Abstract
Currently, there is limited evidence to guide treatment and no standard management guidelines exist for treating frozen shoulder (FS). A general management approach consists of initial evaluation, range of motion (ROM) exercises, intra-articular injection of glucocorticoid, home exercise program (HEP), and/or physical therapies. However, the general approach lacks detail and has limited evidence of its effectiveness. This retrospective cohort study evaluates the short-term recovery of near-full to full-ROM technique followed by an instructed HEP for strengthening and coordinating shoulder girdle muscle group for FS management. This study details our experiences following a general approach to managing FS and aims to fill this knowledge void, providing additional context of the efficacy of FS management in the real-world. Seven-two adult patients with FS (46 females, 26 males; mean age of 66; standard deviation of 15.1; range 23–87) from an orthopedic and physical medicine and sport medicine office between 2014 and 2018 were included in this study. Following general management of FS, patients received a glucocorticoid–lidocaine mixture injection administered to the respective shoulder at the glenohumeral joint space and/or subacromial separately. Immediately, patients underwent active manipulation of the affected shoulder in 3 directions: forward flexion, abduction, and extension in the sagittal plane. Lastly, patients were instructed to perform movements similar to the active manipulation protocol as a HEP. The abduction and forward flexion ROM showed significant improvements with the described protocol. Following treatment, there was a 90.20° and 77.33° increase in average shoulder abduction and forward flexion ROM, respectively (P < .05). The immediate goal of this protocol was to gain maximum ROM in different directions of shoulder mobility. Following the general management of FS, active manipulation under local anesthetic was a highly effective treatment modality for adhesive capsulitis that was time-saving and cost-effective.
Keywords: adhesive capsulitis, frozen shoulder, manipulation, range of motion
1. Introduction
Frozen shoulder (FS), also referred to as adhesive capsulitis of the shoulder, has a lifetime prevalence of 2% to 5.3% in the general population.[1–3] The condition typically surfaces when patients reach their mid-50s, with women being more affected than men. Importantly, studies have shown that among patients who develop FS, 15% develop a long-term disability.[4–8]
Typically, FS presents with severe loss of shoulder motion, pain, and stiffness in the shoulder. FS is typically diagnosed clinically as there are no definitive laboratory tests or radiological markers for this condition.[9] As a result of shoulder stiffness and pain, patients may be limited in the range of motion (ROM) in the shoulder. Patients with FS eventually develop a certain degree of myostatic contracture or tightness of the shoulder girdle. The most common limitations in ROM involves external rotation, abduction, and forward flexion.[2] Over time many patients with FS develop a characteristic “shrug sign”[2] due to glenohumeral joint elevation which indicates compensation due to lack of capsular extensibility. In addition, there is the presence of an impaired scapulothoracic glenohumeral ratio. There is also an accompanying change in the central nervous system motor patterning due to maladaptive movement and adaptive postural deviations[2] such as thoracic kyphosis or anterior positioned shoulders. Consequently, FS patients suffer from significantly impaired activities of daily living (ADLs) and reduced quality of life.[3,10] These patients demonstrated impaired ability in raising the arm and performing overhead activities such as dressing and combing their hair. Treatments for FS also involve, conservative approaches, physical therapy, glucocorticoids given orally or as an intra-articular injection with or without hydrodilation, surgery performing arthroscopic intervention, and passive manipulation under general or local anesthesia (MUA).[9,11–14]
Currently, evidence guiding treatment of FS is limited. The literature reports that the natural history of FS is benign, self-limiting, and typically resolves between 24 months[3] and 30 months.[12] However, incomplete resolution can occur. A general management approach consists of initial evaluation, ROM exercises, intra-articular injection of glucocorticoid, home exercise program (HEP), and/or physical therapies. However, the general approach followed in standard approach is heterogeneous and lacks detail on effectiveness in the literature.[15] In line with the purpose of this study, this technique is being evaluated as a simpler, less invasive, and quicker way to resolve FS. One study highlighted the limited clinical evidence of the effectiveness of treatments in FS from their review of 31 clinical effectiveness studies due to study diversity and poor reporting of outcome data.[12]
The availability of a myriad of treatment options for patients with FS may be overwhelming to the treating health care professional. With no consensus about the optimal treatment strategy, this retrospective study aims to evaluate the efficacy of using focused manipulation with active movement in conjunction with a local injection mixture of corticosteroid and lidocaine to treat FS.
2. Methods
Retrospectively reviewed were 72 charts of patients with FS treated between 2014 and 2018. Calculation included in methods on line 108: The representative population mean (105.9) and standard deviation (SD 11.8) for forward flexion in patients with FS was obtained from Chengjun, Chengwei, & Chengwen study (2021),[16] mean forward flexion ROM before treatment was estimated to be 102, sample size for this retrospective study was n = 72. They were selected to be included in this Northwell Health Institutional Review Board approved retrospective cohort study on December 2020 (#19-1130) that is not clinically registered. Due to the retrospective nature of the study design, the informed written consent was waived. The criteria for inclusion in the study were diagnosis of FS and admission to an orthopedic and physical medicine and sport medicine office from 2014 to 2018. Patients with incomplete medical records were excluded. The inclusion of patients with previous treatment or specific conditions, such as diabetes, was not an exclusion criterion and not taken into account in analyses. This study describes our real-world experience with FS treatment that uses a general accepted clinical approach of management. Informed consent has been waived by the IRB as the study reviewed patients who received standard clinical practice.
2.1. Protocol
Before treatment, patients were evaluated for their shoulder ROM by measuring their forward flexion, abduction, and external rotation which were recorded with visual clinical expertise or the use of a goniometer. During this assessment, both passive and active ROM assessments were completed. After a discussion with the patient and obtaining the patient's informed consent, a mixture of Kenalog (triamcinolone acetonide) and lidocaine injections were guided with ultrasound imaging in aseptic conditions. Injection of 40 to 80 mg Kenalog mixed with 2 to 6 mL lidocaine 1% was administered to the respective shoulder at the glenohumeral joint space and/or subacromial separately.[17] The majority of patients received 1 injection; however, a fraction received 2 injections simultaneously to the mentioned target areas. A few patients given 2 injections based on pain severity and imaging findings did not affect the findings because injections achieved the same result to numb the shoulder so that the technique can be performed.
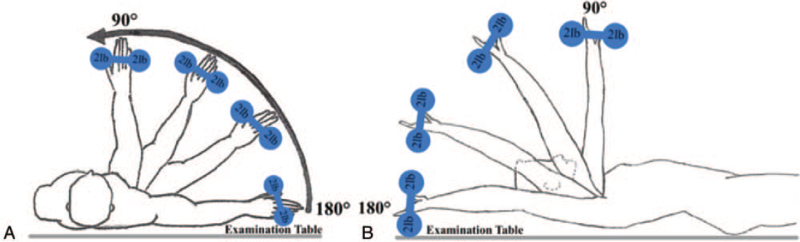
Following injectable administration, the patients’ shoulder underwent active manipulation. All patients were placed in a supine position and asked to perform different movements in 2 directions at the shoulder joint (Fig. 1). Patients were instructed to perform horizontal shoulder abduction and forward flexion aimed toward 90° to 180° while holding a 2-lb weight in their hands and keeping the elbow in full extension. The addition of the weight enhances stretching that follows the force of gravity and promotes muscle strength as the patient lifts the weight against gravity. The addition of the small weight, 2 lb, enhances stretching without overwhelming the patient, allowing for repetition and conditioning of the joint. This is a form of closed kinetic chain exercise with a weight-bearing through the distal end of the extremity, which engages not only the primary muscle to be trained, but allows the afferent nervous system to send proprioceptive information to higher levels. This self-administered exercise also strengthens the muscles to support the limbs. The muscles contract as a team, at the proper moment and intensity to perform activity in a smooth coordinated fashion. During active manipulation, the ROM restoration is gradual based on pain level, discomfort, and degree of stiffness that patients tolerated to perform the repetitive back and forth motions. These motions were performed until the patient could achieve maximum shoulder abduction and forward flexion. After completion of the active manipulations in the supine position, a majority of the patients were able to achieve enough external rotation actively to reach their hand to the back of their head or the lower back while in sitting position (internal rotation). This newfound ROM achieved signals success for the described technique of active shoulder manipulation in FS.
Figure 1.
Schematic of the protocol. (A) After injection, frozen shoulder patients lay supine to the examination table and instructed to perform horizontal shoulder abduction while keeping the elbow in full extension and holding a 2-lb weight. (B) Next, patients were instructed to perform forward flexion. These 2 movements were completed with active manipulation.
The procedure mainly focuses the immediate restoration of mobility in the glenohumeral joint and scapulothoracic articulation that enables long-term coordination of smooth motion by building muscle strength and memory, which is known as active exercise. The protocol described in this study works to restore capsular and soft tissue extensibility by enhancing gradual ROM by active stretching under local anesthetic effect. The tightness by this technique plays a significant role in regaining functional to a full restoration that is absent in other passive manipulations. Patients were instructed to keep their elbows straight to ensure full mobility from about 90° to 180° that occurs in the shoulder girdle articulations. The patients remain awake throughout the procedure and no passive external forces were applied. All mobility restoration by active manipulation was geared toward shoulder girdle articulations.
After injection and active manipulation for up to 10 minutes, patients were instructed to continue with an identical HEP as self-management 2 times per day for 10 minutes for as long as the patient is deriving benefit. A duration of 10 minutes was used as this was a standard time frame that was tolerated for all patients undergoing exercise. Patients following the regime restored coordination in the shoulder for long-term if patients are compliant with the HEP after they have achieved maximum ROM immediately following treatment. However, if patients do not continue with HEP, then the recurrence rate is expectable and the procedure must be repeated.
2.2. Patient demographic and clinical characteristics
Overall 72 patients were included in this retrospective study. There was a wide range of ages for this cohort for both women and men. The average age of the cohort was 66.1 years, (SD, 15.1; range, 23–87 years). There were 46 females (63.9%), average age 66 years (SD, 15.5; range, 23–87 years). There were 26 males (36.1%), average age 66.4 years (SD, 14.1; range, 27–87 years). In 39 (54.1%) patients the right shoulder, 20 (27.8%) patients the left shoulder, and 13 (18.1%) patients the bilateral shoulder was affected. The demographic data of the patients are shown in Table 1.
Table 1.
Characteristics of the frozen shoulder patients.
| Patient characteristics | n (%) | Mean age (yr) | Standard deviation (yr) | Range (yr) |
| Total patients | 72 (100%) | 66.1 | 15.1 | 23 to 87 |
| Males | 26 (36.1%) | 66.4 | 14.1 | 27 to 87 |
| Females | 46 (63.9%) | 66 | 15.5 | 23 to 87 |
| Affected shoulder | ||||
| Right | 39 (54.1%) | |||
| Left | 20 (27.8%) | |||
| Bilateral | 13 (18.1%) | |||
2.3. Statistical analysis
Statistical analysis was performed using Microsoft Excel and Graphpad Prism 6 (GraphPad Software Inc., CA) with a Student t test. Statistical significance was defined as P < .05.
3. Results
3.1. Evaluation
Clinical diagnoses were made by physical examinations with the primary diagnosis being FS, in which patients present with painful and limited ROM. There were other objective clinical relating to FS as well. These secondary clinical findings were grouped into the following 9 categories; restrictive active and passive ROM, suprascapular muscle atrophy in chronic condition, rotator cuff pathology (eg, partial tear, full tear) confirmed on magnetic resonance imaging, reduced rotator cuff strength, glenohumeral osteoarthritis confirmed in either X-ray or magnetic resonance imaging, and muscle spasms.
Clinical evaluations found that 7 patients were diagnosed with decreased rotor cuff strength and 10 patients were diagnosed with a rotator cuff tear. Nine patients were diagnosed with glenohumeral osteoarthritis. All patients demonstrated significant various restricted ranges of motion which included passive and active motion, on initiating ROM, rotation, abduction, forward flexion, impaired scapulothoracic/glenohumeral coordination, and restriction in all directions causes impaired ADLs.
A series of provocative tests are also used to support the underlying conditions: a positive Hawking test, a positive Yergonson test, and a positive impingement test. Most patients had multiple clinical and imaging objective findings. Shoulder girdle muscle atrophy was present in 8 patients. Forty-six patients had shoulder tenderness which included tenderness in the subacromial and anterior glenohumeral region, diffused tenderness on shoulder girdle musculature and para axial thoracic muscles, tenderness on the biceps tendon in the bicipital groove, and tenderness in the acromioclavicular joint.
Sixty-four patients had a positive impingement test/rotator cuff, 4 patients were positive for the Yergason Test, and 61 patients were positive for the Hawkins test.
3.2. Shoulder abduction and forward flexion ROM findings
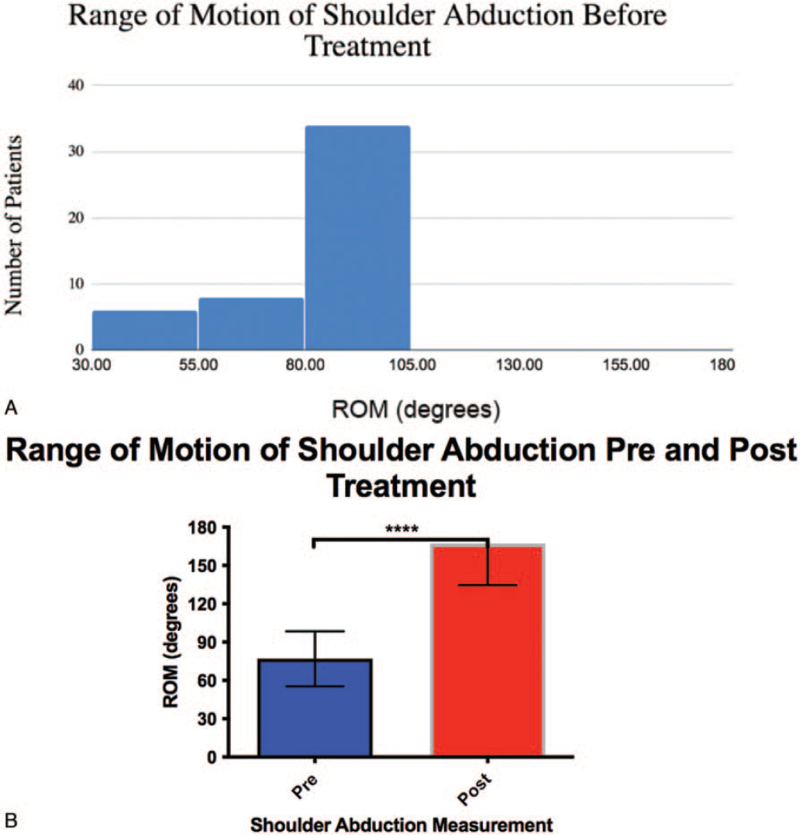
After Kenalog and lidocaine injections and active manipulation, patients were found to have instant ROM restoration in both shoulder abduction and forward flexion. A two-tailed repeated measures Student t test was used to analyze whether there was a significant difference between pretreatment shoulder abduction ROM measurements and post-treatment shoulder abduction ROM measurements for the patient cohort. Figure 2A shows the number of patients with a recorded ROM of shoulder abduction before active manipulation was performed. The null hypothesis that there will be no statistically significant difference between the means for the degree of ROM for shoulder abduction pre and post-treatment for the patient cohort was rejected. The two-tailed repeated measures t test revealed that there was a statistically significant difference of 88.5 ± 25.2°, (95% CI: 90.56–99.85) between the pretreatment shoulder abduction ROM measurements with a mean ± SD of 78.3 ± 20.7°, n = 53; and post-treatment shoulder abduction ROM measurements with a mean ± SD of 167.2 ± 32.6°, n = 71. Figure 2B shows that there is a statistically significant difference in recorded ROM of shoulder abduction in the pre and post-treatment.
Figure 2.
ROM of shoulder abduction prior to and after injection. (A) The bar graph indicates the number of patients within specified ranges of motion for shoulder abduction before injection and active manipulation. The ROM for all patients was recorded to be from 30° to 100° for shoulder abduction. (B) The bar graph demonstrates the average ROM of shoulder abduction pre and postinjection and active manipulation. A statistically significant difference was observed with a Student t test. The error bars represent standard deviation. ROM = range of motion.
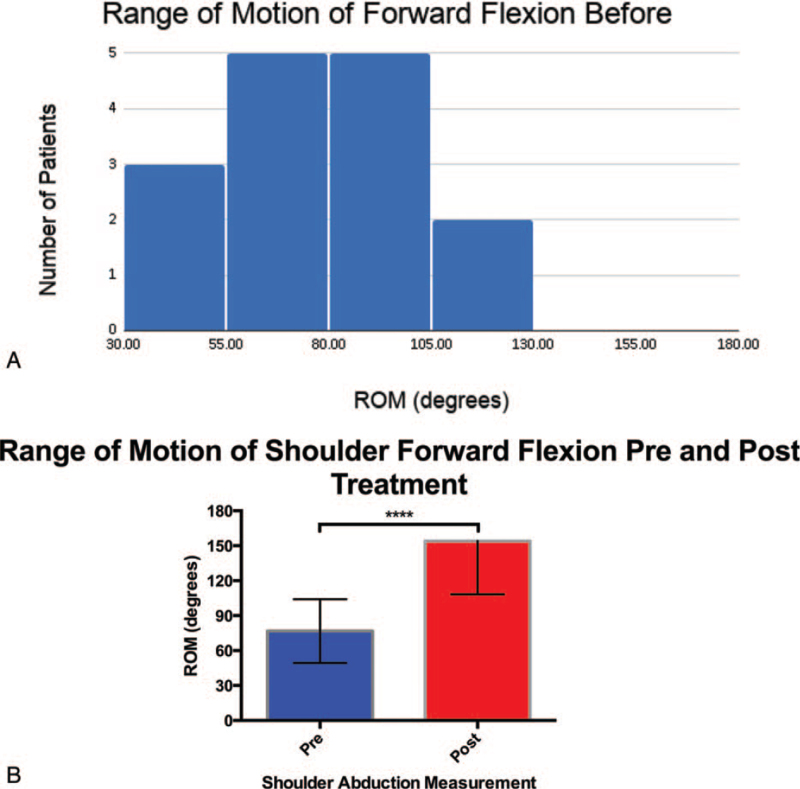
A two-tailed repeated measures Student t test with Welch correction was conducted to determine whether there was a significant difference between pretreatment and post-treatment shoulder forward flexion ROM measurements for the patient cohort. Figure 3A portrays the number of patients with the recorded ROM of forward flexion before active manipulation was performed. The null hypothesis that there will be no statistically significant difference between the means for the degree of ROM for shoulder forward flexion pre and post-treatment for the patient cohort was rejected. The two-tailed repeated measures t test revealed that there was a statistically significant difference of 77.3 ± 36.7° (95% CI: 48.81 to 105.9) between the pretreatment shoulder forward flexion ROM measurements with a mean ± SD of 76.7 ± 27.4°, n = 15; and post-treatment shoulder forward flexion ROM measurements with a mean ± SD of 154.0 ± 45.8°, n = 15. Figure 3B demonstrates that there is a statistically significant difference in recorded ROM of forward flexion in the pre and post-treatment.
Figure 3.
ROM of shoulder forward flexion prior to and after injection. (A) The bar graph shows the number of patients within specified ranges of motion for shoulder forward flexion before injection and active manipulation. The ROM for all patients was recorded to be from 30° to 120° for shoulder forward flexion. (B) The bar graph demonstrates the average ROM of shoulder forward flexion pre and postinjection and active manipulation. A statistically significant difference was observed with a Student t test. The error bars represent standard deviation. ROM = range of motion.
4. Discussion
FS is characterized by motion loss, pain, and stiffness in the shoulder and tends to resolve within 1 to 3 years. However, many patients are unwilling to endure functional limitations and pain until their condition resolves. This study provides additional data with an approach that follows general management of FS that resolves restrictions in motion in a relatively short amount of time.
For this study, the average age of the FS patient cohort was 66.1 years old with 63.9% female (n = 72). Although there is a wide range with a maximum and minimum of 87 and 23, respectively, the majority of patients were in their late 60s. The patient population of this study corresponds well with other FS studies found in the literature where females experience FS more often than men, and the age of onset occurs in a population generally over 50 years.[18]
Our study consisting of 100% of patients with pain in the affected shoulder reported a stiff shoulder with limited ROM of up to 90° and difficulty raising their arm. This agrees with the patients’ complaints and symptoms found in literature, stating that the most common symptoms of FS are shoulder pain, especially pain at night during sleeping, shoulder stiffness, and limited ROM.[13] Moreover, 69.4% of patients reported having trouble sleeping and diminished ADLs. Additionally, a few symptoms reported by this patient population included numbness or tingling in the affected shoulder or arm (34.7%), a palpable snapping or clicking sensation when trying to move the affected shoulder (36.1%). Although patients are not always aware of a FS diagnosis, physical examination confirms the objective finding of the limitations of motion with different etiology. Previous literature described FS as a condition that was “difficult to define, difficult to treat and difficult to explain from the point of view of pathology.”[19] The clinical diagnoses of this patient population were done by physical examination as well as other clinical and imaging findings.
As described above, there are many options for treatment and management of FS: from a conservative approach to surgery, to passive MUA.[9,11–12,20] MUA is a common conservative treatment used that is safe and effective.[21–23] While literature provides evidence that these approaches or combinations thereof have benefits, full restoration of ROM at best takes many months. Past research has found passive MUA to be a simple and invasive procedure to improve symptoms of FS.[24] However, complications after passive MUA do arise, such as shoulder dislocation, rotator cuff tear, fractures, nerve injuries, and postmanipulation instability.[24–26]
To eliminate the number of risks associated with types of MUA, the protocol described in our paper follows a general management approach that involves the injection of Kenalog and lidocaine mixture and manipulation with active movement. This protocol poses a safer treatment modality that allows patients to participate in the restoration of ROM and to stop the procedure when overwhelmed. Thus, manipulation with active movement enables patients to restore their lost ROM to about 90° to 180°, to strengthen muscles, and to return shoulder girdle muscle coordination, which is all dependent on patient compliance and cooperation. Throughout the procedure, patients remain awake and perform the active manipulations according to what they can tolerate as no external force is applied. This technique following a general management approach achieves mobility in both glenohumeral joint and resolves scapulothoracic tightness, which rarely happens in passive manipulation techniques or surgical interventions. The shoulder girdle musculature coordination has a significant role in sustained recovery by gaining muscle memory and reducing all connective and soft tissue tightness. The FS protocol described in this study effectively reduces risks involved with MUA. For example, elderly diagnosed with osteoporosis have a high risk of fracture.[27] However, the proposed active manipulation technique of this study has no evidence of fracture in patients with osteoporosis. These active movements were attempted to build muscle memory, loosen muscle-tendon tightness, and restore central nervous system motor patterning.
In the initial attempt, patients performed these movements until maximum mobility was achieved. The approach used by this study demonstrates that full or almost near full ROM can occur during the first outpatient encounter followed with instructed home exercises resolves the issue in a relatively short amount of time with less discomfort when compared to other treatment modalities. A systemic review and meta-analysis demonstrates that exercise is effective for improving ROM, function, and pain in patients with FS.[28]
The study had several strengths. First, the study investigated a protocol following the general management approach for FSs can be used in every clinic without disrupting practice. Secondly, active manipulation in conjunction with local injections could be easily implemented in a multicenter clinical trial. Finally, this technique has an immediate effect at a low cost, benefitting patients unwilling to undergo invasive treatment, and involves minimal or no side effects.
5. Limitations
This study had several limitations as well. The major limitation of this study is that it is a retrospective study. As such there was no control group and patients were not randomized or blinded to treatments. Secondly, the age range of the patients was wide, which may have an effect on results regarding physiological changes related to aging in muscle power and joint ROM. Thirdly, FS is a complicated condition that can be secondary to injuries or from pathways that are not fully understood. Moreover, long-term patient outcomes were not included as follow-up data was lacking from the retrospective study. Putting aside considerations like patients’ secondary gain from claims, a majority of patients showed good responses.
6. Conclusions
This retrospective cohort study describes the experiences of following a general management approach which focus primarily on the clinical finding of considerable restricted ROM, which could be painful and disabling. The results suggest that immediate active manipulation under local anesthetic mixed with steroid injection and an instructed HEP significantly recovered ROM, as well as strengthen and coordinate shoulder girdle muscle group. This coordination is necessary for smooth function, with minimal or no risk. This study details a real-world experience of a technique that follows the general management of FS and could be used to help patients willing nonsurgical treatment or avoid reverting to more extreme means of FS management. Although the study includes a small sample size, this technique for treating FS may translate to a large population under these particular circumstances and situations.
Author contributions
Conceptualization: Kioomars Moosazadeh.
Data curation: Kioomars Moosazadeh.
Formal analysis: Keva Li, James Gilchriest, Kian Bichoupan, Kioomars Moosazadeh.
Investigation: Kioomars Moosazadeh.
Methodology: Kioomars Moosazadeh.
Project administration: Kioomars Moosazadeh.
Resources: Kioomars Moosazadeh.
Supervision: Kioomars Moosazadeh.
Validation: Kioomars Moosazadeh.
Visualization: Keva Li, Kioomars Moosazadeh.
Writing – original draft: Keva Li, James Gilchriest, Kian Bichoupan, Kioomars Moosazadeh.
Writing – review & editing: Keva Li, James Gilchriest, Kian Bichoupan, Kioomars Moosazadeh.
Footnotes
Abbreviations: ADLs = activities of daily living, FS = frozen shoulder, HEP = home exercise program, MUA = manipulation under anesthesia, ROM = range of motion, SD = standard deviation.
How to cite this article: Li K, Bichoupan K, Gilchriest JA, Moosazadeh K. Real-world experience of treating frozen shoulder using active manipulation under local anesthetic: a retrospective study. Medicine. 2021;100:47(e27839).
The authors have no funding and conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Zreik NH, Malik RA, Charalambous CP. Adhesive capsulitis of the shoulder and diabetes: a meta-analysis of prevalence. Muscles Ligaments Tendons J 2016;6:26–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Page P, Labbe A. Adhesive capsulitis: use the evidence to integrate your interventions. N Am J Sports Phys Ther 2010;5:266–73. [PMC free article] [PubMed] [Google Scholar]
- [3].Reeves B. The natural history of the frozen shoulder syndrome. Scand J Rheumatol 1975;4:193–6. [DOI] [PubMed] [Google Scholar]
- [4].Simmonds FA. Shoulder pain with particular reference to the frozen shoulder. J Bone Joint Surg Br 1949;31B:426–32. [PubMed] [Google Scholar]
- [5].Binder AI, Bulgen DY, Hazleman BL, Roberts S. Frozen shoulder: a longterm prospective study. Ann Rheum Dis 1984;43:361–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Hazleman BL. The painful stiff shoulder. Rheumatol Phys Med 1972;11:413–21. [DOI] [PubMed] [Google Scholar]
- [7].Hand C, Clipsham K, Rees JL, Carr AJ. Long-term outcome of frozen shoulder. J Shoulder Elbow Surg 2008;17:231–6. [DOI] [PubMed] [Google Scholar]
- [8].Shaffer B, Tibone JE, Kerlan RK. Frozen shoulder. A long-term follow-up. J Bone Joint Surg Am 1992;74:738–46. [PubMed] [Google Scholar]
- [9].Dias R, Cutts S, Massoud S. Frozen shoulder. BMJ 2005;331:1453–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Le HV, Lee SJ, Nazarian A, Rodriguez EK. Adhesive capsulitis of the shoulder: review of pathophysiology and current clinical treatments. Shoulder Elbow 2017;9:75–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Brue S, Valentin A, Forssbiad M, Werner S, Mikkelsen C, Cerulli G. Idiopathic adhesive capsulitis of the shoulder: a review. Knee Surg Sports Traumatol Arthrosc 2007;15:1048–54. [DOI] [PubMed] [Google Scholar]
- [12].Maund E, Craig D, Suekarran S, et al. Management of frozen shoulder: a systematic review and cost-effectiveness analysis. Health Technol Assess (Winchester, England) 2012;16:01–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Hsu J, Anakwenze O, Warrender W, Abboud J. Current review of adhesive capsulitis. J Shoulder Elbow Surg 2011;20:502–14. [DOI] [PubMed] [Google Scholar]
- [14].Nevaiser TJ. Adhesive capsulitis of the shoulder: a study of the pathological findings in periarthritis of the shoulder. J Bone Joint Surg 1945;27:211–22. [Google Scholar]
- [15].Kraal T, Beimers L, The B, Sierevelt I, van den Bekerom M, Eygendaal D. Manipulation under anaesthesia for frozen shoulders: outdated technique or well-established quick fix? EFORT Open Rev 2019;4:98–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Song C, Song C, Li C. Outcome of manipulation under anesthesia with or without intra-articular steroid injection for treating frozen shoulder: A retrospective cohort study. Medicine 2021;100:e23893. 10.1097/MD.0000000000023893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Yoon SH, Lee HY, Lee HJ, Kwack KS. Optimal dose of intra-articular corticosteroids for adhesive capsulitis: a randomized, triple-blind, placebo-controlled trial. Am J Sports Med 2013;41:1133–9. [DOI] [PubMed] [Google Scholar]
- [18].Cohen C, Ejnisman B. Itoi E, et al. Epidemiology of frozen shoulder. Shoulder Stiffness. Berlin, Heidelberg: Springer; 2015. 21–30. [Google Scholar]
- [19].Codman EA. The Shoulder: Rupture of the Supraspinatus Tendon and Other Lesions in or about The Subacromial Bursa. Boston: Thomas Todd Co; 1934. [Google Scholar]
- [20].Waszczykowski M, Polguj M, Fabiś J. The impact of arthroscopic capsular release in patients with primary frozen shoulder on shoulder muscular strength. Biomed Res Int 2014;2014:834283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Kraal T, The B, Boer R, et al. Manipulation under anesthesia versus physiotherapy treatment in stage two of a frozen shoulder: a study protocol for a randomized controlled trial. BMC Musculoskelet Disord 2017;18:412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Theodorides AA, Owen JM, Sayers AE, Woods DA. Factors affecting short- and long-term outcomes of manipulation under anaesthesia in patients with adhesive capsulitis of the shoulder. Shoulder Elbow 2014;6:245–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Woods DA, Loganathan K. Recurrence of frozen shoulder after manipulation under anaesthetic (MUA): the results of repeating the MUA. Bone Joint J 2017;99-B:812–7. [DOI] [PubMed] [Google Scholar]
- [24].Wang JP, Huang TF, Ma HL, Hung SC, Chen TH, Liu CL. Manipulation under anaesthesia for frozen shoulder in patients with and without non-insulin dependent diabetes mellitus. Int Orthop 2010;34:1227–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Warner JJP. Frozen shoulder: diagnosis and management. J Am Acad Orthop Surg 1997;5:130–40. [DOI] [PubMed] [Google Scholar]
- [26].Mitra R, Harris A, Umphrey C, Smuck M, Fredericson M. Adhesive capsulitis: a new management protocol to improve passive range of motion. Phys Med Rehabil 2009;1:1064–8. [DOI] [PubMed] [Google Scholar]
- [27].Li G, Thabane L, Papaioannou A, Ioannidis G, Levine MAH, Adachi JD. An overview of osteoporosis and frailty in the elderly. BMC Musculoskelet Disord 2017;18:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Mertens MG, Meert L, Struyf F, Schwank A, Meeus M. Exercise therapy is effective for improvement in range of motion, function, and pain in patients with frozen shoulder: a systematic review and meta-analysis. Arch Phys Med Rehabil 2021;S0003-9993(21)01366-6. [Online publication]. [DOI] [PubMed] [Google Scholar]