ABSTRACT
Background
A globus sensation is one of the most common complaints in otolaryngological practice. Patients with no associated abnormalities detected during the usual examinations performed in ENT clinics, are being diagnosed with globus sensation. Cervical ultrasonography is usually not performed in ENT clinics; however, it is useful in screening diseases of the subcutaneous tissue/organs, whose detection is not possible with the routine ENT examinations. The purpose of our study was to elucidate whether cervical ultrasound examination identifies abnormalities in patients with globus sensation.
Methods
A single-centre retrospective cohort study. Cervical ultrasonographic examinations were performed on patients with globus sensation at the Department of Otolaryngology, Head and Neck Surgery of Tottori university hospital, a tertiary care centre, from January 2013 to September 2017. The subjects were 74 patients who complained of globus sensation with no abnormality in general otolaryngological examination including laryngoscopy.
Results
Ultrasonography detected structural abnormalities in 60.8% of the patients with globus sensation: thyroid disorders in 41 patients, including: 35 patients with thyroid nodules, 4 patients with Hashimoto’s disease, 1 patient with Grave’s disease, and 1 patient with subacute thyroiditis; Sjögren syndrome in 2 patients; and cervical lipoma in 1 patient. Furthermore, 2 patients with thyroid disorders had concomitant esophageal cancer.
Conclusion
Cervical ultrasonography identified thyroid disorders in patients with globus sensation, despite the normal ENT status. Therefore, it would be appropriate to adopt cervical ultrasonography as a routine examination at ENT clinics for patients with globus sensation.
Keywords: cervical ultrasonography, globus sensation, laryngoscope, thyroid disorders, thyroid nodule
Globus sensation is a common complaint, accounting for 3% to 4% of new otolaryngology outpatient referrals.1 The patients complain of a ‘feeling of a lump, foreign body, or tightness in their throat’; however, routine ENT examinations reveal no abnormal findings.2
It was Purcell who first described the symptom, coining the term ‘globus hystericus’ in 1707.3 Initially, globus sensation was thought to be caused by psychological or emotional factors, and therefore, patients with globus sensation were referred to psychiatrists. However, the introduction of medical technology innovations, such as rigid endoscopy and X-rays, made feasible the examination of organic disorders causing globus sensation.2
In 1968, ‘globus hystericus’ was replaced with the term ‘globus pharyngeus’.2 Malcomson et al. claimed that gastropharyngeal reflux disease was one of the causative disorders of globus sensation.2 The definition of globus sensation can vary, depending on medical technology used in routine care. Several studies investigated the correlation between gastropharyngeal reflux disease and globus sensation, using video fluorography and pH monitoring devices.4 More currently, clinicians can use a flexible fiberscope for general examination. For more thorough examination, upper gastrointestinal endoscopy, video-fluorography, and computed tomography are available.
At present, while the mucosal lumen of the oral cavity, pharynx, and larynx can be investigated in detail during routine ENT examination, the subcutaneous tissues, and organs can be investigated only by manipulation. Therefore, screening for diseases of the thyroid, salivary glands, blood vessels, mesenchymal tissue (tumours and cysts), and other subcutaneous organs and tissues, is insufficient.
Ultrasonography has undergone dramatic development recently, and is now widely used. It is non-invasive, and capable of providing real-time fine imaging of internal body structures. Cervical ultrasonography can screen the thyroid, salivary gland, and lymph node diseases, and tumours in the head and neck region. In tertiary care centres, cervical ultrasonography is performed as a routine examination for detection of thyroid diseases and metastatic lymph nodes in head and neck malignancies. However, in most ENT outpatient clinics, cervical ultrasonography is not regularly used.
Therefore, our objective was to examine whether cervical ultrasonography reveals abnormal findings in patients with globus sensation,whom we often encounter in ENT clinics, and to elucidate the usefulness of cervical ultrasonography in ENT clinics.
SUBJECTS AND METHODS
Study design and inclusion criteria
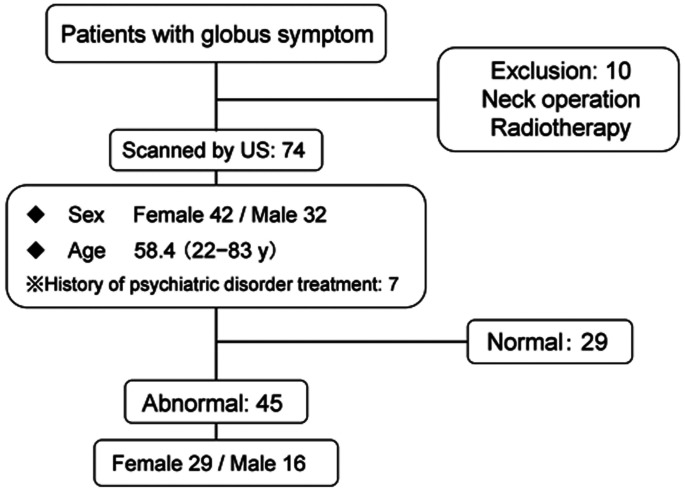
We routinely perform cervical ultrasonography for patients with globus sensation who have no abnormalities revealed through routine ENT examination in our department. Between January 2013 and September 2017, there were 84 consecutive patients who underwent ultrasonography for globus sensation. In this study, we retrospectively reviewed the 84 patients. The routine ENT examinations were defined as visualization, manipulation, inquiry, indirect laryngoscopy, flexible laryngoscopy, and X-ray. Patients with globus sensation who had received irradiation therapy for cervical carcinoma or underwent neck surgery were excluded (Fig. 1).
Fig. 1.
Flow chart showing patients’ demographics and their ultrasonographic results. US, ultrasonography; y, years.
The patients had various chief complaints of the pharyngolaryngeal discomfort, classified into five groups: pain, cough, sensation of dyspnoea, a lump in the throat, and other complaints. The patient’s chief complaints were compared between those with and without abnormalities on cervical ultrasonography using Fisher’s exact test.
Ultrasonographic examination
Cervical ultrasonography was performed on 74 patients with globus symptoms using the ACUSON S2000 ultrasound system (Siemens Healthineers, Mountain View, CA) with linear transducer. The patients underwent a detailed ultrasound scan of the neck, including the thyroid, lymph node, parotid glands, and submandibular glands. In cases in which a tumour was detected, fine needle aspiration cytology for tumour diagnosis was performed, as necessary.
Ethical considerations
All followed procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions. The ethical committee and the institutional review board of Tottori University approved the study protocol (approval No. 1603A147). The requirement for written informed consent was waived due to the retrospective nature of the study. Nevertheless, we provided the patients an opportunity to opt out.
RESULTS
The 74 subjects consisted of 32 men and 42 women. Seven of them had psychiatric disorders. The mean age of the subjects was 58.4 years (range: 22–83 years).
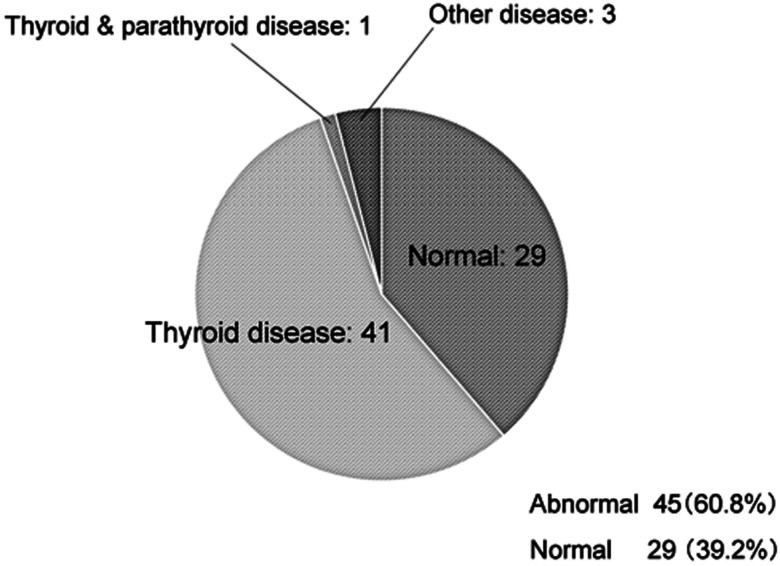
Abnormal ultrasonographic findings were detected in 45 patients (60.8%). Thyroid disorders were revealed in 42 patients (56.8%), salivary gland disorders in 2 patients (3%), and lipoma in 1 patient (1%) (Fig. 2).
Fig. 2.
A pie chart showing the ultrasonographic findings in patients with globus sensation.
The patients with thyroid disorders consisted of 6 patients with diffuse lesions and 35 patients with nodular lesions. The diffuse lesions were a result of Hashimoto’s disease in four cases, and of Grave’s disease and subacute thyroiditis in one case each. The nodular lesions were diagnosed as adenomatous goitre in 20 cases, cyst in 9 cases, thyroid carcinoma in 2 cases, and 4 cases included small nodules with negative cytology results. One patient with adenomatous goitre also had parathyroid adenoma (Table 1).
Table 1. The detailed statement of the diagnoses based on cervical ultrasonography.
| Findings | n | Diagnoses [n] | |
| Thyroid disease | Diffuse lesions | 6 | Hashimoto disease [4] Grave’s disease [1] Subacute thyroiditis [1] |
| Nodular lesions | 35 | Thyroid cancer [2] Adenomatous goitre [20]* Thyroid cyst [9] Not diagnosed [4] |
|
| Others | 1 | Low echo area in thyroid [1] | |
| Other disease | Salivary gland | 2 | Sjögren’s syndrome [1] Low echo area in the parotid gland [1] |
| Subcutaneous mass | 1 | Lipoma | |
| Mass in cervical esophagus | 2 | Esophageal cancer** | |
*One of the cases was AG with Parathyroid adenoma. **These two cases overlap with those of Hashimoto's disease.
Of the two patients with Hashimoto’s disease, one patient displayed saliva pooling in the hypopharynx, and the other swelling of the cervical esophageal mucosa found by ultrasonography. Both underwent follow-up examination and were diagnosed with thoracic esophageal cancer and cervical esophageal, respectively, using upper esophagogastroduodenoscopy.
Further, there was no correlation between the chief complaints and the abnormal ultrasonographic findings (P = 0.937) (Table 2).
Table 2. Comparison of the chief complaints between the patients with globus symptom with normal and abnormal ultrasound findings.
| Abnormal (n = 45) | Normal (n = 29) | Fisher’s exact test | |
| Sensation of dyspnoea | 2 | 1 | P = 0.937 |
| Pain | 18 | 12 | |
| Cough | 2 | 1 | |
| Lump in the throat | 15 | 12 | |
| Others | 8 | 3 |
DISCUSSION
Ultrasonography revealed abnormal findings in 60.8% of the patients, including patients with thyroid disorders. Thyroid nodules were detected in 47.3% of the patients with globus sensation, which indicates the superiority of ultrasonography examination. Only a few patients were diagnosed with salivary gland disease (Sjögren syndrome in all cases). We detected one hardly palpable lipoma, and two cases of esophageal cancer that were confirmed using additional upper gastrointestinal endoscopy (one was distal esophageal cancer, and the other was cervical esophageal cancer). Psychiatric disorders have been thought to be a major cause of globus sensation; however, patients with psychiatric disorders accounted for only a small proportion of the subjects in this study (0.09%). However, the mechanism through which thyroid diseases cause globus sensation is yet unclear.
Previous research indicates that thyroid disease could cause globus sensation depending on thyroid size and the thyroid nodule location in the thyroid.5 Others have reported that an enlarged thyroid gland caused by Grave’s disease or Hashimoto’s disease could cause dysphagia or dyspnoea.6 In our study, thyroid nodules were detected in 47.3% of the patients, showing a higher incidence rate of nodules than in the screening examination performed in 2010 in Japan (6.9–31.6%).7 Marshall et al. examined patients with globus sensation using thyroid ultrasonography and reported a higher incidence of thyroid abnormalities in patients with globus sensation (72.1%) than in controls (33.3%).8 Their study involved only thyroid ultrasonography, whereas we evaluated the entire neck. Only a few patients were diagnosed with salivary gland diseases (Sjögren syndrome in both cases) this is assumed to be because patients with salivary gland diseases are difficult to classify as cases of globus sensation, because they present with their own set of clinical appearances. However, one report indicated that slight abnormal ultrasonographic findings of the salivary gland indicate the initial stage of autoimmune sialadenitis, and the possibility of autoimmune sialadenitis in patients not diagnosed with salivary gland disease is also not excluded.9
Finally, earlier reports confirm that cervical esophageal cancers and postcricoid cancers can be detected using cervical ultrasonography.10
The main ultrasonographic examination findings in patients with globus sensation were thyroid disorders. Most of the thyroid abnormalities detected by ultrasonography were benign. However, a few patients had serious diseases, specifically esophageal cancer and Sjögren syndrome, whose early detection is advantageous. Pharyngeal discomfort may be a symptom of more serious diseases, including esophageal cancer and autoimmune sialadenitis, which are easily missed by conventional ENT routine examination. Late detection can have grave consequences. Cervical ultrasonography was shown as a useful examination method for the detection of these diseases.
Our study had some limitations. The variations in chief complaints and classifying conditions as globus sensation were dependant on each doctor’s decision. Additionally, patients who visited our hospital were introduced from surrounding ENT clinics and general hospital. Therefore, these institutions appear to experience more patients with globus sensation than our hospital, so cervical ultrasonography may be more useful in patients with globus sensation at private ENT clinics or ENT departments of general hospitals.
Our study demonstrated ultrasonography as a more useful method than CT and MRI for the detection of abnormalities in several organs in the head and neck, such as the submandibular glands, parotid glands, lymph nodes, etc. Cervical ultrasonography of the entire neck is not more time-consuming than thyroid ultrasonography, and the procedure is virtually identical. We, therefore, recommend examining the entire neck of patients with globus sensation, rather than only the thyroid region.
Cervical ultrasonography appears useful for the detection of hypopharyngeal and esophageal lesions as causes of globus sensation not otherwise detected using flexible laryngoscopy.
The patients had various chief complaints. We evaluated the correlation between the chief complaints and the abnormal ultrasonographic findings and observed no associations. Therefore, selecting the patients with globus sensation for ultrasonography based on their chief complaints seems inconvenient.
In conclusion, cervical ultrasonography may detect abnormalities such as thyroid and salivary gland abnormalities, cervical mass, or esophageal cancer in patients diagnosed with globus sensation, which are not detected by performing routine ENT examinations. Therefore, we recommend adopting cervical ultrasonography as a routine examination in patients with globus sensation at ENT clinics.
Footnotes
The authors declare no conflict of interest.
REFERENCES
- 1.Moloy PJ,Charter R. The globus symptom. Incidence, therapeutic response, and age and sex relationships. Arch Otolaryngol Head Neck Surg. 1982;108:740-4. 10.1001/archotol.1982.00790590062017 [DOI] [PubMed] [Google Scholar]
- 2.Malcomson KG. Globus hystericus vel pharyngis (a recommaissance of proximal vagal modalities). J Laryngol Otol. 1968;82:219-30. 10.1017/S0022215100068687 [DOI] [PubMed] [Google Scholar]
- 3.Purcell J. A Treatise of Vapours: Or hysterick Fits. The Second Edition, Revis’d and Augmented. London: printed for Edward Place; 1707. [Google Scholar]
- 4.Rasmussen ER,Schnack DT,Ravn AT. A prospective cohort study of 122 adult patients presenting to an otolaryngologist’s office with globus pharyngeus. Clin Otolaryngol. 2018;43:854-60. 10.1111/coa.13065 [DOI] [PubMed] [Google Scholar]
- 5.Nam IC,Choi H,Kim ES,Mo EY,Park YH,Sun DI. Characteristics of thyroid nodules causing globus symptoms. Eur Arch Otorhinolaryngol. 2015;272:1181-8. 10.1007/s00405-015-3525-9 [DOI] [PubMed] [Google Scholar]
- 6.Guldiken B,Guldiken S S,Turgut N,Yuce M,Arıkan E,Tugrul A. Dysphagia as a primary manifestation of hyperthyroidism: a case report. Acta Clin Belg. 2006;61:35-7. 10.1179/acb.2006.007 [DOI] [PubMed] [Google Scholar]
- 7.Shimura H. The frequency and course of thyroid tumor supported by patients data of Ningen Dock in Japan. Nihon Kojosen Gakkai Zasshi. 2010;1:109-13. Japanese. [Google Scholar]
- 8.Marshall JN,McGANN G,Cook JA,Taub N. A prospective controlled study of high-resolution thyroid ultrasound in patients with globus pharyngeus. Clin Otolaryngol. 1996;21:228-31. 10.1111/j.1365-2273.1996.tb01731.x [DOI] [PubMed] [Google Scholar]
- 9.Onda K,Fukuhara T,Matsuda E,Donishi R,Hirooka Y,Takeuchi H,et al. . Impact of screening for salivary gland by ultrasonography. Yonago Acta Med. 2020;63:42-6. 10.33160/yam.2020.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fukuhara T,Matsuda E,Hattori Y,Donishi R,Ehara H,Fujiwara K,et al. . Usefulness of ultrasound for assessing the primary tumor of hypopharyngeal carcinoma. Laryngoscope Investig Otolaryngol. 2017;2:390-4. 10.1002/lio2.126 [DOI] [PMC free article] [PubMed] [Google Scholar]