Abstract
Ursolic acid (UA) is a pentacyclic triterpenoid frequently found in medicinal herbs and plants, having numerous pharmacological effects. UA and its analogs treat multiple diseases, including cancer, diabetic neuropathy, and inflammatory diseases. UA inhibits cancer proliferation, metastasis, angiogenesis, and induced cell death, scavenging free radicals and triggering numerous anti- and pro-apoptotic proteins. The biochemistry of UA has been examined broadly based on the literature, with alterations frequently having been prepared on positions C-3 (hydroxyl), C12–C13 (double bonds), and C-28 (carboxylic acid), leading to several UA derivatives with increased potency, bioavailability and water solubility. UA could be used as a protective agent to counter neural dysfunction via anti-oxidant and anti-inflammatory effects. It is a potential therapeutic drug implicated in the treatment of cancer and diabetic complications diseases provide novel machinery to the anti-inflammatory properties of UA. The pharmacological efficiency of UA is exhibited by the therapeutic theory of one-drug → several targets → one/multiple diseases. Hence, UA shows promising therapeutic potential for cancer and diabetic neuropathy diseases. This review aims to discuss mechanistic insights into promising beneficial effects of UA. We further explained the pharmacological aspects, clinical trials, and potential limitations of UA for the management of cancer and diabetic neuropathy diseases.
Keywords: ursolic acid, clinical trials, diabetic neuropathy, inflammatory diseases, inhibitors, targeted therapy
1. Introduction
Ursolic acid (UA) is a promising triterpenoid compound present in several plants’ leaves, flowers, and fruits [1]. It shows a broad range of pharmaceutical properties and therapeutic effects [2]. UA has been utilized as a herbal medicine with excellent pharmacological activities [3,4]. It mediates alterations in many signaling pathways and subsequently prevents the progression of chronic diseases [5], demonstrating its anti-inflammatory [6], anti-oxidant [7], anti-carcinogenic [8], anti-diabetic [9], neuroprotective effects [10]. UA is effective in the treatment of many inflammatory diseases [4], including Parkinson’s disease [11] and diabetes [12]. In addition, UA has been implicated in neurodegenerative and psychiatric disorders [13]. It has considerable potential as an oral anti-inflammatory and neural repair drug [14], attenuating neuropathic pain in animal models that can probably be attributed to its anti-oxidant and anti-inflammatory properties [15]. The mechanisms of UA by which applies these beneficial consequences might engage regulation of metabolic and atrophy pathway in skeletal muscles, insulin pathway in adipose tissue, apoptotic and NF-κB pathway in tumor cells, level of oxidants and metabolic pathway in the liver, anti-oxidants and inflammation in the brain [16,17,18].
Cancer is the leading cause of human death in economically developed countries [19,20,21]. The cancer burden keeps on enhancing in developing countries due to increasing aging in the population [21,22]; cancer is a major cause of adult deaths worldwide [21,23]. Cancer is a complex disease that may be inhibited [24,25]; cancer progression might take around 10 to 30 years to develop, starting initiation, promotion for development, and progression [24,25]. Hence, the slow growth of the disease potentially permits interference in the development of tumors into advanced stages and metastases. This disease has a high incidence and mortality rate; its treatment indicates a significant clinical challenge. Hence, the advantages of present chemotherapeutics are inadequate because they tend to cause DNA damage in healthy cells [26,27]. However, targeting the regulation of cancer cells without causing toxic effects in healthy cells is a potential strategy for cancer treatment [28,29].
Diabetes mellitus (DM) is a chronic metabolic disorder linked with the emission and sensitivity of insulin [30]. Based on pathogenic developments which cause hyperglycemia, DM is categorized as type 1 or type 2 [31,32,33]. The specific mechanisms to insulin resistance development are still not completely elucidated. A low-grade chronic inflammation, uptake of glucose in adipose and skeletal tissues and various flaws in the intracellular insulin pathway play crucial functions in insulin resistance [34]. Diabetes is a significant health problem, comprising a complex disorder strongly related to nephropathy, cardiomyopathy, and neurodegeneration [35]. Diabetic individuals might suffer from peripheral and central nervous neuropathy, which is linked with impairments in memory and learning [36,37,38,39,40].
Diabetic neuropathy (DN) is a common and challenging complication of DM, leading to the most morbidity and mortality, resulting in a vast economic burden to diabetes care [41,42,43]. Neuropathy is generally widespread; distal symmetric polyneuropathy is very general, leading to sensory disturbances [42,43,44,45]. DN is a failure of sensory function starting distally in the lower extremities, which is considered via pain and substantial morbidity. Hence, 50% of individuals with DM develop DN [46]. DN is a specific neurodegenerative disease of the peripheral nervous system, which targets autonomic and sensory axons at later stages to motor axons with a lesser degree [46]. DN is induced by hyperglycemia and dyslipidemia that modify the insulin signaling pathway, which causes numerous pathological modifications in vascular cells, glia and neurons, leading to dysfunction of nerve and ultimately neuropathy [46,47].
Inflammation engages the activation and employment of phagocytes (neutrophils, macrophages), NK cells, and the discharge of cytokines through activated cells that are crucial to the host defense system. Since the chronic inflammation that continues yet after removal of the pathogen(s) was linked with many diseases, including cancer [48], neoplasms, inflammatory bowel disease [49], Alzheimer’s disease [50], therefore, dysregulation of enzymes and cytokines, might contribute to the pathogenesis of several chronic inflammatory diseases [51]. NF-κB, NF-AT, and AP1 with JNK, ERK, and p38 are well-known for regulating inflammatory cytokines and enzymes targeted through various investigators to improve chronic inflammation [52,53,54]. Inflammation plays a fundamental role in the pathogenesis of DN [55].
The complexities of DN and inflammatory diseases have considerably evolved over the years. Efforts for understanding the etiology of DN and inflammatory diseases are in progress to design attractive therapeutic approaches. In this context, UA may be a potent therapeutic molecule for DN and inflammatory diseases. UA and its derivatives are potential therapeutic candidates that can be explored to treat DN and inflammatory diseases. In this review, we systematically collected current findings concerning biochemistry, potency, pharmacological aspect, drug delivery system, and clinical trials of UA.
2. Structure and Biochemistry of UA
A pentacyclic triterpenoid; UA (3β-3-hydroxy-urs-12-ene-28-oic-acid), contained a C-30 chemical structure made from units of isoprenoid through the A, B, C, D, and E rings [56], with a molecular mass of 456.71 g/mol and has the chemical formula of C30H48O3 [57]. Triterpenoids are secondary metabolites, including more than 20,000 reported compounds linked with many biological mechanism activities [58]. UA was first documented in 1920 [59]. It is soluble in hot glacial acetic acid and alcoholic sodium hydroxide [57]. UA is generally biosynthesized from dammarenyl cations by folding and cyclizing squalene, making the fifth ring of UA via a ring addition, with three oxygen atoms in the transition metal atom [57]. UA biosynthesis found in plant cells derives from cyclical (3S)-oxidosqualene cycling. Hence, the pre-dominant 3S predecessor is changed into a cationic dammarenyl construction undergoing chain growth, making this third separate ring present in the amyrin skeleton, a nucleus in UA [60]. Table 1 illustrates the UA sources with their biological properties.
Table 1.
Sources of UA with their biological properties.
| Plants Species (Family) |
Vegetal Part | UA Content (mg or g) | Type of Study |
Biological Effects | References |
|---|---|---|---|---|---|
| Eucalyptus obliqua (Myrtaceae) | leaves | nr | in vivo | Neuroprotective agent | [70,71] |
| Malus pumila (Rosaceae) | fruits | nr | in vitro | Anti-tumor | [72] |
| Tribulus arabicus (Zygophyllaceae) | aerial parts | 1 g | in vitro and in vivo | Anti-hyperuricemic activity | [73] |
| Panax ginseng (Araliaceae) | roots | nr | in vivo | Anti-hyperlipidemic and anti-oxidant effects | [74] |
| Bursera cuneata (Burseraceae) | aerial parts | 33.3 mg | in vitro and in vivo | Anti-inflammatory and anti-histaminic activity | [75] |
| Sambucus australis (Adoxaceae) | aerial parts | 180 mg | in vitro | Antibacterial and anti-oxidant | [76,77] |
| Fragrae fragrans (Gentianaceae) | fruits | 91 g | in vitro | Anti-proliferation | [78] |
| Saurauja roxburghii (Actinidiaceae) | leaves | nr | in vitro | Cytotoxicity against glioma cells | [79] |
| Ocimum sanctum (Lamiaceae) | whole plant | 11.21 mg | in vitro | Anticancer and anti-proliferation | [80] |
nr = not reported.
UA’s limited bioavailability, solubility, and quick metabolism have hindered their extra clinical functions to therapeutic consequences in various diseases. However, several researchers have identified several alterations to improve UA potency, bioavailability, and solubility in water [61,62]. Many attempts have been completed to synthesize chemical imitation of UA to enhance its efficacy, therapeutic potential and solubility [63,64,65]. The basic construction of UA has been observed in the serum of mice following oral administration and was found to be absorbed well in the gastrointestinal (GI) tract [66]. However, UA was observed in the rat’s cerebrum, 1 h after the oral administration. This suggests the ability of UA in crossing the blood-brain barrier (BBB) [67]. Furthermore, for improving its absorption, UA was administered in liposomes during clinical trials [68,69]. Hence, several preclinical, and clinical trials using UA, indicate promising effects for neurodegenerative and psychiatric diseases [13].
3. Biological Potency of UA
The molecular action of bioactive molecules might open up novel opportunities to the scientific community for developing and improving new therapeutic approaches for tackling dreadful diseases, including neurodegenerative disorders. UA is one such plant-based therapeutic metabolite, which plays a vital function in cell death, angiogenesis, metastasis, and inflammatory processes [59]. Table 2 presents various health benefits, including anti-apoptotic, anti-oxidant, anti-inflammatory, anti-carcinogenic, anti-rheumatic, anti-tumoral, anti-viral, trypanocidal, etc., of UA [81,82]. UA has anti-cancer activity due to low toxicity and commercial accessibility forms [80,83].
Table 2.
UA effects on diabetes and brain pathologies.
| Disease | Experimental Subject | Dosage | Beneficial Effects | References |
|---|---|---|---|---|
| Diabetes | 3T3-L1 adipocytes | 1 μg/mL for 10 min | ↑ Akt, insulin receptor, and GLUT 4 ↑ Glycogen synthase kinase-3β |
[84] |
| Diabetes | Streptozotocin-injected male ICR mice |
0.5 g/kg for 4 weeks | ↓ TNF-α and Glucose ↑ Insulin (pancreatic, plasma) |
[85] |
| Diabetes | Streptozotocin-injected male mice |
200 mg/kg per day for 6 weeks |
↓ Adipocyte dysfunction ↓ Fasting blood glucose ↓ PPAR γ and aP2 ↑ Bone formation |
[86] |
| Metabolic syndrome | Diagnostics of metabolic syndrome patients |
Orally 150 mg/kg for 12 weeks | ↓ Body weight, BMI, and waist circumference ↓ Fasting glucose |
[87] |
| Subarachnoid hemorrhage (SAH) |
Male Sprague Dawley experimental SAH rat model |
25 and 50 mg/kg at 0.5, 24, and 47 h after SAH |
↓ MDA ↑ Neurological score ↑ Cerebral vasospasm ↓ BBB permeability (EB content) ↑ GSH/GSSH ratio, SOD activity, and Catalase activity ↓ Apoptotic index ↓ Caspase-3, -9 mRNA expression |
[88] |
| Parkinson’s disease | Male Swiss albino mice |
5, 25, and 50 mg/kg for 21 days |
↑ Rotarod test ↑ Hanging time ↓ Nitrite level ↓ Narrow beam walking test ↑Acidhomovanilic acid ↑ Dopamine |
[89] |
| Cerebral ischemia and reperfusion injury |
Male Sprague Dawley rats |
5, 10, and 20 mg/kg at 0.5, 24, and 47 h after reperfusion |
↓ Neurological deficit score ↓ Infarct volume ↑ PPARγ protein level ↑ Number of intact neurons ↓MMP-2 & -9 protein levels |
[90] |
| IL-1β or TNF-α- induced C6 glioma invasion |
Rat C6 glioma cells | 5, 10, and 20 μM for 24 h |
↓ MMP-9 activity by TNF-α or IL-1β ↓ IκB kinase activity by IL-1β or TNF-α ↓ IκBα activity by IL-1β or TNF-α ↓ NF-κB activity |
[91] |
| D-Galactose-induced neurodegenerative changes |
Male Kunming strain mice |
10 mg/kg for 8 weeks |
↓ ROS level ↓ AGEs level ↓ Number of CD11b-stained cells, ↓ Carbonyl protein level GFAPstained cells, and RAGE- positive cells ↓ iNOS, IL-6, IL-1β, COX-2, and TNF-α protein levels |
[92] |
| Domoic acid-induced cognitive deficits |
Male ICR mice | 100 mg/kg for 3 weeks | ↑p-Akt ↑ HO-1 ↑ p-FOXO1 ↑ Complex I-V ↑ Electron transport chain activity ↑ APR and ATP |
[93] |
| Adrenocorticotrophic hormone-producing pituitary adenoma |
AtT20 cells (mouse corticotrophic tumor cell line) |
10, 20, and 40 μM for 24 h |
↓ ACTH release ↓ POMC mRNA expression ↓ ACTH protein level ↑ p-JNK/JNK protein level |
[94] |
↓, Decrease; ↑, Increase.
UA is popular due to its anti-proliferative properties, the incentive of tumor cell death, an obstacle of tumorigenesis, and inhibiting the cell cycle in tumors cells. Hence, examining one cell death mechanism that indicated UA could prevent NF-κB pathway through p65 phosphorylation repression, effecting a mandatory reduction in several downstream oncogenes, including Bcl-xL and Bcl-2. The anti-cancer effectiveness of UA is weak due to its lesser solubility that reduces the drug absorption in the human body system, which causes challenges in achieving comprehensive benefits. However, it is required for making its derivatives by semi-synthetic alterations for improving its anti-cancer action. Frequently, the modifications of UA occur on positions C-3, C12–C13, and positions C-28 [63,76,95]. Antimicrobial activity of UA compounds against Mycobacterium tuberculosis H37Rv has been recently reported [96,97]. UA is currently in different phases of clinical studies due to its therapeutic effects and selectivity against several diseases [98,99].
4. Bioavailability and Pharmacokinetic Properties of UA
Cell membrane permeability and pharmacokinetics are vital in the clinical development and improvement of novel biologically active agents/compounds with an outlook for considering their performance in vivo and establishing the most acceptable dosage regimen. Hence, pentacyclic triterpenoids usually suffer from less oral bioavailability [100]. In the organism, a vast inter and intra character absorption variability shows challenges in accomplishing secure and efficient concentration of drug [101]. Physicochemical characters of the molecules are the first reason which affects bioavailability [102]. UA is a low molecular weight compound [58], with three hydrogen bond donors and acceptors. However, these properties for estimating the drug-likeness are in harmony with Lipinski’s rule [103]. UA has more lipophilicity [100] and less wettability [104]. Hence, their absorption is obstructed through slow partitioning between extracellular fluid and cell membrane and poor dissolution. UA can be inserted in the phospholipid bilayer while not taken up via cells [104].
Moreover, aqueous solubility is exaggerated through the crystalline structure of natural UA. Decreased particle size and amorphous state remarkably increased rate of dissolution and solubility of triterpenoid [105]. Adverse characteristics of UA should be addressed in the improvement of pharmaceutical dose shapes. Hence, for overcoming biological barriers, the second main factor is the capability of the drug [102]. The proof from in vitro permeability investigations involves which passive diffusion is the primary process of UA transport [102]. Hence, apparent permeability coefficients, estimated applying Caco-2 monolayers, have been in limits of oral absorption [102], which instant glucuronidation, and sulfation in the intestinal cells, are extremely unlikely [106]. UA is a substrate of cytochrome P450 and P-glycoprotein. Therefore their bio-availability can be limited through biotransformation and active efflux [105,107].
Many pharmacokinetic examinations have exposed where maximal plasma concentration subsequent oral administration of doses up to 300 mg/kg has been low, and removal half-life has been comparatively short (<1 h) [69,105]. This pharmacokinetic outline shows that fast elimination and tissue distribution in the pharmacological results of UA may not be honestly related to plasma concentrations. UA has broad tissue distribution, such as in the animal’s testes, colon, lung, kidney, spleen, brain, liver, heart and bladder [69,108]. The liver is the main organ of the triterpene disposition [108], and liver-related doses limit the toxicity in clinical trial phase I of UA liposomes [109]. UA can cross the blood-brain barrier, and they have potent neuroprotective effects [108]. Targeted delivery for the brain may be attained through particular delivery systems that use UA nano-lipid vesicles in the form of intranasal gel [110]. Hence, high lipophilicity influences triterpenoids for liver metabolism. However, a tissue distribution examination in mice has shown that the UA concentration in plasma was gradually reduced, but the concentration in the liver increased [111].
5. Pharmacological Aspects of UA
5.1. Anti-Diabetic Effect of UA
DM is a chronic disease, which is regulated via deficiency or insulin resistance. DM is one of the main risks for humans globally [103]. Long-term utilization of hypoglycemic agents might decrease their pharmacological action. Due to a complete glucose insufficiency, type 1 diabetes mellitus (DM1) affects hyperglycemia. Hence, this affects various macro and microvascular alterations in pathology, osteopenia, neuropathy, DN, diabetes, and osteoporosis. However, clinical trials have indicated that DM1 enhances tibia, vertebral, proximal humerus and knee rupture risks independent of bone mineral density (BMD) [86]. In diabetic mice, UA is well-recognized to impart beneficial effects in lowering the concentration of blood glucose and curative of related diabetic problems. Hence, UA decreases protein tyrosine phosphatase 1B, gets better phosphorylation of insulin receptors that induce glucose absorption [112].
Obesity and diabetes require inhibition of the pancreatic α-amylase for the treatment because it decreases blood glucose levels in vitro and in vivo [84,113]. A recent study has estimated the UA effects on body weight and glucose tolerance in the metabolic syndrome samples, who obtained UA 150 mg before breakfast to 12–20 weeks [87]. Decreases in blood glucose level, mass index and body weight have been detected in patient samples, suggesting it considerably develops insulin sensitivity. Hence, Chu et al. [114] 0.5% UA diet affected a reduction in body weight and free fatty acids by uncoupling protein 3/AMPK dependent signaling in the HFD mediated obese rats after 06 weeks of the treatment. Reduction in glucose intolerance and body weight gain was observed in mice treated with 0.14% UA diet for up to 6 weeks [115]. Li et al. [113] reported that, in HFD induced obese mice, UA reduced insulin resistance and body weight gain. Hence, 80 μM UA decreases cholesterol and triglyceride levels by reducing the synthesis of fatty acid and enhancing fatty acid oxidation in the hepatocytes, which up-regulation of PPAR-α expression is probably vital to the useful effect of UA [116].
Treatment with UA (50 and 200 mg/kg) reduces lipid accumulation, TG levels and body weight. It enhances HDL cholesterol, insulin sensitivity, brown adipose tissue, and β-oxidation in the HFD-mediated obese rats, which improves energy expenditure [117]. Another exciting study indicated that UA (0.05%) blocks insulin resistance and glucose intolerance through conserving pancreatic β-cells in diabetic mice [85]. Since UA effects were identified by Kunkel et al. [115], UA is the primary controller of glucose levels in diabetes [84]. The AMPK regulation levels through blocking liver enzyme B1 are critical to the treatment of diabetes and obesity. Hence, this suggests the significance of UA in diabetes treatment. The anti-diabetes effect of UA is described in Table 2.
TGR5 activation via a chemical agonist might enhance incretin secretion and decrease the blood sugar level. UA has the potential effect on TGR5. UA concentration enhanced glucose uptake in the CHO-K1 cells, which express TGR5. TGR5 may improve cAMP for activating PKA and downstream pathways. UA stimulated a concentration-dependent increase in GLP-1 emission blocked through triamterene on the efficient concentrations for blocking TGR5 in NCI-H716 cells [118,119]. TGR5 agonist was positive results in T2DM-like animals [120]. UA enhanced the plasma GLP-1 level by activating TGR5 that has been illustrated in vivo with type 1-like diabetic rats. UA may trigger TGR5, increasing GLP-1 secretion in vitro as well as in vivo. However, UA is appropriate to use in the activation of TGR5 [118].
5.2. Neuroprotective Effect of UA
Neurological disorders comprise anxiety, stroke, depression, PD, and AD [76,121,122,123,124]. Long-term neurological effects may not be developed through subarachnoid hemorrhage (SAH) therapies, which decrease the occurrence of cerebral vasospasm, showing their significance in the patient result has been misconstrued. Early brain injury (EBI) was observed as the primary reason for adverse effects in SAH patients.
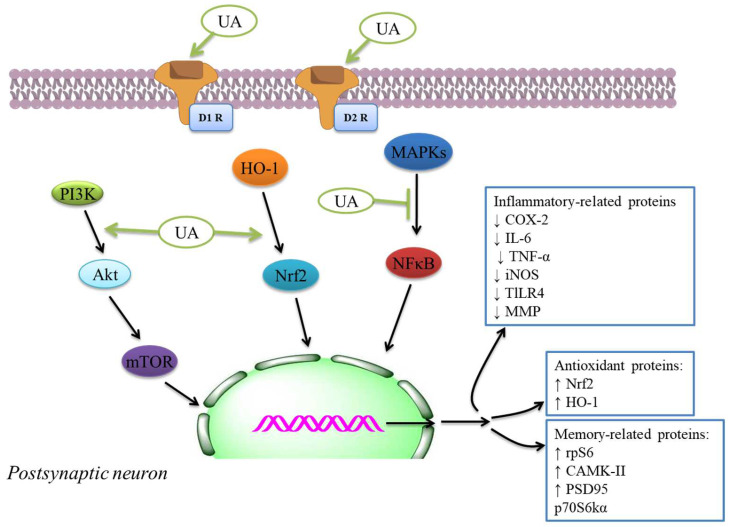
Several reports suggest UA remains a vital and admired anti-oxidant reagent; for example, it has a brain defensive effect for ischemic stroke [88]. Oxidative stress was reported as being amongst the complicated reasons linked with neuronal death following SAH. ROS and H2O2 play a critical function after SAH [125]. Redox-sensitive Nrf2 activation has a central location in getting a better endogenous protection process by which the brain defends itself against ischemic injury and improves from the stroke [126]. Pro-inflammatory and oxidative actions are involved in many CNS-related diseases (Figure 1). The neuroprotective results of UA against a model of ischemia [126]. The results of UA in decreasing EBI might be described through mitigation of oxidative stress at SD rats. Hence, UA may be considered a potential therapeutic drug for neurological diseases [88].
Figure 1.
Anti-inflammatory and anti-oxidant mechanisms of neuronal function and neuroprotection through UA. Glial cells play a critical function in neuro-inflammation and oxidative stress, common in various neurodegenerative diseases. By repressing the making of ROS, AGEs, and LPO products and enhancing anti-oxidant defenses by upregulation of the Nrf2 signaling, UA shows neuroprotective consequences in neuronal cells (Habtemariam S, 2019). UA has various roles in the CNS. (−), inhibition; (+), promotion; ↓, Decrease; ↑, Increase.
PD is a chronic progressive neurodegenerative disease described by motor and non-motor features [127,128,129,130]. Its increasing degenerative effects on muscle regulation and mobility have a key clinical result for caregivers, families and patients [131]. Hence, in age-related developing neurodegenerative disorders, following Alzheimer’s, it is the second most frequent and is characterized via dopaminergic (DA) neuron decrease and neuroinflammation [89,132,133]. The neuroprotective efficacy of UA in 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)-mediated PD mouse models. Hence, the authors identified; UA enhances cognitive deficits, repairs altered dopamine levels, and defends the MPTP intoxicated mouse’s DA neurons. Along with different doses, the main competent dose to PD was 25 mg/kg body wt. [89].
Oxidative stress and excitotoxicity are the two mechanisms that have been continually demonstrated as being involved in a broad range of diseases of the brain and nervous system [134,135,136,137,138,139,140]. It can lead to stable brain harm and reduction of cognitive functions [141,142,143]. The first investigation focusing on the protective consequence of UA on neurons was performed by Shih et al. [144]. UA significantly reduced and repressed free radical production. The study [145] was examined the protective result of UA against galactose-mediated damage in mice brains. Repressing NF-κB through UA as a process for attenuating cognitive deficits and avoiding brain damage was identified by Wang et al. [146] and Li et al. [126]. These models have been lipopolysaccharide-damaged mouse brains after cerebral ischemia [93], illustrating intracellular pathways engaged in UA neuroprotective activity. Hence, UA may trigger PI3K/Akt pathway and repress FoxO1 activity in domoic acid-mediated mice. PI3K/Akt activation appears to motivate UA’s results in the excitotoxicity model [93]. UA was capable of restoring the levels of knowledge and memory-connected proteins, including postsynaptic density protein 95 and Ca2+ calmodulin-dependent protein kinase II mediated via a high-fat diet through activating the mTOR pathway induced via p70 S6 kinase alpha and S6 ribosomal protein in the hippocampus [147]. These results might induce the activation of PI3K and mTOR pathways (Figure 2). Hence, the neuroprotective effects of UA have been examined against the neurochemical and behavioral modifications induced through MPTP for model PD [89].
Figure 2.
Descriptive proposal of the molecular targets altered through UA in a putative synapse. UA can modulate various receptors, including dopamine D1 and D2. UA might trigger nuclear factor (erythroid-derived 2)-like 2/heme oxygenase 1 (Nrf2/HO-1) and PI3K/Akt/mTOR, that can inhibit MAPK/NF-κB-mediated pathways. These intracellular pathways’ inflection can provide the expression of proteins involved in cognitive improvement and anti-oxidant and anti-inflammatory effects. D1R, dopamine receptor 1; D2R, dopamine receptor 2; ↓, Decrease; ↑, Increase.
Oxidative stress and excitotoxicity usually result in mild to severe nervous system defects [2]. Inequity in the cellular homeostasis might everlastingly decrease cognitive function and affect brain injure [141,148], resulting in a variety of brain diseases [149]. Hence, the effects of UA on brain disorders that block oxidative stress [88] and excitotoxicity [144] suggest; it can play a protective function in several brain disorders induced through excitotoxicity and oxidative stress. However, UA represses the apoptotic pathway [88] and wields anti-inflammatory results in the brain [91]. Researchers have identified that UA blocks the activity of MMP-9, which is a potent cause of several tumors in C6 glioma cells [91,150]. UA might repress NF-kB-dependent signaling pathways, which are triggered via TNF-α/IL-1β [151]. In a rat model of cerebral ischemia and reperfusion injury, Wang et al. [90], showed the relationship between UA and MMP-2/-9. Since the activities of MMP-2, and MMP-9, were repressed through UA administration. Hence, UA has a defensive effect against several inflammatory situations of the brain.
In cerebral ischemia and reperfusion injury, TLRs play a critical role by inducing the making of inflammatory mediators, including ILs and TNF-α [152,153,154]. TLR4 was primarily reported as receptors to endogenous ligands such as DAMPs, and HMGB1, during brain injury. UA controls the TLR pathway and shows prominent anti-inflammatory functions. UA demonstrates biological actions in the brain, such as anti-inflammatory, anti-oxidative, anti-rheumatic and anti-tumor effects [155]. UA decreases inflammatory cytokine-making to protect the brain from cerebral ischemia and reperfusion injury, probably by HMGB1/TLR4/NF-κB pathway [156]. UA might be helpful as a potential efficient adjunct for therapy to ischemic brain injury before reperfusion.
5.3. Anti-Inflammatory Effect of UA
Inflammation plays an essential role in developing and progressing multiple diseases, including neuropathy, insulin resistance, and diabetes [157], cancer [158,159,160,161,162]. After injury and microbial attack, the inflammatory reaction is started to recover homeostatic tissue equilibrium between composition and physiological role. Hence, persistent inflammation can cause harm to tissues, affecting non-functioning tissues/organs [163,164]. Inflammation is an obscured incidence connected to the progression of various diseases, including neurodegenerative diseases and cancer [165]. Acute inflammation, with attendant cytokine action and the increased output of ROS, is reported like a tumor-promoting disease [166,167,168]. For detecting the anti-inflammatory activity, the study reported UA’s capability to reduce the making of TNF-α in A549 and RAW 267.4 cell lines infected by Mycobacterium tuberculosis and Con A-stimulated mouse splenocytes.
The authors examined UA action intending to reduce COX-2 and NO synthase levels found in roused cells. Hence, UA showed a considerable inhibitory effect of cytokine levels, immunomodulatory mediators, and liberate of NO. This compound may be used for tuberculosis and antibiotic therapy due to the UA’s anti-inflammatory effectiveness in cells [169]. The study showed in vitro inhibition of COX-2 action was because of UA and cranberry extracts [170], indicating potential anti-inflammatory and anti-oxidant activity (Table 2). The anti-inflammatory activity was investigated by utilizing enzyme inhibitory examine in vitro COX-1 and COX-2 [171,172]. The molecular docking discoveries exhibited; the UA derivatives indicated elevated attraction to effective COX-2 site, potentially showing anti-inflammatory effectiveness by COX-2 inhibition. Hence, UA and its derivatives showed anti-inflammatory activity that might cause the development and improvement of potentially novel and secure COX-2 inhibitors [173,174]. The anti-inflammatory mechanisms inhibit main inflammatory cytokines, iNOS and COX expressions, and anti-oxidant mechanisms like the activation of Nrf2 signaling. The inflammatory and anti-oxidant mechanisms of neuroprotection through UA [175] are also indicated by the plethora of extra systemic results of UA in several experimental models [175]. The effects were linked with the inhibition of NF-κB translocation to the nucleus (Figure 2) and decreased expression of iNOS, COX-2, TNF-α, and interleukin-6 that decreased the phosphorylation of p38MAPK in the mouse brain [146].
Terpenoids could have anti-oxidant results in vivo through mediating anti-oxidant defenses, including CAT, SOD, GPx, and GR, exhibited to their therapeutic potent in AD by a range of assays [176,177,178,179,180]. These compounds display anti-oxidant effects and possess anti-inflammatory functions. They are tackling complex diseases by what has been explained as one drug → multi-targets → one/many disease(s) therapeutic theory [181]. In this perspective, the therapeutic promising of UA like a prototype lead is exhibited in several CNS diseases, mainly by anti-inflammatory and anti-oxidant mechanisms. The anti-oxidant–anti-inflammatory axis was indicated to play a function in the anti-diabetic effect of UA as displayed in streptozotocin-mediated rats [182] in db/db diabetic mouse model [183], DN models [184], diabetic-mediated monocyte dysfunction in mice [185], aortic damage in the STZ-mediated diabetic rats [186].
5.4. Anti-Cancer Effect of UA
Cancer is a complex disease due to tumor heterogeneity, a major limitation of chemoprevention [187,188,189,190,191,192]. The anti-cancer potency of these agents was analyzed in several tumor cells, like, A-549, THP-1, HCT-116, MCF-7, and ordinary adult epithelial cells (FR-2). The anti-cancer potencies of UA and its derivatives against these cells were detected [193]. UA caused Bcl-2 down-regulation and Bax up-regulation and released cyt-c from mitochondria to the cytosol. Hence, UA cleaved caspase-9 and decreased mitochondrial membrane ability. The mechanism of UA is dependent on the death receptor. UA might be used as a promising substance of biological source while it comes to cancer prevention and therapy, changing their metabolism to prevent metastasis and angiogenesis [2,194,195].
Researchers have examined the valuable results of UA on cell metabolism in humans and rodents. Hence, the mechanisms fundamental to the anti-tumor development of UA [196] and tumor cell proliferation [197], inflection of cell death [198], inhibition of cell cycle arrest [199]. UA was showed useful effects on cell death and autophagy in breast cancer cells. Lewinska et al. [198] identified that 20 μM UA blocks the activation of Akt and promotes apoptosis and autophagy in cancer cells. Hence, it also reduces the pERK1/2 level. UA provokes Akt activation, enhances the oxidative system, and reduces the ATP levels, lactate, and glycolytic enzymes, including pyruvate kinase and hexokinase 2 in breast cancer cells [200,201]. It reduces ATP making and activates AMPK that inhibits proliferation in cancer cells [202]. UA can be a potential controller of AMPK that blocks glycolysis and cancer survival in vivo [201]. It inhibits cell proliferation in tumor cells [203]. Yan et al. [204] identified UA activates a pro-apoptotic pathway in liver tumor cells. UA exerts considerably improved pro-apoptotic results through enhancing the caspase-3 and caspase-8 levels and DNA fragmentation in tumor cells. Hence, UA reduces Na+–K+-ATPase action and MMP, showing mitochondrial dysfunction in cancer cells [16].
Autophagy facilitates the continuance of metabolic precursors regeneration and cellular homeostasis. The function of autophagy in cancer might be viewed as a controversial procedure. The process of autophagy may be a selective as well as a non-selective mechanism. Some studies showed that autophagy inhibits cancer progression and development [205], and on the other hand, studies indicated that autophagy has a protective function on cancer cells [206]. UA stimulates autophagy in A549 cells [207]. UA-mediated autophagy in PC3 cells is linked with decreased cell viability [208]. However, UA activates the mTOR/Akt pathway and through the modulation of PI3K/Akt pathway, UA induces autophagy [208]. In response to growth factors and nutrient accessibility, autophagy is triggered via mTOR/PI3K/Akt, which controls protein synthesis and cell growth [209].
6. Drug Delivery System
UA and its derivatives have been involved in various pharmacological applications linked with the prevention of diseases. UA can be used as a potential applicant for developing a comprehensive capable strategy towards preventing and treating health disorders [59]. UA displays a variety of pharmacological effects, less solubility in the aqueous medium that affects its therapeutic function and bioavailability because the polarity and solubility of the material may affect its capability for penetrating biological membranes [210]. Several strategies might be utilized for overcoming these limitations, including particle size reduction, chemical alterations, salt creation of the molecules, application of surfactants, pH adjustment of agent/drug into various delivery systems [211,212]. However, drug delivery systems were exploited with significant achievements for improving UA’s Physicochemical functions and therapeutic application. Besides improving solubility, they also change drug discharge and enhance the bio-availability of hydrophobic agents and drugs [213]. Various nano-carriers have been utilized for UA delivery, including nanoemulsions, polymeric nanoparticles, mesoporous silica nanoparticles, liposomes, solid lipid nanoparticles, and solid dispersions [58].
The study’s pH-sensitive mesoporous silica nanoparticles have been established to be biocompatible and permitted sustained liberation of UA [214]. Moreover, that is increasing the cytotoxic result against HepG2 cells contrasted with free UA. Another study that examined the development in drug dissolution profile [215] estimated the in vitro dissolution summary, trypanocidal effect, and cytotoxicity effect of UA by the nanoemulsions-based delivery system. Nahak et al. [216] reported the loss in UA crystallinity after analyzing the UA loaded in solid–lipid nanoparticles physicochemical characteristics.
The lipid matrix influences the rate of drug discharge and agent/drug discharge patterns, showing an anti-cancer effect more significant than free UA against K562 and B16 cells. Long-circulating and pH SpHL-UA were utilized to improve drug administration intravenously, its anti-tumoral result on LNCaP and MDA-MB-231 tumor cells [217]. Hence, solid dispersions may be an attractive approach for the delivery of UA. These contain molecular combinations of carriers with hydrophobic agents/drugs, which are amphiphilic/hydrophilic, which permit a decrease of drug particle size that may develop the solubility and modulate drug discharge profile [218]. Hence, some new technologies have been applied for producing UA preparations, which may modify the pharmacokinetics procedure and enhance its solubility and bioavailability [219].
7. Preclinical and Clinical Studies of UA
7.1. In Vitro Studies
Extensive studies have produced data representing the in vitro [220] and in vivo [197] anti-tumoral effects of UA [221], identifying its capability for adapting molecular targets engaged in the progression and development of psychiatric and neurodegenerative disorders. However, the capability of UA to apply neuroprotective results against excitotoxicity, a crucial process linked in neurodegenerative disorders, including PD and AD, might be related to its probable therapeutic potency in the management of diseases [13,222]. A broadly applied in vitro PD model contains mediating excitotoxicity for neurons with MPTP, its dynamic metabolite. Since neurotoxic compounds are likely to accumulate in DA neurons, they induce ROS and stimulate oxidative imbalance and inflammatory damage [223]. The neuroprotective result of UA against MPTP has been identified in PC12 cells [224]. AD, one of the largest established progressive neurodegenerative diseases [225], is generally distinguished through cognitive impairment and progressive neurodegeneration [226]. Hence, one of the major neurochemical modifications for AD is making amyloid plaques enclosing protein fragments called Ab [227]. The Ab plaques can stimulate neurotoxic effects via enhancing ROS manufacture, inflammation, and cell death [227].
The participation of inflammatory processes in the progression and development of AD was broadly identified [228]. In particular, enhanced making of cytokines and ROS and neuroinflammation can result from Ab accumulation [228]. Activating MAPKs starts a signaling pathway, which leads to the activation and translocation of NF-κB to the nucleus, which is involved in making and liberating pro-inflammatory molecules [229]. UA can also show defensive activity against an Ab-mediated neuroinflammatory result [230,231]. Treatment of PC12 cell lines by UA inhibited the expression of iNOS and COX-2-mediated through Ab25–35 [231]. This anti-inflammatory result of UA is induced, at any rate partially, via the decline in the phosphorylation level of ERK1/2, c-Jun NH2-protein kinase, and p38MAPK that subsequently can block NF-κB translocation to the nucleus [231].
7.2. Clinical Trials
The final aim of cancer and neurological research is the functioning and implementation of drugs or compounds for clinical utilization. Presently, UA is undergoing phase I studies for evaluating its safety and adverse effects in the patients. Hence, due to less water solubility and low bioavailability of UA was administered as liposomes. Studies have been reported [109,232,233], UA liposomes exhibited adequate toxicity and adverse effects. The most common objections were diarrhea, nausea, and skin troubles. The conclusion of these studies and analysis was the requirement of the continuance of investigates during phase II studies. The combination of UA sub-effective doses with bupropion, fluoxetine used a synergic anti-depressant effect in TST [234,235]. These effects recommend; UA treatment might improve the efficiency of anti-depressants. Monoaminergic neurotransmission may be concerned with the anti-immobility results of UA in TST. This mechanism of action is a characteristic of triple reuptake anti-depressant agents or compounds [236] that act via blocking the reuptake of NE, 5-hydroxytryptamine, and DA. This group of drugs comprises a novel anti-depressant plan and strategy, affording a more quick response outline, an improved efficiency, and fewer side effects compared with particular or double monoamine receive inhibitors in the clinical studies [237,238,239]. Hence, UA administration can be a potential anti-depressant strategy.
A recent study has estimated the new formulation in 63 Chinese persons, including 4 advanced solid tumor patients and 59 normal samples. In the single administration by oral UANL (37, 74, 98, and 130 mg/m2), the high concentration of UA in plasma was attained in 4 h [240]. One clinical trial calculated the result of UA after 8 weeks of resistant exercise in the male samples [241]. In this examination, 16 normal men were given three capsules of UA (450 mg) every day for 8 weeks [241]. The subjects were given UA and decreased their percentage of body fat and enhanced muscle potency without modifications in skeletal muscle mass [241]. In addition, the blood levels of irisin and insulin-like growth factor-1 were enhanced in the subjects. Improvements can be associated with the UA effects in skeletal muscle [241]. Many studies were indicated that the improved making of irisin in the muscle induced through physical exercise could encourage the making of neurotrophins in the hippocampus [242], neurogenesis, and synaptogenesis in rodents [243]. Multiple synthesized methods based on UA with anti-diabetic, anti-inflammatory, and cardioprotective were identified [243], the neuroprotective potential of UA and analogous compounds, advising, which they can be helpful to the management of PD and AD.
8. Conclusions and Future Directions
UA is a natural compound, which humans have securely utilized in different forms. UA shows various biological effects and exhibits its potential effects in the prevention and treatment of several pathologies. Hence, the pharmacological results of UA showed anti-cancer, anti-diabetic, neuroprotective, and anti-inflammatory mechanisms in the cellular and animal models. A new potential opportunity could be managing cancer, diabetic neuropathy, and inflammatory diseases with UA based on its pharmacological functions. UA’s anti-cancer and neuroprotective activity might be linked with its capability to stimulate the anti-oxidant defense systems and down-regulating the pro-inflammatory signaling pathways in the neurodegeneration and ischemic brain alter models in vitro and in vivo. Several in vitro and in vivo studies identified that UA is a promising phytocompound in treating and managing cancer. The beneficial role of UA to neurodegenerative diseases is that it allocates several neurobiological mechanisms, including oxidative stress, neuroplasticity, neuro-inflammation, and impaired signaling pathways.
In addition, preclinical trials have recommended the beneficial effects of UA on traumatic brain injury, cerebral ischemia, and brain hemorrhage. Hence, all these potential preclinical trial studies, merely a limited number of clinical trial studies, have examined the promising beneficial results of UA to the prevention and treatment of cancer and diabetic neuropathy diseases. Hence, UA appears to be a potential therapeutic strategy that justifies prospective clinical trial studies, believing it’s safe to utilize. Preclinical and well-conducted clinical studies have modified practice parameters and more personalized moves toward treating diabetic neuropathy and inflammatory diseases. Our perceptive of clinical studies presentation and best possible therapeutic management of cancer and diabetic neuropathy from the establishment to current paradigm modify in preclinical trials research space.
Accumulating clinical and preclinical studies research in the subsequent decade may and will revolutionize this scenario. Further investigations and applications might facilitate the opportunity for UA to be improved and developed in new drugs to treat several human diseases, including cancer and diabetic neuropathy. In addition, the cellular and molecular mechanisms’ most important effects of UA in cancer and diabetic neuropathy diseases should be further investigated for implementing UA as a workout mimetic.
Acknowledgments
A.M.E. extends his appreciation to the Deanship of Scientific Research at Jouf University for funding his work through Research Grant Number (DSR-2021-01-0364). M.A. expresses thanks to the Indian Council of Medical Research for financial support (Grant No. 45/6/2020-DDI/BMS). M.I.H. expresses gratitude to the Department of Science and Technology, Government of India, for the FIST support (FIST program No. SR/FST/LSI-541/2012).
Abbreviations
| ursolic acid | UA |
| mitochondrial membrane permeabilization | MMP |
| cyclooxygenase 2 | COX-2 |
| nuclear Factor Kappa B | NF-κB |
| mechanistic target of rapamycin | mTOR |
| chronic lymphocytic leukemia | CLL |
| reactive oxygen species | ROS |
| hydrogen peroxide | H2O2 |
| non-small cell lung cancer | NSCLC |
| non-Hodgkin lymphomas | NHL |
| tumor necrosis factor | TNF |
Author Contributions
M.A. (Manzar Alam): conceptualization, writing—original draft preparation, data curation, investigation, methodology; S.A. (Sabeeha Ali): conceptualization, methodology, writing—original draft preparation; S.A. (Sarfraz Alam): data analysis, validation, visualization; A.M.E.: formal analysis, supervision, investigation, and validation; M.A. (Mohd Adnan): methodology, writing—review and editing; A.I.: methodology, writing—review and editing; M.I.H.: conceptualization, writing—original draft preparation, investigation; D.K.Y.: conceptualization, data analysis, validation, project administration, writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This work is supported and funded through the Indian Council of Medical Research (Grant No. 45/6/2020-DDI/BMS).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The information that supports the findings of this study is available in this article.
Conflicts of Interest
All authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Jager S., Trojan H., Kopp T., Laszczyk M.N., Scheffler A. Pentacyclic triterpene distribution in various plants—Rich sources for a new group of multi-potent plant extracts. Molecules. 2009;14:2016–2031. doi: 10.3390/molecules14062016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wozniak L., Skapska S., Marszalek K. Ursolic Acid—A Pentacyclic Triterpenoid with a Wide Spectrum of Pharmacological Activities. Molecules. 2015;20:20614–20641. doi: 10.3390/molecules201119721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hussain H., Green I.R., Ali I., Khan I.A., Ali Z., Al-Sadi A.M., Ahmad I. Ursolic acid derivatives for pharmaceutical use: A patent review (2012–2016) Expert Opin. Ther. Patents. 2017;27:1061–1072. doi: 10.1080/13543776.2017.1344219. [DOI] [PubMed] [Google Scholar]
- 4.Lee S.Y., Kim Y.J., Chung S.O., Park S.U. Recent studies on ursolic acid and its biological and pharmacological activity. EXCLI J. 2016;15:221. doi: 10.17179/excli2016-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Van Kiem P., Hang D.T., Nhiem N.X., Tai B.H., Anh H.L.T., Van Cuong P., Quang T.H., Van Minh C., Van Dau N., Kim Y.A., et al. Sesquiterpene derivatives from marine sponge Smenospongia cerebriformis and their anti-inflammatory activity. Bioorg. Med. Chem. Lett. 2017;27:1525–1529. doi: 10.1016/j.bmcl.2017.02.040. [DOI] [PubMed] [Google Scholar]
- 6.Kashyap D., Sharma A., Tuli H.S., Punia S., Sharma A.K. Ursolic Acid and Oleanolic Acid: Pentacyclic Terpenoids with Promising Anti-Inflammatory Activities. Recent. Pat. Inflamm. Allergy. Drug. Discov. 2016;10:21–33. doi: 10.2174/1872213X10666160711143904. [DOI] [PubMed] [Google Scholar]
- 7.Liobikas J., Majiene D., Trumbeckaite S., Kursvietiene L., Masteikova R., Kopustinskiene D.M., Savickas A., Bernatoniene J. Uncoupling and antioxidant effects of ursolic acid in isolated rat heart mitochondria. J. Nat. Prod. 2011;74:1640–1644. doi: 10.1021/np200060p. [DOI] [PubMed] [Google Scholar]
- 8.Shishodia S., Majumdar S., Banerjee S., Aggarwal B.B. Ursolic acid inhibits nuclear factor-kappaB activation induced by carcinogenic agents through suppression of IkappaBalpha kinase and p65 phosphorylation: Correlation with down-regulation of cyclooxygenase 2, matrix metalloproteinase 9, and cyclin D1. Cancer Res. 2003;63:4375–4383. [PubMed] [Google Scholar]
- 9.Yu S.G., Zhang C.J., Xu X.E., Sun J.H., Zhang L., Yu P.F. Ursolic acid derivative ameliorates streptozotocin-induced diabestic bone deleterious effects in mice. Int. J. Clin. Exp. Pathol. 2015;8:3681–3690. [PMC free article] [PubMed] [Google Scholar]
- 10.Wang Y., He Z., Deng S. Ursolic acid reduces the metalloprotease/anti-metalloprotease imbalance in cerebral ischemia and reperfusion injury. Drug. Des. Devel. Ther. 2016;10:1663–1674. doi: 10.2147/DDDT.S103829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mortiboys H., Aasly J., Bandmann O. Ursocholanic acid rescues mitochondrial function in common forms of familial Parkinson’s disease. Brain. 2013;136:3038–3050. doi: 10.1093/brain/awt224. [DOI] [PubMed] [Google Scholar]
- 12.Alqahtani A., Hamid K., Kam A., Wong K.H., Abdelhak Z., Razmovski-Naumovski V., Chan K., Li K.M., Groundwater P.W., Li G.Q. The pentacyclic triterpenoids in herbal medicines and their pharmacological activities in diabetes and diabetic complications. Curr. Med. Chem. 2013;20:908–931. [PubMed] [Google Scholar]
- 13.Ramos-Hryb A.B., Pazini F.L., Kaster M.P., Rodrigues A.L.S. Therapeutic potential of ursolic acid to manage neurodegenerative and psychiatric diseases. CNS Drugs. 2017;31:1029–1041. doi: 10.1007/s40263-017-0474-4. [DOI] [PubMed] [Google Scholar]
- 14.Zhang Y., Li X., Ciric B., Curtis M.T., Chen W.-J., Rostami A., Zhang G.-X. A dual effect of ursolic acid to the treatment of multiple sclerosis through both immunomodulation and direct remyelination. Proc. Natl. Acad. Sci. USA. 2020;117:9082–9093. doi: 10.1073/pnas.2000208117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bhat R.A., Lingaraju M.C., Pathak N.N., Kalra J., Kumar D., Kumar D., Tandan S.K. Effect of ursolic acid in attenuating chronic constriction injury-induced neuropathic pain in rats. Fundam. Clin. Pharmacol. 2016;30:517–528. doi: 10.1111/fcp.12223. [DOI] [PubMed] [Google Scholar]
- 16.Seo D.Y., Lee S.R., Heo J.-W., No M.-H., Rhee B.D., Ko K.S., Kwak H.-B., Han J. Ursolic acid in health and disease. Korean J. Physiol. Pharmacol. 2018;22:235–248. doi: 10.4196/kjpp.2018.22.3.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dhakal H., Kim M.J., Lee S., Choi Y.A., Kim N., Kwon T.K., Khang D., Kim S.-H. Ursolic acid inhibits FcepsilonRI-mediated mast cell activation and allergic inflammation. Int. Immunopharmacol. 2021;99:107994. doi: 10.1016/j.intimp.2021.107994. [DOI] [PubMed] [Google Scholar]
- 18.Son J., Lee S.Y. Therapeutic Potential of Ursonic Acid: Comparison with Ursolic Acid. Biomolecules. 2020;10:1505. doi: 10.3390/biom10111505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bray F., Ferlay J., Soerjomataram I., Siegel R.L., Torre L.A., Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer. J. Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 20.Ferlay J., Soerjomataram I., Dikshit R., Eser S., Mathers C., Rebelo M., Parkin D.M., Forman D., Bray F. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer. 2015;136:E359–E386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 21.Ferlay J., Shin H.R., Bray F., Forman D., Mathers C., Parkin D.M. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int. J. Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 22.Alam M., Kashyap T., Pramanik K.K., Singh A.K., Nagini S., Mishra R. The elevated activation of NFκB and AP-1 is correlated with differential regulation of Bcl-2 and associated with oral squamous cell carcinoma progression and resistance. Clin. Oral Investig. 2017;21:2721–2731. doi: 10.1007/s00784-017-2074-6. [DOI] [PubMed] [Google Scholar]
- 23.Alam M., Kashyap T., Mishra P., Panda A.K., Nagini S., Mishra R. Role and regulation of proapoptotic Bax in oral squamous cell carcinoma and drug resistance. Head Neck. 2019;41:185–197. doi: 10.1002/hed.25471. [DOI] [PubMed] [Google Scholar]
- 24.Sporn M.B. Perspective: The big C—For Chemoprevention. Nature. 2011;471:S10–S11. doi: 10.1038/471S10a. [DOI] [PubMed] [Google Scholar]
- 25.Alam M., Mishra R. Bcl-xL expression and regulation in the progression, recurrence, and cisplatin resistance of oral cancer. Life. Sci. 2021;280:119705. doi: 10.1016/j.lfs.2021.119705. [DOI] [PubMed] [Google Scholar]
- 26.Ramirez C.N., Li W., Zhang C., Wu R., Su S., Wang C., Gao L., Yin R., Kong A.-N. In Vitro-In Vivo Dose Response of Ursolic Acid, Sulforaphane, PEITC, and Curcumin in Cancer Prevention. AAPS J. 2017;20:19. doi: 10.1208/s12248-017-0177-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rana R., Rathi V., Chauhan K., Jain K., Chhabra S.S., Acharya R., Kalra S.K., Gupta A., Jain S., Ganguly K.N., et al. Exploring the role of epidermal growth factor receptor variant III in meningeal tumors. PLoS ONE. 2021;16:e0255133. doi: 10.1371/journal.pone.0255133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li Y., Wang Y., Zhou Y., Li J., Chen K., Zhang L., Deng M., Deng S., Li P., Xu B. Cooperative effect of chidamide and chemotherapeutic drugs induce apoptosis by DNA damage accumulation and repair defects in acute myeloid leukemia stem and progenitor cells. Clin. Epigenet. 2017;9:1–14. doi: 10.1186/s13148-017-0377-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ali S., Alam M., Hasan G.M., Hassan M.I. Potential therapeutic targets of Klebsiella pneumoniae: A multi-omics review perspective. Brief. Funct. Genom. 2021:elab038. doi: 10.1093/bfgp/elab038. [DOI] [PubMed] [Google Scholar]
- 30.Ward P.S., Thompson C.B. Metabolic reprogramming: A cancer hallmark even warburg did not anticipate. Cancer Cell. 2012;21:297–308. doi: 10.1016/j.ccr.2012.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alam M., Ali S., Mohammad T., Hasan G.M., Yadav D.K., Hassan M. B Cell Lymphoma 2: A Potential Therapeutic Target for Cancer Therapy. Int. J. Mol. Sci. 2021;22:10442. doi: 10.3390/ijms221910442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stumvoll M., Goldstein B.J., van Haeften T.W. Pathogenesis of type 2 diabetes. Endocr. Res. 2007;32:19–37. doi: 10.1080/07435800701743810. [DOI] [PubMed] [Google Scholar]
- 33.Lee J., Kim K.H., Ahn J.C., Kim J.A., Lee G., Son J.S., Choi S.J., Oh Y.H., Park S.M. Prevalence, awareness, treatment, and control of diabetes mellitus by depressive symptom severity: A cross-sectional analysis of NHANES 2011–2016. BMJ Open. Diabetes Res. Care. 2021;9:e002268. doi: 10.1136/bmjdrc-2021-002268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Han S.J., Son Y.J., Kim B.H. Association between Diabetes Mellitus and Oral Health Status in Patients with Cardiovascular Diseases: A Nationwide Population-Based Study. Int. J. Environ. Res. Public Health. 2021;18:4889. doi: 10.3390/ijerph18094889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim H.L., Kim H.M., Kwon C.H., Shin J.H., Jung M.H., Lee C.J., Kim D.-H., Kim W.-H., Kang S.-H., Lee J.-H. Blood pressure levels and cardiovascular risk according to age in patients with diabetes mellitus: A nationwide population-based cohort study. Cardiovasc. Diabetol. 2020;19:181. doi: 10.1186/s12933-020-01156-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sesti G. Pathophysiology of insulin resistance. Best Pract. Res. Clin. Endocrinol. Metab. 2006;20:665–679. doi: 10.1016/j.beem.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 37.Garrahy A., Moran C., Thompson C.J. Diagnosis and management of central diabetes insipidus in adults. Clin. Endocrinol. 2018;90:23–30. doi: 10.1111/cen.13866. [DOI] [PubMed] [Google Scholar]
- 38.Dewanjee S., Das S., Das A.K., Bhattacharjee N., Dihingia A., Dua T.K., Kalita J., Manna P. Molecular mechanism of diabetic neuropathy and its pharmacotherapeutic targets. Eur. J. Pharmacol. 2018;833:472–523. doi: 10.1016/j.ejphar.2018.06.034. [DOI] [PubMed] [Google Scholar]
- 39.Lee M.K., Kim S.G., Watkins E., Moon M.K., Rhee S.Y., Frias J.P., Chung C.H., Lee C.-H., Block B., Cha B.S., et al. A novel non-PPARgamma insulin sensitizer: MLR-1023 clinicalproof-of-concept in type 2 diabetes mellitus. J. Diabetes Complicat. 2020;34:107555. doi: 10.1016/j.jdiacomp.2020.107555. [DOI] [PubMed] [Google Scholar]
- 40.Paek J.H., Kang S.S., Park W.Y., Jin K., Park S.B., Han S., Kim C.-D., Ro H., Lee S., Jung C.W. Incidence of Post-transplantation Diabetes Mellitus Within 1 Year After Kidney Transplantation and Related Factors in Korean Cohort Study. Transplant. Proc. 2019;51:2714–2717. doi: 10.1016/j.transproceed.2019.02.054. [DOI] [PubMed] [Google Scholar]
- 41.Kim H.L., Kim M.A., Park K.T., Choi D.J., Han S., Jeon E.S., Cho M.-C., Kim J.-J., Yoo B.-S., Shin M.-S., et al. Gender difference in the impact of coexisting diabetes mellitus on long-term clinical outcome in people with heart failure: A report from the Korean Heart Failure Registry. Diabet. Med. 2019;36:1312–1318. doi: 10.1111/dme.14059. [DOI] [PubMed] [Google Scholar]
- 42.Moon J., Lee C.J., Lee S.H., Kang S.M., Choi D., Yoo T.H., Park S. The Impact of Diabetes Mellitus on Vascular Biomarkers in Patients with End-Stage Renal Disease. Yonsei. Med. J. 2017;58:75–81. doi: 10.3349/ymj.2017.58.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vinik A.I., Nevoret M.L., Casellini C., Parson H. Diabetic neuropathy. Endocrinol. Metab. Clin. 2013;42:747–787. doi: 10.1016/j.ecl.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 44.Moon E., Lee S.O., Kang T.H., Kim H.J., Choi S.Z., Son M.W., Kim S.Y. Dioscorea Extract (DA-9801) Modulates Markers of Peripheral Neuropathy in Type 2 Diabetic db/db Mice. Biomol. Ther. 2014;22:445–452. doi: 10.4062/biomolther.2014.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Petrofsky J., Laymon M., Lee H. The influence of ageing and diabetic peripheral neuropathy on posture sway, tremor, and the time to achieve balance equilibrium. J. Sports. Med. Phys. Fit. 2019;59:1011–1017. doi: 10.23736/S0022-4707.18.08653-X. [DOI] [PubMed] [Google Scholar]
- 46.Zakin E., Abrams R., Simpson D.M. Diabetic Neuropathy. Semin. Neurol. 2019;39:560–569. doi: 10.1055/s-0039-1688978. [DOI] [PubMed] [Google Scholar]
- 47.Won J.C., Kwon H.S., Moon S.S., Chun S.W., Kim C.H., Park I.B., Kim I.J., Lee J., Cha B.Y., Park T.S. Gamma-Linolenic Acid versus alpha-Lipoic Acid for Treating Painful Diabetic Neuropathy in Adults: A 12-Week, Double-Placebo, Randomized, Noninferiority Trial. Diabetes. Metab. J. 2020;44:542–554. doi: 10.4093/dmj.2019.0099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Feldman E.L., Callaghan B.C., Pop-Busui R., Zochodne D.W., Wright D.E., Bennett D.L., Bril V., Russell J.W., Viswanathan V. Diabetic neuropathy. Nat. Rev. Dis. Primers. 2019;5:1–18. doi: 10.1038/s41572-019-0092-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Singh D.D., Verma R., Parimoo P., Sahu A., Kumar V., Upadhyay E., Yadav D.K. Potential Therapeutic Relevance of CRISPR/Cas9 Guided Epigenetic Regulations for Neuropsychiatric Disorders. Curr. Top. Med. Chem. 2021;21:878–894. doi: 10.2174/1568026621666210317154502. [DOI] [PubMed] [Google Scholar]
- 50.Coussens L.M., Werb Z. Inflammation and cancer. Nature. 2002;420:860–867. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kaser A., Zeissig S., Blumberg R.S. Endoplasmic reticulum stress: Implications for inflammatory bowel disease pathogenesis. Inflamm. Bowel Dis. Annu. Rev. Immunol. 2010;28:573–621. doi: 10.1146/annurev-immunol-030409-101225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lee Y.-J., Han S.B., Nam S.-Y., Oh K.-W., Hong J.T. Inflammation and Alzheimer’s disease. Arch. Pharm. Res. 2010;33:1539–1556. doi: 10.1007/s12272-010-1006-7. [DOI] [PubMed] [Google Scholar]
- 53.O’Shea J.J., Ma A., Lipsky P. Cytokines and autoimmunity. Nat. Rev. Immunol. 2002;2:37–45. doi: 10.1038/nri702. [DOI] [PubMed] [Google Scholar]
- 54.Sica A., Dorman L., Viggiano V., Cippitelli M., Ghosh P., Rice N., Young H.A. Interaction of NF-κB and NFAT with the interferon-γ promoter. J. Biol. Chem. 1997;272:30412–30420. doi: 10.1074/jbc.272.48.30412. [DOI] [PubMed] [Google Scholar]
- 55.Falvo J.V., Uglialoro A.M., Brinkman B.M.N., Merika M., Parekh B.S., Tsai E.Y., King H.C., Morielli A.D., Peralta E.G., Maniatis T., et al. Stimulus-specific assembly of enhancer complexes on the tumor necrosis factor alpha gene promoter. Mol. Cell. Biol. 2000;20:2239–2247. doi: 10.1128/MCB.20.6.2239-2247.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gautam R., Jachak S.M. Recent developments in anti-inflammatory natural products. Med. Res. Rev. 2009;29:767–820. doi: 10.1002/med.20156. [DOI] [PubMed] [Google Scholar]
- 57.Xu H.L., Wang X.T., Cheng Y., Zhao J.G., Zhou Y.J., Yang J.J., Qi M.Y. Ursolic acid improves diabetic nephropathy via suppression of oxidative stress and inflammation in streptozotocin-induced rats. Biomed. Pharmacother. 2018;105:915–921. doi: 10.1016/j.biopha.2018.06.055. [DOI] [PubMed] [Google Scholar]
- 58.Pironi A.M., de Araújo P.R., Fernandes M.A., Salgado H.R.N., Chorilli M. Characteristics, biological properties and analytical methods of ursolic acid: A review. Crit. Rev. Anal. Chem. 2018;48:86–93. doi: 10.1080/10408347.2017.1390425. [DOI] [PubMed] [Google Scholar]
- 59.Kashyap D., Tuli H.S., Sharma A.K. Ursolic acid (UA): A metabolite with promising therapeutic potential. Life Sci. 2016;146:201–213. doi: 10.1016/j.lfs.2016.01.017. [DOI] [PubMed] [Google Scholar]
- 60.Liby K.T., Yore M.M., Sporn M.B. Triterpenoids and rexinoids as multifunctional agents for the prevention and treatment of cancer. Nat. Rev. Cancer. 2007;7:357–369. doi: 10.1038/nrc2129. [DOI] [PubMed] [Google Scholar]
- 61.Szakiel A., Pączkowski C., Pensec F., Bertsch C. Fruit cuticular waxes as a source of biologically active triterpenoids. Phytochem. Rev. 2012;11:263–284. doi: 10.1007/s11101-012-9241-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kim C.S., Subedi L., Kim S.Y., Choi S.U., Kim K.H., Lee K.R. Diterpenes from the Trunk of Abies holophylla and Their Potential Neuroprotective and Anti-inflammatory Activities. J. Nat. Prod. 2016;79:387–394. doi: 10.1021/acs.jnatprod.5b01053. [DOI] [PubMed] [Google Scholar]
- 63.Chen H., Gao Y., Wang A., Zhou X., Zheng Y., Zhou J. Evolution in medicinal chemistry of ursolic acid derivatives as anticancer agents. Eur. J. Med. Chem. 2015;92:648–655. doi: 10.1016/j.ejmech.2015.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Shao J.-W., Dai Y.-C., Xue J.-P., Wang J.-C., Lin F.-P., Guo Y.-H. In vitro and in vivo anticancer activity evaluation of ursolic acid derivatives. Eur. J. Med. Chem. 2011;46:2652–2661. doi: 10.1016/j.ejmech.2011.03.050. [DOI] [PubMed] [Google Scholar]
- 65.Liu J. Oleanolic acid and ursolic acid: Research perspectives. J. Ethnopharmacol. 2005;100:92–94. doi: 10.1016/j.jep.2005.05.024. [DOI] [PubMed] [Google Scholar]
- 66.Leal A.S., Wang R., Salvador J.A.R., Jing Y. Synthesis of novel ursolic acid heterocyclic derivatives with improved abilities of antiproliferation and induction of p53, p21waf1 and NOXA in pancreatic cancer cells. Bioorganic Med. Chem. 2012;20:5774–5786. doi: 10.1016/j.bmc.2012.08.010. [DOI] [PubMed] [Google Scholar]
- 67.Dar B.A., Lone A.M., Shah W.A., Qurishi M.A. Synthesis and screening of ursolic acid-benzylidine derivatives as potential anti-cancer agents. Eur. J. Med. Chem. 2016;111:26–32. doi: 10.1016/j.ejmech.2016.01.026. [DOI] [PubMed] [Google Scholar]
- 68.Shanmugam M.K., Ong T.H., Kumar A.P., Lun C.K., Ho P.C., Wong P.T.H., Hui K.M., Sethi G. Ursolic acid inhibits the initiation, progression of prostate cancer and prolongs the survival of TRAMP mice by modulating pro-inflammatory pathways. PLoS ONE. 2012;7:e32476. doi: 10.1371/journal.pone.0032476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chen Q., Luo S., Zhang Y., Chen Z. Development of a liquid chromatography—Mass spectrometry method for the determination of ursolic acid in rat plasma and tissue: Application to the pharmacokinetic and tissue distribution study. Anal. Bioanal. Chem. 2011;399:2877–2884. doi: 10.1007/s00216-011-4651-x. [DOI] [PubMed] [Google Scholar]
- 70.Sahni R., Parcha V., Dobhal Y., Maithani A. Isolation, characterization of ursolic acid and its synthetic modification as new neuro-protective agent for prevention of cognition defects and oxidative damage. Pharm. Biol. Eval. 2016;3:126–134. [Google Scholar]
- 71.Gupta A., Maheta P., Chauhan R., Pandey S., Yadav J.S., Shah S. Simultaneous quantification of bioactive triterpene acids (ursolic acid and oleanolic acid) in different extracts of eucalyptus globulus (L.) by HPTLC method. Pharmacogn. J. 2018;10:179–185. doi: 10.5530/pj.2018.1.30. [DOI] [Google Scholar]
- 72.Yamaguchi H., Noshita T., Kidachi Y., Umetsu H., Hayashi M., Komiyama K., Funayama S., Ryoyama K. Isolation of ursolic acid from apple peels and its specific efficacy as a potent antitumor agent. J. Health Sci. 2008;54:654–660. doi: 10.1248/jhs.54.654. [DOI] [Google Scholar]
- 73.Abu-Gharbieh E., Shehab N.G., Almasri I.M., Bustanji Y. Antihyperuricemic and xanthine oxidase inhibitory activities of Tribulus arabicus and its isolated compound, ursolic acid: In vitro and in vivo investigation and docking simulations. PLoS ONE. 2018;13:e0202572. doi: 10.1371/journal.pone.0202572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Somova L.O., Nadar A., Rammanan P., Shode F.O. Cardiovascular, antihyperlipidemic and antioxidant effects of oleanolic and ursolic acids in experimental hypertension. Phytomedicine. 2003;10:115–121. doi: 10.1078/094471103321659807. [DOI] [PubMed] [Google Scholar]
- 75.Figueroa-Suárez M.Z., Christen J.G., Cardoso-Taketa A.T., Villafuerte M.D.C.G., Rodríguez-López V. Anti-inflammatory and antihistaminic activity of triterpenoids isolated from Bursera cuneata (Schldl.) Engl. J. Ethnopharmacol. 2019;238:111786. doi: 10.1016/j.jep.2019.03.013. [DOI] [PubMed] [Google Scholar]
- 76.Do Nascimento P.G.G., Lemos T.L.G., Bizerra A., Arriaga Ã.N., Ferreira D.A., Santiago G.M.P., Braz-Filhoand R., Costa J.G.M. Antibacterial and antioxidant activities of ursolic acid and derivatives. Molecules. 2014;19:1317–1327. doi: 10.3390/molecules19011317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ghareeb D.A., ElAhwany A.M., El-Mallawany S.M., Saif A.A. In vitro screening for anti-acetylcholiesterase, anti-oxidant, anti-glucosidase, anti-inflammatory and anti-bacterial effect of three traditional medicinal plants. Biotechnol. Biotechnol. Equip. 2014;28:1155–1164. doi: 10.1080/13102818.2014.969877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Basir D., Julinar J., Agustriana E., Untari B. Oxidation and Acetylation of Ursolic and Oleanolic Acids Isolated from Fragraea fragrans fruits; Antiproliferation of P388 Leukemia Cells. Indones. J. Chem. 2014;14:269–276. doi: 10.22146/ijc.21238. [DOI] [Google Scholar]
- 79.Mazumder K., Tanaka K., Fukase K. Cytotoxic activity of ursolic acid derivatives obtained by isolation and oxidative derivatization. Molecules. 2013;18:8929–8944. doi: 10.3390/molecules18088929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Batra A., Sastry V.G. Extraction of ursolic acid from Ocimum sanctum and synthesis of its novel derivatives: Effects on extracellular homocysteine, dihydrofolate reductase activity and proliferation of HepG2 human hepatoma cells. Pteridines. 2013;24:191–199. doi: 10.1515/pterid-2013-0023. [DOI] [Google Scholar]
- 81.Mendes V.I.S., Bartholomeusz G.A., Ayres M., Gandhi V., Salvador J.A.R. Synthesis and cytotoxic activity of novel A-ring cleaved ursolic acid derivatives in human non-small cell lung cancer cells. Eur. J. Med. Chem. 2016;123:317–331. doi: 10.1016/j.ejmech.2016.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wu P.-P., Zhang B.-J., Cui X.-P., Yang Y., Jiang Z.-Y., Zhou Z.-H., Zhong Y.-Y., Mai Y.-Y., Ouyang Z., Chen H.-S., et al. Synthesis and biological evaluation of novel ursolic acid analogues as potential α-glucosidase inhibitors. Sci. Rep. 2017;7:1–12. doi: 10.1038/srep45578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Stiti N.M., Hartmann M.-A.E. Nonsterol triterpenoids as major constituents of Olea europaea. J. Lipids. 2012;2012:476595. doi: 10.1155/2012/476595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Jung S.H., Ha Y.J., Shim E.K., Choi S.Y., Jin J.L., Yun-Choi H.S., Lee J.R. Insulin-mimetic and insulin-sensitizing activities of a pentacyclic triterpenoid insulin receptor activator. Biochem. J. 2007;403:243–250. doi: 10.1042/BJ20061123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Jang S.-M., Yee S.-T., Choi J., Choi M.-S., Do G.-M., Jeon S.-M., Yeo J., Kim M.-J., Seo K.-I., Lee M.-K. Ursolic acid enhances the cellular immune system and pancreatic β-cell function in streptozotocin-induced diabetic mice fed a high-fat diet. Int. Immunopharmacol. 2009;9:113–119. doi: 10.1016/j.intimp.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 86.Subedi L., Lee J.H., Gaire B.P., Kim S.Y. Sulforaphane Inhibits MGO-AGE-Mediated Neuroinflammation by Suppressing NF-κB, MAPK, and AGE-RAGE Signaling Pathways in Microglial Cells. Antioxidants. 2020;9:792. doi: 10.3390/antiox9090792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ramírez-Rodríguez A.M., González-Ortiz M., Martínez-Abundis E., Acuña Ortega N. Effect of ursolic acid on metabolic syndrome, insulin sensitivity, and inflammation. J. Med. Food. 2017;20:882–886. doi: 10.1089/jmf.2017.0003. [DOI] [PubMed] [Google Scholar]
- 88.Zhang T., Su J., Wang K., Zhu T., Li X. Ursolic acid reduces oxidative stress to alleviate early brain injury following experimental subarachnoid hemorrhage. Neurosci. Lett. 2014;579:12–17. doi: 10.1016/j.neulet.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 89.Rai S.N., Yadav S.K., Singh D., Singh S.P. Ursolic acid attenuates oxidative stress in nigrostriatal tissue and improves neurobehavioral activity in MPTP-induced Parkinsonian mouse model. J. Chem. Neuroanat. 2016;71:41–49. doi: 10.1016/j.jchemneu.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 90.Lee T.H., Khan Z., Subedi L., Kim S.Y., Lee K.R. New bis-thioglycosyl-1,1’-disulfides from Nasturtium officinale R. Br. and their anti-neuroinflammatory effect. Bioorg. Chem. 2019;86:501–506. doi: 10.1016/j.bioorg.2019.01.062. [DOI] [PubMed] [Google Scholar]
- 91.Huang H.C., Huang C.Y., Lin-Shiau S.Y., Lin J.K. Ursolic acid inhibits IL-1β or TNF-α-induced C6 glioma invasion through suppressing the association ZIP/p62 with PKC-ζ and downregulating the MMP-9 expression. Mol. Carcinog. Publ. Coop. Univ. Tex. MD Anderson Cancer Cent. 2009;48:517–531. doi: 10.1002/mc.20490. [DOI] [PubMed] [Google Scholar]
- 92.Lu J., Wu D.-M., Zheng Y.-L., Hu B., Zhang Z.-F., Ye Q., Liu C.-M., Shan Q., Wang Y.-J. Ursolic acid attenuates D-galactose-induced inflammatory response in mouse prefrontal cortex through inhibiting AGEs/RAGE/NF-κB pathway activation. Cereb. Cortex. 2010;20:2540–2548. doi: 10.1093/cercor/bhq002. [DOI] [PubMed] [Google Scholar]
- 93.Wu D.-M., Lu J., Zhang Y.-Q., Zheng Y.-L., Hu B., Cheng W., Zhang Z.-F., Li M.-Q. Ursolic acid improves domoic acid-induced cognitive deficits in mice. Toxicol. Appl. Pharmacol. 2013;271:127–136. doi: 10.1016/j.taap.2013.04.038. [DOI] [PubMed] [Google Scholar]
- 94.Gong Y.Y., Liu Y.Y., Yu S., Zhu X.N., Cao X.P., Xiao H.P. Ursolic acid suppresses growth and adrenocorticotrophic hormone secretion in AtT20 cells as a potential agent targeting adrenocorticotrophic hormone-producing pituitary adenoma. Mol. Med. Rep. 2014;9:2533–2539. doi: 10.3892/mmr.2014.2078. [DOI] [PubMed] [Google Scholar]
- 95.Tian T., Liu X., Lee E.S., Sun J., Feng Z., Zhao L., Zhao C. Synthesis of novel oleanolic acid and ursolic acid in C-28 position derivatives as potential anti-cancer agents. Arch. Pharmacal Res. 2017;40:458–468. doi: 10.1007/s12272-016-0868-8. [DOI] [PubMed] [Google Scholar]
- 96.Jiménez-Arellanes A., Luna-Herrera J., Cornejo-Garrido J., López-García S., Castro-Mussot M.E., Meckes-Fischer M., Mata-Espinosa D., Marquina B., Torres J., Hernández-Pando R. Ursolic and oleanolic acids as antimicrobial and immunomodulatory compounds for tuberculosis treatment. BMC Complementary Altern. Med. 2013;13:1–11. doi: 10.1186/1472-6882-13-258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ali S., Ehtram A., Arora N., Manjunath P., Roy D., Ehtesham N.Z., Hasnain S.E. The M. tuberculosis Rv1523 Methyltransferase Promotes Drug Resistance Through Methylation-Mediated Cell Wall Remodeling and Modulates Macrophages Immune Responses. Front. Cell Infect. Microbiol. 2021;11:622487. doi: 10.3389/fcimb.2021.622487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kataev V.E., Khaybullin R.N., Garifullin B.F., Sharipova R.R. New Targets for Growth Inhibition of Mycobacterium tuberculosis: Why Do Natural Terpenoids Exhibit Antitubercular Activity? Russ. J. Bioorganic Chem. 2018;44:438–452. doi: 10.1134/S1068162018040106. [DOI] [Google Scholar]
- 99.Subedi L., Gaire B.P., Do M.H., Lee T.H., Kim S.Y. Anti-neuroinflammatory and neuroprotective effects of the Lindera neesiana fruit in vitro. Phytomedicine. 2016;23:872–881. doi: 10.1016/j.phymed.2016.05.002. [DOI] [PubMed] [Google Scholar]
- 100.Jc Furtado N.A., Pirson L., Edelberg H., Miranda L.M., Loira-Pastoriza C., Preat V., Larondelle Y., André C.M. Pentacyclic triterpene bioavailability: An overview of in vitro and in vivo studies. Molecules. 2017;22:400. doi: 10.3390/molecules22030400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Tong H.H.Y., Du Z., Wang G.N., Chan H.M., Chang Q., Lai L.C.M., Chow A.H.L., Zheng Y. Spray freeze drying with polyvinylpyrrolidone and sodium caprate for improved dissolution and oral bioavailability of oleanolic acid, a BCS Class IV compound. Int. J. Pharm. 2011;404:148–158. doi: 10.1016/j.ijpharm.2010.11.027. [DOI] [PubMed] [Google Scholar]
- 102.Gao S., Basu S., Yang Z., Deb A., Hu M. Bioavailability challenges associated with development of saponins as therapeutic and chemopreventive agents. Curr. Drug Targets. 2012;13:1885–1899. doi: 10.2174/138945012804545498. [DOI] [PubMed] [Google Scholar]
- 103.Kalani K., Yadav D.K., Khan F., Srivastava S.K., Suri N. Pharmacophore, QSAR, and ADME based semisynthesis and in vitro evaluation of ursolic acid analogs for anticancer activity. J. Mol. Modeling. 2012;18:3389–3413. doi: 10.1007/s00894-011-1327-6. [DOI] [PubMed] [Google Scholar]
- 104.Song J., Wang Y., Song Y., Chan H., Bi C., Yang X., Yan R., Wang Y., Zheng Y. Development and characterisation of ursolic acid nanocrystals without stabiliser having improved dissolution rate and in vitro anticancer activity. AAPS PharmSciTech. 2014;15:11–19. doi: 10.1208/s12249-013-0028-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Yang L., Sun Z., Zu Y., Zhao C., Sun X., Zhang Z., Zhang L. Physicochemical properties and oral bioavailability of ursolic acid nanoparticles using supercritical anti-solvent (SAS) process. Food Chem. 2012;132:319–325. doi: 10.1016/j.foodchem.2011.10.083. [DOI] [PubMed] [Google Scholar]
- 106.Qiang Z., Ye Z., Hauck C., Murphy P.A., McCoy J.-A., Widrlechner M.P., Reddy M.B., Hendrich S. Permeability of rosmarinic acid in Prunella vulgaris and ursolic acid in Salvia officinalis extracts across Caco-2 cell monolayers. J. Ethnopharmacol. 2011;137:1107–1112. doi: 10.1016/j.jep.2011.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Jinhua W., Ying Z., Yuhua L. PXR-ABC drug transporters/CYP-mediated ursolic acid transport and metabolism in vitro and vivo. Arch. Pharm. 2020;353:2000082. doi: 10.1002/ardp.202000082. [DOI] [PubMed] [Google Scholar]
- 108.Yin M.-C., Lin M.-C., Mong M.-C., Lin C.-Y. Bioavailability, distribution, and antioxidative effects of selected triterpenes in mice. J. Agric. Food Chem. 2012;60:7697–7701. doi: 10.1021/jf302529x. [DOI] [PubMed] [Google Scholar]
- 109.Wang X.-H., Zhou S.-Y., Qian Z.-Z., Zhang H.-L., Qiu L.-H., Song Z., Zhao J., Wang P., Hao X.-S., Wang H.-Q. Evaluation of toxicity and single-dose pharmacokinetics of intravenous ursolic acid liposomes in healthy adult volunteers and patients with advanced solid tumors. Expert Opin. Drug Metab. Toxicol. 2013;9:117–125. doi: 10.1517/17425255.2013.738667. [DOI] [PubMed] [Google Scholar]
- 110.Khan K., Aqil M., Imam S.S., Ahad A., Moolakkadath T., Sultana Y., Mujeeb M. Ursolic acid loaded intra nasal nano lipid vesicles for brain tumour: Formulation, optimization, in-vivo brain/plasma distribution study and histopathological assessment. Biomed. Pharmacother. 2018;106:1578–1585. doi: 10.1016/j.biopha.2018.07.127. [DOI] [PubMed] [Google Scholar]
- 111.Zhou X.J., Hu X.M., Yi Y.M., Wan J. Preparation and body distribution of freeze-dried powder of ursolic acid phospholipid nanoparticles. Drug Dev. Ind. Pharm. 2009;35:305–310. doi: 10.1080/03639040802302165. [DOI] [PubMed] [Google Scholar]
- 112.Khusnutdinova E.M.F., Smirnova I.E., Giniyatullina G.N.V., Medvedeva N.Y.I., Yamansarov E.Y., Kazakov D.V., Kazakova O.B., Linh P.T., Viet D.Q., Huong D.T. Inhibition of alpha-glucosidase by synthetic derivatives of lupane, oleanane, ursane and dammarane triterpenoids. Nat. Prod. Commun. 2016;11:1934578X1601100112. doi: 10.1177/1934578X1601100112. [DOI] [PubMed] [Google Scholar]
- 113.Li S., Meng F., Liao X., Wang Y., Sun Z., Guo F., Li X., Meng M., Li Y., Sun C. Therapeutic role of ursolic acid on ameliorating hepatic steatosis and improving metabolic disorders in high-fat diet-induced non-alcoholic fatty liver disease rats. PLoS ONE. 2014;9:e86724. doi: 10.1371/journal.pone.0086724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Chu X., He X., Shi Z., Li C., Guo F., Li S., Li Y., Na L., Sun C. Ursolic acid increases energy expenditure through enhancing free fatty acid uptake and β-oxidation via an UCP3/AMPK-dependent pathway in skeletal muscle. Mol. Nutr. Food Res. 2015;59:1491–1503. doi: 10.1002/mnfr.201400670. [DOI] [PubMed] [Google Scholar]
- 115.Kunkel S.D., Elmore C.J., Bongers K.S., Ebert S.M., Fox D.K., Dyle M.C., Bullard S.A., Adams C.M. Ursolic acid increases skeletal muscle and brown fat and decreases diet-induced obesity, glucose intolerance and fatty liver disease. PLoS ONE. 2012;7:e39332. doi: 10.1371/journal.pone.0039332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Jia Y., Bhuiyan M.J.H., Jun H.-J., Lee J.H., Hoang M.H., Lee H.-J., Kim N., Lee D., Hwang K.Y., Hwang B.Y., et al. Ursolic acid is a PPAR-α agonist that regulates hepatic lipid metabolism. Bioorganic Med. Chem. Lett. 2011;21:5876–5880. doi: 10.1016/j.bmcl.2011.07.095. [DOI] [PubMed] [Google Scholar]
- 117.Jia Y., Kim S., Kim J., Kim B., Wu C., Lee J.H., Jun H., Kim N., Lee D., Lee S.-J. Ursolic acid improves lipid and glucose metabolism in high-fat-fed C57BL/6J mice by activating peroxisome proliferator-activated receptor alpha and hepatic autophagy. Mol. Nutr. Food Res. 2015;59:344–354. doi: 10.1002/mnfr.201400399. [DOI] [PubMed] [Google Scholar]
- 118.Lo S.-H., Li Y., Cheng K.C., Niu C.-S., Cheng J.-T., Niu H.-S. Ursolic acid activates the TGR5 receptor to enhance GLP-1 secretion in type 1-like diabetic rats. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2017;390:1097–1104. doi: 10.1007/s00210-017-1409-9. [DOI] [PubMed] [Google Scholar]
- 119.Loh K., Deng H., Fukushima A., Cai X., Boivin B., Galic S., Bruce C., Shields B.J., Skiba B., Ooms L.S., et al. Reactive oxygen species enhance insulin sensitivity. Cell. Metab. 2009;10:260–272. doi: 10.1016/j.cmet.2009.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Watanabe M., Houten S.M., Mataki C., Christoffolete M.A., Kim B.W., Sato H., Messaddeq N., Harney J.W., Ezaki O., Kodama T., et al. Bile acids induce energy expenditure by promoting intracellular thyroid hormone activation. Nature. 2006;439:484–489. doi: 10.1038/nature04330. [DOI] [PubMed] [Google Scholar]
- 121.Chang K.A., Lee J.H., Suh Y.H. Therapeutic potential of human adipose-derived stem cells in neurological disorders. J. Pharmacol. Sci. 2014;126:293–301. doi: 10.1254/jphs.14R10CP. [DOI] [PubMed] [Google Scholar]
- 122.Choi J.G., Kim S.Y., Jeong M., Oh M.S. Pharmacotherapeutic potential of ginger and its compounds in age-related neurological disorders. Pharmacol. Ther. 2018;182:56–69. doi: 10.1016/j.pharmthera.2017.08.010. [DOI] [PubMed] [Google Scholar]
- 123.Lee K., Jo Y.Y., Chung G., Jung J.H., Kim Y.H., Park C.K. Functional Importance of Transient Receptor Potential (TRP) Channels in Neurological Disorders. Front. Cell. Dev. Biol. 2021;9:611773. doi: 10.3389/fcell.2021.611773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Suh Y.H., Suh W.H. Editorial (Thematic Issue: Molecular and Cellular Engineering Approaches for Neurological Disorders, Diseases, and Injuries Involved the Central and Peripheral Nervous Systems) CNS Neurol. Disord. Drug. Targets. 2016;15:878–880. doi: 10.2174/187152731508160909174157. [DOI] [PubMed] [Google Scholar]
- 125.Zhuang Z., Zhou M.-L., You W.-C., Zhu L., Ma C.-Y., Sun X.-J., Xin J.-X. Hydrogen-rich saline alleviates early brain injury via reducing oxidative stress and brain edema following experimental subarachnoid hemorrhage in rabbits. BMC Neurosci. 2012;13:1–10. doi: 10.1186/1471-2202-13-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Li L., Zhang X., Cui L., Wang L., Liu H., Ji H., Du Y. Ursolic acid promotes the neuroprotection by activating Nrf2 pathway after cerebral ischemia in mice. Brain. Res. 2013;1497:32–39. doi: 10.1016/j.brainres.2012.12.032. [DOI] [PubMed] [Google Scholar]
- 127.Park K.H., Sun S., Lim Y.H., Park H.R., Lee J.M., Park K., Jeon B., Park H.-P., Kim H.C., Paek S.H. Clinical outcome prediction from analysis of microelectrode recordings using deep learning in subthalamic deep brain stimulation for Parkinson‘s disease. PLoS ONE. 2021;16:e0244133. doi: 10.1371/journal.pone.0244133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Kwon O.C., Song J.J., Yang Y., Kim S.H., Kim J.Y., Seok M.J., Hwang I., Yu J.-W., Karmacharya J., Maeng H.-J., et al. SGK1 inhibition in glia ameliorates pathologies and symptoms in Parkinson disease animal models. EMBO Mol. Med. 2021;13:e13076. doi: 10.15252/emmm.202013076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Lee J.M., Kim T.W., Park S.S., Han J.H., Shin M.S., Lim B.V., Kim S.-H., Baek S.-S., Cho Y.S., Kim K.H. Treadmill Exercise Improves Motor Function by Suppressing Purkinje Cell Loss in Parkinson Disease Rats. Int. Neurourol. J. 2018;22:S147–S155. doi: 10.5213/inj.1836226.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Cho Z.H., Min H.K., Oh S.H., Han J.Y., Park C.W., Chi J.G., Kim Y.-B., Paek S.H., Lozano A.M., Lee K.H. Direct visualization of deep brain stimulation targets in Parkinson disease with the use of 7-tesla magnetic resonance imaging. J. Neurosurg. 2010;113:639–647. doi: 10.3171/2010.3.JNS091385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.DeMaagd G., Philip A. Parkinson’s disease and its management: Part 1: Disease entity, risk factors, pathophysiology, clinical presentation, and diagnosis. Pharm. Ther. 2014;40:504. [PMC free article] [PubMed] [Google Scholar]
- 132.Huang Y., Nikolic D., Pendland S., Doyle B.J., Locklear T.D., Mahady G.B. Effects of cranberry extracts and ursolic acid derivatives on P-fimbriated Escherichia coli, COX-2 activity, pro-inflammatory cytokine release and the NF-κβ transcriptional response in vitro. Pharm. Biol. 2009;47:18–25. doi: 10.1080/13880200802397996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Maiti P., Manna J., Dunbar G.L. Current understanding of the molecular mechanisms in Parkinson’s disease: Targets for potential treatments. Transl. Neurodegener. 2017;6:28. doi: 10.1186/s40035-017-0099-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Baek J., Lee M.G. Oxidative stress and antioxidant strategies in dermatology. Redox. Rep. 2016;21:164–169. doi: 10.1179/1351000215Y.0000000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Cha S.H., Hwang Y., Heo S.J., Jun H.S. Diphlorethohydroxycarmalol Attenuates Methylglyoxal-Induced Oxidative Stress and Advanced Glycation End Product Formation in Human Kidney Cells. Oxid. Med. Cell. Longev. 2018;2018:3654095. doi: 10.1155/2018/3654095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Kang I.G., Jung J.H., Kim S.T. The effect of obstructive sleep apnea on DNA damage and oxidative stress. Clin. Exp. Otorhinolaryngol. 2013;6:68–72. doi: 10.3342/ceo.2013.6.2.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Kim M.H., Kim E.H., Jung H.S., Yang D., Park E.Y., Jun H.S. EX4 stabilizes and activates Nrf2 via PKCdelta, contributing to the prevention of oxidative stress-induced pancreatic beta cell damage. Toxicol. Appl. Pharmacol. 2017;315:60–69. doi: 10.1016/j.taap.2016.12.005. [DOI] [PubMed] [Google Scholar]
- 138.Kim Y.J., Kim E.H., Hahm K.B. Oxidative stress in inflammation-based gastrointestinal tract diseases: Challenges and opportunities. J. Gastroenterol. Hepatol. 2012;27:1004–1010. doi: 10.1111/j.1440-1746.2012.07108.x. [DOI] [PubMed] [Google Scholar]
- 139.Nanda S.S., An S.S., Yi D.K. Oxidative stress and antibacterial properties of a graphene oxide-cystamine nanohybrid. Int. J. Nanomed. 2015;10:549–556. doi: 10.2147/IJN.S75768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Oh Y.S., Jun H.S. Effects of Glucagon-Like Peptide-1 on Oxidative Stress and Nrf2 Signaling. Int. J. Mol. Sci. 2017;19:26. doi: 10.3390/ijms19010026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Bondy S.C., LeBel C.P. The relationship between excitotoxicity and oxidative stress in the central nervous system. Free. Radic. Biol. Med. 1993;14:633–642. doi: 10.1016/0891-5849(93)90144-J. [DOI] [PubMed] [Google Scholar]
- 142.Hassan M.I., Naiyer A., Ahmad F. Fragile histidine triad protein: Structure, function, and its association with tumorogenesis. J. Cancer Res. Clin. Oncol. 2010;136:333–350. doi: 10.1007/s00432-009-0751-9. [DOI] [PubMed] [Google Scholar]
- 143.Hassan M.I., Aijaz A., Ahmad F. Structural and functional analysis of human prostatic acid phosphatase. Expert Rev. Anticancer. Ther. 2010;10:1055–1068. doi: 10.1586/era.10.46. [DOI] [PubMed] [Google Scholar]
- 144.Shih Y.-H., Chein Y.-C., Wang J.-Y., Fu Y.-S. Ursolic acid protects hippocampal neurons against kainate-induced excitotoxicity in rats. Neurosci. Lett. 2004;362:136–140. doi: 10.1016/j.neulet.2004.03.011. [DOI] [PubMed] [Google Scholar]
- 145.Lu J., Zheng Y.-L., Wu D.-M., Luo L., Sun D.-X., Shan Q. Ursolic acid ameliorates cognition deficits and attenuates oxidative damage in the brain of senescent mice induced by D-galactose. Biochem. Pharmacol. 2007;74:1078–1090. doi: 10.1016/j.bcp.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 146.Wang Y.-J., Lu J., Wu D.-M., Zheng Z.-H., Zheng Y.-L., Wang X.-H., Ruan J., Sun X., Shan Q., Zhang Z.-F. Ursolic acid attenuates lipopolysaccharide-induced cognitive deficits in mouse brain through suppressing p38/NF-κB mediated inflammatory pathways. Neurobiol. Learn. Mem. 2011;96:156–165. doi: 10.1016/j.nlm.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 147.Lu J., Wu D.-M., Zheng Y.-L., Hu B., Cheng W., Zhang Z.-F., Shan Q. Ursolic acid improves high fat diet-induced cognitive impairments by blocking endoplasmic reticulum stress and IκB kinase β/nuclear factor-κB-mediated inflammatory pathways in mice. Brain. Behavior. Immun. 2011;25:1658–1667. doi: 10.1016/j.bbi.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 148.Turab Naqvi A.A., Hasan G.M., Hassan M.I. Targeting Tau Hyperphosphorylation via Kinase Inhibition: Strategy to Address Alzheimer’s Disease. Curr. Top. Med. Chem. 2020;20:1059–1073. doi: 10.2174/1568026620666200106125910. [DOI] [PubMed] [Google Scholar]
- 149.De Iuliis A., Grigoletto J., Recchia A., Giusti P., Arslan P. A proteomic approach in the study of an animal model of Parkinson’s disease. Clin. Chim. Acta. 2005;357:202–209. doi: 10.1016/j.cccn.2005.03.028. [DOI] [PubMed] [Google Scholar]
- 150.Rana R., Joon S., Chauhan K., Rathi V., Ganguly N.K., Kumari C., Kumar Y.D. Role of Extracellular Vesicles in Glioma Progression: Deciphering Cellular Biological Processes to Clinical Applications. Curr. Top. Med. Chem. 2021;21:696–704. doi: 10.2174/1568026620666201207100139. [DOI] [PubMed] [Google Scholar]
- 151.Rao J.S., Steck P.A., Mohanam S., Stetler-Stevenson W.G., Liotta L.A., Sawaya R. Elevated levels of Mr 92,000 type IV collagenase in human brain tumors. Cancer Res. 1993;53:2208–2211. [PubMed] [Google Scholar]
- 152.Wu D., Lee Y.-C.G., Liu H.-C., Yuan R.-Y., Chiou H.-Y., Hung C.-H., Hu C.-J. Identification of TLR downstream pathways in stroke patients. Clin. Biochem. 2013;46:1058–1064. doi: 10.1016/j.clinbiochem.2013.05.059. [DOI] [PubMed] [Google Scholar]
- 153.Guan J., Wei X., Qin S., Liu X., Jiang Y., Chen Y.X., Chen Y.F., Lu H., Qian J., Wang Z., et al. Continuous tracking of COVID-19 patients’ immune status. Int. Immunopharmacol. 2020;89:107034. doi: 10.1016/j.intimp.2020.107034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Alam M., Hasan G.M., Hassan M.I. A review on the role of TANK-binding kinase 1 signaling in cancer. Int. J. Biol. Macromol. 2021;183:2364–2375. doi: 10.1016/j.ijbiomac.2021.06.022. [DOI] [PubMed] [Google Scholar]
- 155.De Bock M., Thorstensen E.B., Derraik J.G., Henderson H.V., Hofman P.L., Cutfield W.S. Human absorption and metabolism of oleuropein and hydroxytyrosol ingested as olive (O lea europaea L.) leaf extract. Mol. Nutr. Food Res. 2013;57:2079–2085. doi: 10.1002/mnfr.201200795. [DOI] [PubMed] [Google Scholar]
- 156.Wang Y., Li L., Deng S., Liu F., He Z. Ursolic acid ameliorates inflammation in cerebral ischemia and reperfusion injury possibly via high mobility group box 1/Toll-like receptor 4/NFκB pathway. Front. Neurol. 2018;9:253. doi: 10.3389/fneur.2018.00253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Akash M.S.H., Rehman K., Chen S. Role of inflammatory mechanisms in pathogenesis of type 2 diabetes mellitus. J. Cell. Biochem. 2013;114:525–531. doi: 10.1002/jcb.24402. [DOI] [PubMed] [Google Scholar]
- 158.Fernandes J.V., Cobucci R.N.O., Jatobá C.A.N., de Medeiros Fernandes T.A.A., de Azevedo J.W.V., de Araújo J.M.G. The role of the mediators of inflammation in cancer development. Pathol. Oncol. Res. 2015;21:527–534. doi: 10.1007/s12253-015-9913-z. [DOI] [PubMed] [Google Scholar]
- 159.Kim J.Y., Kim Y.M., Park J.M., Han Y.M., Lee K.C., Hahm K.B., Hong K. Cancer preventive effect of recombinant TRAIL by ablation of oncogenic inflammation in colitis-associated cancer rather than anticancer effect. Oncotarget. 2018;9:1705–1716. doi: 10.18632/oncotarget.23083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Jang Y., Kim E.K., Shim W.S. Phytotherapeutic effects of the fruits of Poncirus trifoliata (L.) Raf. on cancer, inflammation, and digestive dysfunction. Phytother. Res. 2018;32:616–624. doi: 10.1002/ptr.6008. [DOI] [PubMed] [Google Scholar]
- 161.Lee H.J., Park J.M., Han Y.M., Gil H.K., Kim J., Chang J.Y., Jeong M., Go E.-J., Hahm K.B. The role of chronic inflammation in the development of gastrointestinal cancers: Reviewing cancer prevention with natural anti-inflammatory intervention. Expert. Rev. Gastroenterol. Hepatol. 2016;10:129–139. doi: 10.1586/17474124.2016.1103179. [DOI] [PubMed] [Google Scholar]
- 162.Kim E.Y., Kim N., Kim Y.S., Seo J.Y., Park I., Ahn H.K., Jeong Y.M., Kim J.H. Prognostic Significance of Modified Advanced Lung Cancer Inflammation Index (ALI) in Patients with Small Cell Lung Cancer_ Comparison with Original ALI. PLoS ONE. 2016;11:e0164056. doi: 10.1371/journal.pone.0164056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Costa J.F.O., Barbosa-Filho J.M., de Azevedo Maia G.L., Guimarães E.T., Meira C.S., Ribeiro-dos-Santos R., de Carvalho L.C.P., Soares M.B.P. Potent anti-inflammatory activity of betulinic acid treatment in a model of lethal endotoxemia. Int. Immunopharmacol. 2014;23:469–474. doi: 10.1016/j.intimp.2014.09.021. [DOI] [PubMed] [Google Scholar]
- 164.Singh D.D., Han I., Choi E.H., Yadav D.K. Immunopathology, host-virus genome interactions, and effective vaccine development in SARS-CoV-2. Comput. Struct. Biotechnol. J. 2020;18:3774–3787. doi: 10.1016/j.csbj.2020.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Subedi L., Subedi L., Gaire B.P., Parveen A., Kim S.Y. Nitric Oxide as a Target for Phytochemicals in Anti-Neuroinflammatory Prevention Therapy. Int. J. Mol. Sci. 2021;22:4771. doi: 10.3390/ijms22094771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Jesus J.A., Lago J.H.G., Laurenti M.D., Yamamoto E.S., Passero L.F.D. Antimicrobial activity of oleanolic and ursolic acids: An update. Evid.-Based Complementary Altern. Med. 2015;2015:620472. doi: 10.1155/2015/620472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Subedi L., Lee J.H., Yumnam S., Ji E., Kim S.Y. Anti-Inflammatory Effect of Sulforaphane on LPS-Activated Microglia Potentially through JNK/AP-1/NF-κB Inhibition and Nrf2/HO-1 Activation. Cells. 2019;8:194. doi: 10.3390/cells8020194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Kumar S., Rana R., Yadav D.K. Atomic-scale modeling of the effect of lipid peroxidation on the permeability of reactive species. J. Biomol. Struct. Dyn. 2021;39:1284–1294. doi: 10.1080/07391102.2020.1730971. [DOI] [PubMed] [Google Scholar]
- 169.Zerin T., Lee M., Jang W.S., Nam K.W., Song H.Y. Anti-inflammatory potential of ursolic acid in Mycobacterium tuberculosis-sensitized and Concanavalin A-stimulated cells. Mol. Med. Rep. 2016;13:2736–2744. doi: 10.3892/mmr.2016.4840. [DOI] [PubMed] [Google Scholar]
- 170.Huang Q., Chen H., Ren Y., Wang Z., Zeng P., Li X., Wang J., Zheng X. Anti-hepatocellular carcinoma activity and mechanism of chemopreventive compounds: Ursolic acid derivatives. Pharm. Biol. 2016;54:3189–3196. doi: 10.1080/13880209.2016.1214742. [DOI] [PubMed] [Google Scholar]
- 171.Bowen-Forbes C.S., Mulabagal V., Liu Y., Nair M.G. Ursolic acid analogues: Non-phenolic functional food components in Jamaican raspberry fruits. Food. Chem. 2009;116:633–637. doi: 10.1016/j.foodchem.2009.02.075. [DOI] [Google Scholar]
- 172.Dwivedi G.R., Rai R., Pratap R., Singh K., Pati S., Sahu S.N., Kant J., Darokar M.P., Yadav D.K. Drug resistance reversal potential of multifunctional thieno[3,2-c]pyran via potentiation of antibiotics in MDR P. aeruginosa. Biomed. Pharmacother. 2021;142:112084. doi: 10.1016/j.biopha.2021.112084. [DOI] [PubMed] [Google Scholar]
- 173.Wei Z.-Y., Chi K.-Q., Wang K.-S., Wu J., Liu L.-P., Piao H.-R. Design, synthesis, evaluation, and molecular docking of ursolic acid derivatives containing a nitrogen heterocycle as anti-inflammatory agents. Bioorganic Med. Chem. Lett. 2018;28:1797–1803. doi: 10.1016/j.bmcl.2018.04.021. [DOI] [PubMed] [Google Scholar]
- 174.Singh D.D., Han I., Choi E.H., Yadav D.K. Recent Advances in Pathophysiology, Drug Development and Future Perspectives of SARS-CoV-2. Front. Cell. Dev. Biol. 2020;8:580202. doi: 10.3389/fcell.2020.580202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Habtemariam S. Antioxidant and anti-inflammatory mechanisms of neuroprotection by ursolic acid: Addressing brain injury, cerebral ischemia, cognition deficit, anxiety, and depression. Oxidative Med. Cell. Longev. 2019;2019:8512048. doi: 10.1155/2019/8512048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Habtemariam S. Iridoids and other monoterpenes in the Alzheimer’s brain: Recent development and future prospects. Molecules. 2018;23:117. doi: 10.3390/molecules23010117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Na H., Mok C., Lee J. Effects of plasma treatment on the oxidative stability of vegetable oil containing antioxidants. Food Chem. 2020;302:125306. doi: 10.1016/j.foodchem.2019.125306. [DOI] [PubMed] [Google Scholar]
- 178.Jeong S.Y., Gu X., Jeong K.W. Photoactivation of N-retinylidene-N-retinylethanolamine compromises autophagy in retinal pigmented epithelial cells. Food Chem. Toxicol. 2019;131:110555. doi: 10.1016/j.fct.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 179.Islam M.Z., Park B.J., Lee Y.T. Effect of salinity stress on bioactive compounds and antioxidant activity of wheat microgreen extract under organic cultivation conditions. Int. J. Biol. Macromol. 2019;140:631–636. doi: 10.1016/j.ijbiomac.2019.08.090. [DOI] [PubMed] [Google Scholar]
- 180.Cho H.T., Kim J.H., Heo W., Lee H.S., Lee J.J., Park T.S., Lee J.H., Kim Y.J. Explosively Puffed Ginseng Ameliorates Ionizing Radiation-Induced Injury of Colon by Decreasing Oxidative Stress-Related Apoptotic Cell Execution in Mice. J. Med. Food. 2019;22:490–498. doi: 10.1089/jmf.2018.4293. [DOI] [PubMed] [Google Scholar]
- 181.Habtemariam S. Going back to the good old days: The merit of crude plant drug mixtures in the 21st century. Int. J. Complementary Altern. Med. 2017;6:1–5. doi: 10.15406/ijcam.2017.06.00182. [DOI] [Google Scholar]
- 182.Wahedi H.M., Chae J.K., Subedi L., Kang M.C., Cho H., Kim S., Kim S.Y. NED416, a novel synthetic Sirt1 activator, promotes cutaneous wound healing via the MAPK/Rho pathway. Int. J. Mol. Med. 2020;46:149–158. doi: 10.3892/ijmm.2020.4564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Li J.-S., Wang W.-J., Sun Y., Zhang Y.-H., Zheng L. Ursolic acid inhibits the development of nonalcoholic fatty liver disease by attenuating endoplasmic reticulum stress. Food Funct. 2015;6:1643–1651. doi: 10.1039/C5FO00083A. [DOI] [PubMed] [Google Scholar]
- 184.Li J., Li N., Yan S., Liu M., Sun B., Lu Y., Shao Y. Ursolic acid alleviates inflammation and against diabetes-induced nephropathy through TLR4-mediated inflammatory pathway. Mol. Med. Rep. 2018;18:4675–4681. doi: 10.3892/mmr.2018.9429. [DOI] [PubMed] [Google Scholar]
- 185.Ullevig S.L., Zhao Q., Zamora D., Asmis R. Ursolic acid protects diabetic mice against monocyte dysfunction and accelerated atherosclerosis. Atherosclerosis. 2011;219:409–416. doi: 10.1016/j.atherosclerosis.2011.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Xiang M., Wang J., Zhang Y., Ling J., Xu X. Attenuation of aortic injury by ursolic acid through RAGE-Nox-NFκB pathway in streptozocin-induced diabetic rats. Arch. Pharmacal Res. 2012;35:877–886. doi: 10.1007/s12272-012-0513-0. [DOI] [PubMed] [Google Scholar]
- 187.Benetou V., Lagiou A., Lagiou P. Chemoprevention of cancer: Current evidence and future prospects. F1000Research. 2015;4:916. doi: 10.12688/f1000research.6684.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Kim J., Bae J.S. Metabolic regulation of macrophages in tumor microenvironment. Curr. Opin. Hematol. 2018;25:52–59. doi: 10.1097/MOH.0000000000000390. [DOI] [PubMed] [Google Scholar]
- 189.Park C., Yun S.J., Ryu S.J., Lee S., Lee Y.S., Yoon Y., Park S.C. Systematic identification of an integrative network module during senescence from time-series gene expression. BMC Syst. Biol. 2017;11:36. doi: 10.1186/s12918-017-0417-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Jeong J., Oh E.J., Yang W.I., Kim S.J., Yoon S.O. Implications of infiltrating immune cells within bone marrow of patients with diffuse large B-cell lymphoma. Hum. Pathol. 2017;64:222–231. doi: 10.1016/j.humpath.2017.04.012. [DOI] [PubMed] [Google Scholar]
- 191.Kim M.S., Jeong J., Seo J., Kim H.S., Kim S.J., Jin W. Dysregulated JAK2 expression by TrkC promotes metastasis potential, and EMT program of metastatic breast cancer. Sci. Rep. 2016;6:33899. doi: 10.1038/srep33899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Park J.M., Lee H.J., Yoo J.H., Ko W.J., Cho J.Y., Hahm K.B. Overview of gastrointestinal cancer prevention in Asia. Best. Pract. Res. Clin. Gastroenterol. 2015;29:855–867. doi: 10.1016/j.bpg.2015.09.008. [DOI] [PubMed] [Google Scholar]
- 193.Rashid S., Dar B.A., Majeed R., Hamid A., Bhat B.A. Synthesis and biological evaluation of ursolic acid-triazolyl derivatives as potential anti-cancer agents. Eur. J. Med. Chem. 2013;66:238–245. doi: 10.1016/j.ejmech.2013.05.029. [DOI] [PubMed] [Google Scholar]
- 194.Singh D.D., Han I., Choi E.H., Yadav D.K. CRISPR/Cas9 based genome editing for targeted transcriptional control in triple-negative breast cancer. Comput. Struct. Biotechnol. J. 2021;19:2384–2397. doi: 10.1016/j.csbj.2021.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Singh D.D., Verma R., Tripathi S.K., Sahu R., Trivedi P., Yadav D.K. Breast Cancer Transcriptional Regulatory Network Reprogramming by using the CRISPR/Cas9 system: An Oncogenetics Perspective. Curr. Top. Med. Chem. 2021 doi: 10.2174/1568026621666210902120754. ahead of print. [DOI] [PubMed] [Google Scholar]
- 196.Huang M.-T., Ho C.-T., Wang Z.Y., Ferraro T., Lou Y.-R., Stauber K., Ma W., Georgiadis C., Laskin J.D., Conney A.H. Inhibition of skin tumorigenesis by rosemary and its constituents carnosol and ursolic acid. Cancer Res. 1994;54:701–708. [PubMed] [Google Scholar]
- 197.Prasad S., Yadav V.R., Sung B., Reuter S., Kannappan R., Deorukhkar A., Diagaradjane P., Wei C. Baladandayuthapani, V.; Krishnan, S.; et al.; Ursolic acid inhibits growth and metastasis of human colorectal cancer in an orthotopic nude mouse model by targeting multiple cell signaling pathways: Chemosensitization with capecitabine. Clin. Cancer Res. 2012;18:4942–4953. doi: 10.1158/1078-0432.CCR-11-2805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Lewinska A., Adamczyk-Grochala J., Kwasniewicz E., Deregowska A., Wnuk M. Ursolic acid-mediated changes in glycolytic pathway promote cytotoxic autophagy and apoptosis in phenotypically different breast cancer cells. Apoptosis. 2017;22:800–815. doi: 10.1007/s10495-017-1353-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Li W., Zhang H., Nie M., Tian Y., Chen X., Chen C., Chen H., Liu R. Ursolic acid derivative FZU-03,010 inhibits STAT3 and induces cell cycle arrest and apoptosis in renal and breast cancer cells. Acta Biochim. Biophys. Sin. 2017;49:367–373. doi: 10.1093/abbs/gmx012. [DOI] [PubMed] [Google Scholar]
- 200.Elstrom R.L., Bauer D.E., Buzzai M., Karnauskas R., Harris M.H., Plas D.R., Zhuang H., Cinalli R.M., Alavi A., Rudin C.M., et al. Akt stimulates aerobic glycolysis in cancer cells. Cancer Res. 2004;64:3892–3899. doi: 10.1158/0008-5472.CAN-03-2904. [DOI] [PubMed] [Google Scholar]
- 201.Robey R.B., Hay N. Is Akt the “Warburg kinase”?—Akt-energy metabolism interactions and oncogenesis. Semin. Cancer Biol. 2009;19:25–31. doi: 10.1016/j.semcancer.2008.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Zheng Q.-Y., Jin F.-S., Yao C., Zhang T., Zhang G.-H., Ai X. Ursolic acid-induced AMP-activated protein kinase (AMPK) activation contributes to growth inhibition and apoptosis in human bladder cancer T24 cells. Biochem. Biophys. Res. Commun. 2012;419:741–747. doi: 10.1016/j.bbrc.2012.02.093. [DOI] [PubMed] [Google Scholar]
- 203.Li J., Liang X., Yang X. Ursolic acid inhibits growth and induces apoptosis in gemcitabine-resistant human pancreatic cancer via the JNK and PI3K/Akt/NF-κB pathways. Oncol. Rep. 2012;28:501–510. doi: 10.3892/or.2012.1827. [DOI] [PubMed] [Google Scholar]
- 204.Yan S.-L., Huang C.-Y., Wu S.-T., Yin M.-C. Oleanolic acid and ursolic acid induce apoptosis in four human liver cancer cell lines. Toxicol. Vitro. 2010;24:842–848. doi: 10.1016/j.tiv.2009.12.008. [DOI] [PubMed] [Google Scholar]
- 205.Kisen G.Ø., Tessitore L., Costelli P., Gordon P.B., Schwarze P.E., Baccino F.M., Seglen P.O. Reduced autophagic activity in primary rat hepatocellular carcinoma and ascites hepatoma cells. Carcinogenesis. 1993;14:2501–2505. doi: 10.1093/carcin/14.12.2501. [DOI] [PubMed] [Google Scholar]
- 206.Kondo Y., Kanzawa T., Sawaya R., Kondo S. The role of autophagy in cancer development and response to therapy. Nat. Rev. Cancer. 2005;5:726–734. doi: 10.1038/nrc1692. [DOI] [PubMed] [Google Scholar]
- 207.Shin S.W., Kim S.Y., Park J.-W. Autophagy inhibition enhances ursolic acid-induced apoptosis in PC3 cells. Biochim. Biophys. Acta Mol. Cell Res. 2012;1823:451–457. doi: 10.1016/j.bbamcr.2011.10.014. [DOI] [PubMed] [Google Scholar]
- 208.Degenhardt K., Mathew R., Beaudoin B., Bray K., Anderson D., Chen G., Mukherjee C., Shi Y., Gélinas C., Fan Y., et al. Autophagy promotes tumor cell survival and restricts necrosis, inflammation, and tumorigenesis. Cancer Cell. 2006;10:51–64. doi: 10.1016/j.ccr.2006.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Shazly G.A., Ibrahim M.A., Badran M.M., Zoheir K.M.A. Utilizing P luronic F-127 and G elucire 50/13 Solid Dispersions for Enhanced Skin Delivery of Flufenamic Acid. Drug Dev. Res. 2012;73:299–307. doi: 10.1002/ddr.21013. [DOI] [Google Scholar]
- 210.Maulvi F.A., Dalwadi S.J., Thakkar V.T., Soni T.G., Gohel M.C., Gandhi T.R. Improvement of dissolution rate of aceclofenac by solid dispersion technique. Powder Technol. 2011;207:47–54. doi: 10.1016/j.powtec.2010.10.009. [DOI] [Google Scholar]
- 211.Singh D.D., Yadav D.K. TNBC: Potential Targeting of Multiple Receptors for a Therapeutic Breakthrough, Nanomedicine, and Immunotherapy. Biomedicines. 2021;9:876. doi: 10.3390/biomedicines9080876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.He Q., Guo S., Qian Z., Chen X. Development of individualized anti-metastasis strategies by engineering nanomedicines. Chem. Soc. Rev. 2015;44:6258–6286. doi: 10.1039/C4CS00511B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Li T., Chen X., Liu Y., Fan L., Lin L., Xu Y., Chen S., Shao J. pH-Sensitive mesoporous silica nanoparticles anticancer prodrugs for sustained release of ursolic acid and the enhanced anti-cancer efficacy for hepatocellular carcinoma cancer. Eur. J. Pharm. Sci. 2017;96:456–463. doi: 10.1016/j.ejps.2016.10.019. [DOI] [PubMed] [Google Scholar]
- 214.De Oliveira E.C.V., Carneiro Z.A., de Albuquerque S.R., Marchetti J.M. Development and evaluation of a nanoemulsion containing ursolic acid: A promising trypanocidal agent. AAPS Pharm. Sci. Tech. 2017;18:2551–2560. doi: 10.1208/s12249-017-0736-y. [DOI] [PubMed] [Google Scholar]
- 215.Nahak P., Karmakar G., Chettri P., Roy B., Guha P., Besra S.E., Soren A., Bykov A.G., Akentiev A.V., Noskov B.A., et al. Influence of lipid core material on physicochemical characteristics of an ursolic acid-loaded nanostructured lipid carrier: An attempt to enhance anticancer activity. Langmuir. 2016;32:9816–9825. doi: 10.1021/acs.langmuir.6b02402. [DOI] [PubMed] [Google Scholar]
- 216.de Araújo Lopes S.C., Novais M.V.M., Teixeira C.S., Honorato-Sampaio K., Tadeu Pereira M.R., Ferreira L.A.N.M., Braga F.C., Oliveira M.C. Preparation, physicochemical characterization, and cell viability evaluation of long-circulating and pH-sensitive liposomes containing ursolic acid. Bio. Med. Res. Int. 2013;2013:467147. doi: 10.1155/2013/467147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Vasconcelos T., Sarmento B., Costa P. Solid dispersions as strategy to improve oral bioavailability of poor water soluble drugs. Drug Discov. Today. 2007;12:1068–1075. doi: 10.1016/j.drudis.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 218.Jinhua W. Ursolic acid: Pharmacokinetics process in vitro and in vivo, a mini review. Arch. Pharm. 2019;352:e1800222. doi: 10.1002/ardp.201800222. [DOI] [PubMed] [Google Scholar]
- 219.Pathak A.K., Bhutani M., Nair A.S., Ahn K.S., Chakraborty A., Kadara H., Guha S., Sethi G., Aggarwal B.B. Ursolic acid inhibits STAT3 activation pathway leading to suppression of proliferation and chemosensitization of human multiple myeloma cells. Mol. Cancer Res. 2007;5:943–955. doi: 10.1158/1541-7786.MCR-06-0348. [DOI] [PubMed] [Google Scholar]
- 220.Shanmugam M.K., Dai X., Kumar A.P., Tan B.K.H., Sethi G., Bishayee A. Ursolic acid in cancer prevention and treatment: Molecular targets, pharmacokinetics and clinical studies. Biochem. Pharmacol. 2013;85:1579–1587. doi: 10.1016/j.bcp.2013.03.006. [DOI] [PubMed] [Google Scholar]
- 221.Subedi L. Venkatesan, R. and Kim, S.Y. Neuroprotective and Anti-Inflammatory Activities of Allyl Isothiocyanate through Attenuation of JNK/NF-κB/TNF-α Signaling. Int. J. Mol. Sci. 2017;18:1423. doi: 10.3390/ijms18071423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Shimohama S., Sawada H., Kitamura Y., Taniguchi T. Disease model: Parkinson’s disease. Trends. Mol. Med. 2003;9:360–365. doi: 10.1016/S1471-4914(03)00117-5. [DOI] [PubMed] [Google Scholar]
- 223.Tsai S.J., Yin M.C. Antioxidative and anti-inflammatory protection of oleanolic acid and ursolic acid in PC12 cells. J. Food Sci. 2008;73:H174–H178. doi: 10.1111/j.1750-3841.2008.00864.x. [DOI] [PubMed] [Google Scholar]
- 224.Santos C.U.Y., Snyder P.J., Wu W.-C., Zhang M., Echeverria A., Alber J. Pathophysiologic relationship between Alzheimer’s disease, cerebrovascular disease, and cardiovascular risk: A review and synthesis. Alzheimer’s Dement. Diagn. Assess. Dis. Monit. 2017;7:69–87. doi: 10.1016/j.dadm.2017.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Bredesen D.E. Neurodegeneration in Alzheimer’s disease: Caspases and synaptic element interdependence. Mol. Neurodegener. 2009;4:1–10. doi: 10.1186/1750-1326-4-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Acharya S., Adamova D., Adolfsson J., Aggarwal M.M., Aglieri Rinella G., Agnello M., Agrawal N., Ahammed Z., Ahn S.U., Aiola S. J/psi Elliptic Flow in Pb-Pb Collisions at sqrt[s_{NN}]=5.02 TeV. Phys. Rev. Lett. 2017;119:242301. doi: 10.1103/PhysRevLett.119.242301. [DOI] [PubMed] [Google Scholar]
- 227.Hane F.T., Lee B.Y., Leonenko Z. Recent progress in Alzheimer’s disease research, part 1: Pathology. J. Alzheimer’s Dis. 2017;57:1–28. doi: 10.3233/JAD-160882. [DOI] [PubMed] [Google Scholar]
- 228.Snow W.M., Albensi B.C. Neuronal gene targets of NF-κB and their dysregulation in Alzheimer’s disease. Front. Mol. Neurosci. 2016;9:118. doi: 10.3389/fnmol.2016.00118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Wilkinson K., Boyd J.D., Glicksman M., Moore K.J., El Khoury J. A high content drug screen identifies ursolic acid as an inhibitor of amyloid β protein interactions with its receptor CD36. J. Biol. Chem. 2011;286:34914–34922. doi: 10.1074/jbc.M111.232116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Yoon J.-H., Youn K., Ho C.-T., Karwe M.V., Jeong W.-S., Jun M. p-Coumaric acid and ursolic acid from corni fructus attenuated β-Amyloid25â 35-induced toxicity through regulation of the NF-κB signaling pathway in PC12 cells. J. Agric. Food Chem. 2014;62:4911–4916. doi: 10.1021/jf501314g. [DOI] [PubMed] [Google Scholar]
- 231.Machado D.G., Neis V.B., Balen G.O., Colla A., Cunha M.P., Dalmarco J.B., Pizzolatti M.G., Prediger R.D., Rodrigues A.L.S. Antidepressant-like effect of ursolic acid isolated from Rosmarinus officinalis L. in mice: Evidence for the involvement of the dopaminergic system. Pharmacol. Biochem. Behavior. 2012;103:204–211. doi: 10.1016/j.pbb.2012.08.016. [DOI] [PubMed] [Google Scholar]
- 232.Zhu Z., Qian Z., Yan Z., Zhao C., Wang H., Ying G. A phase I pharmacokinetic study of ursolic acid nanoliposomes in healthy volunteers and patients with advanced solid tumors. Int. J. Nanomed. 2013;8:129. doi: 10.2147/IJN.S38271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Qian Z., Wang X., Song Z., Zhang H., Zhou S., Zhao J., Wang H. A phase I trial to evaluate the multiple-dose safety and antitumor activity of ursolic acid liposomes in subjects with advanced solid tumors. Bio. Med. Res. Int. 2015;2015:809714. doi: 10.1155/2015/809714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Colla A.R.S., Oliveira Ã., Pazini F.L., Rosa J.M., Manosso L.M., Cunha M.P., Rodrigues A.L.S. Serotonergic and noradrenergic systems are implicated in the antidepressant-like effect of ursolic acid in mice. Pharmacol. Biochem. Behavior. 2014;124:108–116. doi: 10.1016/j.pbb.2014.05.015. [DOI] [PubMed] [Google Scholar]
- 235.Marks D.M., Pae C.-U., Patkar A.A. Triple reuptake inhibitors: The next generation of antidepressants. Curr. Neuropharmacol. 2008;6:338–343. doi: 10.2174/157015908787386078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Trivedi M.H., Fava M., Wisniewski S.R., Thase M.E., Quitkin F., Warden D., Ritz L., Nierenberg A.A., Lebowitz B.D., Biggs M.M. Medication augmentation after the failure of SSRIs for depression. N. Engl. J. Med. 2006;354:1243–1252. doi: 10.1056/NEJMoa052964. [DOI] [PubMed] [Google Scholar]
- 237.Bodkin J.A., Lasser R.A., Wines J.D., Baldessarini R.J. Combining serotonin reuptake inhibitors and bupropion in partial responders to antidepressant monotherapy. J. Clin. Psychiatry. 1997;58:137–145. doi: 10.4088/JCP.v58n0401. [DOI] [PubMed] [Google Scholar]
- 238.Sharma H., Santra S., Dutta A. Triple reuptake inhibitors as potential next-generation antidepressants: A new hope? Future Med. Chem. 2015;7:2385–2406. doi: 10.4155/fmc.15.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Xia Y., Wei G., Si D., Liu C. Quantitation of ursolic acid in human plasma by ultra performance liquid chromatography tandem mass spectrometry and its pharmacokinetic study. J. Chromatogr. B. 2011;879:219–224. doi: 10.1016/j.jchromb.2010.11.037. [DOI] [PubMed] [Google Scholar]
- 240.Bang H.S., Seo D.Y., Chung Y.M., Oh K.-M., Park J.J., Arturo F., Jeong S.-H., Kim N., Han J. Ursolic acid-induced elevation of serum irisin augments muscle strength during resistance training in men. Korean J. Physiol. Pharmacol. 2014;18:441–446. doi: 10.4196/kjpp.2014.18.5.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Wrann C.D., White J.P., Salogiannnis J., Laznik-Bogoslavski D., Wu J., Ma D., Lin J.D., Greenberg M.E., Spiegelman B.M. Exercise induces hippocampal BDNF through a PGC-1α/FNDC5 pathway. Cell. Metab. 2013;18:649–659. doi: 10.1016/j.cmet.2013.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Moon H.-S., Dincer F., Mantzoros C.S. Pharmacological concentrations of irisin increase cell proliferation without influencing markers of neurite outgrowth and synaptogenesis in mouse H19-7 hippocampal cell lines. Metabolism. 2013;62:1131–1136. doi: 10.1016/j.metabol.2013.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Adamova D., Aggarwal M.M., Aglieri Rinella G., Agnello M., Agrawal N., Ahammed Z., Ahn S.U., Aiola S., Akindinov A., Al-Turany M. Azimuthally Differential Pion Femtoscopy in Pb-Pb Collisions at s N N= 2.76 TeV. Phys. Rev. Lett. 2017;118:222301. doi: 10.1103/PhysRevLett.118.222301. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The information that supports the findings of this study is available in this article.