Abstract
Background:
The lack of consensus on how to measure ACEs limits our estimation of their impact on health outcomes and understanding of which ACE clusters drive unmet care coordination (CC) needs.
Objectives:
1) Identify latent classes of ACEs among a representative group of U.S. children; 2) Examine the association between these classes and unmet needs for CC.
Participant and Setting:
Using the 2016-2017 National Survey of Children’s Health, we sampled children ages 0-17 the who had seen >1 healthcare provider within 12 months (n=38,758).
Methods:
We conducted latent class analyses and weighted logistic regression analyses to examine associations between latent classes and unmet need for CC.
Results:
We identified seven distinct classes: household poverty and parental divorce, household poverty and parental death, household poverty only, household substance abuse and witnessing violence, multiple ACEs, household poverty and child discrimination, and household poverty and household mental illness. Children in the following classes had the greatest odds of unmet need for CC: household poverty only (AOR 2.0; 95% CI, 1.42- 2.84), household poverty and household mental illness (AOR 1.67; 95% CI, 1.15- 2.44), multiple ACEs (AOR 2.31; 95% CI, 1.53- 3.50), and household poverty and child discrimination (AOR 3.55; 95% CI, 1.71-7.37) .
Conclusions:
Children who experienced specific combinations of ACEs, have an increased risk of unmet need for CC, with those experiencing both poverty and discrimination having the highest odds of unmet need for CC. Discrimination widens the gap of unmet CC need for poor children.
Keywords: adverse childhood experiences, child health services, latent class analysis
INTRODUCTION
Although adverse childhood experiences (ACEs) have been linked to poor health outcomes in children and adults, there is currently no consensus on quantifying the impact of multiple ACEs.(Anda et al., 2021; Debowska et al., 2017; Hughes et al., 2017; McLennan et al., 2020) ACEs often coexist, and the inter-related nature of different ACEs has significant implications for how they are evaluated.(Dong et al., 2004) Studies examining associations between ACEs and a particular health outcome or health service need have traditionally taken an approach of tabulating dichotomous indicators to calculate a cumulative ACE score. Accumulative score approach provides information about the “dose” of the overall ACE exposure, which is useful for examining dose-dependent relationships. However, there is increasing interest in alternative methods of evaluating ACEs, namely studying ACE clusters which may be greater drivers for a particular health outcome or health service need among children and adults.(Barboza, 2018; Lanier et al., 2018; Lee et al., 2020; Lew & Xian, 2019; McKelvey et al., 2020; O’donnell et al., 2017) One concern is that the cumulative score approach assumes that each ACE is equally weighted and equally impacts the outcome of interest. Further, the cumulative ACE score approach does not sufficiently capture the nuances needed to understand ACEs’ inter-related nature and the complex relationship between ACE clusters and particular child health outcomes or health service needs.(Dong et al., 2004; Finkelhor, 2018; McLaughlin & Sheridan, 2016; Negriff, 2020)
Because ACE exposure is associated with numerous physical and behavioral health outcomes, individuals with more ACE exposures may have unique health services needs and may access multiple systems of care.(M. Bellis et al., 2017; M. A.; Bellis et al., 2019; Koball et al., 2019; Peterson et al., 2018) Caregivers of children who have experienced ACEs may have more challenges in effectively supporting their child through the healthcare system.(Berg et al., 2018; Fairbrother et al., 2005) Care coordination (CC) is a process that can help caregivers in navigating the healthcare system to meet their child’s needs.(Antonelli et al., 2008; Turchi et al., 2009) There is data to suggest that children who have endured ACEs have challenges receiving the needed CC.(Bethell et al., 2014) However, there are critical gaps in identifying the ACE clusters with greater unmet CC needs. Addressing this gap will inform the development of CC interventions across the multiple care systems that children who endure ACEs may access. The aims of this study were as follows: 1) using latent class analysis (LCA), identify classes of ACEs among children who have seen a healthcare provider in the last 12 months, and 2) examine the association between these ACE latent classes and unmet need for CC.
METHODS
Data Source and Study Population
We obtained data from the 2016-2017 National Survey of Children’s Health (NSCH), which is a nationally representative cross-sectional phone, mail, and web-based survey that collects data on the physical and emotional health of children ages 0-17 years old as well as educational activities and use of health services. U.S. households were randomly selected to complete a screening survey identifying the number of children in the home and children with special health need (CSHCN) status. One child was randomly selected from the household, and a caregiver was asked to complete the focal survey for that child.(US Census Bureau, 2018) Our study population was restricted to children 0-17 years old who had seen more than one healthcare provider in the last 12 months and whose caregivers responded to questions about ACE exposures. The Children’s National Hospital Institutional Review Board deemed this study as exempt.
Measures
Adverse Childhood Experiences:
For the NSCH, an expert panel developed nine questions about ACE exposures based on a literature review.(Bethell et al., 2017; Felitti et al., 1998) Parents and caregivers were asked how often the family had difficulty paying for basic necessities with the family’s income (household poverty). The respondents also indicated whether the child had ever experienced the following: parental divorce, parental death, parental incarceration, witnessing domestic violence, being a victim/witness of neighborhood violence, living with a household member with mental illness, living with a household member with substance abuse problems, and being treated unfairly due to race/ethnic group (child discrimination). The first ACE exposure (household poverty) was measured using a 4-point Likert scale (very often, somewhat often, rarely, never). We dichotomized very often and somewhat often to “yes” responses, whereas rarely and never responses were dichotomized to ”no” responses. The remaining eight ACE exposure questions were reported as dichotomous yes/no responses. We used the nine NSCH ACEs variables to identify latent classes of ACE exposures. The ACE latent classes served as the primary independent variable in the logistic regression analyses.
Unmet Need for Care Coordination:
The outcome of interest for the logistic regression analyses was unmet need for CC. The CC questions in the NSCH module were as follows: “Does anyone help you arrange or coordinate this child’s care among the different doctors or services that this child uses?”; “During the past 12 months, have you felt that you could have used extra help arranging or coordinating this child’s care among the different health care providers or services?”; “During the past 12 months, how often did you get as much help as you wanted with arranging or coordinating this child’s health care?”
Based on a system from prior studies, we defined unmet need for CC as caregivers who reported: 1) needing extra help for coordinating care and only sometimes or never receiving as much help as needed, or 2) someone helped with coordinating care, needing extra help, and only sometimes or never receiving as much help as needed. (Brown et al., 2014; Miller et al., 2019)
Study Covariates:
We included child and household characteristics that may influence our independent and outcome variables.(Brown et al., 2017; Council on Children with Disabilities and Medical Home Implementation Project Advisory Committee, 2014; Toomey et al., 2013) Child socio-demographic characteristics included age, sex, race/ethnicity, insurance status (private, public, public and private, or uninsured), CSHCN status. CSHCN denotes having a chronic condition defined using a 5-item CSHCN screener which is part of the NSCH survey.(Bethell et al., 2002) Family socio-demographic characteristics included household income (0-99%, 100-199%, 200-399, or >400% of the Federal Poverty Level [FPL]), family structure (two-parent household, mother-only household, or other family structure), primary language spoken at home (English or another language) and parental education level (less than high school, high school, some college or higher).
Analysis
Latent Class Analysis and Class Enumeration:
Latent class analysis (LCA) is a model-based, person-centered analytic approach of identifying unobserved groups where clustering is based on formal statistical procedures in which the optimal number of classes is determined based on formal statistical procedures.(Collins & Lanza, 2009; B. O. Muthén, 2002; Wang & Wang, 2019) We used LCA to identify distinct classes of children with respect to their ACE exposures. We estimated a series of LCA models with an increasing number of latent classes and iteratively comparing each successive class (k) model with the previous class (k-1) model. Akaike’s information criterion (AIC), Bayesian information criterion (BIC), sample-size adjusted BIC (aBIC), Lo-Mendell-Rubin likelihood ratio test (LMR) and adjusted Lo-Mendell-Rubin likelihood ratio test (aLMR) goodness of fit measures for each model were used for model comparisons. Bootstrap likelihood ratio test (BLRT), was not available for the NSCH’s complex study design. We selected the most optimal model based on: lower AIC, smaller sample size BIC and aBIC, as well as significant values for LMR and aLMR for the k-class model relative to the k-1 class model.(Akaike, 1987; Lo et al., 2001; Nylund et al., 2007; Sclove, 1987) Entropy values closer to one indicated how well the model formed very distinct classes.(Celeux & Soromenho, 1996) After selecting the model of best fit, we used posterior probabilities of class membership to assign each child to their most likely ACE latent class. We named the latent classes based on the common ACE exposure in each group. We used Mplus version 8.4 to estimate the LCA models (L. K. Muthén & Muthén, 1998) and accounted for the complex survey design.
Multivariate Regression to Assess Associations:
The estimated latent class membership was saved as a categorical variable and merged with the original sample data. Then, we conducted logistic regression analyses to examine the association between the latent classes and unmet need for CC. We retained children with no ACE exposures in the study and classified them as the reference group (Class 0). We used a chi-squared test to measure bivariate relationships and logistic regression to examine the association between ACE latent classes and odds of unmet need for CC. The child and household covariates were controlled in the logistic regression model and we applied survey weights derived from the National Center for Health Statistics in all model estimations.
RESULTS
Sample Characteristics
Descriptive statistics of the weighted sample are summarized in Table 1. The average age of the study population (N=38,758) was 8.8 years old. There were slightly more males (52.1%) than females (47.9%). Most children were White Non-Hispanic (53.6%), English speaking (87.6%), privately insured (59.9%), had non-CSHCN status (73.4%), lived in two-parent households (75,1%), and had parents who had received some college education or higher (75.3%). Approximately 48% of children had ≥ 1 or more ACEs.
Table 1:
Descriptive statistics of study population (n= 38,758)
| Frequency | Percentage | Mean (SE) | |
|---|---|---|---|
| Age (years) | 8.84 (8.71-8.96) | ||
| Child Sex | |||
| Female | 18,577 | 47.9% | |
| Male | 20,181 | 52.1% | |
| Child Race/Ethnicity | |||
| White Non-Hispanic | 20,790 | 53.6% | |
| Hispanic | 9,058 | 23.4% | |
| Black Non-Hispanic | 4,887 | 12.6% | |
| Other Non-Hispanic | 4,023 | 10.4% | |
| Insurance | |||
| Private | 23,170 | 59.8% | |
| Public | 11,755 | 30.3% | |
| Public and Private | 2,198 | 5.7% | |
| Uninsured | 1,639 | 4.2% | |
| Household Income | |||
| 0-99% FPL | 7,418 | 19.1% | |
| 100-199% FPL | 7,926 | 20.5% | |
| 200-399% FPL | 10,395 | 26.8% | |
| 400% FPL or more | 13,015 | 33.6% | |
| Family structure | |||
| Two parent family | 29,107 | 75.1% | |
| Single parent (mother only) | 6,244 | 16.1% | |
| Other family type | 3,407 | 8.8% | |
| Parental Education | |||
| Less than high school education | 2,736 | 7.1% | |
| High school or GED Degree | 6,821 | 17.6% | |
| Some college or higher | 29,196 | 75.3% | |
| Household Language | |||
| English | 33,944 | 87.6% | |
| Other Language | 4,814 | 12.4% | |
| CSHCN Status | |||
| Yes | 10,310 | 26.6% | |
| No | 28,448 | 73.4% | |
| Adverse Childhood Experiences | |||
| 0 ACEs | 20,305 | 52.4% | |
| 1 ACEs | 9,658 | 24.9% | |
| 2 ACEs | 4,197 | 10.8% | |
| 3 ACEs | 1,992 | 5.1% | |
| ≥ 4 ACEs | 2,608 | 6.7% |
Latent Class Analysis of the ACEs
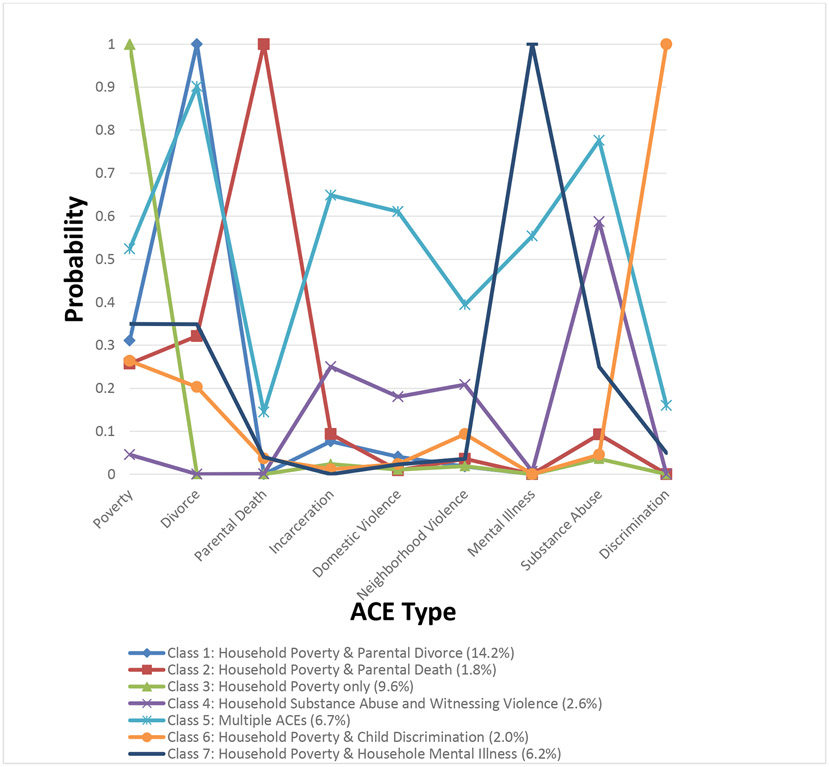
LCA model comparisons are shown in Table 2. All the goodness of fit measures favored seven or more classes. In comparison between seven and eight class models, information criterion indices (AIC, BIC and aBIC) favored eight classes, but LMR and aLMR tests favored seven classes. We selected the seven-class model for further analysis because of an entropy value (entropy = 0.917) closest to one. The seven-class model showed a distinct pattern of ACE clusters (Figure 1): Class 1 – household poverty and parental divorce (14.2%), Class 2 – household poverty and parental death (1.8%), Class 3 – household poverty only (9.6%), Class 4 – household substance abuse and witnessing violence (2.6%), Class 5 – multiple ACEs (6.7%), Class 6 – household poverty and child discrimination (2.0%), and Class 7 – household poverty and household mental illness (6.2%). Children who had not experienced any ACEs were neither included in the LCA nor excluded from the study. Instead, they were assigned to Class 0 – no ACEs (56.9%) reference group.
Table 2:
Latent Class Model Fit Comparisons
| Model | AIC | BIC | aBIC | LMR p-value |
aLMR p-value |
Entropy |
|---|---|---|---|---|---|---|
| 1-Class | 136378.47 | 136447.99 | 136419.39 | - | - | - |
| 2-Class | 127008.51 | 127155.27 | 127094.89 | <.0001 | <0.0001 | .821 |
| 3-Class | 124456.79 | 124680.80 | 124588.64 | <.0001 | <0.0001 | .725 |
| 4-Class | 122503.52 | 122804.78 | 122680.84 | <.0001 | <0.0001 | .776 |
| 5-Class | 121768.61 | 122147.11 | 121991.39 | .0001 | .0002 | .857 |
| 6-Class | 121138.30 | 121594.05 | 121406.55 | .0032 | .0036 | .905 |
| 7-Class | 120635.36 | 121168.35 | 120949.07 | .0019 | .0021 | .917 |
| 8-Class | 120272.16 | 120882.40 | 120631.34 | .2099 | .2141 | .840 |
Note: AIC-Akaike Information Criterion; BIC-Bayesian Information Criterion; aBIC-Adjusted BIC; LMR LR- Lo- Mendell-Rubin likelihood ratio test; ALMR LR- Adjusted LMR LR test; Entropy- Entropy statistic. -: Not applicable.
Figure 1:
Probability of each ACE type across the seven latent classes
Weighted demographic descriptive statistics for each latent class are presented in Table 3. All characteristics were associated with the latent class membership (p<0.05) except for age, gender, and household income. Children in all latent classes were older than the sample average age of 8.8 except Class 0 (no ACEs; 7.95) and Class 3 (household poverty only; 7.97). White Non-Hispanic children accounted for over 50% of the population within Class 0 (no ACEs, 59.1%), and Class 7 (household poverty and household mental illness; 62.2%), while Black Non-Hispanic children were over-represented in Class 6 (household poverty and child discrimination; 38.5%). Children with public insurance were over-represented in Class 2 (household poverty and parental death; 50.9%), Class 3 (household poverty only; 43.2%), and Class 5 (multiple ACEs; 59.0%). Most children lived in two-parent households except those in Class 2 (household poverty and parental death; 46.4% ) and Class 5 (multiple ACEs; 36.5%). Most parents across all classes received some college-level education or higher, with Class 6 (household poverty and child discrimination; 82.4%) having the highest percentage. Children with CSHCN status were over-represented in Class 5 (multiple ACEs; 50.3%). In Table 4, the highest prevalence for unmet need for CC was among children in Class 6 (household poverty and child discrimination).
Table 3:
Descriptive statistics of the latent class groups (n= 38,758)
| Class 0 N= 22,035 |
Class 1 N= 5,511 |
Class 2 N= 704 |
Class 3 N= 3,711 |
Class 4 N= 1,009 |
Class 5 N= 2,613 |
Class 6 N= 768 |
Class 7 N= 2,407 |
p-value | |
|---|---|---|---|---|---|---|---|---|---|
| % of total sample | 56.9% | 14.2% | 1.8% | 9.6% | 2.6% | 6.7% | 2.0% | 6.2% | |
| Average child age | 7.95 | 10.18 | 11.24 | 7.97 | 9.19 | 11.15 | 11.28 | 10.00 | >0.05 |
| Child Sex | |||||||||
| Female | 48.2% | 48.0% | 47.6% | 46.1% | 51.5% | 46.4% | 50.0% | 49.1% | 0.8855 |
| Male | 51.8% | 52.0% | 52.4% | 53.9% | 48.5% | 53.6% | 50.0% | 50.9% | 0.8855 |
| Child Race/Ethnicity | |||||||||
| White Non-Hispanic | 59.1% | 49.1% | 37.8% | 46.7% | 45.6% | 50.0% | 13.8% | 62.2% | ≤0.001 |
| Hispanic | 21.6% | 27.4% | 25.7% | 28.2% | 29.6% | 20.6% | 26.4% | 16.2% | ≤0.001 |
| Black Non-Hispanic | 8.1% | 16.3% | 31.2% | 16.2% | 16.2% | 18.3% | 38.5% | 8.9% | ≤0.001 |
| Other Non-Hispanic | 11.1% | 7.3% | 5.31% | 9.0% | 8.6% | 11.1% | 21.4% | 12.7% | ≤0.001 |
| Insurance | |||||||||
| Private | 74.8% | 46.1% | 38.5% | 39.1% | 51.1% | 26.5% | 56.3% | 59.2% | ≤0.001 |
| Public | 18.5% | 41.3% | 50.9% | 43.2% | 40.6% | 59.0% | 33.3% | 31.4% | ≤0.001 |
| Public and Private | 3.3% | 7.7% | 7.2% | 10.7% | 4.5% | 9.0% | 6.24% | 6.6% | ≤0.001 |
| Uninsured | 3.4% | 5.0% | 3.4% | 7.0% | 3.8% | 5.5% | 4.1% | 2.8% | >0.05 |
| Household Income | |||||||||
| 0-99% FPL | 11.7% | 28.8% | 32.9% | 28.7% | 18.1% | 32.6% | 20.4% | 17.0% | ≤0.001 |
| 100-199% FPL | 15.3% | 24.7% | 25.8% | 31.5% | 23.7% | 26.6% | 19.0% | 22.7% | ≤0.001 |
| 200-399% FPL | 26.9% | 25.3% | 21.3% | 28.1% | 24.2% | 25.6% | 30.9% | 31.4% | <0.05 |
| 400% FPL or more | 46.1% | 21.2% | 20.0% | 11.7% | 34.1% | 15.2% | 29.7% | 29.0% | ≤0.001 |
| Family structure | |||||||||
| Two parent family | 92.3% | 42.3% | 22.2% | 81.7% | 73.6% | 31.4% | 72.8% | 73.5% | ≤0.001 |
| Single parent (mother only) | 42.8% | 41.6% | 46.4% | 13.6% | 14.4% | 36.5% | 22.4% | 19.2% | ≤0.001 |
| Other family type | 3.4% | 16.1% | 31.4% | 4.6% | 12.1% | 32.1% | 4.9% | 7.3% | ≤0.001 |
| Parental Education | |||||||||
| Less than high school education | 5.7% | 8.25% | 9.4% | 10.7% | 11.2% | 8.24% | 8.3% | 3.7% | ≤0.001 |
| High school or GED Degree | 12.4% | 25.1% | 32.7% | 23.5% | 18.5% | 28.8% | 9.3% | 14.5% | ≤0.001 |
| Some college or higher | 81.9% | 66.7% | 57.9% | 65.8% | 70.3% | 63.0% | 82.4% | 81.8% | ≤0.001 |
| Household Language | |||||||||
| English | 86.4% | 90.4% | 91.9% | 80.9% | 88.1% | 96.1% | 81.9% | 94.5% | ≤0.001 |
| Other Language | 13.6% | 9.6% | 8.1% | 19.1% | 11.9% | 3.9% | 18.1% | 5.5% | ≤0.001 |
| CSHCN Status | |||||||||
| Yes | 19.8% | 29.0% | 27.8% | 29.1% | 29.8% | 50.3% | 34.0% | 42.6% | ≤0.001 |
| No | 80.2% | 71.0% | 72.3% | 70.9% | 70.2% | 49.7% | 66.0% | 57.4% | ≤0.001 |
All socio-demographic variables were significantly different at the p <0.05 level between the class groups, except for age (only ages 8 and 10), gender and household income (only at the 200-399% FPL level)
Table 4:
Prevalence of Unmet Need for CC by ACEs Latent Class Membership
| Latent Class | Weighted % with Unmet Need for CC |
|---|---|
| Class 0: No ACEs | 24.2*** |
| Class 1: Household Poverty and Parental Divorce | 29.9*** |
| Class 2: Household Poverty and Parental Death | 34.5*** |
| Class 3: Household Poverty only | 40.9*** |
| Class 4: Household Substance Abuse and Witnessing Violence | 37.9*** |
| Class 5: Multiple ACEs | 50.0*** |
| Class 6: Household Poverty and Child Discrimination | 53.2*** |
| Class 7: Household Poverty and Household Mental Illness | 39.7*** |
p≤0.001
Effect of Latent Class Membership on Report of Unmet Need for CC
After controlling for all covariates, children in Class 3 (household poverty only), Class 5 (multiple ACEs), Class 6 (household poverty and child discrimination), and Class 7 (household poverty and household mental illness) had significantly greater odds of unmet needs for CC compared to children with no ACEs (Table 5). The largest effect size was seen among children in Class 6 (household poverty and child discrimination) who had over three times the odds (aOR 3.55; 95% CI 1.15-2.44) of unmet need for CC.
Table 5:
Associations of Unmet Need for CC and Latent Class Membership
| Latent Class | Unadjusted OR (95% CI) |
Adjusted OR (95% CI) |
|---|---|---|
| Class 0: No ACEs | Reference | Reference |
| Class 1: Household Poverty and Parental Divorce | 1.34 (0.97- 1.86) | 1.06 (0.73 - 1.53) |
| Class 2: Household Poverty and Parental Death | 1.65 (0.73- 3.74) | 1.04 (0.49- 2.22) |
| Class 3: Household Poverty only | 2.17 (1.53- 3.09)*** | 2.01 (1.42- 2.84)*** |
| Class 4: Household Substance Abuse and Witnessing Violence | 1.91 (1.10 - 3.33)* | 1.58 (0.84- 2.97) |
| Class 5: Multiple ACEs | 3.14 (2.28- 4.33)*** | 2.31 (1.53- 3.50)*** |
| Class 6: Household Poverty and Child Discrimination | 3.56 (1.93- 6.58)*** | 3.55 (1.71-7.37)*** |
| Class 7: Household Poverty and Household Mental Illness | 2.06 (1.39- 3.06)*** | 1.67 (1.15- 2.44)* |
Adjusted for age, sex, race insurance status, household income, family structure, parental education, language spoken at home and CSHCN; Ref: Reference
p≤0.05
p≤0.01
p≤0.001
DISCUSSION
The purpose of this study was to examine the association between ACE latent classes and unmet need for CC in U.S. children. This study’s findings validate prior findings, extend the work of previous studies, and provide novel hypotheses for future inquiry. Our findings provide evidence that U.S. children who have seen more than one healthcare professional in the last 12 months have distinct ACE clusters. We also found that children in the following latent classes had significantly higher odds of unmet need for CC compared to children with no ACEs: household poverty only (class 3), multiple ACEs (class 5), household poverty and child discrimination (class 6), as well as the household poverty and household mental illness classes (class 7).
Our latent class findings both corroborate previous studies and identify novel classes. Like prior studies, we found the following latent classes: multiple ACEs,(Barboza, 2018; Lacey et al., 2020; Lanier et al., 2018; Lew & Xian, 2019; Thompson et al., 2020) children with household poverty and household mental illness,(Lanier et al., 2018) children with household poverty only,(Lew & Xian, 2019) children experiencing the combination of household poverty and parental divorce,(Stempel et al., 2017) and children with exposures to household substance abuse and violence.(Lanier et al., 2018)
To our knowledge, the household poverty and child discrimination class has not been identified in prior LCA analyses of ACEs. Perceived racial discrimination has predominantly been studied in adults(Paradies et al., 2015), but growing literature has shown that children experience racial discrimination directly and vicariously through their caregiver’s experience.(Heard-Garris et al., 2018; Pachter & Coll, 2009) Among adults, racial discrimination is associated with deferred or underutilized needed healthcare services, increased mistrust of the healthcare system, and sub-optimal patient-provider communication.(Ben et al., 2017; Burgess et al., 2008) Caregivers who note perception of racial discrimination also reported unmet healthcare needs for the child and decreased patient-family satisfaction.(Auslander, W. F., Thompson, S. J., Dreitzer, D., & Santiago, 1997; Paine et al., 2018) Any or all of these factors may lead to a higher unmet need for CC for children who have experienced racial discrimination.
This finding highlights that racism is a public health threat and an underlying driver of healthcare inequities throughout the life-course.(Feagin & Bennefield, 2014; Malawa et al., 2021) Race/ethnicity and poverty are often conflated, but they have a complex and non-causal relationship. Race is distinct from racism. While the former is a social construct that separates individuals based on physical characteristics such a skin color or ancestry, the latter is a system of prejudice or oppression directed against a person or group of people based on racial classification.(Amutah et al., 2021; Bailey et al., 2020) The finding of highest odds of unmet need for CC among the household poverty and child discrimination latent class compared to children with no ACEs highlights that racism rather than race drives adverse health or healthcare need outcomes. More work is needed to understand how interpersonal and systemic efforts such as acknowledging bias, providing culturally competent care, and improving shared decision making can aide in disrupting institutional racism and its disparate effects on health service delivery outcomes such as unmet need for CC.(Jindal et al., 2020; Johnson, 2020)
Household poverty and household mental illness may be associated with unmet need for CC due to diminished resources and caregiver reserve.(Chaudry & Wimer, 2016; Fairbrother et al., 2005; S. Gupta & Ford-Jones, 2014) In contrast to the discrimination measure, the measurement of poverty and mental illness was assessed within context of the household and not as directly experienced by the child. There also are some systems in place to identify and attempt to address the healthcare system needs of families experiencing poverty or caregivers with mental illness. (Stein Berman et al., 2018; Weiss-Laxer et al., 2016) In contrast, there are limited systems for identifying and addressing the needs of patients who endure discrimination. In this study, poverty was a significant driver in unmet for need CC with differential impact depending on the additional ACE in the cluster. This finding suggests poverty may be a unique and inciting ACE in the accumulation of other ACEs.(Braveman et al., 2018; A. Gupta, 2017; Pelton, 2015) Given the co-occurring nature of ACEs, routine assessments of poverty should continue alongside additional interventions to reduce child exposure to poverty.
Extending work from prior studies, our findings using a nationally representative sample support the use of ACE latent classes to measure exposure to multiple ACEs and estimate associated outcomes. Such an approach provides more nuanced information to understand the inter-related nature of ACEs. The multiple ACEs latent class identified a population with a high ACE combination, which may be a large driver in unmet service needs. The children in the multiple ACEs latent class had a 50% or greater probability of being exposed to parental divorce, household substance abuse, parental incarceration, domestic violence, household mental illness, and poverty. This clustering of ACEs can inform the selection of interventions which may be more specific or intensive to assist in meeting the health needs of children in that sub-group.
Strengths and Limitations
This study has several strengths, including a large and nationally representative population, extending findings from prior studies on ACE latent classes and identifying a novel ACE latent class of poverty and discrimination with high odds of unmet need of CC. The findings of the study should be viewed with some limitations in mind. This cross-sectional survey relies on parental retrospective reports of ACEs and CC needs. No information was collected on the timing and duration of the ACE nor of the timing of CC need in relation to the ACE, thus causality cannot be inferred. CC questions were only asked of parents who noted their child saw more than one healthcare provider and may under-estimate need, as families whose children only see one healthcare provider may have CC needs as well. The NSCH did not evaluate for physical or sexual abuse, which may lead to under-estimation of ACE exposure and the extent of unmet need for CC.
CONCLUSION
Within a population of U.S. children who have seen more than one healthcare provider in the last 12 months, there are ACE latent classes who have increased odds of unmet need for CC. These sub-groups included children in the household poverty only, multiple ACEs, household poverty and child discrimination, as well as the household poverty and household mental illness latent classes. These findings suggest the need to consider how the latent class approach may provide more nuanced information for evaluating the impact of multiple ACEs on health outcomes and health service needs. The sub-group of children exposed to household poverty and child discrimination had the highest odds of unmet need for CC. Additional studies are needed to fill gaps in disrupting institutional factors contributing to discrimination and inequities in health service need outcomes.
Funding:
This study was supported by the NIH/National Center for Advancing Translational Science (NCATS) Clinical and Translational Science Institute at Children’s National (CTS-CN) Award (Grant Numbers UL1TR001876 and KL2TR001877). This article’s contents are solely the authors’ responsibility and do not represent the official views of NCATS or the NIH.
Abbreviations:
- ACEs
Adverse Childhood Experiences
- CC
Care Coordination
- CSHCN
Children with special health care needs
- FPL
Federal Poverty Level
- NSCH
National Survey of Children’s Health
Footnotes
Conflicts of Interest: The authors have no conflicts of interest relevant to this article to disclose
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Chidiogo Anyigbo, Department of Pediatrics, School of Medicine and Health Sciences, The George Washington University, Division of General Pediatrics and Community Health, Children’s National Hospital, 111 Michigan Ave NW, Washington, DC 20010.
Beth A. Tarini, Department of Pediatrics, School of Medicine and Health Sciences, The George Washington University, Children’s National Research Institute, Children's National Hospital, 1 Inventa Place Silver Spring, MD 20910.
Jichuan Wang, Center for Translational Science, Children's Research Institute, 1 Inventa Place Silver Spring, MD 20910.
Paul Lanier, School of Social Work, The University of North Carolina at Chapel Hill, Tate-Turner-Kuralt Building 548-K, 325 Pittsboro Street, Chapel Hill, NC 27599.
REFERENCES
- Akaike H (1987). Factor analysis and AIC. Psychometrika, 52(3). 10.1007/BF02294359 [DOI] [Google Scholar]
- Amutah C, Greenidge K, Mante A, Munyikwa M, Surya SL, Higginbotham E, Jones DS, Lavizzo-Mourey R, Roberts D, Tsai J, & Aysola J (2021). Misrepresenting Race-The Role of Medical Schools in Propagating Physician Bias. N Engl J Med. 10.1056/NEJMms2025768 [DOI] [PubMed] [Google Scholar]
- Anda RF, Porter LE, & Brown DW (2021). Inside the Adverse Childhood Experience Score: Strengths, Limitations, and Misapplications. American Journal of Preventive Medicine, 60(1), 47–48. 10.1016/j.amepre.2020.01.009 [DOI] [PubMed] [Google Scholar]
- Antonelli RC, Stille CJ, & Antonelli DM (2008). Care coordination for children and youth with special health care needs: A descriptive, multisite study of activities, personnel costs, and outcomes. Pediatrics, 122(1), e209–e216. 10.1542/peds.2007-2254 [DOI] [PubMed] [Google Scholar]
- Auslander WF, Thompson SJ, Dreitzer D, & Santiago JV (1997). Mothers’ satisfaction with medical care: perceptions of racism, family stress, and medical outcomes in children with diabetes. Health Soc Work, 22(3), 190–199. 10.1093/hsw/22.3.190 [DOI] [PubMed] [Google Scholar]
- Bailey ZD, Feldman JM, & Bassett MDT (2020). How Structural Racism Works-Racist Policies as a Root Cause of U.S. Racial Health Inequities. N Engl J Med. 10.1056/NEJMms2025396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barboza GE (2018). Latent Classes and Cumulative Impacts of Adverse Childhood Experiences. Child Maltreatment, 23(2), 111–125. 10.1177/1077559517736628 [DOI] [PubMed] [Google Scholar]
- Bellis MA;, Hughes K;, Ford K;, Ramos Rodriguez G;, Sethi, ;, Passmore J, Bellis MA, Hughes K, Ford K, Rodriguez R, Sethi G, Passmore, &, Bellis MA, Hughes K, Ford K, Ramos Rodriguez G, & Sethi D (2019). Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: a systematic review and meta-analysis. Lancet Public Health, 4(10), 517–528. 10.1016/S2468-2667(19)30145-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellis M, Hughes K, Hardcastle K, Ashton K, Ford K, Quigg Z, & Davies A (2017). The impact of adverse childhood experiences on health service use across the life course using a retrospective cohort study. Journal of Health Services Research and Policy, 22(3), 168–177. 10.1177/1355819617706720 [DOI] [Google Scholar]
- Ben J, Cormack D, Harris R, & Paradies Y (2017). Racism and health service utilisation: A systematic review and meta-analysis. PLoS One, 12(12). 10.1371/journal.pone.0189900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg KL, Shiu CS, Feinstein RT, Msall ME, & Acharya K (2018). Adverse Childhood Experiences Are Associated with Unmet Healthcare Needs among Children with Autism Spectrum Disorder. Journal of Pediatrics, 202, 258–264.e1. 10.1016/j.jpeds.2018.07.021 [DOI] [PubMed] [Google Scholar]
- Bethell CD, Carle A, Hudziak J, Gombojav N, Powers K, Wade R, & Braveman P (2017). Methods to Assess Adverse Childhood Experiences of Children and Families: Toward Approaches to Promote Child Well-being in Policy and Practice. Academic Pediatrics, 17(7), S51–S69. 10.1016/j.acap.2017.04.161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bethell CD, Newacheck P, Hawes E, & Halfon N (2014). Adverse childhood experiences: Assessing the impact on health and school engagement and the mitigating role of resilience. Health Affairs, 33(12), 2106–2115. 10.1377/hlthaff.2014.0914 [DOI] [PubMed] [Google Scholar]
- Bethell CD, Read D, Stein REK, Blumberg SJ, Wells N, & Newacheck PW (2002). Identifying Children With Special Health Care Needs: Development and Evaluation of a Short Screening Instrument. AMBULATORY PEDIATRICS, 2(1), 38–48. [DOI] [PubMed] [Google Scholar]
- Braveman P, Heck K, Egerter S, Rinki C, Marchi K, & Curtis M (2018). Economic Hardship in Childhood: A Neglected Issue in ACE Studies? Maternal and Child Health Journal, 22(3), 308–317. 10.1007/s10995-017-2368-y [DOI] [PubMed] [Google Scholar]
- Brown NM, Brown SN, Briggs RD, Germán M, Belamarich PF, & Oyeku SO (2017). Associations Between Adverse Childhood Experiences and ADHD Diagnosis and Severity. Academic Pediatrics, 17(4), 349–355. 10.1016/j.acap.2016.08.013 [DOI] [PubMed] [Google Scholar]
- Brown NM, Green JC, Desai MM, Weitzman CC, & Rosenthal MS (2014). Need and unmet need for care coordination among children with mental health conditions. Pediatrics, 133(3), e530–e537. 10.1542/peds.2013-2590 [DOI] [PubMed] [Google Scholar]
- Burgess DJ, Ding Y, Hargreaves M, Van Ryn M, & Phelan S (2008). The Association between Perceived Discrimination and Underutilization of Needed Medical and Mental Health Care in a Multi-Ethnic Community Sample. Journal of Health Care for the Poor and Underserved, 19(3), 894–911. 10.1353/hpu.0.0063 [DOI] [PubMed] [Google Scholar]
- Celeux G, & Soromenho G (1996). An entropy criterion for assessing the number of clusters in a mixture model. Journal of Classification, 13(2). 10.1007/BF01246098 [DOI] [Google Scholar]
- Chaudry A, & Wimer C (2016). Poverty is Not Just an Indicator: The Relationship between Income, Poverty, and Child Well-Being. Academic Pediatrics, 16(3), S23–S29. 10.1016/j.acap.2015.12.010 [DOI] [PubMed] [Google Scholar]
- Collins L, & Lanza S (2009). Latent Class and Latent Transition Analysis: With Applications in the Social, Behavioral, and Health Sciences. Wiley. [Google Scholar]
- Council on Children with Disabilities and Medical Home Implementation Project Advisory Committee. (2014). Patient- and family-centered care coordination: A framework for integrating care for children and youth across multiple systems. Pediatrics, 133(5), e1451–e1460. 10.1542/peds.2014-0318 [DOI] [PubMed] [Google Scholar]
- Debowska A, Willmott D, Boduszek D, & Jones AD (2017). What do we know about child abuse and neglect patterns of co-occurrence? A systematic review of profiling studies and recommendations for future research. Child Abuse & Neglect, 70, 100–111. 10.1016/j.chiabu.2017.06.014 [DOI] [PubMed] [Google Scholar]
- Dong M, Anda RF, Felitti VJ, Dube SR, Williamson DF, Thompson TJ, Loo CM, & Giles WH (2004). The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse & Neglect, 28, 771–784. 10.1016/j.chiabu.2004.01.008 [DOI] [PubMed] [Google Scholar]
- Fairbrother G, Kenney G, Hanson K, & Dubay L (2005). How do stressful family environments relate to reported access and use of health care by low-income children? Medical Care Research and Review, 62(2), 205–230. 10.1177/1077558704273805 [DOI] [PubMed] [Google Scholar]
- Feagin J, & Bennefield Z (2014). Systemic racism and U.S. health care. Social Science and Medicine, 103, 7–14. 10.1016/j.socscimed.2013.09.006 [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, & Marks JS (1998). Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults. American Journal of Preventive Medicine, 14(4), 245–258. 10.1016/S0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- Finkelhor D (2018). Screening for adverse childhood experiences (ACEs): Cautions and suggestions. Child Abuse & Neglect, 85, 174–179. 10.1016/j.chiabu.2017.07.016 [DOI] [PubMed] [Google Scholar]
- Gupta A (2017). Poverty and child neglect - The elephant in the room? In Families, Relationships and Societies (Vol. 6, Issue 1, pp. 21–36). Policy Press. 10.1332/204674315X14207948135699 [DOI] [Google Scholar]
- Gupta S, & Ford-Jones E (2014). Recognizing and responding to parental mental health needs: What can we do now? Paediatr Child Health, 19(7), 357–361. [PMC free article] [PubMed] [Google Scholar]
- Heard-Garris NJ, Cale M, Camaj L, Hamati MC, & Dominguez TP (2018). Transmitting Trauma: A systematic review of vicarious racism and child health. Social Science and Medicine, 199, 230–240. 10.1016/j.socscimed.2017.04.018 [DOI] [PubMed] [Google Scholar]
- Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, Jones L, & Dunne MP (2017). The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. The Lancet Public Health, 2(8), e356–e366. 10.1016/S2468-2667(17)30118-4 [DOI] [PubMed] [Google Scholar]
- Jindal M, Heard-Garris N, Empey A, Perrin EC, Zuckerman KE, & Johnson TJ (2020). Getting “Our House” in Order: Re-Building Academic Pediatrics by Dismantling the Anti-Black Racist Foundation. Academic Pediatrics, 20(8), 1044–1050. 10.1016/j.jses.2017.08.002 [DOI] [PubMed] [Google Scholar]
- Johnson TJ (2020). Intersection of Bias, Structural Racism, and Social Determinants With Health Care Inequities. Pediatrics, 146(2). 10.1542/peds.2020-003657 [DOI] [PubMed] [Google Scholar]
- Koball AM, Rasmussen C, Olson-Dorff D, Klevan J, Ramirez L, & Domoff SE (2019). The relationship between adverse childhood experiences, healthcare utilization, cost of care and medical comorbidities. Child Abuse and Neglect, 90, 120–126. 10.1016/j.chiabu.2019.01.021 [DOI] [PubMed] [Google Scholar]
- Lacey RE, Howe LD, Kelly-Irving M, Bartley M, & Kelly Y (2020). The Clustering of Adverse Childhood Experiences in the Avon Longitudinal Study of Parents and Children: Are Gender and Poverty Important? Journal of Interpersonal Violence, 8(886260520935096). 10.1177/0886260520935096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanier P, Maguire-Jack K, Lombardi B, Frey J, & Rose RA (2018). Adverse Childhood Experiences and Child Health Outcomes: Comparing Cumulative Risk and Latent Class Approaches. Maternal and Child Health Journal, 22(3), 288–297. 10.1007/s10995-017-2365-1 [DOI] [PubMed] [Google Scholar]
- Lee H, Kim Y, & Terry J (2020). Adverse childhood experiences (ACEs) on mental disorders in young adulthood: Latent classes and community violence exposure. Preventive Medicine, 134. 10.1016/j.ypmed.2020.106039 [DOI] [PubMed] [Google Scholar]
- Lew D, & Xian H (2019). Identifying Distinct Latent Classes of Adverse Childhood Experiences Among US Children and Their Relationship with Childhood Internalizing Disorders. Child Psychiatry and Human Development, 50(4), 668–680. 10.1007/s10578-019-00871-y [DOI] [PubMed] [Google Scholar]
- Lo Y, Mendell N, & Rubin D (2001). Testing the number of components in a normal mixture. Biometrika, 88(3). 10.1093/biomet/88.3.767 [DOI] [Google Scholar]
- Malawa Z, Gaarde J, & Spellen S (2021). Racism as a Root Cause Approach: A New Framework. Pediatrics, 147(1). 10.1542/peds.2020-015602 [DOI] [PubMed] [Google Scholar]
- McKelvey LM, Whiteside-Mansell L, Zhang D, & Selig JP (2020). Adverse Childhood Experiences in Infancy: a Latent Class Approach Exploring Interrelatedness of Risks. Adversity and Resilience Science, 1(1), 81–93. 10.1007/s42844-020-00003-9 [DOI] [Google Scholar]
- McLaughlin KA, & Sheridan MA (2016). Beyond Cumulative Risk: A Dimensional Approach to Childhood Adversity. Current Directions in Psychological Science, 25(4), 239–245. 10.1177/0963721416655883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLennan JD, MacMillan HL, & Afifi TO (2020). Questioning the use of adverse childhood experiences (ACEs) questionnaires. In Child Abuse and Neglect (Vol. 101). Elsevier Ltd. 10.1016/j.chiabu.2019.104331 [DOI] [PubMed] [Google Scholar]
- Miller R, Tumin D, Hayes D, Uffman JC, Raman VT, & Tobias JD (2019). Unmet Need for Care Coordination among Children with Special Health Care Needs. Population Health Management, 22(3), 255–261. 10.1089/pop.2018.0094 [DOI] [PubMed] [Google Scholar]
- Muthén BO (2002). Beyond SEM: General Latent Variable Modeling. Behaviormetrika, 29(1), 81–117. www.statmodel.com [Google Scholar]
- Muthén LK, & Muthén BO (1998). Statistical Analysis With Latent Variables User’s Guide (Eighth Edition). Muthen & Muthen. www.StatModel.com [Google Scholar]
- Negriff S (2020). ACEs are not equal: Examining the relative impact of household dysfunction versus childhood maltreatment on mental health in adolescence. Social Science and Medicine, 245, 112696. 10.1016/j.socscimed.2019.112696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, & Muthén BO (2007). Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Structural Equation Modeling: A Multidisciplinary Journal, 14(4). 10.1080/10705510701575396 [DOI] [Google Scholar]
- O’donnell ML, Schaefer I, Varker T, Kartal D, Forbes D, Bryant RAA, Silove D, Creamer M, Mcfarlane A, Malhi G, Felmingham K, Van Hoof M, Hadzi-Pavlovic D, Nickerson A, & Steel Z (2017). A systematic review of person-centered approaches to investigating patterns of trauma exposure. Clinical Psychology Review, 57, 208–225. 10.1016/j.cpr.2017.08.009 [DOI] [PubMed] [Google Scholar]
- Pachter LM, & Coll CG (2009). Racism and Child Health: A Review of the Literature and Future Directions NIH Public Access. J Dev Behav Pediatr, 30(3), 255–263. 10.1097/DBP.0b013e3181a7ed5a [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paine S-J, Harris R, Stanley J, Cormack D, & Pōmare E (2018). Caregiver experiences of racism and child healthcare utilisation: cross-sectional analysis from New Zealand. Arch Dis Child, 103, 873–879. 10.1136/archdischild-2017-313866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, Gupta A, Kelaher M, & Gee G (2015). Racism as a Determinant of Health: A Systematic Review and Meta-Analysis. PLoS One, 10(9). 10.1371/journal.pone.0138511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelton LH (2015). The continuing role of material factors in child maltreatment and placement. Child Abuse & Neglect, 41, 30–39. 10.1016/j.chiabu.2014.08.001 [DOI] [PubMed] [Google Scholar]
- Peterson C, Florence C, & Klevens J (2018). The economic burden of child maltreatment in the United States, 2015. Child Abuse and Neglect, 86, 178–183. 10.1016/j.chiabu.2018.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sclove SL (1987). Application of model-selection criteria to some problems in multivariate analysis. Psychometrika, 52(3). 10.1007/BF02294360 [DOI] [Google Scholar]
- Stein Berman R, Patel MR, Belamarich PF, & Gross RS (2018). Screening for Poverty and Poverty-Related Social Determinants of Health Practice Gap. Pediatrics in Review, 39(5), 235–246. 10.1542/pir.2017-0123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stempel H, Cox-Martin M, Bronsert M, Dickinson L Miriam, & Allison MA (2017). Chronic School Absenteeism and the Role of Adverse Childhood Experiences. Acad Pediatr, 17(8), 837–843. 10.1016/j.acap.2017.09.013 [DOI] [PubMed] [Google Scholar]
- Thompson LA, Filipp SL, Mack JA, Mercado RE, Barnes A, Bright M, Shenkman EA, & Gurka MJ (2020). Specific adverse childhood experiences and their association with other adverse childhood experiences, asthma and emotional, developmental and behavioral problems in childhood. Pediatric Research. 10.1038/s41390-020-0784-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toomey SL, Chien AT, Elliott MN, Ratner J, & Schuster MA (2013). Disparities in unmet need for care coordination: The national survey of children’s health. Pediatrics, 131(2), 217–224. 10.1542/peds.2012-1535 [DOI] [PubMed] [Google Scholar]
- Turchi RM, Berhane Z, Bethell C, Pomponio A, Antonelli R, & Minkovitz CS (2009). Care coordination for CSHCN: Associations with family-provider relations and family/child outcomes. Pediatrics, 124(SUPPL. 4), S428–S434. 10.1542/peds.2009-1255O [DOI] [PubMed] [Google Scholar]
- US Census Bureau. (2018). 2016 National Survey of Children’s Health Methodology Report. https://www.census.gov/content/dam/Census/programs-surveys/nsch/tech-documentation/methodology/2016-NSCH-Methodology-Report.pdf
- Wang J, & Wang X (2019). Structural Equation Modeling: Applications Using Mplus (Second Edition). Wiley. [Google Scholar]
- Weiss-Laxer NS, Platt R, Osborne LM, Kimmel M, Solomon BS, Mendelson T, Webb L, & Riley AW (2016). Beyond screening: A review of pediatric primary care models to address maternal depression. Pediatric Research, 79(1–2), 197–204. 10.1038/pr.2015.214 [DOI] [PubMed] [Google Scholar]