Abstract
Herpes Simplex Virus (HSV) esophagitis is a relatively rare form of infectious esophagitis. Typically, patients with viral esophagitis are immunocompromised. HSV esophagitis in an immunocompetent patient is uncommonly reported. The objective of this case report is to discuss symptoms, investigations, imaging, and treatment of HSV esophagitis in a healthy adolescent male. A previously healthy 17-year-old male presented to the ED of our facility with a 5-day history of fever, odynophagia, lethargy, and 2 episodes of emesis that failed to resolve with antibiotic treatment. Investigations revealed a low platelet count, mild hyponatremia, hypochloremia, and an elevated AST and ALT. A respiratory infection panel as well as CMV IgG, HIV, Rickettsia, and EBV tests were negative. HSV-1 PCR was positive and upper endoscopy revealed a friable mucosa, erythema, and exudates in the lower esophagus and erythematous duodenopathy. The patient received a diagnosis of HSV esophagitis and was treated with a 14-day course of IV to PO acyclovir. There was a rapid improvement of his symptoms with antiviral therapy.
Keywords: esophagitis, Herpes simplex, odynophagia, viral esophagitis, HSV-1
Introduction
Infectious esophagitis (IE) is relatively rare and almost always occurs in individuals with suppressed immune systems, such as those with HIV/AIDS, organ transplant, cancer, or immunosuppressive medications. Common primary infectious causes of esophagitis are fungal or viral, rarely bacterial, with Candida as the most common cause overall, and Herpes simplex virus (HSV) and Cytomegalovirus (CMV) as the most common viral causes. 1 Healthy individuals can develop fungal esophagitis. For example, individuals taking antibiotics have an increased risk of Candida esophagitis, but they usually also have underlying comorbidities such as diabetes or hypertension. 1 Viral esophagitis, however, is extremely rare in healthy people with no underlying immunosuppression. 2
Approximately 65% of adults are seropositive for HSV, with HSV-1 as the more common cause of HSV esophagitis than HSV-2. Risk factors for HSV esophagitis (HSE) include HIV infection, autoimmune diseases, burns, infections, and malignancy. 3 HSE can be life-threatening in immunocompromised hosts, and therefore it is important to definitively diagnose and manage patients who present with dysphagia or odynophagia.4,5 It is more prevalent in men (3:1 ratio). Initial non-specific symptoms include a temperature of 39°C or greater, prodromal fever, arthralgia, malaise, and appetite loss. In a recent study, it was found that digestive symptoms may include odynophagia (60.7%), dysphagia (37.5%), chest pain (46.4%), sore throat, and respiratory symptoms. 4
Hospital Course
A previously healthy 17-year-old Caucasian male presented to the Emergency Department (ED) with a 5-day history of severe chest pain, sore throat, and fever. During this time, he had a poor oral intake, 2 episodes of vomiting, and lethargy. He initially presented 2 days before to an urgent care clinic, where he received azithromycin for suspected pneumonia. The patient reported a 5-day history of fever with no discernible pattern and odynophagia that radiated down the midline of his chest. He also had 2 episodes of non-bloody, non-bilious emesis that were triggered by eating. He endorsed worsening of his odynophagia with cold or hot liquids. He denied any alleviating factors. Since the onset of odynophagia, the patient reported lethargy, normal appetite, but an inability to eat due to pain. He denied chest pain, palpitations, shortness of breath, cough, nausea, abdominal pain, and a history of reflux. He reported no recent sick contacts, trauma, or ingestion of caustic substances. Family history was notable for paternal early-onset heart disease. He reported occasional use of e-cigarettes and infrequent alcohol consumption but denied illicit substance use. He was not sexually active and had no allergies. He was an active 17-year-old boy who was up to date on all vaccinations.
Investigations on admission included a normal complete blood count (CBC), mild hyponatremia (132 mmol/L; normal range 136-145 mmol/L), mild hypochloremia (95 mmol/L; normal range 95-110 mmol/L), elevated AST (113 U/L; normal range 10-40 U/L), and ALT (121 U/L; normal range 10-44 U/L). Urinalysis (UA) showed amber cloudy urine with mucus, ketones (5 mg/dL; normal range negative), urobilinogen (2 U/dL; normal range <2.0 EU/dL), and protein (30 mg/dL; normal range negative). D-dimer was 0.77 μg/mL (normal range <0.46 µg/mL) and procalcitonin was 0.48 ng/mL (normal range <0.07 ng/mL). The patient was initially transferred to PICU due to increased ferritin (980 ng/mL; normal range 20-300 ng/mL) and concern for Hemophagocytic Lymphohistiocytosis (HLH) based on a low platelet count (127 000/µL; normal range 150 000-350 000/µL). However, repeat labs revealed no acute concerns.
He began treatment with IV ceftriaxone. IV doxycycline was added for 48 hours due to a suspicion of Rickettsial disease suggested by hyponatremia and thrombocytopenia. This antibiotic regimen failed to improve his symptoms. Chest X-ray showed no acute process. Upper endoscopy revealed a friable mucosa, erythema, and exudates in the lower 2/3 of the esophagus and erythematous duodenopathy (Figures 1 and 2). Based on these findings, a viral cause of esophagitis was suggested, and doxycycline and ceftriaxone were discontinued. Serologic studies for CMV, HIV, Rickettsia, and EBV were all negative. HSV-1 PCR of an esophageal biopsy was positive. The patient was subsequently started on IV acyclovir 5 mg/kg Q8H. Overnight, he showed a slight improvement in his odynophagia. The patient continued treatment with acyclovir for 14 days total with the transition to PO 800 mg QID when he could tolerate PO comfortably.
Figure 1.

Endoscopy of middle third of esophagus show erythema, exudates, and friability.
Figure 2.
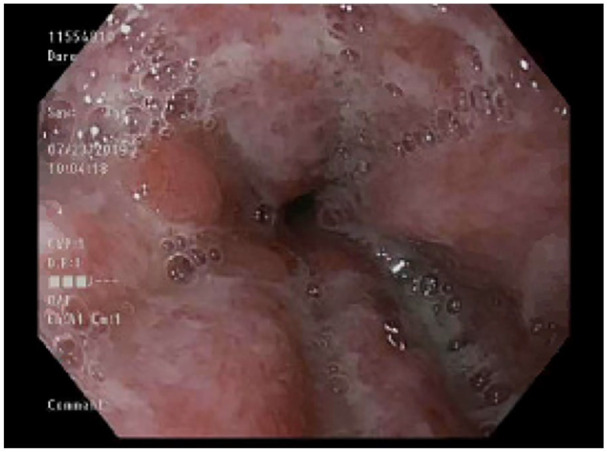
Endoscopy of the lower third of esophagus indicate inflammation, erythema, and exudates.
Discussion
This case of HSE is unusual because our patient was a healthy immunocompetent male with no known risk factors for opportunistic infection. His symptoms were sudden in onset and a thorough review of his history and medications, along with preliminary investigations, showed no evidence of predisposing factors. Current literature suggests that HSE in immunocompetent pediatric patients is rare and if present, patients usually have some underlying and undiagnosed immunodeficiency. 1 However, recent studies have shown a relationship between eosinophilic esophagitis (EoE) in immunocompetent pediatric populations and HSE.6-8 One retrospective study of 16 pediatric patients found that 45% of patients had biopsy-proven eosinophilic esophagitis (EoE) post-resolution of HSE. 7 Another case series of 5 immunocompetent pediatric patients showed 80% active EoE at the time of HSE presentation. 8 EoE symptoms can be indistinguishable from HSE, but endoscopy would show eosinophils and rings in patients with EoE. However, our patient’s endoscopy results did not support concomitant EoE with HSE. Literature does show that it is possible to diagnose HSE in immunocompromised patients before diagnostic criteria for EoE are established.7,8 It is important to have a follow-up with our patient to further investigate this relationship.
HSE is predominantly diagnosed endoscopically and histopathologically. Endoscopy shows multiple small, punched-out ulcers, raised margins, and some fibrin exudate. Usually, the middle or distal esophagus is affected. In our patient, inflammation, erythema, exudates, and friable mucosa were seen in the middle and lower third of the esophagus on endoscopy. There was also erythematous duodenopathy. In HSE histopathology, multinucleated giant cells can be seen with or without Cowdry inclusion bodies. 6 In the proximal esophagus of our patient, squamous mucosa with chronic inflammation and reactive changes was seen, and granulation tissue was found in the distal esophageal biopsy. No evidence of metaplasia, dysplasia, or malignancy was found on biopsy. Although our patient did not have typical endoscopic and histopathologic features of HSE, the diagnosis was made based on odynophagia, esophageal inflammation, and positive HSV-1 PCR.
Although current treatment for immunocompromised individuals with HSE is acyclovir, famciclovir, or valacyclovir, it is usually a self-resolving infection in immunocompetent patients. Some studies show that treatment with acyclovir in immunocompetent patients can cause rapid systemic response.1,2,6 Therefore, our pediatric patient was treated with acyclovir. Within 2 days, there was an improvement in odynophagia symptoms and liver function tests, and the patient was discharged and asked to follow up in primary care or gastroenterology clinic.
Conclusion
HSV-1 esophagitis usually occurs in immunocompromised patients but can rarely present in immunocompetent pediatric individuals. Although causes in healthy pediatric patients are not well studied, it is thought that HSV-1 esophagitis is associated with eosinophilic esophagitis. The main presenting symptom is odynophagia, and it is usually diagnosed using a combination of history, endoscopy, HSV-PCR, and histopathology. The mainstay treatment is acyclovir, and patients may have a rapid improvement of symptoms with treatment initiation.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval and Consent: Written consent was obtained from guardian of the patient for the publication of this case report.
ORCID iDs: Vedika Rajasekaran  https://orcid.org/0000-0001-6001-0436
https://orcid.org/0000-0001-6001-0436
Russell W. Steele  https://orcid.org/0000-0001-8832-0073
https://orcid.org/0000-0001-8832-0073
References
- 1. Wilcox CM. Infectious esophagitis. Gastroenterol Hepatol. 2006;2(8):567-568. [PMC free article] [PubMed] [Google Scholar]
- 2. Ramanathan J, Rammouni M, Baran J, Khatib R. Herpes simplex virus esophagitis in the immunocompetent host: an overview. Am J Gastroenterol. 2000;95(9):2171-2176. doi: 10.1111/j.1572-0241.2000.02299.x [DOI] [PubMed] [Google Scholar]
- 3. Jung KH, Choi J, Gong EJ, et al. Can endoscopists differentiate cytomegalovirus esophagitis from herpes simplex virus esophagitis based on gross endoscopic findings? Medicine (Baltimore). 2019;98(23):e15845. doi: 10.1097/MD.0000000000015845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Canalejo E, García Durán F, Cabello N, García Martínez J. Herpes esophagitis in healthy adults and adolescents: report of 3 cases and review of the literature. Medicine (Baltimore). 2010;89(4):204-210. doi: 10.1097/MD.0b013e3181e949ed [DOI] [PubMed] [Google Scholar]
- 5. Rodrigues F, Brandão N, Duque V, Ribeiro C, António AM. Herpes simplex virus esophagitis in immunocompetent children. J Pediatr Gastroenterol Nutr. 2004;39(5):560-563. doi: 10.1097/00005176-200411000-00022 [DOI] [PubMed] [Google Scholar]
- 6. Hoversten P, Kamboj AK, Katzka DA. Infections of the esophagus: an update on risk factors, diagnosis, and management. Dis Esophagus. 2018;31(12):doy094. doi: 10.1093/dote/doy094 [DOI] [PubMed] [Google Scholar]
- 7. Fritz J, Lerner D, Suchi M. Herpes simplex virus esophagitis in immunocompetent children: a harbinger of eosinophilic esophagitis? J Pediatr Gastroenterol Nutr. 2018;66(4):609-613. doi: 10.1097/MPG.0000000000001748 [DOI] [PubMed] [Google Scholar]
- 8. Zimmermann D, Criblez DH, Dellon ES, et al. Acute herpes simplex viral esophagitis occurring in 5 immunocompetent individuals with eosinophilic esophagitis. ACG Case Rep J. 2016;3(3):165-168. doi: 10.14309/crj.2016.38 [DOI] [PMC free article] [PubMed] [Google Scholar]


