Case
A 20 years old unmarried lady presented with acute onset behavioural changes, irrelevant talking that progressed into delirium of grandeur and persecution, repetitive seizure episodes and finally to a deteriorating general condition with poor Glasgow coma scale, requiring intubation and mechanical ventilation. Her Glasgow coma scale was E1VtM4, and she had perioral dyskinesias and abnormal limb movement. Various differentials were considered including viral or septic encephalitis, dyselectrolytemia, endocrine disorders, and psychiatric illness. She was started on antivirals and antibiotics empirically. Her MRI brain revealed symmetrical hyperintensity of the bilateral external capsules (Fig. 1).
Fig. 1.
MRI brain axial and coronal images show symmetrical involvement of bilateral external capsules. Medial temporal lobes are normal
Though initially there was no fever during the course of her admission, she developed ventilator associated pneumonia and multiple episodes of fever with urinary tract infection and bacteraemia requiring broad spectrum antibiotics meropenem and vancomycin. Serum anti-NMDA receptor antibodies were found to be positive, and a diagnosis of NMDA encephalitis was made. Subsequently, she received intravenous methylprednisolone, Rituximab 500 mg/week for 4 doses. She was planned to receive plasmapheresis after two weeks. However, there was no clinical improvement and she was tracheostomised. Meanwhile, an ultrasound of the pelvis revealed the presence of a complex ovarian cyst of 4*3 cm in the left adnexa. An MRI pelvis was done for further characterization of the left ovarian cystic lesion, which revealed a well-defined cyst with T1 and T2 hyperintense areas within, which showed complete loss of signal on fat suppressed sequences, consistent with fat. An MRI diagnosis of mature cystic teratoma was made (Fig. 2). In the absence of any improvement and the strong suspicion of an ovarian teratoma being the cause of the NMDA encephalitis, the family of the patient was counselled and with due consent, she was taken up for laparotomy under general anaesthesia for cystectomy/oophorectomy. The left ovary had multiple cysts with the largest being a 4*3 cm dermoid cyst with sebaceous material, hair and tooth which was confirmed later on histopathology (Fig. 3). Oophorectomy was performed on the same side to avoid any spill of the contents and as minimal normal ovarian tissue could be identified. The right ovary was preserved as it was normal.
Fig. 2.
Axial MR image shows a left adnexal well defined complex cystic mass with T1 and T2 bright signal intensity areas which show complete loss of signal on fat suppressed sequences, consistent with fat. Dermoid plug is also seen on the right lateral aspect of the cyst. Findings are suggestive of left ovarian teratoma
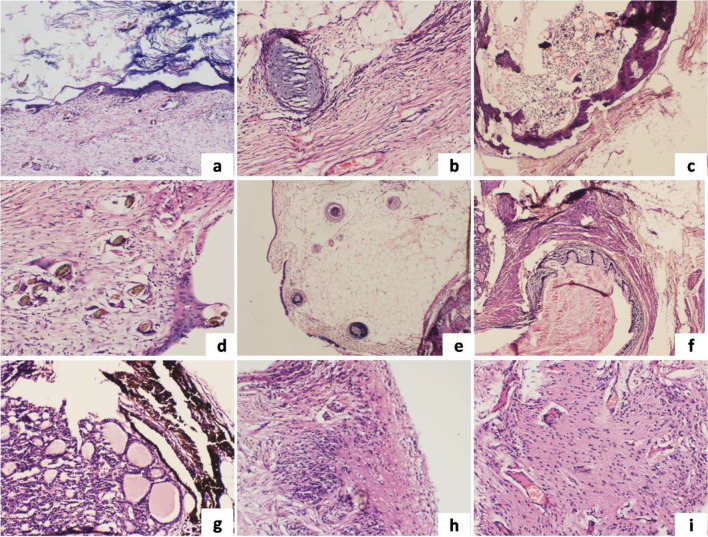
Fig. 3.
A panel of microphotograph from a case of Mature cystic teratoma; a A cyst wall lined by stratified squamous lining epithelium with keratin flakes in the lumen of the cyst (H&E x10X); b A focus showing cartilage (H&E x20X); c A focus showing a fragment of bone with bone marrow elements (H&E x10X); d Foreign body giant cell reaction to hair follicles and keratin (H&E x20X); e Hair follicles with adipose tissue (H&E x10X); f A focus showing intestinal lining epithelium surrounded by lymphoid tissue and smooth muscle layer (H&E x20X); g pigmented choroid with thyroid tissue (H&E x20X); h Mature glial tissue (H&E x10X); i Glial tissue with congested capillaries (H&E x20X)
Though the patient was running fever prior to surgery, peri-operative period was uneventful and the wound healed well. She received another 5-day course of immunoglobulins from day 5 of surgery. The dyskinesia and sepsis subsided over the next two weeks. Delirium and behavioral symptoms restarted but slowly subsided with anti-psychotics. She also underwent physiotherapy. In 4 weeks, she recovered well, was on spontaneous respiration, off tracheostomy tube. Her sensorium improved and good coordinated motor movements recovered. She was discharged after one month of postoperative stay in a stable condition. A year later, she is doing well and is able to cater to her daily activities.
Discussion
NMDA encephalitis was first reported by Dalmau et al. in 2007[1]; it is an autoimmune disorder associated with antibodies against N-methyl D-aspartate receptors in the hippocampus. The incidence of NMDA encephalitis is 1 per 1.5 million, and is the most common of all known autoimmune encephalitis. It is more common in females than males, usually presenting in the adults under 45 years of age. Few cases have been reported in pregnancy too [2].
Patients may present frequently in Neurology and Psychiatry services and thus the entity is lesser known among gynaecologists [3]. Ovarian teratomas constitute 94% of associated tumors, while others include extraovarian teratomas, or other tumors of the breast, lung, ovaries, thymus and pancreas [4]. In a systematic review by Acién et al., mature and immature teratomas comprised 74% and 21.6% of all cases [5]. The tumors are slightly more likely in the right ovary. They can vary in size from microscopic to 10 cm [5].
Typically, patients present with viral prodrome with fever or headaches, psychiatric symptoms, memory loss, cognition, speech, personality or behavioral alteration which may progress on to agitation, paranoid beliefs, seizures, decreased consciousness, respiratory failure and autonomic dysfunction [1, 4]. Movement disorders are common in children [4]. Abnormal movements like choreoathetosis, catatonic, ballistic or dyskinetic movements of limbs, abdominal wall, and opisthotonos-posturing may be seen. Mydriasis, diaphoresis, increased blood pressure, heart rate and respiration, and transient sleep abnormalities are reported [1].
Various authors have suggested that the teratomas contain neural elements with expression of NR2 receptors on the cells. Breech in immune tolerance is postulated which may be influenced by prodromal viral illness and genetic predisposition. Antibodies formed attach to the neural cells in the amygdala and the hippocampus.
EEG abnormalities are seen in 90% cases, while magnetic resonance imaging (MRI) changes and CSF abnormalities are seen in 33% and 73%, respectively [4]. EEG may show characteristic extreme delta-brush.[3] The sensitivity of NMDA-R antibodies is higher in the CSF than serum [4]. CSF lymphocytic pleocytosis is seen. Though proteins maybe increased in some, glucose levels are normal. Bacterial, viral and fungal tests are negative. Autoimmune workup helps to differentiate from other neurological conditions.
As for the ovarian tumor identification, expertise in gynaecological transvaginal ultrasonology clearly improves the sensitivity of ovarian tumor detection. MRI that has a high sensitivity for identifying fat in teratomas may aid in the diagnosis of small lesions or in cases the findings are inconclusive, especially using thin slices [3]. Still, in some cases, teratomas have only been found on post-mortem examination.
Management comprises immunotherapy and tumour removal. Immunotherapy includes steroids, IVIg and plasmapheresis, alone or in combination. Rituximab or monthly cyclophosphamide are useful. Tumor removal leads to rapid recovery as compared to immunotherapy alone [5].
Tumor removal should be done at the earliest, after hemodynamic and psychomotor stabilization of the patient. [5]. A systematic literature review shows that unilateral or bilateral adnexectomy was done in 38% of analyzed cases for mature teratoma. However, ovarian preserving surgery i.e. cystectomy in case of larger cysts and wedge resection of the ovary under transvaginal ultrasound guidance in case of microscopic lesions may help in preserving the ovarian function. Conservative surgery is further advocated as the lesions are usually benign, patients are usually in their reproductive age and may be lacking capacity for consent when surgery is planned [3]. Lesions suspected of immature teratomas should undergo oophrectomy and chemotherapy as required [3].
Titulaer et al reported a favorable outcome in 203/252(81%) while 9% died at a 24-month follow-up [4]. Early treatment by immunotherapy and surgery, lower symptom severity, and no ICU care were associated with better outcome. In their systematic review, Acién et al. found that 88% and 76% of patients with mature and immature teratomas had full recovery months or years later while 11.5% had permanent squeal and 7% died. The median time to discharge and acceptable recovery was 3 months.[5] Relapses may occur in 1/5th of patients, especially where a teratoma is not detected and removed. Dalmau et al. recommend long-term immunosuppression like mycophenolate mofetil and azathioprine for a year in these cases. Patients should undergo 3–6 monthly surveillance scans (MRI/USG) to look for development of teratoma for the next 2–3 years.
To conclude, NMDA encephalitis is a rare but potentially fatal condition associated with ovarian teratomas. Though it does not warrant removal of small asymptomatic teratomas for all, women and their close aides should be aware of the entity, as should be the medical and gynaecological community which will foster the early identification and management if this complication arises.
Sujata Siwatch
(MD, MPH) is working as Associate Professor in Department of Obstetrics & Gynecology, PGIMER, Chandigarh.
Declarations
Conflict of interest
The manuscript has been read and approved by all the authors, that the requirements for authorship as states earlier in this document have been met, and that each author believes that the manuscript represents honest work. There are no conflicts of interest.
Ethical approval
An informed consent for publication was obtained from the patient. The report is in accordance with the 1964 Helsinki Declaration.
Footnotes
Sujata Siwatch is an Associate Professor at the Department of Obstetrics and Gynaecology, PGIMER, Chandigarh, India; Vanita Jain is an Professor at Department of Obstetrics and Gynaecology, PGIMER, Chandigarh, India; Bharti Sharma is a Research Fellow at Department of Obstetrics and Gynaecology, PGIMER, Chandigarh, India; Veenu Singla is a Professor at Department of Radiodiagnosis & Imaging, PGIMER, Chandigarh, India; Karthik Vinay Mahesh is an Assistant Professor at Department of Neurology, PGIMER, Chandigarh, India. Nalini Gupta is a Professor at Department of Cytology and Gynecological Pathology, PGIMER, Chandigarh, India
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dalmau J, Tüzün E, Wu HY, Masjuan J, Rossi JE, Voloschin A, et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol. 2007;61(1):25–36. doi: 10.1002/ana.21050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Joubert B, García-Serra A, Planagumà J, Martínez-Hernandez E, Kraft A, Palm F, et al. Pregnancy outcomes in anti-NMDA receptor encephalitis: case series. NeurolNeuroimmunolNeuroinflammation. 2020;7(3):e668. doi: 10.1212/NXI.0000000000000668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jones BP, Rees R, Saso S, Stalder C, Smith JR, Yazbek J. Ultrasound-guided laparoscopic ovarian preserving surgery to treat anti-NMDA receptor encephalitis. BJOG Int J ObstetGynaecol. 2017;124(2):337–341. doi: 10.1111/1471-0528.14214. [DOI] [PubMed] [Google Scholar]
- 4.Titulaer MJ, McCracken L, Gabilondo I, Armangué T, Glaser C, Iizuka T, et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol. 2013;12(2):157–165. doi: 10.1016/S1474-4422(12)70310-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Acién P, Acién M, Ruiz-Maciá E, Martín-Estefanía C. Ovarian teratoma-associated anti-NMDAR encephalitis: a systematic review of reported cases. Orphanet J Rare Dis. 2014;9:157. doi: 10.1186/s13023-014-0157-x. [DOI] [PMC free article] [PubMed] [Google Scholar]