Abstract
Unipolar depressive disorder (UDD) affects more than 264 million people worldwide and was projected well before the severe acute respiratory syndrome coronavirus 2 pandemic to be the leading cause of disability-adjusted life years lost in 2030. It is imperative for leading economies to implement preventive strategies targeted towards UDD, given consistent policies are currently lacking. Recently established similarities between the aetiological hypotheses of depression and cardiometabolic diseases are shifting paradigms within this field. It is believed that dietary practices could potentially reduce the incidence of depression; similar to their effects on metabolism. Thus, the aim of this review was to compile current evidence on healthy dietary patterns as suitable contributors towards primary prevention strategies against UDD. Most of the well-known biological mechanisms behind depression have been positively associated with healthful diets and dietary patterns to varying degrees. Interestingly, a common factor of UDD is the production and overall effects of inflammatory cytokines, such as interleukin-6, tumor necrosis factor-α, and C-reactive protein. These compounds have been associated with depressive symptoms, disturbances in neuroendocrine function, leaky gut, monoamine activity and brain function, while also being key factors in the development of cardiometabolic diseases. The Mediterranean diet (MD) in particular, is well supported by first-level evidence regarding its preventive qualities against metabolic and cardiovascular diseases and thus considered a model for healthy eating by various organizations. In one of the few clinical trials investigating these associations, the PREDIMED trial, individuals with diabetes assigned to a MD supplemented with mixed tree nuts experienced a 41% relative risk reduction for developing depression. Lastly, there is a need to include health related quality of life as an indicator of physical and mental well-being, considering its putative associations with depression and suicide risk. Going forward, focusing on clinical trials, using precise nutritional assessments, and identifying nutritional biomarkers which may be related to depression are needed to fully support the implementation of dietary recommendations in the field of psychiatry.
Keywords: Depression, Nutrition, Mediterranean, Quality of life, Primary prevention, Epidemiology
Core Tip: Parallel biological mechanisms are being uncovered that link both depression and cardiometabolic diseases. Based on this evidence, it has been theorized that a healthful diet could improve the prognosis and prevent depression incidence, similar to its effects on cardiovascular risk. Current epidemiological studies support the link between healthy diets and better symptom management, biomarkers, and health related quality of life related to depression. However, additional longitudinal studies and dedicated clinical trials are needed to fully understand these initial findings. With greater evidence, healthy dietary patterns, such as the Mediterranean diet, could facilitate the management and reduce the risk of depression.
INTRODUCTION
More than 264 million people suffer from unipolar depressive disorder (UDD) worldwide, making it a leading cause of years of life lost as a result of disability[1]. In 2019, unipolar depressive disorder was ranked in 6th place amongst the top causes of burden of disease for the age groups between 25-49 years[2]. Previous projections had already speculated that depressive disorders would be the leading cause of disability-adjusted life years lost by the year 2030[3]. These estimations will inevitably rise as a result of the COVID-19 pandemic, requiring the implementation of public health policies to contain this expansive global health issue[4].
Current efforts to prevent mental illness, including depression focus on early diagnosis with prompt medical attention and treatment, in addition to sufficient drug availability[5]; in other words, secondary prevention. Despite moderate success in some countries, current research is offering both a better understanding of this condition and the rationale to apply new preventive strategies based on this knowledge. Examples of such research have been carried out by Sanchez-Villegas et al[6,7] in a population of southern Europeans. In this study sample, poor dietary and sedentary behaviors were associated with a higher incidence of mental illnesses (including UDD), which are also determinants typically associated with cardiometabolic health[8]. Due to common biological pathways, nutritional epidemiology now offers further insights in the field of mental illnesses[9].
Regardless of promising reports which support the possibility of improving mental health through nutrition, evidence remains limited[10]. Some of the findings refer to the importance of maternal and early-life nutrition for prevention, but also the role of diet as a determinant of adequate symptom management and enhanced anti-depressant drug efficacy. Such findings have led to an exponential growth and interest in the prevention of UDD through primary prevention strategies[11-13]. Nonetheless, the implementation of such strategies requires solid, reproducible evidence which can only be obtained from nutritional intervention trials.
In this narrative review we summarize the available evidence on the biological mechanisms common to UDD and cardiometabolic diseases, in support of the implementation of dietary interventions as plausible preventive measures for these diseases. For this purpose, we provide an overview of the aetiological hypotheses of depression with a particular interest in the role of diet on these pathways. Finally, current epidemiological evidence on the best known healthful dietary pattern, the Mediterranean diet (MD), will be presented in support of dietary interventions to reduce depression incidence and aid overall prognosis.
AETIOLOGICAL HYPOTHESES OF DEPRESSION
A wide array of determinants are involved in the aetiology of depression, including biological, psychological, and environmental factors[5]. It is not unlikely that these mechanisms coexist in varying degrees with plausible synergistic activity; adding complexity and variability to the causes and clinical manifestation of UDD. Among the most accepted pathways is the dysregulation of hormonal signaling involving the Hypothalamus-Pituitary-Adrenal (HPA) axis, although monoamine activity, neurogenesis, neuronal activity and plasticity play fundamental roles in the aetiology of mental illnesses in general. Of note, oxidative stress and inflammation play a common role in most of these hypotheses[14].
Oxidative stress and pro-inflammatory state
Most of the associated biological mechanisms in depressive disorders are accompanied by the production and release of cytokines, such as interleukin (IL)-1b, IL-2, IL-6, interferon-γ (INT-γ) and tumor necrosis factor (TNF)-α. These disturbances have been confirmed in patients with UDD, among whom plasma levels of certain pro-inflammatory cytokines (TNF-α, IL-6, IL-8, and C-reactive protein among others) are significantly higher than those of healthy individuals[15-17]. Furthermore, effective pharmacological treatment decrease cytokine concentrations, particularly IL-6, C-reactive protein and INT-γ[17,18]. The basis for this aetiological hypothesis is the damage to the blood brain barrier (BBB) caused by the convergence of oxidative stress and pro-inflammatory signals, which impede an adequate brain function[19]. These alterations are particularly noticeable in the BBB tight junction protein, claudin 5 (Cldn5), increasing cytokine permeability to the brain of mice[19,20]. Additionally, altered BBB function promotes the infiltration of various immune cells into the brain, endothelial damage through hdac1 expression, and direct damage to astrocytes, glial cells, and neurons[5,21,22]. Further release of peripheral cytokines originate in tissues such as the adipose tissue and gastrointestinal tract, resulting in vagal nerve stimulation, which also reinforces this pro-inflammatory state[19,23]. Each of these signals converge in the central nervous system (CNS) and result in altered receptor expression, neurogenesis and plasticity[5,19].
Given these connections, inflammatory cytokines have been proposed as biomarkers for depression in association with cardiovascular disease. These markers span various biological levels, including single-nucleotide polymorphisms identified in genome wide analyses, but also molecules such as the neutrophil gelatinase associated lipocalin[24]. Of particular interest are the associations found between the loci coding for the pro-inflammatory cytokine IL-6 and antidepressant responsiveness[25]. Oxidative stress and inflammation are also directly correlated to indoleamine 2,3-dioxygenase (a rate limiting enzyme in the metabolism of tryptophan), which leads to neurotoxicity and serotonin deficiency in the brain; both core features of the pathophysiology of depression[26].
These results are of great interest as UDD can be thought of as an inflammation-based disease, but also indicate potential anti-oxidant properties exerted by anti-depressant drug therapies. Overall, these findings offer new preventive strategies to the field of mood disorders. Regarding the robustness of these findings, a 2015 cumulative meta-analysis analyzing 58 studies evidenced that the role of the most commonly associated inflammatory cytokines on UDD was substantial[16]. Additionally, these results explain the diversity of clinical manifestations and responsiveness to treatment as a result of the interplay between biological pathways and individual factors. In this regard, we cannot disregard the potential effect of confounding as a plausible explanation for these differences, given the lack of clinical trials controlling for the numerous determinants of UDD.
Hypothalamus-pituitary-adrenal axis
Well-defined clinical and biochemical evidence support the role of glucocorticoid dysregulation as a cause of depression. The release of cortisol is the end product of the HPA-axis in response to external stress[5]. Moreover, circulating cortisol levels activate the sympathetic nervous system, and other immune responses that influence neuronal activity. Despite this being a natural response, disparities have been found in both animal and human models revealing individualized responses to external stressors, and thus differences in UDD risk[27]. With regard to this hypothesis of UDD, sustained induced stress will lead to the down regulation of glucocorticoid receptors in the CNS. Normally, cortisol inhibits the further release of corticotropin-releasing hormone and adrenocorticotrophic hormone in a self-regulating cycle. However, this negative feedback is altered in patients with depression, leading to sustained elevated levels of cortisol, alterations of the cortisol circadian rhythm, as well as altered immunological responses[28]. Some of the long-term effects of these disturbances include not only a reduction in the total hippocampal volume and reduced rates of neurogenesis, but also an accumulation of visceral fat and obesity, a higher susceptibility to insulin resistance, and an increase in the production of inflammatory cytokines, which lead to cardiometabolic diseases[29].
To our knowledge a direct influence of dietary habits on the HPA-axis has not been reported, however some authors suggest that the gut-microbiome could mediate these effects[30]. Clinical and biochemical evidence has concluded that alterations in the diversity and particular strains of bacteria comprising the microbiome, also known as dysbiosis, modulate the negative effects of stress on the HPA axis at different stages of life[31]. A particular study on marital-related stress reported an increased release of lipopolysaccharides (LPS) originating in the gut microbiome, as a result of dysbiosis, with a dose-response relationship[32]. LPSs cause damage to the gut-membrane and lead to major adverse cardiovascular events as demonstrated by Pastori et al[33] in 2017. Moreover, damage to the gut membrane results in the translocation of LPSs into the plasma, where they stimulate the differentiation of T-cell lymphocytes, further promoting inflammatory mechanisms[33,34]. Although the objective of the study was to assess the associations between circulating LPS and major adverse cardiovascular events, similar biological mechanisms have been identified in patients with depression[35]. Given the lack of clinical trials in this particular matter, incident depression has been inconsistently associated with cytokines such as LPS and others[35]. Hence, the true nature of this relationship has yet to be explained.
Dietary determinants of dysbiosis include fiber, fatty acid, and probiotic intakes[30,36,37]. In fact, dietary interventions have demonstrated that changes in the microbiome are possibly due to these food items, however incident depression has not been assessed concomitantly[38,39]. Results in a Korean study evaluating dietary fiber and prevalent depression demonstrated significant inverse associations between cereal, seaweed and mushroom fiber, and depressive symptoms[40]. Despite these encouraging findings, significant associations with prevalent depression were only found for the consumption of seaweed fiber (multivariable-adjusted OR 0.45 (95%CI: 0.23-0.88) for the comparison of quartile 4 vs quartile 1 of intake)[40]. Additionally, microbiome changes are highly dependent of the pre-existing diversity of bacteria in the gut. As stated by others, the microbiome demonstrates a resilience to change which is not yet fully understood[41]. Hence, additional research is needed before general recommendations can be made.
Monoamines
Another widely accepted aetiological theory of depression focuses on the role of monoamine synthesis and activity. Indeed, lower concentrations of these monoamines (serotonin, dopamine and noradrenaline) have long been associated with depressive symptoms and ultimately with depressive disorder. Altered monoamine activity is driven by inadequate production and their rapid degradation in the pre-synaptic space[5]. However, some inconsistencies remain unanswered regarding this hypothesis. Primarily, the prolonged response time observed for typical antidepressants which reduce depressive symptoms weeks after initiating treatment despite a normalization of monoamine levels in just a few hours[42,43].
Monoamine production is primarily dependent of vitamin B-6, folate, and vitamin B-12 Levels as precursors[44]. These micronutrients are essential in the metabolism of S-adenosyl methionine and methionine, both of which are critical for monoamine production and other methylation processes within the brain[44]. Sub-optimal levels of folate and B-group vitamins have been associated with higher homocysteine concentrations, which in turn are associated with depressive disorders, Alzheimer’s disease, and altered cognitive disfunction[45]. The role of homocysteine in the hypothesized biological mechanisms of UDD is based on the direct vascular damage and excitotoxicity exerted by its metabolites (homocysteinic acid or cysteine sulfinic acid).
Specific examples of the effects of individual foods on monoamines are scarce, however increased serum levels of dopamine and serotonin have been documented in response to dietary restrictions or supplementation with cocoa extracts[46,47]. Monoamine activity is also dependent on its enzymatic degradation by the monoamine oxidase enzyme (MAO) in the pre-synaptic space; a staple target for anti-depressant drug therapy. In particular, the MAO-B variant of this enzyme is susceptible to dietary interventions as demonstrated by Zellner et al[45]. This study demonstrated that an increase in vitamin B12 was correlated with a lower MAO-B expression (median expression reduction of 26%, adjusted P value < 0.05). In this three-week dietary intervention, a significant reduction of MAO-B was achieved through a high protein diet (approximately 3.0 g of protein/kg per day) primarily consisting of meat products (55% of total protein intake). Based on these observations, B-group vitamin supplements are theorized to have an antidepressant activity as noted in some in vitro and in vivo studies[48,49]. B-group vitamins are crucial for the transformation of homocysteine into methionine through the 5-methyltetrahydrofolate pathway[44], however vitamin B12 supplementation has not been uniformly associated with reduced UDD risk nor symptom improvements. Some clinical trials have noted elevated concentrations of homocysteine and low levels of B-group vitamins in depressed patients at baseline[50-52]. However, two interventions with B-vitamin supplements (the shortest consisting of two years, in a sample of n = 2919 geriatric patients with major depressive disorder) observed non-significant improvements in depressive symptoms[51,53]. Positive reports have been found under particular conditions, yet strong and reproducible evidence is warranted for the widespread use of vitamin B12 supplements as an inexpensive aid to pharmacological treatments[47,54]. Furthermore, a comparative analysis on the effect of folates and B-group vitamins should be conducted controlling for homocysteine reduction and increased monoamine activity through MAO-B suppression. Lastly, when considering the effects of dietary interventions on depressive symptoms, the overall antioxidant properties of a healthy dietary intervention should be considered.
Neurotrophism and neuronal activity
Although few reports exist on the effects of neurogenesis in the development of UDD, initial studies highlight the central role of the brain derived neurotrophic factor (BDNF). BDNF is synthetized and secreted primarily by endothelial cells[55] and is necessary for neuronal development as demonstrated in animal models[56]. The initial transcription and translation of the BDNF gene produces an immature molecule (prepro-BDNF) which is then converted into pro-BDNF and eventually transformed into mature BDNF through a series of protease enzymes[57,58]. Although prepro-BDNF has not been attributed biological activity, pro-BDNF can bind to the p75 neurotrophin receptor (p75NTR) and induce cell senescence in the hippocampus and prefrontal cortex[57-59]. Mature BDNF, on the other hand, has been related to the maturation of neurons, establishment of synaptic connections (through axonal growth and neuronal survival), and interestingly neural plasticity[56,57,60]. Such mechanisms, however, are highly dependent on the site of the brain in which they occur[59]. BDNF secreted into the amygdala and nucleus accumbens has been found to worsen depressive symptoms, whereas the opposite is true in the prefrontal cortex and hippocampus, both in human and animal models[57,58]. The site-specific activity of BDNF was initially thought to be the cause of reduced hippocampal volume, as described in post mortem studies in patients with depression[59,60]. These findings have since been attributed to a single nucleotide polymorphism resulting in the translation of Methionine and not Valine-66 (Val66Met), which hinders the transformation of proBDNF to BDNF[59]. However, the lower hippocampal volume hypothesis has been thoroughly criticized in a recent meta-analysis which highlights the low statistical power of the available evidence, plausible publication bias, and tendency towards the null value of current evidence[61]. Post-mortem studies on patients with depression have also found lower BDNF levels, lower expression of the BDNF receptor (TrkB), and an increased expression of p75NTR in the hippocampus (particularly in suicide patients), all of which correlate to negative effects on depressive symptoms[60,62]. Finally, BDNF has also been suggested to be a mediator of certain antidepressant therapies, such as electroconvulsive therapy and anti-depressant drugs[56,58]. In the particular case of fluoxetine, mice with the knock-in Val66Met variant were completely void from the antidepressant effects of the drug[58]. A major debate in regard to antidepressants has been their delayed effects, leading some researcher to believe that BDNF activity is responsible[58]. This theory is based on the effects of antidepressants on BDNF levels, which stimulate neuronal plasticity and improve neuronal synapse in the hippocampus after a period of time; corresponding with the cessation of depressive symptoms[56].
In relation to diet, post mortem studies report lower levels of retinoic acid receptor-α (RARα) in the prefrontal cortex along with disturbances in the TrkB pathway[62]. Qi et al[62] found that retinoic acid and vitamin A sub-species, could stimulate the TrkB promoter in an in vitro study and potentially improve depression management. Similar to BDNF, vitamin B12 has shown to selectively promote the expression of the BDNF-receptor gene (Ntrk-2) in the prefrontal cortex[48]. Despite observing no significant increase of these receptors in the hippocampus, an acute vitamin B12 supplementation counteracted the stress induced alterations of Ntrk-2 expression and depressive behavior in mice[48].
Given the novelty of these findings, few reports exist on the human effects of BDNF, and fewer which attribute its activity to dietary interventions. To our knowledge, only the PREDIMED (PREvención con DIeta MEDiterranea) trial has reported on the changes of BDNF as a result of a dietary intervention. In the PREDIMED trial, subjects allocated to the MD pattern and supplementation with nuts were less likely to have lower BDNF levels[63]. Moreover, after three years of intervention, a statistically significant increase in BDNF was observed among participants with prevalent depression and allocated to the MD supplemented with nuts. The results suggest that in patients with prevalent depression, BDNF concentrations are influenced by dietary interventions[63]. Despite the success observed in the dietary intervention of the PREDIMED trial, the complexities, regulatory mechanisms, and site-specific neuronal activity of this neurotrophin demand an in depth understanding of its implication in UDD.
Health related quality of life
One of the main reasons for UDD treatment is to improve patients’ health related quality of life (HRQoL), however, this goal has proven difficult to achieve and understand. The perception of health has been broadly studied under two main physical and mental domains since the 70’s[64]. In addition to overall health, external factors contribute greatly to this subjective concept. Bidirectional relationships between HRQoL and UDD have been reported, however, cause-effect relationships remain inconsistent. Some reports include reduced HRQoL at baseline for patients with UDD, in whom perceived health improves after anti-depressant treatment[65,66]. It should be mentioned that not all pharmaco-therapies improve well-being, possibly due to secondary effects or treatment related stress[66]. Hence the need for additional research. Moreover, if HRQoL does not improve, persistent perceived health reduction could worsen UDD and even increase suicide risk[5,67]. Various physical, mental and socioeconomic factors have been identified as determinants of increased suicide risk, all of which contribute varying effects[68]. In these matters, psychotherapy, particularly behavioral cognitive therapy, has proven to be an effective measure to improve HRQoL[69,70]. Unfortunately, these improvements have been limited to mental domains, which could indicate that additional factors are not being considered. On the other hand, diet has been cross-sectionally associated with both physical and mental domains of HRQoL[71-73]. Furthermore, nutrient deficiencies have been related to worsened perceived health, whereas healthy dietary habits seem to improve HRQoL across various age-groups[74,75]. Research in this particular field is scarce, but initial results are beginning to shed light on these associations. A report by Gariballa et al[76] in 2013 found that in addition to changes in homocysteine levels, a significant improvement in HRQoL was observed. The added value of improving HRQoL is not only an effective measure of patient health, but also of the quality of medical care. Clinical trials and prospective studies should focus on the potential mediator effect of nutritional status on the association between depression-related clinical outcomes and perceived health (UDD - Diet - HRQoL).
In the following table (Table 1) a summary of the primary aetiological hypothesis and mechanisms involved in depression are summarized. Furthermore, one-to-one associations and evidence of the potential effects of diet on each of these mechanisms is presented.
Table 1.
Summary of aetiological hypotheses and nutritional determinants of depression
|
Aetiological Hypotheses
|
Main mechanisms
|
Biological disturbances in UDD
|
Relationship with Diet
|
Ref.
|
| Oxidative stress and inflammation | Higher cytokine levels in patients with UDD induce BBB damage and increased permeability to the brain, mainly through claudin 5 dysfunction. Furthermore, oxidative stress and cytokines stimulate the vagal nerve, further promoting a pro-inflammatory in the CNS. | Increased IL-6, TNF-a, C-reactive protein, INT- γ, and other inflammatory cytokines. BBB damage and translocation of cytokines and immune cells into the brain. | Adequate antioxidant intake and lifestyle habits prevent the development of a pro-inflammatory state. | [16,17,19] |
| Glucocorticoids and HPA-axis | Chronic stress leads to the constant release of cortisol and eventually a down regulation of cortisol receptors in the hypothalamus. In addition, altered immune responses promote further neuronal damage and other metabolic diseases. | Increased basal cortisol and LPS. | Healthy gut microbiomes prevent the release of LPS and other cytokines into the plasma, limiting the potential damage of stress and theoretically decreasing UDD risk. | |
| Altered cortisol circadian rhythm. | ||||
| Secondarily, T-cell differentiation and release of inflammatory cytokines. | ||||
| Monoamine activity | Inadequate monoamine production and an increased degradation rate, mediated by the MAO enzyme, are related to depressive symptoms. Although current therapy is based on improving monoamine availability in the synapsis, uncertainties remain regarding this hypothesis. | Reduced monoamine formation and activity. | Vit-B12 and folate are necessary for monoamine production. | [28,29,33,34] |
| Homocysteine (also homocysteinic acid or cysteine sulfinic acid) has detrimental effects on neurons. | Homocysteine accumulation is a result of Vit-B12 deficiency. | |||
| MAO-B activity has been associated with Vit-B12 levels and dietary practices. | ||||
| Neuronal development and activity | Altered BDNF function is caused by oxidative stress and inadequate endothelial function. This neurotrophin is essential for neuronal development, synapse formation and cerebral plasticity, in addition to having anti-depressant effects. However, its antidepressant effects are dependent on brain region and therefore not fully understood | Altered BDNF activity and other markers of endothelial function (IL-6, TNF-a, ICAM-1 and VCAM-1). | Antioxidants, MUFA, and PUFA concentrations regulate endothelial function. | [44–46] |
| Decreased post-mortem hippocampal and prefrontal cortex volumes. | Vit-B12 promotes the expression of genes that code for BDNF-receptors (Ntrk-2). | |||
| The role of Health Related Quality of Life | Lower HRQoL has been associated with depression relapse and increased risk of suicide. | HRQoL is generally lower in patients with depression. Furthermore, pharmacotherapy improves mental components of HRQoL. | Quality of diet has been direct and cross-sectionally associated with HRQoL scores. The effects of diet on homocysteine level influence HRQoL and thus, potentially improve UDD patient status. | [55,57,62,63] |
UDD: Unipolar depressive disorder; IL-6: Interleukin 6; TNF-α: Tumoral necrosis factor-α; INT- γ: Interferon- γ; HPA-axis: Hypothalamus-pituitary-adrenal axis; LPS: Lipopolysaccharides; MAO: Monoamine oxidase; BDNF: Brain derived neurotrophic factor; ICAM: Intercellular adhesion molecule; VCAM: Vascular adhesion molecule; MUFA: Monounsaturated fatty acids; PUFA: Polyunsaturated fatty acids; HRQoL: Health related quality of life.
LINKS TO OTHER CARDIO-METABOLIC DISEASES
Along with UDD, cardiometabolic diseases are amongst the top causes of global burden of disease (GBD)[2]. Based on the mechanisms previously described, more and more evidence supports the role of diet and lifestyle as key determinants of mental health, quality of life, and cardiometabolic disorders[3]. Around the world, unbalanced diets, consumption of sugary beverages, and fast foods have been associated with and increased risk and presence of metabolic disturbances such as elevated fasting plasma glucose, and high blood pressure[77]. Sedentary behavior, a mayor cause of obesity and metabolic syndrome, has been associated with an increased risk for various mental disorders[7]. These observations further reflect the implications of (poor) lifestyle patterns habits on physical and mental health, both of which flourish under similar biological conditions. Likewise, the chronic pro-inflammatory state present in metabolic syndrome is the ideal scenario for glucose intolerance, lower insulin secretion, and the accompanying glucocorticoid dysregulation that precedes the onset of diabetes[78-81]. The cycle of damage persists once these changes have been established due to the detrimental effects of pro-inflammatory cytokines across various organs and systems, including pancreatic β-cells, endothelial cells, various strains of immune cells, among others. Unfortunately, advancements have been limited, however, biomarkers such as the myokine irisin are beginning to emerge as bridging biomarkers both in UDD and cardiometabolic diseases. This myokine, also produced in the adipose tissue, has been found to be a potent predictor of post-stroke depression in addition to solid associations with physical exercise and adiposity[82]. Considering these interactions, it is not outlandish to argue that the actual impact of depression has been underestimated, as prior researchers have suggested[83,84].
WHY A MD PATTERN FOR THE PREVENTION OF DEPRESSION?
The literature surrounding the MD and its characteristics is vast and well documented. When referring to the MD, researchers address a pattern of dietary characteristics and lifestyle found in countries of the Mediterranean basin, specifically in the 1960s[85]. In this geographical and temporal period, diets were characterized for their high consumption of olive oil (as primary source of dietary fats), nuts, fatty fish, local seasonal fruits and vegetables, in addition to a low consumption of meat (with a preference for poultry rather than red meats), dairy products, sugared beverages and confectionary/baked goods, and a moderate consumption of red wine. Furthermore, traditional culinary practices such as the “sofrito” (a tomato and olive oil-based sauce with various vegetables) enhance not only the flavors in this dietary pattern but also their innate nutrients. For the purpose of nutritional epidemiological studies, dietary questionnaires have been developed to assess the consumption of key foods and culinary techniques of this dietary pattern. Pioneering to this field was the development of the MD score (MDS) by A. Trichopoulou and collaborators, which considers the consumption of 9 key foods characteristics of the MD[86,87]. More recently, the 14-item questionnaire developed for the PREDIMED trial is the most wide-spread questionnaire evaluating the adherence to the MD pattern and its health benefits[88]. A novel, more precise approach is presently being developed with the inclusion of metabolomic assessment in order to objectively ascertain adherence to the MD. These analyses are based on the identification of key end-products of human metabolism that prevail when an individual adheres to this dietary pattern; also referred to as the “metabolic signature” of the Mediterranean diet[89].
The cardio-protective effects of the MD are mainly attributed to its anti-inflammatory and antioxidant properties. For this and other reasons, the American College of Cardiology and the American Heart Association amply recommend this dietary pattern in their 2019 guidelines[90], in addition to its inclusion in the Dietary Guidelines for Americans 2020-2025. All three institutions advocate for dietary patterns which emphasize the consumption of seafood, vegetables, fruits and nuts for the prevention of cardiovascular disease. However, in relation to UDD, the 2015 American dietary guidelines advisory committee deemed the evidence on the risk reduction of depression to be limited in its actual state[91]. When compared with other dietary patterns, the MD provides adequate concentrations of most micronutrients, particularly antioxidant compounds[92-94].
Based on these characteristics and reflecting on the biological hypotheses previously described, we could argue that the MD could also be beneficial for UDD prevention. Epidemiological studies have found that these compounds exert positive effects on endothelial function and inflammation based on biomarkers such as TGF-β1 and IL-6, ICAM-1 VCAM-1, among others[95]. As evidenced in the study by Sánchez-Villegas et al[63] in 2011 a dietary intervention with a MD supplemented with nuts in patients improved BDNF concentrations in patients with prevalent depression. Additional benefits to the endothelium of cardiovascular and neural cells originate from the adequate ratio of “healthy fats” in this dietary pattern [reflected in the mono- and polyunsaturated fat (MUFA/PUFA) and mono- and saturated fat (MUFA/SFA) ratios][96,97]. Among the most researched effects of fatty acids on membrane function surround the effects of Omega-3 fatty acids (also n-3). N-3 fatty acids include are polyunsaturated fatty acids (PUFA) that derive from alpha linolenic acid. The two primary forms of n-3 are eicosapentaenoic (EPA) acid and docosahexaenoic (DHA) acid, both of which are found in seafoods. EPA in particular plays a critical role in the adequate functioning of dendritic and synaptic membranes, hence its advised supplementation for patients with UDD[74,98]. In this line, DHA is an integral component of macular and dendritic cell membranes, further supporting its supplementation[6,99]. Consumption of fish and nuts in the MD has demonstrated to improve overall lipid composition (n-3 and other unsaturated fatty acids instead of trans-fatty acids or saturated fatty acids) which ensures adequate membrane functioning[6,98].
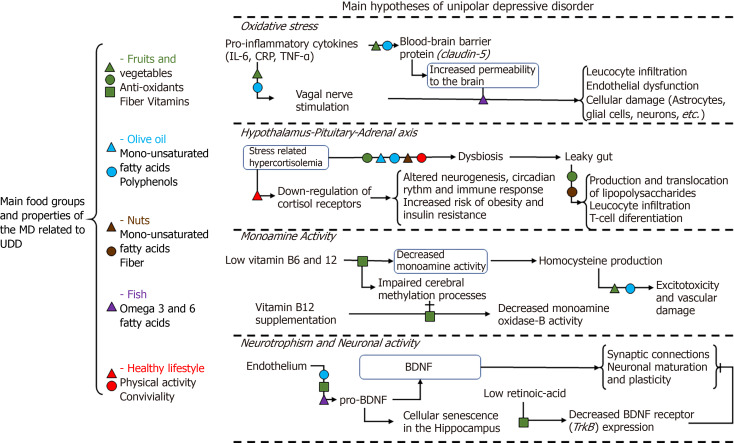
Folate and vitamin B12 intake are a major concern for subjects following plant-based diets. Nonetheless, nutrient deficiencies were scarce in a sample of free-roaming individuals adhering to the MD[93]. These micronutrients are critical for BDNF function but also necessary for an adequate production and activity of monoamines. Green leafy vegetables, legumes, grains, nuts and fruits within the MD have a high nutritional value for their folate and vitamin B12 content as well as other nutrients, such as fiber, vitamins, and minerals. Most of these foods are responsible for the positive effects of the MD on gut microbiome, further evidenced by improvements in insulin sensitivity and diabetes risk[100,101]. In this study, it was estimated that the prevalence of vitamin B12 deficiency among the 4th and 5th quintiles of adherence to the MD was 1%. Hence, the prevention of UDD by a MD pattern has been partially attributed to this dietary pattern’s adequate intake of vitamin B12[102]. This was further supported by a comparison between categories of MD adherence and UDD incidence risk; compared to the lowest adherence to the MDS, the top 4 categories were associated with a risk reduction for incident depression of 26%, 34%, 51% and 42%, respectively[8], observing a significant dose-response relationship[8,103]. Although subject to debate, caloric restriction has been demonstrated to play a role in UDD and aide in the progression of non-alcoholic fatty live disease[104]. Hunger-related stress induced anti-oxidant effects in the brain through increased blood flow and the removal of damaged cellular organelles. Interestingly, the hippocampus is particularly benefited from the increased perfusion, resulting in an increase in neurogenesis mediated by BDNF and a decrease in apoptosis rates[105,106]. However, this theory would imply that the release of glucocorticoids and the subsequent HPA-axis activation, as a result of stress, is also capable of promoting neurogenesis despite its impairment in patients with depression. In a meta-analysis, the mean weighted effects of a very low calorie diet on depressive symptom scores revealed a Hedges’ g = −0.728 (95%CI: −1.204, −0.253)[107]. These results were further analyzed in order to understand the mediator effects of exercise, duration of the caloric restriction, and cognitive behavioral therapy. It was concluded that exercise and longer duration of caloric restrictions partially explain the improvements in depressive symptoms, but more importantly, the exclusion of behavioral therapy yields no significant improvement of symptoms[107]. These mechanisms and the UDD hypotheses to which they are linked, have been summarized in Figure 1.
Figure 1.
Summary of interactions between the Mediterranean diet and the unipolar depressive disorder hypotheses. On the left side of the panel are the main food groups and their bioactive compounds, with known interactions with unipolar depressive disorder pathways. Each bioactive compound has a designated figure and color. The right side of the panel summarizes the aetiological hypotheses of depression and the main contributors to the disease. Black arrows designate the sequence of biological events in each mechanism, whereas “T” shaped lines designate an inhibitor effect. The figures designated for each compound are located within the sequence of biological events to designate the site of interaction with these mechanisms. See the main text for a detailed description of these interactions and associations. MD: Mediterranean diet; UDD: Unipolar depressive disorder; IL-6: Interleukin-6; CRP: C-reactive protein; TNF-α: Tumor necrosis factor-α; BDNF: Brain-derived neurotrophic factor.
These promising reports signal an under-developed field for UDD prevention, however, the long-term psychiatric effects that could arise from the severe acute respiratory syndrome coronavirus 2 pandemic demand for an exponential development of this knowledge. Front line workers should be considered at a double risk for COVID-19 and psychiatric disorders as suggested by the high prevalence of anxiety and burn-out in this group, with serious implications for the health and well-being of the population in general[108,109].
Some of the most noteworthy results from observational studies and clinical trials regarding the role of the MD, individual nutrients, and foods on incident depression are summarized on Table 2. This summary includes studies conducted in the Seguimiento Universidad de Navarra (The SUN study), studying the associations between diet and lifestyle with incident depression.
Table 2.
Summary of the effects of various nutrients, food groups, dietary patterns and lifestyle on prevalent or incident depression
| Dietary components | Total/number of cases | mean follow-up t (yr) | Main Results1 [comparisons between quantiles (q) or the designated categories] |
| Cohort studies | |||
| Nutrients | |||
| Omega-3 fatty acids[6] | 7903/512 | 2.4 | q4 vs q1: OR (95%CI) 0.65 (0.47–0.90). P for trend = 0.376 |
| Trans fatty acids[37] | 12059/657 | 6.1 | q5 vs q1: 1.42 (1.09-1.84); P for trend = 0.003 |
| MUFA[37] | 12059/657 | 6.1 | q5 vs q1: 0.80 (0.62-1.03); P for trend = 0.05 |
| PUFA[37] | 12059/657 | 6.1 | q5 vs q1; 0.76 (0.59-0.99; P for trend = 0.03 |
| Magnesium[123] | 12939/737 | 6.3 | q5 vs q1: 1.11 (0.77-1.59) No association. |
| Nutritional adequacy[124] | 13983/953 | 8.5 | ≥ 4 nutritional deficiencies vs ≤ 1: 1.37 (1.01-1.85) |
| Total Fiber[40] | 548/198 | Cross-sectional | q4 vs q1: OR = 0.54 (95%CI: 0.11–2.63); Non significant association |
| Foods and food groups | |||
| Fast food[125] | 8964/493 | 6.2 | q5 vs q1: 1.36 (1.02-1.81); P for trend = 0.03 |
| Ultra-processed foods[126] | 14907/774 | 10.3 | q4 vs q1: 1.33 (1.07, 1.64); P for trend = 0.004 |
| Baked goods[125] | 8964/493 | 6.2 | q2-5 vs q1: 1.38 (1.06-1.80); |
| Olive oil[37] | 12059/657 | 6.1 | q5 vs q1: 0.80 (0.62-1.04); P for trend = 0.06 |
| Seafoods[127] | 6587/1367 | Cross-sectional | q3 vs q1 of fatty fish consumption: OR 0.72 (0.59–0.88). Higher intakes were non-significant |
| Coffee[128] | 14413/199 | 10 | ≥ 4 cups/d vs < 1 cup/d: 0.37 (0.15–0.95); P for trend = 0.220 |
| Yoghurt[36] | 14542/727 | 9.3 | Low fat: max vs min: 1.32 (1.06–1.65); P for trend = 0.001 |
| Whole fat: max vs min: 0.78 (0.63–0.98); P for trend = 0.02 | |||
| Dietary patterns | |||
| MD score[8] | 10094/480 | 4.4 | 3pts vs 0-2pts: 0.74 (0.57-0.98) |
| 4pts vs 0-2pts: 0.66 (0.50-0.86) | |||
| 5pts vs 0-2pts: 0.49 (0.36-0.67) | |||
| 6-9pts vs 0-2pts: 0.58 (0.44-0.77); P for trend <0.001 | |||
| MD score (updated)[103] | 15093/1051 | 8.5 | q5 vs q1: 0.84 (0.69-1.02); P for trend = 0.001 |
| Pro-vegetarian[103] | 15093/1051 | 8.5 | q5 vs q1: 0.74 (0.61-0.89); P for trend < 0.001 |
| AHEI 2010[103] | 15093/1051 | 8.5 | q5 vs q1: 0.60 (0.49-0.72); P for trend < 0.001 |
| DASH-Fung diet[102] | 14051/410 | 8 | < 2pts vs 3-9pts: 0.76 (0.61-0.94): |
| Pro-inflammatory pattern[129] | 15093/1051 | 8.5 | q5 vs q1: 1.47 (1.17, 1.85); P for trend = 0.010 |
| Lifestyle | |||
| Mediterranean lifestyle[130] | 11800/806 | 8.5 | High vs low : 0.50 (0.32-0.81) |
| Healthy lifestyle score[131] | 14908/774 | 10.4 | Max vs min: 0.68 (0.49-0.95); P for trend 0.010 |
| Alcohol[132] | 13619/459 | 8 | Moderate vs no consumption: 0.62 (0.43-0.89) in female subjects |
| CV risk equation[133] | 16739/927 | 6 | q5 vs q1: 3.45 (2.40-4.95) starting at 40 yr |
| Physical activity[7] | 10381/923 | 6 | q5 vs q1: OR (95% CI) 0.81 (0.65-1.00) P for trend < 0.01 |
| Leisure time physical activity[134] | 6343/311 | 10.5 | > 20 METs-h/wk vs < 10 METs-h/wk; 0.84 (0.72–0.99); P for trend 0.046 |
| Tobacco[135] | 8556/190 | 4 | Smokers vs non-smokers: 1.30 (0.97-1.73) |
| Childhood obesity (5 yr)[136] | 11825/651 | 6.1 | Obese vs low weight: 1.50 (1.06-2.12); P for trend = 0.012 |
| Youth obesity (20 yr)[136] | 11825/651 | 6.1 | Obese vs low weight: 2.22 (1.20-4.08); P for trend = 0.005 |
| Clinical trials | |||
| The PREDIMED study[119] | 3923/224 | 5.4 | MD + EVOO2 or nut supplements vs Low fat diet: multivariable adjusted 0.85 (0.64 to 1.13); Non significant associations |
| The MoodFOOD Study[117] | 512/54 | 1 | Multi-nutrient supplement vs placebo groups: OR = 1.06 (0.87-1.29); Non significant associations. |
Estimates are presented as HR (95%CI) for incident depression unless stated otherwise.
Extra virgin olive oil. MUFA: Monounsaturated fatty acids; PUFA: Polyunsaturated fatty acids; MD: Mediterranean diet.
Epidemiological evidence supporting MD
In recent years epidemiological evidence on the benefits of the MD on UDD include several studies both within and outside the Mediterranean area. In the InChianti cohort study including 1362 participants aged 18-102 years, adherence to a dietary pattern rich in vegetables, olive oil, grains, fruit, fish and moderate in wine and red and processed meat, labelled as the 'typical Tuscan dietary pattern', was associated with a reduction in depressive symptoms over a 9-year follow-up period[99]. In the Greek center of the EPIC cohort, a total of 732 men and women 60 years or older were analyzed to determine the association between risk factors for cognitive function and depressive symptoms in the elderly. Adherence to the Mediterranean Diet, as well as olive oil consumption were associated with better scores in both outcomes[110]. Some non-Mediterranean reports include the study by Rienks et al[111]. In this study, the authors found that a Mediterranean-style diet was inversely associated with both prevalence (cross-sectional analysis) and incidence of depressive symptoms (longitudinal analysis) with an overall risk reduction of 17% among a sample of mid-aged women from the Australian Longitudinal Study on Women's Health. In the Chicago Health and Aging Project, MD adherence was associated with a reduced number of new depressive symptoms over 7.2 years of follow-up; 98.6% fewer symptoms among subjects in the highest tertile of adherence compared with those in the lowest[112].
So far, most of the evidence on diet and UDD derives from cross-sectional studies which could lead to false inferences of causal relationships. Furthermore, methodological analyses must address potential confounding, such as the adherence to a particular dietary pattern as a result of a recent diagnosis of chronic diseases or the co-occurrence of lifestyle-related and sociodemographic factors. These issues could be solved by carrying out large randomized trials with interventions based on changes in the overall food pattern. As of today, only small intervention trials have been carried out attempting to prove these and other hypotheses. The SMILES study was an intervention trial that promoted a healthy diet based on Australian and Greek dietary guidelines. In this trial, a dietary intervention with MD significantly improved depressive symptoms as an aid for standard acute depression treatment[113,114]. Focused on an elderly sample, the MedLey study aimed to determine the effect of an intervention with a Mediterranean dietary pattern on this population’s cognitive function, depressive symptoms, and quality of life. Despite significant improvements in endothelial function and MD adherence, the study showed no improvements in depressive symptoms nor quality of life after six months of intervention[115]. Examples of multi-country intervention trials include the MooDFOOD prevention trial which examined the feasibility and effectiveness of two different nutritional strategies (multi-nutrient supplementation and food-related behavioral change therapy) to prevent depression. The trial included individuals who were overweight, highly burdened with depressive symptoms, but did not meet clinical criteria for an episode of major depressive disorder in the last 6 mo[116]. In comparison to the placebo, micronutrient supplementation and behavioral therapy failed to prevent incident depression[117].In contrast to these results, the HELFIMED trial has shown promising results in patients with self-reported depression. In this trial, a MD intervention supplemented with fish oil for 6 mo significantly improved depressive symptoms and quality of life[118]. To this day, the PREDIMED study is the longest trial (mean follow-up of 5.4 years) evaluating the effects of a dietary intervention on the risk of incident cases of clinical depression. In this trial the relative risk (RR) estimates for an intervention with MD supplemented with extra-virgin olive oil (9% risk reduction) or a Mediterranean Diet supplemented with mixed tree nuts (22% risk reduction) suggested an inverse association. However, the confidence intervals for both estimates were wide and they showed that the results were compatible with a null result. Even when both Mediterranean diets were merged together and analyzed as a single group, the results were not statistically significant. Only when the analysis was limited to participants with type 2 diabetes (approximately 50% of the sample), a significantly reduced risk of depression was observed only for participants in the group with nut supplementation (significant risk reduction: 41%)[119].
Future research of great interest to this field includes the upcoming results from the PREDI-DEP trial, which was designed to study the impact of the MD on UDD. In this trial, patients over 18 years with a record of a major depressive episode, but with total or partial remission in the previous 6 mo, were recruited in four centers across Spain. With a target sample size of 250 participants per arm, subjects were randomly allocated to a MD intervention with supplemental olive oil, or to a control group who received no dietary advice nor supplements. Over the course of 24 mo participants were assessed every 3 mo to evaluate MD adherence (in the group of intervention) and every 4 mo to ascertain changes in depressive symptoms (in the overall sample)[120]. Food frequency questionnaires, HRQoL questionnaires (Short-Form 36), and physical activity questionnaires were administered in addition to blood sample collections, which were collected at baseline, and yearly during two years[121]. The upcoming results of this trial will aide in the endeavor to elucidate the mechanisms behind diet and UDD, in addition to discerning the particular effects of a MD diet supplemented with olive oil on the incidence and overall prognosis of patients at risk for this disease.
INITIAL DIETARY RECOMMENDATIONS FOR THE PREVENTION OF DEPRESSION
Although there are a number of important gaps in the scientific literature to date, existing evidence suggests that a combination of healthful dietary practices (including the adherence to the Mediterranean Diet) may reduce the risk of developing depression. In 2015, a group of experts with several backgrounds (epidemiology, psychiatry and nutrition) constructed the first Dietary Recommendations for the Prevention of Depression[122]. These dietary recommendations also provide additional and/or concurrent benefits for obesity, cardiovascular disease, diabetes and metabolic syndrome, and essentially pose no risk of harm. (1) “Follow ‘traditional’ Mediterranean Diet.”; (2) “Increase your consumption of fruits, vegetables, legumes, whole grain cereals, nuts and seeds.”; (3) “Include a high consumption of foods rich in omega-3 polyunsaturated fatty acids (PUFAs).”; (4) “Limit your intake of processed-foods, ‘fast’ foods, commercial bakery goods and sweets.”; and (5) “Replace unhealthy foods with wholesome nutritious foods.”[123]. Recommendations such as these are crucial steps towards a widespread implementation of diets as preventive measures for diseases, such as UDD, with substantial evidence of its benefits on cardiovascular and metabolic diseases.
CONCLUSION
UDD is and will remain a global health issue that researchers should strive to further understand and prevent. To this day, the hypothesized biological mechanisms that drive this disease include oxidative stress, HPA-axis dysregulation, monoamine and overall neuronal function deregulation. Based on analogous mechanisms, the MD could be a safe and inexpensive contributor to primary prevention strategies for depression, as it is characterized by various advantageous cardiovascular health qualities. Some of these properties include adequate B-group vitamin and folate content, promotion of a healthy gut microbiome, and high levels of various antioxidant compounds. Initial observational studies and trials, such as the PREDIMED study, suggest that implementing nutritional measures has an influence on disease risk and symptoms control. However, dedicated clinical trials are required to confirm the initial observations in order to fully support and understand the impact of diet on unipolar depressive disorder.
ACKNOWLEDGEMENTS
The group would like to acknowledge Ms. Maria Soledad Hershey, PhD candidate at the Department of Preventive Medicine and Public Health at the University of Navarre for providing the English language editing certificate and proofreading this manuscript.
Footnotes
Conflict-of-interest statement: The authors have no conflicts of interest to declare.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review started: February 27, 2021
First decision: June 5, 2021
Article in press: August 27, 2021
Specialty type: Psychiatry
Country/Territory of origin: Spain
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Socea B, Tu WJ S-Editor: Ma YJ L-Editor: A P-Editor: Yu HG
Contributor Information
Octavio Pano, Preventive Medicine and Public Health, University of Navarre, Pamplona 31008, Spain.
Elena H Martínez-Lapiscina, Department of Neurology Center of Neuroimmunology, Hospital Clinic of Barcelona, Institut d’Investigacions Biomèdiques August Pi Sunyer, Barcelona 08036, Spain.
Carmen Sayón-Orea, Department of Preventive Medicine and Public Health, University of Navarra, Pamplona 31008, Spain; IdiSNA, Navarra Institute for Health Research, Pamplona 31008, Spain; Department of Public Health, Navarra Institute of Public Health and Epidemiology, Pamplona 31003, Spain.
Miguel Angel Martinez-Gonzalez, Preventive Medicine and Public Health, University of Navarre, Pamplona 31008, Spain; CIBER Pathophysiology of Obesity and Nutrition, Institute of Health Carlos III, Madrid 28049, Spain; Department of Nutrition, Harvard T.H. Chan School of Public Health, Boston, MA 02115, United States.
Jose Alfredo Martinez, IdiSNA, Navarra Institute for Health Research, Pamplona 31008, Spain; CIBER Pathophysiology of Obesity and Nutrition, Institute of Health Carlos III, Madrid 28049, Spain; Department of Food Sciences and Physiology, University of Navarre, Pamplona 31008, Spain; Precision Nutrition and Cardiometabolic Health Program, IMDEA Food Institute, Madrid 28049, Spain.
Almudena Sanchez-Villegas, CIBER Pathophysiology of Obesity and Nutrition, Institute of Health Carlos III, Madrid 28049, Spain; Department of Clinical Sciences, University of Las Palmas Gran Canaria, Las Palmas Gran Canaria 35080, Spain. asanchez@dcc.ulpgc.es.
References
- 1.GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–1858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743–800. doi: 10.1016/S0140-6736(15)60692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Netw Open. 2020;3:e2019686. doi: 10.1001/jamanetworkopen.2020.19686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Otte C, Gold SM, Penninx BW, Pariante CM, Etkin A, Fava M, Mohr DC, Schatzberg AF. Major depressive disorder. Nat Rev Dis Primers. 2016;2:16065. doi: 10.1038/nrdp.2016.65. [DOI] [PubMed] [Google Scholar]
- 6.Sanchez-Villegas A, Henríquez P, Figueiras A, Ortuño F, Lahortiga F, Martínez-González MA. Long chain omega-3 fatty acids intake, fish consumption and mental disorders in the SUN cohort study. Eur J Nutr. 2007;46:337–346. doi: 10.1007/s00394-007-0671-x. [DOI] [PubMed] [Google Scholar]
- 7.Sanchez-Villegas A, Ara I, Guillén-Grima F, Bes-Rastrollo M, Varo-Cenarruzabeitia JJ, Martínez-González MA. Physical activity, sedentary index, and mental disorders in the SUN cohort study. Med Sci Sports Exerc. 2008;40:827–834. doi: 10.1249/MSS.0b013e31816348b9. [DOI] [PubMed] [Google Scholar]
- 8.Sánchez-Villegas A, Delgado-Rodríguez M, Alonso A, Schlatter J, Lahortiga F, Serra Majem L, Martínez-González MA. Association of the Mediterranean dietary pattern with the incidence of depression: the Seguimiento Universidad de Navarra/University of Navarra follow-up (SUN) cohort. Arch Gen Psychiatry. 2009;66:1090–1098. doi: 10.1001/archgenpsychiatry.2009.129. [DOI] [PubMed] [Google Scholar]
- 9.Sanchez-Villegas A, Martínez-González MA. Diet, a new target to prevent depression? BMC Med. 2013;11:3. doi: 10.1186/1741-7015-11-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sarris J, Logan AC, Akbaraly TN, Amminger GP, Balanzá-Martínez V, Freeman MP, Hibbeln J, Matsuoka Y, Mischoulon D, Mizoue T, Nanri A, Nishi D, Ramsey D, Rucklidge JJ, Sanchez-Villegas A, Scholey A, Su KP, Jacka FN International Society for Nutritional Psychiatry Research. Nutritional medicine as mainstream in psychiatry. Lancet Psychiatry. 2015;2:271–274. doi: 10.1016/S2215-0366(14)00051-0. [DOI] [PubMed] [Google Scholar]
- 11.Lai JS, Hiles S, Bisquera A, Hure AJ, McEvoy M, Attia J. A systematic review and meta-analysis of dietary patterns and depression in community-dwelling adults. Am J Clin Nutr. 2014;99:181–197. doi: 10.3945/ajcn.113.069880. [DOI] [PubMed] [Google Scholar]
- 12.Rahe C, Unrath M, Berger K. Dietary patterns and the risk of depression in adults: a systematic review of observational studies. Eur J Nutr. 2014;53:997–1013. doi: 10.1007/s00394-014-0652-9. [DOI] [PubMed] [Google Scholar]
- 13.Włodarczyk A, Cubała WJ, Stawicki M. Ketogenic diet for depression: A potential dietary regimen to maintain euthymia? Prog Neuropsychopharmacol Biol Psychiatry. 2021;109:110257. doi: 10.1016/j.pnpbp.2021.110257. [DOI] [PubMed] [Google Scholar]
- 14.Marx W, Lane M, Hockey M, Aslam H, Berk M, Walder K, Borsini A, Firth J, Pariante CM, Berding K, Cryan JF, Clarke G, Craig JM, Su KP, Mischoulon D, Gomez-Pinilla F, Foster JA, Cani PD, Thuret S, Staudacher HM, Sánchez-Villegas A, Arshad H, Akbaraly T, O'Neil A, Segasby T, Jacka FN. Diet and depression: exploring the biological mechanisms of action. Mol Psychiatry. 2021;26:134–150. doi: 10.1038/s41380-020-00925-x. [DOI] [PubMed] [Google Scholar]
- 15.Liu JJ, Wei YB, Strawbridge R, Bao Y, Chang S, Shi L, Que J, Gadad BS, Trivedi MH, Kelsoe JR, Lu L. Peripheral cytokine levels and response to antidepressant treatment in depression: a systematic review and meta-analysis. Mol Psychiatry. 2020;25:339–350. doi: 10.1038/s41380-019-0474-5. [DOI] [PubMed] [Google Scholar]
- 16.Haapakoski R, Mathieu J, Ebmeier KP, Alenius H, Kivimäki M. Cumulative meta-analysis of interleukins 6 and 1β, tumour necrosis factor α and C-reactive protein in patients with major depressive disorder. Brain Behav Immun. 2015;49:206–215. doi: 10.1016/j.bbi.2015.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Köhler CA, Freitas TH, Maes M, de Andrade NQ, Liu CS, Fernandes BS, Stubbs B, Solmi M, Veronese N, Herrmann N, Raison CL, Miller BJ, Lanctôt KL, Carvalho AF. Peripheral cytokine and chemokine alterations in depression: a meta-analysis of 82 studies. Acta Psychiatr Scand. 2017;135:373–387. doi: 10.1111/acps.12698. [DOI] [PubMed] [Google Scholar]
- 18.Dahl J, Ormstad H, Aass HC, Malt UF, Bendz LT, Sandvik L, Brundin L, Andreassen OA. The plasma levels of various cytokines are increased during ongoing depression and are reduced to normal levels after recovery. Psychoneuroendocrinology. 2014;45:77–86. doi: 10.1016/j.psyneuen.2014.03.019. [DOI] [PubMed] [Google Scholar]
- 19.Menard C, Pfau ML, Hodes GE, Kana V, Wang VX, Bouchard S, Takahashi A, Flanigan ME, Aleyasin H, LeClair KB, Janssen WG, Labonté B, Parise EM, Lorsch ZS, Golden SA, Heshmati M, Tamminga C, Turecki G, Campbell M, Fayad ZA, Tang CY, Merad M, Russo SJ. Social stress induces neurovascular pathology promoting depression. Nat Neurosci. 2017;20:1752–1760. doi: 10.1038/s41593-017-0010-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blamire AM, Anthony DC, Rajagopalan B, Sibson NR, Perry VH, Styles P. Interleukin-1beta -induced changes in blood-brain barrier permeability, apparent diffusion coefficient, and cerebral blood volume in the rat brain: a magnetic resonance study. J Neurosci. 2000;20:8153–8159. doi: 10.1523/JNEUROSCI.20-21-08153.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dudek KA, Dion-Albert L, Lebel M, LeClair K, Labrecque S, Tuck E, Ferrer Perez C, Golden SA, Tamminga C, Turecki G, Mechawar N, Russo SJ, Menard C. Molecular adaptations of the blood-brain barrier promote stress resilience vs. depression. Proc Natl Acad Sci U S A. 2020;117:3326–3336. doi: 10.1073/pnas.1914655117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cheng Y, Desse S, Martinez A, Worthen RJ, Jope RS, Beurel E. TNFα disrupts blood brain barrier integrity to maintain prolonged depressive-like behavior in mice. Brain Behav Immun. 2018;69:556–567. doi: 10.1016/j.bbi.2018.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee TH, Cheng KK, Hoo RL, Siu PM, Yau SY. The Novel Perspectives of Adipokines on Brain Health. Int J Mol Sci. 2019;20 doi: 10.3390/ijms20225638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gouweleeuw L, Naudé PJ, Rots M, DeJongste MJ, Eisel UL, Schoemaker RG. The role of neutrophil gelatinase associated lipocalin (NGAL) as biological constituent linking depression and cardiovascular disease. Brain Behav Immun. 2015;46:23–32. doi: 10.1016/j.bbi.2014.12.026. [DOI] [PubMed] [Google Scholar]
- 25.Uher R, Perroud N, Ng MY, Hauser J, Henigsberg N, Maier W, Mors O, Placentino A, Rietschel M, Souery D, Zagar T, Czerski PM, Jerman B, Larsen ER, Schulze TG, Zobel A, Cohen-Woods S, Pirlo K, Butler AW, Muglia P, Barnes MR, Lathrop M, Farmer A, Breen G, Aitchison KJ, Craig I, Lewis CM, McGuffin P. Genome-wide pharmacogenetics of antidepressant response in the GENDEP project. Am J Psychiatry. 2010;167:555–564. doi: 10.1176/appi.ajp.2009.09070932. [DOI] [PubMed] [Google Scholar]
- 26.Enko D, Zelzer S, Wenninger J, Holasek S, Schnedl WJ, Baranyi A, Herrmann M, Meinitzer A. Interleukin-6 is associated with tryptophan metabolism and signs of depression in individuals with carbohydrate malabsorption. EXCLI J. 2020;19:1414–1422. doi: 10.17179/excli2020-2940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ebner K, Singewald N. Individual differences in stress susceptibility and stress inhibitory mechanisms. Curr Opin Behav Sci . 2017;14:54–64. [Google Scholar]
- 28.Naughton M, Dinan TG, Scott LV. Corticotropin-releasing hormone and the hypothalamic-pituitary-adrenal axis in psychiatric disease. In: Handbook of Clinical Neurology. Elsevier B.V., 2014: 69–91. [DOI] [PubMed] [Google Scholar]
- 29.Martínez-González MA, Sánchez-Villegas A. Food patterns and the prevention of depression. Proc Nutr Soc. 2016;75:139–146. doi: 10.1017/S0029665116000045. [DOI] [PubMed] [Google Scholar]
- 30.Sun Y, Cheng L, Zeng X, Zhang X, Liu Y, Wu Z, Weng P. The intervention of unique plant polysaccharides - Dietary fiber on depression from the gut-brain axis. Int J Biol Macromol. 2021;170:336–342. doi: 10.1016/j.ijbiomac.2020.12.164. [DOI] [PubMed] [Google Scholar]
- 31.Robertson RC, Seira Oriach C, Murphy K, Moloney GM, Cryan JF, Dinan TG, Paul Ross R, Stanton C. Omega-3 polyunsaturated fatty acids critically regulate behaviour and gut microbiota development in adolescence and adulthood. Brain Behav Immun. 2017;59:21–37. doi: 10.1016/j.bbi.2016.07.145. [DOI] [PubMed] [Google Scholar]
- 32.Kiecolt-Glaser JK, Wilson SJ, Bailey ML, Andridge R, Peng J, Jaremka LM, Fagundes CP, Malarkey WB, Laskowski B, Belury MA. Marital distress, depression, and a leaky gut: Translocation of bacterial endotoxin as a pathway to inflammation. Psychoneuroendocrinology. 2018;98:52–60. doi: 10.1016/j.psyneuen.2018.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pastori D, Carnevale R, Nocella C, Novo M, Santulli M, Cammisotto V, Menichelli D, Pignatelli P, Violi F. Gut-Derived Serum Lipopolysaccharide is Associated With Enhanced Risk of Major Adverse Cardiovascular Events in Atrial Fibrillation: Effect of Adherence to Mediterranean Diet. J Am Heart Assoc. 2017;6 doi: 10.1161/JAHA.117.005784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Simkin DR. Microbiome and Mental Health, Specifically as It Relates to Adolescents. Curr Psychiatry Rep. 2019;21:93. doi: 10.1007/s11920-019-1075-3. [DOI] [PubMed] [Google Scholar]
- 35.Chocano-Bedoya PO, Mirzaei F, O'Reilly EJ, Lucas M, Okereke OI, Hu FB, Rimm EB, Ascherio A. C-reactive protein, interleukin-6, soluble tumor necrosis factor α receptor 2 and incident clinical depression. J Affect Disord. 2014;163:25–32. doi: 10.1016/j.jad.2014.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Perez-Cornago A, Sanchez-Villegas A, Bes-Rastrollo M, Gea A, Molero P, Lahortiga-Ramos F, Martínez-González MA. Intake of High-Fat Yogurt, but Not of Low-Fat Yogurt or Prebiotics, Is Related to Lower Risk of Depression in Women of the SUN Cohort Study. J Nutr. 2016;146:1731–1739. doi: 10.3945/jn.116.233858. [DOI] [PubMed] [Google Scholar]
- 37.Sánchez-Villegas A, Verberne L, De Irala J, Ruíz-Canela M, Toledo E, Serra-Majem L, Martínez-González MA. Dietary fat intake and the risk of depression: the SUN Project. PLoS One. 2011;6:e16268. doi: 10.1371/journal.pone.0016268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Menni C, Jackson MA, Pallister T, Steves CJ, Spector TD, Valdes AM. Gut microbiome diversity and high-fibre intake are related to lower long-term weight gain. Int J Obes (Lond) 2017;41:1099–1105. doi: 10.1038/ijo.2017.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Uemura M, Hayashi F, Ishioka K, Ihara K, Yasuda K, Okazaki K, Omata J, Suzutani T, Hirakawa Y, Chiang C, Aoyama A, Ohira T. Obesity and mental health improvement following nutritional education focusing on gut microbiota composition in Japanese women: a randomised controlled trial. Eur J Nutr. 2019;58:3291–3302. doi: 10.1007/s00394-018-1873-0. [DOI] [PubMed] [Google Scholar]
- 40.Kim CS, Byeon S, Shin DM. Sources of Dietary Fiber Are Differently Associated with Prevalence of Depression. Nutrients. 2020;12 doi: 10.3390/nu12092813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fragiadakis GK, Wastyk HC, Robinson JL, Sonnenburg ED, Sonnenburg JL, Gardner CD. Long-term dietary intervention reveals resilience of the gut microbiota despite changes in diet and weight. Am J Clin Nutr. 2020;111:1127–1136. doi: 10.1093/ajcn/nqaa046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hirschfeld RM. History and evolution of the monoamine hypothesis of depression. J Clin Psychiatry. 2000;61 Suppl 6:4–6. [PubMed] [Google Scholar]
- 43.Wang F, Yang J, Pan F, Bourgeois JA, Huang JH. Editorial: Early Life Stress and Depression. Front Psychiatry. 2019;10:964. doi: 10.3389/fpsyt.2019.00964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Froese DS, Fowler B, Baumgartner MR. Vitamin B12 , folate, and the methionine remethylation cycle-biochemistry, pathways, and regulation. J Inherit Metab Dis. 2019;42:673–685. doi: 10.1002/jimd.12009. [DOI] [PubMed] [Google Scholar]
- 45.Zellner M, Babeluk R, Jakobsen LH, Gerner C, Umlauf E, Volf I, Roth E, Kondrup J. A proteomics study reveals a predominant change in MaoB expression in platelets of healthy volunteers after high protein meat diet: relationship to the methylation cycle. J Neural Transm (Vienna) 2011;118:653–662. doi: 10.1007/s00702-011-0617-6. [DOI] [PubMed] [Google Scholar]
- 46.Perez-Cornago A, Ramírez MJ, Zulet MÁ, Martinez JA. Effect of dietary restriction on peripheral monoamines and anxiety symptoms in obese subjects with metabolic syndrome. Psychoneuroendocrinology. 2014;47:98–106. doi: 10.1016/j.psyneuen.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 47.Ibero-Baraibar I, Perez-Cornago A, Ramirez MJ, Martínez JA, Zulet MA. An Increase in Plasma Homovanillic Acid with Cocoa Extract Consumption Is Associated with the Alleviation of Depressive Symptoms in Overweight or Obese Adults on an Energy Restricted Diet in a Randomized Controlled Trial. J Nutr. 2015;146:897S–904S. doi: 10.3945/jn.115.222828. [DOI] [PubMed] [Google Scholar]
- 48.Trautmann C, Bock A, Urbach A, Hübner CA, Engmann O. Acute vitamin B12 supplementation evokes antidepressant response and alters Ntrk-2. Neuropharmacology. 2020;171:108112. doi: 10.1016/j.neuropharm.2020.108112. [DOI] [PubMed] [Google Scholar]
- 49.Skarupski KA, Tangney C, Li H, Ouyang B, Evans DA, Morris MC. Longitudinal association of vitamin B-6, folate, and vitamin B-12 with depressive symptoms among older adults over time. Am J Clin Nutr. 2010;92:330–335. doi: 10.3945/ajcn.2010.29413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lok A, Mocking RJ, Assies J, Koeter MW, Bockting CL, de Vries GJ, Visser I, Derks EM, Kayser M, Schene AH. The one-carbon-cycle and methylenetetrahydrofolate reductase (MTHFR) C677T polymorphism in recurrent major depressive disorder; influence of antidepressant use and depressive state? J Affect Disord. 2014;166:115–123. doi: 10.1016/j.jad.2014.04.048. [DOI] [PubMed] [Google Scholar]
- 51.Almeida OP, Ford AH, Hirani V, Singh V, vanBockxmeer FM, McCaul K, Flicker L. B vitamins to enhance treatment response to antidepressants in middle-aged and older adults: results from the B-VITAGE randomised, double-blind, placebo-controlled trial. Br J Psychiatry. 2014;205:450–457. doi: 10.1192/bjp.bp.114.145177. [DOI] [PubMed] [Google Scholar]
- 52.Kaner G, Soylu M, Yüksel N, Inanç N, Ongan D, Başmısırlı E. Evaluation of Nutritional Status of Patients with Depression. Biomed Res Int. 2015;2015:521481. doi: 10.1155/2015/521481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.de Koning EJ, van der Zwaluw NL, van Wijngaarden JP, Sohl E, Brouwer-Brolsma EM, van Marwijk HW, Enneman AW, Swart KM, van Dijk SC, Ham AC, van der Velde N, Uitterlinden AG, Penninx BW, Elders PJ, Lips P, Dhonukshe-Rutten RA, van Schoor NM, de Groot LC. Effects of Two-Year Vitamin B12 and Folic Acid Supplementation on Depressive Symptoms and Quality of Life in Older Adults with Elevated Homocysteine Concentrations: Additional Results from the B-PROOF Study, an RCT. Nutrients. 2016;8 doi: 10.3390/nu8110748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schefft C, Kilarski LL, Bschor T, Köhler S. Efficacy of adding nutritional supplements in unipolar depression: A systematic review and meta-analysis. Eur Neuropsychopharmacol. 2017;27:1090–1109. doi: 10.1016/j.euroneuro.2017.07.004. [DOI] [PubMed] [Google Scholar]
- 55.Guo S, Kim WJ, Lok J, Lee SR, Besancon E, Luo BH, Stins MF, Wang X, Dedhar S, Lo EH. Neuroprotection via matrix-trophic coupling between cerebral endothelial cells and neurons. Proc Natl Acad Sci U S A. 2008;105:7582–7587. doi: 10.1073/pnas.0801105105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Björkholm C, Monteggia LM. BDNF - a key transducer of antidepressant effects. Neuropharmacology. 2016;102:72–79. doi: 10.1016/j.neuropharm.2015.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Duman RS, Deyama S, Fogaça MV. Role of BDNF in the pathophysiology and treatment of depression: Activity-dependent effects distinguish rapid-acting antidepressants. Eur J Neurosci. 2021;53:126–139. doi: 10.1111/ejn.14630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Castrén E, Kojima M. Brain-derived neurotrophic factor in mood disorders and antidepressant treatments. Neurobiol Dis. 2017;97:119–126. doi: 10.1016/j.nbd.2016.07.010. [DOI] [PubMed] [Google Scholar]
- 59.Adachi N, Numakawa T, Richards M, Nakajima S, Kunugi H. New insight in expression, transport, and secretion of brain-derived neurotrophic factor: Implications in brain-related diseases. World J Biol Chem. 2014;5:409–428. doi: 10.4331/wjbc.v5.i4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Martinowich K, Manji H, Lu B. New insights into BDNF function in depression and anxiety. Nat Neurosci. 2007;10:1089–1093. doi: 10.1038/nn1971. [DOI] [PubMed] [Google Scholar]
- 61.Molendijk ML, Bus BA, Spinhoven P, Kaimatzoglou A, Oude Voshaar RC, Penninx BW, van IJzendoorn MH, Elzinga BM. A systematic review and meta-analysis on the association between BDNF val(66)met and hippocampal volume--a genuine effect or a winners curse? Am J Med Genet B Neuropsychiatr Genet. 2012;159B:731–740. doi: 10.1002/ajmg.b.32078. [DOI] [PubMed] [Google Scholar]
- 62.Qi XR, Zhao J, Liu J, Fang H, Swaab DF, Zhou JN. Abnormal retinoid and TrkB signaling in the prefrontal cortex in mood disorders. Cereb Cortex. 2015;25:75–83. doi: 10.1093/cercor/bht203. [DOI] [PubMed] [Google Scholar]
- 63.Sánchez-Villegas A, Galbete C, Martinez-González MA, Martinez JA, Razquin C, Salas-Salvadó J, Estruch R, Buil-Cosiales P, Martí A. The effect of the Mediterranean diet on plasma brain-derived neurotrophic factor (BDNF) levels: the PREDIMED-NAVARRA randomized trial. Nutr Neurosci. 2011;14:195–201. doi: 10.1179/1476830511Y.0000000011. [DOI] [PubMed] [Google Scholar]
- 64.Karimi M, Brazier J. Health, Health-Related Quality of Life, and Quality of Life: What is the Difference? Pharmacoeconomics. 2016;34:645–649. doi: 10.1007/s40273-016-0389-9. [DOI] [PubMed] [Google Scholar]
- 65.Köhler S, Unger T, Hoffmann S, Mackert A, Ross B, Fydrich T. The relationship of health-related quality of life and treatment outcome during inpatient treatment of depression. Qual Life Res. 2015;24:641–649. doi: 10.1007/s11136-014-0811-8. [DOI] [PubMed] [Google Scholar]
- 66.Hofmann SG, Curtiss J, Carpenter JK, Kind S. Effect of treatments for depression on quality of life: a meta-analysis. Cogn Behav Ther. 2017;46:265–286. doi: 10.1080/16506073.2017.1304445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Büsselmann M, Nigel S, Otte S, Lutz M, Franke I, Dudeck M, Streb J. High Quality of Life Reduces Depression, Hopelessness, and Suicide Ideations in Patients in Forensic Psychiatry. Front Psychiatry. 2019;10:1014. doi: 10.3389/fpsyt.2019.01014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.McClatchey K, Murray J, Rowat A, Chouliara Z. Risk Factors for Suicide and Suicidal Behavior Relevant to Emergency Health Care Settings: A Systematic Review of Post-2007 Reviews. Suicide Life Threat Behav. 2017;47:729–745. doi: 10.1111/sltb.12336. [DOI] [PubMed] [Google Scholar]
- 69.Kolovos S, Kleiboer A, Cuijpers P. Effect of psychotherapy for depression on quality of life: meta-analysis. Br J Psychiatry. 2016;209:460–468. doi: 10.1192/bjp.bp.115.175059. [DOI] [PubMed] [Google Scholar]
- 70.Chiang LC, Heitkemper MM, Chiang SL, Tzeng WC, Lee MS, Hung YJ, Lin CH. Motivational Counseling to Reduce Sedentary Behaviors and Depressive Symptoms and Improve Health-Related Quality of Life Among Women With Metabolic Syndrome. J Cardiovasc Nurs. 2019;34:327–335. doi: 10.1097/JCN.0000000000000573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pano O, Sayón-Orea C, Gea A, Bes-Rastrollo M, Martínez-González MÁ, Martínez JA. Nutritional Determinants of Quality of Life in a Mediterranean Cohort: The SUN Study. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17113897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.de Cuevillas B, Álvarez Álvarez I, Cuervo M, Fernández Montero A, Navas Carretero S, Martínez JA. Definition of nutritionally qualitative categorizing (proto)nutritypes and a pilot quantitative nutrimeter for mirroring nutritional well-being based on a quality of life health related questionnaire. Nutr Hosp. 2019;36:862–874. doi: 10.20960/nh.02532. [DOI] [PubMed] [Google Scholar]
- 73.Ruano C, Henríquez P, Ruiz-Canela M, Martínez-González MÁ, Bes-Rastrollo M, Sánchez-Villegas A. Commercial Bakery, Fast-Food, and Soft Drink Consumption and Quality of Life in the SUN Project. Food Nutr Sci. 2014;5:1299–1308. [Google Scholar]
- 74.Guligowska A, Pigłowska M, Fife E, Kostka J, Sołtysik BK, Kroc Ł, Kostka T. Inappropriate nutrients intake is associated with lower functional status and inferior quality of life in older adults with depression. Clin Interv Aging. 2016;11:1505–1517. doi: 10.2147/CIA.S114669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ferrer-Cascales R, Sánchez-SanSegundo M, Ruiz-Robledillo N, Albaladejo-Blázquez N, Laguna-Pérez A, Zaragoza-Martí A. Eat or Skip Breakfast? Int J Environ Res Public Health. 2018;15 doi: 10.3390/ijerph15081781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gariballa S. Extending the homocysteine-induced neurotransmitter deficiency and depression of mood hypothesis to quality of life in older patients. Int J Geriatr Psychiatry. 2013;28:878–879. doi: 10.1002/gps.3922. [DOI] [PubMed] [Google Scholar]
- 77.Popa AR, Vesa CM, Uivarosan D, Jurca CM, Isvoranu G, Socea B, Stanescu AMA, Iancu MA, Scarneciu I, Zaha DC. Cross sectional study regarding the association between sweetened beverages intake, fast-food products, body mass index, fasting blood glucose and blood pressure in the young adults from North-western Romania. Revista de Chimie. 2019;70:156–160. [Google Scholar]
- 78.Milaneschi Y, Simmons WK, van Rossum EFC, Penninx BW. Depression and obesity: evidence of shared biological mechanisms. Mol Psychiatry. 2019;24:18–33. doi: 10.1038/s41380-018-0017-5. [DOI] [PubMed] [Google Scholar]
- 79.Berge LI, Riise T. Comorbidity between Type 2 Diabetes and Depression in the Adult Population: Directions of the Association and Its Possible Pathophysiological Mechanisms. Int J Endocrinol. 2015;2015:164760. doi: 10.1155/2015/164760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Moulton CD, Pickup JC, Ismail K. The link between depression and diabetes: the search for shared mechanisms. Lancet Diabetes Endocrinol. 2015;3:461–471. doi: 10.1016/S2213-8587(15)00134-5. [DOI] [PubMed] [Google Scholar]
- 81.Pimenta AM, Lahortiga-Ramos F, Sayon-Orea C, Martínez-González MA, Sánchez-Villegas A. Depression and metabolic syndrome in participants of the "Seguimiento Universidad de Navarra" (SUN) cohort study. J Affect Disord. 2021;284:183–189. doi: 10.1016/j.jad.2021.02.002. [DOI] [PubMed] [Google Scholar]
- 82.Tu WJ, Qiu HC, Liu Q, Li X, Zhao JZ, Zeng X. Decreased level of irisin, a skeletal muscle cell-derived myokine, is associated with post-stroke depression in the ischemic stroke population. J Neuroinflammation. 2018;15:133. doi: 10.1186/s12974-018-1177-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370:851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 84.Dhar AK, Barton DA. Depression and the Link with Cardiovascular Disease. Front Psychiatry. 2016;7:33. doi: 10.3389/fpsyt.2016.00033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Martínez-González MÁ, Hershey MS, Zazpe I, Trichopoulou A. Transferability of the Mediterranean Diet to Non-Mediterranean Countries. What Is and What Is Not the Mediterranean Diet. Nutrients. 2017;9 doi: 10.3390/nu9111226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348:2599–2608. doi: 10.1056/NEJMoa025039. [DOI] [PubMed] [Google Scholar]
- 87.Trichopoulou A, Kouris-Blazos A, Wahlqvist ML, Gnardellis C, Lagiou P, Polychronopoulos E, Vassilakou T, Lipworth L, Trichopoulos D. Diet and overall survival in elderly people. BMJ. 1995;311:1457–1460. doi: 10.1136/bmj.311.7018.1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Schröder H, Fitó M, Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, Lamuela-Raventós R, Ros E, Salaverría I, Fiol M, Lapetra J, Vinyoles E, Gómez-Gracia E, Lahoz C, Serra-Majem L, Pintó X, Ruiz-Gutierrez V, Covas MI. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J Nutr. 2011;141:1140–1145. doi: 10.3945/jn.110.135566. [DOI] [PubMed] [Google Scholar]
- 89.Li J, Guasch-Ferré M, Chung W, Ruiz-Canela M, Toledo E, Corella D, Bhupathiraju SN, Tobias DK, Tabung FK, Hu J, Zhao T, Turman C, Feng YA, Clish CB, Mucci L, Eliassen AH, Costenbader KH, Karlson EW, Wolpin BM, Ascherio A, Rimm EB, Manson JE, Qi L, Martínez-González MÁ, Salas-Salvadó J, Hu FB, Liang L. The Mediterranean diet, plasma metabolome, and cardiovascular disease risk. Eur Heart J. 2020;41:2645–2656. doi: 10.1093/eurheartj/ehaa209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, Himmelfarb CD, Khera A, Lloyd-Jones D, McEvoy JW, Michos ED, Miedema MD, Muñoz D, Smith SC Jr, Virani SS, Williams KA Sr, Yeboah J, Ziaeian B. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;74:1376–1414. doi: 10.1016/j.jacc.2019.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Millen BE, Abrams S, Adams-Campbell L, Anderson CA, Brenna JT, Campbell WW, Clinton S, Hu F, Nelson M, Neuhouser ML, Perez-Escamilla R, Siega-Riz AM, Story M, Lichtenstein AH. The 2015 Dietary Guidelines Advisory Committee Scientific Report: Development and Major Conclusions. Adv Nutr. 2016;7:438–444. doi: 10.3945/an.116.012120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Trujillo-Mayol I, Guerra-Valle M, Casas-Forero N, Sobral MMC, Viegas O, Alarcón-Enos J, Ferreira IM, Pinho O. Western Dietary Pattern Antioxidant Intakes and Oxidative Stress: Importance During the SARS-CoV-2/COVID-19 Pandemic. Adv Nutr. 2021;12:670–681. doi: 10.1093/advances/nmaa171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Serra-Majem L, Bes-Rastrollo M, Román-Viñas B, Pfrimer K, Sánchez-Villegas A, Martínez-González MA. Dietary patterns and nutritional adequacy in a Mediterranean country. Br J Nutr. 2009;101 Suppl 2:S21–S28. doi: 10.1017/S0007114509990559. [DOI] [PubMed] [Google Scholar]
- 94.Peng W, Berry EM, Goldsmith R. Adherence to the Mediterranean diet was positively associated with micronutrient adequacy and negatively associated with dietary energy density among adolescents. J Hum Nutr Diet. 2019;32:41–52. doi: 10.1111/jhn.12602. [DOI] [PubMed] [Google Scholar]
- 95.Casas R, Sacanella E, Urpí-Sardà M, Chiva-Blanch G, Ros E, Martínez-González MA, Covas MI Rosa Ma Lamuela-Raventos, Salas-Salvadó J, Fiol M, Arós F, Estruch R. The effects of the mediterranean diet on biomarkers of vascular wall inflammation and plaque vulnerability in subjects with high risk for cardiovascular disease. A randomized trial. PLoS One. 2014;9:e100084. doi: 10.1371/journal.pone.0100084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ghobadi S, Hassanzadeh-Rostami Z, Mohammadian F, Nikfetrat A, Ghasemifard N, Raeisi Dehkordi H, Faghih S. Comparison of blood lipid-lowering effects of olive oil and other plant oils: A systematic review and meta-analysis of 27 randomized placebo-controlled clinical trials. Crit Rev Food Sci Nutr. 2019;59:2110–2124. doi: 10.1080/10408398.2018.1438349. [DOI] [PubMed] [Google Scholar]
- 97.Sayón-Orea C, Razquin C, Bulló M, Corella D, Fitó M, Romaguera D, Vioque J, Alonso-Gómez ÁM, Wärnberg J, Martínez JA, Serra-Majem L, Estruch R, Tinahones FJ, Lapetra J, Pintó X, Tur JA, López-Miranda J, Bueno-Cavanillas A, Delgado-Rodríguez M, Matía-Martín P, Daimiel L, Sánchez VM, Vidal J, Vázquez C, Ros E, Ruiz-Canela M, Sorlí JV, Castañer O, Fiol M, Navarrete-Muñoz EM, Arós F, Gómez-Gracia E, Zulet MA, Sánchez-Villegas A, Casas R, Bernal-López R, Santos-Lozano JM, Corbella E, Bouzas C, García-Arellano A, Basora J, Asensio EM, Schröder H, Moñino M, García de la Hera M, Tojal-Sierra L, Toledo E, Díaz-López A, Goday A, Salas-Salvadó J, Martínez-González MA. Effect of a Nutritional and Behavioral Intervention on Energy-Reduced Mediterranean Diet Adherence Among Patients With Metabolic Syndrome: Interim Analysis of the PREDIMED-Plus Randomized Clinical Trial. JAMA. 2019;322:1486–1499. doi: 10.1001/jama.2019.14630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Deacon G, Kettle C, Hayes D, Dennis C, Tucci J. Omega 3 polyunsaturated fatty acids and the treatment of depression. Crit Rev Food Sci Nutr. 2017;57:212–223. doi: 10.1080/10408398.2013.876959. [DOI] [PubMed] [Google Scholar]
- 99.Vermeulen E, Stronks K, Visser M, Brouwer IA, Schene AH, Mocking RJ, Colpo M, Bandinelli S, Ferrucci L, Nicolaou M. The association between dietary patterns derived by reduced rank regression and depressive symptoms over time: the Invecchiare in Chianti (InCHIANTI) study. Br J Nutr. 2016;115:2145–2153. doi: 10.1017/S0007114516001318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Nagpal R, Shively CA, Appt SA, Register TC, Michalson KT, Vitolins MZ, Yadav H. Gut Microbiome Composition in Non-human Primates Consuming a Western or Mediterranean Diet. Front Nutr. 2018;5:28. doi: 10.3389/fnut.2018.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Haro C, Montes-Borrego M, Rangel-Zúñiga OA, Alcalá-Díaz JF, Gómez-Delgado F, Pérez-Martínez P, Delgado-Lista J, Quintana-Navarro GM, Tinahones FJ, Landa BB, López-Miranda J, Camargo A, Pérez-Jiménez F. Two Healthy Diets Modulate Gut Microbial Community Improving Insulin Sensitivity in a Human Obese Population. J Clin Endocrinol Metab. 2016;101:233–242. doi: 10.1210/jc.2015-3351. [DOI] [PubMed] [Google Scholar]
- 102.Perez-Cornago A, Sanchez-Villegas A, Bes-Rastrollo M, Gea A, Molero P, Lahortiga-Ramos F, Martinez-Gonzalez MÁ. Relationship between adherence to Dietary Approaches to Stop Hypertension (DASH) diet indices and incidence of depression during up to 8 years of follow-up. Public Health Nutr. 2017;20:2383–2392. doi: 10.1017/S1368980016001531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Sánchez-Villegas A, Henríquez-Sánchez P, Ruiz-Canela M, Lahortiga F, Molero P, Toledo E, Martínez-González MA. A longitudinal analysis of diet quality scores and the risk of incident depression in the SUN Project. BMC Med. 2015;13:197. doi: 10.1186/s12916-015-0428-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Makovicky P, Tumova E, Volek Z, Makovicky P, Sedlacek R. Relationships between variable time, percentage of food restriction and liver histology: which alternative is the best for non-alcoholic fatty liver disease (NAFLD) prevention? Histol Histopathol. 2016;31:1123–1130. doi: 10.14670/HH-11-741. [DOI] [PubMed] [Google Scholar]
- 105.Moore MN. Autophagy as a second level protective process in conferring resistance to environmentally-induced oxidative stress. Autophagy. 2008;4:254–256. doi: 10.4161/auto.5528. [DOI] [PubMed] [Google Scholar]
- 106.Moore MN, Shaw JP, Ferrar Adams DR, Viarengo A. Anti-oxidative cellular protection effect of fasting-induced autophagy as a mechanism for hormesis. Mar Environ Res. 2015;107:35–44. doi: 10.1016/j.marenvres.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 107.Ein N, Armstrong B, Vickers K. The effect of a very low calorie diet on subjective depressive symptoms and anxiety: meta-analysis and systematic review. Int J Obes (Lond) 2019;43:1444–1455. doi: 10.1038/s41366-018-0245-4. [DOI] [PubMed] [Google Scholar]
- 108.Dimitriu MCT, Pantea-Stoian A, Smaranda AC, Nica AA, Carap AC, Constantin VD, Davitoiu AM, Cirstoveanu C, Bacalbasa N, Bratu OG, Jacota-Alexe F, Badiu CD, Smarandache CG, Socea B. Burnout syndrome in Romanian medical residents in time of the COVID-19 pandemic. Med Hypotheses. 2020;144:109972. doi: 10.1016/j.mehy.2020.109972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Cotel A, Golu F, Pantea Stoian A, Dimitriu M, Socea B, Cirstoveanu C, Davitoiu AM, Jacota Alexe F, Oprea B. Predictors of Burnout in Healthcare Workers during the COVID-19 Pandemic. Healthcare (Basel) 2021;9 doi: 10.3390/healthcare9030304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Psaltopoulou T, Kyrozis A, Stathopoulos P, Trichopoulos D, Vassilopoulos D, Trichopoulou A. Diet, physical activity and cognitive impairment among elders: the EPIC-Greece cohort (European Prospective Investigation into Cancer and Nutrition) Public Health Nutr. 2008;11:1054–1062. doi: 10.1017/S1368980007001607. [DOI] [PubMed] [Google Scholar]
- 111.Rienks J, Dobson AJ, Mishra GD. Mediterranean dietary pattern and prevalence and incidence of depressive symptoms in mid-aged women: results from a large community-based prospective study. Eur J Clin Nutr. 2013;67:75–82. doi: 10.1038/ejcn.2012.193. [DOI] [PubMed] [Google Scholar]
- 112.Skarupski KA, Tangney CC, Li H, Evans DA, Morris MC. Mediterranean diet and depressive symptoms among older adults over time. J Nutr Health Aging. 2013;17:441–445. doi: 10.1007/s12603-012-0437-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.O'Neil A, Berk M, Itsiopoulos C, Castle D, Opie R, Pizzinga J, Brazionis L, Hodge A, Mihalopoulos C, Chatterton ML, Dean OM, Jacka FN. A randomised, controlled trial of a dietary intervention for adults with major depression (the "SMILES" trial): study protocol. BMC Psychiatry. 2013;13:114. doi: 10.1186/1471-244X-13-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Jacka FN, O'Neil A, Opie R, Itsiopoulos C, Cotton S, Mohebbi M, Castle D, Dash S, Mihalopoulos C, Chatterton ML, Brazionis L, Dean OM, Hodge AM, Berk M. A randomised controlled trial of dietary improvement for adults with major depression (the 'SMILES' trial) BMC Med. 2017;15:23. doi: 10.1186/s12916-017-0791-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Knight A, Bryan J, Wilson C, Hodgson JM, Davis CR, Murphy KJ. The Mediterranean Diet and Cognitive Function among Healthy Older Adults in a 6-Month Randomised Controlled Trial: The MedLey Study. Nutrients. 2016;8 doi: 10.3390/nu8090579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Roca M, Kohls E, Gili M, Watkins E, Owens M, Hegerl U, van Grootheest G, Bot M, Cabout M, Brouwer IA, Visser M, Penninx BW MooDFOOD Prevention Trial Investigators. Prevention of depression through nutritional strategies in high-risk persons: rationale and design of the MooDFOOD prevention trial. BMC Psychiatry. 2016;16:192. doi: 10.1186/s12888-016-0900-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Bot M, Brouwer IA, Roca M, Kohls E, Penninx BWJH, Watkins E, van Grootheest G, Cabout M, Hegerl U, Gili M, Owens M, Visser M MooDFOOD Prevention Trial Investigators. Effect of Multinutrient Supplementation and Food-Related Behavioral Activation Therapy on Prevention of Major Depressive Disorder Among Overweight or Obese Adults With Subsyndromal Depressive Symptoms: The MooDFOOD Randomized Clinical Trial. JAMA. 2019;321:858–868. doi: 10.1001/jama.2019.0556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Parletta N, Zarnowiecki D, Cho J, Wilson A, Bogomolova S, Villani A, Itsiopoulos C, Niyonsenga T, Blunden S, Meyer B, Segal L, Baune BT, O'Dea K. A Mediterranean-style dietary intervention supplemented with fish oil improves diet quality and mental health in people with depression: A randomized controlled trial (HELFIMED) Nutr Neurosci. 2019;22:474–487. doi: 10.1080/1028415X.2017.1411320. [DOI] [PubMed] [Google Scholar]
- 119.Sánchez-Villegas A, Martínez-González MA, Estruch R, Salas-Salvadó J, Corella D, Covas MI, Arós F, Romaguera D, Gómez-Gracia E, Lapetra J, Pintó X, Martínez JA, Lamuela-Raventós RM, Ros E, Gea A, Wärnberg J, Serra-Majem L. Mediterranean dietary pattern and depression: the PREDIMED randomized trial. BMC Med. 2013;11:208. doi: 10.1186/1741-7015-11-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Steer RA, Ball R, Ranieri WF, Beck AT. Dimensions of the Beck Depression Inventory-II in clinically depressed outpatients. J Clin Psychol. 1999;55:117–128. doi: 10.1002/(sici)1097-4679(199901)55:1<117::aid-jclp12>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 121.Sánchez-Villegas A, Cabrera-Suárez B, Molero P, González-Pinto A, Chiclana-Actis C, Cabrera C, Lahortiga-Ramos F, Florido-Rodríguez M, Vega-Pérez P, Vega-Pérez R, Pla J, Calviño-Cabada MJ, Ortuño F, Navarro S, Almeida Y, Hernández-Fleta JL. Preventing the recurrence of depression with a Mediterranean diet supplemented with extra-virgin olive oil. The PREDI-DEP trial: study protocol. BMC Psychiatry. 2019;19:63. doi: 10.1186/s12888-019-2036-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Opie RS, Itsiopoulos C, Parletta N, Sanchez-Villegas A, Akbaraly TN, Ruusunen A, Jacka FN. Dietary recommendations for the prevention of depression. Nutr Neurosci. 2017;20:161–171. doi: 10.1179/1476830515Y.0000000043. [DOI] [PubMed] [Google Scholar]
- 123.Derom ML, Martínez-González MA, Sayón-Orea Mdel C, Bes-Rastrollo M, Beunza JJ, Sánchez-Villegas A. Magnesium intake is not related to depression risk in Spanish university graduates. J Nutr. 2012;142:1053–1059. doi: 10.3945/jn.111.155572. [DOI] [PubMed] [Google Scholar]
- 124.Sánchez-Villegas A, Pérez-Cornago A, Zazpe I, Santiago S, Lahortiga F, Martínez-González MA. Micronutrient intake adequacy and depression risk in the SUN cohort study. Eur J Nutr. 2018;57:2409–2419. doi: 10.1007/s00394-017-1514-z. [DOI] [PubMed] [Google Scholar]
- 125.Sánchez-Villegas A, Toledo E, de Irala J, Ruiz-Canela M, Pla-Vidal J, Martínez-González MA. Fast-food and commercial baked goods consumption and the risk of depression. Public Health Nutr. 2012;15:424–432. doi: 10.1017/S1368980011001856. [DOI] [PubMed] [Google Scholar]
- 126.Gómez-Donoso C, Sánchez-Villegas A, Martínez-González MA, Gea A, Mendonça RD, Lahortiga-Ramos F, Bes-Rastrollo M. Ultra-processed food consumption and the incidence of depression in a Mediterranean cohort: the SUN Project. Eur J Nutr. 2020;59:1093–1103. doi: 10.1007/s00394-019-01970-1. [DOI] [PubMed] [Google Scholar]
- 127.Sánchez-Villegas A, Álvarez-Pérez J, Toledo E, Salas-Salvadó J, Ortega-Azorín C, Zomeño MD, Vioque J, Martínez JA, Romaguera D, Pérez-López J, López-Miranda J, Estruch R, Bueno-Cavanillas A, Arós F, Tur JA, Tinahones FJ, Lecea O, Martín V, Ortega-Calvo M, Vázquez C, Pintó X, Vidal J, Daimiel L, Delgado-Rodríguez M, Matía P, Corella D, Díaz-López A, Babio N, Muñoz MÁ, Fitó M, García de la Hera M, Abete I, García-Rios A, Ros E, Ruíz-Canela M, Martínez-González MÁ, Izquierdo M, Serra-Majem L. Seafood Consumption, Omega-3 Fatty Acids Intake, and Life-Time Prevalence of Depression in the PREDIMED-Plus Trial. Nutrients. 2018;10 doi: 10.3390/nu10122000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Navarro AM, Abasheva D, Martínez-González MÁ, Ruiz-Estigarribia L, Martín-Calvo N, Sánchez-Villegas A, Toledo E. Coffee Consumption and the Risk of Depression in a Middle-Aged Cohort: The SUN Project. Nutrients. 2018;10 doi: 10.3390/nu10091333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Sánchez-Villegas A, Ruíz-Canela M, de la Fuente-Arrillaga C, Gea A, Shivappa N, Hébert JR, Martínez-González MA. Dietary inflammatory index, cardiometabolic conditions and depression in the Seguimiento Universidad de Navarra cohort study. Br J Nutr. 2015;114:1471–1479. doi: 10.1017/S0007114515003074. [DOI] [PubMed] [Google Scholar]
- 130.Sánchez-Villegas A, Ruíz-Canela M, Gea A, Lahortiga F, Martínez-González MA. The Association Between the Mediterranean Lifestyle and Depression. Clin Psychol Sci. 2016;4:1085–1093. [Google Scholar]
- 131.Ruiz-Estigarribia L, Martínez-González MÁ, Díaz-Gutiérrez J, Sánchez-Villegas A, Lahortiga-Ramos F, Bes-Rastrollo M. Lifestyles and the risk of depression in the "Seguimiento Universidad de Navarra" cohort. Eur Psychiatry. 2019;61:33–40. doi: 10.1016/j.eurpsy.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 132.Gea A, Martinez-Gonzalez MA, Toledo E, Sanchez-Villegas A, Bes-Rastrollo M, Nuñez-Cordoba JM, Sayon-Orea C, Beunza JJ. A longitudinal assessment of alcohol intake and incident depression: the SUN project. BMC Public Health. 2012;12:954. doi: 10.1186/1471-2458-12-954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Molero P, Martinez-Gonzalez MA, Ruiz-Canela M, Lahortiga F, Sánchez-Villegas A, Perez-Cornago A, Gea A. Cardiovascular risk and incidence of depression in young and older adults: evidence from the SUN cohort study. World Psychiatry. 2017;16:111. doi: 10.1002/wps.20390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Fernandez-Montero A, Moreno-Galarraga L, Sánchez-Villegas A, Lahortiga-Ramos F, Ruiz-Canela M, Martínez-González MÁ, Molero P. Dimensions of leisure-time physical activity and risk of depression in the "Seguimiento Universidad de Navarra" (SUN) prospective cohort. BMC Psychiatry. 2020;20:98. doi: 10.1186/s12888-020-02502-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Sánchez-Villegas A, Serrano-Martínez M, Alonso A, de Irala J, Tortosa A, Martínez-González MA. [Role of tobacco use on the incidence of depression in the SUN cohort study] Med Clin (Barc) 2008;130:405–409. doi: 10.1157/13117850. [DOI] [PubMed] [Google Scholar]
- 136.Sánchez-Villegas A, Pimenta AM, Beunza JJ, Guillen-Grima F, Toledo E, Martinez-Gonzalez MA. Childhood and young adult overweight/obesity and incidence of depression in the SUN project. Obesity (Silver Spring) 2010;18:1443–1448. doi: 10.1038/oby.2009.375. [DOI] [PubMed] [Google Scholar]