Abstract
The first purpose of this study was to verify the association between Instability Severity Index Score (ISIS) and Recurrent Shoulder Dislocation (RSD) after a first episode treated conservatively. The second aim is to identify the risk factors associated with RSD after a primary acute shoulder anterior dislocation treated conservatively. A total of 111 patients with first traumatic anterior shoulder dislocation treated at a single trauma centre between January 2014 and March 2016 were enrolled. The main predictive variables of risk factors and the ISIS score were calculated. Among the 85 patients included, 26 cases of RSD were observed (30.6%). Considering the whole population, no significant association between ISIS and RSD were reported. Regarding other risk factors, high-risk working activities and rotator cuff injury had a significantly higher RSD risk. Sex, dominant limb, familiar history, hyperlaxity, contact or overhead sports, competitive sport, post-reduction physiokinesitherapy, return to sports activity time, Hill-Sachs lesion, bony Bankart lesion and great tuberosity fracture did not seem to influence the risk of RSD. No correlation between ISIS score and RSD in patients treated conservatively after a first episode of shoulder dislocation were reported. The only risk factors with a significant association to RSD were high-risk working activities and rotator cuff injury.
Keywords: shoulder instability, Instability Severity Index, shoulder dislocation, ISIS, conservative, surgery, predictivity, recurrent dislocation, risk factor
1. Introduction
The shoulder is the most frequently dislocated joint in the human body. A complete pop out of the humeral head from the glenoid socket is defined as dislocation [1]. The inability of bone and ligamentous structures of the shoulder joint to maintain the humeral head in the glenoid fossa, could cause a condition known as “shoulder instability” [2].
The incidence of shoulder dislocation is estimated between 11 and 51 cases per 100,000 individuals per year [3,4,5], but it is highly variable, as it depends on the population studied. The rate is significantly higher when considering an active population such as the military or athletes [4,5]. Anterior traumatic dislocation is the most frequent type, representing about 96% of all glenohumeral dislocations [6]. Immediate joint reduction and immobilization, followed by rehabilitation, is the most common conservative treatment for primary anterior dislocations. Surgical treatment, however, is generally used in case of recurrence or chronic instability [7]. In the literature, Recurrent Shoulder Dislocation (RSD) following a first traumatic episode ranges from 26% [8] to 92% [9,10].
Young age, male sex [11], and contact sports [12] seem to increase the risk of instability after a primary anterior dislocation, but other studies reported discordant findings [13]. Other risk factors are the type of trauma [14], constitutional hyperlaxity [15], and the presence of a Hill-Sachs lesion on radiography [16].
The Instability Severity Index Score (ISIS) score was created to guide the surgeon’s decision identifying patients with a high risk of RSD after an arthroscopic Bankart surgery [17]. The risk factors considered by this score are age at surgery, glenoid loss of contour on AP radiograph, Hill-Sachs lesion on external rotation anteroposterior (AP) radiograph, degree of sports participation, type of sport and shoulder hyperlaxity [17]. Although ISIS and other scores have tried to assess the risk of RSD after surgery, limited findings are reported on risk factors for RSD after a first episode of dislocation treated conservatively [13,14].
The first purpose of this study is to verify the association between ISIS and RSD after a first episode treated conservatively. The second aim is to identify the risk factors associated with RSD after a primary acute shoulder anterior dislocation treated conservatively.
2. Materials and Methods
2.1. Participants and Setting
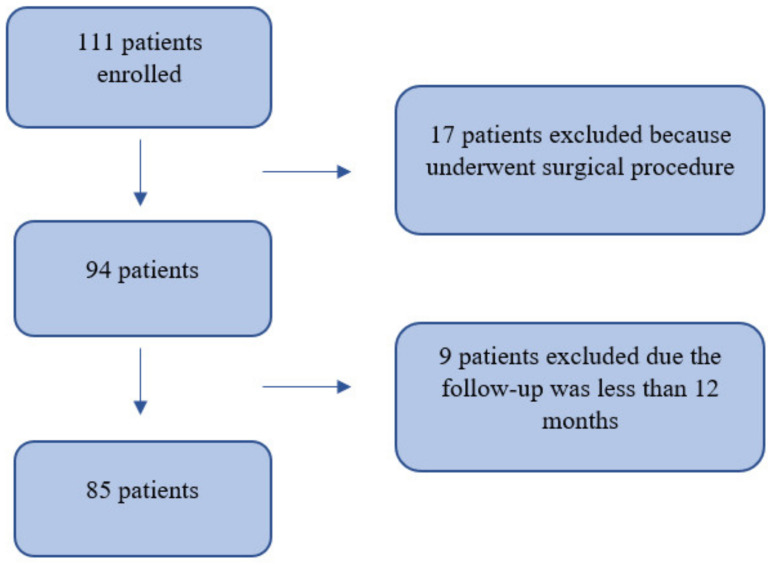
Between January 2014 and March 2016, 111 patients with first traumatic anterior shoulder dislocation treated at a single trauma centre were enrolled. A total of 17 patients were excluded because they underwent a surgical procedure, while 9 patients were excluded due having a follow-up less than 12 months. Therefore, 85 patients were included in this study (Figure 1). The inclusion and exclusion criteria are summarized in Table 1. RSD is defined according to Hobby et al. as “radiological documentation of further dislocation, recurrence of dislocation by re-injury requiring manual reduction, recurrence of symptoms of the shoulder “popping out” or “slipping out” in a position of abduction and external rotation suggestive of subluxation, or symptomatic subluxation or instability preventing the return to full activity [18,19].
Figure 1.
Flow chart.
Table 1.
Inclusion and exclusion criteria.
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
All patients were treated with immobilization using a sling with the arm held in external rotation, neutral flexion, and 15° of abduction for four weeks [20]. All patients were recommended the same physiokinesitherapy; after four weeks of immobilization, active-assisted shoulder range of motion exercises, avoiding elevation or abduction of >90° or external rotation of >30°; after twelve weeks, free range of motion; isometric rotator cuff strengthening exercises at six weeks, and the isotonic exercises at twelve weeks. According to the selection criteria, 94 patients were included in the study. Two orthopaedic surgeons interviewed the patients. Two experienced radiologists viewed X-ray and MRI examinations of the affected shoulder of inclusion patients. In case of controversy, a discussion between the radiologist and the senior orthopaedic surgeon solved the conflicts. The Institutional Review Board (IRB) approved the study before data collection. The mean follow-up time was considered as time elapsed since the injury and the moment of the interview.
2.2. Data Collection
The main predictive variables, including age, gender, affected side, dominant arm, family history of dislocations and hyperlaxity (hyperlaxity is a physiological condition characterized with increased range of motion of various joints of an individual [21]), were recorded during a clinical examination. Patients were divided into two groups accordingly to their working activity, high-risk jobs, and non-high-risk jobs (Table 2). The sports activity practised, and the level (competitive or non-competitive) was recorded and divided into two main types, sports that require contact or overhead force and other sports. The eventual post-reduction physiokinesitherapy performed and the time to return to sports (expressed in months) were reported. Associated injuries such as Hill-Sachs, Bony Bankart, rotator cuff injury, or greater tuberosity fracture were assessed on X-rays and MRI. According to the University of California Los Angeles Shoulder Scale (UCLA) [22] all patients were evaluated for pain and function. Moreover, The Short Shoulder Test (SST) [23] and the Shoulder Pain and Disability Index (SPADI) [24] functional scales were assessed. The ISIS [17] was calculated by the senior surgeon after the first episode of shoulder dislocation. In Table 2, all variables included in this study are described.
Table 2.
Descriptive statistical analyses, frequencies and means of variables included.
| Age | Mean age: 40 ± 14.7 (range 18–65 years) |
| Gender | Males = 67, Females = 18 |
| Affected side | Right = 60, Left = 25 |
| Dominant arm | Yes = 57, No = 28 |
| Family history of dislocations | Yes = 0, No = 85 |
| Hyperlaxity | Yes = 2, No = 83 |
| Working activity | High-risk jobs (paratrooper, bricklayer, military, police, mechanic, jockey, warehouse worker) = 15; Non-high-risk jobs (painter, housewife, pensioner, pharmacist, engineer, waiter, student, driver, fisherman, chef, employee, doctor, computer scientist, trader, hairdresser) = 70 |
| Sports activity practised | Sports that require contact or overhead forced (basket, soccer, martial arts, weightlifting, bodybuilding, rugby, military, tennis, motorbike, swimming and volleyball) = 39; Other sports (fitness exercise, cycling, horseback riding, jogging, skiing, immersion, athletics) = 46 |
| Level of sport | No sport = 29, Non-Competitive = 46, Competitive = 10 |
| Post-reduction physiokinesitherapy | Yes = 52, No = 33 |
| Time to return to sports | From 1 to 8 months |
| Hill-Sachs | Yes = 14, No = 71 |
| Bony Bankart | Yes = 5, No = 80 |
| Rotator cuff injury | Yes = 17, No = 68 |
| Greater tuberosity fracture | Yes = 3, No = 82 |
| UCLA Score | Mean score: 17.4 ± 3.5 |
| SST Score | Mean score: 9.2 ± 18.1 |
| SPADI Score | Mean score: 84.7 ± 26.4 |
| ISIS Score | Score 0–2 = 65, score 3–6 = 19, score > 6 = 1 |
2.3. Statistical Analysis
A priori power analysis was conducted to assess the minimum number of patients required for the study. Assuming a recurred dislocation after conservative treatment of 37.5% as in literature [7], an effect size of 0.2, using α = 0.05, power of 80% and a two-tailed test, a sample size of 52 patients was required.
Data were collected in Microsoft Excel. To assess data normality the Shapiro–Wilk test was used. To determine the statistical differences in the months of follow-up between RDS and not RDS, an independent t-test was used. A binary logistic regression model was used to study the correlations between risk factors, ISIS and the presence of RSD. Demographic data were calculated as descriptive variables using frequencies, means and standard deviation (SD). The statistical analysis was conducted using IBM SPSS (v 26) software (IBM, Armonk, NY, USA). A p-value ≤ 0.05 was considered as significative.
3. Results
A cohort of 85 patients with a first episode of anterior shoulder dislocation was enrolled for this study (67 males and 18 females), with a mean age of 40 ± 14.7 (range 18–65 years old). Of these, 60 patients were injured at the right shoulder instead of 25 at the left shoulder. The first episode of shoulder dislocation occurred in 57 cases in the dominant limb (55 right shoulders; 2 left shoulders). The mean follow-up (intended as time elapsed since the first episode) was 48.1 ± 25.7 months (range 12–156 months). Among the 85 patients included, 26 cases of RSD were observed (30.6%). All descriptive statistical analyses were presented in Table 2.
No statistically significant association between ISIS and RSD were reported (p = 0.4, Table 3).
Table 3.
Variables associated with the presence of RSD, analysed using binary regression logistic model.
| Variables | p-Value |
|---|---|
| ISIS | 0.441 |
| High-risk working activities | 0.024 * |
| Rotator cuff injury | <0.001 * |
| Contact or overhead sports | 0.127 |
| Sex | 0.389 |
| Age | 0.435 |
| Dominant limb | 0.777 |
| Familiar history | N/A |
| Hyperlaxity | 0.577 |
| Competitive sport | 0.383 |
| Post-reduction physiokinesitherapy | 0.180 |
| Return to sports activity time | 0.977 |
| Hill-Sachs lesion | 0.252 |
| Bony_Bankart lesion | 0.999 |
| Great tuberosity fracture | 0.999 |
| UCLA Score | 0.369 |
| SPADI Score | 0.879 |
| SST Score | 0.806 |
* Statistically significant, NA = Not Applicable.
Regarding other risk factors, patients who sustained high-risk working activities had an Odds Ratio (OR) of 4.3 (95%CI = [1.2, 15.5]; p = 0.02) compared to other patients. In patients with a rotator cuff injury the OR was 10.8 (95%CI = [3.1, 37.9]; p < 0.001) compared to other patients.
Concerning other variables (sex, dominant limb, familiar history, hyperlaxity, contact or overhead sports, competitive sport, post-reduction physiokinesitherapy, return to sports activity time, Hill-Sachs lesion, Bony Bankart lesion, greater tuberosity fracture, UCLA Score, SPADI Score, SST Score) no significant association were found. Only 52/85 (61.2%) of the patients undertook physiokinesitherapy after the first episode of dislocation.
A statistically significant difference in average months of follow-up between the group with and without recurrence of dislocation was found (p = 0.04). The mean months of follow-up in RDS group was 59 ± 33.8, while in the not RDS group 43.4 ± 19.7 months.
4. Discussion
The main findings of this study are that among the 85 patients analysed, RSD after a first episode of shoulder dislocation treated conservatively were reported in 30.6% of cases. ISIS was analysed, and no significant association with the risk of RSD was reported.
4.1. Predictivity of ISIS for RSD
Balg and Boileau [17] developed the ISIS score to evaluate the preoperative risk of recurrent instability after an arthroscopic repair, based on six risk factors. They found a 70% risk of RSD after surgery in case of ISIS > 6 points [17]. Phadnis et al. [25] questioned the real efficacy of ISIS, emphasizing the potential advantages and disadvantages. They concluded that even with the lower value of ISIS (score > 4) there is a 70% risk of RSD, in opposition to the results of Balg [17]. There is a lack of literature concerning the use of ISIS in patients treated conservatively. In this study, a possible association between ISIS and RSD after a first episode of dislocation treated conservatively was evaluated. Otherwise, no statically significant association between ISIS (assessed after the first episode of dislocation) and further RSD were founded (neither stratifying the population by age, as reported in Table 3). Other scores such as UCLA, SPADI and SST were analysed, but no significant association with RSD was found. These scores assess shoulder pain and functionality; instead, ISIS investigate the risk of RSD. Therefore, the lack of correlation between UCLA, SPADI, SST and ISIS could be explained by the different aims of the scores. The risk factors that constitute the ISIS were individually analysed.
4.2. Risk Factors of RSD after a First Episode Treated Conservatively
Different studies [26,27,28] have focused on risk factors for RSD identifying the following variables: age, high-risk working activities, rotator cuff injury, contact or overhead sports, sex, trauma on the dominant limb, familiar history, hyperlaxity [29], competitive sport, post-reduction physiokinesitherapy, return to sports activity time, Hill-Sachs lesion [30], Bony Bankart lesion [31] and great tuberosity fracture. Olds et al. [32] identified 39% of the rate of RSD after one year from the first episode of dislocation. In our study of 85 patients, only 26 (30.6%) experienced RSD. This value is lower than other studies [33], because only patients treated conservatively were included in the analysis. Otherwise, in a systematic review of 2014 [7] the rate of RSD for patients treated conservatively was 37.5%, similar to the results of this study.
The second aim of this paper was to identify risk factors for RSD after a first episode of dislocation treated conservatively. Comparing patients with and without RSD, only two parameters were found to be statistically significant. High-risk working activities showed a significant association with RSD (p = 0.02). This could probably be due to the repeated stresses and traumas on the shoulder that increase the risk of recurrence. Moreover, a previous rotator cuff injury seems to have a significant association with RSD (p < 0.001).
Surprisingly, sex, dominant limb, familiar history, hyperlaxity, competitive sport, post-reduction physiokinesitherapy, return to sports activity time, Hill-Sachs lesion, bony Bankart lesion and great tuberosity fracture did not have a significant association with the risk of RSD.
4.3. Limitations
This study has some limitations. Physiokinesitherapy was prescribed to all the patients with specific indications, but we were not certain how it was performed. Moreover, only 60.6% of patients included in the study performed physiokinesitherapy.
Lastly, the strength of this study is that it was conducted only on patients affected by anterior dislocation, demonstrating the selectivity of the results obtained.
5. Conclusions
No correlation between the ISIS score and RSD in patients treated conservatively after a first episode of shoulder dislocation were reported. The only risk factors with a significant association to RSD were high-risk working activities and rotator cuff injury. Sex, dominant limb, familiar history, hyperlaxity, competitive sport, post-reduction physiokinesitherapy, return to sports activity time, Hill-Sachs lesion, bony Bankart lesion and great tuberosity fracture did not seem to influence the risk of RSD. An evaluation of the UCLA, SPADI and SST score was performed, and no significant association was found. Further studies with a higher number of patients are needed to confirm the data obtained.
Author Contributions
Conceptualization, U.G.L. and S.D.S.; methodology, R.P.; software, I.P.; validation, U.G.L., P.P. and V.D.; formal analysis, I.P.; investigation, G.C.; resources, C.C.; data curation, I.P.; writing—original draft preparation, S.D.S.; writing—review and editing, F.C.; visualization, E.F.; supervision, V.D.; project administration, U.G.L., M.N. and M.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of University Campus Bio-Medico of Rome.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to the privacy.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Abrams R., Akbarnia H. StatPearls. StatPearls Publishing; Treasure Island, FL, USA: 2021. Shoulder Dislocations Overview. [PubMed] [Google Scholar]
- 2.Johnson D.J., Tadi P. StatPearls. StatPearls Publishing; Treasure Island, FL, USA: 2021. Multidirectional Shoulder Instability. [PubMed] [Google Scholar]
- 3.Hindle P., Davidson E.K., Biant L.C., Court-Brown C.M. Appendicular Joint Dislocations. Injury. 2013;44:1022–1027. doi: 10.1016/j.injury.2013.01.043. [DOI] [PubMed] [Google Scholar]
- 4.Owens B.D., Agel J., Mountcastle S.B., Cameron K.L., Nelson B.J. Incidence of Glenohumeral Instability in Collegiate Athletics. Am. J. Sports Med. 2009;37:1750–1754. doi: 10.1177/0363546509334591. [DOI] [PubMed] [Google Scholar]
- 5.Zacchilli M.A., Owens B.D. Epidemiology of Shoulder Dislocations Presenting to Emergency Departments in the United States. J. Bone Jt. Surg. Am. 2010;92:542–549. doi: 10.2106/JBJS.I.00450. [DOI] [PubMed] [Google Scholar]
- 6.Goss T.P. Anterior Glenohumeral Instability. Orthopedics. 1988;11:87–95. doi: 10.3928/0147-7447-19880101-10. [DOI] [PubMed] [Google Scholar]
- 7.Longo U.G., Loppini M., Rizzello G., Ciuffreda M., Maffulli N., Denaro V. Management of Primary Acute Anterior Shoulder Dislocation: Systematic Review and Quantitative Synthesis of the Literature. Arthroscopy. 2014;30:506–522. doi: 10.1016/j.arthro.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 8.Te Slaa R.L., Wijffels M.P.J.M., Brand R., Marti R.K. The Prognosis Following Acute Primary Glenohumeral Dislocation. J. Bone Jt. Surg. Br. 2004;86:58–64. doi: 10.1302/0301-620X.86B1.13695. [DOI] [PubMed] [Google Scholar]
- 9.Murray I.R., Ahmed I., White N.J., Robinson C.M. Traumatic Anterior Shoulder Instability in the Athlete. Scand. J. Med. Sci Sports. 2013;23:387–405. doi: 10.1111/j.1600-0838.2012.01494.x. [DOI] [PubMed] [Google Scholar]
- 10.Postacchini F., Gumina S., Cinotti G. Anterior Shoulder Dislocation in Adolescents. J. Shoulder Elb. Surg. 2000;9:470–474. doi: 10.1067/mse.2000.108385. [DOI] [PubMed] [Google Scholar]
- 11.Robinson C.M., Dobson R.J. Anterior Instability of the Shoulder after Trauma. J. Bone Jt. Surg. Br. 2004;86:469–479. doi: 10.1302/0301-620X.86B4.15014. [DOI] [PubMed] [Google Scholar]
- 12.Sachs R.A., Lin D., Stone M.L., Paxton E., Kuney M. Can the Need for Future Surgery for Acute Traumatic Anterior Shoulder Dislocation Be Predicted? J. Bone Jt. Surg. Am. 2007;89:1665–1674. doi: 10.2106/00004623-200708000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Hovelius L., Olofsson A., Sandström B., Augustini B.-G., Krantz L., Fredin H., Tillander B., Skoglund U., Salomonsson B., Nowak J., et al. Nonoperative Treatment of Primary Anterior Shoulder Dislocation in Patients Forty Years of Age and Younger. a Prospective Twenty-Five-Year Follow-Up. J. Bone Jt. Surg. Am. 2008;90:945–952. doi: 10.2106/JBJS.G.00070. [DOI] [PubMed] [Google Scholar]
- 14.Cox C.L., Kuhn J.E. Operative versus Nonoperative Treatment of Acute Shoulder Dislocation in the Athlete. Curr. Sports Med. Rep. 2008;7:263–268. doi: 10.1249/JSR.0b013e318186d26d. [DOI] [PubMed] [Google Scholar]
- 15.Chahal J., Leiter J., McKee M.D., Whelan D.B. Generalized Ligamentous Laxity as a Predisposing Factor for Primary Traumatic Anterior Shoulder Dislocation. J. Shoulder Elb. Surg. 2010;19:1238–1242. doi: 10.1016/j.jse.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 16.Hovelius L., Augustini B.G., Fredin H., Johansson O., Norlin R., Thorling J. Primary Anterior Dislocation of the Shoulder in Young Patients. A Ten-Year Prospective Study. J. Bone Jt. Surg. Am. 1996;78:1677–1684. doi: 10.2106/00004623-199611000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Balg F., Boileau P. The Instability Severity Index Score. A Simple Pre-Operative Score to Select Patients for Arthroscopic or Open Shoulder Stabilisation. J. Bone Jt. Surg. Br. 2007;89:1470–1477. doi: 10.1302/0301-620X.89B11.18962. [DOI] [PubMed] [Google Scholar]
- 18.Gao B., Gao W., Chen C., Wang Q., Lin S., Xu C., Huang D., Su P. What Is the Difference in Morphologic Features of the Thoracic Pedicle Between Patients with Adolescent Idiopathic Scoliosis and Healthy Subjects? A CT-Based Case-Control Study. Clin. Orthop. Relat. Res. 2017;475:2765–2774. doi: 10.1007/s11999-017-5448-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hobby J., Griffin D., Dunbar M., Boileau P. Is Arthroscopic Surgery for Stabilisation of Chronic Shoulder Instability as Effective as Open Surgery? A Systematic Review and Meta-Analysis of 62 Studies Including 3044 Arthroscopic Operations. J. Bone Jt. Surg. Br. 2007;89:1188–1196. doi: 10.1302/0301-620X.89B9.18467. [DOI] [PubMed] [Google Scholar]
- 20.Itoi E., Hatakeyama Y., Sato T., Kido T., Minagawa H., Yamamoto N., Wakabayashi I., Nozaka K. Immobilization in External Rotation after Shoulder Dislocation Reduces the Risk of Recurrence. A Randomized Controlled Trial. J. Bone Jt. Surg. Am. 2007;89:2124–2131. doi: 10.2106/00004623-200710000-00004. [DOI] [PubMed] [Google Scholar]
- 21.ESSKA . In: 360° around Shoulder Instability. Brzóska R., Milano G., Randelli P.S., Kovačič L., editors. Springer; Berlin/Heidelberg, Germany: 2020. [Google Scholar]
- 22.Ellman H., Hanker G., Bayer M. Repair of the Rotator Cuff. End-Result Study of Factors Influencing Reconstruction. J. Bone Jt. Surg. Am. 1986;68:1136–1144. doi: 10.2106/00004623-198668080-00002. [DOI] [PubMed] [Google Scholar]
- 23.Roy J.-S., Macdermid J.C., Faber K.J., Drosdowech D.S., Athwal G.S. The Simple Shoulder Test Is Responsive in Assessing Change Following Shoulder Arthroplasty. J. Orthop. Sports Phys. Ther. 2010;40:413–421. doi: 10.2519/jospt.2010.3209. [DOI] [PubMed] [Google Scholar]
- 24.Roach K.E., Budiman-Mak E., Songsiridej N., Lertratanakul Y. Development of a Shoulder Pain and Disability Index. Arthritis Care Res. 1991;4:143–149. doi: 10.1002/art.1790040403. [DOI] [PubMed] [Google Scholar]
- 25.Phadnis J., Arnold C., Elmorsy A., Flannery M. Utility of the Instability Severity Index Score in Predicting Failure after Arthroscopic Anterior Stabilization of the Shoulder. Am. J. Sports Med. 2015;43:1983–1988. doi: 10.1177/0363546515587083. [DOI] [PubMed] [Google Scholar]
- 26.Bottoni C.R., Wilckens J.H., DeBerardino T.M., D’Alleyrand J.-C.G., Rooney R.C., Harpstrite J.K., Arciero R.A. A Prospective, Randomized Evaluation of Arthroscopic Stabilization versus Nonoperative Treatment in Patients with Acute, Traumatic, First-Time Shoulder Dislocations. Am. J. Sports Med. 2002;30:576–580. doi: 10.1177/03635465020300041801. [DOI] [PubMed] [Google Scholar]
- 27.Southgate D.F.L., Bokor D.J., Longo U.G., Wallace A.L., Bull A.M.J. The Effect of Humeral Avulsion of the Glenohumeral Ligaments and Humeral Repair Site on Joint Laxity: A Biomechanical Study. Arthroscopy. 2013;29:990–997. doi: 10.1016/j.arthro.2013.02.021. [DOI] [PubMed] [Google Scholar]
- 28.Wheeler J.H., Ryan J.B., Arciero R.A., Molinari R.N. Arthroscopic versus Nonoperative Treatment of Acute Shoulder Dislocations in Young Athletes. Arthroscopy. 1989;5:213–217. doi: 10.1016/0749-8063(89)90174-6. [DOI] [PubMed] [Google Scholar]
- 29.Longo U.G., Rizzello G., Loppini M., Locher J., Buchmann S., Maffulli N., Denaro V. Multidirectional Instability of the Shoulder: A Systematic Review. Arthroscopy. 2015;31:2431–2443. doi: 10.1016/j.arthro.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 30.Locher J., Wilken F., Beitzel K., Buchmann S., Longo U.G., Denaro V., Imhoff A.B. Hill-Sachs Off-Track Lesions as Risk Factor for Recurrence of Instability after Arthroscopic Bankart Repair. Arthroscopy. 2016;32:1993–1999. doi: 10.1016/j.arthro.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 31.Longo U.G., Loppini M., Rizzello G., Romeo G., Huijsmans P.E., Denaro V. Glenoid and Humeral Head Bone Loss in Traumatic Anterior Glenohumeral Instability: A Systematic Review. Knee Surg. Sports Traumatol. Arthrosc. 2014;22:392–414. doi: 10.1007/s00167-013-2403-5. [DOI] [PubMed] [Google Scholar]
- 32.Olds M., Ellis R., Donaldson K., Parmar P., Kersten P. Risk Factors Which Predispose First-Time Traumatic Anterior Shoulder Dislocations to Recurrent Instability in Adults: A Systematic Review and Meta-Analysis. Br. J. Sports Med. 2015;49:913–922. doi: 10.1136/bjsports-2014-094342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jakobsen B.W., Johannsen H.V., Suder P., Søjbjerg J.O. Primary Repair versus Conservative Treatment of First-Time Traumatic Anterior Dislocation of the Shoulder: A Randomized Study with 10-Year Follow-Up. Arthroscopy. 2007;23:118–123. doi: 10.1016/j.arthro.2006.11.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to the privacy.