Dear Editor,
High-grade B-cell lymphoma (HGBL) with MYC and BCL2 and/or BCL6 rearrangements is associated with an unfavorable prognosis and poor response to standard chemoimmunotherapy for diffuse large-B-cell lymphoma (DLBCL), prompting the recommendation of more intensive treatment approaches in this setting [1–3]. As this entity is uniquely defined by genetic features and requires a MYC rearrangement, it is recommended that B-cell lymphomas with large-cell or high-grade morphology undergo investigation for rearrangements involving this oncogene [4]. Accordingly, fluorescence in situ hybridization (FISH) to identify MYC rearrangements in aggressive B-cell lymphomas is routinely performed in clinical laboratories to ensure accurate diagnostic classification and therapy selection.
MYC rearrangements in DLBCL and HGBL may involve one of many different partner genes, including the immunoglobulin (IG) heavy chain locus, the kappa or lambda light chain locus, or a non-IG locus. While there is some variability across studies, MYC IG partner genes are found in 48–60% of cases and no IG partner is found in 40–52% of cases [5, 6]. Several non-IG rearrangement partners have been described, including PAX5, BCL6, BCL11A, IKZF1, and SOCS1 [7, 8]. Because of the diversity of rearrangement partners and the variability in breakpoints around the MYC locus, a break-apart (BAP) FISH probe is optimal to interrogate this gene region as it allows the most reliable detection of both IG and non-IG MYC rearrangements. Further refinement of rearrangement partners may be achieved with dual-color dual-fusion (DF) probes spanning MYC and IGH, IG-lambda (IGL) or IG-kappa (IGK). Nonetheless, BAP FISH is the most widely adopted technique to evaluate the MYC locus in the clinical laboratory and is often the only FISH assay performed. As a result, the distribution of MYC partner genes and associated FISH patterns in DLBCL/HGBL remain underexplored. Of importance, evidence is emerging that the partner gene to which MYC is juxtaposed may harbor prognostic significance and high resolution next generation sequencing (NGS) technology demonstrates that the genetic landscape underlying MYC rearrangements is more complex than previously recognized [3, 5, 9, 10]. Taken together, these observations underscore the importance of a large-scale appraisal and characterization of MYC FISH results in aggressive B-cell lymphomas. In the present study, we describe MYC FISH patterns and immunoglobulin rearrangement partners in MYC-rearranged (MYC-R) aggressive B-cell lymphoma cases investigated at the Mayo Clinic between 2013 and 2017 which had a concurrent BAP and DF evaluation. Herein, we provide the largest-scale portrait of FISH results of MYC-R B-cell lymphomas, encompassing more than 930 unselected cases.
This retrospective study was approved by the Mayo Clinic institutional review board. Between August 2013 and December 2017, we routinely performed concurrent BAP MYC and DF MYC/IGH, MYC/IGL, MYC/IGK probe sets in paraffin-embedded tissues to detect MYC rearrangements for all suspected HGBL cases, for which final diagnoses may have included HGBL with MYC and BCL2 and/or BCL6 rearrangements, DLBCL, Burkitt lymphoma and HGBL, NOS. Analysis was performed using commercial BAP MYC and MYC/IGH DF probe sets (Abbott Laboratories, Des Plaines, IL, USA) and laboratory-developed DF probes for MYC/IGL and MYC/IGK as described by Einerson, et al. [11]. A total of 100 interphase nuclei were analyzed per probe set by two qualified clinical cytogenetic technologists and interpreted by a board-certified (ABMGG) clinical cytogeneticist. The MYC BAP probe set includes a red (R) and a green (G) probe which respectively hybridize 5′ and 3′ to the MYC gene (chromosomal location 8q24.1), yielding a fusion (F) signal in the setting of an undisturbed gene. In this report, we include MYC-R cases as detected by abnormal MYC BAP results indicated by balanced (RGF-type pattern) or unbalanced (RF-type or GF-type patterns) rearrangements and concurrent DF results. Unbalanced patterns include loss of a separate green or red signal (such as 1R1F for RF-type patterns or 1G1F for GF-type patterns), suggesting potential loss or gain of material. Cases with MYC/IGH fusion identified in the absence of a MYC rearrangement by the MYC BAP probe were excluded from this study, but have been described by King, et al. [10].
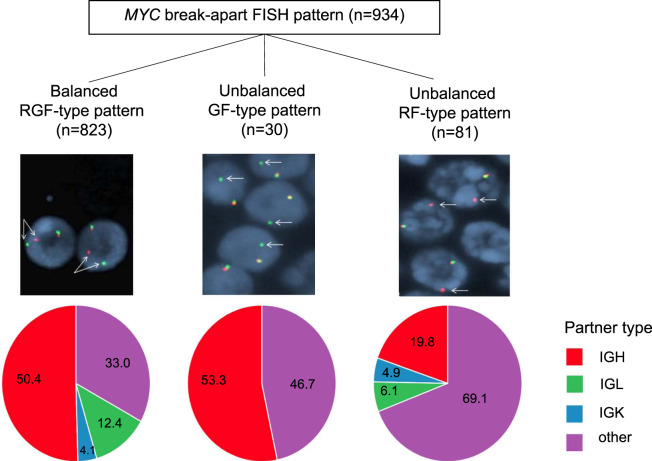
During the four-year study period, a total of 934 independent patient cases were identified to harbor MYC rearrangements. Of these, 592 (63.4%) were translocated to an IG partner, whereas no IG partner was identified in 342 (36.6%) cases. BAP FISH revealed typical balanced results (RGF-type pattern) in 823/934 (88.1%) cases. Among the balanced MYC rearrangement cases, the DF FISH probes identified an IG partner in 551/823 (67.0%) cases; IGH in 415 (50.4%), IGL in 102 (12.4%) and IGK in 34 (4.1%). The remaining 272/823 (33.0%) balanced MYC rearrangements had no IG partner identifiable by DF probe sets. Intriguingly, our data also reveal that a substantial fraction of cases analyzed by the BAP MYC assay harbor unbalanced FISH patterns, as identified in 111 (11.9%) cases. Of these, 81 (8.7%) displayed a RF-type pattern and 30 (3.2%) had a GF-type pattern. Among the RF-type pattern, 25 (30.9%) had an IG partner identified with DF probes (16 IGH, 5 IGL and 4 IGK) while 56 (69.1%) had no detectable IG partner. Among the GF-type pattern, MYC had an IGH partner in 16 (53.3%) cases and no detectable IG partner in 14 (46.7%) cases. No MYC rearrangement involving an IG light chain was found in the GF-type pattern, which may be consistent with IGL/MYC and IGK/MYC rearrangements involving breakpoints located 3’ of MYC [11]. The distribution of FISH patterns is detailed in Fig. 1 and in Supplementary Table 1. In comparison with balanced MYC rearrangements, unbalanced rearrangements are found at an increased frequency in the setting of no identifiable IG partner (RR 1.91, 95% CI 1.61 to 2.27, p-value <0.001), particularly for the RF-type pattern (RR 2.09 95% CI 1.76 to 2.49, p-value <0.001) (Supplementary Table 2).
Fig. 1. MYC break-apart FISH patterns and frequencies.
Representative FISH images of MYC break-apart results, relative frequencies (%) of cases with IG and no IG (other) partners identified by dual-color, dual-fusion FISH probes (from left to right: balanced RGF-type, unbalanced GF-type, unbalanced RF-type patterns).
Few reports have assessed the breadth of MYC FISH rearrangement patterns in DLBCL and HGBL. In a cohort including 51 cases of MYC-R DLBCL detected by FISH BAP, Copie-Bergman, et al., identified a MYC/IGH fusion in 23 cases, a MYC/IGL fusion in 1 case and no IG partner was observed in 26 cases [5]. In a larger patient cohort by Rosenwald et al., encompassing 264 MYC-translocated DLBCL patients, rearrangements involved an IG partner in 107 cases while 88 cases did not display an IG partner [3]. In a previous study by our group including 87 MYC-R cases, the rearrangement partner was IGH in 39, IGL in 7, IGK in 6 and no IG partner was observed in 35 cases [6]. However, there is an overall dearth of literature pertaining to atypical MYC rearrangements by FISH BAP. Our work calls attention to this phenomenon of uncertain significance and its unexpectedly high frequency. While our observations suggest that some of these unbalanced cases appear to represent true MYC rearrangements, as identified by fusion signals with the IG heavy or light chain loci on DF FISH assays, the significance of cases for which no IG partner is identifiable remains unclear (accounting for 7.5% of total cases and 63.0% of unbalanced cases), as these could arise from different genomic alterations such as rearrangements with non-IG partners but also deletions or others. Our study underscores the importance of delineating the genomic mechanisms underlying these atypical FISH findings to allow accurate interpretation of results, especially considering that in multiple myeloma, these have been shown to represent true MYC rearrangements [12].
Importantly, the clinical and prognostic significance of atypical MYC signals by break-apart FISH assays also remain unresolved. As a large reference clinical genomics laboratory with the inability to obtain comprehensive clinical data for patients treated at other institutions, our study is limited by the absence of outcome data to elucidate potential differential prognostic implications of distinct FISH patterns. Additional work to correlate atypical MYC findings with clinical information should be sought. It should also be noted that we solely focused on MYC rearrangements as identified by BAP FISH strategy. However, our group and others have previously highlighted false negative findings with MYC BAP assays, which may occur at a rate of at least 4% [9, 10, 13–15]. Finally, our study may include cases for which the final diagnosis was not restricted to DLBCL or HGBCL, a limitation which is inherent to investigation algorithms of suspected aggressive B-cell lymphoma.
In summary, our study provides the largest portrayal of MYC FISH patterns in aggressive B-cell lymphomas evaluated in paraffin tissue. Importantly, our findings enable appreciation for the existence of frequent unbalanced MYC FISH results with the most used FISH strategy, a MYC BAP probe, resulting in 11.9% of total MYC rearrangement cases with an unbalanced BAP MYC result. In addition, the concurrent application of all 3 DF probes (MYC/IGH, MYC/IGL and MYC/IGK), which are not available/applied in most genomics laboratories, still resulted in 7.5% of total MYC-R cases with an unbalanced BAP MYC FISH result of unclear significance. The genomic alterations leading to these unbalanced FISH patterns should be further explored to guide appropriate interpretation in the clinical laboratory. As a diagnosis of HGBL with MYC and BCL2 and/or BCL6 rearrangements relies, amongst others, on the identification of a MYC rearrangement in a lymphoma with otherwise variable morphology, it is imperative to understand the significance of these atypical FISH findings.
Supplementary information
Acknowledgements
This study was supported by the Mayo Clinic Department of Laboratory Medicine and Pathology.
Author contributions
MG wrote the manuscript; KEP, RPK analyzed the raw data; MG, KEP, RPK, PTG, XX, NLH, EDM, RLK, LBB, JFP reviewed and approved the final manuscript.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Linda B. Baughn, Jess F. Peterson
Supplementary information
The online version contains supplementary material available at 10.1038/s41408-021-00578-1.
References
- 1.Swerdlow, SH, Campo, E, Harris, NL, Jaffe, ES, Pileri SA, Stein, H, et al. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, Revised 4th edn. International Agency for Research on Cancer: Lyon, France, 2017.
- 2.Petrich AM, Gandhi M, Jovanovic B, Castillo JJ, Rajguru S, Yang DT, et al. Impact of induction regimen and stem cell transplantation on outcomes in double-hit lymphoma: a multicenter retrospective analysis. Blood. 2014;124:2354–61. doi: 10.1182/blood-2014-05-578963. [DOI] [PubMed] [Google Scholar]
- 3.Rosenwald A, Bens S, Advani R, Barrans S, Copie-Bergman C, Elsensohn MH, et al. Prognostic significance of MYC rearrangement and translocation partner in diffuse large B-cell lymphoma: a study by the Lunenburg Lymphoma Biomarker Consortium. J Clin Oncol. 2019;37:3359–68. doi: 10.1200/JCO.19.00743. [DOI] [PubMed] [Google Scholar]
- 4.Larson DP, Peterson JF, Nowakowski GS, McPhail ED. A practical approach to FISH testing for MYC rearrangements and brief review of MYC in aggressive B-cell lymphomas. J Hematopathology. 2020;13:127–35. doi: 10.1007/s12308-020-00404-w. [DOI] [Google Scholar]
- 5.Copie-Bergman C, Cuilliere-Dartigues P, Baia M, Briere J, Delarus R, Canioni D, et al. MYC-IG rearrangements are negative predictors of survival in DLBCL patients treated with immunochemotherapy: a GELA/LYSA study. Blood. 2015;126:2466–74. doi: 10.1182/blood-2015-05-647602. [DOI] [PubMed] [Google Scholar]
- 6.McPhail ED, Maurer MJ, Macon WR, Feldman AL, Kurtin PJ, Ketterling RP, et al. Inferior survival in high-grade B-cell lymphoma with MYC and BCL2 and/or BCL6 rearrangements is not associated with MYC/IG gene rearrangements. Haematologica. 2018;103:1899–907. doi: 10.3324/haematol.2018.190157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bertrand P, Bastard C, Maingonnat C, Jardin F, Maisonneuve C, Courel MN, et al. Mapping of MYC breakpoints in 8q24 rearrangements involving non-immunoglobulin partners in B-cell lymphomas. Leukemia. 2007;21:515–23. doi: 10.1038/sj.leu.2404529. [DOI] [PubMed] [Google Scholar]
- 8.Otto C, Scholtysik R, Schmitz R, Kreuz M, Becher C, Hummel M, et al. Novel IGH and MYC translocation partners in diffuse large B-cell lymphomas. Genes Chromosomes Cancer. 2016;55:932–43. doi: 10.1002/gcc.22391. [DOI] [PubMed] [Google Scholar]
- 9.Hilton LK, Tang J, Ben-Neriah S, Alcaide M, Jiang A, Grande BM, et al. The double-hit signature identifies double-hit diffuse large B-cell lymphoma with genetic events cryptic to FISH. Blood. 2019;134:1528–32. doi: 10.1182/blood.2019002600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.King RL, McPhail ED, Meyer RG, Vasmatzis G, Pearce K, Smadbeck JB, et al. False-negative rates for MYC fluorescence in situ hybridization probes in B-cell neoplasms. Haematologica. 2019;104:e248–e251. doi: 10.3324/haematol.2018.207290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Einerson RR, Law ME, Blair HE, Kurtin PJ, McClure RF, Ketterling RP, et al. Novel FISH probes designed to detect IGK-MYC and IGL-MYC rearrangements in B-cell lineage malignancy identify a new breakpoint cluster region designated BVR2. Leukemia. 2006;20:1790–9. doi: 10.1038/sj.leu.2404340. [DOI] [PubMed] [Google Scholar]
- 12.Sharma, N, Smadbeck, JB, Abdallah, N, Zepeda-Mendoza, C, Binder, M, Pearce, KE, et al. The prognostic role of MYC structural variants identified by NGS and FISH in multiple myeloma. Clin Cancer Res. In press. [DOI] [PMC free article] [PubMed]
- 13.Munoz-Marmol AM, Sanz C, Tapia G, Marginet R, Ariza A, Mate JL. MYC status determination in aggressive B-cell lymphoma: the impact of FISH probe selection. Histopathology. 2013;63:418–24. doi: 10.1111/his.12178. [DOI] [PubMed] [Google Scholar]
- 14.Bendig, S, Walter, W, Meggendorfer, M, Bar, C, Fuhrmann, I, Kern, W, et al. Whole genome sequencing demonstrates substantial pathophysiological differences of MYC rearrangements in patients with plasma cell myeloma and B-cell lymphoma. Leuk Lymphoma. In press. [DOI] [PubMed]
- 15.May PC, Foot N, Dunn R, Geoghegan H, Neat MJ. Detection of cryptic and variant IGH-MYC rearrangements in high-grade non-Hodgkin’s lymphoma by fluorescence in situ hybridization: implications for cytogenetic testing. Cancer Genet Cytogenet. 2010;198:71–75. doi: 10.1016/j.cancergencyto.2009.12.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.