Abstract
Basal cell nevus syndrome (BCNS) is a rare neurocutaneous syndrome characterized by tumorigeneses such as basal cell carcinomas, jaw cysts, ovarian fibromas, and cardiac fibromas. We present a 24-year-old female with calcified ovarian fibromas associated with BCNS. She had a surgical history of the maxillary cyst and was diagnosed with BCNS due to the cutaneous pits. Magnetic resonance imaging indicated an 8-cm mass and a 4-cm mass, which had been suspected to be a subserosal myoma and a fibroma, respectively. GnRH agonist was preoperatively administered; however, the size of the masses did not change. In laparoscopy, a tumor consisting of 8- and 5-cm masses in the right ovary was identified, and tumorectomy was performed. Because both tumors were extraordinarily rigid and could not be morcellated with scalpels or scissors, we removed them by the Luer Bone Rongeurs with minilaparotomy. The histopathological diagnosis was the ovarian fibromas with marked calcification.
Keywords: Basal cell nevus syndrome, Gorlin syndrome, ovarian fibroma
INTRODUCTION
Basal cell nevus syndrome (BCNS, Gorlin syndrome) is a rare autosomal dominant disorder with a prevalence of 1 in 60,000 to 1 in 160,000, caused by Patched-1 (PTCH1) or suppressor of fused (SUFU) mutations.[1,2,3,4] In women, BCNS is characterized by the development of tumorigeneses such as basal cell carcinoma (basal cell carcinoma syndrome [BCCS]), jaw cyst, cardiac fibroma, and ovarian fibroma. Ovarian fibroma occurs in 14%–24% of patients diagnosed as BCNS.[5] We experienced a patient with calcified ovarian fibromas associated with BCNS.
CASE REPORT
The patient was a 24-year-old nulliparous female without sexual experience. She had undergone the surgeries of the maxillary cyst at the age of 18 and 20 years. With reference to the diagnosis criteria of this syndrome, she was given the definitive diagnosis as BCNS with the odontogenic keratinocytes of the jaw, the three of more palmar or plantar pits as the major criteria, in addition, with the ovarian fibroma as the minor criteria, whereas she did not have the bilamellar calcification of the falx cerebri, the bifid, fused or markedly splayed ribs, and the first, degree relative with this syndrome. First, she visited a gynecologic clinic for uterine cervical cancer screening. A fist-size pelvic mass was found by transrectal ultrasonography, and then, she was referred to our hospital. The magnetic resonance imaging (MRI) of the pelvis indicated an 8-cm suspected subserosal myoma that showed the iso-intensity to the myometrium on T1-weighted images and exhibited uneven signals on T2-weighted images of the ventral uterine side. Furthermore, a 4-cm tumor was suspected to be an ovarian fibroma because of the hypo-intensity on T1- and T2-weighted images of the right ovary [Figure 1a]. We decided the patient be indicated for the surgery. Although the GnRH agonist was preoperatively administered for 3 months to decrease the size of the myoma, the tumor did not shrink. Before re-evaluation by MRI scans, we had planned to perform the tumorectomy and myomectomy for the right ovarian tumor and uterine myoma. Re-evaluation by MRI indicated that both pelvic masses were originated from the right ovary and that the interstitial of the right ovary was edematous, the massive ovarian edema [Figure 1b]. Therefore, we decided to perform the right ovarian tumorectomy.
Figure 1.
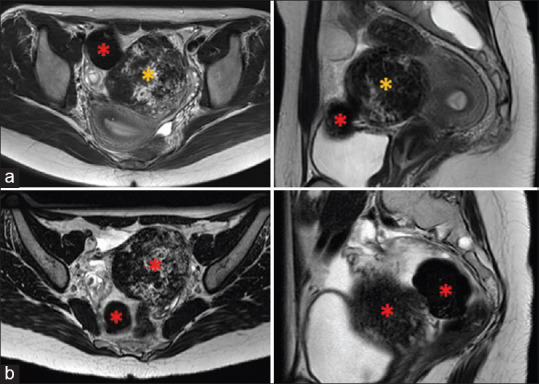
Magnetic resonance imaging findings of the pelvic cavity (T2-weighted images). (a) First visit: A subserosal myoma (8 cm in diameter: yellow asterisk) and a right ovarian fibroma (4 cm in diameter: red asterisk) had been suspected before the surgery. (b) After GnRH treatment: Both pelvic masses (red asterisk) were primary tumors that originated from the right ovary. The massive ovarian edema was observed
Intraoperative findings on laparoscopic surgery showed that there was no uterine myoma, and white and smooth superficial masses of 8 and 5 cm in diameter were found in the right ovary [Figure 2a]. Both tumors were extremely rigid and could not be morcellated with surgical scalpels or Cooper's scissors. We made a 2.5-cm incision in the lower abdomen and then fitted the Smart retractor® (TOP Corporation, Tokyo, Japan) and the Free access® (TOP Corporation) to the abdominal wall [Figure 2b and c]. From this space, the tumors were excised little by little using the Luer Bone Rongeurs (ISO Medical Systems, Tokyo, Japan) and removed them [Figure 2d and e]. The histopathological diagnosis was the ovarian fibroma with marked calcification and no malignancy.
Figure 2.
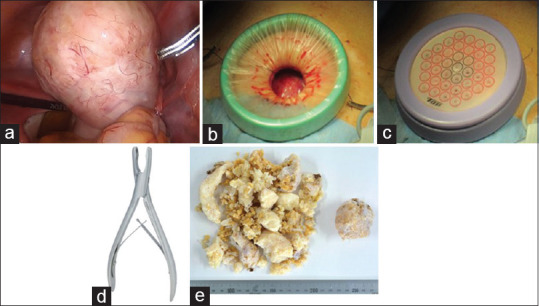
Intraoperative findings and surgical instruments. (a) Right ovarian tumor containing smooth whitish masses of 8 and 5 cm in diameter was laparoscopically found. (b) Smart retractor®, (c) Free access®, and (d) Luer Bone Rongeurs® were used for morcellation and removal of the tumors. (e) Macroscopic finding of the resected tissue after formalin-fixation
We recommended the patient to receive genetic counseling. She had no relatives of BCNS, and sporadic occurrence was suspected. The patient has not shown any findings of recurrence until 1 year after the surgery.
DISCUSSION
BCNS, also known as Gorlin syndrome or nevoid BCCS, is a highly tumorigenic and genetic disease reported by Gorlin and Goltz in 1960.[6] The characteristics of BCNS are the multiple tumorigeneses and the body malformations, such as jaw cysts, pitting-palms, and intracranial calcification, and the composite tumorigeneses, such as BCCS, medulloblastomas, ovarian fibromas, and heart fibromas. The early diagnosis could be difficult because the various clinical symptoms have appeared in childhood. Therefore, the patients could be tended to visit many clinical departments and have delayed diagnosis.[7]
Heterozygous germline mutations of PTCH1 were identified as a responsible gene of BCNS in 1996.[3] PTCH1 is a member of the patched gene family and is the receptor for the sonic hedgehog. Moreover, germline mutations of SUFU that could cause BCNS were identified in 2014.[4] This report showed that the risk of medulloblastoma in BCNS was <2% in PTCH1 mutation-positive individuals, with a risk of up to twenty times higher in SUFU mutation-positive individuals. In addition, BCNS patients often have sporadic genetic mutations, even though BCNS is an autosomal dominant disorder.[7] In this case, by genetic counseling, the sporadic occurrence was probably indicated.
Several ovarian tumors with BCNS have been reported, and ovarian fibromas are the most common. Moreover, they are incidentally found by ultrasonography or at the cesarean section or in case of torsion of the ovary. No case of malignant transformation or no other gynecologic malignancy was reported.[8] On the other hand, a rare ovarian tumor, such as a sclerosing stromal tumor, was described.[9] Ovarian fibroma of BCNS is often bilateral (75%), and calcified in the nodular subtype, which could be distinct from other isolated ones.[7] In this case, severe calcification of unilateral ovarian fibromas was observed. Because the ovarian fibromas are extremely rigid, Luer Bone Rongeurs, Smart retractor®, or Free access® were quite useful for the removal of tumors. After setting Smart retractor® [Figure 2b] covered with Free access® [Figure 2c] after minilaparotomy, we can change over easily the laparoscopic treatment under pneumoperitoneum and the direct approach into the abdominal cavity. Therefore, when the calcification of the tumors is preoperatively suspected, we should prepare these instruments to remove the fibrous tissues.
The fundamental treatment for BCNS does not exist. The progression of BCCS may be fatal for the patient of BCNS. Surgical resection and anticancer drug administration have been generally performed for BCCS. As they tend to occur mainly in elderly patients, the treatment for BCCS could be crucial for the management of BCNS.
Early diagnosis of BCNS is important for two reasons. First, BCNS is a carcinogenic disease. There is a possibility that various tumors will develop age dependently. For the prevention of BCCS, BCNS patients should avoid ultraviolet irradiation. Second, the precise diagnosis can avoid unnecessary examinations.
CONCLUSION
We treated a patient with the calcified ovarian fibromas associated with BCNS. This case showed that laparoscopic-assisted surgery could be performed using several suitable materials. When treating young women with BCNS, we should take notice of the existence of the ovarian tumor. Further investigations would be required for the patient with BCNS to prevent multiple tumorigeneses.
Ethical review
The Institutional Review Boards of Tottori University Faculty of Medicine approved this project (Approval no. 19A198).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We appreciated Dr. Shinya Fujii (Department of Radiology, Tottori University Faculty of Medicine, Yonago, Japan) to give us the advice.
REFERENCES
- 1.Shanley S, Ratcliffe J, Hockey A, Haan E, Oley C, Ravine D, et al. Nevoid basal cell carcinoma syndrome: Review of 118 affected individuals. Am J Med Genet. 1994;50:282–90. doi: 10.1002/ajmg.1320500312. [DOI] [PubMed] [Google Scholar]
- 2.Farndon PA, Del Mastro RG, Evans DG, Kilpatrick MW. Location of gene for gorlin syndrome. Lancet. 1992;339:581–2. doi: 10.1016/0140-6736(92)90868-4. [DOI] [PubMed] [Google Scholar]
- 3.Hahn H, Wicking C, Zaphiropoulous PG, Gailani MR, Shanley S, Chidambaram A, et al. Mutations of the human homolog of drosophila patched in the nevoid basal cell carcinoma syndrome. Cell. 1996;85:841–51. doi: 10.1016/s0092-8674(00)81268-4. [DOI] [PubMed] [Google Scholar]
- 4.Smith MJ, Beetz C, Williams SG, Bhaskar SS, Bhaskar SS, O'Sullivan J, et al. Germline mutations in sufu cause gorlin syndrome-associated childhood medulloblastoma and redefine the risk associated with PTCH1 mutations. J Clin Oncol. 2014;32:4155–61. doi: 10.1200/JCO.2014.58.2569. [DOI] [PubMed] [Google Scholar]
- 5.Kimonis VE, Goldstein AM, Pastakia B, Yang ML, Kase R, DiGiovanna JJ, et al. Clinical manifestations in 105 persons with nevoid basal cell carcinoma syndrome. Am J Med Genet. 1997;69:299–308. [PubMed] [Google Scholar]
- 6.Gorlin RJ, Goltz RW. Multiple nevoid basal-cell epithelioma, jaw cysts and bifid rib.A syndrome. N Engl J Med. 1960;262:908–12. doi: 10.1056/NEJM196005052621803. [DOI] [PubMed] [Google Scholar]
- 7.Gorlin RJ. Nevoid basal cell carcinoma (Gorlin) syndrome. Genet Med. 2004;6:530–9. doi: 10.1097/01.gim.0000144188.15902.c4. [DOI] [PubMed] [Google Scholar]
- 8.Evans DG, Ladusans EJ, Rimmer S, Burnell LD, Thakker N, Farndon PA. Complications of the nevoid basal cell carcinoma syndrome: Results of a population based study. J Med Genet. 1993;30:460–4. doi: 10.1136/jmg.30.6.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grechi G, Clemente N, Tozzi A, Ciavattini A. Laparoscopic treatment of sclerosing stromal tumor of the ovary in a woman with Gorlin-Goltz syndrome: A case report and review of the literature. J. Minim Invasive Gynecol. 2015;22:892–5. doi: 10.1016/j.jmig.2015.03.002. [DOI] [PubMed] [Google Scholar]


