Abstract
Post-9/11 U.S. veterans are clinically complex with multiple co-occurring health conditions that lead to increased morbidity and mortality, risk for suicide, and decreased quality of life, but underutilization and resistance to treatment remain significant problems. Increased isolation and decreased community and social support due to coronavirus disease (COVID-19) have exacerbated mental health risk. This study evaluated the safety and feasibility of home-based telemental health group workshops to improve reintegration and social connection in post-9/11 U.S. military personnel. Seventy-four (61 males/13 females) post-9/11 U.S. military veterans were randomized to receive 12 sessions of STEP-Home cognitive-behavioral group workshop or present-centered group therapy. Treatment was delivered either in person (traditional medical center setting, treatment as usual [TAU]), or via home-based synchronous videoconferencing (VC). The change to VC occurred due to social distancing guidelines during COVID-19. Mean age was 41.0 years (SD = 11.5, range 24–65). Forty-five (36 males/9 females) participated in VC and 29 (25 males/4 females) in TAU. Demographics were similar across treatment milieu. There were no differences in therapist treatment adherence for TAU versus VC. Therapist satisfaction was higher for TAU groups (q value < .05). Veterans showed higher enrollment, attendance, group cohesion, and veteran-to-veteran support for VC compared to TAU (q values < .05). Safety procedures were successfully implemented via VC. Results demonstrate the safety, feasibility, and high satisfaction of group telemental health in U.S. veterans. Higher enrollment and treatment adherence for telemental health delivery resulted in a greater likelihood of receiving an effective treatment dose than TAU. Strong group cohesion and veteran-to-veteran support were achievable via telehealth. Telemental health offers convenient, efficient, and cost-effective care options for veterans and may be particularly helpful for patients with high psychiatric burden.
Keywords: U.S. veterans, feasibility; safety; reintegration; telehealth; group therapy
Underutilization and resistance to mental health treatment are significant problems among veterans (Batten and Pollack, 2008, Hoge et al., 2004, Sayer et al., 2009). Treatment resistance often stems from stigma surrounding mental health treatment, as well as individuals’ perceptions that their impairments are not severe enough to merit treatment (Cooper-Patrick et al., 1997). Hoge et al. found that stigma was greatest among veterans most in need of mental health services. In addition to institutional and cultural barriers, there are also logistical treatment barriers, such as travel, availability of mental health treatment providers, time away from family or work, and scheduling difficulties (Hoge et al., 2004, Schell and Marshall, 2008). Convenient, patient-centered care options, particularly those that are cost-effective and easily accessed and implemented, are needed. An integral part of the mission of the U.S. Veterans Health Administration (VHA) is to adapt treatment models to better address issues most relevant to veteran health, including their mental health and reintegration to civilian life after military service.
Telehealth is one way the VHA has attempted to address barriers to in-person care (Panangala, 2018). Prior to coronavirus disease (COVID-19), telehealth initiatives focused on individual treatment delivery and implementation in rural settings where travel to a VA medical center was prohibitive. However, in 2017, VA telehealth was expanded to include VA Video Connect (VVC), a synchronous, encrypted videoconferencing telehealth platform accessible on a desktop, smartphone, or tablet. COVID-19 has increased VVC rollout. The VHA began the COVID-19 pandemic with a robust telehealth program and has taken a momentous leap forward in this arena to comply with social distancing mandates. Importantly, mental health service is the most frequent service accessed by veterans using VVC (U.S. Department of Veteran Affairs, 2018). Although the use of VHA telemental health has increased tremendously, there remains a need to demonstrate that telemental health, and in particular group telemental health, is feasible, safe, and effective before widespread implementation can occur.
The newest generation of post-9/11 combat veterans have been shown to have more negative attitudes about mental health treatment (Garcia et al., 2014, Sayer et al., 2009), higher dropout rates (Chard et al., 2010, Hoge et al., 2004), and lower engagement with typical VA standard of care compared to veterans serving in other conflicts (Harpaz-Rotem & Rosenheck, 2011). Post-9/11 veterans are a clinically complex group with multiple co-occurring conditions, including high co-prevalence of mild traumatic brain injury (mTBI), posttraumatic stress disorder (PTSD), depression, substance misuse, and chronic pain (Hoge et al., 2008). Poor management of these co-occurring conditions leads to increased morbidity, mortality, risk for suicide, and decreased functional status and quality of life (Amick et al., 2018, Evans et al., 2005, Lippa et al., 2015).
There are many veterans who could benefit from mental health treatment who do not seek it out and are in fact not engaged with any VA care. COVID-19 has led to social distancing guidelines that have profoundly affected human contact and access to medical care, leading to adverse outcomes on social support, mental health, and suicide risk (Reger et al., 2020). Social distancing directives reduced community connection and exacerbated mental health risk to an already socially isolated, at-risk population. The STEP-Home intervention was specifically designed to maximally entice veterans who are not engaged in treatment and may be resistant to “mental health” approaches but could benefit from them. STEP-Home provides an alternative to diagnostically based treatment approaches by instead employing a skills-based transdiagnostic workshop approach. STEP-Home is a cognitive-behavioral group workshop intervention for post-9/11 veterans with high prevalence of clinical comorbidity adapted from the empirically validated intervention Short-Term Executive Plus (Cantor et al., 2014) civilian TBI rehabilitation program. STEP-Home consists of 12 weekly, 90-minute group workshops designed to facilitate veterans’ reintegration “Home” to civilian life after military service. STEP-Home sessions teach cognitive-behavioral skills relevant across diagnostic categories, including problem solving (PS), emotional regulation (ER), and attention training (AT). Skills are integrated and applied across veteran-specific content areas, including work/school and relationships. Psychoeducation regarding common veteran mental health diagnoses, including PTSD, mTBI, and substance use, is provided. We have demonstrated the feasibility and acceptability of the in-person intervention in post-9/11 veterans (Fortier et al., 2018). This study also demonstrated that change in treatment-related skill acquisition was associated with decreased stigma and increased vocational, community, and VA treatment engagement, reintegration status, and cognitive and emotional function postintervention (Fortier et al., 2018).
The purpose of this study was to evaluate the safety and feasibility of home-based group telemental health workshops to improve reintegration in post-9/11 veterans. This study was part of a multisite clinical trial that compared the efficacy of the STEP-Home transdiagnostic skills-based community reintegration group workshop to present-centered group therapy (PCGT). Transition from an in-person traditional medical center (same room) setting (treatment as usual [TAU]) to telemental health (videoconferencing [VC]) delivery occurred as a result of COVID-19 VHA research and patient safety guidelines midstudy allowing direct examination of VC compared to TAU. Therefore, veterans were not randomized to VC or in-person TAU delivery.
Veterans were randomized to the treatment condition, STEP-Home, or PCGT. PCGT was selected as the active control to allow greater certainty that STEP-Home treatment effectiveness was due to specific aspects of the key ingredients of the experimental therapy (STEP-Home) and not merely to nonspecific therapeutic factors. PCGT was initially developed by Schnurr et al. (2003) to include all elements of effective PTSD treatment that are not specifically trauma focused. PCGT is a manualized, evidence-based intervention to control for the nonspecific benefits of the group experience (e.g., therapist contact, instillation of hope, expectation of improvement) with notably low dropout rates (Classen et al., 2001, Classen et al., 2011, Schnurr et al., 2003). PCGT focuses on improving self-awareness, interpersonal relationships, and responses to current life stressors related to trauma or PTSD. For the purposes of this randomized controlled trial (RCT), standard PCGT (Schnurr et al., 2003) was adapted to focus on psychoeducation regarding common difficulties related to veteran reintegration to civilian life and impact on interpersonal relationships.
A major difference between STEP-Home and PCGT is the conceptualization of treatment goals. PCGT encourages veterans to discuss current struggles and stressors related to reintegration into civilian community, conceptualizing the active support and sharing as the treatment goal. PCGT does not offer any specific skills or strategies for how to address these struggles, other than what veterans suggest in the group setting. STEP-Home is an active cognitive-behavioral intervention that provides a concrete framework for understanding the emotions, thoughts, and behaviors resulting from a stressor (ER skills), and then provides a tangible and palatable strategy to solve the problem (PS skills), leading to increased self-awareness and a sense of agency. STEP-Home and PCGT share a similar emphasis on the therapeutic benefits of group dynamics and active veteran-to-veteran support, but STEP-Home’s approach is innovative in teaching and practicing skills both inside and outside of the group. Additional differentiating components of STEP-Home include a focus on providing psychoeducation on TBI, PTSD, and overlapping symptoms, use of AT and anger management strategies, and an intentional design to provide a “gateway” to engagement in other forms of treatment and community programming. STEP-Home builds from the core elements of PCGT (in-group social support and validation) but more formally normalizes post-9/11 veterans’ shared difficulties and creates a greatly needed sense of empowerment and hope for successful transition from military to civilian life.
The purpose of the current study was to evaluate the safety, feasibility, and acceptability of telehealth VC as compared to in-person delivery of these two interventions (STEP-Home and PCGT) to improve reintegration in post-9/11 veterans.
Methods
participants
Veterans were recruited from VA Boston Healthcare System clinics and the community locally and nationwide via study outreach coordinator and social media (Facebook). Inclusion criteria included (a) military service occurring after September 11, 2001 terrorist attacks (post-9/11-era veteran); (b) self-reported difficulty with civilian reintegration (Sayer et al., 2011), postdeployment readjustment (Katz et al., 2010) and/or anger/irritability (Spielberger, 1999); (c) if taking psychoactive medications, stable regimen for a minimum of 30 days; and (d) able to connect to telehealth appointment using personal equipment (computer, tablet, or smartphone) in a private area free from distractions. Critically, formal diagnosis of TBI or PTSD (or other cognitive/psychiatric condition) was not required. Exclusion criteria included (a) history of neurological illness other than TBI; (b) current diagnosis of thought or psychotic disorder; and (c) current active suicidal and/or homicidal ideation, intent, or plan requiring crisis intervention. All procedures were monitored and approved by the Institutional Review Board at the VA Boston Healthcare System (IRB approval #3210). All participants provided written informed consent prior to participation in study activities.
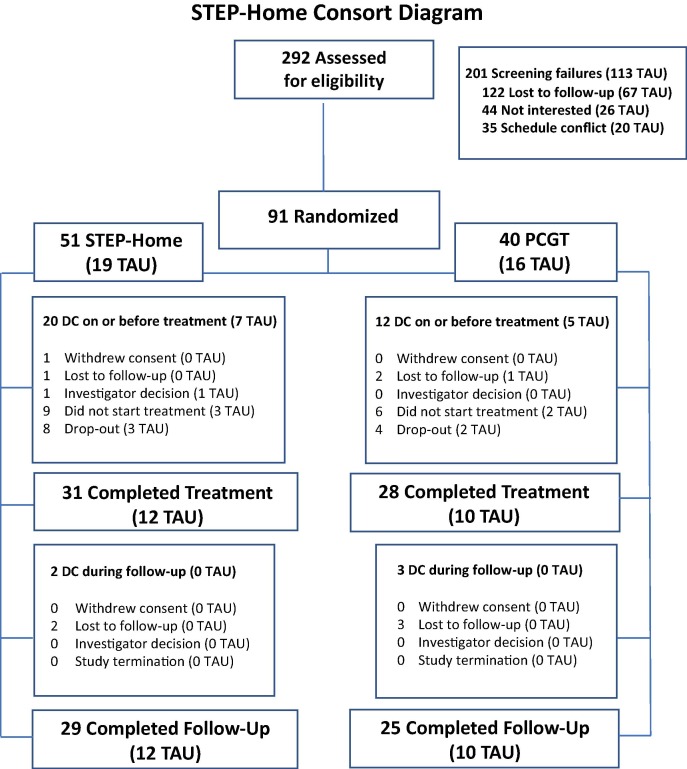
A total of 292 veterans were assessed for eligibility; 91 participants met inclusion criteria and were randomized (see Figure 1 ). Of these 91, 29 completed in-person TAU groups and 45 completed online VC groups. Participants were randomized to treatment condition (STEP-Home vs. PCGT) in a 1:1 ratio using permuted blocks with a size of 20. Participants received 12 weeks of intervention and were assessed at baseline, posttreatment (12 weeks), and follow-up (24 weeks). Participants were paid $20 for baseline, posttreatment, and follow-up assessments. Veterans were not randomized to VC or in-person TAU delivery—rather, this difference in treatment delivery occurred as a result of social distancing guidelines during COVID-19.
Figure 1.
The CONSORT diagram depicts the progress through the phases of the randomized trial and further denotes which participants in each category were treatment as usual (TAU; in person).
interventions
Treatment Groups
Group interventions included the STEP-Home workshop (Fortier et al., 2018) and PCGT (Schnurr et al., 2003).
Treatment Providers
Treatment providers included four clinicians (one licensed psychologist, two master’s-level counselors, and one postdoctoral fellow). All study personnel were supervised weekly by a licensed psychologist.
In-Person TAU and Telehealth VC Procedures
Prior to the first group session, a one-to-one baseline appointment was conducted with study staff to review informed consent procedures and limits of confidentiality. These sessions were conducted in person for TAU and via telehealth for VC. VC participants were also familiarized with VC procedures and tested their network connection at this baseline appointment. Several modifications were made for sharing visual materials for VC sessions, including screen sharing for VC versus a whiteboard for TAU.
measures
Demographics
Demographics included age, race/ethnicity, gender, education, service branch, number of deployments, and service connection.
Premorbid IQ
Premorbid IQ was estimated with the Wechsler Test of Adult Reading (WTAR; 50 items, range = 0–50, Cronbach’s α = 0.93; Wechsler, 2001).
Clinical and Functional Characteristics
Prevalence of psychiatric conditions was obtained via patient medical record review. PTSD severity was assessed with the PTSD Checklist for DSM-5 (PCL-5; 20 items, range = 0–80, α = 0.96; Bovin et al., 2016). Mood, anxiety, and stress were assessed with the Depression Anxiety and Stress Scale (DASS-21; 21-item subscales range = 0–42, α = 0.93; Henry & Crawford, 2005). State anger (range = 15–60), trait anger (range = 10–40), and anger expression index (range = 0–96) were assessed with the State–Trait Anger Expression Inventory (STAXI-2; 57 items, αs > 0.73; Forgays et al., 1997). Neurobehavioral symptoms were assessed with the Neurobehavioral Symptoms Inventory (NSI; 22 items, range = 0–88, α = 0.95; Soble et al., 2014). Functional status was assessed with the World Health Organization Disability Assessment Schedule–II (WHODAS-II; 36 items, range = 0–100, α = 0.86; Ustün et al., 2010) and the Satisfaction With Life Scale (SWLS; 5 items, range = 5–35; Diener et al., 1985). Civilian reintegration status was assessed with the Military to Civilian Questionnaire (M2C-Q; 16 items, range = 0–64, α = 0.95; Sayer et al., 2011) and the Post-Deployment Readjustment Inventory (PDRI; 36 items, range = 36–180, α = 0.97; Katz et al., 2010).
Treatment fidelity was assessed by group leader self-rating (Likert scale range = 1–5) and supervisor rating (Likert scale range = 1–5) of adherence to treatment manuals averaged across the 12 workshops. Group leaders rated overall group cohesion, observable veteran-to-veteran support, and veteran engagement for each group (Likert scale range = 1–5). Ratings were averaged across the 12 workshops. Group leaders rated their satisfaction leading the group (Likert scale range = 1–5). Ratings were averaged across the 12 workshops. Enrollment data were used to assess treatment acceptability (enrollment = ratio enrolled of referred).
Program Satisfaction
Veterans rated their satisfaction with the workshop (Likert scale range = 1–5) postintervention, including pace of treatment delivery, workshop content, relevancy of workshop goals, and willingness to recommend STEP-Home to other veterans. VC veterans also rated their overall program satisfaction using the Client Satisfaction Questionnaire (CSQ-8; 8 items, Likert scale range = 1–4, range = 8–32).
Treatment Adherence and Tolerability
Veteran treatment adherence was assessed by number of sessions attended out of 12. Treatment tolerability was assessed by attrition rate. Veterans who attended fewer than eight sessions were considered “dropouts.” Veterans who completed eight or more sessions were considered “treatment completers.”
A checklist documented patient safety and technical issues, including any adverse events (nonfatal suicide-related behaviors, suicides, psychiatric hospitalizations, emergency room visits, any other behaviors resulting in crisis intervention) and an adequate telehealth delivery environment for safety and privacy. A checklist was used to document telehealth equipment, connectivity status, video, audio, and any disruptions to sessions, including therapists’ rating of VC connectivity for each group.
statistical analysis
Chi-square tests and Fisher’s exact tests were used to identify associations among categorical variables. Wilcoxon’s rank-sum test was used to identify associations among nonparametric continuous variables. The Benjamini and Hochberg false discovery rate (FDR) adjustment was applied to correct for multiple comparisons (q values). All q values were derived from two-sided p values. Analyses were conducted in SAS (version 9.4).
Results
participants
Seventy-four (61 males/13 females) post-9/11 U.S. veterans were enrolled in the RCT: 40 STEP-Home and 34 PCGT; 29 in person (25 males/4 females), 45 online (36 males/9 females). Mean age was 41.0 years (SD = 11.5, range 24–65). Veterans reported an average of two deployments (see Table 1 ). The sample was racially diverse and representative of all military branches with 11 U.S. states represented. Psychiatric and behavioral (sleep, pain) disorders were prevalent with PTSD and pain occurring most frequently. Mood disorders were also frequent. TBI was less frequent but still prevalent. On average, veterans endorsed moderate to severe symptom severity for PTSD, depression, anxiety, stress, and anger. Neurobehavioral symptoms were common. Veterans reported significant difficulty with day-to-day functional abilities, readjustment, and reintegration status.
Table 1.
Demographics Stratified by Treatment Delivery (n = 74) at Baseline
| Covariates | In-person TAU (n = 29) |
Telehealth VC (n = 45) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Range | Range | p value | q value | |||||||
| Age, mean (SD) | 39.9 (10.5) | 24–65 | 41.8 (12.1) | 25–65 | -0.48 | .630 | .964 | |||
| Males, n (%) | 25 (86.2%) | - | 36 (80.0%) | - | 0.47 | .493 | .964 | |||
| Education (years), mean (SD) | 15.5 (1.9) | 12–18 | 14.9 (1.9) | 12–19 | 1.45 | .146 | .964 | |||
| WTAR total score, mean (SD)a | 37.8 (9.3) | 9–47 | 38.4 (6.7) | 24–48 | 0.26 | .795 | .964 | |||
| Race/ethnicity, n (%)b | ||||||||||
| Hispanic | 8 (27.6%) | - | 8 (18.2%) | - | 0.90 | .342 | .964 | |||
| White | 20 (69.0%) | - | 32 (72.7%) | - | 0.12 | .728 | .964 | |||
| Black | 4 (13.8%) | - | 10 (22.7%) | - | 0.90 | .343 | .964 | |||
| Asian | 2 (6.9%) | - | 1 (2.3%) | - | .559F | .964 | ||||
| American Indian/Alaska Native | 1 (3.5%) | - | 0 (0.0%) | - | .397F | .964 | ||||
| Other | 3 (10.3%) | - | 3 (6.8%) | - | .676F | .964 | ||||
| Branch of service, n (%)b | ||||||||||
| Army | 11 (37.9%) | - | 24 (54.6%) | - | 1.93 | .164 | .964 | |||
| Navy | 7 (24.1%) | - | 9 (20.5%) | - | 0.14 | .710 | .964 | |||
| Air Force | 2 (6.9%) | - | 2 (4.6%) | - | .999F | .999 | ||||
| Marines | 4 (13.8%) | - | 10 (22.7%) | - | 0.90 | .343 | .964 | |||
| Coast Guard | 1 (3.5%) | - | 1 (2.3%) | - | .999F | .999 | ||||
| National Guard/Reserves | 11 (37.9%) | - | 14 (31.8%) | - | 0.29 | .590 | .964 | |||
| n deployments, mean (SD)b | 2.3 (2.3) | 0–12 | 2.2 (1.7) | 0–8 | -0.08 | .940 | .999 | |||
| Service connection, mean (SD)c | 79.0 (20.2) | 20–100 | 81.1 (22.6) | 20–100 | -0.78 | .435 | .964 | |||
| Traumatic brain injury, n (%) | 6 (20.7%) | - | 13 (28.9%) | - | 0.62 | .431 | .964 | |||
| Psychiatric conditions, n (%) | ||||||||||
| PTSD | 20 (69.0%) | - | 29 (64.4%) | - | 0.16 | .688 | .964 | |||
| Anxiety | 12 (41.4%) | - | 17 (37.8%) | - | 0.10 | .757 | .964 | |||
| Mood | 18 (62.1%) | - | 25 (55.6%) | - | 0.31 | .579 | .964 | |||
| Alcohol use | 7 (24.1%) | - | 17 (37.8%) | - | 1.50 | .221 | .964 | |||
| Other substance use | 2 (6.9%) | - | 5 (11.1%) | - | .698F | .964 | ||||
| Pain disorder, n (%) | 22 (75.9%) | - | 35 (77.8%) | - | 0.04 | .848 | .998 | |||
| Sleep disturbance, n (%) | 12 (41.4%) | - | 11 (24.4%) | - | 2.36 | .124 | .964 | |||
| n conditions, mean (SD)d | 3.8 (2.0) | 0–7 | 4.5 (3.3) | 0–13 | -0.93 | .352 | .964 | |||
| n | Mean (SD) | Range | n | Mean (SD) | Range | p value | q value | |||
| PCL-5 | 28 | 46.3 (19.8) | 2–73 | 42 | 43.5 (19.8) | 2–80 | 0.81 | .418 | .964 | |
| DASS-21 Depression | 28 | 20.8 (11.5) | 0–40 | 42 | 19.1 (11.8) | 2–42 | 0.69 | .490 | .964 | |
| DASS-21 Anxiety | 28 | 15.5 (10.9) | 0–38 | 42 | 14.7 (11.1) | 0–38 | 0.38 | .705 | .964 | |
| DASS-21 Stress | 28 | 20.6 (10.8) | 0–38 | 42 | 20.4 (10.4) | 0–42 | 0.28 | .782 | .964 | |
| STAXI-2 State Anger | 28 | 23.5 (8.4) | 15–48 | 43 | 24.1 (9.4) | 15–52 | 0.00 | .999 | .999 | |
| STAXI-2 Trait Anger | 28 | 20.6 (6.5) | 10–37 | 43 | 21.5 (6.3) | 10–34 | -0.61 | .544 | .964 | |
| STAXI-2 Anger Expression Index | 28 | 40.8 (9.9) | 14–66 | 43 | 42.0 (13.9) | 11–71 | -0.80 | .423 | .964 | |
| NSI | 29 | 38.4 (19.6) | 0–80 | 42 | 37.1 (16.1) | 9–68 | 0.32 | .752 | .964 | |
| WHODAS-II | 29 | 35.4 (21.8) | 0–80 | 42 | 35.5 (19.4) | 1–74 | -0.11 | .912 | .999 | |
| SWLS | 29 | 13.8 (6.7) | 5–35 | 43 | 15.4 (8.5) | 5–35 | -0.55 | .581 | .964 | |
| M2C-Q | 28 | 32.6 (12.7) | 3–54 | 43 | 31.8 (21.1) | 2–54 | 0.39 | .693 | .964 | |
| PDRI | 28 | 118.1 (28.9) | 42–159 | 43 | 118.9 (32.3) | 36–176 | -0.14 | .892 | .999 | |
Note. TAU = treatment as usual; VC = videoconferencing; SD = standard deviation; WTAR = Wechsler Test of Adult Reading; PTSD = posttraumatic stress disorder; PCL-5 = PTSD Checklist for DSM-5; DASS = Depression Anxiety and Stress Scale; STAXI = State–Trait Anger Expression Inventory; NSI = Neurobehavioral Symptoms Inventory; WHODAS-II = World Health Organization Disability Assessment Schedule–II; SWLS = Satisfaction With Life Scale; M2C-Q = Military to Civilian Questionnaire; PDRI = Post-Deployment Readjustment Inventory. P value refers to two-sided tests. Q value refers to p value adjusted for multiple comparisons using the Benjamini and Hochberg false discovery rate. F denotes Fisher’s exact test.
WTAR total score: n = 28 for TAU, n = 43 for VC.
Race/ethnicity, service branch, and n deployments: n = 29 for TAU, n = 44 for VC.
Among veterans reporting having applied for a service connection: n = 20 for TAU, n = 36 for VC.
Total number of traumatic brain injury, psychiatric, and somatic conditions.
TAU Versus VC Participant Characteristics
Veterans enrolling in TAU and VC workshops did not differ on age, race/ethnicity, gender, education, premorbid intelligence, number of deployments, or prevalence of psychiatric/behavioral conditions. Veterans in VC tended to have a higher number of comorbid psychiatric and/or behavioral conditions (mean = 4.5, SD = 3.3, range = 0–13) compared to those in TAU (mean = 3.8, SD = 2.0, range = 0–7), but number of comorbidities did not significantly differ between groups. Clinical and functional scores were similar for TAU and VC groups at baseline.
treatment fidelity and satisfaction
There were no differences in therapist fidelity to treatment for TAU versus VC (see Table 2 ). Therapist satisfaction for TAU group format was higher (mean = 5.0, SD = 0.0) than VC (mean = 4.5, SD = 0.6, Z = 2.70, q value = .028), although overall satisfaction was high for both modalities. The enrollment rate for VC (31%) was higher than TAU (20%; q value = .048) and veteran satisfaction ratings were similar for TAU (mean = 4.7, SD = 0.6) and VC (mean = 4.8, SD = 0.5). Veterans attended significantly more VC than TAU groups (attendance = 75% TAU, 88% VC, Z = –2.72, q value = .028). Attrition was similar across treatment modality (24% TAU, 18% VC). Seven veterans dropped out of TAU workshops, whereas 22 completed the program (76% treatment completion rate). Eight veterans dropped out of VC workshops, whereas 37 completed the program (82% treatment completion rate). Group cohesion and veteran-to-veteran support were higher for the VC compared to TAU (q value = .028 and 026, respectively). Veteran engagement did not differ by treatment modality but suggested a possible trend toward greater engagement for VC (q value = .079).
Table 2.
Enrollment, Completion, Attendance, Satisfaction, Group Dynamics, and Technology Ratings by Treatment Delivery
| In-person TAU | Telehealth VC |
|||||||
|---|---|---|---|---|---|---|---|---|
| n, % | n, % | p value | q value | |||||
| Enrollment | 29, 20% | 45, 31% | 5.24 | .022 | .048 | |||
| Dropout | 7, 24% | 8, 18% | 0.44 | .506 | .557 | |||
| Treatment completers | 22, 76% | 37, 82% | 0.44 | .506 | .557 | |||
| Attendance | -- 75% | -- 88% | -2.72 | .007 | .026 | |||
| Would recommend program to other veterans | 19, 90% | 34, 94% | .357F | .477 | ||||
| n | Mean (SD) | n | Mean (SD) | p value | q value | |||
| Treatment fidelity | ||||||||
| Therapist self-rating | 144 | 4.97 (.16) | 261 | 4.98 (.14) | -0.56 | .575 | .575 | |
| Supervisor rating | 144 | 4.97 (.16) | 261 | 4.98 (.12) | -0.86 | .390 | .477 | |
| Treatment satisfaction | ||||||||
| Therapist rating | 12 | 5.00 (.00) | 22 | 4.50 (.60) | 2.70 | .007 | .026 | |
| Veteran rating | 21 | 4.67 (.58) | 35 | 4.80 (.47) | -0.98 | .325 | .477 | |
| CSQ-8 (8–32) | - | - | 22 | 30.32 (2.40) | - | - | ||
| Group dynamics, therapist ratings | ||||||||
| Group cohesion | 12 | 3.56 (.64) | 22 | 4.19 (.73) | -2.56 | .010 | .028 | |
| Veteran-to-veteran support | 12 | 3.85 (.51) | 22 | 4.36 (.58) | -2.70 | .007 | .026 | |
| Veteran engagement | 12 | 4.11 (.54) | 22 | 4.43 (.68) | -2.03 | .043 | .079 | |
| Online platform/technology, therapist rating | 22 | 4.23 (.79) | ||||||
Note. TAU = treatment as usual; VC = videoconferencing; SD = standard deviation; CSQ = Client Satisfaction Questionnaire. P value refers to two-sided tests. Q value refers to p value adjusted for multiple comparisons using the Benjamini and Hochberg false discovery rate. F denotes Fisher’s exact test. Attendance = number of sessions attended (out of 12) among treatment completers. Treatment fidelity ratings taken for both therapists at each of the 12-week sessions. Participant ratings = 1–5 Likert scale assessed posttreatment. Therapist ratings = 1–5 Likert scale assessed posttreatment.
No significant differences were found across treatment assignments (STEP-Home vs. PCGT) for enrollment, treatment completion, attendance, satisfaction, group dynamics, or technology ratings (see Supplemental Table 1). Dropouts and treatment completers did not differ on age, race/ethnicity, gender, education, premorbid intelligence, number of deployments, prevalence of positive diagnosis, or number of comorbidities (see Supplemental Table 2).
Therapists rated VC technology status, including audio and video connectivity, as highly successful for VC (mean = 4.3, SD = 0.8). The majority of veterans used a personal computer to connect, although tablets and smartphones were successfully utilized.
Safety Outcomes
No adverse events occurred during either TAU or VC workshops. During eligibility screening, 39 veterans endorsed suicidal ideation but reported no intent or plan to act on those thoughts and thus were enrolled. There were no patient-related incidents requiring crisis intervention during treatment. There were no instances when patient safety or privacy necessitated discontinuation of participation in treatment in TAU or VC, including due to VC video connection.
Descriptive VC Feedback (Satisfaction Questionnaire)
Many veterans who participated in the VC group stated they were not willing to do in-person groups and enrolled specifically for the virtual treatment delivery. Other veterans reported they had dropped out of in-person mental health groups in the past because they found them to be triggering due to PTSD and/or anxiety but were willing to try the VC format because they found it easier to engage in and less anxiety provoking. Many veterans also stated they preferred VC groups for pragmatic reasons (e.g., less travel, particularly to an urban setting; less interference with life commitments).
Discussion
Feasibility data, including enrollment, adherence, and satisfaction, did not differ by treatment assignment, allowing examination of treatment delivery across the two treatment arms. Home-based VC telemental health of both STEP-Home and PCGT was safe and feasible in post-9/11 U.S. veterans with multiple co-occurring psychiatric and somatic conditions (e.g., high psychiatric burden). There were no differences in treatment fidelity based on treatment milieu, indicating that therapists were able to adhere to the treatment manual and deliver treatment effectively via VC. Therapist satisfaction for TAU was higher than VC, but overall satisfaction was high for both treatment delivery formats.
Treatment acceptability, attrition, and satisfaction were generally comparable across treatment milieu. VC groups showed higher enrollment and attendance rates than TAU. This finding supports veteran feedback that online groups are more manageable, particularly for those veterans struggling with PTSD and high psychiatric burden. In particular, veterans with PTSD and anxiety, which reportedly impeded willingness to engage in in-person groups in an urban VA medical center setting, were more willing to participate in VC. This finding is critical because it indicates that veterans with higher mental health needs may be more willing to enroll in VC as compared to TAU at an urban medical center. VC groups showed higher attendance than TAU, indicating higher treatment adherence for online than in-person group mental health. Increased attendance for VC is important because it indicates greater tolerability and probability of receiving an effective treatment dose.
Group dynamics were better for VC as compared to TAU per therapists’ ratings. This finding is critical in that it demonstrates that the social support common to the in-person group treatment setting can be achieved through telehealth. In fact, VC groups showed greater cohesion, most likely indicating strong group integration for both social and therapy-related tasks (e.g., learning CBT skills). A sense of belongingness and community within the workshops is one of the primary goals of reintegration interventions to assist veterans with the transition from the support provided within the military system to the civilian world. Higher group cohesion should lead to stronger motivation to adhere to the treatment and better attendance. Group cohesion is frequently considered essential to effective group therapy—thus, demonstrating that strong group cohesion is achievable via telehealth is critical.
The absence of any safety events provides additional evidence that group telemental health can be delivered safely to veterans in their homes with appropriate safety standards and planning in place. This finding is significant given the high rate of clinical comorbidity and severity of psychiatric symptoms, including PTSD, mood, anger, and reintegration and functional challenges present in the sample. Although there were no adverse events, general patient safety concerns (e.g., nonacute suicidal ideation) were safely assessed and addressed via VC telehealth.
Our data indicate that VC may reach more post-9/11 veterans unwilling to engage in traditional TAU group mental health treatment. There are many veterans who could benefit from mental health treatment who do not seek it out. Hoge et al. (2004) demonstrated that concern about stigma was greatest among veterans most in need of mental health services. Our data support and extend these findings and suggest that post-9/11 veterans with high psychiatric burden and mental health needs are more likely to engage in VC than TAU group treatment. Veterans may prefer online over in-person groups because visiting a VA medical center and/or a major metropolitan area and attending a group, in particular where one sits in a confined space with other veterans discussing military experiences, can trigger PTSD symptoms and/or anxiety. Also, logistical reasons (e.g., increased flexibility in scheduling, reduced travel time) may increase preference for online treatment.
Underutilization and resistance to mental health treatment remain significant problems for post-9/11 veterans (Batten and Pollack, 2008, Hoge et al., 2004, Sayer et al., 2009). The VA has attempted to reduce barriers to in-person care by expanding telehealth and updating connectivity software (Panangala, 2018). However, the focus has been primarily on individual treatment delivery and implementation in rural settings. COVID-19 has increased the rollout for VVC, particularly for mental health service (U.S. Department of Veteran Affairs, 2018). Despite this progress in accessible telehealth platforms, the current approach to care is not fully meeting the needs of post-9/11 veterans. We suggest that acceptable transdiagnostic interventions, such as STEP-Home, are needed to better address post-9/11 veterans’ mental health. In particular, the VA’s VVC software should be expanded to better support interactive group use. Group cohesion requires settings that allow group members to view all group members and leaders simultaneously (rather than just the speaker) for best use.
conclusion
There is a high need for developing and disseminating interventions that lower the barriers for post-9/11 veterans who do not seek traditional forms of therapy or engage regularly in mental health care. Increased isolation due to COVID-19 has exacerbated mental health risk. This study demonstrated that online delivery of group mental health treatment is safe, feasible, and results in greater treatment enrollment, adherence, group cohesion, and veteran-to-veteran support than in-person TAU in post-9/11 veterans with high psychiatric burden. Post-9/11 veterans with the greatest mental health needs may engage more with online treatment formats.
Conflict of Interest Statement
The authors declare that there are no conflicts of interest.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.beth.2021.11.004.
The following are the Supplementary data to this article:
Footnotes
We would like to thank Regina McGlinchey, William Milberg, Wally Musto, and the entire TRACTS team.
VA RR&D Merit Review to CBF (RX-002907) and the Translational Research Center for TBI and Stress Disorders (TRACTS), a VA Rehabilitation Research and Development Traumatic Brain Injury National Research Center (B3001-C).
Clinicaltrials.gov: D2907-R.
References
- Amick M.M., Meterko M., Fortier C.B., Fonda J.R., Milberg W.P., McGlinchey R.E. The deployment trauma phenotype and employment status in veterans of the wars in Iraq and Afghanistan. Journal of Head Trauma Rehabilitation. 2018;33(2):E30–E40. doi: 10.1097/HTR.0000000000000308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batten S.V., Pollack S.J. Integrative outpatient treatment for returning service members. Journal of Clinical Psychology. 2008;4(4):928–939. doi: 10.1002/jclp.20513. [DOI] [PubMed] [Google Scholar]
- Bovin M.J., Marx B.P., Weathers F.W., Gallagher M.W., Rodriguez P., Schnurr P.P., Keane T.M. Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders—Fifth Edition (PCL-5) in veterans. Psychological Assessment. 2016;28(11):1379–1391. doi: 10.1037/pas0000254. [DOI] [PubMed] [Google Scholar]
- Cantor J., Ashman T., Dams-O’Connor K., Dijkers M.P., Gordon W., Spielman L., Tsaousides T., Allen H., Nguyen M., Oswald J. Evaluation of the Short-Term Executive Plus intervention for executive dysfunction after traumatic brain injury: A randomized controlled trial with minimization. Archives of Physical Medicine and Rehabilitation. 2014;95(1):1–9.e3. doi: 10.1016/j.apmr.2013.08.005. [DOI] [PubMed] [Google Scholar]
- Chard K.M., Schumm J.A., Owens G.P., Cottingham S.M. A comparison of OEF and OIF veterans and Vietnam veterans receiving cognitive processing therapy. Journal of Traumatic Stress. 2010;23(1):25–32. doi: 10.1002/jts.20500. [DOI] [PubMed] [Google Scholar]
- Classen C., Butler L.D., Spiegel D. Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine; 2001. A treatment manual of present-focused and trauma-focused group therapies for sexual abuse survivors at risk for HIV infection. [Google Scholar]
- Classen C.C., Palesh O.G., Cavanaugh C.E., Koopman C., Kaupp J.W., Kraemer H.C., Aggarwal R., Spiegel D. A comparison of trauma-focused and present-focused group therapy for survivors of childhood sexual abuse: A randomized controlled trial. Psychological Trauma: Theory, Research, Practice, and Policy. 2011;3(1):84–93. doi: 10.1037/a0020096. [DOI] [Google Scholar]
- Cooper-Patrick L., Powe N.R., Jenckes M.W., Gonzales J.J., Levine D.M., Ford D.E. Identification of patient attitudes and preferences regarding treatment of depression. Journal of General Internal Medicine. 1997;12(7):431–438. doi: 10.1046/j.1525-1497.1997.00075.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diener E., Emmons R.A., Larsen R.J., Griffin S. The satisfaction with life scale. Journal of Personality Assessment. 1985;49(1):71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- Evans D.L., Charney D.S., Lewis L., Golden R.N., Gorman J.M., Krishnan K.R.R., Nemeroff C.B., Bremner J.D., Carney R.M., Coyne J.C., Delong M.R., Frasure-Smith N., Glassman A.H., Gold P.W., Grant I., Gwyther L., Ironson G., Johnson R.L., Kanner A.M.…Valvo W.J. Mood disorders in the medically ill: Scientific review and recommendations. Biological Psychiatry. 2005;58(3):175–189. doi: 10.1016/j.biopsych.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Forgays D.G., Forgays D.K., Spielberger C.D. Factor structure of the State-Trait Anger Expression Inventory. Journal of Personality Assessment. 1997;69(3):497–507. doi: 10.1207/s15327752jpa6903_5. [DOI] [PubMed] [Google Scholar]
- Fortier C.B., Kenna A., Dams-O’Connor K., Fonda J., Levin L.K., Hursh C., Franz H., Milberg W.P., McGlinchey R.E. Feasibility of a skills-based group reintegration workshop for OEF/OIF veterans: STEP-Home. Journal of Head Trauma Rehabilitation. 2018;33(4):E17–E23. doi: 10.1097/HTR.0000000000000362. [DOI] [PubMed] [Google Scholar]
- Garcia H.A., Finley E.P., Ketchum N., Jakupcak M., Dassori A., Reyes S.C. A survey of perceived barriers and attitudes toward mental health care among OEF/OIF veterans at VA outpatient mental health clinics. Military Medicine. 2014;179(3):273–278. doi: 10.7205/MILMED-D-13-00076. [DOI] [PubMed] [Google Scholar]
- Harpaz-Rotem I., Rosenheck R.A. Serving those who served: Retention of newly returning veterans from Iraq and Afghanistan in mental health treatment. Psychiatric Services. 2011;62(1):22–27. doi: 10.1176/ps.62.1.pss6201_0022. [DOI] [PubMed] [Google Scholar]
- Henry J.D., Crawford J.R. The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. British Journal of Clinical Psychology. 2005;44(2):227–239. doi: 10.1348/014466505X29657. [DOI] [PubMed] [Google Scholar]
- Hoge C.W., Castro C.A., Messer S.C., McGurk D., Cotting D.I., Koffman R.L. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine. 2004;351(1):13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Hoge C.W., McGurk D., Thomas J.L., Cox A.L., Engel C.C., Castro C.A. Mild traumatic brain injury in U.S. soldiers returning from Iraq. New England Journal of Medicine. 2008;358(5):453–463. doi: 10.1056/NEJMoa072972. [DOI] [PubMed] [Google Scholar]
- Katz L.S., Cojucar G., Davenport C.T., Pedram C., Lindl C. Post-Deployment Readjustment Inventory: Reliability, validity, and gender differences. Military Psychology. 2010;22(1):41–56. doi: 10.1080/08995600903249222. [DOI] [Google Scholar]
- Lippa S.M., Fonda J.R., Fortier C.B., Amick M.A., Kenna A., Milberg W.P., McGlinchey R.E. Deployment-related psychiatric and behavioral conditions and their association with functional disability in OEF/OIF/OND veterans. Journal of Traumatic Stress. 2015;28(1):25–33. doi: 10.1002/jts.21979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panangala S.V. Congressional Research Service; 2018. The Veterans Choice Program (VCP): Program implementation. [Google Scholar]
- Reger M.A., Stanley I.H., Joiner T.E. Suicide mortality and coronavirus disease 2019—A perfect storm? JAMA Psychiatry. 2020;77(11):1093–1094. doi: 10.1001/jamapsychiatry.2020.1060. [DOI] [PubMed] [Google Scholar]
- Sayer N.A., Frazier P., Orazem R.J., Murdoch M., Gravely A., Carlson K.F., Hintz S., Noorbaloochi S. Military to Civilian Questionnaire: A measure of postdeployment community reintegration difficulty among veterans using Department of Veterans Affairs medical care. Journal of Traumatic Stress. 2011;24(6):660–670. doi: 10.1002/jts.20706. [DOI] [PubMed] [Google Scholar]
- Sayer N.A., Friedemann-Sanchez G., Spoont M., Murdoch M., Parker L.E., Chiros C., Rosenheck R. A qualitative study of determinants of PTSD treatment initiation in veterans. Psychiatry. 2009;72(3):238–255. doi: 10.1521/psyc.2009.72.3.238. [DOI] [PubMed] [Google Scholar]
- Schell T., Marshall G. In: Invisible wounds of war: Psychological and cognitive injuries, their consequences, and services to assist recovery. Tanielian T., Jaycox L.H., editors. RAND; 2008. Survey of individuals previously deployed for OEF/OIF; pp. 87–115. [Google Scholar]
- Schnurr P.P., Friedman M.J., Foy D.W., Shea M.T., Hsieh F.Y., Lavori P.W., Glynn S.M., Wattenberg M., Bernardy N.C. Randomized trial of trauma-focused group therapy for posttraumatic stress disorder: Results from a Department of Veterans Affairs Cooperative Study. Archives of General Psychiatry. 2003;60(5):481–489. doi: 10.1001/archpsyc.60.5.481. [DOI] [PubMed] [Google Scholar]
- Soble J.R., Silva M.A., Vanderploeg R.D., Curtiss G., Belanger H.G., Donnell A.J., Scott S.G. Normative data for the Neurobehavioral Symptom Inventory (NSI) and post-concussion symptom profiles among TBI, PTSD, and nonclinical samples. Clinical Neuropsychologist. 2014;28(4):614–632. doi: 10.1080/13854046.2014.894576. [DOI] [PubMed] [Google Scholar]
- Spielberger C.D. Psychological Assessment Resources; 1999. Manual for the State-Trait Anger Expression Inventory–2. [Google Scholar]
- U.S. Department of Veteran Affairs (2018, February). VA fact sheet: Telemental health in the Department of Veteran Affairs. https://www.va.gov/anywheretoanywhere/docs/TeleMental_Health_factsheet.PDF.
- Ustün T.B., Chatterji S., Kostanjsek N., Rehm J., Kennedy C., Epping-Jordan J., Saxena S., von Korff M., Pull C. Developing the World Health Organization Disability Assessment Schedule 2.0. Bulletin of the World Health Organization. 2010;88(11):815–823. doi: 10.2471/BLT.09.067231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. Psychological Corporation; 2001. Wechsler Test of Adult Reading: WTAR. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.