Abstract
Background:
Contradicting evidence regarding the effects of occlusal splint therapy in the management of Temporomandibular disorder (TMD) and promising results shown by muscle energy technique.
Aim:
To determine and compare the effects of occlusal splint therapy, muscle energy technique, and combined treatment with education for self-management and counseling in the management of TMD.
Study Design and Settings:
Randomized clinical trial.
Methodology:
A total of 160 participants diagnosed with TMD according to Diagnostic Criteria/TMD axis I were randomly allocated into four treatment groups with equal allocation ratio using random numbers table. The main inclusion criteria were the presence of pain in the preauricular area, TMJ and/or muscles of mastication and maximum mouth opening <40 mm. Group A participants received muscle energy technique, Group B participants received occlusal splint therapy, Group C participants received combined treatment, and Group D participants received education for self-management and counseling (control). Control group treatment was provided to all the trial participants.
Statistical Analysis:
Intragroup comparison was made using Friedman test and Wilcoxon test while intergroup comparison was done using Kruskal–Wallis test and Mann–Whitney U test.
Results:
Intensity of pain on a visual analog scale and maximum mouth opening were measured at baseline, at 1 week, at 2 weeks, at 1 month, and after 3 months.
Conclusion:
Muscle energy technique, occlusal splint therapy and combined treatment significantly reduce pain compared to controls and muscle energy and combined treatment are superior to other groups for mouth opening improvements in patients with TMD.
Keywords: Counseling, muscle energy technique, orofacial pain, self-management, stabilization splint, temporomandibular joint disorders
INTRODUCTION
Temporomandibular disorders (TMD) is a collective term that includes many clinical conditions involving the masticatory muscles or temporomandibular joints and associated structures which can be characterized by pain in the preauricular area, TMJ, or muscles of mastication; limitation or deviation in the mandibular range of movements; and TMJ sounds like clicking, popping and crepitus during mandibular function.[1] Other symptoms associated with TMD can be a headache, earache, poor quality of sleep, and depression.[2,3,4] TMD generally affect 5%–12% of the population.[1] It is estimated that 5%–6% of the population reporting clinically significant TMD-related jaw pain during their lifetime.[5,6] The etiology of TMD is multi-factorial and predisposing factors can be anatomical, traumatic, pathophysiological, or psychosocial.[7]
Muscle energy technique is an osteopathic manipulative therapy used in the treatment of musculoskeletal disorders. It has many subtypes; two commonly used subtypes are Postisometric relaxation and Reciprocal inhibition. Muscle energy technique is frequently used in treating excessively tensed muscle which restricts joint movements and causes pain.[8] The muscle energy technique is effective in reducing pain and improving motion in different parts of the body.[8,9] However, there is a lack of enough evidence regarding the use of muscle energy techniques in the management of TMD. Recently two studies have reported significant improvement in the symptoms of TMD with the use of muscle energy technique.[10,11]
In the literature, few studies have documented higher clinical success with the use of stabilization splint in the management of TMD.[12,13,14,15,16,17,18,19,20] Few have reported the role of stabilization splint in reducing muscle activity of temporalis and masseter muscle.[21,22,23] However, several studies have reported that the effects of stabilization splints in TMD are similar to nonoccluding control splints.[24,25,26,27,28,29,30] Because of this contradicting evidence in the literature regarding effects of stabilization splint therapy and promising results shown by the muscle energy technique in the management of TMD; this trial was initiated to determine and compare the effects of stabilization splint therapy, muscle energy technique, combined treatment, and education for self-management and counseling in the management of TMD. The null hypothesis states that there are no significant differences in the effects obtained by stabilization splint therapy, muscle energy technique, combined treatment, and education for self-management and counseling in the management of TMD after 3 months.
METHODOLOGY
Study design and settings
A prospective, multi-arm, multicenter, participants and analyst blinded randomized controlled trial was conducted at four different institutes from Dec 28, 2015 to March 12, 2020.
Sample size
A total sample size of 160 (n = 160) was obtained to achieve the required power of the study with 40 subjects in each group.
Ethics committee approval
Presentation of research protocol was done in front of the two institutional Ethics committees and approvals were received IRB no:- ECR/236/Indt/GJ/2015.
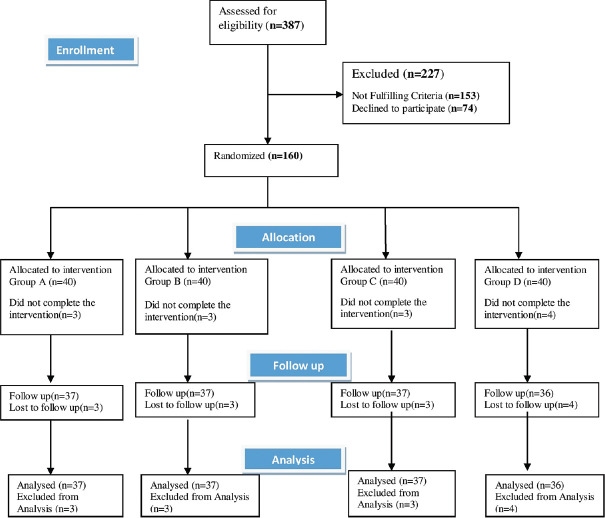
A total of 387 patients were diagnosed with TMD using DC/TMD (Axis I)[31] by the principal investigator and three other dentists. Those who fulfilled the inclusion criteria [Table 1] were given a brief explanation about the research and participants who signed the informed consent were included in the study [Figure 1].
Table 1.
Inclusion and exclusion criteria for trial participants
| Inclusion criteria | Exclusion criteria |
|---|---|
| Patients diagnosed with TMD according to DC/TMD axis I Pain in temporomandibular joint, muscles of mastications, or both plus any one/more of the following Presence of joint sounds like clicking or crepitus A history of jaw lock or limitation of opening or deviation TMJ or masticatory muscle tenderness to palpation Reduced mouth opening including the vertical overlap of <40 mm Sign and symptoms present for >4 weeks Patients of both gender Patients willing to participate in the research Age >20 years |
Patients who were under treatment of analgesics, NSAIDS, muscle relaxants or antidepressants Patients with the absence of maxillary and/or mandibular central incisors Patients who were unable to attend the hospital for the prescribed treatment period The patient who insisted on for a specific treatment (e.g., occlusal adjustments, medication) Presence of complete or removable partial prostheses with distal extension Patients with malignant tumours of the face and jaw History of fracture or surgery of jaw or TMJ Patients who had received any form of treatment for TMD in past Patients who had received orthodontic treatment in past Patients with oral submucous fibrosis |
TMD: Temporomandibular disorders, DC: Diagnostic criteria, NSAIDs: Nonsteroidal anti - inflammatory drugs, TMJ: Temporomandibular Joint
Figure 1.
Flow chart of trial participants according to CONSORT guidelines
Allocation sequence generation and allocation concealment
A person independent of the principal investigator and screening dentists had generated four comparison groups for 160 patients (n = 160) with simple randomization using equal allocation ratio by referring to a random numbers table, written it on the cards, and concealed the cards in sequentially numbered, sealed (with tamper-proof tape), opaque envelopes, and kept in a locker and opened only after envelopes had been irreversibly assigned to the participants.
Blinding
In this study, participants were blinded by not revealing to them detail about the treatment group they belonged to and recalling the participants of the same group on the same day. The statistical analyst was blinded by hiding from him the group names until data were analyzed.
Procedure
Group A (n = 40): Muscle energy technique
In the muscle energy technique following two techniques were used.
Post isometric relaxation
Patients were asked to lay supine on the dental chair with mouth open. The dentist placed gloved thumbs on the occlusal surface of patients' lower back teeth and patients were asked to close the jaw using 20% of total effort while the dentist provided equal resistance with the thumb so that no movement could occur [Figure 2]. After a 5 s hold, patients were asked to relax and the dentist gently opened the jaw to the maximum possible distance.[8] This procedure was repeated five times in 30 min session.
Figure 2.

Position of operator and patient during post isometric relaxation
Reciprocal inhibition
Patients were asked to sit in the dental chair in an upright position and to open the mouth to its comfortable limit. The dentist from behind the dental chair placed one hand below the mandible of the patient and grasped the forehead with another hand for stability [Figure 3]. Patients were then asked to attempt to open the mouth against the resistance applied by the dentist's hand placed below the mandible for 10 s. Then, patients were asked to open the mouth to its new barrier before repeating the procedure.[8] This procedure was repeated 5 times in 30 min session.
Figure 3.

Position of operator and patient during reciprocal inhibition
This muscle energy technique was given three times a week for four weeks.
Group B (n = 40): Occlusal splint therapy
Impressions of the patient's maxillary and mandibular arches were taken in perforated stock metal trays using irreversible hydrocolloid impression material and casts were obtained by pouring the impressions with dental stone. Facebow relation was recorded and the maxillary cast was mounted to a semi-adjustable articulator (Hanau wide vue). Patients were guided to close the jaw in centric relation using bimanual manipulation and this relation was transferred to the articulator using bite registration wax.
Stabilization splints were constructed by adapting ethylene-vinyl acetate sheets (2 mm thickness) on maxillary casts using a vacuum form machine and occlusal surfaces were modified with auto polymerizing acrylic resin to incorporate the contact of all mandibular teeth in centric relation [Figure 4], anterior guidance for disclusion of posterior teeth during protrusion and canine guidance for disclusion during lateral movements. Fit and occlusion of stabilization splints were verified in patients' mouths. Patients were advised to wear the splint at night for a minimum of 12 h. All patients were recalled for adjustments and follow-up at 24 h, 1 week, 2 weeks, 1 month, and 3 months.
Figure 4.

Stabilization splint in Centric relation position in patient's mouth
Group C (n = 40): Muscle energy technique + Occlusal splint therapy (combined treatment)
This group of patients received occlusal splint therapy and muscle energy technique.
Group D (n = 40):-Education for self-management, and counseling (control group)
In this group, patients were treated by education for self-management and counseling alone.
Patients were educated regarding the diagnosis and generally favorable prognosis of TMD when appropriate which included reassurance that TMD is a typically benign condition and self-limiting in the vast majority of cases. Patients were educated regarding the biopsychosocial etiology of TMD, sleep practices, time-limited use of analgesics, anatomy, and functions of TMJ and associated musculature.[32]
Patients were educated regarding identification, monitoring, and avoidance of any parafunctional behavior that can exacerbate the pain and were made conscious to avoid daytime clenching, clicking, or grinding of teeth.[32]
Patients were advised to avoid unilateral chewing, excessive talking, and chewing gum, to take proper rest and sleep, to do deep breathing exercises.
Advised a pain-free diet for 2 weeks followed by a review to check the tolerance to firmer consistency food.[32]
Instructed to apply moist heat to the area of discomfort for 10 min each time for 2–3 times/day.
All the trial participants received education for self-management and counseling in addition to the treatment specified for a particular group.
Outcome measurements and data collection
The primary outcome was measured as intensity of pain on a visual analog scale (VAS) and the secondary outcome was measured by maximum mouth opening as inter incisal opening plus the vertical overlap at baseline, at the end of 1 week, end of 2 weeks, end of 1 month, and follow-up at 3 months.
The VAS is a 10 cm horizontal line with marking from 0 to 10. The left end of the VAS is marked as 0 which describes no pain and the right end of VAS is marked as 10 which describes the worst pain. All patients were asked to mark the intensity of pain perceived by them, on VAS in data sheets provided to them, at described time intervals.
For maximum mouth opening, participants were asked to open the mouth as much as possible without pain, and the distance between labioincisal edges of maxillary and mandibular central incisors was measured vertically using calibrated, millimeter ruler and added by vertical incisal overlap to calculate maximum mouth opening.[1,33] Measurement of MMO was repeated twice and averaged to minimize error.
Statistical analysis
Intragroup comparison according to time interval was made using the Friedman test and if found significant a post hoc test was done by the Wilcoxon test. Intergroup comparison was made using the Kruskal–Wallis test and post hoc analysis was performed by the Mann–Whitney U-test. The Statistical Package for the Social Science (SPSS ver 22, IBM Corp., Armonk, N.Y., USA) was used for statistical analysis. The level of significance was kept at 5% (Confidence Interval 95%).
RESULTS
The age- and gender-wise distribution of trial participants are described in Table 2. The group-wise distribution of diagnostic subgroups of TMD is described in Table 3. The maximum number of patients were of Myofascial pain (28.12%) followed by Disc displacement with reduction (22.5%) and the least number of patients were of Disc displacement without reduction without limited opening (00).
Table 2.
Group wise age and gender distribution of trial participants
| Groups | Age (years) | Gender |
|
|---|---|---|---|
| Male, n (%) | Female, n (%) | ||
| Group A (n=40) | 37.60±10.55 | 23 (14.37) | 17 (10.63) |
| Group B (n=40) | 42.25±9.85 | 14 (8.75) | 26 (16.25) |
| Group C (n=40) | 40.42±10.41 | 18 (11.25) | 22 (13.75) |
| Group D (n=40) | 37.48±10.15 | 18 (11.25) | 22 (13.75) |
| Total (n=160) | 39.44±10.34 | 73 (45.63) | 87 (54.37) |
Table 3.
Group wise distribution of temporomandibular disorders sub groups
| TMD sub classification | Groups |
Total (n=160), n (%) | |||
|---|---|---|---|---|---|
| Group A (n=40), n (%) | Group B (n=40), n (%) | Group C (n=40), n (%) | Group D (n=40), n (%) | ||
| Local myalgia | 3 (1.87) | 3 (1.87) | 2 (1.25) | 2 (1.25) | 10 (6.25) |
| Myofascial pain | 9 (5.62) | 11 (6.87) | 14 (8.75) | 11 (6.87) | 45 (28.12) |
| Myofascial pain with referral | 5 (3.12) | 3 (1.87) | 3 (1.87) | 2 (1.25) | 13 (8.12) |
| Artharlgia | 2 (1.25) | 5 (3.12) | 5 (3.12) | 4 (2.5) | 16 (10) |
| Headache | 1 (0.62) | 0 | 1 (0.62) | 0 | 2 (1.25) |
| Disc displacement with reduction | |||||
| Right | 4 (2.5) | 5 (3.12) | 6 (3.75) | 6 (3.75) | 36 (22.5) |
| Left | 4 (2.5) | 6 (3.75) | 6 (3.75) | 3 (1.87) | |
| Disk displacement with reduction with intermittent locking | |||||
| Right | 4 (2.5) | 2 (1.25) | 2 (1.25) | 3 (1.87) | 15 (9.37) |
| Left | 2 (1.25) | 1 (0.62) | 1 (0.62) | 3 (1.87) | |
| Disk displacement without reduction with limited opening | |||||
| Right | 2 (1.25) | 1 (0.62) | 1 (0.62) | 2 (1.25) | 13 (8.12) |
| Left | 3 (1.87) | 2 (1.25) | 1 (0.62) | 3 (1.87) | |
| Disk displacement without reduction without limited opening | 0 | 0 | 0 | 0 | 0 |
| Degenerative joint disease | 3 (1.87) | 2 (1.25) | 0 | 2 (1.25) | 7 (4.37) |
| Subluxation | 2 (1.25) | 0 | 0 | 1 (0.62) | 3 (1.87) |
TMD: Temporomandibular disorders
Results are presented in detail in Tables 4, 4.1–4.3, 5, 5.1–5.3 and Figures 5 and 6 Pain decreased and maximum mouth opening increased for all the groups after 3 months in comparison to baseline [Tables 4 and 5]. However, the intragroup comparison shows that pain reduction was highly significant (P < 0.001) in three treatment groups (Group A, B, and C) as compared to the control group after 3 months [Table 4.3]; there was no significant (P > 0.05) difference in pain reduction between Group A, B and C after 3 months [Table 4.3]. Intragroup comparison has shown that there was a highly significant (P < 0.001) improvement of mouth opening for Group A and Group C patients as compared to Group B and Group D patients after 3 months. There was no significant (P > 0.05) difference between Group B and Group D in the improvement of mouth opening after 3 months. There was no significant (P > 0.05) difference between Group A and Group C in mouth opening improvement [Table 5.3].
Table 4.
Comparison of Visual Analog Scale at different time interval among groups
| Groups | Minimum | Maximum | Mean±SD | Median | P a |
|---|---|---|---|---|---|
| Baseline | |||||
| Group A (n=40) | 3.00 | 8.00 | 6.05±1.32 | 6.00 | 0.11 |
| Group B (n=40) | 2.00 | 9.00 | 5.75±1.41 | 6.00 | |
| Group C (n=40) | 3.00 | 9.00 | 6.10±1.53 | 6.00 | |
| Group D (n=40) | 3.00 | 9.00 | 5.45±1.28 | 5.50 | |
| After 1 week | |||||
| Group A (n=40) | 2.00 | 8.00 | 5.50±4.40 | 6.00 | 0.08 |
| Group B (n=40) | 2.00 | 9.00 | 5.37±1.29 | 5.00 | |
| Group C (n=39) | 3.00 | 9.00 | 5.64±1.42 | 6.00 | |
| Group D (n=40) | 3.00 | 8.00 | 4.95±1.26 | 5.00 | |
| After 2 weeks | |||||
| Group A (n=38) | 1.00 | 8.00 | 3.58±1.59 | 3.00 | 0.02* |
| Group B (n=39) | 1.00 | 7.00 | 3.97±1.39 | 4.00 | |
| Group C (n=38) | 1.00 | 8.00 | 3.79±1.34 | 4.00 | |
| Group D (n=39) | 2.00 | 8.00 | 4.51±1.47 | 4.00 | |
| After 1 month | |||||
| Group A (n=37) | 0 | 4.00 | 1.62±1.23 | 1.00 | <0.001** |
| Group B (n=37) | 0 | 5.00 | 2.24±1.30 | 2.00 | |
| Group C (n=37) | 0 | 5.00 | 1.43±1.37 | 1.00 | |
| Group D (n=36) | 0 | 7.00 | 3.75±1.70 | 4.00 | |
| After 3 months | |||||
| Group A (n=37) | 0 | 4.00 | 1.22±1.20 | 1.00 | <0.001** |
| Group B (n=37) | 0 | 5.00 | 1.49±1.45 | 1.00 | |
| Group C (n=37) | 0 | 4.00 | 0.89±1.17 | 1.00 | |
| Group D (n=36) | 0 | 7.00 | 3.47±1.98 | 3.00 |
aKruskal-Wallis test, *P<0.05 significant, **P<0.001 highly significant. SD: Standard deviation
Table 4.1.
Pair wise comparison of Visual Analog Scale after 2 weeks between groups
| Groups | Mean difference | P a |
|---|---|---|
| Group A versus Group B | −0.39 | 0.09 |
| Group A versus Group C | −0.21 | 0.27 |
| Group A versus Group D | −0.93 | 0.004* |
| Group B versus Group C | 0.18 | 0.41 |
| Group B versus Group D | −0.54 | 0.21 |
| Group C versus Group D | −0.72 | 0.04* |
aMann-Whitney U test, *P<0.05 significant
Table 4.3.
Pair wise comparison of Visual Analog Scale after 3 months between groups
| Groups | Mean difference | P a |
|---|---|---|
| Group A versus Group B | −0.27 | 0.53 |
| Group A versus Group C | 0.33 | 0.14 |
| Group A versus Group D | −2.25 | <0.001** |
| Group B versus Group C | 0.60 | 0.08 |
| Group B versus Group D | −1.98 | <0.001** |
| Group C versus Group D | −2.58 | <0.001** |
aMann-Whitney U test, *P<0.05 significant, **P<0.001 highly significant
Table 5.
Comparison of mouth opening (mm) at different time interval among groups
| Groups | Minimum | Maximum | Mean±SD | Median | P a |
|---|---|---|---|---|---|
| Baseline | |||||
| Group A (n=40) | 28.00 | 39.50 | 35.31±3.42 | 36.00 | 0.22 |
| Group B (n=40) | 30.00 | 39.00 | 35.85±2.61 | 36.00 | |
| Group C (n=40) | 29.00 | 39.00 | 34.45±3.10 | 35.00 | |
| Group D (n=40) | 29.00 | 39.50 | 35.51±2.69 | 36.00 | |
| After 1 week | |||||
| Group A (n=40) | 28.00 | 40.00 | 35.94±3.37 | 37.00 | 0.55 |
| Group B (n=40) | 30.00 | 39.00 | 35.90±2.59 | 36.00 | |
| Group C (n=39) | 29.00 | 40.50 | 35.27±3.04 | 35.00 | |
| Group D (n=40) | 29.00 | 40.00 | 35.55±2.71 | 36.00 | |
| After 2 weeks | |||||
| Group A (n=38) | 31.50 | 43.00 | 38.24±3.48 | 39.00 | 0.002* |
| Group B (n=39) | 30.00 | 39.00 | 36.04±2.58 | 36.50 | |
| Group C (n=38) | 31.00 | 43.00 | 37.13±3.06 | 37.00 | |
| Group D (n=39) | 29.00 | 40.00 | 35.54±2.75 | 36.00 | |
| After 1 month | |||||
| Group A (n=37) | 33.00 | 44.00 | 39.74±3.26 | 40.50 | <0.001** |
| Group B (n=37) | 30.00 | 39.50 | 36.48±2.35 | 37.00 | |
| Group C (n=37) | 34.00 | 44.00 | 38.84±3.20 | 39.00 | |
| Group D (n=36) | 29.00 | 40.00 | 35.76±2.90 | 36.00 | |
| After 3 months | |||||
| Group A (n=37) | 33.00 | 44.00 | 39.98±3.27 | 41.00 | <0.001** |
| Group B (n=37) | 30.50 | 41.50 | 37.16±2.61 | 37.00 | |
| Group C (n=37) | 34.00 | 45.00 | 39.47±3.17 | 39.00 | |
| Group D (n=36) | 29.00 | 40.00 | 36.07±2.91 | 37.00 |
aKruskal-Wallis test, *P<0.05 significant, **P<0.001 highly significant. SD: Standard deviation
Table 5.1.
Pair wise comparison of mouth opening (mm) after 2 weeks between groups
| Groups | Mean difference | P a |
|---|---|---|
| Group A versus Group B | 2.20 | 0.003* |
| Group A versus Group C | 1.11 | 0.13 |
| Group A versus Group D | 2.70 | 0.001* |
| Group B versus Group C | −1.09 | 0.14 |
| Group B versus Group D | 0.50 | 0.41 |
| Group C versus Group D | 1.59 | 0.04* |
aMann-Whitney U test, *P<0.05 significant
Table 5.3.
Pair wise comparison of mouth opening (mm) after 3 months between groups
| Groups | Mean difference | P a |
|---|---|---|
| Group A versus Group B | 2.82 | <0.001** |
| Group A versus Group C | 0.51 | 0.49 |
| Group A versus Group D | 3.92 | <0.001** |
| Group B versus Group C | −2.31 | 0.003* |
| Group B versus Group D | 1.09 | 0.13 |
| Group C versus Group D | 3.40 | <0.001** |
aMann-Whitney U test, *P<0.05 significant, **P<0.001 highly significant
Figure 5.
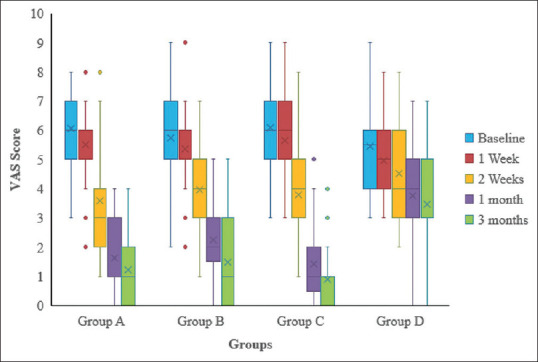
Graphical presentation for comparison of VAS score at different time interval among groups
Figure 6.
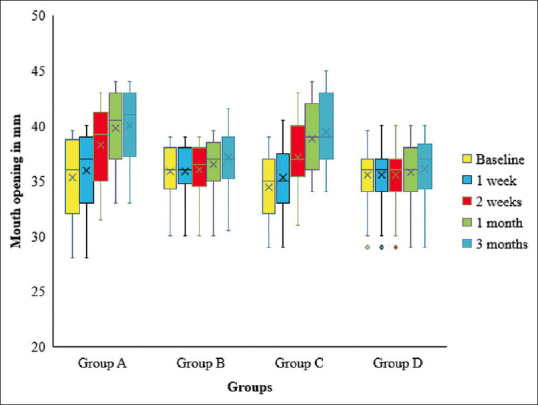
Graphical presentation for comparison of mouth opening (in mm) at different time interval among groups
Table 4.2.
Pair wise comparison of Visual Analog Scale after 1 month between groups
| Groups | Mean difference | P a |
|---|---|---|
| Group A versus Group B | −0.62 | 0.04* |
| Group A versus Group C | 0.19 | 0.36 |
| Group A versus Group D | −2.13 | <0.001** |
| Group B versus Group C | 0.81 | 0.004* |
| Group B versus Group D | −1.51 | <0.001** |
| Group C versus Group D | −2.32 | <0.001** |
aMann-Whitney U test, *P<0.05 significant, **P<0.001 highly significant
Table 5.2.
Pair wise comparison of mouth opening (mm) after 1 month between groups
| Groups | Mean difference | P a |
|---|---|---|
| Group A versus Group B | 3.36 | <0.001** |
| Group A versus Group C | 0.91 | 0.24 |
| Group A versus Group D | 3.98 | <0.001** |
| Group B versus Group C | −2.35 | 0.003* |
| Group B versus Group D | 0.72 | 0.29 |
| Group C versus Group D | 3.07 | <0.001** |
aMann-Whitney U test, *P<0.05 significant, **P<0.001 highly significant
DISCUSSION
The present trial was initiated to find quality evidence regarding the effects of occlusal splint therapy and muscle energy technique in the management of TMD. Pain decreased and maximum mouth opening increased in all four treatment groups, but intragroup comparisons revealed that experimental groups improved pain significantly more than the control group, and muscle energy technique and combined treatment groups improved mouth opening significantly more than occlusal splint therapy and education for self-management and counseling groups. Hence, null hypothesis is rejected. However, there was no significant difference in pain improvement between the muscle energy group, splint group, and combined treatment group after 3 months.
Patients treated by muscle energy technique reported a significant reduction in pain and significant improvement in maximum mouth opening at 2 weeks, 1 month, and 3 months' time intervals in comparison to baseline. These findings are in accordance with the findings of Rajadurai[10] and Trivedi et al.[11] This reduction in pain and improvement in maximum mouth opening can be attributed to the fact that muscle energy technique by stretching the muscle fibers stimulates the Golgi tendon receptors which inhibits the muscle tension leading to relaxation.[34] When the muscle actively contracts its antagonists reflexively relax because of which opening the mouth against resistance relaxes the elevator muscle and vice versa for depressor muscle which can increase MMO.[35] However, these findings are not in accordance with the findings of Freshwater and Gossling.[36] This type of contradictory findings might be because both asymptomatic and symptomatic participants with a limited range of mouth opening were recruited by Freshwater and Gossling so the participants without pain at the start of treatment may not have reported improvement in pain. The sample size of the study was also relatively small.
For Occlusal splint therapy, a significant reduction in pain and improvement in maximum mouth opening was observed after 3 months as compared to baseline. These findings are in accordance with the previous studies by several authors who also reported similar findings with the use of stabilization splint therapy.[12,13,14,15,16,17,18,19,20,37,38] For the combined treatment group also there was a significant reduction in pain and improvement in maximum mouth opening observed after 3 months as compared to baseline.
There was a statistically significant reduction in pain and no significant improvement in mouth opening for the occlusal splint therapy group in comparison to the control group at 1 month and 3 months. These findings are in accordance with the study by Wahlund et al.[39] and Alajbeg et al.[40] who had reported similar results. Present findings are partially supported by previous studies which have shown superior results with splint therapy in comparison to controls.[18,37,38,41,42,43,47] Present findings are not in accordance with some previous studies[19,20,21,22,23,24,25,33,44,45,46,48,49,50,51,52,53] according to which treatment provided in the control groups are similar in effects or superior to occlusal splint therapy. Possible reasons for this type of contradictory findings with the use of stabilization splint therapy could be due to the difference in sample size, different types of treatment in control groups (Some had used control splints, some had used exercise, brief information, or no treatment), no standard protocol for fabrication of stabilization splint used and difference in the duration of studies.
Occlusal splints when fabricated and adjusted properly improves the symptoms of TMD but the exact mechanism by which it works is still not very clear. However, it is believed that splint relaxes the muscles and allows the condyle to seat completely in centric relation, and reduces the overloading of the joint thereby improving the symptoms of TMD.
There was a highly significant reduction in pain and improvement in maximum mouth opening for the patients of counseling group after 3 months in comparison to baseline. These findings are similar to the findings by Pimental et al.,[54] Aggarawal VR et al.,[55] De Barros Pascoal et al.[56] However, the findings of the counseling group were not significant as compared to other groups.
Pain reduction was significant after 1 month and not significant after 3 months for the muscle energy group in comparison to the splint group. However, mouth opening improvement was highly significant for the muscle energy group as compared to the splint group after 1 month and 3 months. There was no statistically significant difference in pain reduction and mouth opening improvement between the muscle energy technique group and the combined treatment group at specified time intervals. These findings suggest that there are no additional benefits of using combined treatment over muscle energy technique alone.
Pain reduction on VAS for patients of combined treatment was statistically significant at 1 month but not significant at 3 months follow-up in comparison to occlusal splint therapy group patients. However, mouth opening improvement was statistically significant for the combined treatment group in comparison to the occlusal splint group after 1 month and 3 months. These findings are partially supported by the findings of Espi Lopez et al.[57] who reported that combined treatment protocol based on manual therapy plus splint therapy tends to improve pain, pain-induced dysfunction, and patients' self-perception of change in patients with TMD.
In the present study, we have used education for self-management and counseling as a treatment for the control group because it is reported that counseling was equally effective in improving muscle tenderness and maximum mouth opening as compared to the occlusal appliance, and counseling and self-management-based therapies are conservative, low cost, and beneficial treatment alternatives.[48]
To avoid inter-examiner error, all the treatments were provided and outcomes were measured by the principal investigator. However, because of that, it was not possible to blind the investigator and assessor which can be the possible limitation of the trial. In this trial, participants and statistical analysts were blinded. The possible heterogeneity of patients could not be taken into account in this study however homogeneity was increased by excluding the diseases or conditions which might have an effect on the treatment outcome of the research.[33] Because of the high number of patients with myofascial pain and disc displacement with the reduction in all groups and overlap of different diagnoses, groups were not homogeneous according to subclassification of TMD which is a limitation of the present study.
CONCLUSION
Within the limitation of this randomized controlled trial, we can conclude that;
Muscle energy technique is effective in reducing pain and increasing maximum mouth opening in patients with TMD at 3 months in comparison to education for self-management and counseling. Muscle energy technique is also effective in improving maximum mouth opening in patients with TMD at 3 months in comparison to occlusal splint therapy; however, its effects on pain reduction are similar to occlusal splint therapy at 3 months. Muscle energy technique provides reduction in pain and improvement in mouth opening similar to combined treatment in the management of TMD at 3 months
Occlusal splint therapy (stabilization splint) is effective in reducing the pain of TMD at 3 months in comparison to education for self-management and counseling; however, its effects on maximum mouth opening are similar to education for self-management and counseling. Occlusal splint therapy and combined treatment do not vary significantly in terms of pain reduction in patients with TMD at 3 months; however, combined treatment significantly improves maximum mouth opening in patients with TMD at 3 months in comparison to occlusal splint therapy
Combined treatment significantly reduces the pain and improves the maximum mouth opening in patients with TMD at 3 months in comparison to education for self-management and counseling.
Future recommendation
Further studies as randomized controlled trials are recommended for a longer duration to assess the effects of Muscle energy technique, occlusal splint therapy, and combined treatment on distinct subgroups of TMD.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: Review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6:301–55. [PubMed] [Google Scholar]
- 2.Gremillion HA. The prevalence and etiology of temporomandibular disorders and orofacial pain. Tex Dent J. 2000;117:30–9. [PubMed] [Google Scholar]
- 3.Benoit P. History and physical examination for TMD. In: Kraus SL, editor. Temporomandibular Disorders. 2nd ed. New York: Churchil Livingstone; 1994. pp. 71–98. [Google Scholar]
- 4.Morris S, Benjamin S, Gray R, Bennett D. Physical, psychiatric and social characteristics of the temporomandibular disorder pain dysfunction syndrome: The relationship of mental disorders to presentation. Br Dent J. 1997;182:255–60. doi: 10.1038/sj.bdj.4809362. [DOI] [PubMed] [Google Scholar]
- 5.Saghafi D, Curl DD. Chiropractic manipulation of anteriorly displaced temporomandibular disc with adhesion. J Manipulative Physiol Ther. 1995;18:98–104. [PubMed] [Google Scholar]
- 6.Goulet JP, Lavigne GJ, Lund JP. Jaw pain prevalence among French-speaking Canadians in Québec and related symptoms of temporomandibular disorders. J Dent Res. 1995;74:1738–44. doi: 10.1177/00220345950740110401. [DOI] [PubMed] [Google Scholar]
- 7.Chandu A, Suvinen TI, Reade PC, Borromeo GL. The effect of an interocclusal appliance on bite force and masseter electromyography in asymptomatic subjects and patients with temporomandibular pain and dysfunction. J Oral Rehabil. 2004;31:530–7. doi: 10.1111/j.1365-2842.2004.01377.x. [DOI] [PubMed] [Google Scholar]
- 8.Chaitow L, editor. Muscle Energy Techniques. 3rd ed. London, United Kingdom: Elsevier Health Science, Churchill Livingstone; 2006. [Google Scholar]
- 9.McCarty WL, Jr, Darnell MW. Rehabilitation of the temporomandibular joint through the application of motion. Cranio. 1993;11:298–307. doi: 10.1080/08869634.1993.11677982. [DOI] [PubMed] [Google Scholar]
- 10.Rajadurai V. The effect of muscle energy technique on temporomandibular joint dysfunction: A randomized clinical trial. [Last accessed on 2021 Jun 29];Asian J Sci Res. 2011 4:71–7. Available from: https://scialert.net/abstract/?doi=ajsr. 2011.71.77 . [Google Scholar]
- 11.Trivedi P, Bhatt P, Dhanakotti S, Nambi G. Comparison of muscle energy technique and myofascial release technique on pain and range of motion in patients with temporomandibular joint dysfunction: A randomized controlled study. Int J Physiother Res. 2016;4:1788–92. [Google Scholar]
- 12.Carraro JJ, Caffesse RG. Effect of occlusal splints on TMJ symptomatology. J Prosthet Dent. 1978;40:563–6. doi: 10.1016/0022-3913(78)90094-x. [DOI] [PubMed] [Google Scholar]
- 13.Clark GT. A critical evaluation of orthopedic interocclusal appliance therapy: Design, theory, and overall effectiveness. J Am Dent Assoc. 1984;108:359–64. doi: 10.14219/jada.archive.1984.0010. [DOI] [PubMed] [Google Scholar]
- 14.Kreiner M, Betancor E, Clark GT. Occlusal stabilization appliances. Evidence of their efficacy. J Am Dent Assoc. 2001;132:770–7. doi: 10.14219/jada.archive.2001.0274. [DOI] [PubMed] [Google Scholar]
- 15.Ekberg E, Nilner M. Treatment outcome of appliance therapy in temporomandibular disorder patients with myofascial pain after 6 and 12 months. Acta Odontol Scand. 2004;62:343–9. doi: 10.1080/00016350410010063. [DOI] [PubMed] [Google Scholar]
- 16.Kirov DN, Krastev DS. Efficacy of stabilization splint in management of myogenous temporomandibular disorders. Int J Sci Res. 2014;3:2012–5. [Google Scholar]
- 17.Zhang C, Wu JY, Deng DL, He BY, Tao Y, Niu YM, et al. Efficacy of splint therapy for the management of temporomandibular disorders: A meta-analysis. Oncotarget. 2016;7:84043–53. doi: 10.18632/oncotarget.13059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang FY, Wang XG, Dong J, Zhang JF, Lü YL. Effect of occlusal splints for the management of patients with myofascial pain: A randomized, controlled, double-blind study. Chin Med J (Engl) 2013;126:2270–5. [PubMed] [Google Scholar]
- 19.Giannakopoulos NN, Katsikogianni EN, Hellmann D, Eberhard L, Leckel M, Schindler HJ, et al. Comparison of three different options for immediate treatment of painful temporomandibular disorders: A randomized, controlled pilot trial. Acta Odontol Scand. 2016;74:480–6. doi: 10.1080/00016357.2016.1204558. [DOI] [PubMed] [Google Scholar]
- 20.Seifeldin SA, Elhayes KA. Soft versus hard occlusal splint therapy in the management of temporomandibular disorders (TMDs) Saudi Dent J. 2015;27:208–14. doi: 10.1016/j.sdentj.2014.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Solberg WK, Clark GT, Rugh JD. Nocturnal electromyographic evaluation of bruxism patients undergoing short term splint therapy. J Oral Rehabil. 1975;2:215–23. doi: 10.1111/j.1365-2842.1975.tb00915.x. [DOI] [PubMed] [Google Scholar]
- 22.Lobbezoo F, van der Glas HW, van Kampen FM, Bosman F. The effect of an occlusal stabilization splint and the mode of visual feedback on the activity balance between jaw-elevator muscles during isometric contraction. J Dent Res. 1993;72:876–82. doi: 10.1177/00220345930720050801. [DOI] [PubMed] [Google Scholar]
- 23.Daif ET. Correlation of splint therapy outcome with the electromyography of masticatory muscles in temporomandibular disorder with myofascial pain. Acta Odontol Scand. 2012;70:72–7. doi: 10.3109/00016357.2011.597776. [DOI] [PubMed] [Google Scholar]
- 24.Nilner M, Ekberg E, Doepel M, Andersson J, Selovuo K, Le Bell Y. Short-term effectiveness of a prefabricated occlusal appliance in patients with myofascial pain. J Orofac Pain. 2008;22:209–18. [PubMed] [Google Scholar]
- 25.Wassell RW, Adams N, Kelly PJ. Treatment of temporomandibular disorders by stabilising splints in general dental practice: Results after initial treatment. Br Dent J. 2004;197:35–41. doi: 10.1038/sj.bdj.4811420. [DOI] [PubMed] [Google Scholar]
- 26.Carlsson GE, Magnusson T. Treatment modalities. In: Bywaters LC, editor. Management of Temporomandibular Disorders in the General Dental Practice. Chicago: Quintessence; 1999. pp. 93–103. [Google Scholar]
- 27.Carlson CR, Bertrand PM, Ehrlich AD, Maxwell AW, Burton RG. Physical self-regulation training for the management of temporomandibular disorders. J Orofac Pain. 2001;15:47–55. [PubMed] [Google Scholar]
- 28.Truelove E, Huggins KH, Mancl L, Dworkin SF. The efficacy of traditional, low-cost and nonsplint therapies for temporomandibular disorder: A randomized controlled trial. J Am Dent Assoc. 2006;137:1099–107. doi: 10.14219/jada.archive.2006.0348. [DOI] [PubMed] [Google Scholar]
- 29.Niemelä K, Korpela M, Raustia A, Ylöstalo P, Sipilä K. Efficacy of stabilisation splint treatment on temporomandibular disorders. J Oral Rehabil. 2012;39:799–804. doi: 10.1111/j.1365-2842.2012.02335.x. [DOI] [PubMed] [Google Scholar]
- 30.Shedden Mora MC, Weber D, Neff A, Rief W. Biofeedback-based cognitive-behavioral treatment compared with occlusal splint for temporomandibular disorder: A randomized controlled trial. Clin J Pain. 2013;29:1057–65. doi: 10.1097/AJP.0b013e3182850559. [DOI] [PubMed] [Google Scholar]
- 31.Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP, et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: Recommendations of the International RDC/TMD Consortium NetworkFNx01 and Orofacial Pain Special Interest Group†. J Oral Facial Pain Headache. 2014;28:6–27. doi: 10.11607/jop.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Durham J, Al-Baghdadi M, Baad-Hansen L, Breckons M, Goulet JP, Lobbezoo F, et al. Self-management programmes in temporomandibular disorders: Results from an international Delphi process. J Oral Rehabil. 2016;43:929–36. doi: 10.1111/joor.12448. [DOI] [PubMed] [Google Scholar]
- 33.Katyayan PA, Katyayan MK, Shah RJ, Patel G. Efficacy of appliance therapy on temporomandibular disorder related facial pain and mandibular mobility: A randomized controlled study. J Indian Prosthodont Soc. 2014;14:251–61. doi: 10.1007/s13191-013-0320-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roberts BL. Soft tissue manipulation: Neuromuscular and muscle energy techniques. J Neurosci Nurs. 1997;29:123–7. doi: 10.1097/01376517-199704000-00006. [DOI] [PubMed] [Google Scholar]
- 35.Royder JO. Structural influences in temporomandibular joint pain and dysfunction. J Am Osteopath Assoc. 1981;80:460–7. [PubMed] [Google Scholar]
- 36.Freshwater Z, Gossling C. The effect of specific iso metric muscle energy technique on range of opening of TMJ: A pilot study. J Osteopath Med. 2003;6:36. [Google Scholar]
- 37.Hosgor H, Bas B, Celenk C. A comparison of the outcomes of four minimally invasive treatment methods for anterior disc displacement of the temporomandibular joint. Int J Oral Maxillofac Surg. 2017;46:1403–10. doi: 10.1016/j.ijom.2017.05.010. [DOI] [PubMed] [Google Scholar]
- 38.Zhang SH, He KX, Lin CJ, Liu XD, Wu L, Chen J, et al. Efficacy of occlusal splints in the treatment of temporomandibular disorders: A systematic review of randomized controlled trials. Acta Odontol Scand. 2020;78:580–9. doi: 10.1080/00016357.2020.1759818. [DOI] [PubMed] [Google Scholar]
- 39.Wahlund K, List T, Larsson B. Treatment of temporomandibular disorders among adolescents: A comparison between occlusal appliance, relaxation training, and brief information. Acta Odontol Scand. 2003;61:203–11. doi: 10.1080/00016350310003891. [DOI] [PubMed] [Google Scholar]
- 40.Alajbeg I, Živković K, Gikić M. The role of stabilization splint in the treatment of temporomandibular disorders. Acta Med Croatica. 2015;69:33–43. [PubMed] [Google Scholar]
- 41.Fricton J, Look JO, Wright E, Alencar FG, Jr, Chen H, Lang M, et al. Systematic review and meta-analysis of randomized controlled trials evaluating intraoral orthopedic appliances for temporomandibular disorders. J Orofac Pain. 2010;24:237–54. [PubMed] [Google Scholar]
- 42.Nitecka-Buchta A, Marek B, Baron S. CGRP plasma level changes in patients with temporomandibular disorders treated with occlusal splints – A randomised clinical trial. Endokrynol Pol. 2014;65:217–23. doi: 10.5603/EP.2014.0030. [DOI] [PubMed] [Google Scholar]
- 43.Conti PC, Corrêa AS, Lauris JR, Stuginski-Barbosa J. Management of painful temporomandibular joint clicking with different intraoral devices and counseling: A controlled study. J Appl Oral Sci. 2015;23:529–35. doi: 10.1590/1678-775720140438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kuzmanovic Pficer J, Dodic S, Lazic V, Trajkovic G, Milic N, Milicic B. Occlusal stabilization splint for patients with temporomandibular disorders: Meta-analysis of short and long term effects. PLoS One. 2017;12:e0171296. doi: 10.1371/journal.pone.0171296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vrbanović E, Alajbeg IZ. Long-term effectiveness of occlusal splint therapy compared to placebo in patients with chronic temporomandibular disorders. Acta Stomatol Croat. 2019;53:195–206. doi: 10.15644/asc53/3/1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fouda AA. No evidence on the effectiveness of oral splints for the management of temporomandibular joint dysfunction pain in both short and long-term follow-up systematic reviews and meta-analysis studies. J Korean Assoc Oral Maxillofac Surg. 2020;46:87–98. doi: 10.5125/jkaoms.2020.46.2.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Alkhutari AS, Alyahya A, Rodrigues Conti PC, Christidis N, Al-Moraissi EA. Is the therapeutic effect of occlusal stabilization appliances more than just placebo effect in the management of painful temporomandibular disorders? A network meta-analysis of randomized clinical trials. J Prosthet Dent. 2021;126:24–32. doi: 10.1016/j.prosdent.2020.08.015. [DOI] [PubMed] [Google Scholar]
- 48.de Freitas RF, Ferreira MÂ, Barbosa GA, Calderon PS. Counselling and self-management therapies for temporomandibular disorders: A systematic review. J Oral Rehabil. 2013;40:864–74. doi: 10.1111/joor.12098. [DOI] [PubMed] [Google Scholar]
- 49.Alencar F, Jr, Becker A. Evaluation of different occlusal splints and counselling in the management of myofascial pain dysfunction. J Oral Rehabil. 2009;36:79–85. doi: 10.1111/j.1365-2842.2008.01913.x. [DOI] [PubMed] [Google Scholar]
- 50.Michelotti A, Iodice G, Vollaro S, Steenks MH, Farella M. Evaluation of the short-term effectiveness of education versus an occlusal splint for the treatment of myofascial pain of the jaw muscles. J Am Dent Assoc. 2012;143:47–53. doi: 10.14219/jada.archive.2012.0018. [DOI] [PubMed] [Google Scholar]
- 51.Qvintus V, Suominen AL, Huttunen J, Raustia A, Ylöstalo P, Sipilä K. Efficacy of stabilisation splint treatment on facial pain-1-year follow-up. J Oral Rehabil. 2015;42:439–46. doi: 10.1111/joor.12275. [DOI] [PubMed] [Google Scholar]
- 52.Kokkola O, Suominen AL, Qvintus V, Myllykangas R, Lahti S, Tolvanen M, et al. Efficacy of stabilisation splint treatment on the oral health-related quality of life – A randomised controlled one-year follow-up trial. J Oral Rehabil. 2018;45:355–62. doi: 10.1111/joor.12622. [DOI] [PubMed] [Google Scholar]
- 53.de Resende CM, de Oliveira Medeiros FG, de Figueiredo Rêgo CR, Bispo AS, Barbosa GA, de Almeida EO. Short-term effectiveness of conservative therapies in pain, quality of life, and sleep in patients with temporomandibular disorders: A randomized clinical trial. Cranio. 2021;39:335–43. doi: 10.1080/08869634.2019.1627068. [DOI] [PubMed] [Google Scholar]
- 54.Pimentel G, Bonotto D, Hilgenberg-Sydney PB. Self-care, education, and awareness of the patient with temporomandibular disorder: A systematic review. [Last accessed on 2021 Jun 27];Braz J Pain. 2018 1:263–9. Available from: https://doi.org/10.5935/2595-0118.20180050 . [Google Scholar]
- 55.Aggarwal VR, Fu Y, Main CJ, Wu J. The effectiveness of self-management interventions in adults with chronic orofacial pain: A systematic review, meta-analysis and meta-regression. Eur J Pain. 2019;23:849–65. doi: 10.1002/ejp.1358. [DOI] [PubMed] [Google Scholar]
- 56.de Barros Pascoal AL, de Freitas RF, da Silva LF, Oliveira AG, Dos Santos Calderon P. Effectiveness of counseling on chronic pain management in patients with temporomandibular disorders. J Oral Facial Pain Headache. 2020;34:77–82. doi: 10.11607/ofph.2163. [DOI] [PubMed] [Google Scholar]
- 57.Espí-López GV, Arnal-Gómez A, Cuerda Del Pino A, Benavent-Corai J, Serra-Añó P, Inglés M. Effect of manual therapy and splint therapy in people with temporomandibular disorders: A preliminary study. J Clin Med. 2020;9:2411. doi: 10.3390/jcm9082411. [DOI] [PMC free article] [PubMed] [Google Scholar]