maritime region (compared with the Grand Lomé Region) (aOR = 1.60; p = 0.034) were more likely to refuse vaccination.
Regarding vaccine hesitancy, HPs aged 50 years (aOR = 0.53; p = 0.005), those working in a public healthcare setting (aOR = 0.20; p = 0.028), those with a history of COVID-19 infection (aOR = 0.13; p < 0.001) and with a good knowledge of COVID-19 vaccination (≥50% level of knowledge) (aOR = 0.35; p < 0.001) were less likely to be hesitant about the COVID-19 vaccine. Female HPs were more likely to be hesitant about receiving the COVID-19 vaccination (aOR = 1.93; p = 0.005) (Fig. 1).
Fig. 1.
Factors associated with COVID-19 vaccine refusal and COVID-19 vaccine hesitancy. OR, odds ratio.
4. Discussion
This study was carried out among HPs in the 2 weeks prior to the vaccination campaign in Togo. We report vaccine acceptance, hesitancy and refusal of 44.1%, 32.2% and 23.7%, respectively.
We defined ‘vaccine hesitancy’ as being undecided about getting the vaccine at the time of the survey and ‘refusal’ as a clear decision to not get vaccinated. However, if we had used the definition from the WHO SAGE Working Group, vaccine hesitancy among HPs in Togo would have been twice that observed in this study. A study conducted in the Middle East Region with 864 healthcare workers reported 59.3% vaccine hesitancy based on the WHO SAGE Working Group definition [18]. A French national study reported that 28.8% of participants did not wish to be vaccinated [17]. In this latter study, refusal was defined as having said ‘no’ to the vaccine or hesitation based on the characteristics of the vaccine. Thus, comparisons between levels of vaccine hesitancy need to consider the different definitions used in the different studies.
In general, in European countries, acceptability of the COVID-19 vaccine among healthcare workers remains high, at around 70%. A study conducted in Italy among healthcare workers reported 75% vaccine acceptability [19], which is higher than results reported in our study. In France, vaccine intention was reported among 2047 HPs during the first wave of the pandemic (i.e. before the arrival of the vaccines on the market); the acceptability of a potential COVID-19 vaccine was estimated to be 76.9% [20].
Data on COVID-19 vaccine hesitancy in Africa are limited. According to a study conducted by the Centres for Disease Control and Prevention (CDC) and the London School of Tropical Medicine and Hygiene, willingness to be vaccinated in the general population ranged from 59% in the DRC to 94% in Ethiopia [21]. A literature review of 31 peer-reviewed published articles reported an acceptance rate of 81.6% in South Africa and 65.2% in Nigeria [9]. A lower vaccine acceptance (27.7%) was reported in HPs in DRC [9].
Several reasons for not getting vaccinated were provided by participants in the current study, including fear of adverse effects and doubt about the effectiveness of the vaccines. Similar results have been reported in other studies. A study in Africa reported that 25% of those who were opposed to vaccination thought that the COVID-19 vaccine was unsafe and 18% thought that vaccines in general were unsafe [21]. In France, the main reason for vaccine refusal to was fear of the adverse effects of vaccines [17]. In Africa, a section of the population does not believe in the existence of COVID-19 and considers that measures taken to respond to it are exaggerated [21]. Other factors, including misinformation campaigns through social networks, have led to an increase in doubt about the vaccine [21]. In most countries around the world, vaccine hesitation has been explained by concerns surrounding the speed of discovery of the vaccine [22,23].
Several studies have reported higher vaccine hesitancy in women [16,[24], [25], [26], [27]]. In the current study, women were also more likely to be hesitant or refuse to be vaccinated. Individuals aged 50 years are considered to be an at-risk population group for SARS-CoV-2 infection because of the high mortality observed in this age group. In a systematic review published in 2021, several studies reported that age was positively associated with vaccine acceptability and that female gender was negatively associated with vaccine uptake [9].
Frontline HPs are at increased risk of transmission of COVID-19. A study in Israel reported lower levels of vaccine hesitancy among participants who were directly involved in the management of patients with COVID-19 [23]; however no association was found in the current study. A good level of knowledge of COVID-19 vaccination was also positively associated with increased vaccine acceptability. This result suggests that continuous training of HPs on COVID-19 should be maintained in the context of a pandemic that persists over time.
This study has some limitations. The study was conducted among HPs and the results cannot not be extrapolated to the general population. However, studies have shown that attitudes of HPs towards vaccines play an important role regarding vaccine hesitancy and confidence in the safety and efficacy of vaccines in the general population [28,29]. Selection bias cannot be excluded given the online recruitment method used in this study. Indeed, in Togo in 2019, there were 56.6% male HPs [30] compared with 79.1% male participants in our study. According to a cross-sectional study in four sub-Saharan African countries, men are more likely to use computers and the Internet than women [31]. Also, selective age group participation can be explained by online recruitment with the use of a web-based questionnaire, which may be more challenging for older adults [32]. However, this approach enabled the study to cover all six health regions of Togo, to include all professional categories of HPs and to reach all age-group categories. Despite vaccine hesitancy and the recent discovery of the COVID-19 vaccine, public sensitisation may help to improve vaccine coverage. Indeed, teams from the Ministry of Health supported this sensitisation on vaccination, which ultimately resulted in an observed vaccination coverage of 95% in HPs in Togo [33]. Another limitation of this study is the lack of documentation on comorbidities, which has previously been reported to be associated with vaccine acceptability [17].
This study clearly shows that acceptance before the vaccination campaign was mixed among HPs, especially young HPs. In addition, the novelty of the COVID-19 vaccines, particularly the mRNA vaccine, and the lack of information about the vaccines may have influenced acceptance of the vaccine by HPs. Sensitisation and information campaigns remain an effective way of combating misinformation, resulting in increased acceptance of vaccination in the context of an ongoing global pandemic.
Ethical approval
Ethical approval was obtained from the national Bioethics Committee for Health Research in Togo (N°011/2021/CBRS). Informed consent was sought from participants through an note detailing the objectives of the study and an introductory consent to participate question.
Funding
This work was supported by a Non Governmental Organization, the “Centre Africain de Recherche en Epidémiologie et en Santé Publique de Lomé, Togo” (CARESP-Togo). CARESP-Togo funded the data analysis and manuscript writing.
Consent for publication
Not applicable.
Availability of data and material
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Authors' contributions
Didier Koumavi Ekouevi and Moustafa Mijiyawa conceived the study protocol. Fifonsi Adjidossi Gbeasor-Komlanvi, Kossivi Agbélénbko Afanvi, Yao Rodion Konu, Yawo Agbobli, Arnold Junior Sadio and Wendpouire Ida Carine Zida-Compaore drafted the analysis plan and wrote the first draft of the manuscript. Martin Kouame Tchankoni performed the statistical analyses. Josée Nayo-Apetsianyi, Sibabe Agoro, Aboudramane Lambokale, Dzifa Nyametso, Tchiguiri N'tapi and Kodjo Aflagah supervised the data collection. All authors contributed to data analyses through review and interpretation of the results. All authors read, revised and approved the final manuscript.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We are thankful to the health professionals who participated in this study and to the Ministry of Health of Togo who disseminated the questionnaire through its communication platforms.
References
- 1.World Health Organization, Statement on the second meeting of the International Health Regulations Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV) [Internet]. 2020 [cited 2021 Apr 26] 2005. https://www.who.int/news/item/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov Available from:
- 2.World Health Organization WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020 [Internet] 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 [cited 2021 Apr 26]. Available from.
- 3.World Health Organization Weekly epidemiological update - 16 February 2021 [Internet] 2021. https://www.who.int/publications/m/item/weekly-epidemiological-update---16-february-2021 [cited 2021 Apr 28]. Available from.
- 4.World Health Organization Overview of public health and social measures in the context of COVID-19 [Internet] 2020. https://www.who.int/publications-detail-redirect/overview-of-public-health-and-social-measures-in-the-context-of-covid-19 [cited 2021 Apr 26]. Available from:
- 5.World Health Organization WHO issues its first emergency use validation for a COVID-19 vaccine and emphasizes need for equitable global access [Internet] 2020. https://www.who.int/news/item/31-12-2020-who-issues-its-first-emergency-use-validation-for-a-covid-19-vaccine-and-emphasizes-need-for-equitable-global-access [cited 2021 Apr 28]. Available from:
- 6.World Health Organization COVID-19 vaccines [Internet] 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines [cited 2021 Apr 28]. Available from:
- 7.MacDonald N.E., SAGE Working Group on Vaccine Hesitancy Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015 Aug 14;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 8.Randolph H.E., Barreiro L.B. Herd immunity: understanding COVID-19. Immunity. 2020 May 19;52(5):737–741. doi: 10.1016/j.immuni.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines. 2021 Feb;9(2):160. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization Epidémie à Coronavirus, COVID-19, le Togo déclare un premier cas confirmé [Internet]. Regional Office for Africa. 2020. https://www.afro.who.int/fr/news/epidemie-coronavirus-covid-19-le-togo-declare-un-premier-cas-confirme [cited 2021 Apr 28]. Available from:
- 11.Togolaise République. Situation au Togo [Internet]. COVID 19. 2021. https://covid19.gouv.tg/situation-au-togo/ [cited 2021 Apr 28]. Available from.
- 12.World Health Organization Countries and multiple candidate vaccines engaged in COVID-19 vaccine Global Access Facility [Internet] 2020. https://www.who.int/news/item/24-08-2020-172-countries-and-multiple-candidate-vaccines-engaged-in-covid-19-vaccine-global-access-facility cited 2021 Apr 28]. Available from: 172.
- 13.World Health Organization COVID-19 national deployment and vaccination plan: submission and review process, 29 January 2021 [Internet] 2021. https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-NDVP-country_plans-2021.1 [cited 2021 Apr 28]. Available from:
- 14.World Bank, Data Bank. CountryProfile [Internet]. [cited 2021 Mar 26]. Available from: https://databank.worldbank.org/views/reports/reportwidget.aspx?Report_Name=CountryProfile&Id=b450fd57&tbar=y&dd=y&inf=n&zm=n&country=TGO.
- 15.Togolaise République. vol. 66p. Disponible sur; 2010. https://inseed.tg/download/2958/ (Direction Générale de la Statistique et de la Comptabilité Nationale du Togo (DGSCN). Résultats définitifs du 4ième Recensement Général de la Population et de l'Habitat (4ième RGPH4). Lomé : DGSCN). [Google Scholar]
- 16.Lin Y., Hu Z., Zhao Q., Alias H., Danaee M., Wong L.P. Understanding COVID-19 vaccine demand and hesitancy: a nationwide online survey in China. PLoS Neglected Trop. Dis. 2020 Dec 17;14(12) doi: 10.1371/journal.pntd.0008961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schwarzinger M., Watson V., Arwidson P., Alla F., Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health. 2021 Apr 1;6(4):e210–e221. doi: 10.1016/S2468-2667(21)00012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aoun A.H., Aon M.H., Alshammari A.Z., Moussa S.A. 2021 Aug 24. COVID-19 Vaccine Hesitancy among Health Care Workers in the Middle East Region.https://openpublichealthjournal.com/VOLUME/14/PAGE/352/FULLTEXT/ Open Public Health J [Internet] [cited 2021 Nov 1];14(1). Available from. [Google Scholar]
- 19.Ledda C., Costantino C., Cuccia M., Maltezou H.C., Rapisarda V. Attitudes of healthcare personnel towards vaccinations before and during the COVID-19 pandemic. Int. J. Environ. Res. Publ. Health. 2021 Jan;18(5):2703. doi: 10.3390/ijerph18052703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gagneux-Brunon A., Detoc M., Bruel S., Tardy B., Rozaire O., Frappe P., et al. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross-sectional survey. J. Hosp. Infect. 2021 Feb;108:168–173. doi: 10.1016/j.jhin.2020.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Samarasekera U. Feelings towards COVID-19 vaccination in Africa. Lancet Infect. Dis. 2021 Mar 1;21(3):324. doi: 10.1016/S1473-3099(21)00082-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coustasse A., Kimble C., Maxik K. COVID-19 and vaccine hesitancy: a challenge the United States must overcome. J. Ambul. Care Manag. 2021 Mar;44(1):71–75. doi: 10.1097/JAC.0000000000000360. [DOI] [PubMed] [Google Scholar]
- 23.Dror A.A., Eisenbach N., Taiber S., Morozov N.G., Mizrachi M., Zigron A., et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur. J. Epidemiol. 2020 Aug;35(8):775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rhodes A., Hoq M., Measey M.-A., Danchin M. Intention to vaccinate against COVID-19 in Australia. Lancet Infect. Dis. 2021 May;21(5):e110. doi: 10.1016/S1473-3099(20)30724-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roozenbeek J, Schneider CR, Dryhurst S, Kerr J, Freeman ALJ, Recchia G, et al. Susceptibility to misinformation about COVID-19 around the world. R Soc Open Sci. 7(10):201199. [DOI] [PMC free article] [PubMed]
- 26.Ward J.K., Alleaume C., Peretti-Watel P. The French public's attitudes to a future COVID-19 vaccine: the politicization of a public health issue. Soc. Sci. Med. 1982;265:113414. doi: 10.1016/j.socscimed.2020.113414. 2020 Nov. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hacquin A.-S., Altay S., Araujo E de, Chevallier C., Mercier H. PsyArXiv; 2020. Sharp Rise in Vaccine Hesitancy in a Large and Representative Sample of the French Population: Reasons for Vaccine Hesitancy.https://psyarxiv.com/r8h6z/ [Internet] [cited 2021 Apr 29]. Available from: [Google Scholar]
- 28.Paterson P., Meurice F., Stanberry L.R., Glismann S., Rosenthal S.L., Larson H.J. Vaccine hesitancy and healthcare providers. Vaccine. 2016 Dec 20;34(52):6700–6706. doi: 10.1016/j.vaccine.2016.10.042. [DOI] [PubMed] [Google Scholar]
- 29.Arda B., Durusoy R., Yamazhan T., Sipahi O.R., Taşbakan M., Pullukçu H., et al. Did the pandemic have an impact on influenza vaccination attitude? a survey among health care workers. BMC Infect. Dis. 2011 Apr 7;11:87. doi: 10.1186/1471-2334-11-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ministère de la Santé et de l'Hygiène Publique du Togo. Annuaire des statistiques sanitaires-Année. 2019. p. 127.https://pdfhost.io/edit?doc=9380a1a1-8097-4159-a96c-54ac8486f4ea [Internet] Available from: [Google Scholar]
- 31.Yaya S., Ghose B. Patterns of computer and Internet use and its association with HIV knowledge in selected countries in sub-Saharan Africa. PLoS One. 2018 Jun 27;13(6) doi: 10.1371/journal.pone.0199236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kelfve S., Kivi M., Johansson B., Lindwall M. Going web or staying paper? The use of web-surveys among older people. BMC Med. Res. Methodol. 2020 Oct 8;20(1):252. doi: 10.1186/s12874-020-01138-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Togolaise République. Bulletin d’information N°2); 2021. Ministère de la Santé, de l'Hygiène Publique et de l'Accès universel aux Soins. Vaccination du personnel de santé du pays contre la COVID-19; p. 4p. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.