Abstract
Background:
Analyzing outcomes and the minimal clinically important difference (MCID) after anterior cruciate ligament reconstruction (ACLR) is of increased interest in the orthopaedic literature. The purposes of this study were to report outcomes after ACLR at medium to long-term follow-up, identify the threshold preoperative outcome values that would be predictive of achieving the MCID postoperatively, and analyze outcome maintenance at medium to long-term follow-up after ACLR.
Methods:
Active athletes who underwent ACLR were identified in an institutional ACL registry. Patient-reported outcome measures (PROMs) were administered preoperatively and at the 2-year and >5-year postoperative follow-up; measures included the International Knee Documentation Committee (IKDC) form, the 12-item Short Form Health Survey (SF-12) Physical Component Summary (PCS) and Mental Component Summary (MCS), and Lysholm scale. We calculated the MCID from baseline to each of the 2 follow-up periods (2-year and mean 7.7-year). Logistic regression was performed to investigate factors associated with achievement of the MCID.
Results:
A total of 142 patients (mean follow-up, 7.7 years [range, 6.6 to 9.1 years]) underwent ACLR. The mean age and body mass index at the time of surgery were 27.2 ± 13.0 years and 23.2 ± 3.0 kg/m2, respectively. Final postoperative outcome scores improved significantly from baseline for the IKDC (50.9 ± 14.7 to 87.9 ± 11.2), SF-12 PCS (41.6 ± 8.9 to 55.6 ± 3.2), and Lysholm scale (62.2 ± 17.6 to 90.5 ± 10.3) (p < 0.0001), while the SF-12 MCS did not improve significantly (54.2 ± 8.0 to 54.4 ± 6.0) (p = 0.763). Between 2- and >5-year follow-up, the SF-12 PCS showed significant improvement (54.6 ± 4.5 to 55.6 ± 3.2; p = 0.036), while no change was noted in the IKDC (87.6 ± 11.1 to 87.9 ± 11.2), SF-12 MCS (55.5 ± 5.3 to 54.4 ± 6.0), and Lysholm scale (89.8 ± 10.6 to 90.5 ± 10.3) (p ≥ 0.09). At the time of final follow-up, the MCID was achieved by 94.7% of patients for the IKDC, 80.8% for the Lysholm, 79.0% for the SF-12 PCS, and 28.2% for the SF-12 MCS. At 2-year follow-up, 95.3% of patients were either “very” or “somewhat” satisfied with their surgery, compared with 88.6% at the time of final follow-up.
Conclusions:
We found a high level of maintained function following ACLR. The IKDC, SF-12 PCS, and Lysholm scores improved significantly after ACLR at the time of final follow-up and were not significantly different between follow-up periods. Approximately 95% and 89% of patients reported being satisfied with the outcome of surgery at the 2-year and final follow-up, respectively.
Level of Evidence:
Therapeutic Level IV. See Instructions for Authors for a complete description of levels of evidence.
Anterior cruciate ligament reconstruction (ACLR) is commonly performed to restore knee stability, improve function, relieve pain, and return recreational and competitive athletes to sports1,2. Patients and surgeons are increasingly looking to preoperative metrics to predict the likelihood of achieving a satisfactory outcome after ACLR3-6. To accomplish this, patient-reported outcome measures (PROMs), such as the International Knee Documentation Committee (IKDC) Subjective Knee Evaluation, the 12-item Short Form Health Survey (SF-12), and the Lysholm scale, have become widely used as benchmarks to measure postoperative improvement7. These questionnaires are readily administered to patients in the preoperative setting and can be followed longitudinally at prescribed intervals during the postoperative period.
The minimal clinically important difference (MCID) is most often defined as the smallest change in outcome that a patient is able to perceive and appreciate8-10. Often, for setting guidelines and flagging ineffective treatments, the MCID is a useful tool for determining the efficacy of a treatment, shifting focus from statistical significance to clinical value10. While others have used PROMs to predict which patients will achieve the MCID at early follow-up, there is currently a paucity of literature predicting achievement of the MCID in ACLR patients at later follow-up4,5.
The purposes of the current study were to (1) report outcomes after ACLR at medium to long-term follow-up, (2) identify threshold preoperative PROMs predictive of achieving the MCID after ACLR, and (3) analyze outcome maintenance from early to medium and long-term follow-up after ACLR. We hypothesized that (1) patient satisfaction would be high and there would be significant improvement in PROMs, (2) threshold preoperative outcome scores that are predictive of postoperative outcome could be defined, and (3) there would be maintenance of achievement of the MCID from early to medium/long-term follow-up.
Materials and Methods
Patients who underwent primary ACLR were prospectively enrolled in an institutional ACL registry from 2009 to 2013. Institutional review board approval was obtained for database querying and to contact patients for follow-up.
Key demographic and clinical variables as well as PROMs were recorded preoperatively and at the 6-month, 1-year, 2-year, and >5-year postoperative follow-ups. Demographic and clinical variables recorded in the registry include age, sex, race/ethnicity, sports participation, mechanism of injury, laterality, graft type, and presence of meniscal tears. PROMs recorded in the registry include the IKDC Subjective Knee Evaluation, the SF-12 Physical Component Summary (PCS) and Mental Component Summary (MCS), the Lysholm scale, and the Marx Activity Scale. Similar to use of the Single Assessment Numeric Evaluation (SANE), patients were also asked to score their knee function on a scale of 0 to 100, with 0 being the worst it has been and 100 being the best it has been (“knee grade”).
There were 2,324 ACLRs performed during the study period by 24 fellowship-trained sports medicine surgeons. The registry was queried for active athletes, defined as patients with a maximum score on the Marx Activity Scale. Patients achieving a maximum Marx Activity Scale score are those who participated in sports ≥4 times per week prior to their injured state. A total of 294 patients from 19 surgeons were identified as being eligible for the study. Because of the methods for registry tracking and data recording, we are unable to provide details regarding the patients who did not meet the inclusion criteria. Patients were contacted by mail and/or telephone by 1 of the authors who had no involvement in the data analysis. Patients were asked to report subsequent knee surgery on the operative or contralateral extremity and to rate their satisfaction with the outcome of their ACLR on an ordinal satisfaction scale: very satisfied, somewhat satisfied, neither satisfied nor dissatisfied, somewhat dissatisfied, or very dissatisfied. Use of this satisfaction scale has been previously reported in the sports medicine literature5,11. There were 142 patients who reported preoperative PROMs in their injured state (completed in the time period between injury and surgery) as well as had a minimum of 2-year and >5-year follow-up (final follow-up).
Statistical Analysis
Data analysis was performed using SAS software, version 9.4 (SAS Institute). The threshold for statistical significance indicating clinical importance was p < 0.05. The Wilcoxon matched-pair signed-rank test was used for statistical comparison of continuous variables, including preoperative versus postoperative and 2-year versus >5-year PROMs. The chi-square test was used for statistical comparison of categorical variables, including patient satisfaction between 2-year and final follow-ups.
The MCID is calculated using either a distribution, anchor, or consensus method8-10. For this study, the distribution method was selected, and the MCID was calculated using half the standard deviation of the difference in outcome scores for each PROM instrument3,12-15. For each PROM instrument, we calculated the MCID from baseline to 2-year and final follow-ups. In addition, to evaluate whether there are preoperative patient-reported outcome scores that could be predictive of achieving the MCID, threshold analyses were performed. Receiver operating characteristic (ROC) curve calculations with area under the curve (AUC) analysis were performed to determine whether threshold preoperative scores could be identified that significantly differentiated patients who did and did not achieve the MCID. Once threshold values were identified, an AUC of ≥0.7 was used to determine whether these threshold values were significantly predictive.
Univariate and multivariate logistical regression analysis was performed to investigate demographic and clinical factors associated with increased or decreased odds of achieving the MCID. Demographic factors, including age and body mass index (BMI), were assessed as continuous variables, while race/ethnicity (White versus non-White), sport (cutting sports, including soccer, lacrosse, football, and basketball, versus skiing and racket sports), and sex were assessed as categorical variables. Clinical factors including duration of follow-up and preoperative PROMs were assessed as continuous variables, while mechanism of injury (contact versus non-contact), laterality, graft type, meniscus pathology, and subsequent knee surgery were assessed as categorical variables. Multivariate logistical regression analysis was performed on variables that achieved a p value of <0.15 during univariate analysis. Odds ratios (ORs) were calculated only for significant predictors in multivariate logistical regression analysis.
Source of Funding
No external funding was received in support of this study.
Results
Demographics of Included Patients
One hundred and forty-two patients completed final follow-up, at a mean of 7.7 years postoperatively (range, 6.6 to 9.1 years). The mean age at the time of surgery (and standard deviation) was 27.2 ± 13.0 years (range, 13 to 63 years). Fifty percent of the patients were female, the mean BMI was 23.2 ± 3.0 kg/m2 (range, 15.7 to 31.3 kg/m2), and 86.6% of the patients were White. Participation in soccer was most common (30.3%), followed by skiing (28.2%) and basketball (17.6%). The majority of injuries (71.8%) resulted from a non-contact mechanism. Meniscal tears were identified in 76 (53.5%) of the patients, involving the lateral meniscus only (n = 32, 22.5%), medial meniscus only (n = 26, 18.3%), and both menisci (n = 18, 12.7%) (Table I).
TABLE I.
Demographic Characteristics*
| No. | % | Mean | SD | Range | |
|---|---|---|---|---|---|
| Total | 142 | 100.0 | |||
| Age (yr) | 142 | 100.0 | 27.2 | 13.0 | 13-63 |
| BMI (kg/m2) | 135 | 95.1 | 23.2 | 3.0 | 15.7-31.3 |
| Laterality | |||||
| Left | 78 | 54.9 | |||
| Right | 64 | 45.1 | |||
| Sex | |||||
| Female | 71 | 50.0 | |||
| Male | 71 | 50.0 | |||
| Race/ethnicity | |||||
| White | 123 | 86.6 | |||
| Black or African American | 5 | 3.5 | |||
| Asian or Pacific Islander | 6 | 4.2 | |||
| Hispanic | 6 | 4.2 | |||
| Other | 1 | 0.7 | |||
| Missing | 1 | 0.7 | |||
| Sport | |||||
| Soccer | 43 | 30.3 | |||
| Skiing | 40 | 28.2 | |||
| Basketball | 25 | 17.6 | |||
| Lacrosse | 13 | 9.2 | |||
| Football | 9 | 6.3 | |||
| Tennis | 7 | 4.9 | |||
| Badminton | 2 | 1.4 | |||
| Missing | 3 | 2.1 | |||
| Injury mechanism | |||||
| Non-contact | 102 | 71.8 | |||
| Contact | 37 | 26.1 | |||
| Missing | 3 | 2.1 | |||
| Meniscal pathology | |||||
| Lateral | 32 | 22.5 | |||
| Medial | 26 | 18.3 | |||
| Both | 18 | 12.7 | |||
| None | 54 | 38.0 | |||
| Missing | 12 | 8.5 | |||
| Another knee surgery | |||||
| No | 111 | 78.2 | |||
| Yes | 31 | 21.8 | |||
| Treatment | |||||
| No | 2 | 1.4 | |||
| Yes, same knee | 16 | 11.3 | |||
| Yes, contralateral knee | 13 | 9.2 | |||
| Graft | |||||
| BTB autograft | 74 | 52.1 | |||
| HT autograft | 33 | 23.2 | |||
| Allograft | 25 | 17.6 | |||
| Missing | 10 | 7.0 |
SD = standard deviation, BMI = body mass index, BTB = bone-tendon-bone, and HT = hamstring tendon.
PROMs
Compared with baseline measures, the mean postoperative IKDC, SF-12 PCS, and Lysholm scale scores improved significantly (p < 0.0001), while the SF-12 MCS did not improve significantly (p = 0.763) at the time of final follow-up (Table II). The mean postoperative knee grade score was 85.4 ± 14.2 (range, 20 to 100), but no comparison to the preoperative state was performed because the score was not collected preoperatively in the registry. Comparing scores between 2-year and final follow-up, no significant changes were observed in the mean IKDC, SF-12 MCS, or Lysholm scores (p > 0.05) (Fig. 1). By contrast, the SF-12 PCS improved significantly (p = 0.036), while knee grade (p = 0.001) scores were significantly worse between 2-year and final follow-up (Table III).
Fig. 1.
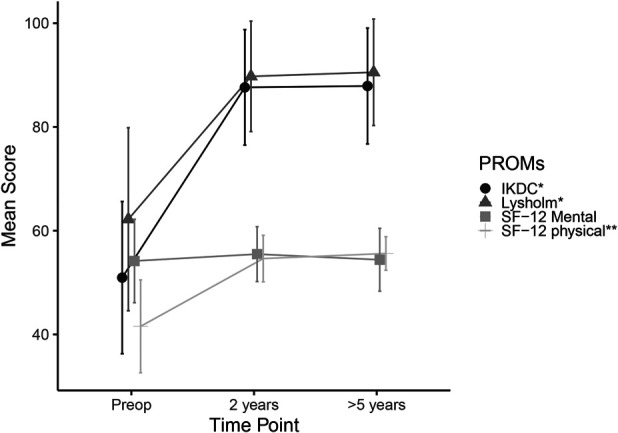
Change in mean IKDC, Lysholm scale, SF-12 MCS, and SF-12 PCS scores over time. Error bars represent 1 standard deviation. Asterisks indicate significance as follows: *baseline to 2-year (p < 0.001) and baseline to final follow-up (p < 0.0001); **baseline to 2-year (p < 0.001), baseline to final follow-up (p < 0.0001), and 2-year to final follow-up (p < 0.05). The Wilcoxon matched-pair signed-rank test was used for comparison between the follow-up periods.
TABLE II.
Change in PROMs from Preoperatively to Final Postoperative Follow-up*
| No. | % | Mean | SD | Min. | Max. | P Value | |
|---|---|---|---|---|---|---|---|
| Follow-up duration (mo) | 142 | 100.0 | 92.9 | 8.7 | 79.0 | 109.0 | |
| IKDC | |||||||
| Preop. | 141 | 99.3 | 50.9 | 14.7 | 13.8 | 88.5 | |
| Postop. | 132 | 93.0 | 87.9 | 11.2 | 42.5 | 100.0 | |
| Net change | 131 | 92.3 | 36.9 | 17.4 | –33.4 | 73.6 | <0.0001 |
| SF-12 MCS | |||||||
| Preop. | 136 | 95.8 | 54.2 | 8.0 | 27.3 | 69.1 | |
| Postop. | 130 | 91.5 | 54.4 | 6.0 | 29.8 | 62.8 | |
| Net change | 124 | 87.3 | 0.4 | 9.3 | –28.3 | 23.8 | 0.763 |
| SF-12 PCS | |||||||
| Preop. | 136 | 95.8 | 41.6 | 8.9 | 25.3 | 60.2 | |
| Postop. | 130 | 91.5 | 55.6 | 3.2 | 36.8 | 61.5 | |
| Net change | 124 | 87.3 | 13.7 | 9.6 | –10.1 | 31.2 | <0.0001 |
| Lysholm scale | |||||||
| Preop. | 141 | 99.3 | 62.2 | 17.6 | 21.0 | 100.0 | |
| Postop. | 121 | 85.2 | 90.5 | 10.3 | 55.0 | 100.0 | |
| Net change | 120 | 84.5 | 27.9 | 20.2 | –32.0 | 74.0 | <0.0001 |
PROMs = patient-reported outcome measures, SD = standard deviation, IKDC = International Knee Documentation Committee, SF-12 = 12-item Short Form Health Survey, PCS = Physical Component Summary, and MCS = Mental Component Summary.
TABLE III.
Change in PROMs Between 2-Year and Final Postoperative Follow-up*
| No. | % | Mean | SD | Min. | Max. | P Value | |
|---|---|---|---|---|---|---|---|
| IKDC | |||||||
| 2-yr | 141 | 99.3 | 87.6 | 11.1 | 47.1 | 100.0 | |
| 5-yr | 132 | 93.0 | 87.9 | 11.2 | 42.5 | 100.0 | |
| Net change | 132 | 93.0 | 0.4 | 15.0 | –2.9 | 2.2 | 0.972 |
| SF-12 MCS | |||||||
| 2-yr | 137 | 96.5 | 55.5 | 5.3 | 33.5 | 63.8 | |
| 5-yr | 130 | 91.5 | 54.4 | 6.0 | 29.8 | 62.8 | |
| Net change | 126 | 88.7 | –1.2 | 8.0 | –0.2 | 2.6 | 0.090 |
| SF-12 PCS | |||||||
| 2-yr | 137 | 96.5 | 54.6 | 4.5 | 35.1 | 63.2 | |
| 5-yr | 130 | 91.5 | 55.6 | 3.2 | 36.8 | 61.5 | |
| Net change | 126 | 88.7 | 1.0 | 5.0 | –1.9 | –0.1 | 0.036 |
| Lysholm scale | |||||||
| 2-yr | 139 | 97.9 | 89.8 | 10.6 | 55.0 | 100.0 | |
| 5-yr | 121 | 85.2 | 90.5 | 10.3 | 55.0 | 100.0 | |
| Net change | 119 | 83.8 | 0.9 | 13.9 | –3.5 | 1.6 | 0.672 |
| Knee grade | |||||||
| 2-yr | 141 | 99.3 | 89.1 | 12.8 | 5.0 | 100.0 | |
| 5-yr | 141 | 99.3 | 85.4 | 14.2 | 20.0 | 100.0 | |
| Net change | 140 | 98.6 | –3.8 | 14.2 | 1.4 | 6.1 | 0.001 |
PROMs = patient-reported outcome measures, SD = standard deviation, IKDC = International Knee Documentation Committee, SF-12 = 12-item Short Form Health Survey, PCS = Physical Component Summary, and MCS = Mental Component Summary.
Patient Satisfaction
Among patients who responded to the satisfaction question, 95.3% reported being “very satisfied” or “somewhat satisfied” with the outcome of surgery at the 2-year follow-up compared with 88.7% of patients at the >5-year follow-up. There was a significant decrease in the number of patients reporting that they were “very satisfied” between 2- and >5-year follow-up (p < 0.0001) (Table IV).
TABLE IV.
Postoperative Patient Satisfaction
| 2-Yr | >5-Yr | |||
|---|---|---|---|---|
| No. | % | No. | % | |
| Very satisfied | 106 | 74.6 | 93 | 65.5 |
| Somewhat satisfied | 16 | 11.3 | 32 | 22.5 |
| Neither satisfied nor dissatisfied | 1 | 0.7 | 2 | 1.4 |
| Somewhat dissatisfied | 5 | 3.5 | 11 | 7.7 |
| Very dissatisfied | 0 | 0.0 | 3 | 2.1 |
| Missing | 14 | 9.9 | 1 | 0.7 |
MCID
The MCIDs calculated using the distribution method at 2-year and final follow-up are reported in Table V. The postoperative MCID decreased for all PROMs between 2-year and final follow-up. ROC curve analysis for preoperative PROMs revealed that scoring below the following values was predictive of achieving the MCID: IKDC, 62.1 (AUC, 0.952), SF-12 PCS, 50.3 (AUC, 0.988), SF-12 MCS, 53.2 (AUC, 0.949), and Lysholm, 74.0 (AUC, 0.933). At mean 7.7-year follow-up, threshold postoperative scores for the MCID were achieved by 94.7% of patients for the IKDC, 80.8% for the Lysholm, 79.0% for the SF-12 PCS, and 28.2% for the SF-12 MCS scores.
TABLE V.
MCID Postoperative Threshold Values and Achievement*
| 2-Yr MCID Threshold | 2-Yr % Achieved | >5-Yr MCID Threshold | >5 Yr % Achieved | |
|---|---|---|---|---|
| IKDC | 9.5 | 92.9 | 8.7 | 94.7 |
| SF-12 MCS | 5.1 | 31.3 | 4.7 | 28.2 |
| SF-12 PCS | 5.2 | 76.3 | 4.8 | 79.0 |
| Lysholm | 10.6 | 81.2 | 10.1 | 80.8 |
MCID = minimal clinically important difference, IKDC = International Knee Documentation Committee, SF-12 = 12-item Short Form Health Survey, PCS = Physical Component Summary, and MCS = Mental Component Summary.
Univariate and Multivariate Logistical Regression Analyses
Logistical regression analyses were used to identify patient and surgical variables associated with achieving the MCID at the time of final follow-up. In the univariate analysis, the presence of any meniscal tear was associated with significantly decreased odds of achieving the MCID for the IKDC score (p = 0.022); however, this association was not significant in the multivariate analysis. On multivariate analysis, higher preoperative IKDC, SF-12 MCS, SF-12 PCS, and Lysholm scores were associated with significantly decreased odds of achieving the MCID for the IKDC (OR = 0.83, 95% confidence interval [CI] = 0.72 to 0.96; p = 0.01), SF-12 MCS (OR = 0.62, 95% CI = 0.50 to 0.76; p < 0.0001), SF-12 PCS (OR = 0.49, 95% CI = 0.33 to 0.74; p = 0.001), and Lysholm (OR = 0.82, 95% CI = 0.75 to 0.89; p < 0.0001) scores, respectively. Additionally, patients with skiing as their primary sport had significantly increased odds of achieving the MCID for the Lysholm score compared with those participating primarily in cutting sports including soccer, lacrosse, football, and basketball (OR = 43.4, 95% CI = 2.0 to 927.8).
Discussion
In this study, we analyzed outcomes at medium to long-term follow-up (mean, 7.7 years) in an active cohort of patients who underwent ACLR. We confirmed our hypotheses that there would be significant improvement in PROMs, high patient satisfaction, and a high rate of achievement of the MCID as well as maintenance of the MCID out to medium/long-term.
Patients improved from baseline to final follow-up with respect to IKDC, SF-12 PCS, and Lysholm scale scores. From the 2-year to the final follow-up, these scores did not differ significantly other than in the SF-12 PCS, which improved, and knee grade, which slightly worsened over that time period.
There is evidence that maximum improvement after ACLR occurs around 1 year postoperatively, and this study demonstrates that improvements are largely preserved at a mean follow-up of 7.7 years16. The MOON (Multicenter Orthopaedic Outcomes Network) group also noted that patient-reported outcome scores were improved at 2 years and preserved at 6 and 10 years postoperatively2. The mean IKDC score for our cohort was similar to theirs (88 versus 86) at the time of final follow-up. Additionally, there is a paucity of literature examining the SF-12 MCS and PCS scores after ACLR. This includes defining the MCID for the SF-12 MCS and PCS as well as their results at midterm follow-up. This study adds to the literature by serving as a potential reference for further studies.
While the rate of patients who were “very satisfied” decreased from 2-year to final follow-up, from 74.6% to 65.5%, the vast majority of patients (88.6%) were either “very satisfied” or “somewhat satisfied” at the time of final follow-up. In a systematic review, Kahlenberg et al.11 demonstrated that reporting on satisfaction after ACLR has declined in the past decade. As health care moves toward valuing care from the patient’s perspective, it is increasingly important to demonstrate that a given procedure increases patient satisfaction17,18. This study demonstrates that ACLR leads to high levels of patient satisfaction at a mean follow-up of 7.7 years. Despite high satisfaction, it is interesting to note that the proportion of patients who reported they were “very satisfied” with the surgery declined between the 2 follow-up periods. This may be related to the known sequelae of early posttraumatic osteoarthritis that has been shown to occur in patients who experience an ACL tear and reconstruction19,20. Further research should be conducted to determine the variables that patients consider in terms of satisfaction following ACLR.
The threshold MCID value decreased for all outcome scores from 2-year to final follow-up. Prior studies have examined the MCID for the IKDC form for a mix of pathological conditions, but there is limited evidence examining the MCID after ACLR21. The MCIDs at final postoperative follow-up were similar to those of a previous study examining 231 patients with 2-year follow-up (8.7 versus 9.0 for the IKDC, 4.7 versus 4.3 for the SF-12 MCS, 4.8 versus 5.2 for the SF-12 PCS, and 10.1 versus 10.0 for the Lysholm scale, respectively)22. This is the first study, to our knowledge, to examine the MCID at longer-term follow-up after ACLR and demonstrates that a majority of patients achieved the MCID for the IKDC (94.7%), the Lysholm scale (80.8%), and the SF-12 PCS (79%), but only 28.2% achieved the MCID for the SF-12 MCS. The lack of MCID achievement for the SF-12 MCS is likely explained by the fact that the SF-12 MCS is a relatively stable construct that is intrinsic to the patient and less likely to change with surgical intervention.
The preoperative threshold values for achieving the MCID are useful for preoperative counseling of patients. It is increasingly recognized that more focus should be placed on achieving clinically important differences than just significant differences. It is encouraging for surgeons and patients to know that those with lower scores preoperatively are more likely to clinically benefit from ACLR. Similarly, Chen et al.4 demonstrated that lower PROMIS (Patient-Reported Outcomes Measurement Information System) physical function scores preoperatively were associated with an increased likelihood of achieving the MCID postoperatively. Conversely, it is also important for patients and surgeons to understand that higher preoperative scores correlate negatively with achieving the MCID. This finding may be subject to a ceiling effect, in that patients who start with higher scores have less room for improvement (and therefore for reaching the MCID).
An additional distinction of this study compared with others is the inclusion criterion of a maximum score on the Marx Activity Scale preoperatively, indicating that the patients are very active at baseline (preinjury state). By contrast, the MOON study with 10-year follow-up included patients with a preoperative Marx Activity Scale score ranging from 8 to 162. Furthermore, the type of sport has been shown to have an effect on outcomes after ACLR. On multivariate analysis, patients whose primary sport was skiing had increased odds of achieving the MCID for the Lysholm score compared with those who primarily participated in cutting sports. Skiing and snowboarding have previously been identified with a high rate of return to sport and previous performance levels23. This information can also be utilized in preoperative counseling of patients based on their primary sport.
This study had several limitations. We used an institutional registry, which includes ACLRs performed by 24 surgeons; there is, therefore, heterogeneity in graft choice, surgical technique, treatment of meniscal tears, and postoperative rehabilitation. Additionally, the role of preoperative physical therapy was not accounted for in this cohort. Patients who participate in post-injury but presurgical physical therapy may have improved baseline PROMs, which could confound the results of predicting the MCID. Baseline PROMs were obtained at the patients’ first visit with the orthopaedic surgeon, but there could be a subset of patients who were already participating in physical therapy prior to being evaluated. Given that our study was a retrospective review of prospectively collected data, the MCID was calculated using a distribution method. This precluded us from performing any sensitivity analysis around the MCID values as there was no opportunity to introduce an anchor question.
Conclusions
We found a high level of maintained function at >5 years following ACL reconstruction—specifically, the IKDC, SF-12 PCS, and Lysholm scores showed significant improvement after ACLR at >5-year follow-up, and overall outcomes did not differ significantly between 2- and >5-year follow-up. Approximately 95% of the patients reported being satisfied with the outcome of surgery at 2-year follow-up, and this had only diminished to 89% by final follow-up. The high percentage of patients achieving the MCID remained consistent from 2-year to final follow-up, indicating clinical outcome maintenance in the medium to long term.
Acknowledgments
Note: On behalf of the HSS ACL Registry Group, the authors acknowledge members of the Sports Medicine Institute at the Hospital for Special Surgery who contributed patients to the ACL registry utilized in this study: Struan H. Coleman, MD, PhD; Frank A. Cordasco, MD, MS; Stephen Fealy, MD; Jo A. Hannafin, MD, PhD; John D. MacGillivray, MD; Robert G. Marx, MD; Michael J. Maynard, MD; Stephen J. O’Brien, MD, MBA; Andrew D. Pearle, MD; Anil S. Ranawat, MD; Scott A. Rodeo, MD; Howard A. Rose, MD; Beth E. Shubin Stein, MD; Sabrina M. Strickland, MD; Russell F. Warren, MD; and Thomas L. Wickiewicz, MD.
Footnotes
A list of the HSS ACL Registry Group members is provided in a Note at the end of the article.
Investigation performed at the Sports Medicine Institute, Hospital for Special Surgery, New York, NY
Disclosure: The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A337).
Contributor Information
Collaborators: Struan H. Coleman, Frank A. Cordasco, Stephen Fealy, Jo A. Hannafin, John D. MacGillivray, Robert G. Marx, Michael J. Maynard, Stephen J. O’Brien, Andrew D. Pearle, Anil S. Ranawat, Scott A. Rodeo, Howard A. Rose, Beth E. Shubin Stein, Sabrina M. Strickland, Russell F. Warren, and Thomas L. Wickiewicz
References
- 1.Mohtadi NG, Chan DS. Return to Sport-Specific Performance After Primary Anterior Cruciate Ligament Reconstruction: A Systematic Review. Am J Sports Med. 2018. Nov;46(13):3307-16. Epub 2017 Oct 13. [DOI] [PubMed] [Google Scholar]
- 2.Spindler KP, Huston LJ, Chagin KM, Kattan MW, Reinke EK, Amendola A, Andrish JT, Brophy RH, Cox CL, Dunn WR, Flanigan DC, Jones MH, Kaeding CC, Magnussen RA, Marx RG, Matava MJ, McCarty EC, Parker RD, Pedroza AD, Vidal AF, Wolcott ML, Wolf BR, Wright RW; MOON Knee Group. Ten-Year Outcomes and Risk Factors After Anterior Cruciate Ligament Reconstruction: A MOON Longitudinal Prospective Cohort Study. Am J Sports Med. 2018. Mar;46(4):815-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berliner JL, Brodke DJ, Chan V, SooHoo NF, Bozic KJ. John Charnley Award: Preoperative Patient-reported Outcome Measures Predict Clinically Meaningful Improvement in Function After THA. Clin Orthop Relat Res. 2016. Feb;474(2):321-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen RE, Papuga MO, Voloshin I, Nicandri GT, Goldblatt JP, Bronstein RD, Rouse LM, Maloney MD. Preoperative PROMIS Scores Predict Postoperative Outcomes After Primary ACL Reconstruction. Orthop J Sports Med. 2018. May 8;6(5):2325967118771286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nwachukwu BU, Voleti PB, Berkanish P, Chang B, Cohn MR, Williams RJ, 3rd, Allen AA. Return to Play and Patient Satisfaction After ACL Reconstruction: Study with Minimum 2-Year Follow-up. J Bone Joint Surg Am. 2017. May 3;99(9):720-5. [DOI] [PubMed] [Google Scholar]
- 6.Werner BC, Chang B, Nguyen JT, Dines DM, Gulotta LV. What Change in American Shoulder and Elbow Surgeons Score Represents a Clinically Important Change After Shoulder Arthroplasty? Clin Orthop Relat Res. 2016. Dec;474(12):2672-81. Epub 2016 Jul 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Makhni EC, Padaki AS, Petridis PD, Steinhaus ME, Ahmad CS, Cole BJ, Bach BR, Jr. High Variability in Outcome Reporting Patterns in High-Impact ACL Literature. J Bone Joint Surg Am. 2015. Sep 16;97(18):1529-42. [DOI] [PubMed] [Google Scholar]
- 8.Nwachukwu BU, Chang B, Rotter BZ, Kelly BT, Ranawat AS, Nawabi DH. Minimal Clinically Important Difference and Substantial Clinical Benefit After Revision Hip Arthroscopy. Arthroscopy. 2018. Jun;34(6):1862-8. Epub 2018 Apr 10. [DOI] [PubMed] [Google Scholar]
- 9.Nwachukwu BU, Fields K, Chang B, Nawabi DH, Kelly BT, Ranawat AS. Preoperative Outcome Scores Are Predictive of Achieving the Minimal Clinically Important Difference After Arthroscopic Treatment of Femoroacetabular Impingement. Am J Sports Med. 2017. Mar;45(3):612-9. Epub 2016 Oct 23. [DOI] [PubMed] [Google Scholar]
- 10.Katz NP, Paillard FC, Ekman E. Determining the clinical importance of treatment benefits for interventions for painful orthopedic conditions. J Orthop Surg Res. 2015. Feb 3;10:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kahlenberg CA, Nwachukwu BU, Ferraro RA, Schairer WW, Steinhaus ME, Allen AA. How Are We Measuring Patient Satisfaction After Anterior Cruciate Ligament Reconstruction? Orthop J Sports Med. 2016. Dec 10;4(12):2325967116673971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chesworth BM, Mahomed NN, Bourne RB, Davis AM; OJRR Study Group. Willingness to go through surgery again validated the WOMAC clinically important difference from THR/TKR surgery. J Clin Epidemiol. 2008. Sep;61(9):907-18. Epub 2008 Feb 14. [DOI] [PubMed] [Google Scholar]
- 13.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003. May;41(5):582-92. [DOI] [PubMed] [Google Scholar]
- 14.Quintana JM, Escobar A, Bilbao A, Arostegui I, Lafuente I, Vidaurreta I. Responsiveness and clinically important differences for the WOMAC and SF-36 after hip joint replacement. Osteoarthritis Cartilage. 2005. Dec;13(12):1076-83. Epub 2005 Sep 9. [DOI] [PubMed] [Google Scholar]
- 15.Wyrwich KW, Bullinger M, Aaronson N, Hays RD, Patrick DL, Symonds T; Clinical Significance Consensus Meeting Group. Estimating clinically significant differences in quality of life outcomes. Qual Life Res. 2005. Mar;14(2):285-95. [DOI] [PubMed] [Google Scholar]
- 16.Agarwalla A, Puzzitiello RN, Liu JN, Cvetanovich GL, Gowd AK, Verma NN, Cole BJ, Forsythe B. Timeline for Maximal Subjective Outcome Improvement After Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2019. Aug;47(10):2501-9. Epub 2018 Nov 12. [DOI] [PubMed] [Google Scholar]
- 17.Graham B, Green A, James M, Katz J, Swiontkowski M. Measuring patient satisfaction in orthopaedic surgery. J Bone Joint Surg Am. 2015. Jan 7;97(1):80-4. [DOI] [PubMed] [Google Scholar]
- 18.Nwachukwu BU, Hamid KS, Bozic KJ. Measuring Value in Orthopaedic Surgery. JBJS Rev. 2013. Nov 19;1(1):01874474-201311000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Cinque ME, Dornan GJ, Chahla J, Moatshe G, LaPrade RF. High Rates of Osteoarthritis Develop After Anterior Cruciate Ligament Surgery: An Analysis of 4108 Patients. Am J Sports Med. 2018. Jul;46(8):2011-9. Epub 2017 Oct 6. [DOI] [PubMed] [Google Scholar]
- 20.Wang LJ, Zeng N, Yan ZP, Li JT, Ni GX. Post-traumatic osteoarthritis following ACL injury. Arthritis Res Ther. 2020. Mar 24;22(1):57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res (Hoboken). 2011. Nov;63(Suppl 11):S208-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nwachukwu BU, Chang B, Voleti PB, Berkanish P, Cohn MR, Altchek DW, Allen AA, Williams RJ. Preoperative Short Form Health Survey Score Is Predictive of Return to Play and Minimal Clinically Important Difference at a Minimum 2-Year Follow-up After Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2017. Oct;45(12):2784-90. Epub 2017 Jul 20. [DOI] [PubMed] [Google Scholar]
- 23.Erickson BJ, Harris JD, Fillingham YA, Cvetanovich GL, Bhatia S, Bach BR, Jr, Bush-Joseph CA, Cole BJ. Performance and Return to Sport After Anterior Cruciate Ligament Reconstruction in X-Games Skiers and Snowboarders. Orthop J Sports Med. 2013. Nov 7;1(6):2325967113511196. [DOI] [PMC free article] [PubMed] [Google Scholar]


