Throughout the COVID-19 pandemic, numerous reports have emerged that women account for a majority of confirmed COVID-19 cases and men represent a majority of confirmed deaths, leading to a higher calculated case fatality rate (CFR, deaths among confirmed cases) among men than among women (Alkhouli, Nanjundappa, Annie, Bates, & Bhatt, 2020; Dudley & Lee, 2020; Green, Nitzan, Schwartz, Niv, & Peer, 2021; Ramírez-Soto, Arroyo-Hernández, & Ortega-Cáceres, 2021; Undurraga, Chowell, & Mizumoto, 2021). There has been much speculation around the cause of this seemingly widespread pattern, with biological sex differences in genetics and hormones foregrounded as potential explanations (Al-Bari, Hossain, & Zahan, 2021; Alwani et al., 2021; Scully, Haverfield, Ursin, Tannenbaum, & Klein, 2020; Sharma, Volgman, & Michos, 2020). Yet there is an important limitation to comparing CFRs by sex: if men and women are not tested at similar rates, the resulting systematic skew in CFR denominators (confirmed cases) by sex limits the validity of any comparisons. The case study of COVID-19 offers an important teachable and generalizable example for women's health scholars of the caution that is needed in interpreting sex disparities in CFRs.
Available U.S. data indicate that women are tested for COVID-19 at higher rates than are men (Illinois Department of Public Health, 2021; Indiana State Department of Health, 2021; Minnesota Department of Health, 2021). There is evidence that this is not the result of a higher infection rate among women, because the percent positivity is higher among men in the two states where test results are available by sex: Minnesota (7.26% among men, 5.09% among women) and Missouri (9.89% among men, 7.54% among women) (Minnesota Department of Health, 2021; Missouri Department of Health and Senior Services, 2021). Rather, this pattern is likely due to several sex- and gender-linked factors that lead to wider surveillance-type testing of women in the United States. These factors include prioritization of pregnant people for testing (American College of Obstetricians and Gynecologists, 2020), high rates of testing among health care workers, who are disproportionately women (Cheeseman Day & Christnacht, 2019), and gendered health behaviors such as higher health care use among women (Vaidya, Partha, & Karmakar, 2012). Given the wider surveillance-type testing of women in the United States, it is likely that a greater number of cases, especially mild and asymptomatic cases, are detected in women than in men. Consequently, the CFR will seem to be artificially lower in women than in men, making sex comparisons of CFR an inappropriate measure of sex disparities in COVID-19 outcomes.
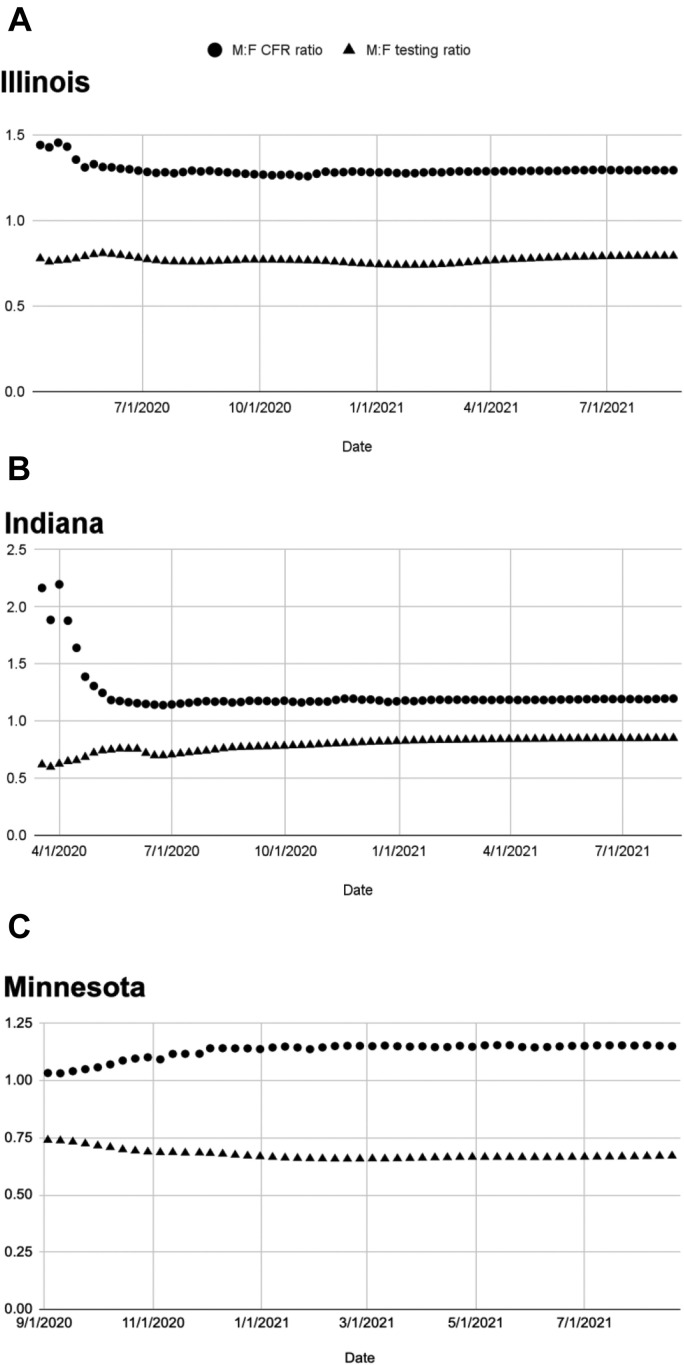
Publicly available data from U.S. state COVID-19 dashboards confirm that gender differences in COVID-19 testing predict sex disparities in calculated CFRs. Weekly sex-disaggregated data on cumulative COVID-19 testing ratios (number of tests conducted among men/boys compared with women/girls) and CFR ratios (women/girls as the reference) are shown in Figure 1 for the three states for which these data are publicly downloadable: Illinois, Indiana, and Minnesota (Illinois Department of Public Health, 2021; Indiana State Department of Health, 2021; Minnesota Department of Health, 2021). In Illinois, both the testing and CFR ratios have remained relatively stable over the course of the pandemic. In Indiana, as the testing ratio grew closer to 1, representing more equal testing among men and women, the CFR ratio fell closer to 1, indicating more similar fatality rates by sex. In Minnesota, as the testing ratio fell further below 1, representing a shrinking proportion of tests being conducted among men, the CFR ratio rose above 1, indicating more disparate fatality rates by sex.
Figure 1.
Cumulative testing ratio and CFR ratio by state. (A) Illinois, April 12, 2020, through August 22, 2021. (B) Indiana, March 25, 2020, through August 18, 2021. (C) Minnesota, September 3, 2020, through August 19, 2021.
Although these three states label their data as disaggregated by “gender,” it is not clear whether this refers to gender identity or sex assigned at birth. This ambiguity is a problem across U.S. state COVID-19 dashboards, limiting our understanding of gender and sex disparities in COVID-19 outcomes and precluding analysis of the effect of the pandemic on transgender and nonbinary individuals (Jillson & Shattuck-Heidorn, 2021). Here, we refer to gender/sex disparities, given that the data are not currently available to disentangle gender, sex, and their interaction in shaping COVID-19 outcomes (Danielsen & Noll, 2020).
Nevertheless, the available data do demonstrate that gender/sex comparisons of CFRs are subject to systematic bias owing to differential testing rates. Nonrandom COVID-19 testing in the population means that there is considerable uncertainty around CFR estimates in men and women (Mullahy, Venkataramani, Millimet, & Manski, 2021). Specifically, widespread lower testing among men compared with women likely artificially inflates the CFR among men, as demonstrated by the predictive, inverse relationship between testing skew and CFR ratio. The more disparate testing becomes between men and women, the greater the observed sex disparity in CFR; when testing becomes more similar, observed CFRs become more similar.
These data raise questions about sex comparisons of COVID-19 CFRs and claims that men, simply because they are male, are more likely to die than women once infected. This is not to say that any sex difference claim is misleading, or that there are no sex differences in COVID-19 outcomes. Much data have shown higher mortality among men during the COVID-19 pandemic, although this varies over time and place (Akter, 2021; Global Health 50/50, 2021) and by racial group (Rushovich et al., 2021) and may not be unexpected given higher baseline mortality in men (Krieger, Chen, & Waterman, 2020). Many sex- and gender-linked factors likely contribute to observed disparities in mortality, including differential distribution of comorbidities (James et al., 2018), longer life expectancy among women (Kochanek, Xu, & Arias, 2020), occupational sex segregation (U.S. Bureau of Labor Statistics, 2020), and gendered health behaviors (Haischer et al., 2020; Olcaysoy Okten, Gollwitzer, & Oettingen, 2020). However, it is evident that CFRs by themselves are an inappropriate metric to study gender/sex disparities in COVID-19. Analysis of data from outside the United States would be informative for assessing the relationship between testing skew and CFR ratio across contexts. For example, the inverse relationship likely holds true in India, but with higher testing rates among men; limited testing availability and lower health care access among women likely artificially inflates the CFR among women in India (Dehingia & Raj, 2021).
Women's health scholars and anyone interested in understanding and eliminating gender/sex disparities in health outcomes need reliable measures of those disparities. Moreover, accurate measures of the impact of a pandemic are necessary to inform public health surveillance programs, containment measures, and future pandemic preparedness. At a minimum, the reporting of CFRs by sex should note the possibility of testing skew. Data reporting should also make clear whether data are disaggregated by gender identity or birth sex. Ideally, additional variables including race, ethnicity, socioeconomic status, occupation, and comorbidity should also be collected and reported. These interacting social and demographic factors are necessary to better understand the distribution and causes of disparities in COVID-19 testing and outcomes (Rushovich et al., 2021). COVID-19 CFRs are an illustrative example of the need to critically examine commonly used metrics of sex disparities in order to avoid incomplete or inaccurate conclusions and to mount an effective public health response.
Biographies
Annika Gompers, MPhil, is a Clinical Data Coordinator in the Research Division of the Department of Obstetrics and Gynecology at Beth Israel Deaconess Medical Center. She works on studies relating to health care access and quality, gender bias, and sexual health.
Joseph D. Bruch, PhD, is a visiting scholar in Health Care Policy at Harvard Medical School. His research focuses on how health systems and health policies address social determinants of health.
Sarah S. Richardson, PhD, is Professor of the History of Science and of Studies of Women, Gender, and Sexuality at Harvard University. Her work argues for conceptual rigor and social responsibility in scientific research on sex, gender, sexuality, and reproduction.
Footnotes
The authors report no funding sources for this work and no financial conflicts of interest.
References
- Akter S. The gender gap in COVID-19 mortality in the United States. Feminist Economics. 2021;27(1–2):30–47. [Google Scholar]
- Al-Bari M.A.A., Hossain S., Zahan M.K.-E. Exploration of sex-specific and age-dependent COVID-19 fatality rate in Bangladesh population. World Journal of Radiology. 2021;13(1):1–18. doi: 10.4329/wjr.v13.i1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alkhouli M., Nanjundappa A., Annie F., Bates M.C., Bhatt D.L. Sex differences in case fatality rate of COVID-19: Insights from a multinational registry. Mayo Clinic Proceedings. 2020;95(8):1613–1620. doi: 10.1016/j.mayocp.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alwani M., Yassin A., Al-Zoubi R.M., Aboumarzouk O.M., Nettleship J., Kelly D.…Shabsigh R. Sex-based differences in severity and mortality in COVID-19. Reviews in Medical Virology. 2021;1–11 doi: 10.1002/rmv.2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American College of Obstetricians and Gynecologists Novel coronavirus 2019 (COVID-19). ACOG Clinical. 2020. www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2020/03/novel-coronavirus-2019 Available: Accessed 24/03/2021.
- Cheeseman Day J., Christnacht C. Women hold 76% of all health care jobs, gaining in higher-paying occupations. United States Census Bureau. 2019. www.census.gov/library/stories/2019/08/your-health-care-in-womens-hands.html Available: Accessed 24/03/2021.
- Danielsen A.C., Noll N. Communicating about COVID-19 and sex disparities: A guide for media, scientists, public health officials, and educators. GenderSci Lab. 2020. www.genderscilab.org/blog/covid-communication Available: Accessed 9/11/2021.
- Dehingia N., Raj A. Sex differences in COVID-19 case fatality: Do we know enough? Lancet Global Health. 2021;9(1):e14–e15. doi: 10.1016/S2214-109X(20)30464-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dudley J.P., Lee N.T. Disparities in age-specific morbidity and mortality from SARS-CoV-2 in China and the Republic of Korea. Clinical Infectious Diseases. 2020;71:863–865. doi: 10.1093/cid/ciaa354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Global Health 50/50 The COVID-19 sex-disaggregated data tracker. The Sex, Gender, and COVID-19 Project. 2021. https://globalhealth5050.org/the-sex-gender-and-covid-19-project/the-data-tracker/ Available: Accessed 9/11/2021.
- Green M.S., Nitzan D., Schwartz N., Niv Y., Peer V. Sex differences in the case-fatality rates for COVID-19—A comparison of the age-related differences and consistency over seven countries. PLoS One. 2021;16(4):e0250523. doi: 10.1371/journal.pone.0250523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haischer M.H., Beilfuss R., Hart M.R., Opielinski L., Wrucke D., Zirgaitis G.…Hunter S.K. Who is wearing a mask? Gender-, age-, and location-related differences during the COVID-19 pandemic. PLoS One. 2020;15(10):e0240785. doi: 10.1371/journal.pone.0240785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Illinois Department of Public Health COVID-19 county historical demographics. Illinois Department of Public Health. 2021. www.dph.illinois.gov/content/covid-19-county-historical-demographics Available: Accessed 24/08/2021.
- Indiana State Department of Health COVID-19 case demographics daily trend. Indiana Management Performance Hub. 2021. https://hub.mph.in.gov/dataset/covid-19-case-demographics-daily-trend Available: Accessed 24/08/2021.
- James S.L., Abate D., Abate K.H., Abay S.M., Abbafati C., Abbasi N.…Murray C.J.L. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–1858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jillson K., Shattuck-Heidorn H. The “unknown” side of state COVID-19 gender/sex reporting. GenderSci Lab. 2021. www.genderscilab.org/blog/unknown-covid19-gendersex-reporting Available: Accessed 09/11/2021.
- Kochanek K., Xu J., Arias E. Mortality in the United States, 2019 (No. 395; NCHS Data Brief). National Center for Health Statistics. 2020. www.cdc.gov/nchs/products/databriefs/db395.htm Available: Accessed 09/11/2021. [PubMed]
- Krieger N., Chen J.T., Waterman P.D. Excess mortality in men and women in Massachusetts during the COVID-19 pandemic. Lancet. 2020;395(10240):1829. doi: 10.1016/S0140-6736(20)31234-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minnesota Department of Health COVID-19 weekly report. Minnesota Department of Health. 2021. www.health.state.mn.us/diseases/coronavirus/stats/index.html Available: Accessed 24/08/2021.
- Missouri Department of Health and Senior Services Data downloads. MO.Gov. 2021. https://health.mo.gov/living/healthcondiseases/communicable/novel-coronavirus/data/data-download.php Available: Accessed 24/08/2021.
- Mullahy J., Venkataramani A., Millimet D.L., Manski C.F. Embracing uncertainty: The value of partial identification in public health and clinical research. American Journal of Preventive Medicine. 2021;61:e103–e108. doi: 10.1016/j.amepre.2021.01.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okten I.O., Gollwitzer A., Oettingen G. Gender differences in preventing the spread of coronavirus. Behavioral Science & Policy. 2020;6(2):109–122. [Google Scholar]
- Ramírez-Soto M.C., Arroyo-Hernández H., Ortega-Cáceres G. Sex differences in the incidence, mortality, and fatality of COVID-19 in Peru. PLoS One. 2021;16(6):e0253193. doi: 10.1371/journal.pone.0253193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rushovich T., Boulicault M., Chen J.T., Danielsen A.C., Tarrant A., Richardson S.S., Shattuck-Heidorn H. Sex disparities in COVID-19 mortality vary across US racial groups. Journal of General Internal Medicine. 2021;36:1696–1701. doi: 10.1007/s11606-021-06699-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scully E.P., Haverfield J., Ursin R.L., Tannenbaum C., Klein S.L. Considering how biological sex impacts immune responses and COVID-19 outcomes. Nature Reviews Immunology. 2020;20(7):442–447. doi: 10.1038/s41577-020-0348-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma G., Volgman A.S., Michos E.D. Sex differences in mortality from COVID-19 pandemic: Are men vulnerable and women protected? JACC: Case Reports. 2020;2(9):1407–1410. doi: 10.1016/j.jaccas.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Undurraga E.A., Chowell G., Mizumoto K. COVID-19 case fatality risk by age and gender in a high testing setting in Latin America: Chile, March–August 2020. Infectious Diseases of Poverty. 2021;10(1):11. doi: 10.1186/s40249-020-00785-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Bureau of Labor Statistics Labor Force Statistics from the Current Population Survey. 2020. www.bls.gov/cps/cpsaat11.htm Available: Accessed 24/03/2021.
- Vaidya V., Partha G., Karmakar M. Gender differences in utilization of preventive care services in the United States. Journal of Women’s Health. 2012;21(2):140–145. doi: 10.1089/jwh.2011.2876. [DOI] [PubMed] [Google Scholar]