Abstract
Natural aquatic environments represent one of the most important vehicles of bacterial dissemination. Therefore, we aimed to isolate staphylococci from surface waters and to investigate the presence of antimicrobial resistance genes and virulence factors as well as the genetic lineages of all Staphylococcus aureus isolates. Staphylococci were recovered from water samples collected from 78 surface waters, including rivers, streams, irrigation ditches, dams, lakes, and fountains. The presence of antimicrobial resistance genes and virulence factors was investigated by PCR. Multilocus sequence typing and spa-typing were performed in all S. aureus isolates. From the 78 water samples, 33 S. aureus, one S. pseudintermedius, and 51 coagulase-negative staphylococci (CoNS) were identified. Among the S. aureus isolates, four MRSA were identified, and all harbored the mecC gene. Fourteen S. aureus were susceptible to all antimicrobials tested and the remaining showed resistance to penicillin, erythromycin and/or tetracycline encoded by the blaZ, ermT, msr(A/B), tetL, and vgaA genes. Regarding the clonal lineages, one mecC-MRSA isolate belonged to spa-type t843 and sequence type (ST) 130 and the other three to t742 and ST425. The remaining S. aureus were ascribed 14 spa-types and 17 sequence types. Eleven species of CoNS were isolated: S. sciuri, S. lentus, S. xylosus, S. epidermidis, S. cohnii spp. urealyticus, S. vitulinus, S. caprae, S. carnosus spp. Carnosus, S. equorum, S. simulans, and S. succinus. Thirteen CoNS isolates had a multidrug resistance profile and carried the following genes: mecA, msr(A/B), mph(C), aph(3′)-IIIa, aac(6′)-Ie–aph(2′’)-Ia, dfrA, fusB, catpC221, and tetK. A high diversity of staphylococci was isolated from surface waters including mecCMRSA strains and isolates presenting multidrug-resistance profiles. Studies on the prevalence of antibiotic-resistant staphylococci in surface waters are still very scarce but extremely important to estimate the contribution of the aquatic environment in the spread of these bacteria.
Keywords: Staphylococcus aureus, coagulase-negative staphylococci, MRSA, mecC, water, aquatic ecosystems, environment
1. Introduction
The incidence of antimicrobial resistant bacteria (ARB) is increasing worldwide and is becoming one of the greatest medical challenges of our time. According to a report by O’Neill (2014), if action is not taken, such as the development of new antimicrobial agents, the number of deaths caused by ARB will reach 10 million a year by 2050 exceeding the number of deaths by cancer. Furthermore, the same report showed that the economic losses caused by ARB infections will surpass 100 trillion dollars [1]. While antimicrobial resistance has existed for millions of years, the misuse and overuse of antimicrobial agents in the last decades has led to the development of multidrug-resistant bacteria some of which showing resistance to all classes of antimicrobials [2,3]. Although these superbugs are mostly found in the hospital environment, current data has shown that these bacteria can spill over from their anthropogenic sources into natural ecosystems where they can create secondary reservoirs leading to the spread of these bacteria and their resistance determinants through the environment [4]. Effluents from wastewater treatment plants, industry, hospitals and farms will eventually reach some water source making the aquatic environments a major pool for ARB and antimicrobial resistance genes (ARG) [5,6,7,8]. Water is the primary source by which ARB enter the natural ecosystems and it is also a vehicle of transportation of these bacteria. In fact, recent studies have reported the presence of ARB and ARG conferring resistance to sulfonamides, tetracyclines, quinolones and macrolides in surface waters, such as rivers, beaches, lakes, among others [9,10,11]. Lately, the ESKAPE bacteria, which includes Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa and Enterobacter spp., have been detected in habitats with anthropogenic or agricultural influence [12]. Although staphylococci are the least prevalent in water when compared to E. coli, Enterococcus and other ESKAPE pathogens, they can be used as indicators to understand the drive of antibiotic resistance in the environment [13], since they have been associated to anthropogenic activities [14,15] but are also found in environments with limited human activity [16]. Staphylococcus species are able to tolerate a wide range of temperatures, dryness, dehydration and low water activity which favors their survival in the natural environment [17]. The genus Staphylococcus is composed of at least 50 species and 24 subspecies, of which, S. aureus, S. epidermidis, S. saprophyticus and S. pseudintermedius stand out for their capacity to cause human and animal infections [18]. Some of these staphylococci species are part of the normal flora in humans and some in animal species. S. aureus is the major pathogen associated with nosocomial infections in humans. However, although coagulase-negative staphylococci (CoNS) have been considered rarely pathogenic in the past, it is now known that these strains are also frequently associated with clinical infections [17,19]. Furthermore, increasing rates of antibiotic resistance reported in both S. aureus and CoNS are concerning, particularly resistance to methicillin [20]. The genes responsible for methicillin resistance are located in a genetic locus called staphylococcal cassette chromosome mec (SCCmec) [21]. The mecA gene is the most common gene encoding resistance to methicillin. However, other genes, mecB, mecC and mecD, have been recently reported [22,23,24]. mecC is part of the SCCmec type XI and it has been mainly reported associated with S. aureus and CoNS in wildlife and environmental samples [25,26,27]. Monoresistance and multiresistance have been reported among both S. aureus and CoNS isolated from the environment, in particular in the aquatic ecosystems [21]. The presence of S. aureus and CoNS in the aquatic environment, particularly surface water and drinking water, has been reported across the globe [27,28,29,30,31,32]. However, these studies focus mainly on the prevalence and diversity of staphylococci species and most of them does not investigate the antimicrobial resistance nor the genetic lineages of these isolates. Despite the increasing interest in the aquatic environment as a source of clinically relevant ARB since surface water is one of the most relevant vehicles of bacterial dissemination, including staphylococci [27], in natural watersheds ARB are not well investigated and their potential impacts on human and animal health are not well understood [33]. Thus, in order for a better understanding the dissemination of S. aureus and CoNS in superficial water, we aimed to investigate their presence and diversity in rivers, streams, irrigation ditches, dams, lakes and fountains in Portugal. Furthermore, we also investigated the phenotypic resistance, the antimicrobial resistance genes and virulence of all isolates as well as the genetic lineages of all S. aureus isolates.
2. Results
2.1. Distribution of Staphylococci in Surface Waters
All water samples analyzed showed bacterial growth. However only 60 (76.9%) out of the 78 samples were positive for staphylococci. A total of 85 staphylococci were recovered from the water samples. The distribution of CoNS and coagulase-positive staphylococci (CoPS) among the different sources is shown in Table 1. Staphylococci were isolated from 48 lotic waters (rivers, streams, and irrigation ditches) and 12 lentic waters (dams, lakes, and fountains). CoPS were detected in 33 (42.3%) of the 78 water samples whereas CoNS were found in 42 (53.8%) samples. Only two species of CoPS were detected: S. aureus (n = 33) and S. pseudintermedius (n = 1). S. pseudintermedius isolate was recovered from water of an irrigation ditch. Regarding the CoNS, 11 species were isolated: S. sciuri (n = 28), S. lentus (n = 5), S. xylosus (n = 5), S. epidermidis (n = 4), S. cohnii spp. urealyticus (n = 2), S. vitulinus (n = 2), S. caprae (n = 1), S. carnosus spp. carnosus (n = 1), S. equorum (n = 1), S. simulans (n = 1), S. succinus (n = 1). All isolates, including the 34 CoPS and the 51 CoNS, were further characterized.
Table 1.
The distribution of CoNS and CoPS among the different water sources.
| Source | Number of Samples | Number of CoPS | Number of CoNS |
|---|---|---|---|
| Rivers | 29 | 11 | 22 |
| Streams | 19 | 6 | 14 |
| Irrigation ditches | 12 | 8 | 8 |
| Dams | 10 | 5 | 4 |
| Fountains | 4 | 1 | 1 |
| Lakes | 4 | 3 | 2 |
| Total | 78 | 34 | 51 |
2.2. Characterization of CoPS
All CoPS were characterized regarding their antimicrobial resistance profiles and virulence factors. S. aureus isolates were also typed by MLST, spa- and agr-typing (Table 2). Among the 33 S. aureus, four were methicillin-resistant S. aureus (MRSA) and all harbored the mecC gene conferring resistance to methicillin. The remaining 29 S. aureus were susceptible to cefoxitin and were categorized as methicillin-susceptible S. aureus (MSSA). Regarding the mecC-positive MRSA isolates, all were resistant to penicillin and cefoxitin and carried the blaZ-SCCmecIX which is characteristic of mecC-MRSA strains. All isolates belonged to agr III. Three out of the four mecC-positive isolates were ascribed to ST425 and spa-type t742 and one isolate belonged to ST130 and spa-type t843. Thirteen MSSA isolates were resistant to penicillin and 12 harbored the blaZ gene. Resistance to erythromycin was detected in 3 MSSA strains conferred by the ermT (n = 2), msr(A/B) and vgaA genes. One isolate also showed resistance to tetracycline and harbored the tetL gene. The remaining 14 MSSA isolates were susceptible to all antimicrobials tested. The scn gene was detected in 10 MSSA and these isolates could be ascribed to IEC system types A (n = 2), B (n = 3), C (n = 1) and D (n = 4). The great majority of the MSSA isolates harbored the virulence genes hla, hlb and hld, and the genes tst and eta genes were carried by only one isolate each. Regarding the MLST, a total of 22 STs were determined; 17 STs were identified belonging to several different CCs: ST30 (CC30), ST8 (CC8), ST617 (CC45), ST398 (CC398), ST49, ST3223, ST352 (CC97), ST425 (CC425), ST133, ST130, ST582 (CC15), and ST243 (CC30); and five new STs identified for the first time in this study: ST6832 (CC1), ST6833, ST6834, ST6835, and ST6836. MSSA isolates were also ascribed to 14 spa-types: t008 (n = 7), t098 (n = 4), t208 (n = 4), t742 (n = 2), t267 (n = 2), t4735 (n = 2), t9413 (n = 1), t350 (n = 1), t571 (n = 1), t1451 (n = 1), t8083 (n = 1), t1532 (n = 1), t1877 (n = 1) and t021 (n = 1). All agr types were detected with agr type I being the most common (n = 14), followed by type II (n = 5) and type III and IV (n = 3). Finally, the S. pseudintermedius isolate did not show phenotypic resistance to cefoxitin; however, it harbored the mecA gene. This isolate also showed resistance to erythromycin, clindamycin, and chloramphenicol and carried the catpC221 gene. None of the virulence genes tested were detected in S. pseudintermedius strain.
Table 2.
Genetic characterization and molecular typing of 33 S. aureus recovered from surface waters.
| Isolate | Water Source | Antimicrobial Resistance | Virulence Factors | Molecular Typing | ||||
|---|---|---|---|---|---|---|---|---|
| Phenotype | Genotype | IEC System | Other Genes | ST (CC) | spa | agr | ||
| VS2847 | River | PEN, FOX | blaZ-SCCmecIX | - | hld | 425 | t742 | III |
| VS2848 | River | PEN, FOX | blaZ-SCCmecIX | - | hld | 425 | t742 | III |
| VS2846 | Irrigation ditch | PEN, FOX | blaZ-SCCmecIX | - | hld | 130 | t843 | III |
| VS2849 | River | PEN, FOX | blaZ-SCCmecIX | - | hld | 425 | t742 | III |
| VS2850 | Dam | PEN | blaZ | A | hla, hlb, hld | 30 (30) | t9413 | III |
| VS2851 | Lake | PEN | blaZ | A | hla, hlb, hld | 8 (8) | t008 | I |
| VS2852 | Lake | PEN | blaZ | D | hla, hlb, hld | 8 (8) | t008 | I |
| VS2853 | Dam | PEN | blaZ | D | hla, hlb, hld | 8 (8) | t008 | I |
| VS2854 | River | PEN | blaZ | - | hla, hlb, hld | 8 (8) | t008 | I |
| VS2855 | River | PEN | blaZ | D | hla, hlb, hld | 8 (8) | t008 | I |
| VS2856 | Dam | PEN | blaZ | D | hla, hlb, hld | 8 (8) | t008 | I |
| VS2857 | Fountain | PEN | blaZ | - | hla, hlb, hld | 8 (8) | t008 | I |
| VS2858 | Dam | PEN | blaZ | B | hla, hld | 617 (45) | t350 | I |
| VS2859 | River | ERY | ermT | B | hla, hld | 398 | t571 | I |
| VS2860 | Stream | PEN, ERY | blaZ, ermT, msr(A/B) | C | hla, hld | 398 | t1451 | I |
| VS2861 | Irrigation ditch | Susceptible | - | - | hla, hlb, hld | 49 (49) | t208 | II |
| VS2862 | River | Susceptible | - | - | hla, hlb, hld | 49 (49) | t208 | II |
| VS2863 | Irrigation ditch | Susceptible | - | - | hla, hlb, hld | 49 (49) | t208 | n.d. |
| VS2864 | River | Susceptible | - | - | hla, hlb, hld | 3223 | t742 | n.d. |
| VS2865 | Irrigation ditch | Susceptible | - | - | hla, hlb, hld | 6832 (1) | t098 | III |
| VS2866 | Stream | PEN | - | - | hla, hlb, hld | 352 (97) | t267 | I |
| VS2867 | Irrigation ditch | Susceptible | - | - | hla, hlb, hld | 6833 | t098 | IV |
| VS2868 | Stream | Susceptible | - | - | hla, hlb, hld | 352 (97) | t267 | I |
| VS2869 | Irrigation ditch | Susceptible | - | - | hla, hlb | 6834 | t208 | II |
| VS2870 | Irrigation ditch | Susceptible | - | - | hla, hlb, hld | 6833 | t098 | IV |
| VS2871 | Stream | PEN, TET | blaZ, tetL | - | hla, hlb, hld, tst | 425 | t742 | II |
| VS2872 | River | Susceptible | - | - | hla, hlb, hld | 6835 | t098 | IV |
| VS2873 | River | ERY | vgaA | - | hla, hlb, hld | 133 | t4735 | I |
| VS2874 | River | Susceptible | - | - | - | 6836 | t8083 | n.d. |
| VS2875 | River | Susceptible | - | - | hla, hlb | 133 | t4735 | I |
| VS2876 | Stream | Susceptible | - | - | hla, | 130 | t1532 | III |
| VS2877 | Dam | PEN | blaZ | B | hla, hld, eta | 582 (15) | t1877 | II |
| VS2878 | Lake | Susceptible | - | - | - | 243 (30) | t021 | n.d. |
Abbreviations. PEN: penicillin, FOX: cefoxitin, ERY: erythromycin, n.d. not determined, ST: sequence type (by MLST).
2.3. Characterization of CoNS
The presence of resistance genes and virulence factors were investigated in all CoNS isolates and the phenotypic and genotypic results are shown in Table 3. All isolates were screened for the presence of the mecA gene even when they were not showing phenotypic resistance to cefoxitin. Out of the 51 isolates, 48 (94.1%) harbored the mecA gene. Phenotypic resistance to penicillin was found in 20 (39.2%) CoNS; however, the blaZ gene was not detected in any of them. S. sciuri (n = 28) was the most common species of staphylococci isolated from surface waters. These isolates also showed resistance to clindamycin and fusidic acid and carried the ermT and msr(A/B) genes. Sixteen S. sciuri isolates were susceptible to all antibiotics tested. S. lentus and S. xylosus isolates (one of each) showed resistance to tetracycline and carried the tetK gene. Two S. lentus isolates were also resistant to clindamycin and harbored the msr(A/B) and mph(C) genes. Four strains of S. epidermidis were isolated from water samples. Two of these isolates had a multidrug-resistant profile showing resistance to at least four antimicrobial classes. Consequently, a high diversity of resistance genes were detected among these isolates, namely, mecA (resistance to methicillin), msr(A/B) and mph(C) (resistance to macrolides and licosamides), aac(6′)-Ie–aph(2′’)-Ia and aph(3′)-IIIa (resistance to aminoglicosides), dfrA and fusB (resistance to trimethoprim-sulfamethoxazole), and catpC221 (resistance to chloramphenicol). Two S. cohnii spp. urealyticus and two S. vitulinus isolates were also recovered from water samples all carrying the mecA gene. One of the S. cohnii spp. urealyticus isolates also showed resistance to clindamycin and erythromycin and harbored the msr(A/B) and mph(C) genes. One isolate of each species (S. caprae, S. succinus, S. carnosus spp. carnosus, S. equorum and S. simulans) was also recovered from surface waters and all, except S. simulans, carried the mecA gene. The virulence genes tested were absent in the almost all isolates with the exception of 2 S. sciuri strains which carried the hld gene.
Table 3.
Species identification, resistance genes, and virulence factors identified among the CoNS isolated from surface water.
| Species | Number of Isolates | Antimicrobial Resistance | Virulence | |
|---|---|---|---|---|
| Phenotype | Genotype | |||
| S. sciuri | 28 | PEN 12, CD 9, FD 11 | MecA 27, ermT 2, msr(A/B) 2 | Hld 2 |
| S. lentus | 5 | PEN 2, CD 2, TET 1 | MecA 5, msr(A/B) 1, mph(C) 2, tetK 1 | - |
| S. xylosus | 5 | PEN 1, CD 1, TET 1 | MecA 4, tetK 1 | - |
| S. epidermidis | 4 | PEN 3, FOX 2, CIP 1, LNZ 1, CN 2, TOB 2, KAN 2, ERY 1, CD 2, C 1, FD 1, SXT 1 | MecA 4, aac(6′)-Ie–aph(2′’)-Ia 1, aph(3’)-IIIa 2, msr(A/B) 3, mph(C) 2, catpC221 1, fusB 1, dfrA 1 | - |
| S. cohnii spp. urealyticus | 2 | PEN 2, ERY 1, CD 1, FD 1 | MecA 2, msr(A/B), mph(C) | - |
| S. vitulinus | 2 | Susceptible | mecA2 | - |
| S. caprae | 1 | FD | mecA | - |
| S. succinus | 1 | Susceptible | mecA | - |
| S. carnosus spp. carnosus | 1 | Susceptible | mecA | - |
| S. equorum | 1 | Susceptible | mecA | - |
| S. simulans | 1 | Susceptible | - | - |
Note: the superscript number after each antibiotic and gene indicates the number of strains showing resistance to that antibiotic and harboring that gene, respectively. Abbreviations. C: chloramphenicol; CD: clindamycin; CN: gentamycin; CIP: ciprofloxacin; ERY: erythromycin; FD, fusidic acid; KAN: kanamycin; LNZ: linezolid; PEN: penicillin; SXT: trimethoprim-sulfamethoxazole; TET: tetracycline; TOB: tobramycin.
3. Discussion
Surface waters are one of the most relevant vehicles of bacterial dissemination [34]. Studies have shown the presence of staphylococci in rivers, fresh water and seawater [28,35,36]. In our study, we collected a total of 78 surface water samples and recovered 85 staphylococci from 60 (76.9%) samples. These results are comparable with the results obtained by a similar study conducted in Spain in which 89.4% of the surface water samples were positive for staphylococci [21] and in Hawai‘i where 98.1% were positive for Staphylococcus spp. [16]. In fact, studies have shown that staphylococci have the ability to survive in water environments for several days [35,37]. Furthermore, Faria et al. showed that CoNS are able to survive wastewater treatment and have been frequently detected in treated effluents [38]. In our study, 42.9% of water samples were positive for S. aureus, a high value obtained by Gerken et al. in 162 river/stream and anchialine pools samples in Hawai‘I (8.1%). Hatcher et al. evaluated the presence of S. aureus and other non-aureus staphylococci in 183 surface water samples recovered from nine locations near a swine lagoon spray fields and isolated 24 (13.1%) S. aureus which is also a lower prevalence than that obtained in this study. In the same study, 155 non-aureus staphylococci were recovered from water samples belonging to 10 different species and S. epidermidis was the most common species followed by S. warneri and S. saprophyticus [31]. In contrast, in our study, the most common species found was S. sciuri followed by S. lentus and S. xylosus. Nevertheless, S. epidermidis and S. saprophyticus are usually associated with human and animal infections while staphylococci belonging to the S. sciuri group, which includes the species S. sciuri, S. vitulinus, S. lentus, S. fleurettii and S. stepanovicci, are considered more opportunistic than primary pathogens [39]. In fact, in the study by Heß and Gallert, the prevalence of staphylococci was investigated in sewage and in river waters and it was noted that the prevalence of S. saprophyticus was higher than S. sciuri group strains in sewage, but the percentage of S. saprophyticus decreased in favor of S. sciuri group isolates in river water [29].
Thirty-three (42.9%) surface water samples were positive for CoPS with only water sample carrying both one S. aureus and one S. pseudintermedius. Among the 33 S. aureus strains recovered from 33 different water samples, four (12.1%) mecC-positive MRSA were identified. Three of the four isolates belonged to ST425 (CC425) and spa-type t742 and one isolate belonged to ST130 (CC130) and t843. MRSA strains carrying the mecC gene were first report in 2011 in MRSA isolates from human samples in Ireland [24]. Since then, many studies have reported the presence of these gene in MRSA strains often associated with wild animals [40,41,42]. In Portugal, mecC-MRSA has been previously reported in only one study conducted by our team in wild rodents [40]. Nevertheless, the mecC-positive isolates were ascribed to a different ST and spa-type (ST1945 and t1535) than those found in this study. Therefore, this is the first report of both mecC-MRSA in environmental samples and mecC-positive strains belonging to ST425-t742 and ST130-t843 in Portugal. S. aureus CC130 have been widely reported among livestock. However, recently, MRSA CC130 has been repeatedly isolated from wild animals and humans and generally associated with the mecC gene [40,43]. In fact, MRSA CC130 and primarily spa-type t843 are most commonly reported type of mecC-MRSA in both humans and animals [42]. It has been suggested that mecC-MRSA arose from animals since both ST130 and ST425 has been regarded as one of the animal-adapted lineages of S. aureus [43]. MRSA ST425 is also one of the most common lineages of mecC-positive strains [44]. As far as we know, among the many studies conducted in environmental samples, including surface waters, only one study reported the presence of a mecC-MRSA strains [27]. In that study by Porrero et al., 3 mecC-MRSA were recovered from river water and all belonged to ST425 and spa-type t11212. The same authors have reported the same genetic lineage in mecC-MRSA strains recovered from wild animals in the same area and suggested a possible transmission of bacteria between wildlife and the water environment [45]. Nevertheless, since our study is the second report of mecC in environmental water samples and most of our isolates belong to ST425, we can suggest that perhaps this lineage of mecC-MRSA is associated with natural aquatic systems. As expected, all mecC-MRSA isolates showed resistance to β-lactams and they all carried to the blaZ allotype associated with SCCmec XI (blaZ-SCCmecXI) as already reported in other similar isolates [40,44]. Our mecC-MRSA isolates were negative for PVL, tst and IEC genes. Although these results are in accordance with the studies conducted in mecC-MRSA strains belonging to CC130 and CC425 [46,47,48].
There was a high diversity of genetic lineages among the MSSA isolates. Seven isolates belonged to ST8 (CC8) and spa-type t008 which was the most common lineage. These strains were collected from almost all water sources investigated in this study, including a public fountain. S. aureus ST8-t008 are highly related with the community acquired MRSA (CA-MRSA) epidemic clone USA300 [49]. Epidemiologic studies have identified S. aureus ST8-t008 has a common clone circulating in both North America and Europe [50,51]. However, unlike our isolates, USA300 isolates are PVL-positive [52]. MRSA and MSSA ST8, usually related with t008, has been isolated from river water in Austria [28] and surface water and seawater in the United States [14,31,53]. Three of our isolates belonged to ST49 and t208. This particular clone is commonly associated with pigs, disease wild squirrels and other wild animals [41,54,55,56]. Although CC49 isolates are rare in other hosts this clone have been reported among humans, horses and urban effluents [57,58,59]. The spa-type t208 is usually associated with ST49. In our study, one isolate ascribed to t208 belonged to the new ST6834 which is a single-locus variant of ST49 that differs by only 1 nucleotide base within the tpi gene. Ten of the 29 MSSA isolates were IEC-positive suggesting a possible human origin [60] with the following ST pairings observed: A in ST30 (n = 1) and ST8 (n = 1), B in ST617 (n = 1), ST398 (n = 1) and ST582 (n = 1), C in ST398 (n = 1) and D in ST8 (n = 4). IEC types B and D are more common in agr I isolates whereas type A is frequently associated with agr III isolates which is in accordance with our results [61]. Two MSSA-CC398 isolates were ascribed to IEC types B and C and typed as t571 and t1451, respectively. MSSA-CC398 strains carrying the IEC genes are scarce out of the human niche suggesting a spread of this clone from humans to the environment [62]. Nevertheless, they have been isolated from pigs and equids [61,62]. It is important to point out that, although none of the ST398 isolates were recovered from dams’ water, half of the strains carrying the IEC genes were isolated from this source. Many dams in Portugal are used as water reservoirs for drinking and for recreational activities such as swimming. Studies have suggested that bathers in recreational waters may influence the prevalence of staphylococci in those waters [53]. Furthermore, recreational use of water may represent an entry of staphylococci particularly in lakes and freshwater recreational beaches [63], although only a few studies investigated the genetic lineages of MRSA and MSSA isolated from water. A high diversity of STs and spa-types was reported, and many coincide with those obtained in this study. MRSA and MSSA belonging to CC133, CC425, CC15, CC30 and CC45 have been isolated from surface water and freshwater in the US and Spain [14,21,31,35]. However, most the isolates belonging to these CCs were ascribed to different spa-types of those obtained in our study. Other STs and spa-types identified in our study are frequently associated with livestock and humans [64,65,66,67]. In fact, many streams and irrigation ditches were located near cattle grazing lands. Tetracycline resistance is usually a marker of livestock-associated S. aureus. However, in our study, only one MSSA isolate showed resistance to tetracycline conferred by the tetL gene. This particular isolate was ST425-t742 and belonged to agr type II, unlike the mecC-positive ST425-t742 isolates which belonged to agr III. MSSA ST3223 was only reported in a study conducted in wild boars from the same region of the surface waters collected in this study [68]. Five new STs were detected in this study among five isolates. ST6832 differs from ST1 by one-point mutation on the arcC locus and belongs to CC1. ST6833 and ST6835 also vary from ST1956 by a single point mutation. Isolates belonging to ST6832, ST6833 and ST6835 were ascribed to spa-type t098. Strains belonging to t098 have been reported among humans and wild animals and usually associated with ST1 [69,70,71]. One isolate was ascribed to the new ST6834 and spa-type t208. ST6834 is a single-locus variant of ST49 which is commonly associated with spa-type t208 and has been detected in pigs and wild squirls [72,73]. Finally, the new ST6836 differs from ST2049 by one-point mutation on the aroE locus. S. aureus isolates belonging to ST2049 have been reported in freshwater sites in the USA [35].
All mecA-positive strains detected in our study were CoNS. Forty-eight (94.1%) of the 51 CoNS isolates harbored the mecA gene which is a very high prevalence when compared to similar researches [21,29,74]. Studies have reported the presence of a wide diversity of staphylococci in surface waters [21,29]. Susceptibility to cefoxitin among the mecA-carrying isolates may be due to the presence of dormant gene which are inactive in vitro [75]. In our study, 11 species of staphylococci were identified. Staphylococci belonging to the S. sciuri group were the most prevalent. It has been suggested that the S. sciuri group is the evolutionary precursor of the mecA gene since homologues of this gene have been found in S. sciuri group species [25]. These staphylococci are part of the microbiota of many animals and very infrequently cause disease [39]. Heß and Gallert reported similar results. Contrary, in other studies S. epidermidis was the most common species in surface water [21,31]. A study conducted with drinking water samples reported S. warneri as the most prevalent species [75]. From the few studies investigating the presence of CoNS in aquatic systems, S. warneri have been isolated in all, except one, which suggests that natural water may be a reservoir of this staphylococci species [21,29,31,74,75,76]. Nevertheless, no S. warneri was isolated in our study. Twenty-six (50.1%) of the 51 CoNS isolates were susceptible to all antibiotics tested, 9 (17.6%) isolates were resistant to one or two classes of antimicrobials and 16 (31.4%) were multidrug-resistant. In the study by Gomez et al., the diversity and antimicrobial resistance of CoNS isolated from surface waters was evaluated and a higher incidence of 23.7% of multidrug-resistant staphylococci was identified [21]. Antimicrobial resistance was more common in clinically important isolates. Two of the four S. epidermidis, one isolated from a stream and other from an irrigation ditch, showed resistance to 4 and 8 antimicrobial classes, respectively. This is concerning since, unlike most CoNS, S. epidermidis is an important nosocomial opportunist pathogen [75].
In this study, the majority of surface water samples (more than 75%) carried staphylococci. Unlike E. coli and Enterococcus spp. which are indicators of fecal contamination, staphylococci are present in the skin and mucous membranes of humans and several animal species and so it does not need the shed of feces to spread through the environment [13,25]. Nevertheless, some S. aureus isolated in this study showed a probable human origin indicating a possible human contamination. Some areas where water samples were collected were remote and there were no livestock nearby which suggests that either the staphylococci present in those samples had come from wild animals or they may present in the natural environment without the need of prior contamination. Nevertheless, animals and humans using these waters for recreational activities or dinking may be affected by staphylococci infections or colonization. However, there is limited information on the link between staphylococci-contaminated waters and the onset of human infections [14].
4. Materials and Methods
4.1. Study Area
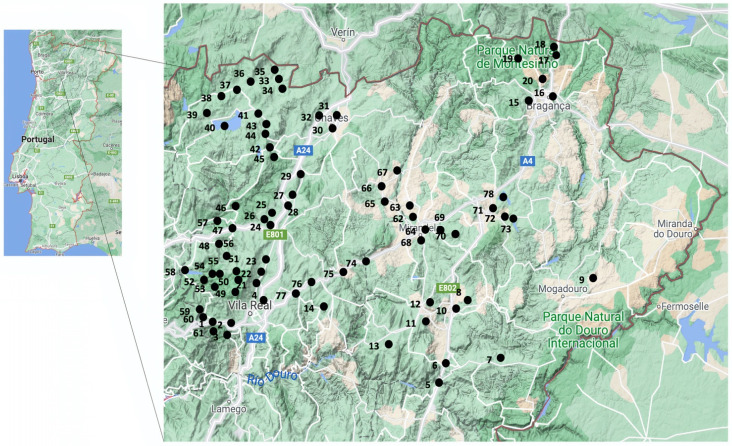
Seventy-eight locations were sampled across the Trás-os-Montes and Alto Douro region in Portugal (Figure 1). All rivers and streams sampled belonged to the Douro River Basin. This is an international hydrographic region with a total area of about 79,000 km2, of which 19,000 km2 are located in Portugal. This watershed starts and is delimited by Spain to the east, and by the Atlantic Ocean to the west.
Figure 1.
Sampling locations of surface waters across the Trás-os-Montes and Alto Douro region. Each number correspond to the number of water sample in Table S1.
4.2. Sample Collection
Between September and November 2019, 78 water samples were collected from surface waters including: 29 rivers, 19 streams, 12 irrigation ditches, 10 dams (water reservoirs), 4 fountains, and 4 lakes (Supplementary Materials: Table S1). Water was sampled into sterile 500 mL plastic bottles with sodium thiosulfate and preserved at 4–8 °C. All samples were filtered on the same day they were collected.
4.3. Bacterial Isolation
Water samples were filtered through a cellulose nitrate 0.45 μm pore membrane filter (Whatman, UK). The filters were then inserted into tubes containing 5 mL of BHI (Brain Heart Infusion) broth supplemented with 6.5% of NaCl and incubated at 37 °C for 24 h. After the incubation period, the inoculum was seeded onto Mannitol Salt agar and Baird-Parker agar plates for staphylococci and S. aureus isolation and onto ORSAB plates with 2 mg/L of oxacillin for MRSA and MRS isolation. The plates were incubated for 24 h at 37 °C. Up to 4 colonies presenting different morphological characteristics were recovered from each plate and further identified by biochemical methods, such as DNase, coagulase, and catalase tests. The species identification of all isolates was carried out by MALDI-TOF (Bruker Daltonics, Bremen, Germany).
4.4. Antimicrobial Susceptibility Testing
Antimicrobial susceptibility testing was performed by agar disk diffusion according to the EUCAST guidelines with the exception of kanamycin that followed the CLSI. S. aureus ATCC® 25923 was the quality control strain. The following 14 antimicrobials were used: cefoxitin (30 μg), chloramphenicol (30 μg), ciprofloxacin (5 μg), clindamycin (2 μg), erythromycin (15 μg), fusidic acid (10 μg), gentamicin (10 μg), kanamycin (30 μg), linezolid (10 μg), mupirocin (200 μg), penicillin (1 U), tetracycline (30 μg), tobramycin (10 μg), and trimethoprim/sulfamethoxazole (1.25/23.75 μg). Isolates were considered multidrug-resistant if they had resistance to three or more structurally unrelated antimicrobials.
4.5. Antimicrobial Resistance Genes and Virulence Factors
For DNA extraction, isolates were grown on BHI agar and incubated at 37 °C for 18–24 h. After the incubation, the bacterial cells were enzymatically lysed as previously described [77]. The extracted DNA was stored in a freezer at −20 °C until used. Methicillin resistance was confirmed by PCR with primers targeting the mecA and mecC genes as previously described [78,79]. All isolates were screened for the presence antimicrobial resistance genes according to their phenotypic resistance. The presence of antimicrobial resistant genes encoding resistance to penicillin (blaZ and blaZ-SCCmecXI), macrolides and lincosamides (ermA, ermB, ermC, ermT, mphC, msr(A/B), lnuA, lnuB, vgaA and vgaB), aminoglycosides (aac(6’)-Ie-aph(2’’)-Ia, aph(3’)-IIIa, ant(4’)-Ia and str), fusidic acid (fusA, fusB, fusC and fusD), tetracyclines (tetM, tetL, tetK and tetO), chloramphenicol (fexA, fexB, catpC194, catpC221 and catpC223), trimethoprim/sulfamethoxazole (dfrA, dfrD, dfrG and dfrK) and linezolid (cfr) was investigated by PCR as described elsewhere [80]. S. aureus strains were tested by PCR for lukF/lukS-PV encoding Panton-Valentine Leukocidin. All isolates were screened for the presence of virulence genes encoding alpha-, beta- and delta-hemolysins (hla, hlb and hld), exfoliative toxins (eta, etb and etd2) and toxic shock syndrome toxin (tst) [80]. The presence of scn gene was investigated in all S. aureus isolates since it is a marker of the immune evasion cluster (IEC) system and is common to all IEC groups. If the presence of scn genes was confirmed, the presence of the chp, sak, sea and sep genes was studied to determine the IEC group [81]. Positive and negative controls used in all experiments belonged to the strain collection of the University of Trás-os-Montes and Alto Douro.
4.6. Molecular Typing
All S. aureus isolates were typed by multilocus sequence typing (MLST), spa- and agr-typing. MLST was performed by amplification and sequencing the internal fragments of seven housekeeping genes (arcC, aroE, glpF, gmk, pta, tpi, and yqiL) as previously described [82]. The sequence types (ST) were obtained by comparing the allelic profile of each isolate to the MLST database (https://pubmlst.org, accessed on 31 August 2021). spa typing was performed by amplifying the polymorphic X region of the spa gene and the obtained sequences were analyzed using Ridom® Staph-type software (version 1.5, Ridom GmbH, Würzburg, Germany) [83]. Isolates were characterized by agr-typing (I–IV) by PCR using specific primers and conditions [84].
5. Conclusions
In this study, the presence of staphylococci was equally distributed among rivers, streams, irrigation ditches, dams (water reservoirs), lakes, and fountains. A high diversity of clonal lineages of S. aureus was isolated from different sources of surface water, including two genetic lineages of mecC-MRSA (ST425-t742 and ST130-t843) reported for the first time in Portugal. Furthermore, 11 species of CoNS were also isolated from water samples. Most staphylococci showed resistance to one or two antimicrobial agents but some isolates, such as S. epidermidis, showed resistance to several classes of antibiotics. This is of particular concern since many of these antimicrobial classes are applied to treat both human and animal infections. Antimicrobials used in hospitals, veterinary medicine, and residues from industries may be introduced into the natural environment reaching surface waters, causing selective pressure on microbial communities leading to the development and spread of antimicrobial resistance. The resistance situation in aquatic environments was rarely investigated and continuous surveillance of antimicrobial resistant bacteria in surface waters used for recreational or domestic purposes is needed.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/antibiotics10111416/s1, Table S1: Origin, source, and location of the 78 surface waters samples recovered in this study and respective isolates.
Author Contributions
Conceptualization, V.S.; methodology, V.S.; validation, V.S., M.T.T.-J., M.C. and P.P.; investigation, V.S., V.M. and L.R.; resources, V.S. and A.S.; data curation, E.F., V.M. and L.R.; writing—original draft preparation, V.S.; writing—review and editing, V.S., M.C. and P.P.; supervision, J.L.C., G.I. and P.P. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded by the R&D Project CAREBIO2: Comparative assessment of antimicrobial resistance in environmental biofilms through proteomics—towards innovative theranostic biomarkers, with reference NORTE-01-0145-FEDER-030101 and PTDC/SAU-INF/30101/2017, financed by the European Regional Development Fund (ERDF) through the Northern Regional Operational Program (NORTE 2020) and the Foundation for Science and Technology (FCT). This work was supported by the Associate Laboratory for Green Chemistry-LAQV, which is financed by national funds from FCT/MCTES (UIDB/50006/2020 and UIDP/50006/2020) and by CITAB (UIDB/04033/2020). Vanessa Silva is grateful to FCT (Fundacão para a Ciência e a Tecnologia) for financial support through the PhD grant SFRH/BD/137947/2018.
Data Availability Statement
Data is contained within the article or supplementary material.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.O’Neill J. Antimicrobial Resistance: Tackling a Crisis for the Health and Wealth of Nations: December 2014; Review on Antimicrobial Resistance. 2014. [(accessed on 31 August 2021)]. Available online: https://wellcomecollection.org/works/rdpck35v.
- 2.Swift B.M.C., Bennett M., Waller K., Dodd C., Murray A., Gomes R.L., Humphreys B., Hobman J.L., Jones M.A., Whitlock S.E., et al. Anthropogenic environmental drivers of antimicrobial resistance in wildlife. Sci. Total Environ. 2019;649:12–20. doi: 10.1016/j.scitotenv.2018.08.180. [DOI] [PubMed] [Google Scholar]
- 3.Davies J., Davies D. Origins and evolution of antibiotic resistance. Microbiol. Mol. Biol. Rev. 2010;74:417–433. doi: 10.1128/MMBR.00016-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dolejska M., Literak I. Wildlife Is Overlooked in the Epidemiology of Medically Important Antibiotic-Resistant Bacteria. Antimicrob. Agents Chemother. 2021;63:e01167-19. doi: 10.1128/AAC.01167-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang Y., Song W., Lin H., Wang W., Du L., Xing W. Antibiotics and antibiotic resistance genes in global lakes: A review and meta-analysis. Environ. Int. 2018;116:60–73. doi: 10.1016/j.envint.2018.04.011. [DOI] [PubMed] [Google Scholar]
- 6.Khan N.A., Ahmed S., Farooqi I.H., Ali I., Vambol V., Changani F., Yousefi M., Vambol S., Khan S.U., Khan A.H. Occurrence, sources and conventional treatment techniques for various antibiotics present in hospital wastewaters: A critical review. TrAC Trends Anal. Chem. 2020;129:115921. doi: 10.1016/j.trac.2020.115921. [DOI] [Google Scholar]
- 7.Senta I., Krizman-Matasic I., Terzic S., Ahel M. Comprehensive determination of macrolide antibiotics, their synthesis intermediates and transformation products in wastewater effluents and ambient waters by liquid chromatography–tandem mass spectrometry. J. Chromatogr. A. 2017;1509:60–68. doi: 10.1016/j.chroma.2017.06.005. [DOI] [PubMed] [Google Scholar]
- 8.Yang Y., Liu Z., Xing S., Liao X. The correlation between antibiotic resistance gene abundance and microbial community resistance in pig farm wastewater and surrounding rivers. Ecotoxicol. Environ. Saf. 2019;182:109452. doi: 10.1016/j.ecoenv.2019.109452. [DOI] [PubMed] [Google Scholar]
- 9.Yang Y., Xu C., Cao X., Lin H., Wang J. Antibiotic resistance genes in surface water of eutrophic urban lakes are related to heavy metals, antibiotics, lake morphology and anthropic impact. Ecotoxicology. 2017;26:831–840. doi: 10.1007/s10646-017-1814-3. [DOI] [PubMed] [Google Scholar]
- 10.Sabri N.A., Schmitt H., Van der Zaan B., Gerritsen H.W., Zuidema T., Rijnaarts H.H.M., Langenhoff A.A.M. Prevalence of antibiotics and antibiotic resistance genes in a wastewater effluent-receiving river in the Netherlands. J. Environ. Chem. Eng. 2020;8:102245. doi: 10.1016/j.jece.2018.03.004. [DOI] [Google Scholar]
- 11.Garner E., Benitez R., von Wagoner E., Sawyer R., Schaberg E., Hession W.C., Krometis L.-A.H., Badgley B.D., Pruden A. Stormwater loadings of antibiotic resistance genes in an urban stream. Water Res. 2017;123:144–152. doi: 10.1016/j.watres.2017.06.046. [DOI] [PubMed] [Google Scholar]
- 12.Savin M., Bierbaum G., Hammerl J.A., Heinemann C., Parcina M., Sib E., Voigt A., Kreyenschmidt J. Antibiotic-resistant bacteria and antimicrobial residues in wastewater and process water from German pig slaughterhouses and their receiving municipal wastewater treatment plants. Sci. Total Environ. 2020;727:138788. doi: 10.1016/j.scitotenv.2020.138788. [DOI] [PubMed] [Google Scholar]
- 13.Finley R.L., Collignon P., Larsson D.G.J., McEwen S.A., Li X.-Z., Gaze W.H., Reid-Smith R., Timinouni M., Graham D.W., Topp E. The Scourge of Antibiotic Resistance: The Important Role of the Environment. Clin. Infect. Dis. 2013;57:704–710. doi: 10.1093/cid/cit355. [DOI] [PubMed] [Google Scholar]
- 14.Thapaliya D., Hellwig E.J., Kadariya J., Grenier D., Jefferson A.J., Dalman M., Kennedy K., DiPerna M., Orihill A., Taha M., et al. Prevalence and Characterization of Staphylococcus aureus and Methicillin-Resistant Staphylococcus aureus on Public Recreational Beaches in Northeast Ohio. GeoHealth. 2017;1:320–332. doi: 10.1002/2017GH000106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zieliński W., Korzeniewska E., Harnisz M., Hubeny J., Buta M., Rolbiecki D. The prevalence of drug-resistant and virulent Staphylococcus spp. in a municipal wastewater treatment plant and their spread in the environment. Environ. Int. 2020;143:105914. doi: 10.1016/j.envint.2020.105914. [DOI] [PubMed] [Google Scholar]
- 16.Gerken T.J., Roberts M.C., Dykema P., Melly G., Lucas D., De Los Santos V., Gonzalez J., Butaye P., Wiegner T.N. Environmental Surveillance and Characterization of Antibiotic Resistant Staphylococcus aureus at Coastal Beaches and Rivers on the Island of Hawai’i. Antibiotics. 2021;10:980. doi: 10.3390/antibiotics10080980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Silva V., Caniça M., Capelo J.L., Igrejas G., Poeta P. Diversity and genetic lineages of environmental staphylococci: A surface water overview. FEMS Microbiol. Ecol. 2020;96:fiaa191. doi: 10.1093/femsec/fiaa191. [DOI] [PubMed] [Google Scholar]
- 18.Gherardi G., Di Bonaventura G., Savini V. Staphylococcal Taxonomy. Elsevier Inc.; Amsterdam, The Netherlands: 2018. [Google Scholar]
- 19.Kim E., Kim H.-J., Yang S.-M., Kim C.-G., Choo D.-W., Kim H.-Y. Rapid Identification of Staphylococcus Species Isolated from Food Samples by Matrix-Assisted Laser Desorption/Ionization Time-of-Flight Mass Spectrometry. J. Microbiol. Biotechnol. 2019;29:548–557. doi: 10.4014/jmb.1901.01046. [DOI] [PubMed] [Google Scholar]
- 20.May L., Klein E.Y., Rothman R.E., Laxminarayan R. Trends in antibiotic resistance in coagulase-negative staphylococci in the United States, 1999 to 2012. Antimicrob. Agents Chemother. 2014;58:1404–1409. doi: 10.1128/AAC.01908-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gómez P., Casado C., Sáenz Y., Ruiz-Ripa L., Estepa V., Zarazaga M., Torres C. Diversity of species and antimicrobial resistance determinants of staphylococci in superficial waters in Spain. FEMS Microbiol. Ecol. 2017:93. doi: 10.1093/femsec/fiw208. [DOI] [PubMed] [Google Scholar]
- 22.Becker K., van Alen S., Idelevich E.A., Schleimer N., Seggewiß J., Mellmann A., Kaspar U., Peters G. Plasmid-Encoded Transferable mecB-Mediated Methicillin Resistance in Staphylococcus aureus. Emerg. Infect. Dis. 2018;24:242–248. doi: 10.3201/eid2402.171074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lakhundi S., Zhang K. Methicillin-Resistant Staphylococcus aureus: Molecular Characterization, Evolution, and Epidemiology. Clin. Microbiol. Rev. 2018;31:e00020-18. doi: 10.1128/CMR.00020-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shore A.C., Deasy E.C., Slickers P., Brennan G., O’Connell B., Monecke S., Ehricht R., Coleman D.C. Detection of staphylococcal cassette chromosome mec type XI carrying highly divergent mecA, mecI, mecR1, blaZ, and ccr genes in human clinical isolates of clonal complex 130 methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 2011;55:3765–3773. doi: 10.1128/AAC.00187-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Silva V., Capelo J.L., Igrejas G., Poeta P. Molecular Epidemiology of Staphylococcus aureus Lineages in Wild Animals in Europe: A Review. Antibiotics. 2020;9:122. doi: 10.3390/antibiotics9030122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.MacFadyen A.C., Harrison E.M., Ellington M.J., Parkhill J., Holmes M.A., Paterson G.K. A highly conserved mecC-encoding SCCmec type XI in a bovine isolate of methicillin-resistant Staphylococcus xylosus. J. Antimicrob. Chemother. 2018;73:3516–3518. doi: 10.1093/jac/dky333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Porrero M.C., Harrison E., Fernández-Garayzábal J.F., Paterson G.K., Díez-Guerrier A., Holmes M.A., Domínguez L. Detection of mecC-Methicillin-resistant Staphylococcus aureus isolates in river water: A potential role for water in the environmental dissemination. Environ. Microbiol. Rep. 2014;6:705–708. doi: 10.1111/1758-2229.12191. [DOI] [PubMed] [Google Scholar]
- 28.Lepuschitz S., Mach R., Springer B., Allerberger F., Ruppitsch W. Draft Genome Sequence of a Community-Acquired Methicillin-Resistant Staphylococcus aureus USA300 Isolate from a River Sample. Genome Announc. 2017;5:e01166-17. doi: 10.1128/genomeA.01166-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Heß S., Gallert C. Demonstration of staphylococci with inducible macrolide–lincosamide–streptogramin B (MLSB) resistance in sewage and river water and of the capacity of anhydroerythromycin to induce MLSB. FEMS Microbiol. Ecol. 2014;88:48–59. doi: 10.1111/1574-6941.12268. [DOI] [PubMed] [Google Scholar]
- 30.Ramessar K., Olaniran A.O. Antibiogram and molecular characterization of methicillin-resistant Staphylococcus aureus recovered from treated wastewater effluent and receiving surface water in Durban, South Africa. World J. Microbiol. Biotechnol. 2019;35:142. doi: 10.1007/s11274-019-2715-9. [DOI] [PubMed] [Google Scholar]
- 31.Hatcher S.M., Myers K.W., Heaney C.D., Larsen J., Hall D., Miller M.B., Stewart J.R. Occurrence of methicillin-resistant Staphylococcus aureus in surface waters near industrial hog operation spray fields. Sci. Total Environ. 2016;565:1028–1036. doi: 10.1016/j.scitotenv.2016.05.083. [DOI] [PubMed] [Google Scholar]
- 32.Sood A., Pandey P., Bisht S., Sharma S. Anthropogenic activities as a source of high prevalence of antibiotic resistant Staphylococcus aureus in the River Ganga. Appl. Ecol. Env. Res. 2014;12:33–48. doi: 10.15666/aeer/1201_033048. [DOI] [Google Scholar]
- 33.Cho S., Jackson C.R., Frye J.G. The prevalence and antimicrobial resistance phenotypes of Salmonella, Escherichia coli and Enterococcus sp. in surface water. Lett. Appl. Microbiol. 2020;71:3–25. doi: 10.1111/lam.13301. [DOI] [PubMed] [Google Scholar]
- 34.Gómez P., González-Barrio D., Benito D., García J.T., Viñuela J., Zarazaga M., Ruiz-Fons F., Torres C. Detection of methicillin-resistant Staphylococcus aureus (MRSA) carrying the mecC gene in wild small mammals in Spain. J. Antimicrob. Chemother. 2014;69:2061–2064. doi: 10.1093/jac/dku100. [DOI] [PubMed] [Google Scholar]
- 35.Levin-Edens E., Soge O.O., No D., Stiffarm A., Meschke J.S., Roberts M.C. Methicillin-resistant Staphylococcus aureus from Northwest marine and freshwater recreational beaches. FEMS Microbiol. Ecol. 2012;79:412–420. doi: 10.1111/j.1574-6941.2011.01229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Akanbi O.E., Njom H.A., Fri J., Otigbu A.C., Clarke A.M. Antimicrobial susceptibility of Staphylococcus aureus isolated from recreational waters and beach sand in Eastern Cape Province of South Africa. Int. J. Environ. Res. Public Health. 2017;14:1001. doi: 10.3390/ijerph14091001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moore J.E., Moore R.E., Shteinberg M., Kis-Papo T., Millar B.C. Survival of Mycobacterium abscessus and Staphylococcus aureus in saline waters of the Dead Sea: Implications for health tourists. J. Travel Med. 2020 doi: 10.1093/jtm/taaa089. [DOI] [PubMed] [Google Scholar]
- 38.Faria C., Vaz-Moreira I., Serapicos E., Nunes O.C., Manaia C.M. Antibiotic resistance in coagulase negative staphylococci isolated from wastewater and drinking water. Sci. Total Environ. 2009;407:3876–3882. doi: 10.1016/j.scitotenv.2009.02.034. [DOI] [PubMed] [Google Scholar]
- 39.Rey Pérez J., Zálama Rosa L., García Sánchez A., Hermoso de Mendoza Salcedo J., Alonso Rodríguez J.M., Cerrato Horrillo R., Zurita S.G., Gil Molino M. Multiple Antimicrobial Resistance in Methicillin-Resistant Staphylococcus sciuri Group Isolates from Wild Ungulates in Spain. Antibiotics. 2021;10:920. doi: 10.3390/antibiotics10080920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Silva V., Gabriel S.I., Borrego S.B., Tejedor-Junco M.T., Manageiro V., Ferreira E., Reis L., Caniça M., Capelo J.L., Igrejas G., et al. Antimicrobial Resistance and Genetic Lineages of Staphylococcus aureus from Wild Rodents: First Report of mecC-Positive Methicillin-Resistant S. aureus (MRSA) in Portugal. Animals. 2021;11:1537. doi: 10.3390/ani11061537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Monecke S., Gavier-Widén D., Hotzel H., Peters M., Guenther S., Lazaris A., Loncaric I., Müller E., Reissig A., Ruppelt-Lorz A., et al. Diversity of Staphylococcus aureus Isolates in European Wildlife. PLoS ONE. 2016;11:e0168433. doi: 10.1371/journal.pone.0168433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bengtsson B., Persson L., Ekström K., Unnerstad H.E., Uhlhorn H., Börjesson S. High occurrence of mecC-MRSA in wild hedgehogs (Erinaceus europaeus) in Sweden. Vet. Microbiol. 2017;207:103–107. doi: 10.1016/j.vetmic.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 43.García-Álvarez L., Holden M.T.G., Lindsay H., Webb C.R., Brown D.F.J., Curran M.D., Walpole E., Brooks K., Pickard D.J., Teale C., et al. Meticillin-resistant Staphylococcus aureus with a novel mecA homologue in human and bovine populations in the UK and Denmark: A descriptive study. Lancet. Infect. Dis. 2011;11:595–603. doi: 10.1016/S1473-3099(11)70126-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Giacinti G., Carfora V., Caprioli A., Sagrafoli D., Marri N., Giangolini G., Amoruso R., Iurescia M., Stravino F., Dottarelli S., et al. Prevalence and characterization of methicillin-resistant Staphylococcus aureus carrying mecA or mecC and methicillin-susceptible Staphylococcus aureus in dairy sheep farms in central Italy. J. Dairy Sci. 2017;100:7857–7863. doi: 10.3168/jds.2017-12940. [DOI] [PubMed] [Google Scholar]
- 45.Porrero M.C., Valverde A., Fernández-Llario P., Díez-Guerrier A., Mateos A., Lavín S., Cantón R., Fernández-Garayzabal J.-F., Domínguez L. Staphylococcus aureus carrying mecC gene in animals and urban wastewater, Spain. Emerg. Infect. Dis. 2014;20:899–901. doi: 10.3201/eid2005.130426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Monecke S., Gavier-Widen D., Mattsson R., Rangstrup-Christensen L., Lazaris A., Coleman D.C., Shore A.C., Ehricht R. Detection of mecC-Positive Staphylococcus aureus (CC130-MRSA-XI) in Diseased European Hedgehogs (Erinaceus europaeus) in Sweden. PLoS ONE. 2013;8:e66166. doi: 10.1371/journal.pone.0066166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kerschner H., Harrison E.M., Hartl R., Holmes M.A., Apfalter P. First report of mecC MRSA in human samples from Austria: Molecular characteristics and clinical data. New Microbes New Infect. 2015;3:4–9. doi: 10.1016/j.nmni.2014.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Worthing K.A., Coombs G.W., Pang S., Abraham S., Saputra S., Trott D.J., Jordan D., Wong H.S., Abraham R.J., Norris J.M. Isolation of mecC MRSA in Australia. J. Antimicrob. Chemother. 2016;71:2348–2349. doi: 10.1093/jac/dkw138. [DOI] [PubMed] [Google Scholar]
- 49.Tavares A., Faria N.A., de Lencastre H., Miragaia M. Population structure of methicillin-susceptible Staphylococcus aureus (MSSA) in Portugal over a 19-year period (1992–2011) Eur. J. Clin. Microbiol. Infect. Dis. 2014;33:423–432. doi: 10.1007/s10096-013-1972-z. [DOI] [PubMed] [Google Scholar]
- 50.Satta G., Ling C.L., Cunningham E.S., McHugh T.D., Hopkins S. Utility and limitations of Spa-typing in understanding the epidemiology of staphylococcus aureus bacteraemia isolates in a single University Hospital. BMC Res. Notes. 2013;6:398. doi: 10.1186/1756-0500-6-398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Johnson W.L., Sohn M.B., Taffner S., Chatterjee P., Dunman P.M., Pecora N., Wozniak R.A.F. Genomics of Staphylococcus aureus ocular isolates. PLoS ONE. 2021;16:e0250975. doi: 10.1371/journal.pone.0250975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.David M.Z., Boyle-Vavra S., Zychowski D.L., Daum R.S. Methicillin-Susceptible Staphylococcus aureus as a Predominantly Healthcare-Associated Pathogen: A Possible Reversal of Roles? PLoS ONE. 2011;6:e18217. doi: 10.1371/journal.pone.0018217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Plano L.R.W., Shibata T., Garza A.C., Kish J., Fleisher J.M., Sinigalliano C.D., Gidley M.L., Withum K., Elmir S.M., Hower S., et al. Human-Associated Methicillin-Resistant Staphylococcus aureus from a Subtropical Recreational Marine Beach. Microb. Ecol. 2013;65:1039–1051. doi: 10.1007/s00248-013-0216-1. [DOI] [PubMed] [Google Scholar]
- 54.Hofer U. Squirrel-killing Staphylococcus aureus. Nat. Rev. Microbiol. 2021;19:481. doi: 10.1038/s41579-021-00591-y. [DOI] [PubMed] [Google Scholar]
- 55.Fountain K., Blackett T., Butler H., Carchedi C., Schilling A.-K., Meredith A., Gibbon M.J., Lloyd D.H., Loeffler A., Feil E.J. Fatal exudative dermatitis in island populations of red squirrels (Sciurus vulgaris): Spillover of a virulent Staphylococcus aureus clone (ST49) from reservoir hosts. Microb. Genom. 2021;7:565. doi: 10.1099/mgen.0.000565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mrochen D.M., Schulz D., Fischer S., Jeske K., El Gohary H., Reil D., Imholt C., Trübe P., Suchomel J., Tricaud E., et al. Wild rodents and shrews are natural hosts of Staphylococcus aureus. Int. J. Med. Microbiol. 2018;308:590–597. doi: 10.1016/j.ijmm.2017.09.014. [DOI] [PubMed] [Google Scholar]
- 57.Deplano A., Vandendriessche S., Nonhoff C., Denis O. Genetic diversity among methicillin-resistant Staphylococcus aureus isolates carrying the mecC gene in Belgium. J. Antimicrob. Chemother. 2014;69:1457–1460. doi: 10.1093/jac/dku020. [DOI] [PubMed] [Google Scholar]
- 58.Haenni M., Châtre P., Dupieux C., Métayer V., Maillard K., Bes M., Madec J.-Y., Laurent F. mecC-positive MRSA in horses. J. Antimicrob. Chemother. 2015;70:3401–3402. doi: 10.1093/jac/dkv278. [DOI] [PubMed] [Google Scholar]
- 59.Porrero M., Valverde A., Mateos A., Cantón R., Gortázar C., Fernández-Garayzábal J.-F., Domínguez L. Staphylococcus aureus Genetic Lineages Found in Urban Effluents and River Water. Int. J. Water Wastewater Treat. 2016;2:1–5. [Google Scholar]
- 60.Cuny C., Layer F., Hansen S., Werner G., Witte W. Nasal Colonization of Humans with Occupational Exposure to Raw Meat and to Raw Meat Products with Methicillin-Susceptible and Methicillin-Resistant Staphylococcus aureus. Toxins (Basel) 2019;11:190. doi: 10.3390/toxins11040190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Little S.V., Hillhouse A.E., Lawhon S.D., Bryan L.K. Analysis of Virulence and Antimicrobial Resistance Gene Carriage in Staphylococcus aureus Infections in Equids Using Whole-Genome Sequencing. mSphere. 2021;6:e00196-20. doi: 10.1128/mSphere.00196-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mama O.M., Morales L., Ruiz-Ripa L., Zarazaga M., Torres C. High prevalence of multidrug resistant S. aureus-CC398 and frequent detection of enterotoxin genes among non-CC398 S. aureus from pig-derived food in Spain. Int. J. Food Microbiol. 2020;320:108510. doi: 10.1016/j.ijfoodmicro.2020.108510. [DOI] [PubMed] [Google Scholar]
- 63.Tolba O., Loughrey A., Goldsmith C.E., Millar B.C., Rooney P.J., Moore J.E. Survival of epidemic strains of healthcare (HA-MRSA) and community-associated (CA-MRSA) meticillin-resistant Staphylococcus aureus (MRSA) in river-, sea- and swimming pool water. Int. J. Hyg. Environ. Health. 2008;211:398–402. doi: 10.1016/j.ijheh.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 64.Umeda K., Nakamura H., Yamamoto K., Nishina N., Yasufuku K., Hirai Y., Hirayama T., Goto K., Hase A., Ogasawara J. Molecular and epidemiological characterization of staphylococcal foodborne outbreak of Staphylococcus aureus harboring seg, sei, sem, sen, seo, and selu genes without production of classical enterotoxins. Int. J. Food Microbiol. 2017;256:30–35. doi: 10.1016/j.ijfoodmicro.2017.05.023. [DOI] [PubMed] [Google Scholar]
- 65.Rossi B.F., Bonsaglia E.C.R., Castilho I.G., Dantas S.T.A., Salina A., Langoni H., Pantoja J.C.F., Budri P.E., Fitzgerald-Hughes D., Júnior A.F., et al. Genotyping of long term persistent Staphylococcus aureus in bovine subclinical mastitis. Microb. Pathog. 2019;132:45–50. doi: 10.1016/j.micpath.2019.04.031. [DOI] [PubMed] [Google Scholar]
- 66.Lahuerta-Marin A., Guelbenzu-Gonzalo M., Pichon B., Allen A., Doumith M., Lavery J.F., Watson C., Teale C.J., Kearns A.M. First report of lukM-positive livestock-associated methicillin-resistant Staphylococcus aureus CC30 from fattening pigs in Northern Ireland. Vet. Microbiol. 2016;182:131–134. doi: 10.1016/j.vetmic.2015.11.019. [DOI] [PubMed] [Google Scholar]
- 67.Pérez-Montarelo D., Viedma E., Larrosa N., Gómez-González C., Ruiz de Gopegui E., Muñoz-Gallego I., San Juan R., Fernández-Hidalgo N., Almirante B., Chaves F. Molecular Epidemiology of Staphylococcus aureus Bacteremia: Association of Molecular Factors With the Source of Infection. Front. Microbiol. 2018;9:2210. doi: 10.3389/fmicb.2018.02210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sousa M., Silva N., Manageiro V., Ramos S., Coelho A., Gonçalves D., Caniça M., Torres C., Igrejas G., Poeta P. First report on MRSA CC398 recovered from wild boars in the north of Portugal. Are we facing a problem? Sci. Total Environ. 2017;596–597:26–31. doi: 10.1016/j.scitotenv.2017.04.054. [DOI] [PubMed] [Google Scholar]
- 69.Porrero M.C., Mentaberre G., Sánchez S., Fernández-Llario P., Gómez-Barrero S., Navarro-Gonzalez N., Serrano E., Casas-Díaz E., Marco I., Fernández-Garayzabal J.F., et al. Methicillin resistant Staphylococcus aureus (MRSA) carriage in different free-living wild animal species in Spain. Vet. J. 2013;198:127–130. doi: 10.1016/j.tvjl.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 70.Shuaibu S.A., Onaolapo J.A., Olayinka B.O. Towards Understanding the Clonality of Methicillin Resistant Staphylococcus aureus in Sokoto State Nigeria. Rep. Heal. Care. 2019;5:44–53. [Google Scholar]
- 71.Aggarwal S., Jena S., Panda S., Sharma S., Dhawan B., Nath G., Singh N.P., Nayak K.C., Singh D.V. Antibiotic Susceptibility, Virulence Pattern, and Typing of Staphylococcus aureus Strains Isolated From Variety of Infections in India. Front. Microbiol. 2019;10:2763. doi: 10.3389/fmicb.2019.02763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Overesch G., Büttner S., Rossano A., Perreten V. The increase of methicillin-resistant Staphylococcus aureus(MRSA) and the presence of an unusual sequence type ST49 in slaughter pigs in Switzerland. BMC Vet. Res. 2011;7:30. doi: 10.1186/1746-6148-7-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Simpson V.R., Davison N.J., Kearns A.M., Pichon B., Hudson L.O., Koylass M., Blackett T., Butler H., Rasigade J.P., Whatmore A.M. Association of a lukM-positive clone of Staphylococcus aureus with fatal exudative dermatitis in red squirrels (Sciurus vulgaris) Vet. Microbiol. 2013;162:987–991. doi: 10.1016/j.vetmic.2012.10.025. [DOI] [PubMed] [Google Scholar]
- 74.Seyedmonir E., Yilmaz F., Icgen B. mecA Gene Dissemination Among Staphylococcal and Non-staphylococcal Isolates Shed in Surface Waters. Bull. Environ. Contam. Toxicol. 2015;95:131–138. doi: 10.1007/s00128-015-1510-z. [DOI] [PubMed] [Google Scholar]
- 75.Čuvalová Z., Pipová M., Kantíková M., Brtková A., Fajber J. Virulence factors and antimicrobial resistance of coagulase-negative staphylococci isolated from drinking water. Open Life Sci. 2015;10:328–338. doi: 10.1515/biol-2015-0034. [DOI] [Google Scholar]
- 76.Yilmaz F., Orman N., Serim G., Kochan C., Ergene A., Icgen B. Surface Water-Borne Multidrug and Heavy Metal-Resistant Staphylococcus Isolates Characterized by 16S rDNA Sequencing. Bull. Environ. Contam. Toxicol. 2013;91:697–703. doi: 10.1007/s00128-013-1112-6. [DOI] [PubMed] [Google Scholar]
- 77.Silva V., Almeida F., Carvalho J.A., Castro A.P., Ferreira E., Manageiro V., Tejedor-Junco M.T., Caniça M., Igrejas G., Poeta P. Emergence of community-acquired methicillin-resistant Staphylococcus aureus EMRSA-15 clone as the predominant cause of diabetic foot ulcer infections in Portugal. Eur. J. Clin. Microbiol. Infect. Dis. 2020;39:179–186. doi: 10.1007/s10096-019-03709-6. [DOI] [PubMed] [Google Scholar]
- 78.Cuny C., Layer F., Strommenger B., Witte W. Rare occurrence of methicillin-resistant Staphylococcus aureus CC130 with a novel mecA homologue in humans in Germany. PLoS ONE. 2011;6:e24360. doi: 10.1371/journal.pone.0024360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zhang K., Sparling J., Chow B.L., Elsayed S., Hussain Z., Church D.L., Gregson D.B., Louie T., Conly J.M. New quadriplex PCR assay for detection of methicillin and mupirocin resistance and simultaneous discrimination of Staphylococcus aureus from coagulase-negative staphylococci. J. Clin. Microbiol. 2004;42:4947–4955. doi: 10.1128/JCM.42.11.4947-4955.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Silva V., Vieira-Pinto M., Saraiva C., Manageiro V., Reis L., Ferreira E., Caniça M., Capelo J.L., Igrejas G., Poeta P. Prevalence and Characteristics of Multidrug-Resistant Livestock-Associated Methicillin-Resistant Staphylococcus aureus (LA-MRSA) CC398 Isolated from Quails (Coturnix Coturnix Japonica) Slaughtered for Human Consumption. Animals. 2021;11:2038. doi: 10.3390/ani11072038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.van Wamel W.J.B., Rooijakkers S.H.M., Ruyken M., van Kessel K.P.M., van Strijp J.A.G. The innate immune modulators staphylococcal complement inhibitor and chemotaxis inhibitory protein of Staphylococcus aureus are located on beta-hemolysin-converting bacteriophages. J. Bacteriol. 2006;188:1310–1315. doi: 10.1128/JB.188.4.1310-1315.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Enright M.C., Day N.P., Davies C.E., Peacock S.J., Spratt B.G. Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones of Staphylococcus aureus. J. Clin. Microbiol. 2000;38:1008–1015. doi: 10.1128/JCM.38.3.1008-1015.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Harmsen D., Claus H.H.H.H., Witte W., Rothgänger J., Claus H.H.H.H., Turnwald D., Vogel U. Typing of Methicillin-Resistant Staphylococcus aureus in a University Hospital Setting by Using Novel Software for spa Repeat Determination and Database Management. J. Clin. Microbiol. 2003;41:5442–5448. doi: 10.1128/JCM.41.12.5442-5448.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Shopsin B., Mathema B., Alcabes P., Said-Salim B., Lina G., Matsuka A., Martinez J., Kreiswirth B.N. Prevalence of agr specificity groups among Staphylococcus aureus strains colonizing children and their guardians. J. Clin. Microbiol. 2003;41:456–459. doi: 10.1128/JCM.41.1.456-459.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data is contained within the article or supplementary material.