Abstract
Background:
Children at end of life have unique and complex care needs. Although there is increasing evidence about pediatric concurrent hospice care, the health care services received while in hospice have not received sufficient attention.
Objectives:
To examine the health care services, unique clusters of health care services, and characteristics of the children in the clusters.
Methods:
Multiple data sources were used including national Medicaid claims data. Children under 21years in pediatric concurrent hospice care were included. Using Medicaid categories assigned to claims, health care services were distributed across 20 categories. Latent class analysis was used to identify clusters of health care services. Demographic profiles of the clusters were created.
Results:
The 6,243 children in the study generated approximately 500,0000 non-hospice, health care service claims while enrolled in hospice care. We identified 3 unique classes of health care services use: low (61.1%), moderate (18.1%), and high (20.8%) intensity. The children in the three classes exhibited unique demographic profiles.
Conclusions:
Health care services cluster together in unique fashion with distinct patterns among children in concurrent hospice care. The findings suggest that concurrent hospice care is not a one-size-fit all solution for children. Concurrent hospice care may be customized and require attention to care coordination to ensure high-quality care.
Keywords: Pediatric hospice care, concurrent hospice care, health care services, Medicaid, latent class analysis, administrative data
Children at end of life have unique and complex care needs. Most of these children have experienced poor health their entire, short life. They have spent a majority of their time in the health care system with frequent hospitalizations and extensive home care.1 For many children, the home has become a mini intensive care unit (ICU) that includes sophisticated medical equipment, complicated medication management, disease-directed treatments, and special nursing care around the clock.2 As their disease progresses and the goals of care shift towards a focus on comfort, children and families may seek additional support through hospice. Pediatric hospice services offer a layer of care focused on pain and symptom management, along with respite and bereavement support.3 With the enactment of the 2010 Affordable Care Act (ACA, Section 2302), children and families have a choice to enroll in hospice care and continue to receive health care services (e.g., life-prolonging care, disease-directed care, curative care) focused on their terminal illness.4,5 As an example, a child with cancer in hospice may continue their chemotherapy and radiation treatments to reduce tumor size or the risk of further metastasis. Thus, concurrent hospice care may offer children a holistic and integrated approach to end of life care.
Although there is increasing evidence about pediatric concurrent hospice care,6–12 the health care services received while in hospice have not received sufficient attention. In a series of case reports, Miller and colleagues identified the health care services used by three pediatric patients cared for by the Pediatric Advanced Care Team at the Children’s Hospital of Philadelphia.13 Among the children in hospice care with degenerative neurologic disorders, progressive inflammatory polyneuropathy, and Huntington’s disease with intractable seizure, the most common health care services were special feedings, medications, ventilators, and private duty nursing. Nurses providing concurrent hospice care in California, New Jersey, and New York identified that their pediatric patients often received IV infusions, private duty nursing, chemotherapy, radiation therapy, and transfusions.14 This preliminary evidence suggests that differences may exist in health care services based on diagnosis and region. Still, national estimates of health care service prevalence and magnitude during concurrent hospice care are unknown. In addition, it is unclear whether there are distinct patterns in the health care services received by children at end of life.
We sought to examine the prevalence of health care services, unique clusters of health care services, and the characteristics of the children in the clusters among a national sample of pediatric concurrent hospice care patients. This study contributes to the pediatric end-of-life literature in several important ways. First, using large national data, the study comprehensively identified the health care services used by children during concurrent hospice care, which has not been done previously. Second, this is the first study that examined the unique clusters of health care services and the characteristics of the children in those clusters. This information is important for nurses, clinicians, and other professionals working with children to identify populations at risk for complicated and potentially fragmented end-of-life care between hospice and non-hospice, health care service providers. A better understanding of these children will enable resources and strategies to be targeted to address their unique needs, and ultimately ensure their quality of care at end of life.
Methods
Study Design and Data
Our study was a retrospective cohort analysis of pediatric decedents. We used national claims data from the 2011 to 2013 Center for Medicare & Medicaid Services Medical Analytical Extract (MAX) files. The MAX files are person-level, administrative claims files prepared by Center for Medicare & Medicaid Services from data submitted by all 50 states and the District of Columbia. We used four MAX files: Personal Summary, Other Therapy, Inpatient, and Prescription Drugs. The Personal Summary files include enrollment and demographic information. These files combine eligibility information, summary claims, and payment data into one record per enrollee. The Other Therapy files include a variety of procedure and diagnoses information. For this study, these files provided claims data on hospice care, along with International Classification of Diseases (9th version ICD-9) and Current Procedural Terminology (CPT) codes. The Inpatient files include hospitalization data with service dates and procedure codes and Prescription Drug files that contain information on prescription fill date and national drug codes. The MAX files are available through Center for Medicare & Medicaid Services, who maintains data quality. We used Medicaid claims data because it is one of the few data sources that includes national pediatric hospice information. In addition, data from 2011 were used because this is the first full year that pediatric concurrent hospice care was enacted and 2013 because it was the most current year for which MAX data were available.
Sample
The Medicaid data files contained 21,383 children enrolled in Medicaid hospice benefit. The sample was restricted to children who used at least one health care service on the same day as hospice care, using their Medicaid claims activity dates.15,16. Because pediatric concurrent hospice care is only available for children under 21 years, we excluded patients over 21 years and those whose birth or death dates were missing. The final sample was 6,243 children who received pediatric concurrent hospice care. Institutional Review Board approval for this study was obtained from the University of Tennessee, Knoxville.
Measures
We used the Medicaid type of service codes that Center for Medicare & Medicaid Services assigned to each non-hospice, health service claim. Twenty categories were applicable to the children in our study: inpatient hospital, durable health equipment, home health, medications, labs & x-rays, other services, targeted case management, physician services, outpatient hospital, personal care, private duty nursing, transportation, rehabilitation, physical therapy/occupational therapy/speech therapy, clinic, other practitioners, psychiatric services, dental services, residential care, and nurse practitioner services. Although some of the categories could have been collapsed because of low count, current evidence suggests that increasing the number of indicators and using high quality indicators improves convergence and reduces parameter bias in statistical analysis.17 For the analysis, the presence of each health service was dichotomized as “yes” or “no.”
For this study, we created a set of demographic variables from the administrative Medicaid data. Age group categories were <1 yr, 1–5 years, 6–14 years, and 15–20 years. Gender was female or male. Race was categorized as Caucasian, Black, and other races. Ethnicity was either Hispanic or non-Hispanic. The presence of multiple complex chronic conditions was the measure of comorbidities.18 Dichotomized variables were created for mental/behavioral health conditions and technology dependence.19,20 Rural/urban was a binary variable based on where the child resided.21 Region was categorized as Midwest, Northeast, South, and West.
Statistical Analysis
Latent class analysis was used to examine clusters of health care services received during pediatric concurrent hospice care. Latent class analysis identifies discrete subgroups or latent classes of similar cases within an overall population.22 This analysis method analyzes individual patterns of data, such as health care services, and identifies common types called classes. Each child is probabilistically assigned to a class. This results in subgroups of children, who are similar to each other and most distinct from those in other classes. We used this method because it accommodated the categorical variables, unlike factor analysis, and unlike cluster analysis, it generated probabilities of class membership.
Latent class analysis is a multi-step process. First, we used the 20 health care services as class indicators and estimated the smallest set of clusters that best fit the data. Several model fit indices were evaluated including Lo-Mendell-Rubin (LMR) likelihood ratio, log likelihood, Akaike information criterion (AIC), Bayesian information criteria (BIC), and entropy values.23,24 Because there is no definitive goodness-of-fit statistics in latent class analysis, several indices were evaluated. A latent class model was considered the best-fit model if it had a lower AIC or BIC value and higher entropy score. Second, the clusters within the best-fit model were described. This included estimating the conditional item-response probabilities of each health care service into the cluster. The probabilities ranged from 0 (non-class membership) to 1 (perfect class membership). Using these conditional probabilities of health care services, we assigned descriptive labels to the latent classes. Third, we examined the demographic characteristics of membership in a given latent class using descriptive statistics (i.e., frequencies). Stata version 15.0 was used for all analyses.25
Results
Figure 1 illustrates the distribution of health services used during pediatric concurrent hospice care. The 6,243 children in the study generated approximately 500,0000 non-hospice, health care service claims while enrolled in hospice care. The most common type of service was inpatient hospital (e.g., enteral infusions, parenteral infusions, mechanical ventilation, transfusions), followed by durable medical equipment (e.g., enteral feeding supplies, oxygen equipment, suctions/pumps), home health (e.g., nursing, therapeutic exercise), and medications (e.g., phenobarbital, sulfamethoxazole and trimethoprim combination, albuterol sulfate). The least commonly used services were dental, residential care, and nurse practitioner.
Figure 1.
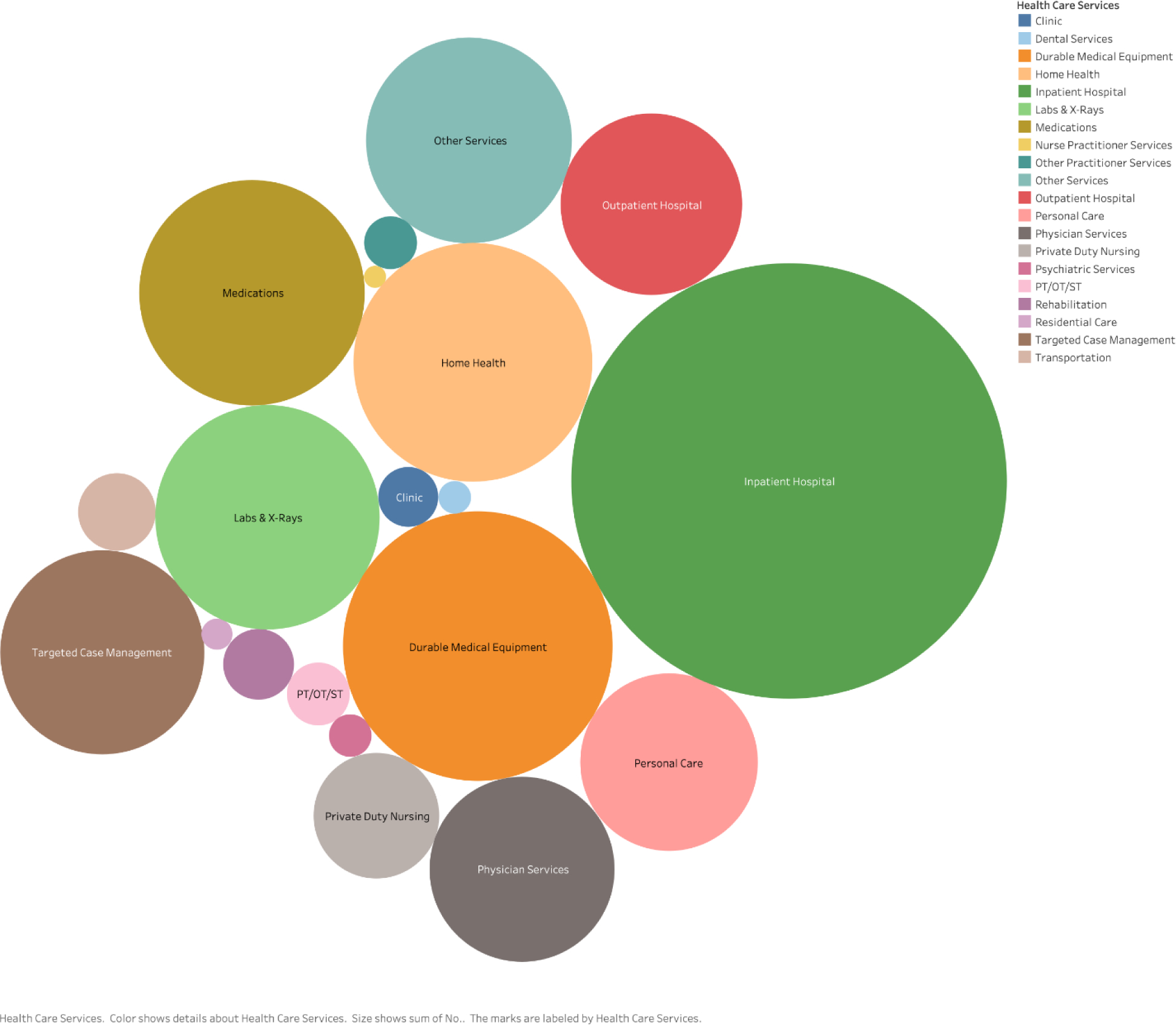
Distribution of Health Care Services Among Children in Concurrent Care
The latent class model fit indices are listed in Table 1. The Lo-Mendell-Rubin probability was unchanged across the 5 different models tested and did not provide strong evidence of class fit. However, as the number of classes increased, AIC and BIC decreased which indicated improved model fit. Improved fit of the model was present only up to three classes as evidenced by the high entropy value.
Table 1.
Model Fit Indices for Latent Class Models
| LMR Testing hypothesis | ------- | 1 class vs. 2 classes | 2 classes vs. 3 classes | 3 classes vs. 4 classes | 4 classes vs. 5 classes |
| No. of parameters | 20 | 41 | 62 | 83 | 104 |
| LMR df | ------- | 21 | 21 | 21 | 21 |
| LMR Coefficient | ------- | 8,243.30 | 1,182.88 | 912.44 | 548.60 |
| LMR probability | ------- | < .001 | < .001 | < .001 | .001 |
| Log likelihood | −33,933.68 | −29,654.82 | −29,040.82 | −28,567.20 | −28,282.44 |
| AIC | 67,907.36 | 59,391.63 | 58,205.65 | 57,300.39 | 56,770.89 |
| BIC | 68,042.14 | 59,667.94 | 58,623.48 | 57,859.75 | 57,465.03 |
| Entropy | ------- | 0.880 | 0.896 | 0.866 | 0.851 |
Note: LMR: Lo-Mendell Rubin test; df: degrees of freedom; AIC: Akaike information criterion; BIC: Bayesian information criterion
For the three-class solution, conditional item-response probabilities are presented in Table 2. We identified 3 unique classes or clusters of health care services use: low, moderate, and high intensity. These labels were assigned based on the number of services in the class with a frequency >10%, frequency range (10% to 100%), and type of service (inpatient vs. outpatient vs. home-based). A total of 61.1% of the sample was expected to belong to Class 1, which had a response pattern we have characterized as “low intensity” health care service use. Children in Class 1 had a high likelihood of using medications (100%) and a moderate likelihood of physician use (54%) and laboratory/x-ray use (16%). All other health care services were very low or less than 10% for Class 1. Class 2 (18.1%) was characterized as “moderate intensity.” These children had a 100% likelihood of using medications and outpatient hospital with moderate likelihood of using laboratory/x-ray (38%), durable medical equipment (32%), and physician (17%). The remaining services were low. Class 3 (20.8%) was characterized as “high intensity.” High intensity children had high likelihood of using medications (99%), physician (87%), laboratory/x-ray (77%), durable medical equipment (74%), outpatient hospital (69%), and inpatient hospital (54%). They had moderate likelihood of using other services (41%), transportation (35%), and home health (30%). Low likelihood of use was found in targeted case management (25%), clinic (18%), personal care (15%), psychiatric services (14%), Physical Therapy/Occupational Therapy/Speech Therapy (10%), and nurse practitioner (10%) with all other services being very low likelihood of use.
Table 2.
Conditional Probabilities of Health Care Services within Three-Class Model (N=6,243)
| Inpatient Hospital | 0.05 | 0.01 | 0.54 |
| Durable Medical Equipment | 0.05 | 0.32 | 0.74 |
| Home Health | 0.01 | 0.01 | 0.30 |
| Medications | 1.00 | 1.00 | 0.99 |
| Labs & X-Rays | 0.16 | 0.38 | 0.77 |
| Other Services | 0.02 | 0.01 | 0.41 |
| Targeted Case Management | 0.01 | 0.01 | 0.25 |
| Physician | 0.54 | 0.17 | 0.87 |
| Outpatient Hospital | 0.03 | 1.00 | 0.69 |
| Personal Care | 0.01 | 0.01 | 0.15 |
| Private Duty Nursing | 0.01 | 0.01 | 0.06 |
| Transportation | 0.03 | 0.01 | 0.35 |
| Rehabilitation | 0.01 | 0.01 | 0.09 |
| PT/OT/ST | 0.01 | 0.01 | 0.10 |
| Clinic | 0.02 | 0.02 | 0.18 |
| Other Practitioner | 0.02 | 0.01 | 0.06 |
| Psychiatric Services | 0.01 | 0.04 | 0.14 |
| Dental | 0.01 | 0.01 | 0.08 |
| Residential Care | 0.01 | 0.01 | 0.04 |
| Nurse Practitioner | 0.01 | 0.01 | 0.10 |
Note: (perfect prediction of class membership = 1.00, perfect prediction of non-class membership = 0.00)
After the latent classes were identified, we examined the demographic composition of the classes (Table 3). The class with low intensity of health care service use during hospice care was primarily 1 to 5 years (36.3%), male (51.5%), Caucasian (59.2%), and non-Hispanic (73.5%). The most common health condition was cardiovascular (18.8%) and approximately a quarter had comorbidities, mental/behavioral health conditions, and technology dependence. They commonly resided in urban areas (60.1%) in the Northeast (75.3%). The children in the moderate intensity group were mostly 1 to 5 years (50.5%), female (50.7%), Black (47.8%), and non-Hispanic (88.0%). The most common health condition was cardiovascular problems (11.7%) and less than a quarter of the sample had comorbidities and technology dependence, while 36.7% had mental/behavioral health conditions. These children frequently resided in urban communities (80.3%) in the Midwest (79.9%). The high intensity group was predominately 1 to 5 years (35.4%), male (53.2%), other races (54.8%), and non-Hispanic (76.5%). It was most common for them to have a neurological/muscular condition (72.3%) with significant rates of comorbidities (88.6%), mental/behavioral health conditions (69.4%), and technology dependence (75.2%). Class 3 children commonly resided in rural communities (51.3%) in the South (48.5%).
Table 3.
Characteristics of Children within Three-Class Model (N=6243)
| Variables | Overall | Class 1 Low Intensity n=3814 |
Class 2 Moderate Intensity n=1133 |
Class 3 High Intensity n=1296 |
|---|---|---|---|---|
| Age Groups (%) | ||||
| <1 yr | 10.9 | 11.1 | <10.0 | 14.8 |
| 1 to 5 yrs | 38.0 | 36.3 | 50.5 | 35.4 |
| 6 to 14 yrs | 31.1 | 32.1 | 29.0 | 27.1 |
| 15 to 20 yrs | 20.0 | 20.5 | 15.0 | 22.7 |
| Gender (%) | ||||
| Female | 48.5 | 48.5 | 50.7 | 46.8 |
| Male | 51.5 | 51.5 | 49.3 | 53.2 |
| Race (%) | ||||
| Caucasian | 51.1 | 59.2 | 45.2 | 32.3 |
| Black | 24.0 | 20.6 | 47.8 | 12.9 |
| Other Races | 24.9 | 20.2 | <10.0 | 54.8 |
| Ethnicity (%) | ||||
| Hispanic | 23.2 | 26.5 | 12.0 | 23.5 |
| Non-Hispanic | 76.8 | 73.5 | 88.0 | 76.5 |
| Health Conditions (%) | ||||
| Cardiovascular | 26.2 | 18.8 | 11.7 | 60.8 |
| Neurological/muscular | 25.6 | 14.9 | <10.0 | 72.3 |
| Cancer | 13.8 | <10.0 | <10.0 | 32.0 |
| Comorbidities (%) | 38.6 | 26.7 | 21.4 | 88.6 |
| Mental/Behavioral Health Conditions (%) | 41.7 | 33.8 | 36.7 | 69.4 |
| Technology Dependence (%) | 31.9 | 21.3 | 17.9 | 75.2 |
| Rural/Urban (%) | ||||
| Urban | 61.4 | 60.1 | 80.3 | 48.7 |
| Rural | 38.6 | 39.9 | 19.7 | 51.3 |
| Region (%) | ||||
| Midwest | 22.9 | <10.0 | 79.9 | 19.8 |
| Northeast | 49.3 | 75.3 | 12.5 | <10.0 |
| South | 17.8 | 11.4 | <10.0 | 48.5 |
| West | 10.0 | <10.0 | <10.0 | 26.6 |
Note: Health conditions are not mutually exclusive; <10.0 is noted for values under 10% per Data Use Agreement
Discussion
In a national sample of Medicaid beneficiaries, three distinct latent classes adequately accounted for variation in patterns of non-hospice, health care services use among children in concurrent hospice care. The clusters of health care services exhibited unique service patterns and demographic profiles from one another. Thus, this analysis presented a novel way to understand the services and the children who used them.
The findings revealed a significant number and wide variety of health care services among children in the study. We identified approximately 500,000 claims for health care services during hospice enrollment with activity in 20 different categories of care, which is consistent with prior studies.13,14 However, our results demonstrated that much of the care delivery focused on feeding and breathing. This finding raises an interesting question - are these types of health care services (e.g., feeding, breathing) related to the care of the child’s condition for which a diagnosis of terminal illness has been made under concurrent hospice care (ACA, Section 2302) or are they hospice services focused on management of common pediatric end-of-life symptoms?26 Since concurrent hospice care’s inception in 2010, it has been unclear among non-hospice medical providers, hospice agencies, and Medicaid personnel, who should be responsible and who will be paid for the health care services.10,14 Our data highlight the basis of the confusion and suggest that additional research is warranted that investigates approaches to identify differences between health care versus hospice care services for children.
In addition, the vast number of services used by children in the sample suggests that care coordination in concurrent hospice care might be significant. Our prior work has shown that coordination during concurrent hospice care varies by state with some states requiring hospice nurses to coordinate (e.g., West Virginia, Oklahoma), while other states require a team effort between providers (e.g., Indiana).9 Thus, the current approaches to care coordination might be overwhelmed by the volume and intensity of health services care among these children. Future research might examine the different types of care coordination and the effectiveness of those approaches in managing a large volume of health care services along with hospice services for children in concurrent hospice care.
Another interesting result was in the different health care services used by class type. While we anticipated that children in concurrent hospice care would have high intensity of health care use, the low intensity group was unexpected. More than half of low intensity children (54%) visited their physician (e.g., pediatrician, primary care physician) and 16% had laboratory and imaging tests done as their only health care services. It is possible that children and families simply wanted to maintain a relationship with a few essential providers even at end of life.27,28 Pediatric concurrent hospice care might enable children and families to minimize such discontinuity of care by providing care with both the physician and hospice care teams, while honoring the decision-making of parents.29 Our finding suggests that concurrent hospice care might be responsive to the preferences and needs of children and families that promote continuous, patient- and family-centered care. Our data did not enable us to examine the role of the physician, location of service, or the specific services provided; however, additional research is warranted that investigates the nature of the encounter with the physician.
Given that the study sample was composed of national Medicaid beneficiaries, it was not surprising to find geographic variation in cluster composition. We identified that low intensity was predominately in the Northeast region, moderate in the Midwest, and high in the South. This finding was consistent with our prior work, which found significant variation in implementation of pediatric concurrent hospice care at the state-level.9 The current study also showed rural/urban differences with classes 1 and 2 predominately urban and class 3 was rural. One possible explanation for these differences is that pediatric health varies geographically, even at end of life. For example, areas in the South such as Appalachia have struggled with health and health outcomes for more than a century, which is especially a problem in rural Appalachia. The health of the children in this area is consistently worse than the national average. Infant mortality rates are 16% higher than in the general population with some rural counties ranging from 17.1 to 500.0 deaths per 1,000 live births.30 In addition, there is a historic distrust of hospice in the South.31,32 Although many areas in the South are medically underserved, it is possible that pediatric concurrent care allows children and families to continue high intensity health care through the pediatric hospitals in their region.33 Thus, pediatric concurrent hospice care may be an important mechanism for access to expanded health care services in areas of poor pediatric health and hospice underutilization.
This study had several limitations to note. The goal of our study was to assess clustering of health care services during concurrent hospice care for Medicaid children. Thus, the findings primarily generalize to this group of children, and results might be different among children in private insurance or Tricare who receive concurrent hospice care. The intention of the study was to describe patterns of health care service use, therefore; we used a pooled cross-sectional data of claims during a three-year period. In addition, the study used data from 2011 to 2013, which is aged. However, these were the most current Medicaid data available. Given that Center for Medicare & Medicaid Services Medicaid data typically takes several years to acquire, ensure a secure data environment, and manage/clean the large complex data files, these data provided the first-ever and most currently available snapshot of the national health care services used by children in concurrent hospice care. Finally, the findings of this study may not be applicable outside the US because pediatric concurrent hospice care is uniquely a US Medicaid approach to pediatric end-of-life care.
To our knowledge, this was the first latent class analysis study of the health care services used during pediatric concurrent hospice care. These services were purposefully selected because of their clinical significance and Medicaid documentation. The results suggest that health care services cluster together in unique fashion with distinct patterns of low, moderate, and high intensity. Additionally, the demographic composition of the clusters differed widely. Accordingly, health care services for children in concurrent hospice care is not a one-size-fits-all solution, which non-hospice and hospice clinicians should consider when caring for a child in concurrent hospice care. Pediatric concurrent hospice care may be customized and require attention to care coordination to ensure high-quality care at end of life for children.
Acknowledgements:
Special thanks to Ms. Jamie Butler and Ms. Whitney Stone for their assistance with the manuscript.
Funding Source:
This publication was made possible by Grant Number R01NR017848 from the National Institute of Nursing Research and National Institute of Health Office of the Director (PI: Lindley). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Nursing Research or National Institutes of Health.
Footnotes
The Author(s) declare(s) that there is no conflict of interest
Contributor Information
Lisa C. Lindley, Nightingale Endowed Faculty Fellow, College of Nursing, University of Tennessee, Knoxville, Knoxville, Tennessee 37996.
Radion Svynarenko, College of Nursing, University of Tennessee, Knoxville, Knoxville, Tennessee 37996.
Kim Mooney-Doyle, School of Nursing, University of Maryland, Baltimore, MD 21201.
Annette Mendola, Department of Medicine, The University of Tennessee Medical Center, Knoxville, TN 37920.
Wendy C. Naumann, University of Tennessee, Knoxville, College of Nursing, Columbus, OH 43221.
Jessica Keim-Malpass, School of Nursing, University of Virginia, Charlottesville, Virginia 22908.
References
- 1.Rogerson CM, Beardsley AL, Nitu ME, Cristea AI. Health care resource utilization for children requiring prolonged mechanical ventilation via tracheostomy. Respir Care. 2020; epub. [DOI] [PubMed] [Google Scholar]
- 2.Lindley LC, Mixer SJ, Mack JW. Home care for children with multiple complex chronic conditions at the end of life: the choice of hospice versus home health. Home Health Care Serv Q. 2017;35(3–4):101–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Academy of Pediatrics, Section on Hospice and Palliative Medicine and Committee on Hospital Care. Pediatric palliative and hospice care commitments, guidelines, and recommendations. Pediatrics. 2013;132(5);966–972. [DOI] [PubMed] [Google Scholar]
- 4.Lindley LC. Health care reform and concurrent curative care for terminally ill children: a policy analysis. J Hosp Palliat Nurs. 2011;13:81–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Keim-Malpass J, Hart TG, Miller JR. Coverage of palliative and hospice care for pediatric patients with a life-limiting illness: A policy brief. J Ped Health Care. 2013;27:511–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lindley LC, Richar CS, Hoit T, Steinhorn DM. The cost of pediatric concurrent hospice care: an economic analysis of relevant cost components, review of the literature, and case illustration. J Palliat Med. 2021;Epub. [DOI] [PubMed] [Google Scholar]
- 7.Lindley LC, Cozad MJ, Svynarenko R, Keim-Malpass J, Mack JW. A national profile of children receiving pediatric concurrent hospice care, 2011 to 2013. J Hosp Palliat Nurs. 2021;23(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lindley LC, Svynarenko R, Beebe L. Mental health and developmental disabilities in US children admitted to hospice care: a comparison of age groups. Int J Palliat Nurs. 2021.epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laird JM, Keim-Malpass J, Mack JW, Cozad MJ, Lindley LC. Examining variation in state Medicaid implementation of ACA: the case of Concurrent Care for Children. Health Aff (Millwood). 2020;39(10):1770–1775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lindley LC, Morvant A. How to hospitalize a child receiving concurrent hospice care. NHPCO Pediatric e-Journal. 2020;60:61–64. [Google Scholar]
- 11.Lindley LC, Keim-Malpass J, Svynarenko R, Cozad MJ, Mack JW, Hinds PS. Pediatric concurrent hospice care: a scoping review and directions for future research. J Hosp Palliat Nurs. 2020;22(3):238–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lindley LC, Edwards SL, Bruce DJ. Factors influencing the implementation of healthcare reform: an examination of the Concurrent Care for Children provision. Am J Hosp Palliat Med. 2014;31(5):527–533. [DOI] [PubMed] [Google Scholar]
- 13.Miller EG, Laragione G, Kang TI, Feudtner C. Concurrent care for the medically complex child: lessons of implementation. J Palliat Med. 2012;15:1281–1283. [DOI] [PubMed] [Google Scholar]
- 14.National Hospice and Palliative Care Organization – Children’s Project on Palliative/Hospice Services. [Internet]. ChiPPS Pediatric Palliative Care Newsletter – November 2013 (#33). [cited 2017 Jan 15]. Available from: https://www.nhpco.org/palliative-care-overview/pediatric-palliative-and-hospice-care/chipps-pediatric-e-journal/
- 15.Mor V, Joyce NR, Cote DL, Gidwani RA, et al. The rise of concurrent care for veterns with advanced cancer at end of life. Cancer. 2016;22(5):782–790. [DOI] [PubMed] [Google Scholar]
- 16.Mor V, Wagner TH, Levy C, Ersek M, Miller SC, Gidwani-Marszowski R, et al. Association of expanded VA hospice care with aggressive care and cost for veterans with advanced lung cancer. JAMA Oncol. 2019;5(6):810–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wurpts IC, Geiser C. Is adding more indicators to a latent class analysis beneficial or detrimental? Results of a Monte-Carlo study. Front Psychol. 2014;5:920–935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lindley LC, Mack JW, Bruce DJ. Clusters of multiple complex chronic conditions: a latent class analysis of children at end of life. J Pain Symptom Manage. 2016;51(5),868–874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex technology dependence and transplantation. BMC Pediatr. 2014;14:199–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Garfield LD, Brown DS, Allaire BT, Ross RE, Nicol GE, Raghaven R. Psychotropic drug use among preschool children in the Medicaid program from 36 states. Am J Public Health. 2005;105(3):524–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Health Resources and Services Administration, Federal Office of Rural Health Policy. [Internet]. Defining rural population. 2018. [cited 2019 Dec 3]. Available from: https://www.hrsa.gov/rural-health/about-us/definition/index.html
- 22.Muthen B Latent variable hybrids: overview of old and new models. In: Hancock GR, Samuelson KM, editors. Advances in latent variable mixture models. Charlotte, NC: Information Age Publishing; 2008. p. 1–24. [Google Scholar]
- 23.Lo Y, Mendell N, Rubin D. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–778. [Google Scholar]
- 24.Nyland KL, Asparouhov T, Muthen B. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Struct Equ Modeling. 2007;14:535–569. [Google Scholar]
- 25.StataCorp LLC. Stata statistical software: Release 15. College Station, TX: StataCorp LP; 2017. [Google Scholar]
- 26.Hendricks-Ferguson V Physical symptoms of children receiving pediatric hospice care at home during the last week of life. Oncol Nurs For. 2008;35(6):e108–e115. [DOI] [PubMed] [Google Scholar]
- 27.Zimmerman K, Bergstraesser E, Engberg S, Ramelet AS, et al. When parents face the death of their child: a nationwide cross-sectional survey of parental perspectives on their child’s end-of-life care. BMC Palliat Care. 2016;epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boyden JY, Ersek M, Deatrick JA, Widger K, LaRagione G, Lord B, Feudtner C. What do parents’ value regarding pediatric palliative and hospice care in the home setting? J Pain Symptom Manage. 2021;61(1),12–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.October TW, Fisher KR, Feudtner C, Hinds PS. The parental perspective: “being a good parent” when making decisions in the PICU. Pediatr Crit Care Med. 2014;15(4):291–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Appalachian Regional Commission. [Internet]. Health disparities in Appalachia: child health. [cited 2019 Nov 24]. Available from: https://www.arc.gov/wp-content/uploads/2021/02/Health_Disparities_in_Appalachia_Child_Health_Domain.pdf
- 31.Mixer S, Fornehed ML, Varney J, Lindley LC. Culturally congruent end-of-life care for rural Appalachian people and their families. J Hosp Palliat Nurs. 2014;16(8):525–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fornehed MC, Mixer SJ, Lindley LC. Families’ decision making at end of life in rural Appalachia. J Hosp Palliat Nurs. 2020;22(3):188–195. [DOI] [PubMed] [Google Scholar]
- 33.Casimir G Why children’s hospitals are unique and so essential. Front Pediatr. 2019;7(305): epub. [DOI] [PMC free article] [PubMed] [Google Scholar]


