Abstract
The authors propose a typology of “work schedule patching,” the ongoing adjustments made to plug scheduling holes after employers post schedules. Patching occurs due to changes in employer work demands, or employee nonwork demands necessitating scheduling adjustments, which are reactive or proactive. Using qualitative data from eight health-care facilities, the authors identified three narratives justifying schedule patching implementation approaches (share-the-pain, work-life-needs, and reverse-status-rotation) with variation in formalization and improvisation. Exploratory analysis showed a suggestive link between improvised work–life scheduling and lower pressure ulcers. This article advances theory on balancing the “service triangle” of scheduling in-service economies including health care.
Keywords: work scheduling, health care, work hours, flexibility, staffing coverage, nursing, nursing homes
Q: What are the challenges or issues that you hear over and over again … something that seems to be a constant issue?
A: “Schedules, constant, constantly being revised and it’s difficult to meet all their needs.”
—Evening supervisor commenting on employee callouts due to nonwork schedule demands, Site A
“Because we’re not packing paper plates or making widgets. We’re taking care of people, and that’s the bigger issue.”
—Nurse practice educator, Site F
A fundamental tension in long-term skilled nursing care is managing the conflicting (and often changing) needs of patients, employers, and employees while staffing facilities 24 hours a day, 7 days a week. These tensions are reconciled largely through the work schedule, which has a “heavy lift,” serving as a medium through which competing emotional, social, economic, and organizational pressures play out. Patients’ care conditions can change in unpredictable ways. Employers must serve patients’ needs while managing costs. And employees in long-term care, who are predominantly female and often head of the household, are frequently juggling competing demands in their lives on and off the job.
Despite the importance of effectively managing work scheduling in skilled nursing facilities, our understanding is limited regarding how best to accommodate tensions in the “service triangle” between employers, employees, and patients in service economies including health-care settings (Lopez, 2010; Subramanian & Suquet, 2018). Assigned schedules often change markedly after posting to accommodate the inherent unpredictability in long-term care. Managing the schedule is not a minor undertaking, as these schedules have strict round-the-clock regulated staffing requirements (Bowblis & Lucas, 2012). Further, there are persistent shortages in the long-term care workforce (Paraprofessional Healthcare Institute, 2017). Long-term care and more generally healthcare organizations are striving to provide quality care and remain financially sound while facing rising cost pressures, uncertain regulatory demands, high turnover, and labor shortages (Avgar, Givan, & Liu, 2011). Virtually every developed country around the globe is experiencing a growth in their aging population (United Nations, Department of Economic and Social Affairs, Population Division, 2015), making paid long-term care work one of the fastest growing occupations (Bureau of Labor Statistics, 2017).
Given this context, it is not surprising that scheduling in ways that balance workers’ interests with those of patients and managers remains cognitively, emotionally, and physically challenging for all stakeholders. A study quantifying work–family conflict among nurses reported that half described chronic work interference with family, and family interference with work occurrences at least once a week, with the remainder (41%) reporting at least several monthly work interferences with family demands (Grzywacz, Frone, Brewer, & Kovner, 2006). Consistent patient–staff assignments link to quality of care, as patients and employees are more likely to understand personal care demands, resulting in higher worker and caregiver satisfaction (Burgio, Fisher, Fairchild, Scilley, & Hardin, 2004). Improving organizational cultural support of health-care employees’ work–family needs increases their well-being by reducing psychological distress, with the strongest benefits for those juggling elder and childcare demands (Kossek et al., 2020). The management of scheduling also affects employee caring work behaviors such as absenteeism, presenteeism (when workers are present at work but not fully engaged; Dhaini et al., 2016), and preventable medical errors (Aspden, Wolcott, Bootman, & Cronenwett, 2007).
Given these growing pressures and unpredictability of scheduling, the goal of this article is to explore a critical understudied issue: What happens between employees and management on the ground as they make scheduling adjustments after the formal work schedules are developed? We label this “schedule patching,” and, as we describe later, it is widely prevalent in health care and service work generally. Often overlooked in the organizations literature is how schedule patching is not a relatively isolated incident, but a recurring sociocultural phenomenon. In this article, we describe the phenomenon of schedule patching, which we define as the ongoing adjustments made to plug scheduling holes after the employer posts the planned schedule. We focus on qualitative data from frontline managers and professionals in eight long-term care skilled nursing facilities augmented by archival data on the quality of patient care.
Our research objective is to describe how and why established work schedules unravel as a dynamic process shaped by multiple stakeholders in the “service triangle” of health care, with relevance to the service employment sector generally, by proposing a typology of work schedule patching. We offer grounded theory regarding the narratives organizational actors use to justify decisions regarding schedule patching and identify patterns of variation in the formalization of implementation strategies. We also conduct a brief and highly exploratory analysis regarding how schedule patching approaches relate to patient outcomes using archival data on pressure ulcers—an indicator of staffing influences on quality of care (Berlowitz, Bezerra, Brandeis, Kader, & Anderson, 2000). Our goal is to build theory inductively; thus, most of our theory is in the results and discussion. However, to orient the reader to our results, we begin with a concise literature review of issues relevant to work schedules and their implementation.
Literature Review
Our brief review in the following section offers three main points: Scheduling and schedule patching in health care is (a) a dynamic sociocultural process that includes employee- and employer-driven fluctuations, (b) often involves improvised procedures, and (c) has critical implications for multiple stakeholders of the health-care service triangle (Lopez, 2010).
Work Scheduling
Work scheduling often begins as a rational process distributing hours across employees to match organizational staffing needs with employee availability and patient staffing demands. Most of the health-care scheduling literature takes a “solutions-oriented approach” with writers describing “best” practices regarding “how to” make schedules, conduct self-scheduling, or implement scheduling software (Bard & Purnomo, 2005). This research discusses the technical mechanics of prioritizing different types of workers with varying skill sets and worker cost levels to align with staffing regulations, and how to avoid paying unplanned overtime or health-care benefits (Bard & Purnomo, 2005). Yet critics question whether this literature, which often uses large quantitative datasets to depict a positive association between overall staffing levels and patient outcomes, captures actual staffing practice (Harrington, Carrillo, & Garfield, 2015).
A second stream of studies is on scheduling intervention experiments designed to increase schedule predictability and employee control. Many studies involve hourly retail workers, who like the health-care workforce, is primarily composed of women in low-income jobs (often with families) directly serving customers (Kim, 2000). Scholars in this literature note that employers often transfer economic risk in market fluctuations to the employees through varying their schedules to meet shifting consumer demand, frequently with little advance warning (Lambert, 2008). This increases schedule unpredictability, which relates to higher work–life conflict for these mostly hourly (and often female) workers (Henly & Lambert, 2014). With the goals of reducing schedule unpredictability, Lambert, Henly, Schoeny, and Jarpe (2019) have conducted randomized intervention field experiments where employers agree to post schedules farther in advance than usual industry practice, which is often less than a week’s notice. Although the results of the benefits from advance schedule posting (up to a month ahead) were null, the authors surmised that increasing schedule predictability is still an important goal. Anticipating schedule changes must involve not only employers but also employee input (Lambert et al., 2019). Building on these findings, another experiment at 28 Gap retail stores used multiple intervention tactics (Williams, Lambert, & Kesavan, 2017). Employers not only posted schedules in advance and placed workers on established schedules, but a scheduling application allowed employers to allocate extra hours at the last minute to interested workers and for workers to make shift trades quickly.
A third stream of research emanates from research on work–family climate and culture that examines shared assumptions, beliefs, and perceptions regarding the extent to which an employer expects employees to sacrifice performance in the family role to carry out the work role (Kossek, Noe, & Colquitt, 2001; Thompson, Beauvais, & Lyness, 1999). Taking a work–family culture research approach moves beyond examining scheduling as a prescriptive matter of “how to” schedule hours but might identify schemas that underlie occupational cultures and arrangements regarding how schedules “should be” implemented and the “rules” justifying schedule changes. Clawson and Gerstel’s (2014) study, for example, examines occupations from doctors to nursing assistants in the health-care sector. They observed that while all workers experience scheduling unpredictability, class and gender intersect in ways that negatively influence scheduling experiences. Most relevant to the current study is their finding that nursing employees, who are mostly female and working class, faced particularly challenging hours and harsher penalties for taking any time off, no matter how valid their needs. In a similar vein, Kossek, Pisczcek, McAlpine, Hammer, and Burke (2016) identified the work scheduler as an understudied organizational actor who is an intermediary job crafter of the employment relationship between employee and employer. The scheduler engages in various crafting approaches (patient, employer- or employee-centered, or balancing) to bootstrap and fill “scheduling holes.” Our current study extends previous work by showing that not only is scheduling unpredictable (Henly & Lambert, 2014), often involving schedulers’ job crafting or customizing tasks to meaningfully balance multiple stakeholder demands (Kossek et al., 2016), but it is an organizational culturally driven phenomenon. Scheduling decisions, particularly those involving “patching,” become cues that create, support, and justify a cultural context. We identify types of scheduling patching and narratives used to rationalize the implementation of often-improvised schedule patching changes.
The Need for Scheduling Improvisation in an Unpredictable Service Triangle
Schedule changes matter a great deal to balancing a three-way relationship involving patient, employee, and employer interests (Lopez, 2010). Long-term care work itself is inherently improvised as it entails organizing employees and matching resources to care for people with varying needs that entail not only physical care, but emotional and empathetic care, all in a chronically underresourced work context (Stiehl, Kossek, Leana, & Keller, 2018). Long-term skilled nursing facilities are among the most challenging and unpredictable health-care contexts with elderly patients undergoing declines in independence, increased mental and physical suffering, culminating in the end of life. Falls, other serious injuries, and escalating medical needs often require changes in staff with requisite skills, high emotional labor, and stress resilience capacity (Bolton, 2000). Many patients have already experienced the death of a partner, and live isolated from family, most of whom primarily visit during busy holiday seasons when the facility is understaffed.
Besides unpredictable patient demands, the lives of the workforce are often unpredictable. Most direct care employees are women, and many do “double” or “triple duty,” caring not only for patients at work but also their own children, aging parents, or other dependents when off the job (Kossek et al., 2017). Workers who care for people on and off the job may face “compassion fatigue” and burnout (Ward-Griffin, St-Amant, & Brown, 2011). Many are living at or near the poverty line (Mittal, Rosen, & Leana, 2009) and are single parents. Such employees often lack personal resources to manage last-minute work scheduling demands that challenge their ability to juggle transportation, childcare, and their own personal and health-care needs. Worse yet, schedule changes can decrease pay and benefits (eligibility), further jeopardizing their family’s economic stability.
Because of the unpredictability in patient needs, as well as the instability of a workforce marked by high work–family conflict and turnover (Mukamel et al., 2009), scheduling actors engage in considerable levels of schedule patching. Staff turnover, high use of temporary employees, shifts in patient census or care acuity, and changing regulations combine to make schedule patching an essential and time-consuming aspect of the day-to-day job of a scheduler in long-term care facilities. Far from orderly or rational, our data (described later) suggest that work scheduling is an ongoing, ever-changing, and improvised organizational process.
Just as Moorman and Miner’s (1998) definition of organizational improvisation involves the designing, planning, and execution of organizational action converging simultaneously in time, managing scheduling changes often occurs with little window between planning and executing changes to meet worker, patient, and employer demands. Miner, Bassoff, and Moorman (2001) refer to improvisation as a distinct type of “real-time, short-term learning” (p. 331) that can often occur outside of formal plans. For example, Kossek et al.’s (2016) study of work schedulers found that the most effective ones engaged in bootstrapping, in essence making up solutions as they went along. At the same time, what our results show later is not chaos, but instead improvised, organized patterns of schedule patching enactment.
Methods
Sample, Data, and Organizational Context
Our examination of schedule patching used qualitative data analysis (Creswell, 2003), supplemented with exploratory quantitative analysis. We draw on 48 in-depth interviews conducted during 2009–2011 to capture the baseline context, prior to the implementation of a randomized field trial intervention study in eight skilled nursing facilities in the United States. The sites were affiliates of a for-profit corporation called “Leef”1 that participated in the Work, Family & Health Network study, which was funded from 2008 to 2013 through a cooperative agreement between the National Institutes of Health and the Centers for Disease Control and Prevention (see Bray et al., 2013; Kossek, Hammer, Kelly, & Moen, 2014).2 Table 1 shows the sites ranged in size from 38 to 142 beds (mean=94), and from 35 to 135 residents (mean=88).
Table 1.
Facilities Summary.
| Facility | Number of beds | Number of residents | Number of units | Number of interviews conducted |
|---|---|---|---|---|
|
| ||||
| A | 120 | 110 | 4 | 8 |
| B | 142 | 135 | 3 | 4 |
| C | 135 | 127 | 3 | 6 |
| D | 96 | 89 | 3 | 5 |
| E | 90 | 83 | 2 | 6 |
| F | 90 | 84 | – | 9 |
| G | 38* | 35 | 4 | 5 |
| H | 44 | 42 | 2 | 5 |
Note.
Besides 38 long-term beds, nursing home G has 40 specialty-assisted living beds.
Interview participants.
Table 2 summarizes the job roles of the interviewees included in the sample: administrator or assistant administrator (9), director of nursing (8), unit manager (13), scheduler (7), supervisor (6), and nurse (5). Interviews were voluntary, and these actors were contacted as they represented key professional and managerial job roles reflective of the leadership organizational structure in most U.S. long-term care facilities. The interviews were semistructured typically ranging from 30 to 45 minutes. Most were taped when permission was granted, transcribed verbatim, and augmented by field notes summarizing data. Interviewees described their job role and demands, key challenges, work–life issues, organizational staffing strategies, and how different types of scheduling challenges were resolved.
Table 2.
Interviewees and Job Descriptions.
| Informant jobs |
Number of interviews per job | Description of job roles | ||
|---|---|---|---|---|
| Management | Middle staff | Direct care staff | ||
|
| ||||
| Sr. Administrator | 1 | Provides leadership and management of the Center for all day-to-day operations abiding government standards and nursing home policies while promoting the highest quality resident care | ||
| Administrator | 7 | |||
| Administrator in training | 1 | |||
| Director of nursing | 7 | Responsible for day-to-day operation of nursing department | ||
| Assistant director of nursing | 1 | Assistant director of nursing works under the DON; typically a licensed practicing registered nurse; assists managing nursing department | ||
| Unit manager | 13 | Responsible for daily operation and management of nurses and nursing aides | ||
| Scheduler | 7 | Manages and evaluates Center Labor Management Process according to policy and collective bargaining agreements to optimize clinical, financial, and human resources operating results | ||
| Supervisor | 1 | Supervises and assists the Licensed Nursing Assistants (LNA)/Certified Nursing Assistants (CNA). Completes administrative work (doctor calls, patient admissions). When DON or unit manager are off, covers their operational responsibilities. Manages interactions with families. Assists nurses on floor (medication, treatments) | ||
| Evening supervisor | 4 | |||
| Weekend supervisor | 1 | |||
| Nurse | 2 | Use physical assessment skills and nursing principles to manage range of acute-care and rehabilitation patients, develops/implements patients’ individualized care plans | ||
| Nurse practice educator | 3 | Nursing practice educators provide training to nurses, in charge of infection control. Track infections, maintains patient lists on antibiotics, checks IVs, and audits | ||
Note. DON = director of nursing.
Data Analysis and Approach
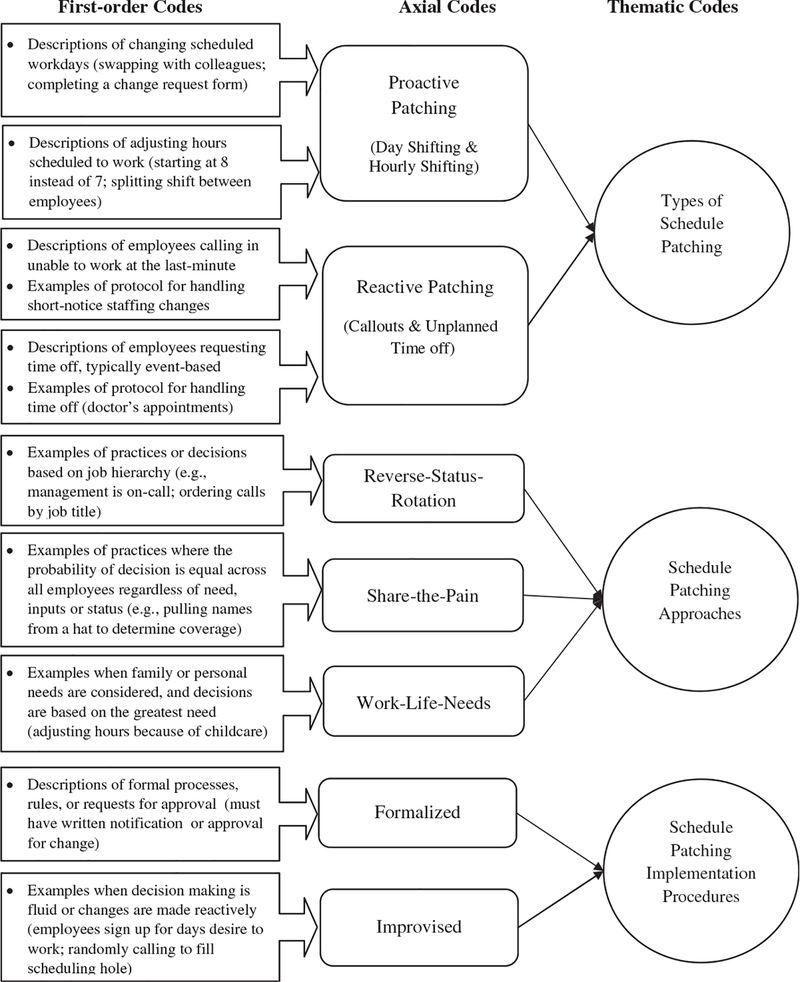
We used a three-step grounded theory approach to identify main data themes (Strauss & Corbin, 1990). First, we inductively developed categories by open coding (Gioia, Corley, & Hamilton, 2013) to analyze informants’ scheduling perspectives by facility (coded A–H in our results) and developed common categories. Second, we created first-order themes using similar categories from the first step, consolidating codes by facility. Third, we reassessed the passages using higher order codes iteratively repeating steps until achieving saturation and consensus (Glaser & Strauss, 1967). We used an inclusion rule that at least two incumbents at a facility had to mention a theme for it to be included.
Findings
Three main findings emerged from our data analysis (see Figure 1). First, schedule patching is a recurring organizational phenomenon that can be either or both proactive and reactive. Second, organizations used several approaches to make adjustments to fill schedule holes: We label these share-the-pain, work-life-needs, and reverse-status-rotation scheduling rationales. Third, approaches varied in their degree of formalization.
Figure 1.
Thematic codes.
Schedule Patching Types
Work schedule patching, the ongoing adjustments made to plug scheduling holes after employees’ work schedules are posted, is a recurring organizational phenomenon that happen due to employer work demands or employee non-work demands for schedule changes. Patching can be proactive and reactive (Table 3). While both types refer to changes made after the schedule is posted, proactive patching anticipates scheduling holes, whereas reactive patching addresses last-minute holes. In the following, we describe each type from employee and employer vantages.
Table 3.
Types of Schedule Changes: Fostering Schedule Patching.
| Schedules | Subtype | Definition | Example | Quotes from interviews |
|---|---|---|---|---|
|
| ||||
| Proactive | Day shifting | Ability to change or adjust the planned or scheduled days one regularly works |
Employee driven: Nurse with childcare demands on Tuesdays and Thursdays swaps days with colleague to workdays that accommodate her schedule. Employer driven: Scheduler uses census to determine how many employees are needed and then informs employees of days scheduled to work. |
“(Workers) change with one another. They have a schedule change form. If they need to … somebody will work for somebody else.”—Director of Nursing, A “Scheduler, she takes care of all that, she’s responsible for filling in any holes in the schedule and she processes.”—Unit Manager, H |
| Hourly shifting | Ability to change or adjust the hours one regularly works |
Employee driven: Certified nursing assistant has personal demands that prevent them from arriving to the predetermined shift times. Employer driven: Manager arranges for employees to work a longer or shorter shift. |
“Somebody having childcare problems, can’t get to work at 3:00pm. I can get to work at four, okay we can do that for three weeks until you get your sitter in line.”—Administrator, A “We have holidays sometimes where on Christmas or New Year’s three nurses work one shift because they all do two hours, two hours, two hours, or whatever, which is fine. It fits their need plus it fits our need.”—Director of Nursing, A |
|
| Reactive | Callouts | A worker does not show, calls in because unable to come to work, or worker is asked to work |
Employee driven: Nurse calls in because of last-minute personal emergency (e.g., sick, child is sick, death). Employer driven: Patient demand is higher than expected or filling a hole/cancellation. |
“I’m having a family issue, there’s no way I’m going to able to make it in.”—Supervisor describes employee, D “Certainly, if they are short or if they need assistance … they’ll page (or call) us and we’ll come in.”—Unit Manager, E |
| Time off | A worker requests time off (not vacation) or is given time off |
Employee driven: Worker needs time off for personal reason. Employer driven: Patient demand lower than expected. |
“I have a doctor’s appointment; do you mind if I leave like at 1:00?” or “Can I go and can can I come back?”—Unit Manager about employee, B “We usually have to send someone home early … now that our census is down.”—Director of Nursing, B |
|
Proactive schedule patching.
Proactive schedule patching involves two planned time shifting adjustments pertaining to either day or hourly shifting. A director of nursing (Facility D) explains day shifting by recounting the temporary accommodation of an employee who expressed, “I don’t have child care on Tuesdays and Thursdays, so I need those two days off.” An administrator (Facility A) discusses hourly shifting: “If somebody is having trouble getting to work say by 11, (and instead) has to arrive at noon … [the worker] will be given an adjusted schedule [for] two or three weeks.” A supervisor (Facility H) provides another hourly shifting example concerning a “worker (who) was scheduled for nights from 10:30 to 6:30, but she could never [arrive] at 10:30, so they changed her time to 11 to 7 and she was on time every night.”
Day shifting refers to the ability to change or adjust the planned or scheduled days an employee regularly works. Employees hire into an established shift such as second shift on Mondays through Fridays, or the first shift on weekends and Mondays. Having set days promotes continuity of care. As a nurse (Facility F) expresses, “with primary assignments, the staff get to know and care about the residents and likewise the residents care about the staff.” Yet the facility sometimes wants the flexibility to allocate an employee to new workdays, due to occupancy rate or census changes, or turnover by another worker. One administrator (Facility G) describes challenges in managing a fluctuating patient census, often having to cut or add time while maintaining quality of care: “The stress people feel [increases] when the census numbers call for you [the manager] to cut a half a person” or “take away a whole position for a day.” This could be because “a couple of patients have gone to the hospital,” or there are “emptying beds.” Given these varying census demands, employers benefit from day shifting.
From an employee perspective, it is beneficial to have predictable and set days to plan life outside of work. Yet sometimes employees’ personal lives also change. An example of employee-driven proactive day shifting includes a nurse who changes scheduled workdays from Tuesday, Thursday, and Friday to Monday, Wednesday, and Friday to accommodate childcare demands over the summer. Having day shifting flexibility where employees’ preferences are considered, or permitting individuals to swap with colleagues to change planned workdays, is desirable for the employee. Our data suggest that how the organization responds to employee requests and the process by which changes are made varied across our sample.
Hourly shifting refers to the ability to change or adjust the hours an employee regularly works. From an employer perspective, the time an employee arrives and departs for shift work directly affects labor costs; thus, employers are motivated to have stringent start and stop times. A director of nursing (Facility B) describes the chain reaction of planning for someone adjusting hours: “We have had people start a little later … at 7:15 or 3:15 for childcare issues … although we’re starting to see some problems with it … they’re coming in even later and it’s making the other shift late.” Yet there are circumstances when employers do desire the ability to make adjustments to extend or shorten an employee’s hourly shift such as splitting coverage during the holidays. Another director of nursing (Facility A) explains, during “holidays sometimes on Christmas or New Year’s, [she] may have three nurses work one shift by having each work a few hours instead of one doing the full shift.” In this way, “it fits [the employers’] need and [the employees’] need.”
From the employee perspective, hourly shifting as a form of schedule patching can be highly desirable. Having to arrive at a precise start time and leave at a precise end time can cause stress and interfere with personal needs. Being able to start at 8 a.m. rather than 7 a.m. shapes the difference in permitting an employee to drop off a child at school. An administrator (Facility B) stated that she “allow(ed) some people to come in late because of childcare and stuff.” For shiftwork, this can be challenging, as it still requires “someone else to leave later,” which can increase employer costs if adjustments trigger overtime. Having an employer that is willing to facilitate pairing employees with complementary scheduling demands or practices that permit employees to coordinate with each other were important forms of schedule adjustments sought by employees but was not available in every facility.
Reactive schedule patching.
Reactive schedule patching is a response to short-notice needs for change and involves last-minute “hole filling” for callouts such as when someone did not show up, or adjustments for unplanned partial day or full-day time off requests for unexpected reasons (car breaking down, sitter not showing up). When an employee does not show up to work or calls in because she or he is unable to come to work, the employee creates a scheduling hole to be filled. Employers may also initiate last-minute patching, such as when an additional worker is needed unexpectedly to care for a deteriorating patient. Often the responsibility to find coverage falls on the employer and the scheduler contacts unscheduled workers to “call them in.” A supervisor (Facility A) explains, “At the last minute if someone hasn’t come into work, the scheduler or manager will find someone by calling people.”
Unplanned “holes” in the schedule associated with workers’ last-minute needs for time off is another example of reactive scheduling. This form of time off is distinctive from planned vacation in that unplanned time off is driven by last-minute personal needs (doctor’s appointment, teacher meeting) or business needs (sending an employee home because patient demand is lower than expected). For unplanned time off requests, some facilities “really encourage staff to find their own coverage unless it’s something like bereavement.” Yet in other facilities, the “scheduler … will do her best to try to find someone for coverage.” More often, it is something that employees self-manage. An administrator (Facility C) explains, even though workers have “pretty much consistent assignments on consistent days … [there are] special request [s],” and “workers change with one another … somebody will work for somebody else,” but “management still has to be concerned about switching and the overtime it may create.” A unit manager (Facility B) comments,
Most [employees] will try to book appointments as late (in the day) as they can” and “usually what happens is … an aide will come to [her] and say, ‘I have a doctor’s appointment, do you mind if I leave at 1:00?’ … or one girl could only get an appointment at 9:00, so she asked, ‘Can I go and can I come back? I’ll punch in, punch out’.
From an employee perspective, having the ability to take time off with little to no notice is desirable. From an employer perspective, being able to make fine-tune staffing adjustments to keep costs low by reducing workers or efficiently replacing them with “just-in-time scheduling” is desirable. An administrator (Facility G) describes last-minute staffing reductions: “The other day … we were carrying full staff even though we were down seven beds,” so he sent workers home.
Organizational Schedule Patching Approaches
Having examined how employer and employee needs create scheduling holes prompting proactive and reactive organizational responses, in this section, we describe justification narratives for schedule patching decisions. Figure 1 identifies three main narratives: (a) work-life-needs, (b) share-the-pain, and (c) reverse-status-rotation. Work-life-needs approaches give priority to employees deemed as having the greatest work–life necessity, defined as having family care demands, or credible personal hardship (e.g., illness).
A director of nursing (Facility C) comments, “We usually err on the side of the employee; somebody has a sick parent, sick child, then that comes first.” She elaborated, I had a [single mother] the other day who has no father [to help with childcare] and I just said, ‘Let’s find somebody to replace you.’ And we just did, because we do that and it’s a practice, people are very willing to help each other because, ‘You did it for me and I’ll do it for you’. And so it’s reciprocated … here, that’s the way to do things.
Share-the-pain approaches distributed schedule patching coverage demands across all employees collectively and “equally.” For example, as a last resort for finding coverage or filling callouts, Facility D offered all employees the opportunity to volunteer and, in exchange, “give them another day off but if they still have no takers, then all [employees] names go into a hat.” Facility B handles time off requests on a “first come, first serve” basis. The director of nursing explains,
The first come, first serve thing is so it’s fair … I have the proof and the backup that this is how many people asked for time off and this is why they got it and you didn’t, because they were first … I feel better, just trying to be fair … everybody is the same.
These strategies allocated scheduling regardless of personal need, work effort, seniority, or job status.
Reverse-status-rotation approaches used job hierarchical rank (whether one was a manager, supervisor, nurse, or aide) to determine who has to fill in scheduling gaps. If there is an employee callout, managers, as the highest rank, were required to come in to cover other lower-level employees’ jobs, even if not under their direct supervision. Thus, a manager must become a frontline worker when needed. One unit manager describes how “on-call rotation” pertains to managers: “If [facility E] is short or needs assistance, they’ll page us [managers] and we’ll come in … but for [lower-level direct care] staff, there’s not an on-call rotation.” Although the length of on-call rotation varied across facilities (7 days a week every 5 weeks, one weekend every 8 weeks, or 1 week a month), this reverse-status-rotation was common. At all facilities, managers were expected to be readily available even off work. Facility C unit manager explained, “Once we [managers] go home, we [have] to keep the phones on … and be ready for any calls, in case anything is to happen.”
Organizational Schedule Patching: Implementation Approaches
Schedule patching used two main implementation approaches: (a) improvised—enacted ad hoc or on the ground and (b) formalized—enacted bureaucratically, often as part of a “system.” Improvised approaches involved informal changes often between the scheduler and the employee, with a minimum number of parties involved, notifying management of the change after-the-fact. An example of an improvised implementation procedure is allowing employees to swap with one another and simply notify the scheduler of the schedule change, without requiring written approval.
In contrast, formalized implementation procedures have a specified approval chain of command and typically entail at least three organizational parties (management, scheduler, and employees) for the schedule change. For example, at five facilities, employees are required to complete a written request form, acquire management signatures, and then submit the form to the scheduler to swap days. Overall, formalized implementation procedures are not just concerned with who the burden falls to for patching, but almost always involve greater organizational process time with multistep procedures.
Schedule Patching Patterns
Applying the axial coding definitions in Figure 1, we analyzed work site patterns across patching types, approaches, and implementation procedures (see Table 4). We found share-the-pain and work-life-needs were the most frequently used schedule patching approaches. Of the seven facilities that used share-the-pain approaches, most (four) only used formalized procedures, one only used improvised procedures, and two facilities used a mixed approach, alternating between the two. Formalized procedures are generally associated more with proactive patching, whereas reactive patching tends to be associated with improvised procedures.
Table 4.
Organizational Patterns of Schedule Patching.
| Implementation of patching approaches |
|||
|---|---|---|---|
| Formalized | Improvised | ||
|
| |||
| Types of patching adjustments | |||
| Proactive | Day shifting | Share-the-pain (Facilities A, B, E, F, G) “Workers have a schedule change form. If they need the day off, somebody will work for somebody else. [The form] goes through the nursing department, supervisors down to certified nursing assistants … and then to the scheduler.”—Director of Nursing, A Workers have to “work with a scheduler [and management] … If I say, ‘I might need the day off and somebody said they’ll switch with me’ … if they can get somebody to agree to switch with them, then signatures in writing from both people [will] get the switch done.”—Administrator, G |
Share-the-pain (Facility H) “We have self-scheduling … so there’s a book where staff put in the days that they want to work … And if we want to make changes, we can make changes.”—Supervisor, H Work-life-needs (Facilities C, D) “Some preferences are considered, you know, ‘I don’t have child care on Tuesdays and Thursdays, so I need those 2 days off’. So, if the scheduler is able to do it, she’ll accommodate.”—Unit Manager, D |
| Proactive | Hourly shifting | Share-the-pain (Facilities E, F, G) “When we hire somebody, we hire them for a certain amount of hours … everybody has a set schedule. If they want to change hours, they have to put it in writing, and they have to give at least 2 weeks….One nurse wanted to work different hours, but it wasn’t available, so it would be the next available time.”—Director of Nursing, E “All [workers] have to work it out so [they] can be here when the normal start of the shift is … We tried accommodating early/late hours in the past … for school. We’ve tried it for daycare situations, but it doesn’t fly … it just, it’s too much of a hardship for the facility and for the other employees.”—Administrator, F |
Work-life-needs (Facilities A, B, C, D, H) “We are pretty flexible in our scheduling … change isn’t just about the residents, it’s also about the staff. And some of them have children and childcare issues. So, we’re sometimes flexible with making someone’s time in at 7:30. Or they have more than one job and the job that they’re leaving ends at 3:00 and they can’t get here until 3:30, so we’ll—we try to be flexible with that.”—Director of Nursing, D “Because of child care issues, we’ve made some people 8 to 2, and we’ve bent as much as we could for people … we really try.”—Director of Nursing, C |
| Reactive | Callouts | Share-the-pain (Facilities B, D) “We’ll kind of enforce that somebody’s got to stay. And (the facility) offers, if you stay, we can give them another day off. If we still have no takers, then the [employees] names go in the hat.”—Director of Nursing, D Reverse-status-rotation (Facilities A, B, C, D, E, F, G, H) “All the managers are on-call … but they know the on-call schedule for a whole year, so (they) plan around it … the only people that will ever be (expected to come) in would be somebody in a supervisor’s position.”—Unit Manager, B |
Share-the-pain (Facilities A, E) “There’s not an on-call rotation for staff. It’s just you call and if someone’s available, they can come in”; “the callouts are all treated the same. We try to be fair about it.”—Unit Manager, A Work-life-needs (Facilities C, H) “If there’s a callout … then (the scheduler or supervisor) will have to start calling around trying to find somebody … we have a phone list of employees phone numbers and … it’s really up to the staff if they want to give a mobile phone number or not. I don’t (give my number), I don’t feel like I have any availability if I am not on the schedule already.”—Supervisor, H |
| Reactive | Time off | Share-the-pain (Facility E) “If they need to request time off, there is always a procedure to. They would fill out a form. And then it would go to director of nursing (DON) or the assistant DON, and then when it’s approved, it will go back to the scheduler and they take them off.” … “You put in a request slip and if you have the time, they give it to you.”—Nurse, E |
Share-the-pain (Facilities B, D, F, G, H) “We try to encourage staff to give us notice for time off requests. But we understand that things happen sometimes, so (we) really encourage them to find their own coverage. And if they can’t, we do what we can to accommodate. Sometimes they’ll get calls in the middle of their shift, it’s a problem or emergency … we’ll work around trying to get them out so that they can go take care of whatever the problem is.”—Director of Nursing, D Work-life-needs (Facilities A, C) “If somebody dies. If a parent dies, a spouse dies, then they get the day off … they’re given an amount of time off….My sister planned a surprise birthday party for my niece and I had to go, because she’s my goddaughter, that’s a lot different … it becomes the employee’s responsibility to find somebody to work for her … it should be (the employee’s) responsibility to find somebody … (the scheduler) realizes that some people will just call in and then we’re still stuck, so she … helps look for someone.”—Unit Manager, A |
Note. Schedule patching adjustments: Proactive: planned time shifting of days/hours. Reactive: last-minute hole-filling (callouts, time off). Scheduling patching approaches: Share-the-pain: allocating schedule patching consistently across employees regardless of need/status. Work-life-needs: patching based on employees’ personal needs. Reverse-status-rotation: occurs to handle callouts, based on job status hierarchy. Schedule patching implementation procedures: Formalized: use of formal, processes or procedures. Improvised: ad hoc decisions made informally on the ground. DON = director of nursing.
Regarding the six facilities using share-the-pain approaches to address proactive, schedule patching for day or hourly shifting, all but one (5 out of 6) implemented formalized responses. Across all of these facilities, we found similar descriptions in our data. Many, like this administrator from facility G, explains,
Most people are hired [for] a certain number of hours and days. But any worker who wants a change has to follow the same procedure to work with the scheduler [and management] … if they can get somebody to agree to switch with them, then signatures in writing from both people [will] get the switch done.
However, for share-the-pain reactive (callouts/time off) patching, most responses were improvised (two facilities used this strategy for callouts, and five facilities for time off). For callouts, schedulers would either randomly call around asking employees to come in or gave employees an “equal opportunity” to volunteer their phone numbers. One nurse said, “I refuse, I don’t have a cell phone. When I am not [at facility E], [employer] does not need to contact me.” We also found that for workers desiring time off after a schedule is posted, the expectation was for the employee to find his or her own replacement. Yet how organizations went about identifying a replacement was often improvised by the scheduler and the employee working together to find coverage. Generally, the employee was ultimately responsible for swapping with someone and coordinating the change. Overall, these findings suggest that the facilities tried to ensure universal treatment in scheduling allocations by relying on formalized implementation for proactive time shifting (formal request forms, management approval). However, in reaction to callouts or unplanned time off, employer actors improvised procedures. They might try to quickly solve the gap by asking employees to find coverage at the same time as they randomly started calling workers so each employee had the same likelihood of having to come in.
Nearly two thirds (63%) of facilities used work-life-needs approaches, and all were improvised. When facilities make schedule adjustments because of an employee’s childcare, illness, or emergency needs, all did so on a case-by-case basis. Thus, no formalized procedures existed focusing on response to employee work-life-needs.
The third approach (reverse-status-rotation) was a secondary approach for reactive patching used by all facilities as a formalized implementation procedure. Reverse-status-rotation only was used when seeking coverage for callouts, as a backup strategy after other approaches failed. For example, when the organization failed to find coverage among the direct care staff, managers were called to fulfill the responsibility. Facilities arranged rotating on-call schedules for managers to come in and cover the work if no lower-level workers were available.
Exploratory Post Hoc Analysis
To investigate the efficacy of the various approaches for patient outcomes, we conducted an exploratory post hoc analysis (see Appendix A) linking facility schedule patching approaches to pressure ulcers, which medical researchers use as a measure of quality of care (Berlowitz et al., 2000). Using Poisson regression, which is appropriate for analyzing count data (McCullagh & Nelder, 1989), we conducted a regression between the most frequently used approaches in a facility (share-the-pain and work-life-needs) and the incidence (expressed as a percentage) of patient pressure ulcers. We found that facilities that have a greater tendency to use work-life-needs approaches had lower rates of patient pressure ulcers (p value=.002). We also examined the patterns of implementation procedures for managing schedule patching and found that greater improvisation predicted lower incidents of preventable pressure ulcers (p=.000). Although our sample size is too small to reach a definitive conclusion regarding the efficacy of the various approaches, these results suggest that flexibility in scheduling, especially when it concerns employee work-life-needs and being able to improvise on the ground, may be associated with better patient care.
Discussion
This article identifies and examines the phenomenon of work schedule patching, the iterative adjustments made to work schedules in organizations after they are posted. We offer a new typology and theory of schedule patching that is relevant to the service sector including health care. Schedule patching is a necessity in each of the facilities we studied. At the same time, it presents an opportunity for each facility to express its values regarding how they prioritize employee, patient, and employer needs. Clearly, patching is a dynamic phenomenon that can influence the emotional well-being of employees and managers, their families, and patients. Many have characterized schedules in health care as being “unpredictable,” but such generalities overlook the complexity of what occurs after the formal schedule is posted to reflect worker, employer, and patient inputs. We contribute to the literature by identifying the phenomenon of schedule patching and describing scheduling as involving multifaceted often-improvised socially enacted practices that have critical implications for multiple stakeholders’ well-being.
We show that the work schedule reflects an institutional vehicle through which growing structural intergroup tensions play out. Such pressures reflect conflicts between service workers needs to control their nonwork schedule demands, which increasingly clash with the work scheduling interests of employers (controlling costs, meeting regulations) and “customers” care needs. Our study reveals the mutual constitution of organizational control and patching in the negotiation of the health-care service triangle and adds a temporal dimension by identifying scheduling disruptions as inevitable and inherently requiring patching.
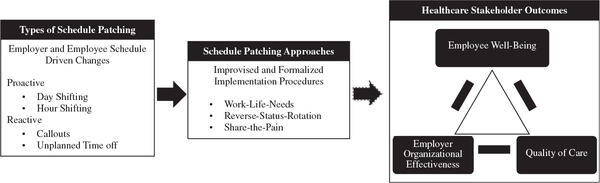
Model of Patching Approaches
Figure 2 summarizes our findings in a schedule patching model. We found that patching occurs due to employers’ work and employees’ nonwork hole-filling needs. Scheduling holes can be proactive (planned day or hourly shifting) or reactive (callouts, unplanned time off). Holes are then filled using three main socially developed approaches that vary in how they impact the well-being of multiple actors in the service triangle: employee, employer, and patient.
Figure 2.
Schedule patching: types, approaches, and outcomes.
The most common justification to manage schedule patching was share-the-pain, which used formalize procedures (e.g., names in a hat) to distribute the costs of hole-filling across individuals regardless of need or status. The next most frequent narrative emphasized “work-life-needs”—usually improvised. Our data suggested employers did not invest many resources into developing formalized ways to effectively support scheduling changes for work-life-needs.
Reverse-status-rotation patching, where more senior workers had to cover schedule gaps, was the third approach. Health-care organizations often are characterized as hierarchical. Yet we found that, ironically, a critical part of frontline supervisors’ jobs is to “fill in” to cover lower status roles if a subordinate does not show up. Previous research has not examined this variation in scheduling enactment norms, where those in higher positions are tapped first to fill unplanned schedule “holes.” Thus, greater schedule control is not necessarily an “earned” benefit—that is, based on performance or seniority—in any of the facilities. Indeed, we found the opposite. Those in higher status jobs were more likely to be called to bear the burden of patching schedule holes. These findings provide a rich rendering of how administrators and managers navigate demands and, counterintuitively, even cede some of their own power and privilege to operate as a backstop when other systems for callouts fail.
Lastly, our results regarding the relationship between schedule patching strategies and quality of care while exploratory are nonetheless intriguing: Facilities that used patching strategies that considered employee’s needs showed lower rates of patient pressure ulcers. Our model provides a useful guide for future research that empirically links stakeholder well-being outcomes to different patching approaches.
Conclusion
Future research might use larger samples with both survey and archival data to address health-care quality linkages. Such research might extend studies showing that hourly employees reporting lower work–family conflict and higher organizational support for work–family needs are more likely to follow safety rules (Kossek et al., 2017). Future research also should examine whether employees in facilities where managers tend to use work-life-needs patching are more likely to have lower work–family conflict (Kossek, Pichler, Bodner, & Hammer, 2011). This may result in workers who are better able to focus on patients rather than being distracted by concerns outside of work and thus be more attentive to patient safety (see Leana, Meuris, & Lamberton, 2018, for evidence regarding nursing home worker distraction and patient safety).
Future research might draw on our work to study the implications of different approaches for employee well-being. For example, when organizations emphasize work-life-needs approaches, do employees experience less emotional exhaustion and more contentment in their family lives? Furthermore, studies are needed examining how patients’ and workers’ families are emotionally affected by schedule patching approaches. Given our data suggests that patching for work-life-needs is often improvised as needs arise unexpectedly and responded to ad hoc, could workers’ personal and family lives, as well as patient outcomes be improved by following proactive formalized approaches? If so, what would such proactive, more formalized policies and systems look like? These outcomes could be contrasted with reverse-status-rotation and sharing-the-pain approaches, which may lead to burnout and emotional exhaustion and have long-term negative impacts on staff well-being, turnover, and patient care because they ignore workers’ emotional and personal needs. We also did not find any scheduling approaches driven by “merit” or higher construed social inputs, effort, or contributions such as superior performance or tenure. Perhaps employers avoid placing further demands on workers who receive relatively low pay for demanding work, fearing they will lose these increasingly scarce workers to competing facilities. In the process, any motivational benefits to tying schedule preference “rewards” to performance or seniority is lost.
Future research should examine whether the heightened emotional experience of managers in facilities following reserve-status-rotation rubrics experience these ad hoc duties as stressful and extra work. Studies might examine whether such role-based status incongruences of scheduling regimes discourage employees with family responsibilities perhaps from seeking leadership roles.
Future research might also identify the conditions under which a formalized work-life-needs approach is implemented—perhaps for educational or maternity leaves or to hire a regular temp for employees with chronic illnesses. Unfortunately, such work–life benefits are relatively unavailable to the low-income health-care workforce. Kossek and Lautsch (2018) note that the availability and consequences of how employers carry out work–life arrangements help create and perpetuate job inequality by fostering negative outcomes including work–family conflict and strain, for workers at all levels, but especially for those lower-level employees who most need work–life schedule control to better match work hours with changing family scheduling needs.
Future studies should investigate whether facilities with greater use of improvisation might be more likely to have more positive worker–manager interactions that could involve joint problem-solving on many organizational issues. By definition, improvised on-the-ground enactment is likely to involve greater use of face-to-face, peer, subordinate, and supervisor social interactions, than formalized implementation. Such interaction, even if reactive, may lead to greater collaboration to solve new or uncertain challenges in resource-challenged contexts. Such a relationship is consistent with the job crafting literature findings that collaborative crafting is more likely to lead to better outcomes (Leana, Appelbaum, & Shevchuk, 2009).
Turning to limitations, one weakness is that our sample includes only nonunion workers. Future unionized samples might examine how need and seniority-based scheduling approaches may clash in helping to reconcile conflicting cross-generational workforce demands. Another limitation is that we focused on how managers and nurse professionals “managed” scheduling. Future research should also include nursing assistants—often studied separately—to augment the manager perspectives studied. A third limitation is that we used a sample with all facilities from the same corporation. While this has the strength of ensuring that corporate policies are similar and that the varied approaches are reflective of local culture, a drawback is there may be other approaches not appearing in this sample that future research should identify. Another weakness is that we lack data on employees’, managers’ or patients’ families who are affected emotionally in how the scheduling service triangle is enacted. This is a ripe area for future studies as families are a silent stakeholder typically excluded from the service triangle.
Overall, the multiple stakeholders concerned with the delivery of health care—employers, employees, and patients—all have an interest in effective staff scheduling. Employees want control over their lives and working conditions. Employers want control over costs and quality. Patients want control over quality of care and its empathetic and safe delivery (Leana et al., 2018). Yet optimizing scheduling for all parties may be difficult, if not impossible, to achieve. A patient may not heal as expected; a worker may need to leave early due to family care demands; regulated staffing requirements and labor cost reimbursement levels may shift as a patient’s health level declines. The effective management of scheduling and schedule patching plays a critical role in supporting the well-being of the lives of employees, patients, and frontline managers. Given the prevalence and importance of schedule patching, however, it is well worth understanding how to implement it better for all actors as a growing “contested terrain” (Edwards, 1979) of the service triangle.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research, conducted through the Work, Family & Health Network, www.WorkFamilyHealthNetwork, organized by Rosalind Berkowitz King and Lynne Casper, was funded via cooperative agreement among the National Institutes of Health, Centers for Disease Control and Prevention, Eunice Kennedy Shriver National Institute of Child Health and Human Development (Grant # U01HD051217, U01HD051218, U01HD051256, U01HD051276), National Institute on Aging (Grant # U01AG027669), the National Heart, Lung and Blood Institute (R01HL107240), Office of Behavioral and Science Sciences Research, and National Institute for Occupational Safety and Health (Grant # U01OH008788, U01HD059773). This publication’s contents are those of the authors and not representatives of funders’ views.
Biography
Ellen Ernst Kossek (PhD, Yale University) is the Basil S. Turner professor of Management & research director at the Susan Butler Center for Leadership Excellence at Purdue University and the first elected President of the Work-Family Researchers Network. She has won awards including the work–life legacy award for advancing the work–life movement. Her research examines transforming gender, inclusion, flexibility, and work–family-life employment practices.
Lindsay Mechem Rosokha is a PhD student at Purdue University studying organizational behavior and human resources. She holds a master’s degree in human resource management from Purdue University and a bachelor’s degree in psychology from the University of Texas. Her research interests include work–nonwork interface, leadership, and diversity.
Carrie Leana is the George Love professor of Organizations and Management, director of the Center for Healthcare Management at the University of Pittsburgh, where she holds appointments in the Business School and the School of Medicine. Her current research is on financial precarity and inequality. She is Editor of The Academy of Management Annals.
Appendix A
Description and Results of Exploratory Post-Hoc Analysis
We obtained each facility’s rate of patients’ medium to severe preventable pressure ulcers (Medicare.gov, 2017). For the patching types (time shifting, time off), we created a variable that was 0 for share-the-pain and 1 for work-life-needs approaches. Next, we created an average score, reflecting each facility’s overall tendency to utilize work-life-needs for patching. Using a similar approach to construct the implementation score, 0 denoted use of formalized and 1 denoted improvised implementation. The sample mean did not equal the variance, which is a mild violation of the assumption of a Poisson distribution. To correct, we followed Cameron and Trivedi’s (2009) correction recommendations using R-studio Version 1.0.143, with robust standard errors and results.
Poisson regression results for pressure ulcers
| Value | Robust SE | p value | |
|---|---|---|---|
|
| |||
| Patching approach | |||
| Intercept | −2.491 | 0.178 | .000 |
| Work-life-needs (vs. share-the-pain) | −0.825 | 0.270 | .002 |
| Implementation procedure | |||
| Intercept | −2.325 | 0.155 | .000 |
| Improvised (vs. formalized) | −0.817 | 0.203 | .000 |
Note. N = 8; significant at p < .05 level.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
All organization and individuals’ names are pseudonyms.
For more information, see Work, Family & Health Network, www.WorkFamilyHealthNetwork.org.
References
- Aspden P, Wolcott J, Bootman L, & Cronenwett L (2007). Preventing medication errors. Institute of Medicine report on medical errors. Washington, DC: National Academy Press. [Google Scholar]
- Avgar A, Givan R, & Liu M (2011). Patient-centered but employee delivered: Patient care innovation, turnover, and organizational outcomes in hospitals. Industrial and Labor Relations Review, 64, 423–440. [Google Scholar]
- Bard J, & Purnomo H (2005). Short-term nurse scheduling in response to daily fluctuations in supply and demand. Health Care Management Science, 8, 315–324. [DOI] [PubMed] [Google Scholar]
- Berlowitz DR, Bezerra HQ, Brandeis GH, Kader B, & Anderson JJ (2000). Are we improving the quality of nursing home care: The case of pressure ulcers? Journal of the American Geriatrics Society, 48(1), 59–62. [DOI] [PubMed] [Google Scholar]
- Bolton S (2000). Who cares? Offering emotion work as a ‘gift’ in the nursing labour process. Journal of Advanced Nursing, 32, 580–586. [DOI] [PubMed] [Google Scholar]
- Bowblis JR, & Lucas JA (2012). The impact of state regulations on nursing home care practices. Journal of Regulatory Economics, 42, 52–72. [Google Scholar]
- Bray JW, Kelly EL, Hammer LB, Almeida DM, Dearing JW, King RB, & Buxton OM (2013). An integrative, multilevel, and transdisciplinary research approach to challenges of work, family, and health (RTI Press Publication No. MR-0024–1303). Research Triangle Park, NC: RTI Press. [PubMed] [Google Scholar]
- Bureau of Labor Statistics. (2017). 2016–2026 Occupational outlook handbook: Fastest growing occupations. Washington, DC: Bureau of Labor Statistics, U.S. Department of Labor. Retrieved from https://www.bls.gov/ooh/fastest-growing.htm [Google Scholar]
- Burgio L, Fisher S, Fairchild J, Scilley K, & Hardin M (2004). Quality of care in the nursing home: Effects of staff assignment and work shift. The Gerontologist, 44, 368–377. [DOI] [PubMed] [Google Scholar]
- Cameron AC, & Trivedi PK (2009). Microeconometrics with STATA. College Station, TX: StataCorp LP. [Google Scholar]
- Clawson J, & Gerstel N (2014). Unequal time: Gender, class and family in employment schedules. New York, NY: Russell Sage Foundation. [Google Scholar]
- Creswell JW (2003). Research design: Qualitative, quantitative, and mixed methods approaches (2nd ed.). Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Dhaini S, Zuniga F, Ausserhofer D, Simon M, Kunz R, De Geest S, & Schwendimann R (2016). Absenteeism and presenteeism among care workers in Swiss nursing homes and their association with psychosocial work environment: A multi-site cross-sectional study. Gerontology, 62, 386–395. doi: 10.1159/000442088 [DOI] [PubMed] [Google Scholar]
- Edwards RC (1979). Contested terrain: The transformation of the workplace in the twentieth century. New York, NY: Basic Books. [Google Scholar]
- Gioia D, Corley K, & Hamilton A (2013). Seeking qualitative rigor in inductive research: Notes on the Gioia methodology. Organizational Research Methods, 16(1), 15–31. doi: 10.1177/1094428112452151 [DOI] [Google Scholar]
- Glaser BG, & Strauss A (1967). The discovery of grounded theory: Strategies for qualitative research. Chicago, IL: Aldine. [Google Scholar]
- Grzywacz J, Frone M, Brewer C, & Kovner C (2006). Quantifying work-family conflict among registered nurses. Research in Nursing and Health, 29, 414–426. doi: 10.1002/nur.20133 [DOI] [PubMed] [Google Scholar]
- Harrington C, Carrillo H, & Garfield R (2015). Nursing facilities, staffing residents and facility deficiencies 2009–2014 (Publication 8761). Menlo Park, CA: Kaiser Family Foundation. Retrieved from www.kff.org [Google Scholar]
- Henly JR, & Lambert S (2014). Unpredictable work timing in retail jobs: Implications for employee work-life conflict. Industrial and Labor Relations Review, 67(3), 986–1016. [Google Scholar]
- Kim M (2000). Women paid low wages: Who they are and where they work. Monthly Labor Review, 123, 26. [Google Scholar]
- Kossek E, Hammer L, Kelly E, & Moen P (2014). Designing organizational work, family & health change initiatives. Organizational Dynamics, 43, 53–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kossek E, & Lautsch B (2018). Work-life flexibility for whom? Occupational status and work-life inequality in upper, middle, and lower level jobs. Academy of Management Annals, 12(1), 5–36. doi: 10.5465/annals.2016.0059 [DOI] [Google Scholar]
- Kossek EE, Noe RA, & Colquitt JA (2001). Caregiving decisions, well-being and performance: The effects of place and provider as a function of dependent type and work-family climates. Academy of Management Journal, 44(1), 29–44. [Google Scholar]
- Kossek EE, Petty RA, Michel JS, Bodner TB, Yragui N, Perrigino M, & Hammer L (2017). Work-family subcultures: Workgroup multilevel influences on family supportive supervisor behaviors (FSSB) affecting individual sleep quality and safety performance. In Las Heras M, Chinchilla N, & Grau Grau M (Eds.), Work-family balance, technology and globalization (pp. 62–85). Newcastle upon Tyne, England: Cambridge Scholars Publishing. [Google Scholar]
- Kossek E, Pichler S, Bodner T, & Hammer L (2011). Workplace social support and work-family conflict: A meta-analysis clarifying the influence of general and work-family specific supervisor and organizational support. Personnel Psychology, 64, 289–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kossek E, Pisczcek M, McAlpine K, Hammer L, & Burke L (2016). Filling the holes: Work schedulers as job crafters of employment practice in long-term health care. Industrial and Labor Relations Review, 69(4), 961–990. doi: 10.1177/0019793916642761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kossek EE, Thompson RJ, Lawson KM, Bodner T, Perrigino M, Hammer LB,…Bray JW. (2019). Caring for the elderly at work and home: Can a randomized organizational intervention improve psychological health? Journal of Occupational Health Psychology, 24(1), 36–54. doi: 10.1037/ocp0000104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert S (2008). Passing the buck: Labor flexibility practices that transfer risk onto hourly workers. Human Relations, 61, 1203–1227. [Google Scholar]
- Lambert SJ, Henly JR, Schoeny M, & Jarpe M (2019). Increasing schedule predictability in hourly jobs: Results from a randomized experiment in a U.S. retail firm. Work and Occupations, 46(2), 176–226. [Google Scholar]
- Leana C, Appelbaum E, & Shevchuk I (2009). Work process and quality of care in early childhood education: The role of job crafting. Academy of Management Journal, 52, 1169–1192. [Google Scholar]
- Leana C, Meuris J, & Lamberton C (2018). More than a feeling: The role of empathetic care in promoting safety in health care. Industrial and Labor Relations Review, 71, 394–425. doi: 10.1177/0019793917720432 [DOI] [Google Scholar]
- Lopez S (2010). Workers, managers, and customers: Triangles of power in work communities. Work and Occupations, 37, 251–271. [Google Scholar]
- McCullagh P, & Nelder J (1989). Generalized linear models. New York, NY: Chapman & Hall. [Google Scholar]
- Medicare.gov. (2017). FSQRS. Retrieved from https://www.cms.gov/medicare/provider-enrollment-and-certification/certificationandcomplianc/fsqrs.html
- Miner AS, Bassoff P, & Moorman C (2001). Organizational improvisation and learning: A field study. Administrative Science Quarterly, 46(2), 304–337. [Google Scholar]
- Mittal V, Rosen J, & Leana C (2009). A dual-driver model of retention and turnover in the direct care workforce. The Gerontologist, 49, 622–634. [DOI] [PubMed] [Google Scholar]
- Moorman C, & Miner AS (1998). Organizational improvisation and organizational memory. Academy of Management Review, 23(4), 698–723. [Google Scholar]
- Mukamel DB, Spector WD, Limcangco R, Wang Y, Feng Z, & Mor V (2009). The costs of turnover in nursing homes. Medical Care, 47(10), 1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paraprofessional Healthcare Institute. (2017). The future of long term care. Retrieved from https://60caregiverissues.org/the-future-of-long-term-care-issue-1.html
- Stiehl E, Kossek E, Leana C, & Keller Q (2018). A multilevel model of care flow: Examining the generation and spread of care in organizations. Organizational Psychology Review, 8(1), 31–69. doi: 10.1177/2041386617740371 [DOI] [Google Scholar]
- Strauss A, & Corbin J (1990). Basics of qualitative research: Grounded theory procedures and techniques. New York, NY: Sage Publications. [Google Scholar]
- Subramanian D, & Suquet J (2018). Unpacking the service triangle: Arranging power relations between frontline occupations. Work and Occupations, 45(1), 38–81. doi: 10.1177/0730888417736095 [DOI] [Google Scholar]
- Thompson CA, Beauvais LL, & Lyness KS (1999). When work–family benefits are not enough: The influence of work–family culture on benefit utilization, organizational attachment, and work–family conflict. Journal of Vocational Behavior, 54(3), 392–415. [Google Scholar]
- United Nations, Department of Economic and Social Affairs, Population Division. (2015). World population ageing, 2015 (ST/ESA/SER.A/390). Retrieved from http://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2015_Report.pdf
- Ward-Griffin C, St-Amant O, & Brown JB (2011). Compassion fatigue within double duty caregiving: Nurse-daughters caring for elderly parents. Online Journal of Issues in Nursing, 16, 4. doi: 10.3912/OJIN.Vol16No01Man04 [DOI] [PubMed] [Google Scholar]
- Williams JC, Lambert S, & Kesavan S (2017). How the Gap used an App to give workers more control over their schedules. Harvard Business Review. Retrieved from https://hbr.org/2017/12/how-the-gap-used-an-app-to-give-workers-more-control-over-their-schedules [Google Scholar]