Abstract
Hepatocellular carcinoma (HCC) is an aggressive and chemoresistant cancer type. The development of novel therapeutic strategies is still urgently needed. Personalized or precision medicine is a new trend in cancer therapy, which treats cancer patients with specific genetic alterations. In this study, a gene signature was identified from the transcriptome of HCC patients, which was correlated with the patients’ poorer prognoses. This gene signature is functionally related to mitotic cell cycle regulation, and its higher or lower expression is linked to the mutation in tumor protein p53 (TP53) or catenin beta 1 (CTNNB1), respectively. Gene–drug association analysis indicated that the taxanes, such as the clinically approved anticancer drug paclitaxel, are potential drugs targeting this mitotic gene signature. Accordingly, HCC cell lines harboring mutant TP53 or wild-type CTNNB1 genes are more sensitive to paclitaxel treatment. Therefore, our results imply that HCC patients with mutant TP53 or wild-type CTNNB1 genes may benefit from the paclitaxel therapy.
Keywords: bioinformatics, hepatocellular carcinoma, precision medicine, taxanes
1. Introduction
Primary liver cancer is still the sixth most common cancer type and the third leading cause of cancer-related death in the world [1]. Most (75–85%) of primary liver cancer cases involve hepatocellular carcinoma (HCC), whose major risk factors include chronic hepatitis B or C virus (HBV or HCV) infection, aflatoxin contamination in foods, excess body weight, heavy alcohol intake, smoking, and type 2 diabetes [1]. HCC development involves a complex, multi-step histological process of normal hepatocyte malignant transformation involving various genetic and epigenetic alterations [2]. The most frequent genetic alterations include mutations in telomerase reverse transcriptase (TERT) promoter, tumor protein p53 (TP53), and catenin beta 1 (CTNNB1) genes, as well as copy number variations and aberrations in DNA methylation [3]. TERT promoter mutations occur in dysplastic nodules and early HCC, and this gene is viewed as a gatekeeper for malignant transformation. TP53 and CTNNB1 mutations function as drivers during HCC development. Additional molecular alterations include focal DNA amplification (for example, vascular endothelial growth factor A/VEGFA, MYC proto-oncogene, bHLH transcription factor/MYC) and deletions (for example, cyclin-dependent kinase inhibitor 2A/CDKN2A, axin 1/AXIN1), and DNA methylation of promoter regions [3].
The current options for HCC management include surgical resection, liver transplantation, percutaneous local ablations (such as ethanol injection and radiofrequency thermal ablation), transarterial chemoembolization, transarterial radioembolization, and systemic pharmacological therapies [4,5]. The main curative treatments for HCC are surgical resection and liver transplantation, which are, however, only suitable for 15% to 25% of patients [6]. Furthermore, HCC is a chemoresistant and extremely refractory tumor type, and no reliable and effective treatments are available for those with advanced or metastatic disease [6]. Molecular targeted agents and immunotherapy have been regarded as treatment options in recent years. Although several multi-kinase inhibitors, such as sorafenib, regorafenib, lenvatinib, and cabozantinib, have been approved for treating advanced HCC [7,8,9,10], they only provide a short increase in median overall survival [7,8,10,11,12]. Immune checkpoint inhibitors, such as human anti-PD-1 monoclonal antibodies (nivolumab and pembrolizumab) and human anti-CTLA4 monoclonal antibody (ipilimumab), were approved for advanced HCC from 2017 to 2020, which greatly extend the patients’ overall survival [13,14,15].
Personalized or precision medicine has become a new trend in cancer treatment, which helps doctors select treatment for patients based on their genetic alterations [16]. Because HCC is a highly heterogeneous disease, grouping HCC patients into relatively homogeneous molecular subtypes may offer a significant clinical benefit through precision treatment [17]. HCC is usually classified based on tumor burden [18]. Recent advances in multi-omics technologies provide an opportunity for developing personalized treatment against HCC. For example, next-generation sequencing analyses of HCC identified new mutational signatures and defined new tumor subtypes that may benefit from targeted treatments in the future [19,20].
In this study, an integrated bioinformatics analysis determined that a prognostic mitotic gene signature is associated with TP53/CTNNB1 mutation statuses in HCC. This gene signature could be targeted by paclitaxel, a clinically approved anticancer drug. Our results support that HCC patients with mutant TP53 or wild-type CTNNB1 genes may benefit from the paclitaxel anticancer therapy.
2. Materials and Methods
2.1. Cancer Genomics Analysis
Four microarray data sets from HCC patients, including GSE14520 [21], GSE45267 [22], GSE50579 [23], and GSE62232 [19], were obtained from the public Gene Expression Omnibus (GEO) depository database at the National Center for Biotechnology Information (NCBI). The differentially expressed genes (DEGs) between HCC tumor and adjacent normal tissues were obtained using the GEO2R online tool [24], and the criteria used to define DEGs were as follows: an adjusted p-value < 0.01 and |Log2 fold-change| > 1. The full DEG list is shown in File S1. The overlapped genes among four microarray data sets were visualized by a heat map generated using MORPHEUS software (https://software.broadinstitute.org/morpheus/; accessed on 21 January 2021). The prognostic values of these overlapped genes in HCC patients were further explored by GEPIA2 (http://gepia2.cancer-pku.cn/; accessed on 21 January 2021) [25] and/or cBioPortal (https://www.cbioportal.org/; accessed on 21 January 2021) [26,27], using The Cancer Genome Atlas (TCGA) hepatocellular liver carcinoma (LIHC) data set.
2.2. Pathway Enrichment Analysis
For pathway enrichment in Gene Ontology (GO) biological process, Kyoto Encyclopedia of Genes and Genomes (KEGG), and Reactome, selected genes were analyzed by STRING (https://string-db.org/; accessed on 21 January 2021), a database of known and predicted protein–protein interactions based on computational prediction, knowledge transfer between organisms, and interactions aggregated from other primary databases [28]. The following parameters were used: organism = Homo sapiens; network type = full network; network edges = evidence; active interaction sources = experiments and databases; minimum required interaction score = 0.4; max number of interactors to show = queried proteins only.
2.3. Gene–Drug Association Analysis
Gene–drug association was analyzed using GLAD4U (http://dlad4u.zhang-lab.org/; accessed on 26 January 2021) [29] via the WebGestalt website (http://www.webgestalt.org/; accessed on 26 January 2021) [30]. GLAD4U is a gene retrieval and prioritization tool based on existing biomedical literature [29]. WebGestalt is a functional enrichment analysis web tool that integrates various primary databases, including GLAD4U [30]. The gene–drug interaction network was further constructed using STITCH (http://stitch.embl.de/; accessed on 26 January 2021), a database of known and predicted interactions between chemicals and proteins based on computational prediction, knowledge transfer between organisms, and interactions aggregated from other primary databases [31]. The following parameters were used: organism = Homo sapiens; network edges = evidence; active interaction sources = experiments and databases; minimum required interaction score = 0.4; max number of interactors to show = queried proteins only.
2.4. Cancer Cell Drug Sensitivity Analysis
The drug sensitivity data, gene mutation status, and gene expression levels in HCC cell lines (Table S1) were downloaded from CellMinerCDB (https://discover.nci.nih.gov/cellminercdb/; accessed on 25 July 2021) [32] using the data in the Cancer Therapeutics Response Portal (CTRP; https://portals.broadinstitute.org/ctrp.v2.1/; accessed on 25 July 2021) [33,34,35]. The CTRP database links cancer cells’ genetic features to drug sensitivity [33,34,35], and CellMinerCDB is an interactive web-based tool allowing integration and analysis of genetic and pharmacological data in cancer cell lines across various data sets, including the CTRP [32].
3. Results
3.1. Identification of a Prognostic Mitotic Gene Signature in Hepatocellular Carcinoma
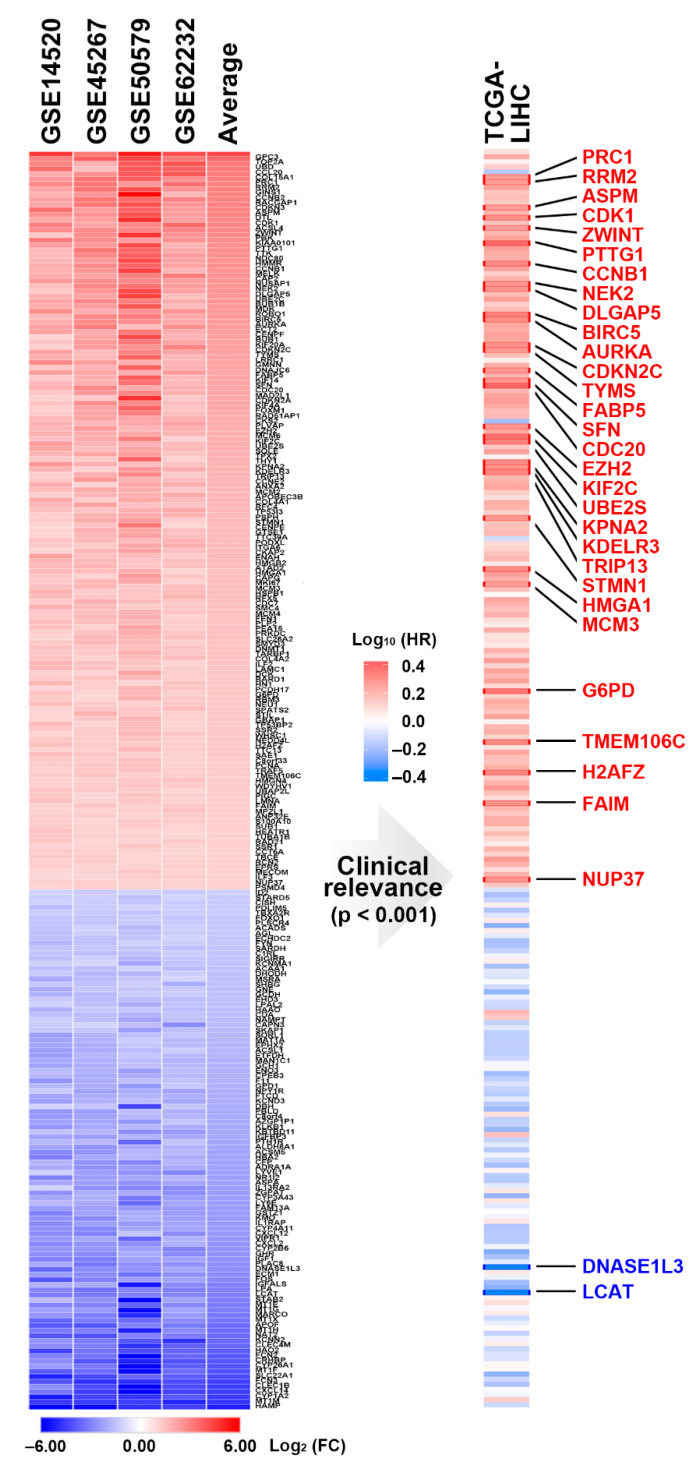
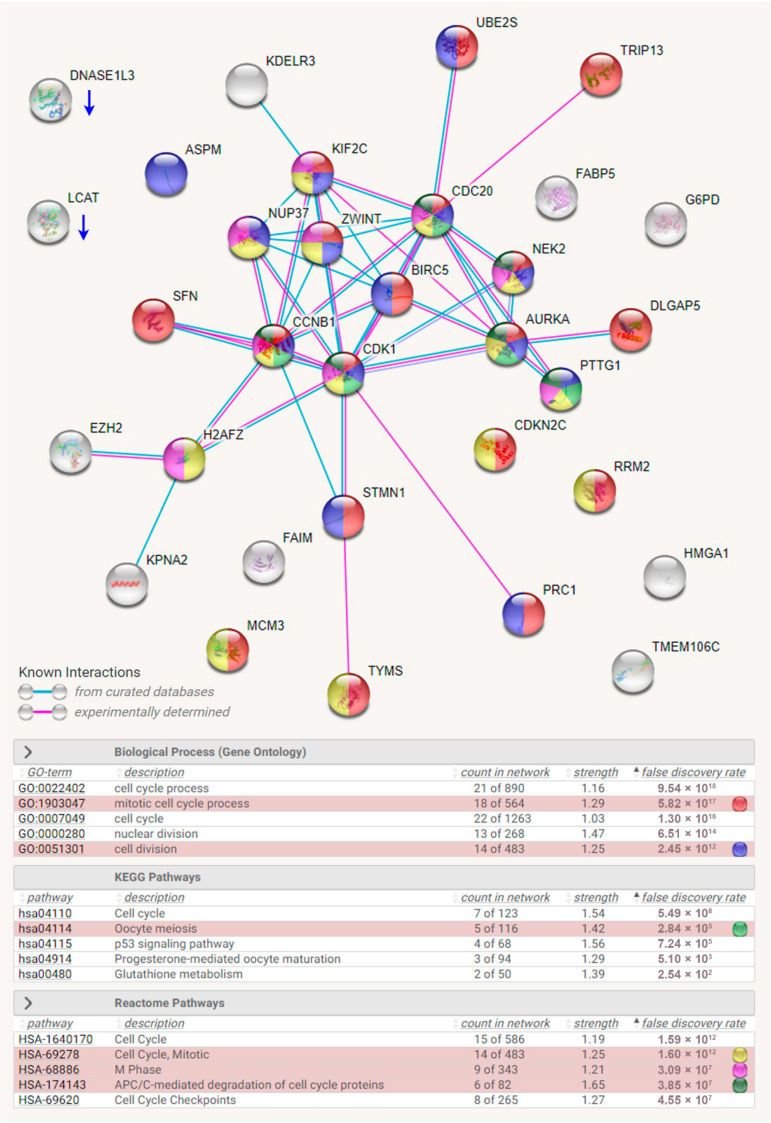
To identify a common gene signature in HCC patients, four microarray data sets (Table 1) were employed, and the common DEGs and their fold-change values are visualized in Figure 1 (left). To characterize the most essential genes in HCC patients, the prognostic roles of these DEGs in patients’ overall survival were analyzed using the TCGA-LIHC data set. As shown in Figure 1 (right), 30 upregulated and 2 downregulated genes were significantly linked to the patients’ overall survival. The interactions of these 32 genes were constructed by STRING [28]. Pathway enrichment results found that most of the upregulated genes are related to the cell cycle procession, especially mitosis (Figure 2). For example, mitosis is initiated by activating cyclin-dependent kinase 1 (CDK1) with its binding partner, cyclin B1 (CCNB1). Aurora kinase A (AURKA) and NIMA (never in mitosis gene A)-related kinase 2 (NEK2) are also mitotic kinases. Once activated, these mitotic kinases simultaneously or sequentially phosphorylate more than 1000 mitotic substrates (such as cell division cycle 20/CDC20 and pituitary tumor transforming gene 1/PTTG1) to regulate mitotic progression [36]. These results indicate that the commonly upregulated genes contributing to poor prognoses of HCC patients are correlated with the aberrant regulation of mitosis.
Table 1.
Microarray data sets for hepatocellular carcinoma patients.
Figure 1.
A prognostic gene signature for hepatocellular carcinoma (HCC). Left: The common gene signature in HCC was obtained from four data sets and ranked according to the average gene expression levels. Right: The prognostic impact of each gene in HCC was analyzed using the TCGA-LIHC data set. The genes highlighted in red or blue indicate these genes predicted better or poorer overall survival of HCC patients, respectively.
Figure 2.
Pathway enrichment for the prognostic gene signature in hepatocellular carcinoma. The interaction network construction and pathway enrichment for the common gene signature in HCC was performed using the STRING database. The selected pathways are highlighted in different colors.
3.2. The Mitotic Gene Signature Is Associated with the Mutation Statuses of TP53 and CTNNB1 Genes
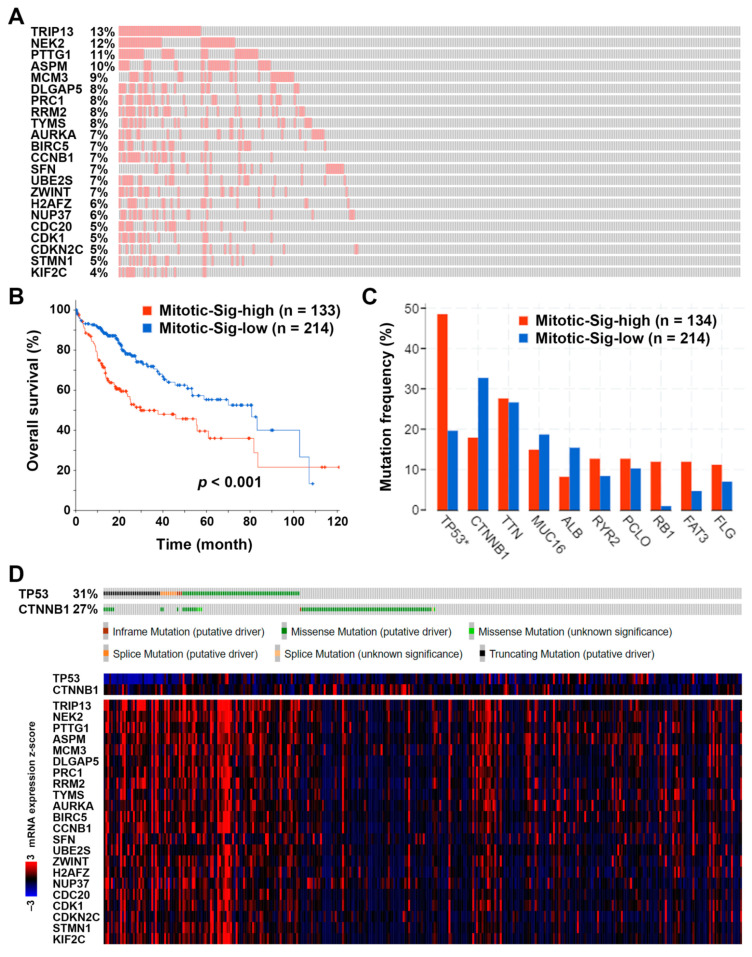
The 22 genes (mitotic gene signature) annotated to the cell cycle and mitosis (Figure 2) were further analyzed using the TCGA-LIHC data for their mRNA expression levels. Among 348 HCC patients, 134 (38.5%) exhibited higher expression of mitotic gene signature (Figure 3A). Consistent with the result in Figure 1 (right), patients with higher mitotic gene signature expression had poorer overall survival (Figure 3B). Therefore, this mitotic gene signature may be utilized for the prediction of HCC patients’ prognoses.
Figure 3.
The association between the prognostic mitotic gene signature and gene mutations in hepatocellular carcinoma. (A) A waterfall plot shows the mRNA upregulation of the mitotic gene signature in HCC patients. (B) The prognostic impact of the mitotic gene signature expression on the overall survival of HCC patients. (C) The gene mutation frequency in HCC patients with high or low expression levels of mitotic gene signature. * indicates significant differences (p < 0.05) between two groups. (D) Upper: The genetic mutation statuses of TP53 and CTNNB1 genes in HCC patients. (D) Lower: The heat map for the mRNA expression levels of TP53, CTNNB1, and mitotic gene signature.
Interestingly, the higher mitotic gene signature expression significantly correlated with TP53 gene mutation (Figure 3C). According to the TCGA-LIHC data set, 31% of HCC patients harbored TP53 mutations (including missense, truncating, splicing, and inframe mutations), and they tended to have higher mitotic gene signature expression (Figure 3D). We also noticed that HCC patients harboring CTNNB1 mutations seemed to have lower mRNA expression levels of the mitotic gene signature, although no statistically significant differences existed (Figure 3C,D). Given the finding that TP53 and CTNNB1 gene mutations usually occur in a mutually exclusive manner in HCC [3], the overexpression of this mitotic gene signature may result from the TP53 mutation during HCC development.
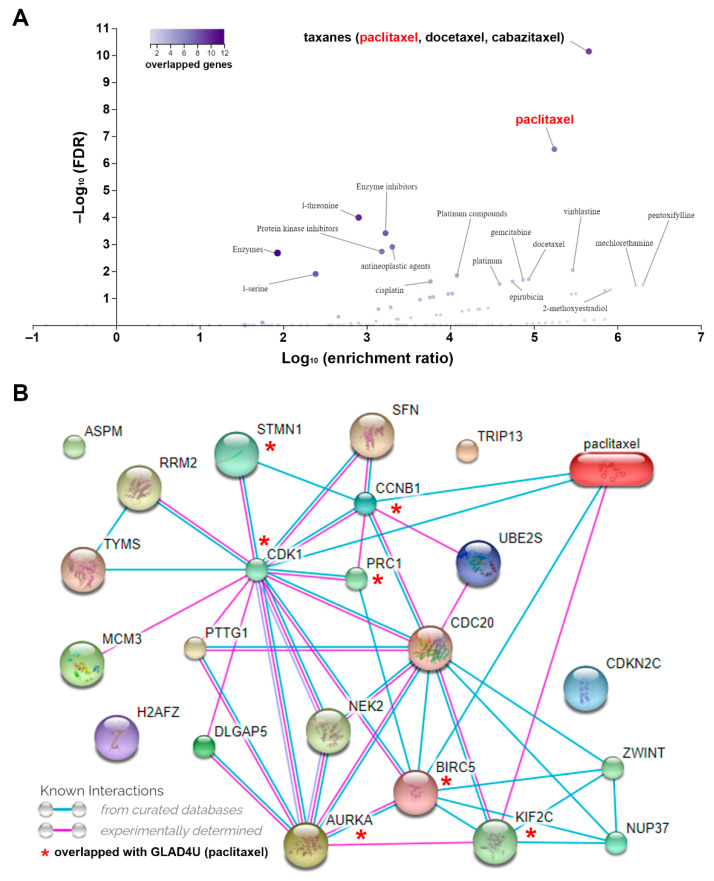
3.3. Paclitaxel Provides Therapeutic Benefit for Hepatocellular Carcinoma Cells Harboring Mutant TP53 or Wild-Type CTNNB1 Genes
To identify potential drugs that targeted the mitotic gene signature, we used the GLAD4U web-based tool to search drug-gene interactions [29]. As shown in Figure 4A, taxanes (paclitaxel, docetaxel, and cabazitaxel) were the most significant drugs linking to the mitotic gene signature. As a representative, the paclitaxel-gene interacting network was further constructed using the STITCH database [31]. The common genes associated with paclitaxel were CDK1, CCNB1, baculoviral IAP repeat containing 5 (BIRC5), kinesin family member 2C (KIF2C), stathmin 1 (STMN1), protein regulator of cytokinesis 1 (PRC1), and AURKA (Figure 4B). Taxanes belong to microtubule-stabilizing agents that cause inhibition of mitosis by preventing the degradation of microtubules [37]. Thus, it is reasonable to say that paclitaxel could target aberrant mitosis in HCC.
Figure 4.
Prediction of potential drugs targeting the mitotic gene signature. (A) The association between drugs and mitotic gene signature. (B) The network between paclitaxel and mitotic gene signature.
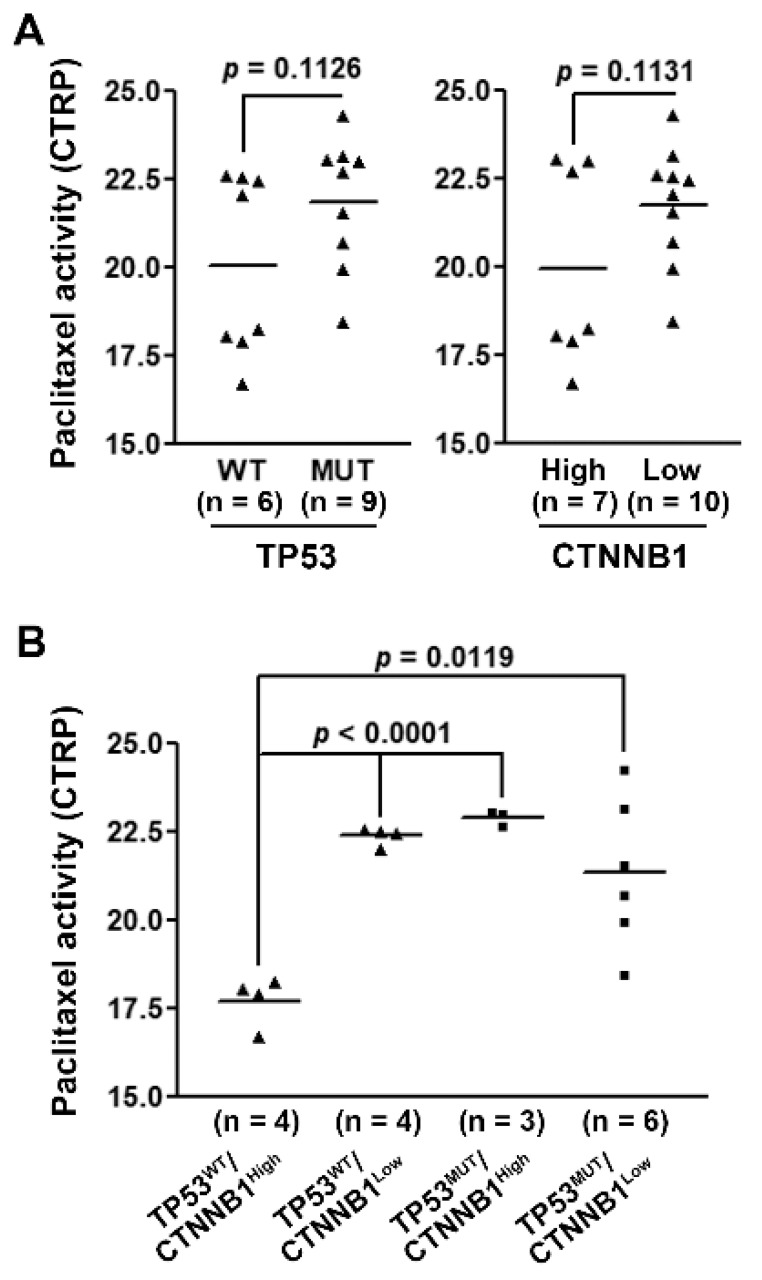
Because the mitotic gene signature correlated with TP53 and CTNNB1 gene mutations in HCC patients (Figure 3C,D), we hypothesized that HCC subtyping based on TP53 and CTNNB1 gene mutation statuses might exhibit a potential benefit from paclitaxel treatment. To demonstrate this possibility, the relationship between drug activity and gene mutations in HCC cell lines was retrieved from the CTRP database [33,34,35]. However, only one HCC cell line harbored CTNNB1 gene mutation (Figure S1A). Because CTNNB1 mutations were associated with higher CTNNB1 mRNA expression levels in HCC patients (Figure S1B), we used CTNNB1 gene expression levels to compare with paclitaxel drug activity in HCC cell lines. As shown in Table S1, HCC cells divided by either TP53 mutation status or CTNNB1 expression level exhibited no significantly different sensitivity to paclitaxel treatment (Figure 5A). Interestingly, HCC cells simultaneously harboring wild-type TP53 and higher CTNNB1 expression were the most resistant to paclitaxel (Figure 5B), confirming that higher mitotic gene signature expression contributes to the increased sensitivity to paclitaxel.
Figure 5.
The role of TP53 and CTNNB1 gene statuses in the paclitaxel drug sensitivity in hepatocellular carcinoma cells. The paclitaxel drug activity in HCC cell lines according to the TP53 mutation status (A, left), CTNNB1 mRNA expression (A, right), or their combination (B).
4. Discussion
Because HCC is highly aggressive and resistant to chemotherapy, novel therapeutic strategies are still urgently needed. Precision medicine is a new and emerging strategy that helps doctors better understand disease and provide new options for patients. However, as novel medicines will not benefit all patients, finding biomarkers is critical. Cancer bioinformatics is one of the useful tools aiding in the discovery of biomarkers and the prediction of therapy efficacy. In this paper, we present a successful example of using bioinformatics tools to uncover biomarkers for the precision HCC treatment.
According to our findings, the overexpression of mitotic gene signature is associated with poorer overall survival and TP53 gene mutation in HCC patients. The overexpression of mitotic genes may represent abnormal mitosis that is required for rapid tumor growth. Consistently, a higher mitotic index is observed in HCC patients and is associated with their poorer prognoses [38,39,40]. In addition, aberrant p53 protein expression is associated with higher mitotic and proliferative indexes in HCC tumors [41], further supporting our results. However, our conclusion may be limited by the HCC patients’ clinical statuses. For example, a localized or advanced stage may also contribute to HCC patients’ prognoses, which should be further clarified in-depth.
Immunotherapy, such as immune checkpoint inhibitors, has become a promising new strategy for treating advanced HCC [42]. Between 2017 and 2020, two human anti-PD-1 monoclonal antibodies (nivolumab and pembrolizumab) and an anti-CTLA4 monoclonal antibody (ipilimumab) were approved for advanced HCC, extending patients’ overall survival significantly [13,14,15]. Higher tumor mutation burden (TMB-H) has been viewed as a predictive biomarker for better responses of cancer patients to anti-PD-1 and anti-CTLA4 therapy, because the increasing numbers of mutant-protein-derived tumor antigens allow the enhanced immunogenicity [43]. The TP53 gene is one of the most frequent driver mutations during HCC development [3] and is positively correlated with TMB-H [44,45]. Because the mitotic gene signature is positively associated with TP53 gene mutation in HCC, this signature may be used to predict the efficacy of immunotherapy. Supportively, a higher immune cell infiltration is associated with a higher mitotic index in gastrointestinal stromal tumors [46].
Mutations in TP53 and CTNNB1 genes in HCC usually occur in a mutually exclusive manner [3]. In contrast to TP53 mutation, CTNNB1 mutation has been found to define immune-cold HCC, meaning that CTNNB1-mutated HCC tends to be refractory to immune checkpoint inhibitors [47,48]. Our results also showed that the overexpression of mitotic gene signature is negatively associated with CTNNB1 gene mutation, which further supports the predictive value of the mitotic gene signature to immune checkpoint inhibitors.
Taxanes are widely used chemotherapy for many cancers [49,50]. For example, the nanoparticle albumin-bound-paclitaxel is approved for treating breast cancer, non-small cell lung cancer, and pancreatic cancer. Docetaxel is approved for treating breast cancer, non-small cell lung cancer, and prostate cancer. Cabazitaxel is approved for treating prostate cancer. However, taxanes have not yet been approved for HCC. Only a few clinical studies for taxanes in HCC have been previously performed. Phase II trials of paclitaxel and docetaxel have not produced satisfactory results [51,52] in unresectable and advanced HCC patients, respectively. Our bioinformatics analysis may provide a basis for further clinical trial designs of taxanes for HCC using TP53/CTNNB1 mutation as biomarkers. However, one limitation is that only a few HCC cell lines with different TP53/CTNNB1 gene statuses were used to predict sensitivities to paclitaxel treatment. More HCC cell lines, or more clinically relevant patient-derived organoids, should be used to confirm these results.
The major effect of taxanes is to stabilize microtubules [37]. Our analysis showed that the main targets for paclitaxel are CDK1, CCNB1, BIRC5, KIF2C, STMN1, PRC1, and AURKA. Several of these are associated with microtubules. For example, STMN1 is a microtubule-destabilizing protein whose expression is upregulated by gain-of-function mutant p53 during HCC development. Loss of STMN1 sensitizes HCC tumor cells to microtubule-targeting agents, including paclitaxel [53]. PRC1 is a microtubule-binding protein regulating cytokinesis. Inhibition of PRC1 and paclitaxel treatment exhibits synergistic anticancer activity against HCC [54]. KIF2C, a mitotic centromere-associated kinesin, is a microtubule-based motor protein that serves as a therapeutic target for HCC [54]. BIRC5, also known as survivin, is a microtubule-associated protein and participates in the assembly of the bipolar mitotic spindle [55]. Therefore, targeting the mitotic gene signature in HCC may influence microtubule dynamics, leading to the enhancement in taxane’s anticancer activity.
Drug discovery is still a risky, time-consuming, and expensive process, with only a few novel anticancer medications receiving approval in recent years [56,57,58]. Drug repurposing is an unconventional strategy that uses existing therapeutic drugs to treat new disease indications or specific patient populations [59,60,61]. Drug repurposing has several advantages, including cost savings and bypassing safety concerns, since extensive drug data are frequently available [59,60,61]. Because taxanes have been used as anticancer chemotherapy for decades [49,50], repurposing taxanes such as paclitaxel to treat HCC would be a feasible strategy.
5. Conclusions
In conclusion, we used bioinformatic approaches to establish a predictive mitotic gene signature in HCC linked to the mutation statuses of the TP53 and CTNNB1 genes. We also discovered that paclitaxel, a clinically approved anticancer drug, can be utilized to treat HCC patients with mutant TP53 or wild-type CTNNB1 genes, providing a precision treatment option for the future.
Acknowledgments
This work was financially supported by the TMU Research Center of Cancer Translational Medicine from The Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the Ministry of Education (MOE) in Taiwan.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/jpm11111199/s1, Figure S1: The correlation between CTNNB1 gene mutation and mRNA expression levels in CTRP-HCC (A) and TCGA-LIHC (B) data sets, Table S1: The TP53 and CTNNB1 gene statuses in HCC cell lines, File S1: The differentially expressed genes (DEGs) prepared from microarray data sets.
Author Contributions
Conceptualization, J.-C.L. and P.-M.Y.; methodology, J.-C.L., V.A., M.A. and C.-Y.W.; validation, J.-C.L.; formal analysis, J.-C.L.; investigation, J.-C.L.; resources, T.-P.L., C.-Y.W. and P.-M.Y.; data curation, T.-P.L. and P.-M.Y.; writing—original draft preparation, T.-P.L. and P.-M.Y.; writing—review and editing, T.-P.L. and P.-M.Y.; visualization, J.-C.L., T.-P.L., V.A., M.A., C.-Y.W. and P.-M.Y.; supervision, T.-P.L. and P.-M.Y.; project administration, P.-M.Y.; funding acquisition, T.-P.L. and P.-M.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Ministry of Science and Technology, grant numbers MOST109-2314-B-195-006, MOST109-2314-B-038-040, and MOST110-2314-B-195-022; Mackay Memorial Hospital, grant numbers MMH-108-086, MMH110-09, and MMH-110-79; the health and welfare surcharge of tobacco products (WanFang Hospital, Chi-Mei Medical Center, and Hualien Tzu-Chi Hospital Joing Cancer Center Grant-Focus on Colon Cancer Research), grant number MOHW110-TDU-B-212-144020.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data supporting this study can be obtained from the public databases or are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sung H., Ferlay J., Siegel R.L., Laversanne M., Soerjomataram I., Jemal A., Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Rossetto A., De Re V., Steffan A., Ravaioli M., Miolo G., Leone P., Racanelli V., Uzzau A., Baccarani U., Cescon M. Carcinogenesis and Metastasis in Liver: Cell Physiological Basis. Cancers. 2019;11:1731. doi: 10.3390/cancers11111731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Craig A.J., von Felden J., Garcia-Lezana T., Sarcognato S., Villanueva A. Tumour evolution in hepatocellular carcinoma. Nat. Rev. Gastroenterol. Hepatol. 2020;17:139–152. doi: 10.1038/s41575-019-0229-4. [DOI] [PubMed] [Google Scholar]
- 4.Yang J.D., Hainaut P., Gores G.J., Amadou A., Plymoth A., Roberts L.R. A global view of hepatocellular carcinoma: Trends, risk, prevention and management. Nat. Rev. Gastroenterol. Hepatol. 2019;16:589–604. doi: 10.1038/s41575-019-0186-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Llovet J.M., Montal R., Sia D., Finn R.S. Molecular therapies and precision medicine for hepatocellular carcinoma. Nat. Rev. Clin. Oncol. 2018;15:599–616. doi: 10.1038/s41571-018-0073-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roberts L.R., Gores G.J. Hepatocellular carcinoma: Molecular pathways and new therapeutic targets. Semin. Liver Dis. 2005;25:212–225. doi: 10.1055/s-2005-871200. [DOI] [PubMed] [Google Scholar]
- 7.Llovet J.M., Ricci S., Mazzaferro V., Hilgard P., Gane E., Blanc J.F., de Oliveira A.C., Santoro A., Raoul J.L., Forner A., et al. Sorafenib in advanced hepatocellular carcinoma. N. Engl. J. Med. 2008;359:378–390. doi: 10.1056/NEJMoa0708857. [DOI] [PubMed] [Google Scholar]
- 8.Bruix J., Qin S., Merle P., Granito A., Huang Y.H., Bodoky G., Pracht M., Yokosuka O., Rosmorduc O., Breder V., et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;389:56–66. doi: 10.1016/S0140-6736(16)32453-9. [DOI] [PubMed] [Google Scholar]
- 9.Kudo M., Finn R.S., Qin S., Han K.H., Ikeda K., Piscaglia F., Baron A., Park J.W., Han G., Jassem J., et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: A randomised phase 3 non-inferiority trial. Lancet. 2018;391:1163–1173. doi: 10.1016/S0140-6736(18)30207-1. [DOI] [PubMed] [Google Scholar]
- 10.Abou-Alfa G.K., Meyer T., Cheng A.L., El-Khoueiry A.B., Rimassa L., Ryoo B.Y., Cicin I., Merle P., Chen Y., Park J.W., et al. Cabozantinib in Patients with Advanced and Progressing Hepatocellular Carcinoma. N. Engl. J. Med. 2018;379:54–63. doi: 10.1056/NEJMoa1717002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheng A.L., Kang Y.K., Chen Z., Tsao C.J., Qin S., Kim J.S., Luo R., Feng J., Ye S., Yang T.S., et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: A phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009;10:25–34. doi: 10.1016/S1470-2045(08)70285-7. [DOI] [PubMed] [Google Scholar]
- 12.Zhu A.X., Kang Y.K., Yen C.J., Finn R.S., Galle P.R., Llovet J.M., Assenat E., Brandi G., Pracht M., Lim H.Y., et al. Ramucirumab after sorafenib in patients with advanced hepatocellular carcinoma and increased alpha-fetoprotein concentrations (REACH-2): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019;20:282–296. doi: 10.1016/S1470-2045(18)30937-9. [DOI] [PubMed] [Google Scholar]
- 13.El-Khoueiry A.B., Sangro B., Yau T., Crocenzi T.S., Kudo M., Hsu C., Kim T.Y., Choo S.P., Trojan J., Welling T.H.R., et al. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): An open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet. 2017;389:2492–2502. doi: 10.1016/S0140-6736(17)31046-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhu A.X., Finn R.S., Edeline J., Cattan S., Ogasawara S., Palmer D., Verslype C., Zagonel V., Fartoux L., Vogel A., et al. Pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib (KEYNOTE-224): A non-randomised, open-label phase 2 trial. Lancet Oncol. 2018;19:940–952. doi: 10.1016/S1470-2045(18)30351-6. [DOI] [PubMed] [Google Scholar]
- 15.Saung M.T., Pelosof L., Casak S., Donoghue M., Lemery S., Yuan M., Rodriguez L., Schotland P., Chuk M., Davis G., et al. FDA Approval Summary: Nivolumab Plus Ipilimumab for the Treatment of Patients with Hepatocellular Carcinoma Previously Treated with Sorafenib. Oncologist. 2021;26:797–806. doi: 10.1002/onco.13819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nassar S.F., Raddassi K., Ubhi B., Doktorski J., Abulaban A. Precision Medicine: Steps along the Road to Combat Human Cancer. Cells. 2020;9:2056. doi: 10.3390/cells9092056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu Y., Liu Z., Xu X. Molecular subtyping of hepatocellular carcinoma: A step toward precision medicine. Cancer Commun. 2020;40:681–693. doi: 10.1002/cac2.12115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Minagawa M., Ikai I., Matsuyama Y., Yamaoka Y., Makuuchi M. Staging of hepatocellular carcinoma—Assessment of the Japanese TNM and AICCIUICC TNM systems in a cohort of 13,772 patients in Japan. Ann. Surg. 2007;245:909–922. doi: 10.1097/01.sla.0000254368.65878.da. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schulze K., Imbeaud S., Letouze E., Alexandrov L.B., Calderaro J., Rebouissou S., Couchy G., Meiller C., Shinde J., Soysouvanh F., et al. Exome sequencing of hepatocellular carcinomas identifies new mutational signatures and potential therapeutic targets. Nat. Genet. 2015;47:505–511. doi: 10.1038/ng.3252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fujimoto A., Furuta M., Totoki Y., Tsunoda T., Kato M., Shiraishi Y., Tanaka H., Taniguchi H., Kawakami Y., Ueno M., et al. Whole-genome mutational landscape and characterization of noncoding and structural mutations in liver cancer. Nat. Genet. 2016;48:500–509. doi: 10.1038/ng.3547. [DOI] [PubMed] [Google Scholar]
- 21.Roessler S., Jia H.L., Budhu A., Forgues M., Ye Q.H., Lee J.S., Thorgeirsson S.S., Sun Z., Tang Z.Y., Qin L.X., et al. A unique metastasis gene signature enables prediction of tumor relapse in early-stage hepatocellular carcinoma patients. Cancer Res. 2010;70:10202–10212. doi: 10.1158/0008-5472.CAN-10-2607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang H.W., Hsieh T.H., Huang S.Y., Chau G.Y., Tung C.Y., Su C.W., Wu J.C. Forfeited hepatogenesis program and increased embryonic stem cell traits in young hepatocellular carcinoma (HCC) comparing to elderly HCC. BMC Genom. 2013;14:736. doi: 10.1186/1471-2164-14-736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Neumann O., Kesselmeier M., Geffers R., Pellegrino R., Radlwimmer B., Hoffmann K., Ehemann V., Schemmer P., Schirmacher P., Lorenzo Bermejo J., et al. Methylome analysis and integrative profiling of human HCCs identify novel protumorigenic factors. Hepatology. 2012;56:1817–1827. doi: 10.1002/hep.25870. [DOI] [PubMed] [Google Scholar]
- 24.Wilhite S.E., Barrett T. Strategies to explore functional genomics data sets in NCBI’s GEO database. Methods Mol. Biol. 2012;802:41–53. doi: 10.1007/978-1-61779-400-1_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tang Z., Kang B., Li C., Chen T., Zhang Z. GEPIA2: An enhanced web server for large-scale expression profiling and interactive analysis. Nucleic Acids Res. 2019;47:W556–W560. doi: 10.1093/nar/gkz430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cerami E., Gao J., Dogrusoz U., Gross B.E., Sumer S.O., Aksoy B.A., Jacobsen A., Byrne C.J., Heuer M.L., Larsson E., et al. The cBio cancer genomics portal: An open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012;2:401–404. doi: 10.1158/2159-8290.CD-12-0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gao J., Aksoy B.A., Dogrusoz U., Dresdner G., Gross B., Sumer S.O., Sun Y., Jacobsen A., Sinha R., Larsson E., et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci. Signal. 2013;6:pl1. doi: 10.1126/scisignal.2004088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Szklarczyk D., Gable A.L., Lyon D., Junge A., Wyder S., Huerta-Cepas J., Simonovic M., Doncheva N.T., Morris J.H., Bork P., et al. STRING v11: Protein-protein association networks with increased coverage, supporting functional discovery in genome-wide experimental datasets. Nucleic Acids Res. 2019;47:D607–D613. doi: 10.1093/nar/gky1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jourquin J., Duncan D., Shi Z., Zhang B. GLAD4U: Deriving and prioritizing gene lists from PubMed literature. BMC Genom. 2012;13((Suppl. 8)):S20. doi: 10.1186/1471-2164-13-S8-S20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liao Y., Wang J., Jaehnig E.J., Shi Z., Zhang B. WebGestalt 2019: Gene set analysis toolkit with revamped UIs and APIs. Nucleic Acids Res. 2019;47:W199–W205. doi: 10.1093/nar/gkz401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Szklarczyk D., Santos A., von Mering C., Jensen L.J., Bork P., Kuhn M. STITCH 5: Augmenting protein-chemical interaction networks with tissue and affinity data. Nucleic Acids Res. 2016;44:D380–D384. doi: 10.1093/nar/gkv1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Luna A., Elloumi F., Varma S., Wang Y., Rajapakse V.N., Aladjem M.I., Robert J., Sander C., Pommier Y., Reinhold W.C. CellMiner Cross-Database (CellMinerCDB) version 1.2: Exploration of patient-derived cancer cell line pharmacogenomics. Nucleic Acids Res. 2021;49:D1083–D1093. doi: 10.1093/nar/gkaa968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Basu A., Bodycombe N.E., Cheah J.H., Price E.V., Liu K., Schaefer G.I., Ebright R.Y., Stewart M.L., Ito D., Wang S., et al. An interactive resource to identify cancer genetic and lineage dependencies targeted by small molecules. Cell. 2013;154:1151–1161. doi: 10.1016/j.cell.2013.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rees M.G., Seashore-Ludlow B., Cheah J.H., Adams D.J., Price E.V., Gill S., Javaid S., Coletti M.E., Jones V.L., Bodycombe N.E., et al. Correlating chemical sensitivity and basal gene expression reveals mechanism of action. Nat. Chem. Biol. 2016;12:109–116. doi: 10.1038/nchembio.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Seashore-Ludlow B., Rees M.G., Cheah J.H., Cokol M., Price E.V., Coletti M.E., Jones V., Bodycombe N.E., Soule C.K., Gould J., et al. Harnessing Connectivity in a Large-Scale Small-Molecule Sensitivity Dataset. Cancer Discov. 2015;5:1210–1223. doi: 10.1158/2159-8290.CD-15-0235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Crncec A., Hochegger H. Triggering mitosis. FEBS Lett. 2019;593:2868–2888. doi: 10.1002/1873-3468.13635. [DOI] [PubMed] [Google Scholar]
- 37.Jordan M.A., Wilson L. Microtubules as a target for anticancer drugs. Nat. Rev. Cancer. 2004;4:253–265. doi: 10.1038/nrc1317. [DOI] [PubMed] [Google Scholar]
- 38.Ha S.Y., Choi M., Lee T., Park C.K. The Prognostic Role of Mitotic Index in Hepatocellular Carcinoma Patients after Curative Hepatectomy. Cancer Res. Treat. 2016;48:180–189. doi: 10.4143/crt.2014.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nanashima A., Tanaka K., Yamaguchi H., Shibasaki S., Morino S., Yoshinaga M., Sawai T., Nakagoe T., Ayabe H. Fibrosis and inflammatory activity in noncancerous tissue and mitotic index of cancer tissue in patients with hepatocellular carcinoma: Relationship to clinicopathological factors and prognosis after hepatic resection. Dig. Dis. Sci. 2003;48:1517–1522. doi: 10.1023/A:1024759606402. [DOI] [PubMed] [Google Scholar]
- 40.Ouchi K., Sugawara T., Ono H., Fujiya T., Kamiyama Y., Kakugawa Y., Mikuni J., Yamanami H., Komatsu S., Horikoshi A. Mitotic index is the best predictive factor for survival of patients with resected hepatocellular carcinoma. Dig. Surg. 2000;17:42–48. doi: 10.1159/000018799. [DOI] [PubMed] [Google Scholar]
- 41.Nagao T., Kondo F., Sato T., Nagato Y., Kondo Y. Immunohistochemical detection of aberrant p53 expression in hepatocellular carcinoma: Correlation with cell proliferative activity indices, including mitotic index and MIB-1 immunostaining. Hum. Pathol. 1995;26:326–333. doi: 10.1016/0046-8177(95)90066-7. [DOI] [PubMed] [Google Scholar]
- 42.Liu Z., Liu X., Liang J., Liu Y., Hou X., Zhang M., Li Y., Jiang X. Immunotherapy for Hepatocellular Carcinoma: Current Status and Future Prospects. Front. Immunol. 2021;12:765101. doi: 10.3389/fimmu.2021.765101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chan T.A., Yarchoan M., Jaffee E., Swanton C., Quezada S.A., Stenzinger A., Peters S. Development of tumor mutation burden as an immunotherapy biomarker: Utility for the oncology clinic. Ann. Oncol. 2019;30:44–56. doi: 10.1093/annonc/mdy495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li L., Rao X., Wen Z., Ding X., Wang X., Xu W., Meng C., Yi Y., Guan Y., Chen Y., et al. Implications of driver genes associated with a high tumor mutation burden identified using next-generation sequencing on immunotherapy in hepatocellular carcinoma. Oncol. Lett. 2020;19:2739–2748. doi: 10.3892/ol.2020.11372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ou Q., Yu Y., Li A., Chen J., Yu T., Xu X., Xie X., Chen Y., Lin D., Zeng Q., et al. Association of survival and genomic mutation signature with immunotherapy in patients with hepatocellular carcinoma. Ann. Transl Med. 2020;8:230. doi: 10.21037/atm.2020.01.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sun X., Sun J., Yuan W., Gao X., Fu M., Xue A., Li H., Shu P., Fang Y., Hou Y., et al. Immune Cell Infiltration and the Expression of PD-1 and PD-L1 in Primary PDGFRA-Mutant Gastrointestinal Stromal Tumors. J. Gastrointest. Surg. 2021;25:2091–2100. doi: 10.1007/s11605-020-04860-8. [DOI] [PubMed] [Google Scholar]
- 47.Harding J.J., Nandakumar S., Armenia J., Khalil D.N., Albano M., Ly M., Shia J., Hechtman J.F., Kundra R., El Dika I., et al. Prospective Genotyping of Hepatocellular Carcinoma: Clinical Implications of Next-Generation Sequencing for Matching Patients to Targeted and Immune Therapies. Clin. Cancer Res. 2019;25:2116–2126. doi: 10.1158/1078-0432.CCR-18-2293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pinyol R., Sia D., Llovet J.M. Immune Exclusion-Wnt/CTNNB1 Class Predicts Resistance to Immunotherapies in HCC. Clin. Cancer Res. 2019;25:2021–2023. doi: 10.1158/1078-0432.CCR-18-3778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rowinsky E.K. The development and clinical utility of the taxane class of antimicrotubule chemotherapy agents. Annu. Rev. Med. 1997;48:353–374. doi: 10.1146/annurev.med.48.1.353. [DOI] [PubMed] [Google Scholar]
- 50.Ojima I., Lichtenthal B., Lee S., Wang C., Wang X. Taxane anticancer agents: A patent perspective. Expert Opin. Ther. Pat. 2016;26:1–20. doi: 10.1517/13543776.2016.1111872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chao Y., Chan W.K., Birkhofer M.J., Hu O.Y., Wang S.S., Huang Y.S., Liu M., Whang-Peng J., Chi K.H., Lui W.Y., et al. Phase II and pharmacokinetic study of paclitaxel therapy for unresectable hepatocellular carcinoma patients. Br. J. Cancer. 1998;78:34–39. doi: 10.1038/bjc.1998.438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hebbar M., Ernst O., Cattan S., Dominguez S., Oprea C., Mathurin P., Triboulet J.P., Paris J.C., Pruvot F.R. Phase II trial of docetaxel therapy in patients with advanced hepatocellular carcinoma. Oncology. 2006;70:154–158. doi: 10.1159/000093007. [DOI] [PubMed] [Google Scholar]
- 53.Singer S., Ehemann V., Brauckhoff A., Keith M., Vreden S., Schirmacher P., Breuhahn K. Protumorigenic overexpression of stathmin/Op18 by gain-of-function mutation in p53 in human hepatocarcinogenesis. Hepatology. 2007;46:759–768. doi: 10.1002/hep.21736. [DOI] [PubMed] [Google Scholar]
- 54.Liu X., Li Y., Meng L., Liu X.Y., Peng A., Chen Y., Liu C., Chen H., Sun S., Miao X., et al. Reducing protein regulator of cytokinesis 1 as a prospective therapy for hepatocellular carcinoma. Cell Death Dis. 2018;9:534. doi: 10.1038/s41419-018-0555-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fortugno P., Wall N.R., Giodini A., O’Connor D.S., Plescia J., Padgett K.M., Tognin S., Marchisio P.C., Altieri D.C. Survivin exists in immunochemically distinct subcellular pools and is involved in spindle microtubule function. J. Cell Sci. 2002;115:575–585. doi: 10.1242/jcs.115.3.575. [DOI] [PubMed] [Google Scholar]
- 56.Hay M., Thomas D.W., Craighead J.L., Economides C., Rosenthal J. Clinical development success rates for investigational drugs. Nat. Biotechnol. 2014;32:40–51. doi: 10.1038/nbt.2786. [DOI] [PubMed] [Google Scholar]
- 57.Mullard A. 2015 FDA drug approvals. Nat. Rev. Drug Discov. 2016;15:73–76. doi: 10.1038/nrd.2016.15. [DOI] [PubMed] [Google Scholar]
- 58.Mullard A. 2016 FDA drug approvals. Nat. Rev. Drug Discov. 2017;16:73–76. doi: 10.1038/nrd.2017.14. [DOI] [PubMed] [Google Scholar]
- 59.Pantziarka P., Bouche G., Meheus L., Sukhatme V., Sukhatme V.P., Vikas P. The Repurposing Drugs in Oncology (ReDO) Project. Ecancermedicalscience. 2014;8:442. doi: 10.3332/ecancer.2014.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sleire L., Forde H.E., Netland I.A., Leiss L., Skeie B.S., Enger P.O. Drug repurposing in cancer. Pharmacol. Res. 2017;124:74–91. doi: 10.1016/j.phrs.2017.07.013. [DOI] [PubMed] [Google Scholar]
- 61.Ashburn T.T., Thor K.B. Drug repositioning: Identifying and developing new uses for existing drugs. Nat. Rev. Drug Discov. 2004;3:673–683. doi: 10.1038/nrd1468. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data supporting this study can be obtained from the public databases or are available on request from the corresponding author.