Abstract
Lower household income is associated with poorer self-reported health status, especially in the elderly. Considering the importance of subjective health in this fragile population, it would be worthwhile to explore the physical and mental health factors that may help to predict good or poor self-rated health (SRH) status. We first described three main categories (individual, physical, and psychological) between low-income seniors with good and poor SRH. Next, statistically significant physical and mental health factors affecting poor SRH were identified. In this study, original data from the 2017 National Survey of Older Persons in South Korea were analyzed. People aged 65 years and over with low household income were eligible. A total of 1405 men and 2945 women (n = 4350) were enrolled, and less than half of participants (47.5%, n = 2066) belonged to the poor SRH cohort. We applied individual variable-adjusted models and found that poor SRH was significantly associated with ADL limitation (odds ratio (OR): 2.91, 95% confidence interval (CI) 2.11–4.01), IADL limitation (OR: 1.80, 95% CI: 1.52–2.13), malnutrition (OR: 1.76, 95% CI: 1.53–2.04), and depression (OR: 3.65, 95% CI: 3.10–4.31) on logistic regression analysis. Our findings suggest that limited ADL/IADL, poor nutrition, and depression need to be emphasized to improve subjective health status in low-income adults. Early recognition and timely intervention might help them to live better and happier, ultimately relieving social healthcare burdens.
Keywords: self-rated health, risk factor, older adults, low income
1. Introduction
In this era of worldwide aging, the rapidly increasing number of the aged population unavoidably results in personal, national, and global healthcare issues. As a matter of fact, the Republic of Korea is now one of the world’s fastest aging countries. Our country officially became an aged society in 2017 (which was just 17 years after we reached aging society status in 2000) and is estimated to enter a super-aged society by the end of 2026 [1]. Accordingly, the proportion of the elderly population has risen sharply, and this means that more and more people are exposed to health problems, economic difficulties, loneliness, and feelings of alienation as they get old. In 2020, our national health and welfare expenditure for this special population was KRW 12 trillion, which was equivalent to 1% of the gross domestic product (GDP) [2].
Another hot topic of the present time is the phenomenon of economic polarization resulting in health inequality among members of society. In other words, we live in a ‘looks equal but not equal’ community where individual health status depends on socioeconomic backgrounds such as education and household income despite the help from the social welfare system. When it comes to senior adults, this social problem gets even worse. It was found that people with low income levels have poorer functional/physical capability and worse psychological well-being [3].
Self-rated health (SRH) status is clinically important because this can serve as a predictor of one’s future morbidity or mortality, especially in the elderly [4,5,6,7,8]. Subjective health assessment is a relatively feasible and reliable tool to assess the responder’s overall health. It incorporates physical health factors, as well as mental factors such as overall sense of well-being and satisfaction in daily life [9,10]. A ‘poor or negative’ self-assessment of health represents not only physical distress but also emotional and social conditions of the individual. Thus, poor SRH seemed to be strongly associated with chronic illness, frequent hospital visits, and even mortality [11].
Considering the importance of SRH in this vulnerable population, it would be meaningful to explore the physical and mental health factors that may help to predict poor SRH in low-income adults. Using large-scale national data, we compared individual, physical, and mental health factors in those with good and poor subjective health groups. Then, we tried to identify significant physical and mental health variables affecting SRH by controlling for individual subcategories.
2. Materials and Methods
2.1. Source of Data
We obtained original data from the 2017 National Survey of Older Persons (NSOP) with approval from the National Statistical Office [12]. The database was constructed through random stratification of 10,299 Korean adults living in general residential facilities and was designed to represent the elderly population. The national survey was conducted from June to August 2017 through direct interviews with senior citizens aged 65 and over in 934 survey areas. Surveys were carried out by 60 professional surveyors (fifteen teams of four surveyors each, one supervisor in a team) who were previously trained by skilled research personnel.
2.2. Participants Selection and Study Design
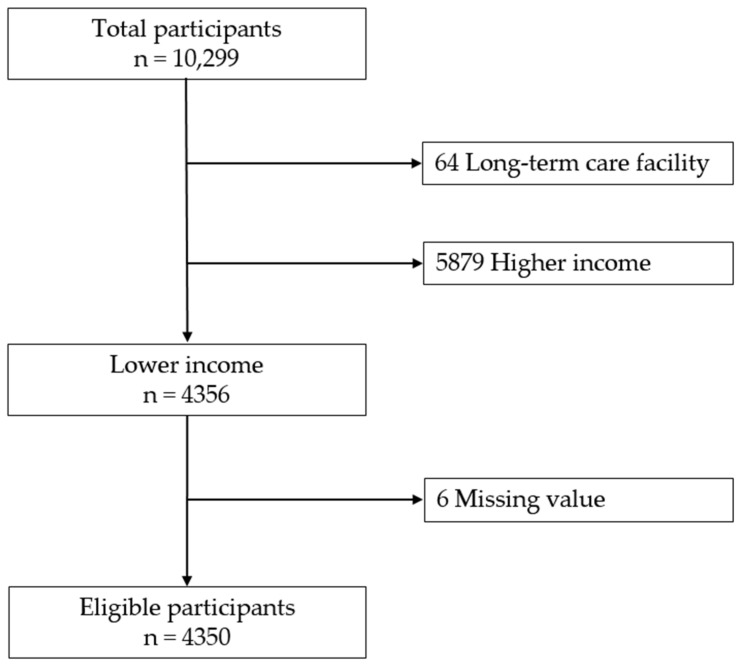
In this survey, household income was measured by totaling annual income from any (personal or public) sources. We divided our study population into five categorical income groups, called quintiles. The first quintile refers to those with the lowest income, and the fifth quintile the highest (i.e., Q1 (the lowest quintile), Q2, Q3, Q4, and Q5 (the highest quintile)). A person with ‘lower household income’ was defined as one who belonged to either Q1 or Q2. Older adults who met the following criteria were eligible: (a) lower household income, (b) community dwelling, and (c) without missing data. Finally, 4350 respondents were enrolled in this study (Figure 1).
Figure 1.
Flow diagram of inclusion of study population.
Using descriptive and correlational study designs, we evaluated predictors of poor subjective health in adults with lower income with respect to individual, physical, and psychological categories. We then built variable-adjusted prediction models to identify physical and psychological factors that correlated with poor SRH in logistic regression analysis.
2.3. Measurements
2.3.1. Subjective Health Assessment
Using a 5-point Likert question (“In general, how would you rate your current health status?”), we assessed the self-rated health status of the participants. Five answers were classified into dichotomous values: “good” (very good, good, and fair) and “poor” (poor and very poor).
2.3.2. Individual Variables
Variables in individual categories were classified into four subcategories: demographic, socioeconomic, health status, and health-related behavior. Age, gender, marital status (living with a spouse or living without a spouse), and living status (alone, living with a spouse, living with children, and others) belonged to the demographic subcategory. Education level (0–6 years, 7–9 years, 10–12 years, or ≥13 years) belonged to the socioeconomic subcategory. Body mass index (BMI), chronic illness (such as arthritis, diabetes, and hypertension), and current number of medications (0, 1, 2, or ≥3) were categorized as the health status subgroup. Finally, the health-related behavior subgroup was made up of exercise, smoking (never/past or current), and drinking.
The presence or absence of chronic disease was evaluated by questions such as “have you been suffering from any diseases like high blood pressure, diabetes, or arthritis for more than 3 months?” and “have you ever been diagnosed with the above diseases by a doctor?”. Subjects who replied “yes” to both questions were determined to have a chronic disease. Physical exercise of 150 min or more per week was considered to correspond to the recommended level according to the World Health Organization (WHO) criteria [13]. The amount of exercise was classified as within the recommended level, below the recommended level, and none. Alcohol intake was evaluated on the basis of the National Institute on Alcohol Abuse and Alcoholism criteria [14]. Drinking less than one standard drink (a 350 mL glass of beer) per day was considered as an acceptable amount and drinking more than one standard drink a day was regarded as excessive in this study. The others who did not drink at all were determined as “none”.
2.3.3. Physical Variables
Variables in the physical category encompassed visual, auditory, activities of daily living (ADL), instrumental activities of daily living (IADL), and nutritional status.
Visual discomfort was classified as “discomfort” in older adults who replied “uncomfortable” or “very uncomfortable.” Auditory discomfort was defined as “discomfort” in those who responded “uncomfortable” or “very uncomfortable.”
The ADL evaluation was performed in reference to the Korean Activities Daily Living scale [15]. This tool consists of seven queries: “bathing”, “bowel and bladder continence”, “dressing”, “eating food”, “face washing, brushing teeth, and shampooing”, “getting up and walking across the room”, and “toilet use”. Each query was estimated by a three-point rating (total independence, partial dependence, and total dependence), and a higher score indicated more severe limitations to daily routine. For example, a score of 0 (total independence) was regarded as “no limitation”. Scores 1 and 2 (partial and complete dependence, respectively) were regarded as “limitations”. Respondents who had ALD limitation in more than one query were considered to have “limitation to ADL”.
The presence of IADL limitation was estimated according to the Korean Instrumental Activity of Daily Living scale [15]. This scale is composed of ten domains: “ability to make and receive phone calls”, “going out for a short walk”, “laundry”, “managing money”, “performing household chores”, “personal grooming”, “preparing meals”, “shopping”, “taking medications on time”, and “using public transportation”. Total independence fell into “no limitation,” and the others (such as partial, complete, little, much dependence, and cannot be done at all) were recorded as “limitation”. Respondents with restrictions in more than one query were assessed to have “limitation to IADL”.
Individual nutritional status was evaluated on the basis of the ‘Determine Your Nutritional Health’ questionnaire from the Nutrition Screening Initiative [16], which consists of ten binary (“yes” or “no”) questions. A “yes” response to each item was scored in a range of 1 to 4, whereas a “no” response was scored as 0. The total score from 10 items was classified as good nutrition risk (0–2), moderate risk (3–5), and high risk (≥6). In our study, good nutrition risk was defined as “good nutrition”, and moderate and high risk were considered to be “poor nutrition”.
2.3.4. Psychological Variables
Depressive mood was determined according to the 15-item Geriatric Depression Scale in the Korean version (short form of GDS-K; SGDS-K) [17]. The best cut-off value for screening depressive mood was proposed as ≥8 (total scores ranged from 0 to 15). In our study, scores of 8 or more and less than 8 were classified as “depressed” and “not depressed”, respectively.
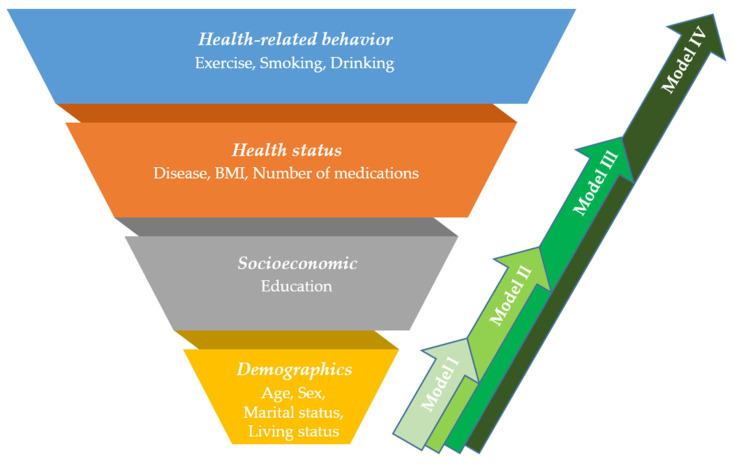
2.4. Statistical Analysis
Descriptive statistics were performed using the χ2 or t-test to compare differences in the subjective health status in individual, physical, and psychological categories. After analyzing each independent variable for univariate regression, statistically significant variables were chosen to carry out multivariate regression. After that, we built new individual-variable adjusted models to reduce the potential confounding effects of individual variables. Elements from individual categories (including demographic, socioeconomic, health status, and health-related behavior subcategories) were combined into groups and were entered into regression models one by one. In designing the model, we assumed that variables in the demographic subcategory (i.e., age, sex, marital status, and living status) were the least modifiable among the four subcategories. Other subcategories, such as socioeconomic, health status, and health-related behaviors could be more easily modified (depending on one’s own effort) in consecutive order. Based on this hypothesis, we first built Model I (consisting of only the demographic subcategory), and then we encompassed easily modifiable subcategories in a stepwise way, which were presented as Models II, III, and IV (Model I: demographic variables only, Model II: demographic and socioeconomic variables, Model III: demographic, socioeconomic, and health status variables, Model IV: all the individual variables in four subcategories) (Figure 2). Odds ratios (ORs) and corresponding 95% confidence intervals (CIs) were also calculated. The statistical significance referred to a value of p < 0.05. Data were analyzed using the IBM SPSS software, version 22.0 (IBM, Armonk, NY, USA).
Figure 2.
Suggested individual-variable adjusted models in this study. The demographic, socioeconomic, health status, and health-related behavior subcategories were combined, and four models were established.
3. Results
3.1. Self-Rated Health Status
Among 4350 participants with lower household income, about half of them (47.5%, n = 2066) perceived themselves as unhealthy.
3.2. Differences in Individual Characteristics between Groups with Good and Poor SRH
Differences in SRH status according to individual variables are summarized in Table 1. In terms of demographic, socioeconomic, health status, and health-related behavior components, almost all the items (except age and living status) revealed statistical significance between good and poor SRH groups.
Table 1.
Differences in individual variables between groups with good and poor SRH (n = 4350).
| Individual Variables | Classification | Good SRH | Poor SRH | χ2 | p | |
|---|---|---|---|---|---|---|
| (n = 2284) | (n = 2066) | |||||
| n (%) or | n (%) or | |||||
| M ± SD * | M ± SD * | |||||
| Demographic | Age | 76.1 ± 6.0 | 77.0 ± 6.1 | 4.96 | 0.979 | |
| Sex | Male | 817 (35.8) | 588 (28.5) | 26.51 | <0.001 | |
| Female | 1467 (64.2) | 1478 (71.5) | ||||
| Marital status | Living with spouse | 1120 (49.0) | 918 (44.4) | 9.23 | 0.002 | |
| Living without spouse | 1164 (51.0) | 1148 (55.6) | ||||
| Living status | Alone | 1072 (46.9) | 1042 (50.4) | 7.46 | 0.059 | |
| Living with spouse | 1071 (46.9) | 884 (42.8) | ||||
| Living with children | 98 (4.3) | 99 (4.8) | ||||
| Others | 43 (1.9) | 41 (2.0) | ||||
| Socioeconomic | Education | 0–6 years | 1580 (69.2) | 1626 (78.7) | 52.10 | <0.001 |
| 7–9 years | 345 (15.1) | 224 (10.8) | ||||
| 10–12 years | 280 (12.2) | 176 (8.5) | ||||
| ≥13 years | 79 (3.5) | 40 (1.9) | ||||
| Health status | Disease | Hypertension | 1342 (58.9) | 1392 (67.4) | 34.52 | <0.001 |
| Diabetes | 400 (17.5) | 616 (29.8) | 91.72 | <0.001 | ||
| Dementia | 24 (1.1) | 54 (2.6) | 15.05 | <0.001 | ||
| Arthritis | 605 (26.5) | 955 (46.2) | 183.70 | <0.001 | ||
| BMI ** | Underweight (<18.5) | 80 (3.5) | 125 (6.1) | 34.02 | <0.001 | |
| Normal (≥18.5, <25) | 1636 (71.6) | 1337 (64.7) | ||||
| Overweight (≥25) | 568 (24.9) | 604 (29.2) | ||||
| Number of medication(s) | 0 | 408 (17.9) | 88 (4.3) | 466.82 | <0.001 | |
| 1 | 308 (13.5) | 99 (4.8) | ||||
| 2 | 343 (15.0) | 149 (7.2) | ||||
| ≥3 | 1225 (53.6) | 1730 (83.7) | ||||
| Health-related Behavior | Exercise | None | 628 (27.5) | 899 (43.5) | 167.84 | <0.001 |
| <150 min. a week | 472 (20.7) | 477 (23.1) | ||||
| ≥150 min. a week | 1184 (51.8) | 690 (33.4) | ||||
| Smoking | Never/Past | 207 (9.1) | 150 (7.3) | 4.68 | 0.031 | |
| Current | 2077 (90.9) | 1916 (92.7) | ||||
| Drinking | None | 1712 (74.9) | 1726 (83.5) | 55.16 | <0.001 | |
| ≤1 standard drink/day | 212 (9.3) | 157 (7.6) | ||||
| >1 standard drink/day | 360 (15.8) | 183 (8.9) | ||||
* M ± SD, mean ± standard deviation. ** BMI, body mass index.
3.3. Differences in Physical and Psychological Factors between Good and Poor SRH Groups
Statistically significant differences were observed between good and poor SRH in view of physical characteristics. Visual or auditory discomforts, ADL limitation, IADL limitation, and poor nutrition were more frequently observed in the poor SRH group. There also was a significant difference between the two groups in terms of psychological factor such as depression (Table 2).
Table 2.
Differences in physical and psychological characteristics between good and poor SRH groups (n = 4350).
| Physical & Psychological Variables | Classification | Good SRH | Poor SRH | χ2 | p | |
|---|---|---|---|---|---|---|
| (n = 2284) | (n = 2066) | |||||
| n (%) | n (%) | |||||
| Physical | Visual discomfort | No | 1447 (63.4) | 1081 (52.3) | 54.22 | <0.001 |
| Yes | 837 (36.6) | 985 (47.7) | ||||
| Hearing discomfort | No | 1843 (80.7) | 1521 (73.6) | 30.94 | <0.001 | |
| Yes | 441 (19.3) | 545 (26.4) | ||||
| ADL * limitation | No | 2223 (97.3) | 1739 (84.2) | 231.14 | <0.001 | |
| Yes | 61 (2.7) | 327 (15.8) | ||||
| IADL ** limitation | No | 1815 (79.5) | 1110 (53.7) | 326.25 | <0.001 | |
| Yes | 469 (20.5) | 956 (46.3) | ||||
| Nutrition | Good | 1364 (59.7) | 662 (32.0) | 333.96 | <0.001 | |
| Poor | 920 (40.3) | 1404 (68.0) | ||||
| Psychological | Depression | NoYes | 1968 (86.2) | 1103 (53.4) | 561.42 | <0.001 |
| 316 (13.8) | 963 (46.6) | |||||
* ADL, Activities of daily living. ** IADL, Instrumental activities of daily living.
3.4. Multivariable Logistic Regression Analysis of Variables Associated with Poor SRH in Low-Income Seniors Using Individual-Variable Adjusted Models
To assess the physical and mental health factors influencing the risk of poor SRH, we introduced the four individual variable-adjusted models as stated above. In Model IV, poor SRH in lower-income adults was significantly correlated with limitation to ADL (odds ratio (OR): 2.91, 95% confidence interval (CI): 2.12–4.01), limitation to IADL (OR: 1.80, 95% CI: 1.52–2.13), malnutrition (OR: 1.76, 95% CI: 1.52–2.04), and depression (OR: 3.65, 95% CI: 3.10–4.31) in multivariate logistic regression analysis (Table 3). In particular, all four factors were consistently significant from our Model I to IV.
Table 3.
Multivariable logistic regression analysis of factors associated with poor SRH in low-income older adults.
| Variables | Model I | Model II | Model III | Model IV |
|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Visual discomfort | 1.24 (1.08–1.43) *** | 1.23 (1.07–1.42) *** | 1.10 (0.92–1.31) | 1.09 (0.95–1.27) |
| Hearing discomfort | 1.08 (0.91–1.27) | 1.08 (0.91–1.28) | 1.14 (0.98–1.31) | 1.11 (0.93–1.32) |
| ADL * limitation | 3.24 (2.38–4.41) *** | 3.25 (2.38–4.42) *** | 3.11 (2.26–4.27) *** | 2.91 (2.12–4.01) *** |
| IADL ** limitation | 2.05 (1.75–2.40) *** | 1.99 (1.70–2.33) *** | 1.91 (1.61–2.25) *** | 1.80 (1.52–2.13) *** |
| Poor nutrition | 2.10 (1.82–2.41) *** | 2.09 (1.82–2.40) *** | 1.73 (1.50–2.00)*** | 1.76 (1.52–2.04) *** |
| Depression | 3.77 (3.22–4.40) *** | 3.73 (3.19–4.37) *** | 3.80 (3.23–4.48) *** | 3.65 (3.10–4.31) *** |
Model I: adjusted for demographic (age, sex, marital status, and living status) subcategory only. Model II: adjusted for demographic and socioeconomic (education) subcategories. Model III: adjusted for demographic, socioeconomic, and health status (disease, BMI, and number of medications) subcategories. Model IV: adjusted for demographic, socioeconomic, health status, and health-related behavior (exercise, smoking, and drinking) subcategories. * ADL, Activities of daily living. ** IADL, Instrumental activities of daily living. *** p < 0.05.
4. Discussion
4.1. Healthcare Issues among Low-Income Adults
Nowadays, one out of five older adults manages their lives on limited earnings, with little room for additional or unexpected health-related expenses. Low-income seniors are more likely to suffer from a chronic illness that requires medical attention than high-income adults [18]. European studies on healthcare inequality according to socioeconomic status suggested that differences in individual income and education level played a role in generating disparities in one’s health level [19,20,21]. As mentioned earlier, an adult with lower income faces each day with a worse physical and mental sense of well-being.
4.2. Self-Rated Health Status in Low-Income Adults
Self-assessed health refers to how individuals evaluate their own health status, and it is a simple but strong indicator for one’s general well-being. This measurement integrates various personal, social, functional, and mental conditions for evaluation. Understanding the importance of individual health status is essential with regard to disease prevention and health promotion [22]. A person with poor SRH is likely to be in physical, emotional, or social distress. As a result, poor SRH could serve as a powerful predictor of frequent outpatient visits, long inpatient stays, and eventual mortality in the elderly. For elderly people who already regard themselves as unhealthy, it is very important to early detect and timely support their physical and psychological shortcomings. As you can imagine, people in a better socioeconomic condition are expected to have better self-perceived health status [23]. On the other hand, we easily assume that the elderly people in a worse socioeconomic position are more ready to give negative answers on self-health assessment items. However, we should also keep in mind that not all low-income adults regard themselves as having poor subjective health. In our survey, less than half of the low-income respondents (47.5%, n = 2066) perceived themselves as unhealthy. For this reason, we thought it would be worthwhile to explore and identify factors associated with poor self-reported health in low-income adults. We hoped that insights from our study might help people at risk of negative SRH to live better and happier by early detection and management, ultimately reducing social healthcare burdens.
4.3. Factors Affecting Subjective Health in Low-Income Elderly People
Many studies proposed that age, gender, education level, household income, along with many other factors, were in close relationship with one’s subjective health [24]. More often than not, outcomes from this straightforward subjective measurement require careful interpretation depending on individualized circumstances or situations. Herein, we focused on the subjective health of community-dwelling and low-income elderly people. With respect to demographic, socioeconomic, health status, and health-related behavior characteristics, all variables except age and living status showed statistical significance between good and poor SRH groups. Likewise, significant differences were observed between the two groups in terms of physical and mental health characteristics such as visual/auditory discomfort, limitation to ADL/IADL, nutrition, and depression. We made a unique effort to identify relevant items affecting self-assessed health status by controlling individual confounders. To set up new risk-adjusted models, individual factors were grouped into four subcategories. Variables from the demographic subcategory (i.e., age, sex, and marital status) were considered as the least modifiable out of four subcategories. In consecutive order, socioeconomic, health status, and health-related behavior variables were considered more easily modifiable than demographic ones. Instead of combining all individual variables at once, we added subcategories one by one to find out which combinations (or models) would be helpful in controlling confounders. In a multiple logistic regression analysis, we identified elements that were coherent throughout all four models. Four factors (ADL limitation, IADL limitation, poor nutrition, and depression) were statistically significant between good and poor self-perceived health groups.
Older adults with ADL and/or IADL limitations are more dependent on daily living activities. They often complain of poor quality of life (QOL), resulting in an increase in healthcare demand [25]. In our study, both ADL and IADL limitations turned out to be significant risk factors for poor SRH. However, we have to keep in mind that there could be possible bidirectional interactions between limited ADL/IADL and poor SRH; limitations to ADL/IADL can be a consequence of poor SRH and vice versa. Malnutrition is also an important issue in view of QOL and even survival. Malnutrition in seniors is common and is easily overlooked or mismanaged by healthcare providers in the real world [26]. Adequate nutritional assessment and intervention are needed to maintain good nutritional health and sense of well-being.
Depression seemed to be the most powerful predictor of negative SRH in our study. According to the 2014 national survey using the Short Form of Geriatric Depression Scale (SGDS), about a third (33.1%) of people aged 65 and over had depressive symptoms [27]. Mental health in old age was influenced by complex causes: death of a spouse, loss of job, decrease in income, chronic illness, and so on. Difficulties in maintaining good relationships with family members and neighbors also caused mental health problems, including depression [28,29]. In a study on geriatric depression with regard to socioeconomic status, depressive mood was frequently observed when the elderly had any of the following episodes: living alone, receiving insufficient medical care, low education level, smoking/drinking, and reduced physical activities [30]. Another study revealed that negative SRH and inability to perform activities of daily living were in direct association with depressive mood [31].
4.4. Strengths and Limitations of Our Research
Our study findings showed that three physical health factors (ADL/IADL limitations and poor nutrition) and a mental health factor (depression) were strongly associated with poor SRH in the elderly with lower household income. In fact, the ADL, IADL, and SRH are multidimensional concepts themselves. Individual, physical, and psychological components affect them either positively or negatively. Based on our findings, any limitation to ADL/IADL, poor nutrition, and depression must be detected as early as possible to improve geriatric subjective health assessment. Good SRH makes a person a healthy member of our society. In addition, healthcare managers and public health policymakers may benefit from our study findings that early detection and management of the elderly at risk of poor SRH reduce social health care expenses in the long run.
Four major limitations could be found in our research. First, this analysis had a cross-sectional design, and this made it difficult to find causality. The cause-and-effect relationship between low income and negative SRH could be unclear, which was an inherent limitation of the study design. Second, there may remain recall bias since the main data source was from the interview. Third, education level was the only item in a socioeconomic subcategory. In other words, other social determinants of health [32] (such as family relations, solidarity network, affiliation, proxy services, and so on) need to be considered in future studies. Finally, our major disadvantage originated from using secondary data as a backbone. It may provide unclear answers to the researcher’s research-related questions or does not contain additional information which the researcher would like to investigate. It requires special attention while interpreting our secondary data analyses. Thus, our study findings necessitate extensive validations in future research.
5. Conclusions
Our findings suggest that low-income elderly people with limited ADL/IADL, poor nutrition, and depression are at risk of poor SRH. Considering the importance of SRH in these fragile populations, early recognition (i.e., active screening of malnutrition and depression in the healthcare facilities) and timely intervention (i.e., consultation to rehabilitation services and mental health professionals) are very important. Our sincere efforts might help them to live better and happier, ultimately relieving worldwide healthcare burdens.
Author Contributions
Conceptualization, M.B.; methodology, M.B.; validation, E.K.; formal analysis, M.B.; investigation, E.K.; resources, E.K.; data curation, M.B.; writing original draft preparation, M.B. and E.K.; writing—review and editing, H.A. All authors have read and agreed to the published version of the manuscript.
Funding
This study received no funding.
Institutional Review Board Statement
This research utilized existing public data without any personal information. Thus, the Institutional Review Board (IRB) determined that it was exempt from IRB review (IRB No. GNAH-2021-10-001).
Informed Consent Statement
Not applicable.
Data Availability Statement
Our data are readily available upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Statistics Korea (KOSTAT) Population Projections for Korea (2017–2067) Statistics Korea (KOSTAT); Daejeon, Korea: 2019. [Google Scholar]
- 2.Statistics Korea (KOSTAT) 2020 Population and Housing Census. Statistics Korea (KOSTAT); Daejeon, Korea: 2021. [Google Scholar]
- 3.Arendt J.N. Income and “Outcomes” for Elderly: DO the Poor have A Poorer Life? Soc. Indic. Res. 2005;70:327–347. doi: 10.1007/s11205-004-1545-8. [DOI] [Google Scholar]
- 4.Mossey J.M., Shapiro E. Self-rated health: A predictor of mortality among the elderly. Am. J. Public Health. 1982;72:800–808. doi: 10.2105/AJPH.72.8.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benyamini Y., Idler E.L. Community Studies Reporting Association between Self-Rated Health and Mortality:Additional Studies, 1995 to 1998. Res. Aging. 1999;21:392–401. doi: 10.1177/0164027599213002. [DOI] [Google Scholar]
- 6.Bond J., Dickinson H.O., Matthews F., Jagger C., Brayne C. Self-rated health status as a predictor of death, functional and cognitive impairment: A longitudinal cohort study. Eur. J. Ageing. 2006;3:193–206. doi: 10.1007/s10433-006-0039-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee Y. The predictive value of self assessed general, physical, and mental health on functional decline and mortality in older adults. J. Epidemiol. Community Health. 2000;54:123–129. doi: 10.1136/jech.54.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh-Manoux A., Guéguen A., Martikainen P., Ferrie J., Marmot M., Shipley M. Self-rated health and mortality: Short- and long-term associations in the Whitehall II study. Psychosom. Med. 2007;69:138–143. doi: 10.1097/PSY.0b013e318030483a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rohrer J.E., Young R., Sicola V., Houston M. Overall self-rated health: A new quality indicator for primary care. J. Eval. Clin. Pract. 2007;13:150–153. doi: 10.1111/j.1365-2753.2006.00692.x. [DOI] [PubMed] [Google Scholar]
- 10.Holzhausen M., Martus P. Validation of a new patient-generated questionnaire for quality of life in an urban sample of elder residents. Qual. Life Res. 2013;22:131–135. doi: 10.1007/s11136-012-0115-9. [DOI] [PubMed] [Google Scholar]
- 11.Gutman G.M., Stark A., Donald A., Beattie B.L. Contribution of self-reported health ratings to predicting frailty, institutionalization, and death over a 5-year period. Int. Psychogeriatr. 2001;13((Suppl. 1)):223–231. doi: 10.1017/S1041610202008165. [DOI] [PubMed] [Google Scholar]
- 12.Chung K. National Survey of Older Koreans: Findings and Implications. The Korean Institute for Health and Social Affairs; Seoul, Korea: 2018. [Google Scholar]
- 13.WHO Guidelines Approved by the Guidelines Review Committee . Global Recommendations on Physical Activity for Health. World Health Organization; Geneva, Switzerland: 2010. [Google Scholar]
- 14.Allen J.P. Assessing Alcohol Problems: A Guide for Clinicians and Researchers. 2nd ed. NIH Publications; Bethesda, MD, USA: 2003. [Google Scholar]
- 15.Won C.W., Yang K.Y., Rho Y.G., Kim S.Y., Lee E.J., Yoon J.L., Cho K.H., Shin H.C., Cho B.R., Oh J.R., et al. The Development of Korean Activities of Daily Living(K-ADL) and Korean Instrumental Activities of Daily Living(K-IADL) Scale. J. Korean Geriatr. Soc. 2002;6:107–120. [Google Scholar]
- 16.Dwyer J. Strategies to Detect and Prevent Malnutrition in the Elderly: The Nutrition Screening Initiative. Nutr. Today. 1994;29:14–24. doi: 10.1097/00017285-199409000-00004. [DOI] [Google Scholar]
- 17.Cho M.J., Bae J.N., Suh G.H., Hahm B.J., Kim J.K., Lee D.W., Kang M.H. Validation of Geriatric Depression Scale, Korean Version(GDS) in the Assessment of DSM-III-R Major Depression. J. Korean Neuropsychiatr. Assoc. 1999;38:48–63. [Google Scholar]
- 18.Rowland D., Lyons B. Medicare, Medicaid, and the elderly poor. Health Care Financ. Rev. 1996;18:61–85. [PMC free article] [PubMed] [Google Scholar]
- 19.Marmot M.G., Smith G.D., Stansfeld S., Patel C., North F., Head J., White I., Brunner E., Feeney A. Health inequalities among British civil servants: The Whitehall II study. Lancet. 1991;337:1387–1393. doi: 10.1016/0140-6736(91)93068-K. [DOI] [PubMed] [Google Scholar]
- 20.Mackenbach J.P., Kunst A.E., Cavelaars A.E., Groenhof F., Geurts J.J. Socioeconomic inequalities in morbidity and mortality in western Europe. The EU Working Group on Socioeconomic Inequalities in Health. Lancet. 1997;349:1655–1659. doi: 10.1016/S0140-6736(96)07226-1. [DOI] [PubMed] [Google Scholar]
- 21.Cavelaars A.E., Kunst A.E., Geurts J.J., Crialesi R., Grötvedt L., Helmert U., Lahelma E., Lundberg O., Matheson J., Mielck A., et al. Differences in self reported morbidity by educational level: A comparison of 11 western European countries. J. Epidemiol. Community Health. 1998;52:219–227. doi: 10.1136/jech.52.4.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ebrahimi Z., Wilhelmson K., Eklund K., Moore C.D., Jakobsson A. Health despite frailty: Exploring influences on frail older adults’ experiences of health. Geriatr. Nurs. 2013;34:289–294. doi: 10.1016/j.gerinurse.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 23.Seo Y.S. A Study on Health Behaviors and Health Status by Socioeconomic Status of Middle-Aged and Elderly. Graduate School of the Catholic University of Korea; Seoul, Korea: 2011. [Google Scholar]
- 24.Cho Y.H., Park Y.C. The Age, lifestyle and Health Status of the Elderly in a Small City. J. Korea Gerontol. Soc. 2003;23:141–153. [Google Scholar]
- 25.Liang Y., Welmer A.K., Wang R., Song A., Fratiglioni L., Qiu C. Trends in Incidence of Disability in Activities of Daily Living in Chinese Older Adults: 1993–2006. J. Am. Geriatr. Soc. 2017;65:306–312. doi: 10.1111/jgs.14468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arends J., Baracos V., Bertz H., Bozzetti F., Calder P.C., Deutz N.E.P., Erickson N., Laviano A., Lisanti M.P., Lobo D.N., et al. ESPEN expert group recommendations for action against cancer-related malnutrition. Clin. Nutr. 2017;36:1187–1196. doi: 10.1016/j.clnu.2017.06.017. [DOI] [PubMed] [Google Scholar]
- 27.Jung S.H. A Study on the Correlation between Social Support and Depressed in the Elderly: Analysis of the 2014 Survey of Living Conditions and Welfare Needs of Korean Older Persons. Graduate School of Public Health Yonsei University; Seoul, Korea: 2017. [Google Scholar]
- 28.Kim D.-B., Sohn E.-S. A Meta-analysis of the Variables Related to Depression in Elderly. J. Korean Gerontol. Soc. 2005;25:167–187. [Google Scholar]
- 29.Chon J.Y., Yee N.H. Depression in the Elderly for the Mediating Effect of Coping Strategies of Family Conflict. J. Korean Gerontol. Soc. 2011;31:1169–1187. [Google Scholar]
- 30.Lee H.J., Jung E.H. Socioeconomic Status and Elderly Health in Life Course Perspective: Testing of Multi-mediational Effects of Socioeconomic Status in Early Adult and Middle Aged. Health Soc. Welf. Rev. 2016;36:53–84. [Google Scholar]
- 31.Kim M.H., Lee G.Y., Chung S. A Path Analysis on Depression among the Elderly. J. Korean Gerontol. Soc. 2000;20:211–226. [Google Scholar]
- 32.WHO Commission on Social Determinants of Health, World Health Organization . Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health: Commission on Social Determinants of Health Final Report. World Health Organization; Geneva, Switzerland: 2008. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Our data are readily available upon reasonable request.