Abstract
This study presents a conceptual and quantitative approach to assess service linkages among people living with HIV (PLWH). We use network analytic techniques to document linkages among service providers based on client reports of service utilization. Data are provided by a cohort study of 1012 PLWH in New York City interviewed up to 8 times from 2002 to 2015. Participants in each interview reported service needs, services received, and location of services for primary care, behavior health, case management, and housing, food, or other social services. Each reported clinic or agency was linked to entries in a database of medical and social service providers, which included details on organizational characteristics. Based on connections indicated by clients' reported referrals, service co-location within a single agency, or service site part of a larger parent organization, we constructed networks of linkages operationally defining which service areas were linked with others. Case management and primary care were services most commonly linked with other services. The most common pairing was case management and housing services. Individuals with more linkages in their care networks, as measured by average number of connections per provider, were associated with greater odds of adherence to antiretroviral medication and suppressed viral load. Further, higher levels of service linkage were associated with reduced emergency department visits and hospital admission rates. This study offers an innovative approach to analyzing linkages and outcomes from the perspective of service users in terms of their care experiences and provides insights into patient self-management of what are often multiple medical and support service needs. Study limitations include the use of data from a single urban setting and gaps in service reports.
Keywords: HIV/AIDS, linkage, network analysis, medical and social services
Introduction
Achieving the goals of Ending the Epidemic, as recognized by the National HIV/AIDS Strategy and an increasing number of state and jurisdictional plans,1 will require integrated systems of care that address all dimensions of wellness, not only diagnosis and treatment of disease but also social and economic factors that affect the well-being of those most affected by the epidemic.2 Through advances in prevention, diagnosis, and treatment in the past three decades, people living with HIV (PLWH) receiving proper care are beginning to approach the life expectancy of uninfected individuals.3 However, many PLWH have complex needs that cut across different health care sectors, including an array of chronic illness comorbidities (cardiovascular disease, diabetes, and respiratory disease) as well as mental health and/or problem drug use.4–7 Equally important are challenges securing and maintaining basic needs of housing, food, transportation, financial security, and supportive services, which have been shown to have a significant negative impact on engagement in HIV care, clinical outcomes, and quality of life of PLWH.8–11
While the need for integrated services has been widely recognized, the evidence base evaluating effects of service integration for individual patients is limited.6,12–14 Haldane et al.6 provided a review of interventions integrating care for HIV, hypertension, diabetes, and cardiovascular disease, and argued that the extant literature is made up of mostly descriptive articles unable to reveal program effectiveness. Similarly, Chuah et al.12 identified several studies documenting positive outcomes associated with integrating HIV and mental health services, but they identified a lack of evaluation of integration efforts that consider long-term patient health outcomes. However, there is progress being made. The US Health Resources and Services Administration HIV/AIDS Bureau (HRSA HAB) funded a national initiative to establish and evaluate patient-centered medical homes to better integrate multiple medical, behavioral health, and social needs among homeless or unstably housed PLWH; early evaluations have demonstrated benefits of integration of services for health outcomes.15,16
An important contributing factor to the lack of consistent evidence on outcomes of service integration for PLWH relates to conceptualization and measurement issues. One concern is that there are a wide variety of definitions and measures of service integration used by researchers and practitioners.17–19 These differences in data sources and measurement tools then limit cross-study comparisons. Reviews of the integration literature indicate that most studies focus on perceived benefits of integration as reported by managers and service team members, which can provide useful descriptive process measures with the potential for positive outcomes for patient care. However, studies that include actual patient outcome measures are limited.12,17
There is need for measuring service integration as experienced by the patient/client as well as at the system level. This could include possible cross-sectoral linkages (health, housing, employment, transportation, etc.), a dimension that may be missed by focusing on individual patients as the sole object of integration.19,20 Developing data tools other than, or in addition to, provider or patient questionnaires would enable gathering a broader range of data for measuring integration and integration outcomes.21 Indicators derived from administrative or other existing databases may fill an important gap when combined with patient-centered approaches.
We conceptually define integration of HIV care as “a way of organizing care delivery,” by linking services utilized by PLWH across different service sectors through organizational, structural connections that are put in place to benefit patients in terms of clinical outcomes.20 Our operational definition of service integration is based on patterns of formal or informal linkages between and among service organizations utilized by PLWH as they access medical and other providers to address their multiple health, behavioral health, and social service needs. In this regard, we focus on linkages as a type of service integration, adapting Leutz's principles of integration.22 Linkage refers to the relationships between service organizations or service systems (e.g., health care and human services) that serve a population without relying on any special provision for establishing and maintaining links. This is distinct from coordination, which requires structures and individuals with specific responsibility to “coordinate,” and full service integration, which indicates organizational structures and processes for organizing care among a network of providers that involves information sharing, pooling of financial, professional, or other resources, and formal agreements to define relationships.
Service linkages, which may result from nothing more than a shared understanding of patient needs among providers and/or patients themselves, and when and how to initiate a referral to another service agency, are important to investigate in their own right. Evaluating linkages and outcomes from the perspective of service users can provide insight into their care experiences as they attempt to meet their needs by accessing a system of providers.
The purpose of this article is to present an approach to operationally defining service linkages as a type of integration using medical and social service organizational connectedness and network analytic techniques that can be used for both descriptive analysis and predicting health and medical care outcomes. Based on our conceptual definition of integration, we sought to answer three primary research questions:
-
1.
What service areas tend to be linked?
-
2.
Does greater linkage among service area predict better medical care and health outcomes for PLWH?
-
3.
Which, if any, specific service area, when linked with others, predicts better health outcomes for PLWH?
Methods
Data sources
Data for analysis are provided by the Community Health Advisory and Information Network (CHAIN) project, an ongoing (since 1994), community-based cohort study of PLWH in New York City (NYC). Detailed methodology has been described elsewhere;23,24 and a summary can be found online at www.nyhiv.org/data_chain.html Briefly, a two-stage probability sampling strategy was used. First, a stratified sample of medical and non-medical service providers from across NYC was selected. Then, in collaboration with service staff, patients/clients were recruited, either through random selection of PLWH from an agency-provided anonymous list of clients or through on-site sequential enrollment across multiple days. Participants were interviewed from 2002 to 2015 at 12- to 18-month intervals, allowing for repeated measurements for each participant over time. Each interview was conducted in person by trained interviewers, in English or Spanish using a structured protocol. Supplementing interview data is a comprehensive agency data base of HIV medical and social service providers created and regularly updated based on study participants' reports during interviews of provider names and location of where they have gone for services. Agency information is verified by an editing process that reviews provider lists, resources directories, and information provided by providers on websites or annual reports and includes details about service sites, programs and treatments, and linkages within and across organizations within which they may be embedded.
This study uses data from CHAIN study's second cohort recruited in 2002–2004 and followed through 8 waves of interviews; 693 participants responded to an average number of 5.04 interviews during the study. To improve the sample size and reduce loss to follow-up, a refresher cohort was added to the study in 2009–2010; 319 participants in the refresher cohort responded to an average of 2.95 interviews (out of a maximum of 4) through 2015 (Table 1). Sample attrition for reasons other than death (n = 247, 24%) or migration out of NYC (n = 85, 8%) has remained low; the additional reasons for loss to follow-up by final interview included physical or mental incapacitation (n = 17, 2%) or institutionalization (n = 12, 1%). At each interview period, 80–90% of persons completing a prior interview were located and reinterviewed.
Table 1.
Sample Characteristics at Baseline Interview
| n (%) | |
|---|---|
| Total | 1012 (100) |
| Age, years | |
| <36 | 109 (10.8) |
| 36–49 | 551 (54.5) |
| 50+ | 352 (34.8) |
| Mean (SD), years | 46.1 (8.9) |
| Gender | |
| Male | 604 (59.7) |
| Female | 391 (38.6) |
| Non-cisgendera | 17 (1.6) |
| Race/Ethnicity | |
| White non-Hispanic | 86 (8.5) |
| Black non-Hispanic | 553 (54.6) |
| Hispanic/Latino | 351 (34.7) |
| Othera | 22 (2.2) |
| Income | |
| Annual income <$7500 | 256 (25.3) |
| Income ≥$7500 | 756 (74.7) |
| Education | |
| Less than high school | 411 (40.6) |
| High school or GED | 438 (49.6) |
| Some college or more | 162 (16.0) |
| Housing needs | |
| No needs | 77 (7.6) |
| Needs rental assistance | 608 (60.4) |
| Needs permanent housing | 171 (17.0) |
| Needs permanent, supportive housing | 151 (15.0) |
| Substance use | |
| No problem substance useb | 294 (29.1) |
| Past problem substance use | 484 (47.8) |
| Current problem substance use | 234 (23.1) |
| Mental Health functioning | |
| Good mental health score | 535 (52.9) |
| Low mental health scorec | 477 (47.1) |
| Physical Health functioning | |
| Good physical health score | 305 (30.1) |
| Low physical health scored | 707 (69.9) |
| Viral load | |
| Undetectable (<400 copies/mL)e | 628 (62.1) |
| Unsuppressed | 350 (34.6) |
| Missing | 34 (3.5) |
| HIV diagnosis year | |
| Before 1997 | 641 (63.3) |
| 1997–2005 | 314 (31.0) |
| After 2005 | 44 (4.3) |
| Missing | 13 (1.3) |
Analyses exclude assessments of effects of “Non-cisgender” identity and “Other” racial identities due to low sample sizes.
Problem substance use indicated by use of heroin, cocaine, crack, or methamphetamine, any IDU, or problem drinking (one or more yes to CAGE questions or drink weekly or more often and have five or more drinks on those days when drinks). Current use refers to within 6 months of interview.
MOS SF-12 Mental Health Summary Score (MCS) below 42.0 indicating clinically significant symptomology.
MOS SF-12 Physical Health Summary Score (PCS) below 50.0, mean score for general population.
Indicated by self-report or review of medical record.
IDU, injection drug use; SD, standard deviation; SF-12, 12-item Short Form Health Survey.
The CHAIN cohort study is regularly reviewed and approved by Institutional Review Boards (IRB) of Columbia University Medical Center and the NYC Department of Health and Mental Hygiene.
Measures
Measuring service linkage
At each interview, participants were asked about objective and subjective medical and social service need and service utilization during the past 6 months, and information was collected about all organizations/clinics/agencies where they received any services. Over time, we have constructed a database of over 6500 service sites, detailing the names, addresses, and formal organizational linkages (e.g., described on websites or in agency reports) that describe each service provider. All agencies named were coded with an identifier that was attached to individual respondents' service utilization data.
Table 2 provides a summary of the nine types of services we explored in this study: primary HIV medical care; dental or other oral health services; visits to medical practitioners such as optometrists; mental health treatment; substance use treatment; assistance with housing needs; food or meal services; assistance with financial needs; and case management. These nine services were selected for analysis since these were the services utilized by at least 10% of participants at some time between 2002 and 2015.
Table 2.
Services and Provider Types Examined for Service Integration Analysis
| Service categorya | Description of service providers and service utilizationb |
|---|---|
| HIV primary care | Doctor, nurse, or other medical provider who respondent considers is in charge of his/her overall HIV health care. |
| Dental care/Oral health services | Clinic or office where received services by a dentist, oral surgeon, or other dental care provider for any of the following: examination, cleaning teeth, X-rays, filings, extractions, root canal, crown/bridge or denture work, gum care, or other dental-related need. |
| Medical practitioner | Service site where received assistance from a medical practitioner (separate from other medical care) such as optometrist, foot doctor, chiropractor, and nutritionist. |
| Substance use treatment or services | Agency or program where received professional drug or alcohol treatment, including detox, inpatient or outpatient treatment, residential treatment, methadone maintenance, EAP, individual treatment counselor, psychologist, or psychiatrist focused on treating substance use disorder. |
| Housing assistance or services | Agency or program where received assistance to secure or maintain housing (e.g., provision of housing, rental assistance, housing placement assistance), address safety, housing quality or physical access issues, or other housing-related needs. |
| Financial assistance | Agency or program where received assistance to address financial needs, including receipt of emergency funds and assistance with obtaining or maintaining benefits/entitlements such as SSI, SSDI, and TANF. |
| Mental health treatment or services | Professional mental health provider (psychiatrist, psychologist, CSW, and therapist) visited for treatment or services. |
| Food or meal services | Agency or program providing assistance with obtaining food (pantry bag and voucher) or meals (congregate or home-delivered meals). |
| Case managementc | Assistance by a case manager, case worker, or other paid employee to help arrange services, including revising or developing a plan for addressing needs, helping get specific social services, periodically checking on needs, filling out forms for benefits, counseling about personal life, substance use, risk behaviors, and/or treatment adherence, or addressing other service-related need. |
Services accessed by at least 10% of study participants interviewed 2002–2015.
Services, treatment, or other assistance receiving currently or received within 6 months of interview.
Considered up to four agencies or programs providing case management services.
CSW, clinical social worker; EAP, employee assistance program; SSI, social security insurance; SSDI, social security disability insurance; TANF, temporary assistance for needy families.
For each service reported during each interview, we constructed networks of services that represented connections between service providers using information about each individual agency and any parent organization of which it is a component as documented in the agency database. For example, if a participant reported Dr. Smith as his/her primary medical provider for HIV care at Hope Hospital and also went to the Social Work Department of Hope Hospital for help with housing needs and saw a case manager there who provided assistance, we would be able to identify linkages between three services: HIV primary care, case management, and housing.
We additionally defined linkage between agencies based on self-report referral patterns. For HIV primary care, mental health, and drug treatment, respondents were asked if they were referred by any other service provider or agency when they went to the specific provider for the first time,. If any provider or agency had referred the participant, this was classified as a service linkage. Note that linkages were only ascertainable through referral patterns, service site locations, or affiliation with parental organizations, as no data were available regarding contractual relationships or other formal organizational linkages such as memoranda of understanding.
If participants identified multiple service providers within a service area, such as using multiple case managers, all agency organizational information for each of these providers was used to create linkages between other service areas. That is, for our analysis, we are tracing linkages among types of service providers, not linkages among individual service agencies with one another. Relatedly, we did not distinguish between within-agency and between-agency linkages; although would be preferred for establishing the importance of types of linkages, these data were not readily available.
Construction of this multi-level dataset allowed for both cross-sectional and longitudinal representations of how different service areas were formally connected by organizational structure and formally or informally connected by referral patterns. Two representations of service networks were created using repeated cross-sectional and over time data. All service use variables are standardized based on reports of services utilized within the past 6 months. We first documented the current array of services utilized within 6 months of current interview. For longitudinal analyses, we documented the current array of services utilized, merged with all previous interviews.
Overall measures of linkages were calculated using the number of linkages between service areas, the average number of linkages per service area, and the total number of service areas utilized. In network analyses, these are commonly referred to as the number of edges, the average degree, and the number of nodes, respectively. To measure the extent of linkages for each specific service area, we calculated the number of linkages between the service area and the other service area utilized by respondents (the degree of each node). We constructed these measures using the cumulative, merged networks of services to avoid issues of gaps between data collection time points.
For measuring the percentage of service linkages observed, we utilized the current representation of service networks. The number of possible linkages between n service areas accessed is n(n − 1)/2, which corresponds to a complete, Kn-graph. Therefore, by dividing the number of observed linkages by the number of possible linkages based only on the service areas accessed by each participant, we measured the percentage of possible service linkages actualized. In network terminology, this is referred to as the graph density. Because the networks observed in each interviewed varied in size, we calculated the percentage of possible linkages only for current representations of service networks.
In summary, we constructed four network-level measures of service linkage based on how service providers are organizationally connected (edges, average degree, number of nodes, and density). Supplementing these global measures, we also assessed the level of linkage for each service based on the number of other services to which it linked. These measures allowed us to assess 13 different ways to measure service connections at a system- and service-specific level.
Outcome measures and covariates
Positive health outcomes included adherent antiretroviral therapy (ART) use and suppressed viral load. Adherent ART use is indicated by taking any recommended ART regimen prescribed by physician and adherence to medication regimen is indicated by reports of taking medications “exactly as prescribed, almost never missing a dose” and not missing any medication in the 2 days preceding the interview. Not adherent includes those who are not taking any antiretroviral medication and those taking medications listed under “not recommended” or “should be changed” regimens in the Department of Health and Human Services' guidelines in effect at the time of the interview. Viral load suppression is based on respondent report (or when available, laboratory report) of most recent HIV viral load as a numerical value below reliably detectable cut point at the time (<400 copies 2002–2008; <200 2009 or after), or when medical provider reported viral load test results as “undetectable,” or, in a few cases, simply as “good.” Viral load test results above the cut point, or provider reported as either “detectable” or “bad,” were classified as unsuppressed viral load. Brief validation studies have shown good reliability for medications taken and viral load test results.25,26 Positive outcomes examined also include health quality of life or good physical health functioning indicated by Physical Component Summary >50.0 on the Medical Outcome Study, The 12-item Short Form Health Survey (SF-12).27
Negative health outcomes included missing two or more scheduled medical appointments, an indicator of lack of retention in HIV care;28 any emergency room (ER) visit; or any hospital inpatient stay during the past 6 months. Covariates included are sociodemographics, including race/ethnicity, education, gender, and men who have sex with men experience, and indicators of service need, including food insecurity, low mental health functioning (Mental Component Summary <42.0 on the SF-12 inventory27), housing need, extreme poverty (income <$7500 per annum), and problem drug use. Problem drug use was indicated as use of heroin, crack/cocaine, and methamphetamine, any injection drug use, or problem drinking. Food insecurity was assessed using questions adapted from the United States Department of Agriculture 6-item.29 Housing need was operationalized at four levels: none, needs rental assistance to maintain housing, needs to obtain permanent housing (i.e., currently homeless or in temporary housing), or needs permanent supportive housing (housing plus supportive services).8
Data analysis
We used mixed-effects logistic models to predict each of the six binary outcomes of interest, using robust standard errors to account for repeated measurements of the same participants over time. We calculated unadjusted odds ratios (OR) and adjusted odds ratios for each outcome, using a single explanatory variable (one measure of integration such as average degree) as a lone predictor and as a predictor alongside covariates, respectively, in the models. For measuring the effect of additional service linkages, the number of services utilized is also included in all relevant models to adjust for confounding due to greater likelihood of connections with greater numbers of services. We conducted all mixed-effects analyses in Stata/SE 15 (StataCorp 2017, College Station, TX) and visualized patterns of agency linkages using the igraph package (Csardi and Nepusz, 2006) in R (R Foundation for Statistical Computing 2013, Vienna, Austria). To account for the lack of independence of observations due to repeated measures of individuals in the study, robust standard errors with random intercepts were included. Because we were interested in individual specific estimates, we employed generalized linear models, as opposed to general estimating equations that can provide population-level estimates. No data imputation was done for missing observations and variables, although cohort retention was very high (80–90% follow-up for each wave) and item missing was negligible. All models include only PLWH who reported the relevant service information; for example, the effect of additional linkages to primary care services only includes PLWH who accessed and reported primary care service.
Results
Linkages among services
Across 4430 observations provided by 1012 individuals completing an average of 3–5 interviews, we documented 4835 linkages between service-providing agencies (data summarized in Table 3). Within these 4835 linkages, some service areas were more likely to be linked with others; case management and HIV primary care services are the most common services to be linked with other services. The most common pairing of services organizationally or through referral was between case management and housing services.
Table 3.
Most Common Services to Be Linked and Most Common Linkages Between Services
| Service category | Proportion of all service linkages that occur for each service category, % |
|---|---|
| Total number of service linkages n = 4835a | |
| Case management | 24.2 |
| HIV primary care | 19.6 |
| Medical practitioners | 12.5 |
| Housing services | 11.4 |
| Mental health treatment | 10.2 |
| Food or meal services | 9.9 |
| Dental services | 5.4 |
| Financial assistance | 3.7 |
| Substance use treatment | 3.2 |
| Most common service category linkages (pairs) | Proportion of all linkages, % |
|---|---|
| Case management and housing |
13.7 |
| HIV primary care and case management |
12.1 |
| HIV primary care and medical practitioners |
10.1 |
| HIV primary care and mental health treatment |
7.0 |
| Case management and food/Meal services | 6.7 |
A total of 4835 linkages between service-providing agencies were documented across 4430 observations of 1012 individuals (reported during an average 4.8 interviews).
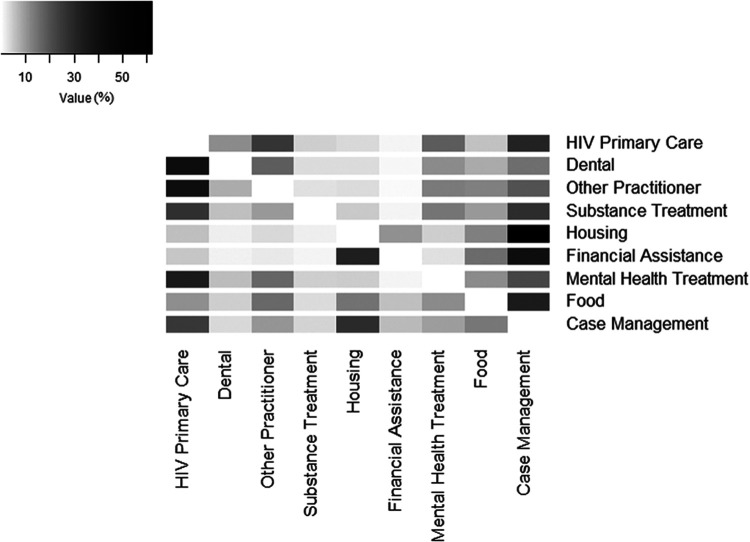
Figure 1 provides a graphical depiction of the service areas most commonly linked with each service area. For example, examining linkages to housing services, ∼60% of all of the agency linkages with housing services were linkages with case management.
FIG. 1.
The most common service linkages for each service type (by row). The most common service linkages are indicated by darker colors; absent or less frequent connections are whiter, lighter colors. For example, examining Housing, the most common service linkage is with Case Management, and the least common service linkages are with Dental Services and Substance Treatment.
Linkage of services among PLWH appears to be low despite high rates of service utilization. The average number of services utilized at any point before or currently at the time of interview by participants was 4.30 (range, 1–9). The average number of linkages between service areas for participants was 2.08 (range, 0–21). Further, we calculated the average number of linkages per service to be 0.25 (range, 0–3), that is, the average participant had only one linkage for every four service areas they utilized. The service networks were also not densely integrated, with an average density of 7% (range, 0–23%).
Overall measures of linkage and health outcomes
Positive outcomes
Table 4 presents associations between positive outcomes and measures of overall service linkage based on networks of linked services. Unadjusted for covariates, greater linkage of service areas was associated with more positive health outcomes. For each additional linkage documented between services respondents accessed, respondents had greater odds of adherent ART use [OR: 1.10, 95% confidence interval (CI): 1.04–1.15] and suppressed viral load (OR: 1.15, 95% CI: 1.07–1.22). Respondents with 25% of their services currently connected with each other also had greater odds of suppressed viral load (OR: 2.24, 95% CI: 1.15–4.35) compared to those with no linkages among services. Respondents reporting a higher average number of linkages among their services were also more likely to have adherent ART use (OR: 1.43, 95% CI: 1.22–1.67) and suppressed viral load (OR: 1.56, 95% CI: 1.28–1.91). Each additional service also predicted greater odds of suppressed viral load (OR: 1.27, 95% CI: 1.17–1.38) and adherence to ART (OR: 1.24, 95% CI: 1.17–1.32), regardless of linkages among them.
Table 4.
Odds Ratios (95% Confidence Interval) Predicting Outcomes for Measures of Linkage for Service Networks Overall
| Adherent ART use |
Suppressed viral load |
Good physical health functioning |
||||
|---|---|---|---|---|---|---|
| OR | AORb | OR | AORa | OR | AORa | |
| Overall measures of service linkage | ||||||
| One additional linkage between any two servicesc | 1.10*** (1.04–1.15) | 1.05° (0.99–1.12) | 1.15*** (1.07–1.22) | 1.07** (1.02–1.13) | 0.98 (0.92–1.03) | 1.01 (0.95–1.07) |
| Comparing 0–25% of all linkages between services | 1.45 (0.80–2.63) | 1.28 (0.57–2.86) | 2.24* (1.15–4.35) | 2.05° (0.93–4.49) | 1.55 (0.79–3.04) | 1.52 (0.66–3.48) |
| Increase, by 1, the average number of linkages for each service | 1.43*** (1.22–1.67) | 1.16° (0.98–1.39) | 1.56*** (1.28–1.91) | 1.18° (0.99–1.41) | 0.81* (0.68–0.97) | 0.90 (0.75–1.07) |
| Each additional service added to the array of services utilizedd | 1.24*** (1.17–1.32) | 1.10* (1.02–1.17) | 1.27*** (1.17–1.38) | 1.11* (1.02–1.20) | 0.91** (0.86–0.98) | 0.94° (0.88–1.01) |
| Missed medical appointments |
ER visit |
Hospital admission |
||||
|---|---|---|---|---|---|---|
| OR | AORa | OR | AORa | OR | AORa | |
| Overall measures of service linkage | ||||||
| One additional linkage between any two servicesc |
0.98 (0.94–1.03) |
1.01 (0.96–1.06) |
0.95* (0.91–0.99) |
0.95* (0.91–0.99) |
1.02 (0.96–1.06) |
1.01 (0.96–1.06) |
| Comparing 0–25% of all linkage between services |
0.74 (0.36–1.55) |
0.99 (0.47–2.10) |
0.45** (0.27–0.76) |
0.59° (0.33–1.05) |
0.43** (0.23–0.79) |
0.48* (0.23–0.97) |
| Increase, by 1, the average number of linkages for each service |
0.87° (0.75–1.01) |
0.96 (0.83–1.11) |
0.91 (0.80–1.03) |
0.92 (0.81–1.04) |
1.04 (0.90–1.21) |
1.03 (0.89–1.21) |
| Each additional service added to the array of services utilizedd | 0.96 (0.90–1.02) | 1.00 (0.94–1.06) | 1.00 (0.95–1.05) | 1.00 (0.95–1.05) | 1.02 (0.96–1.08) | 0.99 (0.94–1.06) |
Adjusted for race/ethnicity, gender, sexual orientation, poverty, problem drug use, mental health functioning, food insecurity, housing need, and ART.
Adjusted for race/ethnicity, gender, sexual orientation, poverty, problem drug use, mental health functioning, food insecurity, and housing need.
For both OR and AOR, this is also adjusted for the number of services utilized at the time of interview.
Addition of an individual service to a patient's service network regardless of linkages among them.
p < 0.001; **p < 0.01; *p < 0.05; °p < 0.10.
AOR, adjusted odds ratio; ART, antiretroviral therapy; ER, emergency room; OR, odds ratio.
Conversely, greater integration of services was associated with poorer physical health functioning. We interpreted this finding with caution, as ∼70% of individuals reported poor physical health at baseline interview, and the effects of overall linkage measures are not significant when adjusting for other covariates.
Negative outcomes
Table 4 also presents associations between negative outcomes and measures of overall service linkage. Compared to predicting positive outcomes, many fewer overall linkage measures predicted negative outcomes. Each additional service linkage predicted a reduction in the odds of visiting the ER (OR: 0.95, 95% CI: 0.91–0.99). Having a current network of services with 25% of all possible linkages, compared to no linkages, predicted reduced odds of visiting the ER (OR: 0.45, 95% CI: 0.27– 0.76) and being admitted to the hospital (OR: 0.43, 95% CI: 0.23–0.79). These findings remained significant or marginally significant after adjusting for covariates. We found no significant association between average degree of connectedness for services and the addition of services to an individual's service network for predicting negative health outcomes.
Health outcomes and service-specific measures of linkage
Positive outcomes
Table 5 presents associations between connectedness of each service and positive outcomes. Linkage of particular services, mainly HIV primary care, dental services, visits to medical practitioners, case management, and housing services, predicts greater odds of positive outcomes. We found greater odds of adherent ART use for each additional linkage to HIV primary care (OR: 1.28, 95% CI: 1.15–1.44), dental (OR: 1.16, 95% CI: 1.00–1.34), medical practitioners (OR: 1.16, 95% CI: 1.02–1.32), substance use treatment (OR: 1.32, 95% CI: 1.11–1.57), case management (OR: 1.23, 95% CI: 1.11–1.37), and housing (OR: 1.32, 95% CI: 1.11–1.57), which are not statistically significant when adjusting for covariates. We also found greater odds of viral suppression for each additional service linkage to HIV primary care (OR: 1.34, 95% CI: 1.17–1.55), dental (OR: 1.28, 95% CI: 1.06–1.54), medical practitioners (OR: 1.32, 95% CI: 1.09–1.61), case management (OR: 1.36, 95% CI: 1.18–1.56), and housing (OR: 1.26, 95% CI: 1.02–1.55). After adjusting for covariates, these effects are minimized, with only marginally significant positive effects noted for integration of HIV primary care, medical practitioners, and case management.
Table 5.
Odds Ratios (95% Confidence Interval) Predicting Outcomes for Measures of Service Linkage for Specific Services Accessed
| Adherent ART use |
Suppressed viral load |
Good physical health functioning |
||||
|---|---|---|---|---|---|---|
| OR | AORc | OR | AORa | OR | AORa | |
| Addition of one service linkage withb | ||||||
| HIV primary care | 1.28*** (1.15–1.44) | 1.10 (0.97–1.25) | 1.34*** (1.17–1.55) | 1.11° (0.98–1.26) | 0.87* (0.77–0.99) | 0.92 (0.81–1.05) |
| Dental services | 1.16* (1.00–1.34) | 1.06 (0.89–1.27) | 1.28** (1.06–1.54) | 1.10 (0.92–1.32) | 1.01 (0.83–1.23) | 1.10 (0.90–1.33) |
| Medical practitioners | 1.16* (1.02–1.32) | 1.06 (0.91–1.24) | 1.32** (1.09–1.61) | 1.19° (0.99–1.42) | 0.96 (0.81–1.15) | 1.04 (0.87–1.24) |
| Substance use treatment | 1.32* (1.03–1.68) | 1.26 (0.93–1.71) | 1.14 (0.91–1.42) | 1.04 (0.83–1.29) | 1.04 (0.81–1.33) | 1.16 (0.90–1.50) |
| Mental health treatment | 0.98 (0.84–1.14) | 0.96 (0.81–1.14) | 1.00 (0.82–1.22) | 0.97 (0.81–1.17) | 0.89 (0.72–1.10) | 0.98 (0.79–1.21) |
| Case management | 1.23*** (1.11–1.37) | 1.06 (0.94–1.20) | 1.36*** (1.18–1.56) | 1.12° (0.99–1.28) | 0.85** (0.76–0.96) | 0.90° (0.80–1.02) |
| Housing services | 1.32** (1.11–1.57) | 1.17 (0.96–1.41) | 1.26* (1.02–1.55) | 1.07 (0.87–1.31) | 1.04 (0.86–1.26) | 1.05 (0.86–1.29) |
| Food services | 1.04 (0.90–1.20) | 0.99 (0.85–1.18) | 1.01 (0.83–1.23) | 1.00 (0.82–1.21) | 0.90 (0.75–1.10) | 0.97 (0.80–1.17) |
| Financial assistance | 1.03 (0.80–1.31) | 0.95 (0.71–1.28) | 1.18 (0.85–1.65) | 1.14 (0.82–1.57) | 1.03 (0.72–1.46) | 1.14 (0.81, 1.61) |
| Missed medical appointments |
ER visit |
Hospital admission |
||||
|---|---|---|---|---|---|---|
| OR | AORa | OR | AORa | OR | AORa | |
| Addition of one service linkage withb | ||||||
| Primary care |
0.91° (0.81–1.01) |
0.97 (0.87–1.08) |
0.96 (0.87–1.04) |
0.96 (0.88–1.05) |
1.06 (0.95–1.18) |
1.05 (0.94–1.16) |
| Dental |
0.85* (0.73–0.99) |
0.88° (0.76–1.02) |
0.88° (0.77–1.01) |
0.88° (0.76–1.00) |
0.99 (0.84–1.16) |
0.98 (0.83–1.15) |
| Other practitioners |
0.99 (0.87–1.14) |
1.05 (0.92–1.20) |
0.95 (0.83–1.08) |
0.93 (0.81–1.06) |
1.11 (0.97–1.27) |
1.10 (0.96–1.25) |
| Substance use treatment |
0.89 (0.72–1.11) |
0.99 (0.80–1.22) |
0.86 (0.69–1.05) |
0.88 (0.71–1.09) |
1.03 (0.86–1.23) |
1.09 (0.91–1.30) |
| Mental health treatment |
1.04 (0.88–1.22) |
1.05 (0.90–1.23) |
1.07 (0.94–1.22) |
1.02 (0.90–1.16) |
1.17* (1.01–1.35) |
1.12 (0.96–1.30) |
| Case management |
0.88* (0.79–0.97) |
0.94 (0.85–1.04) |
0.92° (0.84–1.00) |
0.93° (0.85–1.01) |
0.96 (0.86–1.06) |
0.97 (0.88–1.08) |
| Housing |
0.87 (0.72–1.05) |
0.92 (0.77–1.10) |
0.94 (0.80–1.10) |
0.97 (0.84–1.13) |
0.97 (0.83–1.15) |
1.03 (0.89–1.20) |
| Food assistance |
1.03 (0.87–1.22) |
1.01 (0.87–1.19) |
0.97 (0.85–1.10) |
0.95 (0.84–1.08) |
1.04 (0.90–1.20) |
1.02 (0.89–1.18) |
| Financial assistance | 0.97 (0.72–1.31) | 0.92 (0.70–1.20) | 0.96 (0.74–1.26) | 0.97 (0.74–1.26) | 0.85 (0.65–1.12) | 0.88 (0.68, 1.15) |
Adjusted for race/ethnicity, gender, sexual orientation, poverty, problem drug use, mental health functioning, food insecurity, housing need, and ART.
Addition of an additional service linkage of any type to each of the services listed.
Adjusted for race/ethnicity, gender, sexual orientation, poverty, problem drug use, mental health functioning, food insecurity, and housing need.
p < 0.001; **p < 0.01; *p < 0.05; °p < 0.10.
AOR, adjusted odds ratio; ART, antiretroviral therapy; ER, emergency room; OR, odds ratio.
Similar to findings between physical health and overall measures of service linkage, respondents with more connections to HIV primary care and case management were also more likely to report having worse physical health; we interpreted this result with caution as noted above.
Because the number of connections each service has depends on the number of services utilized by the participant, we also adjusted these models to account for networks with more services included. When adjusting for the total number of services utilized by respondents, connectedness of primary care, dental, medical practitioners, and case management significantly predicted better health outcomes (data not shown); higher levels of linkage with housing did not significantly predict outcomes. This indicates that linking each service, other than housing, predicts better outcomes beyond simply having more isolated services in the network.
Negative outcomes
Table 5 (lower panel) also presents associations between connectedness of each specific service and negative medical care outcomes. Again, the relationship between service linkage indicators and reduction of negative outcomes is weaker than the relationship between service linkages and positive health outcomes. We found that additional linkages to dental (OR: 0.85, 95% CI: 0.73–0.99) and case management (OR: 0.88, 95% CI: 0.79–0.97) predicted reduced odds of missing two or more medical appointments. Similarly, each additional linkage to dental and case management marginally predicted reduced odds of visiting the ER.
Discussion
This study documents wide variability in linkage of services among PLWH and provides strong evidence that linked health and social services predict better health and medical care outcomes for HIV-positive persons. Overall, connections between services among study participants were relatively low despite a service-rich environment and high rates of service utilization. Most linkages between services appear to link through case management, primary care, and housing, indicating the importance of these services within the overall care management of PLWH. Each additional linkage added to a respondent's network of medical and social services appears to be important for achieving suppressed viral load, with greater density of service linkages associated with higher odds of positive health outcomes. Beyond overall linkage among services used, we identified specific service areas that appear to confer greater benefit with greater linkage with other services. Additional service linkages with HIV primary care, dental, medical practitioners, case management, and housing services are associated with higher odds of adherent ART use and viral suppression. These findings vary in significance when taking into account covariates such as age, race, education, mental health, and substance use challenges. This may indicate that service integration effects are not homogenous across different demographic and risk groups and may be a mechanism through which outcomes are influenced.
Our findings are consistent with the growing awareness of the benefits of service integration or care coordination to address the multiple, co-occurring medical and supportive service needs of PLWH.16 We found that greater linkage of medical services with social services and case management is associated with greater odds of positive outcomes, especially adherent ART use and viral suppression, controlling for a wide range of client characteristics and service needs associated with worse retention in care, adherence, and viral load outcomes. Our analytical approach has documented the positive benefits of linkages or organizational ties between services, as experienced by individual clients, regardless of whether or not there is any deliberate information sharing or service coordination at the organizational level. Further research would be required to assess the extent to which these network analyses correspond to actional coordination of care.
This conceptual approach to using network connectivity for measuring service linkage adds to a growing body of literature focusing on network analysis and public health. This is the first study to employ network analysis for predicting longitudinal health outcomes for PLWH. Studies examining networks of services for HIV-positive populations most commonly assess agency linkages descriptively.30–34 Predicting outcomes associated with service provider connectivity is significantly less common, although there have been outcome studies focused on other health condition or populations at risk.35,36 A study at the aggregate level found that counties in North Carolina with greater density of linkages among providers with STD or HIV prevention initiatives had lower syphilis rates, and authors inferred that agencies working together would also improve HIV prevention.37 More recently, an intervention for improving connections among service providers for PLWH in Ethiopia demonstrated that increased integration was associated with higher rates of adherent ART use.38 These findings corroborate our results, indicating the potential benefits of increased overall service linkage for promoting positive outcomes among PLWH.
There are a number of limitations to this study based on data availability and analytical approach. The causal effect of integration of services on outcomes is not directly assessed or ascertainable, as the study utilizes cohort data and is not experimental in nature. A further limitation is that reports of services used only during the 6 months before interviews may reduce recall bias, but results in gaps in service utilization over time; thus, the data may not accurately represent the full spectrum of services and service linkages experienced by participants. Although we include covariates to control for major indicators of service need, the lack of a particular service in a network may have occurred for a number of reasons, including utilization of the service outside of 6 months before interview, which is our observation period. Loss to follow-up in our study, although minimal, may bias the results, as some participants were no longer able to be contacted, or missed interview waves. The use of self-report data for both service utilization and referrals to services used may be subject to presentation and recall bias. However, it is unlikely that inaccurate reporting of referrals may have influenced the strength of associations found. Referral connections between organizations were assessed only for three of the nine services (primary care, mental health services, and substance use treatment), and the majority of connections were documented using the linked agency-level database rather than self-report referral information. Further, data collection through comprehensive in-person interviews by trained interviewers following protocols to use memory aids and probe for incomplete or inconsistent reports, and checks with agency-generated information, strengthens our confidence in reliability of respondent reports.
In addition, there are benefits to using patient self-report data. Our analysis of service linkages provides a useful perspective based on information from those who utilize the services themselves. Evaluating linkages and outcomes from the perspective of service users in terms of their care experiences as they journey through a system of providers functionally available to them (known, acceptable, and accessible by them) can provide insight into processes of both organizational and patient self-management of multiple needs. Benefits of organizational structures based on contracts or other mechanisms supporting service integration are beneficial to the extent that arrangements actively engage patients.
Further, adjusting for race, gender, and HIV risk factors, which in some cases resulted in null findings for the effect of integration measures on outcomes, may obscure the true effect of linking services together. Prior research indicates that there are differences in retention and continuity of care across gender identities, race, and injection drug use, including in NYC, where this study was based.39–41 Therefore, these factors may be part of the causal pathway between integrated care and HIV health outcomes; adjustment for these variables may not be necessary, or indeed, inappropriate, as they could dilute the true effect of linkage on health outcomes. Similarly, integration may be related to specific integration initiatives funded by the Affordable Care Act or Ryan White Care Act, which would be a factor in the causal path between integration and outcomes;42 as such, it should not be considered a potential confounder.
Measuring the impact of integrated care from the perspective of service users provides important information not accessible by measuring integration only from systems' or organizational perspectives. In addition, our network analytic approach to analyzing service linkages based on patient service encounters offers an approach to understanding “systems” of care without an additional effort to collect information from organizational managers and program staff. Analyzing linkages among service providers by tracking client encounters with service providers as documented in administrative data bases maintained by funders (e.g., state Medicaid data, Ryan White contract data) and/or government agencies, especially analyses using integrated data sets (e.g., health, mental health, social services), holds substantial potential for understanding systems of care and individual and population outcomes associated with different service linkage patterns.43 Better understanding of outcomes associated with different patterns of service integration can inform interventions targeting identified services for linkage and testing of benefits for individual patient health and quality of life, as well as health care cost savings.
Acknowledgments
We would like to thank the Technical Review Team (TRT), which provides oversight for the CHAIN Project. TRT members include Dr. Peter Messeri at the Mailman School of Public Health, Columbia University, a former Principal Investigator of the CHAIN study, and representatives from New York City Department of Health and Mental Hygiene (NYC DOHMH); Westchester County Department of Health, New York State AIDS Institute; and the HIV Health and Human Services Planning Council of New York. We are especially grateful to the staff of the agencies in New York City and the Tri-County Region who help introduce the project to their clients and patients. Finally and most importantly, we thank the many persons living with HIV who have shared their time and experience with us as CHAIN Project participants since 1994.
Data Availability
Data are not available for sharing due to its identifiable individual and service provider information. Any questions or concerns can be directed to the corresponding author.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
CHAIN research is supported through a contract with the NYC DOHMH as part of its Ryan White HATEA grant, H89HA00015, from the Department of Health and Human Services, HRSA HAB. Contents of this report are solely the responsibility of the report authors and do not necessarily represent the official views of the US Health Resources and Services Administration, the City of New York, or Westchester Department of Health.
References
- 1. NASTAD. Ending the HIV epidemic: Jurisdictional plans. Published 2019. Available at: https://www.nastad.org/maps/ending-hiv-epidemic-jurisdictional-plans (Last accessed August 8, 2019).
- 2. Valdiserri RO. The evolution of HIV prevention programming: Moving from intervention to system. AIDS Educ Prev 2018;30:187–198. [DOI] [PubMed] [Google Scholar]
- 3. Nakagawa F, May M, Phillips A. Life expectancy living with HIV: Recent estimates and future implications. Curr Opin Infect Dis 2013;26:17–25. [DOI] [PubMed] [Google Scholar]
- 4. Bing EG, Burnam MA, Longshore D, et al. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Arch Gen Psychiatry 2001;58:721–728. [DOI] [PubMed] [Google Scholar]
- 5. Guaraldi G, Orlando G, Zona S, et al. Premature age-related comorbidities among HIV-infected persons compared with the general population. Clin Infect Dis 2011;53:1120–1126. [DOI] [PubMed] [Google Scholar]
- 6. Haldane V, Legido-Quigley H, Chuah FLH, et al. Integrating cardiovascular diseases, hypertension, and diabetes with HIV services: A systematic review. AIDS Care 2018;30:103–115. [DOI] [PubMed] [Google Scholar]
- 7. Wainberg ML, McKinnon K, Cournos F. Epidemiology of psychopathology in HIV. In: Joska JA, Stein DJ, Grant I, eds. HIV and Psychiatry, 1st ed. Sussex, United Kingdom: John Wiley and Sons Limited; 2014:1–33. [Google Scholar]
- 8. Aidala AA, Yomogida M, Kim J.. Housing Need and Housing Assistance in New York City and Tri-County Region. New York, NY: Mailman School of Public Health, Columbia University, 2016. [Google Scholar]
- 9. Behavioral and Clinical Characteristics of Persons Diagnosed with HIV Infection—Medical Monitoring Project, Atlanta, GA: Centers for Disease Control, 2018. [Google Scholar]
- 10. Ford MA, Spicer CM, eds. Centers for Disease Control, Monitoring HIV Care in the United States: Indicators and Data Systems, Institute of Medicine of the National Academics, 2012. [PubMed] [Google Scholar]
- 11. Weiser SD, Young SL, Cohen CR, et al. Conceptual framework for understanding the bidirectional links between food insecurity and HIV/AIDS. Am J Clin Nutr 2011;94:1729S–1739S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chuah FLH, Haldane VE, Cervero-Liceras F, et al. Interventions and approaches to integrating HIV and mental health services: A systematic review. Health Policy Plan 2017;32(Suppl 4):iv27–iv47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Higa DH, Marks G, Crepaz N, Liau A, Lyles CM. Interventions to improve retention in HIV primary care: A systematic review of U.S. studies. Curr HIV/AIDS Rep 2012;9:313–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Soto TA, Bell J, Pillen MB. Literature on integrated HIV care: A review. AIDS Care 2004;16(Suppl 1):S43–S55. [DOI] [PubMed] [Google Scholar]
- 15. Phillips HJ, Tinsley MJ, Rajabiun S. Building a medical home for HIV-positive, multiply diagnosed homeless populations. Am J Public Health 2018;108(Suppl 7):S518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sarango M, Hohl C, Gonzalez N, Palmeros A, Powell ML, Hirschi M. Strategies to build a patient-centered medical home for multiply diagnosed people living with HIV who are experiencing homelessness or unstable housing. Am J Public Health 2018;108:S519–S521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Armitage GD, Suter E, Oelke ND, Adair CE. Health systems integration: State of the evidence. Int J Integr Care 2009;9:e82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Shigayeva A, Atun R, McKee M, Coker R. Health systems, communicable diseases and integration. Health Policy Plan 2010;25(Suppl 1):i4–i20. [DOI] [PubMed] [Google Scholar]
- 19. Singer SJ, Burgers J, Friedberg M, Rosenthal MB, Leape L, Schneider E. Defining and measuring integrated patient care: Promoting the next frontier in health care delivery. Med Care Res Rev 2011;68:112–127. [DOI] [PubMed] [Google Scholar]
- 20. Strandberg-Larsen M, Krasnik A. Measurement of integrated healthcare delivery: A systematic review of methods and future research directions. Int J Integr Care 2009;9:e01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Suter E, Oelke ND, da Silva Lima MAD, et al. Indicators and measurement tools for health systems integration: A knowledge synthesis. Int J Integr Care 2017;17:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Leutz WN. Five laws for integrating medical and social services: Lessons from the United States and the United Kingdom. Milbank Q 1999;77:77–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Aidala AA, Lee G, Abramson DM, Messeri P, Siegler A. Housing need, housing assistance, and connection to HIV medical care. AIDS Behav 2007;11(Suppl 2):101–115. [DOI] [PubMed] [Google Scholar]
- 24. Messeri P, Abramson DM, Aidala AA, Lee F, Lee G. The impact of ancillary HIV services on engagement in medical care in New York City. AIDS Care 2002;14(Suppl 1):15–29. [DOI] [PubMed] [Google Scholar]
- 25. Mariller M, Abramson D, Sobieszczyk M.. The Validity of Self-Reported Clinical Markers and Medication Regimens: A Pilot Study. New York, NY: Mailman School of Public Health, Columbia University, 2004. [Google Scholar]
- 26. Messeri P, McAllister-Hollod L, Irvine M.. Validating Self-Reported HIV Test Data Using Surveillance Registry Data. New York, NY: Mailman School of Public Health, Columbia University, 2013. [Google Scholar]
- 27. Ware J, Kosinski M, Keller S.. SF-36 Physical and Mental Health Summary Scales: A User's Manual, 5th ed. Boston, MA: Health Assessment Lab, 1994. [Google Scholar]
- 28. Mugavero MJ, Norton WE, Saag MS. Health care system and policy factors influencing engagement in HIV medical care: Piecing together the fragments of a fractured health care delivery system. Clin Infect Dis 2011;52(Suppl 2):S238–S246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Aidala AA, Yomogida M, Vardy Y, Food and Nutrition Study Team. Food and Nutrition Services, HIV Medical Care, and Health Outcomes. New York, NY: Mailman School of Public Health, Columbia University, 2014. [Google Scholar]
- 30. Costenbader E, Mangone E, Mueller M, Parker C, MacQueen KM. Rapid organizational network analysis to assess coordination of services for HIV testing clients: An exploratory study. J HIV/AIDS Soc Serv 2018;17:16–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Jain KM, Maulsby C, Kinsky S, et al. Exploring changes in interagency collaboration following AIDS United's positive charge: A five-site HIV linkage and retention in care program. Heal Educ Behav 2016;43:674–682. [DOI] [PubMed] [Google Scholar]
- 32. Khosla N, Marsteller JA, Hsu YJ, Elliott DL. Analysing collaboration among HIV agencies through combining network theory and relational coordination. Soc Sci Med 2016;150:85–94. [DOI] [PubMed] [Google Scholar]
- 33. Kwait J, Valente DTW, Celentano DD. Interorganizational relationships among HIV/AIDS service organizations in Baltimore: A newtwork analysis. J Urban Health 2001;78:468–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Messeri P, Kim S, Whetten K. Measuring HIV services integration activities. J HIV/AIDS Soc Serv 2003;2:19–44. [Google Scholar]
- 35. Provan KG, Sebastian G. Research notes networks within networks: Service link overlap. Management 1993;41:453–464. [Google Scholar]
- 36. Rosenheck R, Morrissey J, Lam J, et al. Service system integration, access to services, and housing outcomes in a program for homeless persons with severe mental illness. Am J Public Health 1998;88:1610–1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Thomas JC, Carter C, Torrone E, Levandowski BA. Pulling together: Interagency coordination and HIV/STD prevention. J Public Health Manag Pract 2008;14:E1–E6. [DOI] [PubMed] [Google Scholar]
- 38. Thomas JC, Reynolds HW, Alterescu X, Bevc C, Tsegaye A. Improving referrals and integrating family planning and HIV services through organizational network strengthening. Health Policy Plan 2016;31:302–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rebeiro P, Althoff KN, Buchacz K, et al. Retention among North American HIV-infected persons in clinical care, 2000–2008. J Acquir Immune Defic Syndr 2013;62:356–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Torian LV, Wiewel EW. Continuity of HIV-related medical care, New York City, 2005–2009: Do patients who initiate care stay in care? AIDS Patient Care STDS 2011;25:79–88. [DOI] [PubMed] [Google Scholar]
- 41. Almirol EA, McNulty MC, Schmitt J, et al. Gender differences in HIV testing, diagnosis, and linkage to care in healthcare settings: Identifying African American women with HIV in Chicago. AIDS Patient Care STDS 2018;32:399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kay ES, Batey DS, Mugavero MJ. The Ryan White HIV/AIDS Program: Supplementary Service Provision Post-Affordable Care Act. AIDS Patient Care STDS 2018;32:265–271. [DOI] [PubMed] [Google Scholar]
- 43. Fantuzzo J, Culhane DP, eds. Actionable Intelligence: Using Integrated Data Systems to Achieve a More Effective, Efficient, and Ethical Government, 1st ed. New York, NY: Palgrave Macmillan, 2015. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are not available for sharing due to its identifiable individual and service provider information. Any questions or concerns can be directed to the corresponding author.