Abstract
Purpose
Considering the risk of coronavirus disease (COVID-19) transmission through infected droplets, emergency department (ED) operations in response to febrile patients should be planned. We investigated the general and clinical characteristics of febrile patients visiting the ED and changes in admission rates via the ED during the COVID-19 outbreak.
Materials and Methods
We performed a retrospective analysis of prospectively collected patients who visited 402 EDs in the Republic of Korea with febrile symptoms between January 27 and May 31, 2020 and compared them to those enrolled before the COVID-19 outbreak. The primary outcome was admission rate; the secondary outcome was length of stay (LOS) in the ED.
Results
In total, 266519 patients had febrile symptoms at ED presentation after the COVID-19 outbreak. In 2019, before the outbreak, there were 437762 patients. The rate of ED visits among pediatric patients (aged <15 years) decreased to 21.4% after the COVID-19 outbreak, compared with 41.8% in 2019. The proportion of patients admitted after ED management was higher after the outbreak (31.3%) than before (25.2%). The adjusted odds ratio for admission was 1.04 (95% confidence interval: 1.02–1.05) after the outbreak. Compared to before the COVID-19 outbreak, the median ED LOS increased by 16 min after the outbreak.
Conclusion
This study confirmed that admission rates and ED LOS increased for febrile patients visiting the ED after the COVID-19 outbreak. This could provide evidence for developing ED-related strategies in response to the ongoing COVID-19 outbreak and other infectious disease pandemics.
Keywords: COVID-19, emergency service, fever
INTRODUCTION
Febrile symptoms are one of the main clinical complaints observed in 5% of all patients and 15% of older patients in the emergency department (ED).1 The high-risk febrile patient group comprises individuals aged >65 years or those with chronic disease and accounts for approximately 70%–90% of hospitalization cases and 7%–9% of 30-day mortality cases.2 Therefore, in the ED, these individuals should be appropriately classified, and emergency treatment should be provided according to severity. Coronavirus disease (COVID-19) is currently prevalent worldwide, and 71%–78% of COVID-19 patients experience fever as a major symptom.3
The COVID-19 outbreak has caused major changes in terms of ED responses to febrile patients with suspected COVID-19.4 In the ED, the evaluation and management of critical patients should be rapidly performed while simultaneously isolating patients and preventing secondary transmission. Accordingly, more ED resources are consumed and more time is spent in the management of febrile patients with COVID-19.5,6 The spread of COVID-19 through respiratory droplet transmission has raised concerns regarding the need to secure ED resources and plan for ED operations in response to febrile patients.7
Studies that analyzed clinical characteristics and outcomes focusing on febrile patients visiting the ED during the COVID-19 outbreak are rare, and none have been specifically conducted with national data. The objective of this study was to investigate the general and clinical characteristics of febrile patients in the ED and to analyze changes in admission rates via the ED during the COVID-19 outbreak. The study results could provide information that might help in enhancing ED operations during another pandemic or epidemic.
MATERIALS AND METHODS
Study design and setting
This retrospective observational study was performed with a prospectively collected nationwide dataset from the National Emergency Medical Center (NEMC) in the Republic of Korea. The present study adhered to the STROBE statement8 and the principles embodied in the Declaration of Helsinki, and the study procedure was approved by the Institutional Review Board of the National Medical Center (approval number NMC-2007-026). The requirement for informed consent was waived because data were collected in an anonymized form and did not include personally identifiable information.
Korea is divided administratively and geographically into 17 provinces, and EDs are evenly distributed in a hierarchical structure in each province. EDs are designated as level 1, 2, or 3 by the Ministry of Health and Welfare, and the designation is based on the ED's human resources, emergency equipment, and availability of medical services and specialists.9 In South Korea, the first case of COVID-19 was reported on January 20, 2020, and a total of 11468 cases of COVID-19 have been confirmed as of May 2020.10 The Korean government declared the third stage of an infectious disease crisis beginning on January 27, 2020. The third stage was declared when it was confirmed that a new type of infectious disease introduced into a domestic area had been transmitted to a region or person. The epidemic curve of the cumulative number of cases had plateaued in April 2020.11 Notably, on February 18, 2020, the COVID-19 outbreak in South Korea began in Daegu/Gyeongbuk, and it spread mainly among a religious group called Shincheonji.12 This region was the hub of the COVID-19 outbreak, with the highest number of cases in South Korea (8210 of 11468 cases) nationwide (71.6%) during the study period.13
Study population
This study evaluated all consecutive patients with febrile symptoms between January 27, 2020 and May 31, 2020 after COVID-19 and compared them with those before COVID-19 in 2019. Patients with cardiac arrest at the time of ED arrival were excluded from the study. Febrile symptoms were defined as the presence of at least one code in the main symptom column among 66 codes filtered by fever, febrile, and hyperthermia or a recorded temperature of ≥37.5℃ in the body temperature column at the time of ED visit using an automated computer system.
Data resources and collection
The present study was conducted using data from the Korean National ED Information System (NEDIS). All patients visiting EDs in Korea are required to enroll with the NEDIS. It is a nationwide registry for monitoring indicators of emergency medical care by collecting medical information from all EDs in real time and for providing basic resources for policy establishment.14 Patient information transmitted to the central server of the NEDIS from each ED is classified into seven tables. Among them, information on age, sex, ED region, ED level, reason for visit, visiting route, insurance status, vital signs, Korea triage and acuity scale (KTAS) level, symptom duration, disposition, admission unit, and ED length of stay (LOS) was extracted from the emergency treatment history table. The KTAS consists of five acuity levels: level 1 (resuscitation) to level 5 (non-urgent).15 Insurance status is divided into five stages. Medical care type 1 is provided to recipients of basic livelihood aid; they do not need to pay for medical expenses. Medical care type 2 is provided to recipients of conditional livelihood aid; they need to pay 15% of medical expenses. Fever focus of the study subjects was classified into six categories using the discharge diagnosis column in the discharge diagnosis table.
This nationwide registry is managed according to the standardized protocol distributed by the NEMC and has been revised several times until January 2019 since its establishment in 2003; recently, it has been updated to version 3.2. Data transmission errors are automatically screened on the central server in real time, and the administrator is supposed to manually review and retransmit transmission errors that occur in each ED. Administrators are supposed to be regularly trained in standardized registry management.
Outcome measures
The primary outcome was the admission rate after emergency care. Data from the disposition after emergency care column from the NEDIS was classified into four categories: admission, discharge, transfer, and death. Data are configured in such a way that information on patient disposition could be automatically transmitted to the NEDIS from each ED within 2 weeks. It is not possible to track patients who have passed through multiple EDs in one event with data from NEDIS because the NEDIS information obtained from each hospital excludes personally identifiable information. The secondary outcome was LOS in the ED.
Statistical analyses
Continuous variables were analyzed using the independent-sample t-test or the Wilcoxon rank-sum test, and categorical variables were analyzed and compared using the chi-square or Fisher's exact tests. To investigate associations between the effect of the COVID-19 outbreak and rate of admission among febrile patients, adjusted odds radios with 95% confidence intervals of the primary outcome were calculated using multivariable logistic regression. We adjusted for sex, age, KTAS level, visiting route, insurance status, ED region, reason for visit, and ED level as potential confounding factors in the analysis. These variables exhibited a significant association with the independent (COVID-19 outbreak) and the dependent (admission rate) variables in univariable logistic regression analysis. Subgroup analysis was performed to confirm the study outcomes according to age, sex, KTAS level, and ED region using the chi-square test (the rate of admission) or the Mann-Whitney U test (ED LOS).
RESULTS
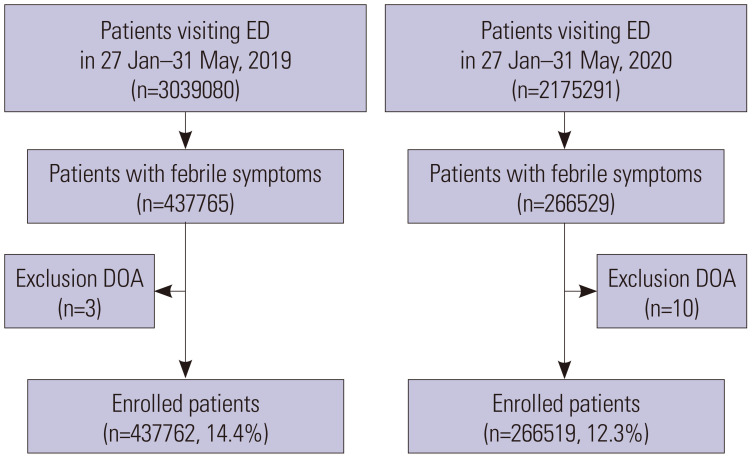
From January 27 to May 31, 2020, a total of 2175291 patients visited EDs in Korea. Among them, 266519 (12.3%) with febrile symptoms at ED presentation were included. Meanwhile, 3039080 patients visited the EDs between January 27 and May 31, 2019; of these, 437762 (14.4%) patients who had febrile symptoms were included in the present study (Fig. 1). Table 1 shows a comparison of general and clinical characteristics between the two periods. The rate of ED visits in patients aged <15 years decreased to 21.4% after the COVID-19 outbreak, compared with that of 41.8% before the COVID-19 outbreak.
Fig. 1. Flowchart of the patient enrollment process. ED, emergency department; DOA, death on arrival.
Table 1. Patient Demographics.
| Variables | Overall (n=704281) | 2019 (n=437762) | 2020 (n=266519) | p value | |
|---|---|---|---|---|---|
| Age | <0.001 | ||||
| <15 year | 239943 (34.1) | 182930 (41.8) | 57013 (21.4) | ||
| 15–65 year | 328106 (46.6) | 183054 (41.8) | 145052 (54.4) | ||
| >65 year | 136231 (19.3) | 71777 (16.4) | 64454 (24.2) | ||
| Not recorded | 0 | ||||
| Sex | <0.001 | ||||
| Male | 365493 (51.9) | 225765 (51.6) | 139728 (52.4) | ||
| Female | 338788 (48.1) | 211997 (48.4) | 126791 (47.6) | ||
| Not recorded | 1 | ||||
| Insurance status | <0.001 | ||||
| National health insurance | 652870 (92.9) | 409753 (93.7) | 243117 (91.7) | ||
| Medical care type I | 27650 (3.9) | 14872 (3.4) | 12778 (4.8) | ||
| Medical care type II | 6017 (0.9) | 3717 (0.8) | 2300 (0.9) | ||
| No insurance | 6647 (0.9) | 3975 (0.9) | 2672 (1.0) | ||
| Others | 9358 (1.3) | 5203 (1.2) | 4155 (1.6) | ||
| Not recorded | 1739 | ||||
| Reason for visit | <0.001 | ||||
| Medical problem | 666022 (94.7) | 418337 (95.8) | 247685 (93.0) | ||
| External factor | 37248 (5.3) | 18565 (4.2) | 18683 (7.0) | ||
| Not recorded | 1011 | ||||
| Visiting route | <0.001 | ||||
| EMS | 91394 (13.0) | 46701 (10.7) | 44693 (16.8) | ||
| Direct visit | 518630 (73.6) | 336683 (76.9) | 181947 (68.3) | ||
| Transferred | 81924 (11.6) | 48293 (11.0) | 33631 (12.6) | ||
| Others | 12333 (1.8) | 6085 (1.4) | 6248 (2.3) | ||
| Not recorded | 0 | ||||
| KTAS | <0.001 | ||||
| Level 1 | 4831 (0.7) | 2537 (0.6) | 2294 (0.9) | ||
| Level 2 | 32118 (4.6) | 18957 (4.4) | 13161 (5.0) | ||
| Level 3 | 311684 (45.0) | 192394 (44.7) | 119290 (45.5) | ||
| Level 4 | 320897 (46.3) | 203878 (47.4) | 117019 (44.7) | ||
| Level 5 | 22982 (3.3) | 12712 (3.0) | 10270 (3.9) | ||
| Not recorded | 11769 | ||||
| ED region | <0.001 | ||||
| Daegu/Gyeongbuk | 60770 (8.6) | 38466 (8.8) | 22304 (8.4) | ||
| Others | 643511 (91.4) | 399296 (91.2) | 244215 (91.6) | ||
| Not recorded | 0 | ||||
| ED level | <0.001 | ||||
| Level 1 | 200540 (28.5) | 121204 (27.7) | 79336 (29.8) | ||
| Level 2 | 397287 (56.4) | 247546 (56.5) | 149741 (56.2) | ||
| Level 3 | 106454 (15.1) | 69012 (15.8) | 37442 (14.0) | ||
| Not recorded | 0 | ||||
| Disposition | <0.001 | ||||
| Discharge | 493879 (70.5) | 319344 (73.0) | 174535 (66.3) | ||
| Transfer | 13145 (1.9) | 7449 (1.7) | 5696 (2.2) | ||
| Admission | 192513 (27.5) | 110113 (25.2) | 82400 (31.3) | ||
| Death | 937 (0.1) | 397 (0.1) | 540 (0.2) | ||
| Not recorded | 3807 | ||||
| Admission unit | <0.001 | ||||
| General ward | 150015 (82.8) | 90597 (87.6) | 59418 (76.5) | ||
| Intensive care unit | 18139 (10.0) | 9937 (9.6) | 8202 (10.6) | ||
| General isolation ward | 10024 (5.5) | 2405 (2.3) | 7619 (9.8) | ||
| Intensive care isolation unit | 2555 (1.4) | 364 (0.4) | 2191 (2.8) | ||
| Others | 347 (0.2) | 128 (0.1) | 219 (0.3) | ||
| Not recorded | 523201 | ||||
| ED LOS (minutes), median (interquartile) | 136.0 [72.0, 247.0] | 131.0 [74.0,227.0] | 147.0 [68.0,286.0] | <0.001 | |
| Symptom duration (hours), median (interquartile) | 14.3 [4.0,4 3.0] | 14.9 [4.2,43.5] | 13.4 [3.6,42.0] | <0.001 | |
EMS, emergency medical service; KTAS, Korean triage and acuity scale; ED, emergency department; LOS, length of stay.
Data are presented as n (%).
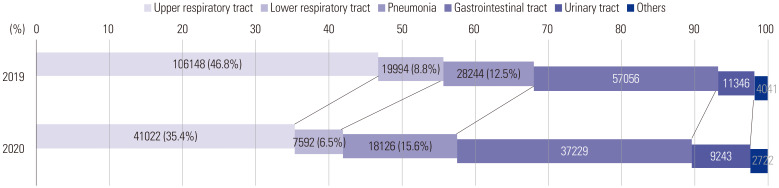
The proportion of patients who were hospitalized after treatment in the ED was higher after the COVID-19 outbreak (31.3%) than before the outbreak (25.2%). The proportion of patients admitted to the intensive care unit after ED increased to 13.4% after the COVID-19 outbreak, compared with 10.0% before the outbreak, and the proportion of patients admitted to the isolation unit increased from 2.7% to 12.6%. After the COVID-19 outbreak in 2020, the median ED LOS increased by 16 min, compared with that before the outbreak in 2019. Among the study subjects, the proportion of patients with respiratory tract infection as a discharge diagnosis at the ED decreased from 55.6% before the COVID-19 outbreak to 41.9% after the COVID-19 outbreak; however, the proportion of patients with pneumonia as the discharge diagnosis at the ED increased from 12.5% to 15.6% (Fig. 2). Multivariable logistic regression analysis was performed to confirm whether the COVID-19 outbreak was associated with admission rates after ED management (Table 2). The results indicated that the COVID-19 outbreak had an effect in terms of increasing admission rates after ED management, compared with that before the outbreak in 2019 (p<0.01).
Fig. 2. Change in the proportion of enrolled patients with a focus on fever during the coronavirus disease (COVID-19) outbreak.
Table 2. Adjusted Odds Ratios for Admission Rate.
| Univariable analysis | Multivariable analysis | ||||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | p value | OR | 95% CI | p value | ||
| Year | |||||||
| 2019 | Ref | Ref | |||||
| 2020 | 1.33 | 1.32–1.35 | <0.001 | 1.04 | 1.02–1.05 | <0.001 | |
| Age | |||||||
| <15 year | 0.65 | 0.64–0.65 | <0.001 | 0.59 | 0.58–0.60 | <0.001 | |
| 15–65 year | Ref | Ref | |||||
| >65 year | 5.29 | 5.22–5.36 | <0.001 | 3.33 | 3.28–3.38 | <0.001 | |
| Sex | |||||||
| Male | Ref | Ref | |||||
| Female | 1.06 | 1.05–1.07 | <0.001 | 1.10 | 1.09–1.12 | <0.001 | |
| KTAS | |||||||
| Level 1 | Ref | Ref | |||||
| Level 2 | 0.54 | 0.50–0.57 | <0.001 | 0.90 | 0.83–0.97 | <0.005 | |
| Level 3 | 0.19 | 0.18–0.20 | <0.001 | 0.38 | 0.36–0.41 | <0.001 | |
| Level 4 | 0.07 | 0.07–0.07 | <0.001 | 0.19 | 0.18–0.21 | <0.001 | |
| Level 5 | 0.05 | 0.04–0.05 | <0.001 | 0.11 | 0.10–0.12 | <0.001 | |
| Visiting route | |||||||
| EMS | Ref | Ref | |||||
| Direct visit | 0.25 | 0.25–0.25 | <0.001 | 0.55 | 0.54–0.56 | <0.001 | |
| Transferred | 2.17 | 2.12–2.21 | <0.001 | 2.90 | 2.83–2.96 | <0.001 | |
| Others | 1.83 | 1.76–1.90 | <0.001 | 2.61 | 2.50–2.72 | <0.001 | |
| Insurance status | |||||||
| National health insurance | Ref | <0.001 | Ref | ||||
| Medical care type I | 2.83 | 2.76–2.90 | <0.001 | 1.46 | 1.42–1.50 | <0.001 | |
| Medical care type II | 0.80 | 0.75–0.85 | <0.001 | 1.00 | 0.93–1.07 | 0.935 | |
| General | 0.49 | 0.46–0.53 | <0.001 | 0.53 | 0.49–0.57 | <0.001 | |
| Others | 1.08 | 1.04–1.13 | <0.001 | 1.14 | 1.08–1.21 | <0.001 | |
| Reason of visit | |||||||
| Disease | Ref | Ref | |||||
| Non-disease | 0.87 | 0.85–0.90 | <0.001 | 0.75 | 0.73–0.78 | <0.001 | |
| ED level | |||||||
| Level 1 | Ref | Ref | |||||
| Level 2 | 0.70 | 0.69–0.71 | <0.001 | 0.94 | 0.93–0.95 | <0.001 | |
| Level 3 | 0.40 | 0.40–0.41 | <0.001 | 0.78 | 0.76–0.80 | <0.001 | |
| ED region | |||||||
| Others | Ref | Ref | |||||
| Daegu/Gyeongbuk | 1.07 | 1.05–1.09 | <0.001 | 0.97 | 0.95–0.99 | <0.009 | |
OR, odds ratio; CI, confidence interval; KTAS, Korean triage and acuity scale; EMS, emergency medical service; ED, emergency department.
We performed subgroup analysis according to age, sex, and severity to more closely investigate the effect of the COVID-19 outbreak on admission rate and ED LOS. Subgroup analysis was also conducted to confirm the effect in Daegu city/Gyeongbuk province, where a massive regional outbreak occurred during the study period. We found that the difference in admission rate after COVID-19 was greater in the <15 years age group (4.2%) than in the other age groups. In addition, admission rates in the KTAS 2 and KTAS 3 groups after the outbreak increased by 7.9% and 9.4%, respectively, compared with that before the outbreak (Fig. 3). ED LOS also increased significantly in patients >65 years of age and in patients with high KTAS levels (KTAS level 3 or higher). Notably, the median value increased by 115 min in the KTAS level 1 patient group requiring immediate resuscitation (p<0.01). We confirmed that the Daegu-Gyeongbuk region was associated with a longer ED LOS (p<0.01) (Fig. 4).
Fig. 3. Subgroup analysis of admission rates. KTAS, Korean triage and acuity scale; ED, emergency department.
Fig. 4. Subgroup analysis on ED LOS. KTAS, Korean triage and acuity scale; ED, emergency department; LOS, length of stay.
DISCUSSION
The present study confirmed that the general and clinical characteristics of patients visiting the ED with febrile symptoms during the COVID-19 outbreak period differed from those of patients visiting before the outbreak using nationwide data. The total number of patients who visited the ED with febrile symptoms significantly decreased; in particular, the proportion of pediatric patients decreased significantly. A decline in the number of patients visiting the ED during the COVID-19 outbreak has been reported in previous studies performed in other countries.16,17,18 In the planning of an effective ED response strategy to epidemic outbreaks such COVID-19, understanding the characteristics of the patients presenting to the ED with symptoms requiring evaluation for the disease would be extremely helpful. In this study, we confirmed that the number of ED visits among individuals <15 years decreased. In Korea, the government has implemented intensive policies, including social distancing and behavior changes, and citizens are instructed to perform good personal hygiene, such as wearing a mask, washing hands, and not participating in gatherings, to prevent local disease transmission during the COVID-19 outbreak.19 Additionally, the government has closed schools, which may be associated with the decrease in ED visits among patients aged <15 years. In Korea, there is a pattern of an increase in the number of pediatric patients visiting the ED with febrile symptoms from December to March, which overlaps with the annual influenza epidemic,20 and public gatherings could promote the spread of respiratory infections21,22 Therefore, it is possible that these policies have had an effect on blocking the transmission of respiratory infectious diseases with febrile symptoms.
The present study confirmed that the admission rate of ED patients with febrile symptoms increased after the COVID-19 outbreak. This is because the proportion of patients with high severity increased during this period. The present study shows that the proportion of patients with relatively less critical infections in the upper or lower respiratory tract has decreased during the ongoing COVID-19 outbreak. Accordingly, we can assume that the increased proportion of admission rates may be related with a decrease in unnecessary ED visits. In addition, the significant increase in ED LOS identified in the present study is consistent with the findings of previous studies. Chua, et al.18 reported that ED waiting times increased regardless of the severity of patients. In addition, a study performed at the ED in a tertiary hospital in China confirmed that a high workload for fever screening caused a delay in resuscitation and that the time spent on actual treatment was reduced.23 They also explained that the increased time taken to screen for COVID-19 was associated with a delay in definitive care for critically ill patients or migration to the intensive care unit increased the likelihood of poor outcomes. Moreover, a delay in responding to suspected COVID-19 cases may inadvertently cause collateral damage, such as an increase in in-hospital cardiac arrest incidence in the ED.24 The present study results showed that the COVID-19 outbreak has elicited an increase in ED LOS in older patients and patients with high KTAS levels. Since these groups are more likely to progress to a critically ill stage, their increased ED LOS could cause more fatal outcomes than that of other groups. In addition, we confirmed that the increase in ED LOS in the region with a large number of confirmed cases (Daegu/Gyeongbuk) was greater than that in other regions. It is presumed that the influx of patients with suspected COVID-19 in these regions increased rapidly and that ED resources were saturated and insufficient to meet the increased load. Therefore, when a life-threatening infectious disease such as COVID-19 outbreak occurs, it is necessary to rearrange ED resources to respond to an increased admission rate and to prevent adverse effects of a prolonged ED LOS on patients with febrile symptoms.25,26
The ED plays a dual important role in responding to large-scale infectious diseases in the community. Since a large number of patients with suspected infectious diseases are present in the community, the ED plays a role in preemptively screening patients and isolating them quickly. Simultaneously, proper management for critically ill patients, which is the natural purpose of the ED, should not be compromised owing to an epidemic.24 Accordingly, the increase in ED LOS observed in our results suggests that a strategy for preventing transmission in the ED is needed. Screening and triage of patients with suspected infection using a non-face-to-face treatment system secures the safety of medical staff and increases the evaluation time while reducing patient waiting times in the ED.27 Therefore, the present study could provide evidence for developing such strategies.
The present study has some limitations. Although our study used a prospectively collected nationwide dataset, there is a possibility of potential bias due to the retrospective study design. In particular, variables not collected by NEDIS could not be assessed in regards to their association between COVID-19 and admission rates. Across countries, febrile patients with suspected COVID-19 have different epidemiological characteristics, and quarantine policies for them also differ.28 Therefore, it would not be prudent to generalize the results of the present study to other regions. ED disposition and ED LOS are also nonclinical measures and do not fully provide information on a patient's clinical condition or outcomes. Lastly, we could not confirm whether the patient had undergone real-time polymerase chain reaction (RT-PCR) testing to confirm COVID-19. The RT-PCR test could be associated with ED LOS.
In summary, our study determined the characteristics of febrile patients admitted to the ED during the COVID-19 outbreak on a nationwide basis and confirmed that the admission rate and ED LOS increased. It is expected that these efforts will help to improve the ED process in response to the ongoing COVID-19 outbreak, as well as to any future infectious disease pandemics. Also, our data may help improve the development of related policies by relevant authorities.
Footnotes
The authors have no potential conflicts of interest to disclose.
- Conceptualization: Seung Joon Lee, Hyun Wook Ryoo, and Ji Hoon Kim.
- Data curation: Seung Joon Lee and Yun-Suk Pak.
- Formal analysis: Seung Joon Lee and Yun-Suk Pak.
- Methodology: Hyeon Chang Kim, Seung Joon Lee, and Ji Hoon Kim.
- Project administration: Ji Hoon Kim.
- Resources: Yun-Suk Pak.
- Software: Seung Joon Lee.
- Supervision: Hyun Wook Ryoo.
- Visualization: Arom Choi.
- Writing—original draft: Seung Joon Lee, Arom Choi, and Ji Hoon Kim.
- Writing—review & editing: all authors.
- Approval of final manuscript: all authors.
DATA AVAILABILITY
The data are available on request from the lead author.
References
- 1.DeWitt S, Chavez SA, Perkins J, Long B, Koyfman A. Evaluation of fever in the emergency department. Am J Emerg Med. 2017;35:1755–1758. doi: 10.1016/j.ajem.2017.08.030. [DOI] [PubMed] [Google Scholar]
- 2.Ron W, Robert H, Marianne GH. Rosen's emergency medicine: concepts and clinical practice. 9th ed. Philadelphia: Elsevier; 2018. [Google Scholar]
- 3.Peyrony O, Marbeuf-Gueye C, Truong V, Giroud M, Rivière C, Khenissi K, et al. Accuracy of emergency department clinical findings for diagnosis of coronavirus disease 2019. Ann Emerg Med. 2020;76:405–412. doi: 10.1016/j.annemergmed.2020.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park M, Cook AR, Lim JT, Sun Y, Dickens BL. A systematic review of COVID-19 epidemiology based on current evidence. J Clin Med. 2020;9:967. doi: 10.3390/jcm9040967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Teo KC, Leung WCY, Wong YK, Liu RKC, Chan AHY, Choi OMY, et al. Delays in stroke onset to hospital arrival time during COVID-19. Stroke. 2020;51:2228–2231. doi: 10.1161/STROKEAHA.120.030105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pessoa-Amorim G, Camm CF, Gajendragadkar P, De Maria GL, Arsac C, Laroche C, et al. Admission of patients with STEMI since the outbreak of the COVID-19 pandemic: a survey by the European Society of Cardiology. Eur Heart J Qual Care Clin Outcomes. 2020;6:210–216. doi: 10.1093/ehjqcco/qcaa046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wee LE, Fua TP, Chua YY, Ho AFW, Sim XYJ, Conceicao EP, et al. Containing COVID-19 in the emergency department: the role of improved case detection and segregation of suspect cases. Acad Emerg Med. 2020;27:379–387. doi: 10.1111/acem.13984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med. 2007;4:e297. doi: 10.1371/journal.pmed.0040297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim EN, Kim MJ, You JS, Shin HJ, Park IC, Chung SP, et al. Effects of an emergency transfer coordination center on secondary overtriage in an emergency department. Am J Emerg Med. 2019;37:395–400. doi: 10.1016/j.ajem.2018.05.060. [DOI] [PubMed] [Google Scholar]
- 10.Korea Disease Control and Prevention Agency. Korea Disease Control and Prevention Agency report for status on domestic occurrence of COVID-19. [accessed on 2020 June 1]. Available at: https://www.kdca.go.kr/board/board.es?mid=a20501000000&bid=0015&list_no=367381&cg_code=&act=view&nPage=146 .
- 11.Kang CR, Lee JY, Park Y, Huh IS, Ham HJ, Han JK, et al. Coronavirus disease exposure and spread from nightclubs, South Korea. Emerg Infect Dis. 2020;26:2499–2501. doi: 10.3201/eid2610.202573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park JY, Han MS, Park KU, Kim JY, Choi EH. First pediatric case of coronavirus disease 2019 in Korea. J Korean Med Sci. 2020;35:e124. doi: 10.3346/jkms.2020.35.e124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee JY, Hong SW, Hyun M, Park JS, Lee JH, Suh YS, et al. Epidemiological and clinical characteristics of coronavirus disease 2019 in Daegu, South Korea. Int J Infect Dis. 2020;98:462–466. doi: 10.1016/j.ijid.2020.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kang DY, Cho KJ, Kwon O, Kwon JM, Jeon KH, Park H, et al. Artificial intelligence algorithm to predict the need for critical care in prehospital emergency medical services. Scand J Trauma Resusc Emerg Med. 2020;28:17. doi: 10.1186/s13049-020-0713-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee JH, Park YS, Park IC, Lee HS, Kim JH, Park JM, et al. Over-triage occurs when considering the patient's pain in Korean Triage and Acuity Scale (KTAS) PLoS One. 2019;14:e0216519. doi: 10.1371/journal.pone.0216519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Westgard BC, Morgan MW, Vazquez-Benitez G, Erickson LO, Zwank MD. An analysis of changes in emergency department visits after a state declaration during the time of COVID-19. Ann Emerg Med. 2020;76:595–601. doi: 10.1016/j.annemergmed.2020.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bjørnsen LP, Næss-Pleym LE, Dale J, Laugsand LE. Patient visits to an emergency department in anticipation of the COVID-19 pandemic. Tidsskr Nor Laegeforen. 2020;140:1–5. doi: 10.4045/tidsskr.20.0277. [DOI] [PubMed] [Google Scholar]
- 18.Chua WLT, Quah LJJ, Shen Y, Zakaria ND, Wan PW, Tan K, et al. Emergency department ‘outbreak rostering’ to meet challenges of COVID-19. Emerg Med J. 2020;37:407–410. doi: 10.1136/emermed-2020-209614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim S, Ko Y, Kim YJ, Jung E. The impact of social distancing and public behavior changes on COVID-19 transmission dynamics in the Republic of Korea. PLoS One. 2020;15:e0238684. doi: 10.1371/journal.pone.0238684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ministry of Health and Welfare, National Emergency Medical Center. Monitoring system for emergency medical care [Internet] [accessed on 2019 April 1]. Available at: https://dw.nemc.or.kr/nemcMonitoring/menuview/ReportViewMain.do?isRealtimeOnly=Y&rFNo=20 .
- 21.Fitzgerald DA, Nunn K, Isaacs D. Consequences of physical distancing emanating from the COVID-19 pandemic: an Australian perspective. Paediatr Respir Rev. 2020;35:25–30. doi: 10.1016/j.prrv.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Litvinova M, Liu QH, Kulikov ES, Ajelli M. Reactive school closure weakens the network of social interactions and reduces the spread of influenza. Proc Natl Acad Sci U S A. 2019;116:13174–13181. doi: 10.1073/pnas.1821298116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang J, Zong L, Zhang J, Sun H, Harold Walline J, Sun P, et al. Identifying the effects of an upgraded ‘fever clinic’ on COVID-19 control and the workload of emergency department: retrospective study in a tertiary hospital in China. BMJ Open. 2020;10:e039177. doi: 10.1136/bmjopen-2020-039177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sung CW, Lu TC, Fang CC, Huang CH, Chen WJ, Chen SC, et al. Impact of COVID-19 pandemic on emergency department services acuity and possible collateral damage. Resuscitation. 2020;153:185–186. doi: 10.1016/j.resuscitation.2020.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Whitwell K, Maynard R, Barry N, Cowling V, Sood T. Strategic planning and response to COVID-19 in a London emergency department. Emerg Med J. 2020;37:567–570. doi: 10.1136/emermed-2020-209797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Choi A, Kim HY, Cho A, Noh J, Park I, Chung HS. Efficacy of a fourtier infection response system in the emergency department during the coronavirus disease-2019 outbreak. PLoS One. 2021;16:e0256116. doi: 10.1371/journal.pone.0256116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lin CH, Tseng WP, Wu JL, Tay J, Cheng MT, Ong HN, et al. A double triage and telemedicine protocol to optimize infection control in an emergency department in Taiwan during the COVID-19 pandemic: retrospective feasibility study. J Med Internet Res. 2020;22:e20586. doi: 10.2196/20586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lai CC, Wang CY, Wang YH, Hsueh SC, Ko WC, Hsueh PR. Global epidemiology of coronavirus disease 2019 (COVID-19): disease incidence, daily cumulative index, mortality, and their association with country healthcare resources and economic status. Int J Antimicrob Agents. 2020;55:105946. doi: 10.1016/j.ijantimicag.2020.105946. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data are available on request from the lead author.