Abstract
Pediatric osteomyelitis remains challenging to treat. Detailed epidemiological data are required to estimate future developments. Therefore, we aimed to analyze how the incidence has changed over the last decade depending on age, gender, osteomyelitis subtype, and anatomical localization. Cases were quantified for patients aged 20 years or younger, using yearly reported ICD-10 diagnosis codes from German medical institutions for the time period 2009 to 2019. Incidence rates of osteomyelitis increased by 11.7% from 8.2 cases per 100,000 children in 2009 to 9.2 cases per 100,000 children in 2019. The age-specific incidence rate revealed the highest occurrence of osteomyelitis in patients aged 10–15 years (15.3/100,000 children), which increased by 23% over the observation period, followed by the age group 5–10 years (9.7/100,000 children). In 2019, out of all diagnoses, 39.2% were classified as acute, 38.4% as chronic, and 22.4% were unspecified, whereby chronic cases increased by 38.7%. The lower extremity was mainly affected, with 58.9% of osteomyelitis diagnoses in 2019. In conclusion, pediatric osteomyelitis is a serious issue, even in a developed and industrialized country such as Germany. Considering the recent incidence increase, the permanent need for appropriate treatment should let pediatricians and orthopedic surgeons deal with diagnosis and treatment protocols.
Keywords: osteomyelitis, bone infection, pediatrics, epidemiology
1. Introduction
Osteomyelitis is one of the most prevalent musculoskeletal infections in children. Bone infection is most commonly caused by Staphylococcus aureus and can occur as a hematogenous infection or after a direct inoculation of bacteria, for instance, due to surgery or open fractures [1,2]. Clinically, the management is challenging. Antibiotic treatment without surgical intervention is a feasible option in cases of acute osteomyelitis, which is regarded within 2 weeks after onset of symptoms. In chronic osteomyelitis, which is defined after more than 2 weeks after onset of symptoms, surgical treatments (including debridement and dead space management) are necessary to achieve eradication of infection [1]. Reliable data on the incidence of pediatric osteomyelitis is of great importance for the evaluation of advances in treatment approaches, prevention strategies, and future developments.
Recently, the epidemiology of osteomyelitis was described for the adult population in Germany, based on nationwide registry data. The authors reported an increase of 10.44% over the last decade and an incidence of 16.7 cases per 100,000 inhabitants for the year 2018 [3]. Some literature also provided insights in the epidemiology of osteomyelitis in pediatric patients [4,5]. However, no current data is available on the epidemiology of acute and chronic osteomyelitis for children in a European country.
Therefore, we analyzed nationwide registry data from Germany, the European country with the highest population numbers. Furthermore, the purpose of this study was to determine changes of pediatric osteomyelitis incidence rates between 2009 and 2019, depending on osteomyelitis subtype, anatomical region, age, and gender.
2. Materials and Methods
Data consisting of ICD-10 diagnosis codes, reported annually from German medical institutions, was provided by the Federal Statistical Office of Germany (Destatis) for the time period 2009 to 2019. These include all inpatient diagnoses, which are reported from medical institutions of all 16 German federal states, including private ones. Patients aged 20 years or younger diagnosed with osteomyelitis were identified using the ICD-10 code “M86.-”. The prevalence was estimated for gender, age groups in five-year increments, osteomyelitis subtype, and affected region, respectively. The subgroup “acute osteomyelitis” was composed by applying the ICD-10 codes “M86.0, M86.1, M86.2”; whereas, chronic osteomyelitis cases were estimated using the codes “M86.3, M86.4, M86.5, M86.6”. Unspecified osteomyelitis cases were determined by “M86.8, M86.9”. For the upper extremity, the subgroup the codes “-1, shoulder”, “-2, humerus”, “-3, radius and ulna”, and “-4, hand” were included. The lower extremity subgroup was compiled using the codes “-5, femur”, “-6, tibia and fibula” and “-7, ankle and foot”. The incidence rate was estimated based on Germany’s total population of those aged 20 years or younger for each year provided by Destatis [6]. Data were analyzed with SPSS Version 26.0 (IBM, SPSS Inc., Armonk, NY, USA).
3. Results
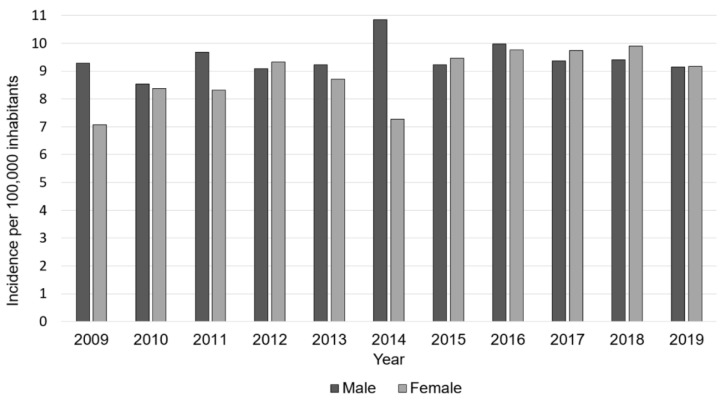
In 2019, 1486 osteomyelitis cases in the German population aged younger than 20 years were registered. Compared to 1336 cases in 2009, the incidence increased by 11.7%, from 8.2 cases per 100,000 inhabitants to 9.2 cases per 100,000 inhabitants. Since 2009, total numbers steadily increased, reaching a maximum in 2016, followed by a subsequent decrease of diagnoses. Over the years, male cases were slightly more often reported than female cases; whereas, the gender distribution was equal in 2019 (Table 1, Figure 1).
Table 1.
Pediatric osteomyelitis incidence changes between 2009 and 2019.
| Year | Total Numbers | Incidence per 100,000 Children | Relative to 2009 [%] | Ratio Male/Female [%] |
|---|---|---|---|---|
| 2009 | 1336 | 8.2 | 53/47 | |
| 2010 | 1314 | 8.5 | +3.0 | 58/42 |
| 2011 | 1333 | 9.0 | +9.8 | 52/48 |
| 2012 | 1417 | 9.2 | +12.1 | 55/45 |
| 2013 | 1380 | 9.0 | +9.4 | 51/49 |
| 2014 | 1409 | 9.1 | +10.99 | 53/47 |
| 2015 | 1475 | 9.3 | +13.8 | 61/39 |
| 2016 | 1581 | 9.9 | +20.3 | 51/49 |
| 2017 | 1545 | 9.6 | +16.4 | 52/48 |
| 2018 | 1560 | 9.6 | +17.4 | 51/49 |
| 2019 | 1486 | 9.2 | +11.7 | 50/50 |
Figure 1.
Development of osteomyelitis incidence from 2009 to 2019, divided by gender. The light grey bars present the incidence of male cases, and the dark grey bars present the incidence of female cases.
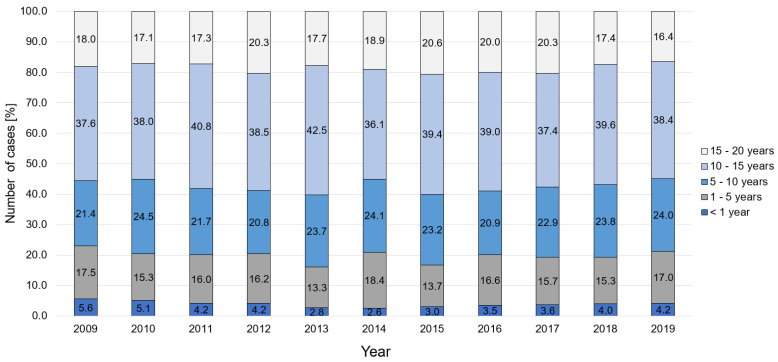
Regarding the internal infection proportion, most patients were aged 10–15 years (38.4%), followed by patients aged 5–10 years (24.0%) and patients aged 1–5 years (17.0%) in 2019 (Figure 2). The age-specific incidence rate per 100,000 children revealed the highest occurrence of osteomyelitis in patients aged 10–15 years (15.3/100,000 children), which increased by 23% over the observation period. The second most affected group were children aged 5–10 years, with an incidence rate of 9.7/100,000 children; whereby, cases increased by 25.3% in the last decade. This was followed by an incidence of 8.1/100,000 children aged younger than 1 year; whereby, less children were diagnosed with osteomyelitis in comparison to 2009 (−25.9%). Additionally, for children aged 1–5 years, the incidence decreased by 5.6%, to 6.4 cases/100,000 children (Table 2).
Figure 2.
Age-dependent changes in incidence of osteomyelitis cases.
Table 2.
Historic development of age-specific incidence rate, per 100,000 children.
| Year | <1 Year Old | 1–5 Years Old | 5–10 Years Old | 10–15 Years Old | 15–20 Years Old |
|---|---|---|---|---|---|
| 2009 | 11.0 | 6.7 | 7.7 | 12.5 | 5.5 |
| 2010 | 10.0 | 6.0 | 9.2 | 12.8 | 5.5 |
| 2011 | 8.8 | 6.6 | 8.7 | 14.0 | 6.0 |
| 2012 | 8.9 | 6.8 | 8.5 | 14.3 | 7.1 |
| 2013 | 5.6 | 5.4 | 9.4 | 15.7 | 6.0 |
| 2014 | 5.0 | 7.4 | 9.7 | 13.7 | 6.6 |
| 2015 | 6.0 | 5.6 | 9.6 | 15.8 | 7.3 |
| 2016 | 7.1 | 7.0 | 9.2 | 16.7 | 7.6 |
| 2017 | 7.1 | 6.4 | 9.7 | 15.6 | 7.4 |
| 2018 | 7.9 | 6.1 | 10.1 | 16.6 | 6.5 |
| 2019 | 8.1 | 6.4 | 9.7 | 15.3 | 6.0 |
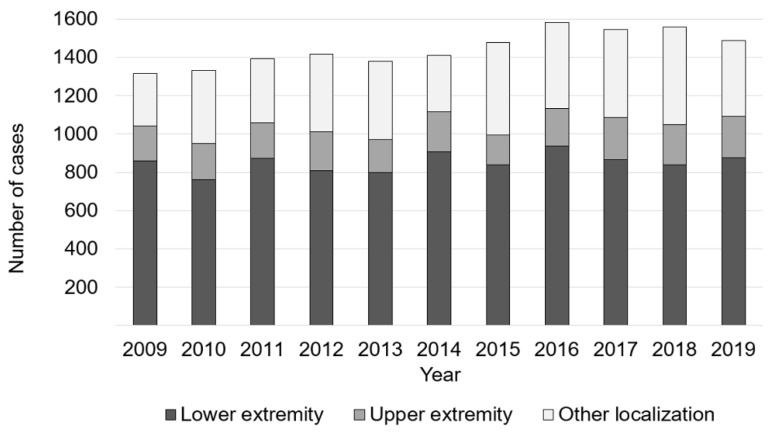
The lower extremity was the most frequently infected region, with 58.9% in 2019. Here, the number of cases increased from 816 in 2009 to 875 in 2019. In 14.7% of all cases bone, infection was present at the upper extremity. Other anatomical localizations were affected in 26.4% (Figure 3).
Figure 3.
Anatomical region dependent changes osteomyelitis cases.
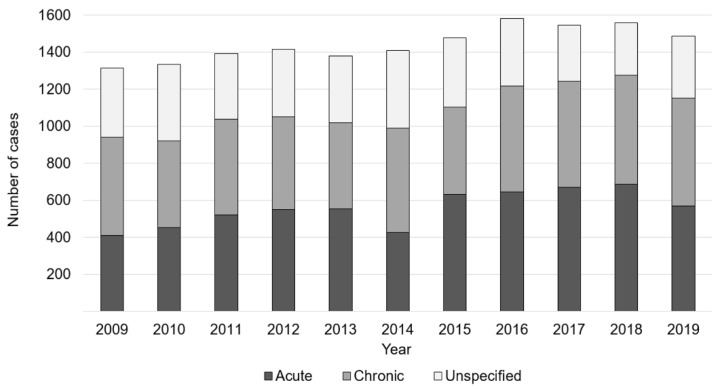
In 2019, out of all diagnoses, 39.2% were classified as acute, 38.4% as chronic, and 22.4% were unspecified. Cases which were classified as acute increased by 10.2%, from 529 to 583 between 2009 and 2019. Additionally, chronic osteomyelitis cases rose by 38.7%, from 411 to 570 cases; whereas, unspecified osteomyelitis diagnoses declined by 11.0%, from 374 to 333 (Figure 4).
Figure 4.
Development of osteomyelitis prevalence, classified as acute, chronic, and unspecified.
4. Discussion
In this cross-sectional study, developments of the epidemiology of pediatric osteomyelitis were analyzed for osteomyelitis subtype, anatomical localization, gender, and age group, respectively. The results show that the annual incidence increased by 11.7%, to 9.2 cases per 100,000 children. The incidence is comparable to other studies. For instance, the incidence rate of non-vertebral osteomyelitis was calculated as 10/100,000 children in Norway [4] and 7.8–9.1/100,000 children in South Korea [7]. However, country-specific differences are also evident. A ten year retrospective review of pediatric osteomyelitis treatment in two orthopedic departments in New Zealand reported an annual rate of 1:4000 for acute hematogenous in patients aged 0–15; whereby, the incidence declined over the years [8]. In the U.S., hospitalization rates ranged from 1.34 to 1.66/100,000 children for acute osteomyelitis, which is less than estimated for Germany [5]. Among the countries, osteomyelitis incidence in indigenous children of northern Australia was the highest reported globally, with rates of 82 per 100,000 children, compared to 9 per 100,000 for nonindigenous children [9]. Where some authors report decreases in incidence [10], others report an increasing incidence [11], which could partly reflect advances in microbiological diagnosis [12,13]. Here, the age-specific incidence rates of osteomyelitis showed decreasing trends among children aged <1 year; whereas, the incidence rates increased among children aged >5 years. This was in contrast to other studies, reporting more cases in children aged <3 years, compared with older children under the age of 16 years (OR 2.9, 95%: CI 2.3–3.7) [4]. The study further shows that gender distribution was equal, which is consistent with findings from studies performed in countries such as Norway [4]. However, other publications reported more frequent osteomyelitis diagnoses in males than in females [11,14]. In the reported data, the lower extremity was more often affected, which is consistent with the literature, reporting the highest infection rates for the femur and tibia [15]. In addition, out of all diagnoses, 39.2% were classified as acute, 38.4% as chronic, and 22.4% were unspecified in 2019. The widely used classification by Waldvogel and colleagues distinguishes between acute and chronic; whereby, acute osteomyelitis is defined by symptoms for a duration of less than two weeks [1]. However, different definitions exist in the literature [16], which might influence the presented statistics and results in potential misclassification of acute and chronic diagnoses. Furthermore, chronic cases heightened by 38.7% over the years. Hence, early diagnosis, advances in prevention strategies, and prompt treatment are of fundamental importance, as a mature biofilm limits the susceptibility to antibiotics, leading to a requirement of surgical treatment [17].
The biggest limitation of this study is due to the fact that the analysis was solely based on inpatient data. However, surgical treatment is required in the majority of osteomyelitis cases. Furthermore, the analysis of ICD-10 codes does not allow to distinguish between hematogenous and postoperative infections, or to determine possible driving comorbidity factors, such as immune deficiencies or fractures. In the same stance, it was not possible to derive information about the underlying pathogens and treatment procedures. Finally, correct coding cannot be assured.
5. Conclusions
In conclusion, pediatric osteomyelitis remains a challenge even in a developed and industrialized country such as Germany. Considering the recent incidence increase, the permanent need for appropriate treatment should let pediatricians and orthopedic surgeons deal with diagnosis and treatment protocols, to maintain and further improve the treatment for our young patients.
Acknowledgments
We thank the Federal Statistical Office of Germany (Destatis) for their support of this work.
Author Contributions
Conceptualization, N.W. and M.R.; methodology, N.W., S.B., V.A. and M.R.; validation, V.A. and M.R.; formal analysis, N.W. and S.B.; investigation, N.W.; writing—original draft preparation, N.W.; writing—review and editing, N.W., S.B, V.A. and M.R.; visualization, N.W.; supervision, M.R. and V.A.; project administration, M.R. and V.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki. Approval was waived by the Ethics Committee of the University Hospital Regensburg.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Waldvogel F.A., Medoff G., Swartz M.N. Osteomyelitis: A review of clinical features, therapeutic considerations and unusual aspects. N. Engl. J. Med. 1970;282:198–206. doi: 10.1056/NEJM197001222820406. [DOI] [PubMed] [Google Scholar]
- 2.Congedi S., Minotti C., Giaquinto C., Da Dalt L., Donà D. Acute infectious osteomyelitis in children: New treatment strategies for an old enemy. World J. Pediatr. 2020;16:446–455. doi: 10.1007/s12519-020-00359-z. [DOI] [PubMed] [Google Scholar]
- 3.Walter N., Baertl S., Alt V., Rupp M. What is the burden of osteomyelitis in Germany? An analysis of inpatient data from 2008 through 2018. BMC Infect. Dis. 2021;21:550. doi: 10.1186/s12879-021-06274-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Riise Ø.R., Kirkhus E., Handeland K.S., Flatø B., Reiseter T., Cvancarova M., Nakstad B., Wathne K.-O. Childhood osteomyelitis-incidence and differentiation from other acute onset musculoskeletal features in a population-based study. BMC Pediatr. 2008;8:45. doi: 10.1186/1471-2431-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Okubo Y., Nochioka K., Testa M. Nationwide survey of pediatric acute osteomyelitis in the USA. J. Pediatr. Orthop. B. 2017;26:501–506. doi: 10.1097/BPB.0000000000000441. [DOI] [PubMed] [Google Scholar]
- 6.Statistisches Bundesamt (Destatis) [(accessed on 2 May 2021)]. Available online: http://www-genesis.destatis.de/genesis/online.
- 7.Kim J., Lee M.U., Kim T.-H. Nationwide epidemiologic study for pediatric osteomyelitis and septic arthritis in South Korea: A cross-sectional study of national health insurance review and assessment service. Medicine. 2019;98:e15355. doi: 10.1097/MD.0000000000015355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Street M., Puna R., Huang M., Crawford H. Pediatric Acute Hematogenous Osteomyelitis. J. Pediatr. Orthop. 2015;35:634–639. doi: 10.1097/BPO.0000000000000332. [DOI] [PubMed] [Google Scholar]
- 9.Brischetto A., Leung G., Marshall C.S., Bowen A.C. A Retrospective Case-Series of Children With Bone and Joint Infection From Northern Australia. Medicine. 2016;95:e2885. doi: 10.1097/MD.0000000000002885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blyth M.J., Kincaid R., Craigen M.A., Bennet G.C. The changing epidemiology of acute and subacute haematogenous osteomyelitis in children. J. Bone Joint Surg. Br. 2001;83:99–102. doi: 10.1302/0301-620X.83B1.0830099. [DOI] [PubMed] [Google Scholar]
- 11.Malcius D., Trumpulyte G., Barauskas V., Kilda A. Two decades of acute hematogenous osteomyelitis in children: Are there any changes? Pediatr. Surg. Int. 2005;21:356–359. doi: 10.1007/s00383-005-1432-7. [DOI] [PubMed] [Google Scholar]
- 12.Iliadis A.D., Ramachandran M. Paediatric bone and joint infection. EFORT Open Rev. 2017;2:7–12. doi: 10.1302/2058-5241.2.160027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thomsen I., Creech C.B. Advances in the diagnosis and management of pediatric osteomyelitis. Curr. Infect. Dis. Rep. 2011;13:451–460. doi: 10.1007/s11908-011-0202-z. [DOI] [PubMed] [Google Scholar]
- 14.Grammatico-Guillon L., Maakaroun Vermesse Z., Baron S., Gettner S., Rusch E., Bernard L. Paediatric bone and joint infections are more common in boys and toddlers: A national epidemiology study. Acta Paediatr. 2013;102:e120-5. doi: 10.1111/apa.12115. [DOI] [PubMed] [Google Scholar]
- 15.Peltola H., Pääkkönen M. Acute osteomyelitis in children. N. Engl. J. Med. 2014;370:352–360. doi: 10.1056/NEJMra1213956. [DOI] [PubMed] [Google Scholar]
- 16.Masters E.A., Trombetta R.P., Mesy Bentley K.L., de Boyce B.F., Gill A.L., Gill S.R., Nishitani K., Ishikawa M., Morita Y., Ito H., et al. Evolving concepts in bone infection: Redefining “biofilm”, “acute vs. chronic osteomyelitis”, “the immune proteome” and “local antibiotic therapy”. Bone Res. 2019;7:20. doi: 10.1038/s41413-019-0061-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cierny G., Mader J.T., Penninck J.J. A clinical staging system for adult osteomyelitis. Clin. Orthop. Relat. Res. 2003:7–24. doi: 10.1097/01.blo.0000088564.81746.62. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.