Abstract
Simple Summary
Recent clinical trials suggest that combination therapies that include either gemcitabine or 5-fluorouracil (5-FU) both give significant survival benefits for pancreatic cancer patients. The tumor level of the nucleoside transporter hENT1 is prognostic in patients treated with adjuvant gemcitabine but not adjuvant 5-FU. This work shows for the first time that hENT1 is only predictive of benefit from gemcitabine over 5-FU in patients with low levels of CDA transcript. A choice between adjuvant 5-FU based combination therapies (such as FOLFIRINOX) and gemcitabine-based therapy (e.g., GemCap) could be made based on a combination of hENT1 protein and CDA mRNA measured in a resected tumor.
Abstract
Gemcitabine or 5-fluorouracil (5-FU) based treatments can be selected for pancreatic cancer. Equilibrative nucleoside transporter 1 (hENT1) predicts adjuvant gemcitabine treatment benefit over 5-FU. Cytidine deaminase (CDA), inside or outside of the cancer cell, will deaminate gemcitabine, altering transporter affinity. ESPAC-3(v2) was a pancreatic cancer trial comparing adjuvant gemcitabine and 5-FU. Tissue microarray sections underwent in situ hybridization and immunohistochemistry. Analysis of both CDA and hENT1 was possible with 277 patients. The transcript did not correlate with protein levels for either marker. High hENT1 protein was prognostic with gemcitabine; median overall survival was 26.0 v 16.8 months (p = 0.006). Low CDA transcript was prognostic regardless of arm; 24.8 v 21.2 months with gemcitabine (p = 0.02) and 26.4 v 14.6 months with 5-FU (p = 0.02). Patients with low hENT1 protein did better with 5-FU, but only if the CDA transcript was low (median survival of 5-FU v gemcitabine; 29.3 v 18.3 months, compared with 14.2 v 14.6 with high CDA). CDA mRNA is an independent prognostic biomarker. When added to hENT1 protein status, it may also provide treatment-specific predictive information and, within the frame of a personalized treatment strategy, guide to either gemcitabine or 5FU for the individual patient.
Keywords: 5-fluorouracil, gemcitabine, pyrimidine, biomarker, predictive marker, prognostic marker, chemotherapy
1. Introduction
Pancreatic Ductal Adenocarcinoma (PDAC) is predicted to overtake breast cancer as the second leading cause of cancer death in the USA shortly, with limited survival despite improved therapeutic options [1,2,3].
Studies by the European Study Group for Pancreatic Cancer (ESPAC) and others show that adjuvant chemotherapy with either 5-fluorouracil (5-FU)/Folinic Acid (FA) or gemcitabine following surgery improves survival [4,5,6,7,8,9,10]. Combining gemcitabine or 5-FU with other chemotherapeutics further increases survival, including gemcitabine with capecitabine [11] or 5-FU with FA, irinotecan, and oxaliplatin (FOLFIRINOX) [12]. It is evident from trials in different population cohorts that selecting therapies based on individual profiling leads to improved survival rates [13]. Genetic variations in the patient and in their tumor [14] cause different protein patterns that can stratify patients into different sub-groups [15,16,17,18,19]. Broad classification allows association with prognosis [20], but the further subdivision is needed for treatment-specific predictions.
The activity of pyrimidine-based drugs is dependent on proteins involved in the trans-membrane uptake and metabolism of endogenous and exogenous pyrimidines [21,22]. Gemcitabine is a nucleoside analog of deoxycytidine that is transported into the cell by membrane transporter proteins, a major mediator being human equilibrative nucleoside transporter 1 (hENT1). We have previously reported that high protein expression of hENT1 was associated with improved overall survival in patients treated with gemcitabine in the ESPAC-3(v2) trial population, but not in those treated with 5-FU [23].
hENT1 has less affinity for cytidine than for its deaminated form (uridine) [24], it has much less affinity for nucleobases (e.g., 5-FU) than nucleosides (e.g., gemcitabine), although it has a greater affinity for nucleobases than other nucleoside transporters [25]. Deamination of gemcitabine by cytidine deaminase (CDA) outside of the cell would increase its transport into the cell, where it can be converted back into gemcitabine or exert a direct toxic effect [26]. Deamination inside the cell increases transport out. CDA is predominantly in the cytoplasm of cells but is also seen within the nucleus [27]. CDA can also be secreted into the extracellular space [28], and although intracellular CDA is the main determinant of gemcitabine sensitivity in cell lines, even with just pancreatic cancer cell lines, secreted CDA still accounts for a substantial amount of gemcitabine metabolism [29]. In vivo, CDA is produced by cancer and stromal cells. Bacteria found in PDAC (e.g., gammaproteobacteria) also produce CDA, perhaps contributing to resistance to gemcitabine [30].
Intracellular gemcitabine is phosphorylated by deoxycitidine kinase and nucleotide kinases to its active metabolites [31]. The phosphorylated forms of gemcitabine (as with all nucleotides) are not transported by hENT1, trapping them inside the cell. They can still be deaminated by CDA, reducing cytotoxicity as fluorouridine triphosphate is less readily incorporated into DNA [32].
It is estimated that approximately 90% of intracellular gemcitabine is metabolized by endogenous CDA [33], leaving little gemcitabine triphosphate to incorporate into DNA. Germline polymorphisms of CDA have been associated with response to gemcitabine [34] as has CDA expressed from bacteria [30] and induction of CDA expression by macrophages [35,36].
In this study, the expression of CDA mRNA and protein was analyzed in tissue from patients in the ESPAC-3(v2) trial. ESPAC-3(v2) compared gemcitabine with 5-fluorouracil plus FA (leucovorin) as adjuvant therapy. Since CDA will alter the import and export of gemcitabine and its metabolites into cells by hENT1, and hENT1 expression is known to be predictive for gemcitabine efficacy, we further assessed the combined predictive value of CDA with hENT1 expression.
2. Materials and Methods
2.1. Study Design
Translational analysis of ESPAC-3(v2) was granted ethical approval by the Liverpool Research Ethics Committee (07/H1005/87). Good Clinical Practice Standard Operating Procedures were employed throughout. The trial was originally analyzed on an intention-to-treat basis but for the translational study, patients in the treatment arms were included only if treatment was received [4,5,10]. This study was conducted in accordance with REMARK criteria [37].
2.2. Tissue Microarray Manufacture
Tissue microarrays (TMA) were manufactured as previously reported [23]. Arrays contained cores from 434 patients, 88 patients in duplicate per array, and a total of 4–8 cores per patient across arrays. Tumor regions were identified by an experienced pancreatic pathologist (FC) using haematoxylin and eosin-stained sections. Each core on each TMA was coded and linked separately to trial identifiers ensuring blinding of the analysts to outcome and treatment.
2.3. RNAscope® In Situ Hybridization (ISH)
Four µm TMA sections were baked at 60 °C for 60 min. Sections were deparaffinized in xylene, dehydrated in ethanol, and air-dried. RNAscope® 2.0HD Assay-Brown kits (ACD, Newark, CA, USA) were used, according to manufacturer’s instructions, to detect mRNA transcripts of CDA and hENT1: TMAs were heated to 100–104 °C in a citrate buffer to unmask target mRNA and permeabilize cells, followed by treatment with a protease inhibitor. The 15 probes for CDA hybridized between position 31 and 957 of the mature mRNA (NM_001785.2) and the 20 probes for hENT1 were designed to hybridize to the mature mRNA for gene SLC29A1 (NM_001078177.1) between positions 479 and 1774. PPIB and DapB were used as positive and negative controls. Probes were hybridized for 2 h at 40 °C. Signal amplification from the hybridized probes allowed detection of transcripts by 3,3′-diaminobenzidine. Counterstaining with hematoxylin localized the brown punctate dots within the cells.
2.4. Quantification Using RNAscope SpotStudio® Software
Sections were scanned with an Aperio ScanScope® microscopy scanner (Leica Microsystems [UK] Ltd., Milton Keynes, UK) at ×40 magnification. All cores were manually reviewed by FC, identifying cancerous regions. Damaged tissue was omitted, as were areas with debris/artifacts obscuring the area of interest. The pathologist and scientists involved were blinded to patient data, including treatment and outcome. RNAscope Spot Studio® v 1.0 Software (ACD) was used to detect and count dots on a cell by cell basis over the entire cancerous region. Full details of the assessment can be found in the Supplementary Materials. Parameters were the mean number of spots per cell (spot clusters were taken as equivalent to 10 spots when included) or proportion of cells with a given range of spots. The ranges were: Group 1, zero spots per cell, Group 2, 1–5 spots per cell and Group 3 ≥ 6 spots per cell. For each patient, the scores for individual cores were averaged as a mean value. The positive control, PPIB, showed detectable spots corresponding to individual transcripts whereas the negative control, DapB, had none. Following the computerized analysis of each TMA, a final manual quality check of every individual core was performed.
2.5. Immunohistochemistry
Immunohistochemistry with hENT1 antibody (10D7G2) or CDA antibody (ab137605, Abcam, Cambridge, UK) was performed as previously reported [23] The intensity of hENT1 cytoplasmic and membrane staining was scored by FC, accompanied by a research assistant (Elizabeth Garner), and H-scores were derived for each core ([intensity score] × [percentage of stained tumor cells]) with mean H-score calculated for each patient (Figure S2). For CDA an automated scoring system was used, described in Supplementary Materials.
2.6. Statistical Analysis
Overall survival, measured from the date of randomization, was estimated using the method of Kaplan–Meier [38] with unadjusted differences between groups assessed using the log-rank test. Analyses were carried out using Cox proportional hazards models to assess the impact of biomarkers, individually and in combination, on overall survival. All models included tumor stage, lymph node involvement, and resection margins as prognostic factors with the effect of biomarkers nested within treatment effect. This allowed for the effects of prognostic clinical factors to be calculated across the patient cohort, whereas the effects of biomarkers are allowed to differ between treatment arms.
The assumption of proportionality was assessed via inspection of the Schoenfeld residuals. Comparing the residuals against the rank sum of time produced a global test for proportionality.
All statistical tests were two-sided and p < 0.05 was considered significant. All analyses were carried out using R version 3.3 (R Core Team).
3. Results
Tissue samples representing 290 out of 434 patients (67%) were of sufficient quality to allow scoring of mRNA. Restricting to patients that had matched protein hENT1 H-scores [23] gave 277 patients for the final analysis.
3.1. Determining Expression Levels of hENT1 and CDA in PDAC
CDA and hENT1 mRNA expression was detected only in epithelial cells and not in the surrounding stromal matrix. Representative images of RNA analysis are shown in Figure 1. Different assessment methods were compared and found to give equivalent ranking (high to low expression) for the patients (Tables S1, S2 and Figure S1). Mean single spots per cell excluding clusters (MSPC) were chosen for all analyses. The relationship between mRNA and protein expression was investigated in patientC cores where matched mRNA and protein data were available, this showed no correlation for either CDA or hENT1 (see Figure S3).
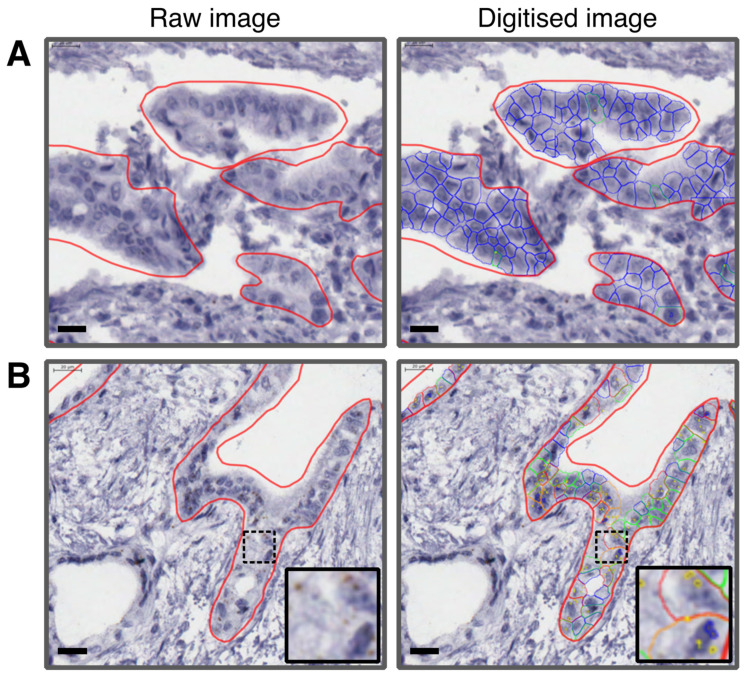
Figure 1.
Representative images of tissue cores showing CDA mRNA expression before and after SpotStudio® analysis. (A) Raw and digitized images of tissue expressing low CDA mRNA. (B) Raw and digitized images of tissue expressing high CDA, with inset example of cells with high CDA expression. Thick red line surrounds areas with tumor cells. Blue lines = Cells without any spots. Green lines = Cells with one single spot. Orange lines = Cells with between two and five spots. Thin red lines = Cells with six or more spots. Scale bar = 20 µm.
3.2. Univariate and Multivariable Analyses of Clinical and Pathological Characteristics
The ESPAC-3(v2) clinical trial was designed to show differences in survival according to treatment and so variation in clinicopathological features was minimized at trial randomization. However, univariate analysis by Cox proportional hazard regression, subdividing the chemotherapy treatment groups, showed that resection margin status (HR 1.56: 95% CI 1.20–2.03 p = 0.001), lymph node involvement (HR 1.94: 95% CI 1.39–2.71 p < 0.001) and tumor stage (HR 1.51: 95% CI 1.15–2.00 p = 0.004) were all significant prognostic factors for patients treated with 5-FU. Tumor diameter was a significant prognostic factor for gemcitabine (HR 1.64: 95% CI 1.14–2.39 p = 0.010), but did not reach statistical significance as a prognostic factor for 5-FU treated patients (HR 1.31: 95% CI 0.89–1.96 p = 0.177) (Table 1).
Table 1.
Univariate analysis of clinical and pathological factors in the 5-FU and gemcitabine arms.
| Summary Statistics | Hazard Ratio (95% Confidence Interval) | |||||
|---|---|---|---|---|---|---|
| Characteristic | Level | 5-Fluorouracil | Gemcitabine | 5-Fluorouracil | Gemcitabine | Total |
| Resection Margin | n = 132 | n = 145 | n = 277 | |||
| Negative | 70 (53%) | 86 (59%) | 1 | 1 | 1 | |
| Positive | 62 (47%) | 59 (41%) | 1.80 (1.23–2.63) | 1.35 (0.94–1.94) | 1.56 (1.20–2.03) | |
| Wald χ2 = 9.05, p = 0.003 * |
Wald χ2 = 2.62 p = 0.106 |
Wald χ2 = 11.22, p = 0.001 |
||||
| WHO | n = 132 | n = 145 | n = 277 | |||
| 0 | 52 (39%) | 49 (34%) | 1 | 1 | 1 | |
| 1 | 67 (51%) | 80 (55%) | 1.26 (0.86–1.96) | 1.40 (0.94–2.07) | 1.33 (1.01–1.76) | |
| 2 | 13 (10%) | 16 (11%) | 0.68 (0.29–1.59) | 1.24 (0.68–2.25) | 0.92 (0.56–1.53) | |
| Wald χ2 = 2.89, p = 0.236 |
Wald χ2 = 2.75 p = 0.253 |
Wald χ2 = 5.24, p = 0.073 |
||||
| Lymph Node Status | n = 132 | n = 145 | n = 277 | |||
| Negative | 29 (22%) | 29 (20%) | 1 | 1 | 1 | |
| Positive | 103 (78%) | 116 (80%) | 2.40 (1.47–3.90) | 1.56 (0.99–2.46) | 1.94 (1.39–2.71) | |
| Wald χ2 = 12.30, p = 0.001 |
Wald χ2 = 3.63, p = 0.057 |
Wald χ2 = 15.18 p < 0.001 |
||||
| Tumor Stage | n = 131 | n = 144 | n = 275 | |||
| 01/02 | 38 (29%) | 46 (32%) | 1 | 1 | 1 | |
| 03/04 | 93 (70%) | 98 (68%) | 1.69 (1.10–2.59) | 1.39 (0.95–2.01) | 1.51 (1.15–2.00) | |
| Wald χ2= 5.81, p = 0.016 |
Wald χ2 = 2.95, p = 0.086 |
Wald χ2 = 8.47, p = 0.004 |
||||
| Tumor Grade | N = 129 | n = 142 | n = 271 | |||
| Well | 7 (5%) | 10 (7%) | 1 | 1 | 1 | |
| Moderately | 89 (67%) | 98 (68%) | 0.60 (0.37–0.96) | 0.83 (0.44–1.58) | 0.72 (0.47–1.01) | |
| Poorly | 33 (25%) | 34 (23%) | 0.67 (0.35–1.28) | 1.19 (0.58–2.44) | 0.91 (0.55–1.51) | |
| Wald χ2 = 4.54, p = 0.103 |
Wald χ2 = 2.75, p = 0.753 |
Wald χ2 = 3.60 p = 0.165 |
||||
| Local Invasion | n = 132 | n = 142 | n = 274 | |||
| No | 73 (55%) | 72 (50%) | 1 | 1 | 1 | |
| Yes | 59 (45%) | 70 (48%) | 1.25 (0.85–1.84) | 1.10 (0.77–1.58) | 1.17 (0.90–1.52) | |
| Wald χ2 = 1.31, p = 0.252 |
Wald χ2 = 0.26, p = 0.607 |
Wald χ2 = 1.37 p = 0.242 |
||||
| Maximum Tumor diameter | n = 128 | n = 139 | n = 267 | |||
| <30 mm | 69 (52%) | 58 (40%) | 1 | 1 | 1 | |
| ≥30 mm | 59 (45%) | 81 (56%) | 1.31 (0.89–1.95) | 1.64 (1.13–2.39) | 1.47 (1.12–1.92) | |
| Wald χ2 = 1.82, p = 0.177 |
Wald χ2 = 6.73, p = 0.010 |
Wald χ2 = 7.84 p = 0.005 |
||||
| Diabetes mellitus | n = 129 | n = 141 | n = 270 | |||
| No | 102 (77%) | 106 (73%) | 1 | 1 | 1 | |
| Yes | 27 (20%) | 35 (24%) | 1.06 (0.65–1.75) | 0.99 (0.64–1.53) | 1.02 (0.74–1.41) | |
| Wald χ2 = 0.07, p = 0.797 |
Wald χ2 = 0.00, p = 0.951 |
Wald χ2 = 0.01, p = 0.905 |
||||
| Gender | n = 132 | n = 145 | n = 277 | |||
| Male | 75 (57%) | 88 (61%) | 1 | 1 | 1 | |
| Female | 57 (43%) | 57 (39%) | 0.88 (0.59–1.32) | 1.25 (0.86–1.81) | 1.06 (0.81–1.39) | |
| Wald χ2= 0.38, p = 0.537 |
Wald χ2 = 1.42, p = 0.234 |
Wald χ2 = 0.16, p = 0.686 |
||||
| Age, years | n = 132 | n = 145 | n = 277 | |||
| ≥64 | 65 (49%) | 80 (55%) | 1 | 1 | 1 | |
| <64 | 67 (51%) | 65 (45%) | 1.37 (0.93–2.02) | 0.84 (0.58–1.21) | 1.07 (0.83–1.40) | |
| Wald χ2= 2.55, p = 0.110 |
Wald χ2 = 0.90, p = 0.342 |
Wald χ2 = 0.28, p = 0.598 |
||||
| Smoking | n = 125 | n = 128 | n = 253 | |||
| Never | 52 (39%) | 58 (40%) | 1 | 1 | 1 | |
| Ex | 51 (39%) | 52 (36%) | 0.93 (0.60–1.43) | 1.08 (0.70–1.66) | 1.00 (0.74–1.35) | |
| Current | 22 (17%) | 18 (12%) | 0.91 (0.53–1.57) | 1.76 (1.02–3.05) | 1.20 (0.81–1.78) | |
| Wald χ2 = 0.17, p = 0.917 |
Wald χ2 = 4.16, p = 0.125 |
Wald χ2 = 0.95, p = 0.623 |
||||
* Significant values in bold.
3.3. Overall Survival Analysis
CDA protein expression level was not found to be prognostic for either treatment group (Figure S4A,B). hENT1 mRNA was not prognostic in patients treated with 5-FU; surprisingly there was a trend toward better survival in patients with low hENT1 mRNA treated with gemcitabine (Figure S4C,D).
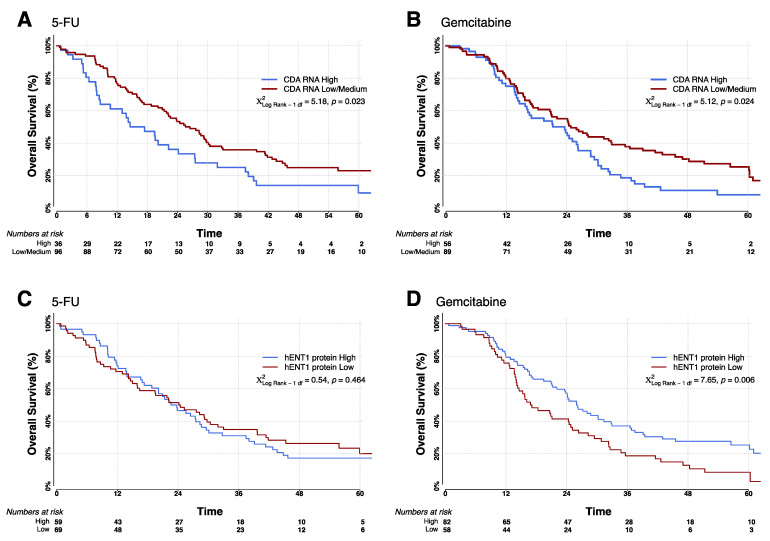
High expression of CDA mRNA conferred a poorer patient outcome regardless of chemotherapy; this was more pronounced in patients treated with 5-FU than in patients treated with gemcitabine. The median survival for patients treated with 5-FU expressing the upper tertile (high) CDA mRNA was 14.6 (95% CI = 8.4–24.1) months compared with 26.4 (95% CI = 21.4–29.7) months for the remaining patients, defined as low CDA expressers (χ2 = 5.18, p = 0.02) (Figure 2A). For patients treated with gemcitabine, high CDA expressers had a median survival of 21.2 (95% CI = 15.7–26.2) months compared with 24.8 (95% CI = 18.3–33.0) months for low CDA expressers (Figure 2B, χ2 = 5.14, p = 0.02).
Figure 2.
Kaplan-Meier survival curves separated by both treatment arms (5-FU and gemcitabine) and biomarker expression levels. (A,B): Survival curves for patients with low and high CDA mRNA levels (low ≤ 0.61, high > 0.61 MSPC), for patients randomized to adjuvant treatment with 5-FU (A) and gemcitabine (B). (C,D): Survival curves for low and high hENT1 expressing patients (low ≤48, high >48 H-Score), for patients randomized to adjuvant treatment with 5-FU (C) and gemcitabine (D). All groups and the number of at-risk individuals are shown in each graph. All p-values were determined by log-rank analyses using two-sided χ2 tests.
hENT1 protein expression, as expected from previously published data [23], was prognostic for patients treated with gemcitabine, despite 20% fewer patients being included in the current analysis (HR = 0.60 (95% CI = 0.42–0.86), Wald χ2 = 7.90, p = 0.05). The median survival was 26.0 (95% CI = 21.2–32.8) months for high expressers (as defined previously [23]) compared with 16.8 (95% CI = 14.1–24.8) months for low expressers (χ2 = 7.58, p = 0.006) (Figure 2C,D). There was no correlation between high or low hENT1 protein expression and survival in 5-FU treated patients.
To rule out confounding factors and investigate the interaction between the biomarker combination and treatment, CDA mRNA expression was first considered as a continuous variable. With Cox regression this was shown to be significantly prognostic with 5-FU treatment (Table 2), giving an HR of 4.35 (95% CI = 1.14–16.62, p = 0.03). The same trend was seen in the gemcitabine arm but in this case, it did not reach statistical significance (HR=3.15, 95% CI = 0.93–10.68, p = 0.07). When the Cox model was used with CDA mRNA expression subdivided into upper tertile and the rest, the same trends were seen in both arms, but in this case, it reached significance for gemcitabine and not 5-FU (5-FU: HR 1.41 (95% CI = 0.91−2.17), p = 0.12; gemcitabine: HR 1.62 (95% CI = 1.12−2.39), p = 0.011). The lack of significance for the 5-FU arm was largely due to the impact of nodal status on the model.
Table 2.
Cox regression analysis of biomarkers in the 5-FU and gemcitabine arms.
| 5FU | Gemcitabine | ||||||
|---|---|---|---|---|---|---|---|
| Characteristic | est (se) | HR (95% CI) | Pval | est (se) | HR (95% CI) | p-Value | |
| Single biomarker: CDA or hENT1 combined with stage, resection margin and lymph node involvement | |||||||
| CDA mRNA Expression | Per unit increase in MSPC | 1.47 (0.685) | 4.35 (1.14, 16.62) | 0.032 | 1.15 (0.623) | 3.15 (0.93, 10.68) | 0.066 |
| CDA mRNA Expression (Low vs. High) | Low | 1 (Reference) | 1 (Reference) | ||||
| High | 0.34 (0.221) | 1.41 (0.91, 2.17) | 0.120 | 0.49 (0.192) | 1.62 (1.12, 2.39) | 0.011 * | |
| hENT1 protein expression | Per unit increase in (log) H-score | −0.03 (0.159) | 0.97 (0.71, 1.33) | 0.861 | −0.26 (0.129) | 0.77 (0.60, 0.99) | 0.047 |
| hENT1 protein expression (Low vs. High) | Low | 1 (Reference) | 1 (Reference) | ||||
| High | 0.18 (0.207) | 1.21 (0.80, 1.81) | 0.374 | −0.43 (0.192) | 0.65 (0.45, 0.95) | 0.025 | |
| Multiple biomarker: CDA and hENT1 combined with stage, resection margin and lymph node involvement | |||||||
| CDA mRNA Expression (Low vs. High) | Low | 1 (Reference) | 1 (Reference) | ||||
| High | 0.39 (0.226) | 1.48 (0.95, 2.31) | 0.082 | 0.50 (0.193) | 1.65 (1.13, 2.41) | 0.009 | |
| hENT1 protein expression (Low vs. High) | Low | 1 (Reference) | 1 (Reference) | ||||
| High | 0.28 (0.212) | 1.32 (0.87, 1.99) | 0.193 | −0.41 (0.191) | 0.66 (0.46, 0.96) | 0.030 | |
* Significant values in bold.
Of the clinicopathological factors, only tumor stage correlated with CDA (Table S3), although this association was weak. All models included tumor stage, lymph node involvement, and resection margin. A test of proportionality was carried out (see Statistical Methods), this was not significant [ = 18.84, p = 0.096]. The term which had the biggest contribution towards non-proportionality was tumor stage. Removing this term had no effect on the model interpretation. Therefore, the tumor stage did not explain the relationship between CDA and survival (Table 2).
When CDA mRNA and protein were combined, the mRNA expression level, as expected, was prognostic in the 5-FU arm. Stratification with protein level made little difference. However, no significant prognostic effect of mRNA or protein was observed in the gemcitabine arm when the mRNA level was stratified by protein (Figure S5A,B). The small numbers in the subgroups (dividing by treatment, mRNA, protein, and nodal status) meant that regression analysis was inappropriate. Stratification of hENT1 protein with hENT1 mRNA showed that the protein remained a prognostic marker in the gemcitabine arm, but this was only statistically significant where hENT1 mRNA was low (Figure S5C,D).
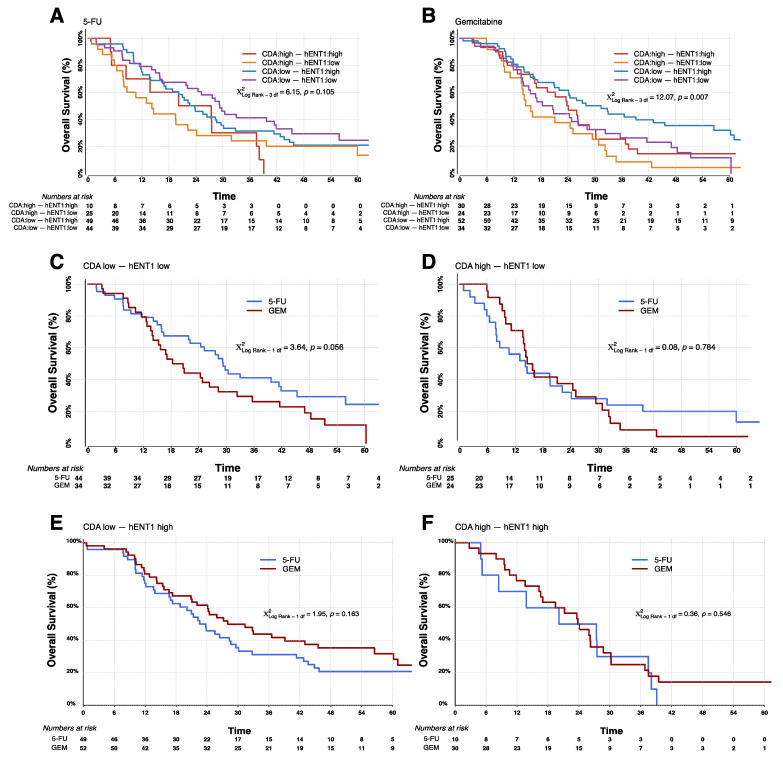
From Table 2 we know that hENT1 is a predictive marker in a model incorporating CDA mRNA. The question remained whether a combination of CDA mRNA and hENT1 protein would give greater predictive power than hENT1 alone. All combinations are shown in Table 3. Kaplan-Meier survival curves confirm that the combined biomarkers were only significantly prognostic in the gemcitabine treatment arm (Figure 3A,B). Correspondingly, 5-FU gave a survival advantage over gemcitabine in patients with low hENT1 and low CDA (Figure 3C) while, gemcitabine gave a survival advantage where hENT1 is high and there is low CDA (Figure 3E), but where CDA is high, hENT1 seems to have negligible predictive value (Figure 3D,F). With gemcitabine, patients expressing low CDA mRNA with high hENT1 protein have the longest overall median survival of 28.0 (95% CI = 21.1–45.5) months compared with 23.8 (95% CI = 16.6−28.7) months in patients with high hENT1 protein and high CDA mRNA. When treated with 5-FU, patients with high hENT1 protein and low CDA mRNA have a median survival of 22.6 (95% CI = 16.9–29.6) months, and patients with high hENT1 protein and high CDA mRNA 20.1 months (95% CI = 5.0−37.5). In contrast, individuals with low CDA mRNA and low hENT1 protein do better with 5-FU: median survival 29.3 (95% CI = 21.9–41.9) months compared to survival of 18.3 (95% CI = 13.9–28.3) months with gemcitabine (Table 3). This confirms the previous reports that patients with low hENT1 would benefit from 5-FU rather than gemcitabine. However, patients with low hENT1 and high levels of CDA transcript have poor survival when treated with either gemcitabine or 5-FU (median 14.6 and 14.2 months respectively).
Table 3.
Median overall survival in subgroups split by treatment arm, 5-FU or gemcitabine (GEM), cytidine deaminase (CDA) mRNA, and human equilibrative nucleotide transporter-1 (hENT1) protein status.
| Arm | Biomarker Expression (High or Low) | Number | Median OS | 95% Confidence Interval | Log Rank | p-Value |
|---|---|---|---|---|---|---|
| 5-FU/FA | CDA High | 36 | 14.6 | 8.4–24.1 | 5.17 | 0.0229 |
| CDA Low | 96 | 26.4 | 21.4–29.7 | |||
| GEM | CDA High | 56 | 21.2 | 15.7–26.2 | 5.14 | 0.0234 |
| CDA Low | 89 | 24.8 | 18.3–33.0 | |||
| 5-FU/FA | hENT1 High | 59 | 22.6 | 17.3–28.6 | 0.53 | 0.4658 |
| hENT1 Low | 69 | 24.1 | 15.9–30.4 | |||
| GEM | hENT1 High | 82 | 26.0 | 21.2–32.8 | 7.58 | 0.0059 |
| hENT1 Low | 58 | 16.8 | 14.1–24.8 | |||
| 5-FU | CDA Low, hENT1 Low | 44 | 29.3 | 21.9–41.9 | 6.14 | 0.1050 |
| CDA High, hENT1 Low | 25 | 14.2 | 7.9–24.1 | |||
| CDA Low, hENT1 High | 49 | 22.6 | 16.9–29.6 | |||
| CDA High, hENT1 High | 10 | 20.1 | 5.0–37.5 | |||
| GEM | CDA Low, hENT1 Low | 34 | 18.3 | 13.9–28.3 | 12.0 | 0.0073 |
| CDA High, hENT1 Low | 24 | 14.6 | 11.1–25.1 | |||
| CDA Low, hENT1 High | 52 | 28.0 | 21.1–45.5 | |||
| CDA High, hENT1 High | 30 | 23.8 | 16.6–28.7 |
Significant values in bold.
Figure 3.
Kaplan-Meier survival curves for analyses of combined CDA mRNA and hENT1 protein biomarker interaction looking at all expression level combinations (CDA low, hENT1 low; CDA high, hENT1 low; CDA low, hENT1 high; CDA high, hENT1 high). Graphs show response to treatment with 5-FU (A) and gemcitabine (B). In (C,D) the same data as above is presented showing the difference in survival for patients treated with 5-FU compared to gemcitabine in patients with low hENT1 protein and either low CDA (C) or high CDA (D), and patients with high hENT1 protein and either low CDA (E) or high CDA (F). All groups and the number of at-risk individuals are shown for each graph. All p-values were determined by log-rank analyses using two-sided χ2 tests.
4. Discussion
Analysis of CDA mRNA expression showed that it was prognostic for both 5-FU and gemcitabine, with high expression of CDA mRNA correlating with poor survival, regardless of the type of chemotherapy. This was not seen with CDA protein; no discernible difference in survival between low and high CDA in either treatment group.
CDA protein may come from a variety of sources, including bacteria, furthermore secreted CDA could be lost from the extracellular space during tissue processing. The mRNA sequence assayed is specific for the product of the cancer cell’s CDA gene. As ESPAC-3(v2) was an adjuvant study, the survival of the patient will depend on the response of metastatic or residual cancer cells to therapy. These residual cells will reside in a different environment to the primary tumor, but inherent factors (e.g., genetic or epigenetic) that influence expression may be shared with the resected tumor cells. Indeed there is compelling evidence that driver mutations are generally maintained in metastases and heterogeneity is due mainly to the gain (or loss) of passenger mutations [39].
High levels of hENT1 protein are significantly associated with survival only in gemcitabine-treated patients [23]. hENT1 mRNA expression was not prognostic with 5-FU and for gemcitabine, the trend was for longer survival with low (not high) mRNA.
hENT1 mRNA and protein expression showed no correlation, as also reported in previous studies [40,41]. Indeed, Tavano et al. described an inverse relationship between protein and mRNA expression [42]. This suggests that post-transcriptional mechanisms determine protein levels in pancreatic tumor cells. The immunohistochemistry protocol with the 10D7G2 antibody provides the most informative prognostic information
High expression of CDA protein has been linked to gemcitabine resistance [35,43]. In our study CDA mRNA was associated with a worse prognosis with gemcitabine treatment but was also prognostic with 5-FU treatment. CDA may influence the flux of 5-FU metabolism and its toxicity. Salvage pathways involving orotate phosphoribosyl transferase (OPRT) play an important role in pancreatic cancer cell metabolism [44]; conversion of cytidine to uracil (and then orotate) by CDA will change the rate of salvage and the rate of 5-FU metabolism and uptake [45]. Alternatively, low CDA may associate with better outcomes for reasons completely independent of benefits from 5-FU or gemcitabine, for example, because there is a lower proliferation rate and therefore less nucleoside turnover in less aggressive tumors.
CDA mRNA levels made the greatest difference to survival in patients treated with 5-FU who had low hENT1. By contrast, for patients with low hENT1 treated with gemcitabine the impact of CDA was marginal. Perhaps gemcitabine concentration is so low in these cancer cells that no survival benefit for the patient is offered, hence there is no benefit to be lost by the action of CDA. Alternatively, a low level of hENT1 could result in deaminated gemcitabine not being rapidly transported out of cells, reducing the benefit of having low levels of the deaminase.
Empirically, patients with low hENT1 and low CDA survive significantly better if given 5-FU than if given gemcitabine: median overall survival with 5-FU 29.3 months (95% CI: 21.9–41.9) compared to just 18.3 months (95% CI:13.9–28.3). While, patients with high hENT1 benefit from gemcitabine over 5-FU, irrespective of CDA mRNA levels, it is clear that patients with low hENT1 and low CDA would benefit more from 5-FU. Patients with low hENT1 and high CDA appear not to benefit from gemcitabine or 5-FU with a median survival of just 14 months in either case. The recommendation for the selection of adjuvant therapy would be to first test for the hENT1 protein level. It can be assumed that patients with a high level of hENT1 would benefit from gemcitabine, while those with a low level should have an additional analysis for CDA transcript. A low level of CDA mRNA would support the use of 5-FU based therapy. One caveat to this recommendation is that at present only one antibody (10D7G2) is appropriate for measuring hENT1 level for this purpose [46] and this is in short supply. Development of both hENT1 IHC and CDA ISH is ongoing.
In this paper, we are considering a subset of the patients in the JAMA paper describing the full set of patients on the ESPAC 3(v2) clinical trial [5]. Indeed the requirement for data with both CDA and hENT1 means that this group of patients is even more restricted than the patients assessed in the original paper describing the predictive value for hENT1 [23]. Bias in the selection of the patients is a concern. Notable differences in comparison to the previous reports are that performance status, tumor grade, local invasion, and smoking all failed to reach significance in the current publication, all of these can be explained by a reduction in power due to smaller numbers.
A similar reduction in power was seen in our JNCI paper which identified hENT1 as a biomarker. Median survivals for patients treated with gemcitabine having low hENT1/high hENT1 protein in our original paper was 17.1/26.2 months. These values are very close to the observation of 16.8/26.0 months seen with our more restricted population. For 5FU treated patients the values of 25.6/21.9 months in the previous paper were a little further from the values seen here (22.6/24.1 months), but still not suggestive of any particular bias.
5. Conclusions
We have demonstrated that patients stratified for adjuvant treatment with gemcitabine using hENT1 protein can be further stratified using CDA transcript level. The benefit of 5-FU over gemcitabine in patients with low hENT1 protein is lost in patients with high CDA. Further work is required to see how this can be applied to patients treated with combination therapies such as FOLFIRINOX, gemcitabine with nab-paclitaxel, or gemcitabine with capecitabine.
Acknowledgments
We are grateful to all of those who participated in, and contributed to, the ESPAC-1 and ESPAC-3 trials and provided the tissues. We thank Elizabeth Garner and Hayley Whitaker for technical assistance. We thank all of the Senior Trial Coordinators on the ESPAC trials including Charlotte Rawcliffe, Chloe Smith, Sara Martin and the principal Data Manager was Ronald Wall to whom we are all very grateful.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/cancers13225758/s1, Figure S1: Comparison of Analysis 1 vs. Analysis 2 SpotStudio® configurations. Figure S2: Examples of the range of CDA IHC staining intensity across different cores. Figure S3: Comparison of CDA and hENT1 mRNA expression with protein levels. Figure S4: Kaplan-Meier survival curves for analyses of CDA protein and hENT1 mRNA alone. Figure S5: Kaplan-Meier survival curves for analyses of combined CDA mRNA with CDA protein or combined hENT1 protein with hENT1 mRNA. Table S1: Parameter settings for each analysis to determine optimum spot detection and scoring. Table S2: Cox model fit for survival hazard using different methods of determining CDA mRNA expression. Table S3: Relationship between CDA mRNA expression and clinical and pathological factors in the 277 chemotherapy-treated patients. Supplementary Methods: (Quality assessment of the SpotStudio® platform: comparing the outcomes of two different software setups. Immunohistochemistry staining of tissue microarrays with CDA antibody. Quantification using Definiens® software).
Author Contributions
Conceptualization: K.A., N.O.E., D.H.P., A.E. and W.G. Resources: F.C., C.M.H., J.R.M., A.G.S., J.W.V., R.C., D.C., N.C.T., D.G., J.S., B.G., T.H., R.M.C., A.A., M.M.L., J.M., M.W.B., P.G. and J.P.N. Formal analysis: R.J., K.A., N.O.E., A.E. and W.G. Writing-original draft preparation: E.C., R.J, K.A., N.O.E., D.H.P., A.E., W.G., F.C. and C.M.H. Writing—review and editing: All authors. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by grant funding from Cancer Research UK and the NIHR which supported the Liverpool Experimental Cancer Medicine Centre (C18616/A25153), and North West Cancer Research (CR1185).
Institutional Review Board Statement
Translational analysis of ESPAC-3(v2) was granted ethical approval by the Liverpool Research Ethics Committee (07/H1005/87). All participants gave written informed consent to both participation in the trial and the use of their clinical samples for research.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to blinding of authors to trial data when carrying out experimental analysis.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Siegel R.L., Miller K.D., Jemal A. Cancer statistics, 2018. CA Cancer J. Clin. 2018;68:7–30. doi: 10.3322/caac.21442. [DOI] [PubMed] [Google Scholar]
- 2.Kleeff J., Korc M., Apte M., La Vecchia C., Johnson C.D., Biankin A.V., Neale R.E., Tempero M., Tuveson D.A., Hruban R.H., et al. Pancreatic cancer. Nat. Rev. Dis. Primers. 2016;2:16022. doi: 10.1038/nrdp.2016.22. [DOI] [PubMed] [Google Scholar]
- 3.Rahib L., Smith B.D., Aizenberg R., Rosenzweig A.B., Fleshman J.M., Matrisian L.M. Projecting cancer incidence and deaths to 2030: The unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014;74:2913–2921. doi: 10.1158/0008-5472.CAN-14-0155. [DOI] [PubMed] [Google Scholar]
- 4.Neoptolemos J., Stocken D.D., Friess H., Bassi C., Dunn J., Hickey H., Beger H., Fernandez-Cruz L., Dervenis C., Lacaine F., et al. A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer. N. Engl. J. Med. 2004;350:1200–1210. doi: 10.1056/NEJMoa032295. [DOI] [PubMed] [Google Scholar]
- 5.Neoptolemos J.P., Stocken D.D., Bassi C., Ghaneh P., Cunningham D., Goldstein D., Padbury R., Moore M.J., Gallinger S., Mariette C., et al. Adjuvant chemotherapy with fluorouracil plus folinic acid vs gemcitabine following pancreatic cancer resection: A randomized controlled trial. JAMA. 2010;304:1073–1081. doi: 10.1001/jama.2010.1275. [DOI] [PubMed] [Google Scholar]
- 6.Oettle H., Neuhaus P., Hochhaus A., Hartmann J.T., Gellert K., Ridwelski K., Niedergethmann M., Zulke C., Fahlke J., Arning M.B., et al. Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: The CONKO-001 randomized trial. JAMA. 2013;310:1473–1481. doi: 10.1001/jama.2013.279201. [DOI] [PubMed] [Google Scholar]
- 7.Oettle H., Post S., Neuhaus P., Gellert K., Langrehr J., Ridwelski K., Schramm H., Fahlke J., Zuelke C., Burkart C., et al. Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer-A Randomized controlled trial. JAMA. 2007;297:267–277. doi: 10.1001/jama.297.3.267. [DOI] [PubMed] [Google Scholar]
- 8.Valle J., Palmer D., Jackson R., Cox T., Neoptolemos J., Ghaneh P., Rawcliffe C.L., Bassi C., Stocken D.D., Cunningham D., et al. Optimal Duration and Timing of Adjuvant Chemotherapy After Definitive Surgery for Ductal Adenocarcinoma of the Pancreas: Ongoing Lessons From the ESPAC-3 Study. J. Clin. Oncol. 2014;32:504–512. doi: 10.1200/JCO.2013.50.7657. [DOI] [PubMed] [Google Scholar]
- 9.Neoptolemos J.P., Dunn J.A., Stocken D.D., Almond J., Link K., Beger H., Bassi C., Falconi M., Pederzoli P., Dervenis C., et al. ESPAC-1: A European, randomized controlled study of adjuvant chemoradiotherapy and chemotherapy in resectable pancreatic cancer. Lancet. 2001;358:1576–1585. doi: 10.1016/S0140-6736(01)06651-X. [DOI] [PubMed] [Google Scholar]
- 10.Neoptolemos J.P., Stocken D.D., Smith C.T., Bassi C., Ghaneh P., Owen E., Moore M., Padbury R., Doi R., Büchler M.W. Adjuvant 5-fluorouracil and folinic acid vs observation for pancreatic cancer: Composite data from the ESPAC-1 and -3(v1) trials. Br. J. Cancer. 2009;100:246–250. doi: 10.1038/sj.bjc.6604838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Neoptolemos J.P., Palmer D.H., Ghaneh P., Psarelli E.E., Valle J.W., Halloran C.M., Faluyi O., O’Reilly D.A., Cunningham D., Wadsley J., et al. Comparison of adjuvant gemcitabine and capecitabine with gemcitabine monotherapy in patients with resected pancreatic cancer (ESPAC-4): A multicentre, open-label, randomised, phase 3 trial. Lancet. 2017;389:1011–1024. doi: 10.1016/S0140-6736(16)32409-6. [DOI] [PubMed] [Google Scholar]
- 12.Conroy T., Hammel P., Hebbar M., Ben Abdelghani M., Wei A.C., Raoul J.-L., Choné L., Francois E., Artru P., Biagi J.J., et al. FOLFIRINOX or gemcitabine as adjuvant therapy for pancreatic cancer. N. Engl. J. Med. 2018;379:2395–2406. doi: 10.1056/NEJMoa1809775. [DOI] [PubMed] [Google Scholar]
- 13.Massard C., Michiels S., Ferté C., Le Deley M.-C., Lacroix L., Hollebecque A., Verlingue L., Ileana E., Rosellini S., Ammari S., et al. High-throughput genomics and clinical outcome in hard-to-treat advanced cancers: Results of the MOSCATO 01 trial. Cancer Discov. 2017;7:586–595. doi: 10.1158/2159-8290.CD-16-1396. [DOI] [PubMed] [Google Scholar]
- 14.Biankin A.V., Waddell N., Kassahn K.S., Gingras M.-C., Muthuswamy L.B., Johns A.L., Miller D.K., Wilson P.J., Patch A.-M., Wu J., et al. Pancreatic cancer genomes reveal aberrations in axon guidance pathway genes. Nature. 2012;491:399–405. doi: 10.1038/nature11547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Waddell N., Pajic M., Patch A.-M., Chang D.K., Kassahn K.S., Bailey P., Johns A.L., Miller D., Nones K., Quek K., et al. Whole genomes redefine the mutational landscape of pancreatic cancer. Nature. 2015;518:495–501. doi: 10.1038/nature14169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bailey P., Chang D.K., Nones K., Johns A.L., Patch A.-M., Gingras M.-C., Miller D.K., Christ A.N., Bruxner T.J.C., Quinn M.C., et al. Genomic analyses identify molecular subtypes of pancreatic cancer. Nature. 2016;531:47–52. doi: 10.1038/nature16965. [DOI] [PubMed] [Google Scholar]
- 17.Lowery M., Jordan E.J., Basturk O., Ptashkin R.N., Zehir A., Berger M.F., Leach T., Herbst B., Askan G., Maynard H., et al. Real-Time Genomic Profiling of Pancreatic Ductal Adenocarcinoma: Potential Actionability and Correlation with Clinical Phenotype. Clin. Cancer Res. 2017;23:6094–6100. doi: 10.1158/1078-0432.CCR-17-0899. [DOI] [PubMed] [Google Scholar]
- 18.Aguirre A.J., Nowak J.A., Camarda N., Moffitt R.A., Ghazani A.A., Hazar-Rethinam M., Raghavan S., Kim J., Brais L.K., Ragon D., et al. Real-time genomic characterization of advanced pancreatic cancer to enable precision medicine. Cancer Discov. 2018;8:1096–1111. doi: 10.1158/2159-8290.CD-18-0275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cancer Genome Atlas Research Network Electronic address aadhe, Cancer Genome Atlas Research N. Integrated genomic characterization of pancreatic ductal adenocarcinoma. Cancer Cell. 2017;32:e113. doi: 10.1016/j.ccell.2017.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moffitt R.A., Marayati R., Flate E.L., Volmar K.E., Loeza S.G.H., Hoadley K.A., Rashid N.U., Williams L.A., Eaton S.C., Chung A.H., et al. Virtual microdissection identifies distinct tumor- and stroma-specific subtypes of pancreatic ductal adenocarcinoma. Nat. Genet. 2015;47:1168–1178. doi: 10.1038/ng.3398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Costello E., Greenhalf W., Neoptolemos J.P. New biomarkers and targets in pancreatic cancer and their application to treatment. Nat. Rev. Gastroenterol. Hepatol. 2012;9:435–444. doi: 10.1038/nrgastro.2012.119. [DOI] [PubMed] [Google Scholar]
- 22.Young J.D., Yao S.Y.M., Sun L., Cass C.E., Baldwin S.A. Human equilibrative nucleoside transporter (ENT) family of nucleoside and nucleobase transporter proteins. Xenobiotica. 2008;38:995–1021. doi: 10.1080/00498250801927427. [DOI] [PubMed] [Google Scholar]
- 23.Greenhalf W., Ghaneh P., Neoptolemos J., Palmer D.H., Cox T., Lamb R.F., Garner E., Campbell F., Mackey J.R., Costello E., et al. Pancreatic cancer hENT1 expression and survival from gemcitabine in patients from the ESPAC-3 trial. J. Natl. Cancer Inst. 2014;106:djt347. doi: 10.1093/jnci/djt347. [DOI] [PubMed] [Google Scholar]
- 24.Ward J.L., Sherali A., Mo Z.-P., Tse C.-M. Kinetic and pharmacological properties of cloned human equilibrative nucleoside transporters, ENT1 and ENT2, stably expressed in nucleoside transporter-deficient PK15 cells. ENT2 exhibits a low affinity for guanosine and cytidine but a high affinity for inosine. J. Biol. Chem. 2000;275:8375–8381. doi: 10.1074/jbc.275.12.8375. [DOI] [PubMed] [Google Scholar]
- 25.Yao S.Y., Ng A.M., Cass C.E., Baldwin S.A., Young J.D. Nucleobase transport by human equilibrative nucleoside transporter 1 (hENT1) J. Biol. Chem. 2011;286:32552–32562. doi: 10.1074/jbc.M111.236117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Derissen E.J.B., Huitema A.D.R., Rosing H., Schellens J.H.M., Beijnen J.H. Intracellular pharmacokinetics of gemcitabine, its deaminated metabolite 2′,2′-difluorodeoxyuridine and their nucleotides. Br. J. Clin. Pharmacol. 2018;84:1279–1289. doi: 10.1111/bcp.13557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Somasekaram A., Jarmuz A., How A., Scott J., Navaratnam N. Intracellular localization of human cytidine deaminase. Identification of a functional nuclear localization signal. J. Biol. Chem. 1999;274:28405–28412. doi: 10.1074/jbc.274.40.28405. [DOI] [PubMed] [Google Scholar]
- 28.Ge Y., Jensen T.L., Stout M.L., Flatley R.M., Grohar P.J., Ravindranath Y., Matherly L.H., Taub J.W. The role of cytidine deaminase and GATA1 mutations in the increased cytosine arabinoside sensitivity of Down syndrome myeloblasts and leukemia cell lines. Cancer Res. 2004;64:728–735. doi: 10.1158/0008-5472.CAN-03-2456. [DOI] [PubMed] [Google Scholar]
- 29.Bjånes T.K., Jordheim L.P., Schjøtt J., Kamceva T., Cros-Perrial E., Langer A., de Garibay G.R., Kotopoulis S., Mc Cormack E., Riedel B. Intracellular cytidine deaminase regulates gemcitabine metabolism in pancreatic cancer cell lines. Drug Metab. Dispos. 2020;48:153–158. doi: 10.1124/dmd.119.089334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Geller L.T., Barzily-Rokni M., Danino T., Jonas O.H., Shental N., Nejman D., Gavert N., Zwang Y., Cooper Z.A., Shee K., et al. Potential role of intratumor bacteria in mediating tumor resistance to the chemotherapeutic drug gemcitabine. Science. 2017;357:1156–1160. doi: 10.1126/science.aah5043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Giovannetti E., Peters G.J. Molecular targets of gemcitabine action: Rationale for development of novel drugs and drug combinations. Curr. Pharm. Des. 2012;18:2811–2829. doi: 10.2174/138161212800626175. [DOI] [PubMed] [Google Scholar]
- 32.Honeywell R.J., Ruiz van Haperen V.W., Veerman G., Smid K., Peters G.J. Inhibition of thymidylate synthase by 2′,2′-difluoro-2′-deoxycytidine (Gemcitabine) and its metabolite 2′,2′-difluoro-2′-deoxyuridine. Int. J. Biochem. Cell Biol. 2015;60C:73–81. doi: 10.1016/j.biocel.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 33.Alvarellos M.L., Lamba J., Sangkuhl K., Thorn C.F., Wang L., Klein D.J., Altman R.B., Klein T.E. PharmGKB summary: Gemcitabine pathway. Pharm. Genom. 2014;24:564–574. doi: 10.1097/FPC.0000000000000086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tibaldi C., Giovannetti E., Vasile E., Mey V., Laan A.C., Nannizzi S., Di Marsico R., Antonuzzo A., Orlandini C., Ricciardi S., et al. Correlation of CDA, ERCC1, and XPD polymorphisms with response and survival in gemcitabine/cisplatin-treated advanced non-small cell lung cancer patients. Clin. Cancer Res. 2008;14:1797–1803. doi: 10.1158/1078-0432.CCR-07-1364. [DOI] [PubMed] [Google Scholar]
- 35.Weizman N., Krelin Y., Shabtayorbach A., Amit M., Binenbaum Y., Wong R.J., Gil Z. Macrophages mediate gemcitabine resistance of pancreatic adenocarcinoma by upregulating cytidine deaminase. Oncogene. 2013;33:3812–3819. doi: 10.1038/onc.2013.357. [DOI] [PubMed] [Google Scholar]
- 36.Binenbaum Y., Fridman E., Yaari Z., Milman N., Schroeder A., Ben David G., Shlomi T., Gil Z. Transfer of miRNA in macrophage-derived exosomes induces drug resistance in pancreatic adenocarcinoma. Cancer Res. 2018;78:5287–5299. doi: 10.1158/0008-5472.CAN-18-0124. [DOI] [PubMed] [Google Scholar]
- 37.McShane L.M., Altman D.G., Sauerbrei W., Taube S.E., Gion M., Clark G.M. Statistics Subcommittee of the NCIEWGoCD. REporting recommendations for tumour MARKer prognostic studies (REMARK) Br. J. Cancer. 2005;93:387–391. doi: 10.1038/sj.bjc.6602678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kaplan E., Meier P. Non-parametric estimation from incomplete observations. J. Am. Stat. Assoc. 1958;53:457–481. doi: 10.1080/01621459.1958.10501452. [DOI] [Google Scholar]
- 39.Zhong Y., Macgregor-Das A., Saunders T., Whittle M.C., Makohon-Moore A., Kohutek Z.A., Poling J., Herbst B.T., Javier B.M., Cope L., et al. Mutant p53 together with TGFbeta signaling influence organ-specific hematogenous colonization patterns of pancreatic cancer. Clin. Cancer Res. 2017;23:1607–1620. doi: 10.1158/1078-0432.CCR-15-1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Farrell J.J., Elsaleh H., Garcia M., Lai R., Ammar A., Regine W.F., Abrams R., Benson A.B., Macdonald J., Cass C.E., et al. Human equilibrative nucleoside transporter 1 levels predict response to gemcitabine in patients with pancreatic cancer. Gastroenterology. 2009;136:187–195. doi: 10.1053/j.gastro.2008.09.067. [DOI] [PubMed] [Google Scholar]
- 41.Giovannetti E., Del Tacca M., Mey V., Funel N., Nannizzi S., Ricci S., Orlandini C., Boggi U., Campani D., Del Chiaro M., et al. Transcription analysis of human equilibrative nucleoside transporter-1 predicts survival in pancreas cancer patients treated with gemcitabine. Cancer Res. 2006;66:3928–3935. doi: 10.1158/0008-5472.CAN-05-4203. [DOI] [PubMed] [Google Scholar]
- 42.Tavano F., Fontana A., Pellegrini F., Burbaci F.P., Rappa F., Cappello F., Copetti M., Maiello E., Lombardi L., Graziano P., et al. Modeling interactions between Human Equilibrative Nucleoside Transporter-1 and other factors involved in the response to gemcitabine treatment to predict clinical outcomes in pancreatic ductal adenocarcinoma patients. J. Transl. Med. 2014;12:248. doi: 10.1186/s12967-014-0248-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Funamizu N., Okamoto A., Kamata Y., Misawa T., Uwagawa T., Gocho T., Yanaga K., Manome Y. Is the resistance of gemcitabine for pancreatic cancer settled only by overexpression of deoxycytidine kinase? Oncol. Rep. 2009;23:471–475. doi: 10.3892/or_00000657. [DOI] [PubMed] [Google Scholar]
- 44.Nio Y., Toga T., Maruyama R., Fukushima M. Expression of orotate phosphoribosyl transferase in human pancreatic cancer: Implication for the efficacy of uracil and tegafur-based adjuvant chemotherapy. Oncol. Rep. 2007;18:59–64. doi: 10.3892/or.18.1.59. [DOI] [PubMed] [Google Scholar]
- 45.Traut T.W., Jones M.E. Uracil metabolism—UMP synthesis from orotic acid or uridine and conversion of uracil to beta-alanine: Enzymes and cDNAs. Prog. Nucleic Acid Res. Mol. Biol. 1996;53:1–78. doi: 10.1016/s0079-6603(08)60142-7. [DOI] [PubMed] [Google Scholar]
- 46.Raffenne J., Nicolle R., Puleo F., Le Corre D., Boyez C., Marechal R., Emile J.F., Demetter P., Bardier A., Laurent-Puig P., et al. hENT1 Testing in Pancreatic Ductal Adenocarcinoma: Are We Ready? A Multimodal Evaluation of hENT1 Status. Cancers. 2019;11:1808. doi: 10.3390/cancers11111808. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to blinding of authors to trial data when carrying out experimental analysis.