Abstract
Idiopathic pulmonary fibrosis (IPF) is a chronic, progressive, fibrosing interstitial lung disease (ILD) of unknown aetiology, with a median survival of 2–4 years from the time of diagnosis. Although IPF has unknown aetiology by definition, there have been identified several risks factors increasing the probability of the onset and progression of the disease in IPF patients such as cigarette smoking and environmental risk factors associated with domestic and occupational exposure. Among them, cigarette smoking together with concomitant emphysema might predispose IPF patients to lung cancer (LC), mostly to non-small cell lung cancer (NSCLC), increasing the risk of lung cancer development. To this purpose, IPF and LC share several cellular and molecular processes driving the progression of both pathologies such as fibroblast transition proliferation and activation, endoplasmic reticulum stress, oxidative stress, and many genetic and epigenetic markers that predispose IPF patients to LC development. Nintedanib, a tyrosine–kinase inhibitor, was firstly developed as an anticancer drug and then recognized as an anti-fibrotic agent based on the common target molecular pathway. In this review our aim is to describe the updated studies on common cellular and molecular mechanisms between IPF and lung cancer, knowledge of which might help to find novel therapeutic targets for this disease combination.
Keywords: idiopathic pulmonary fibrosis, lung cancer, myofibroblast, cancer associated fibroblasts (CAFs), mechanotrasduction
1. Introduction
Interstitial lung diseases represent a broad spectrum of lung pathologies that affect the lung parenchyma causing diffuse inflammation and fibrosis [1]. Among them, idiopathic pulmonary fibrosis (IPF) is a rare lung disease with an unknown cause and a median survival of 2–4 years from the time of diagnosis. The onset and progression of IPF leads to massive changes in the architecture of lungs and their biomechanical properties that often culminate in respiratory failure due to the impairment of alveolar gas-exchange and the decline of lung functions [2,3]. Although the diagnosis of IPF can be extremely challenging due to the heterogenous nature of this disease [4], it is recognized by clinicopathological criteria, including the radiographic and histological hallmarks pattern of usual interstitial pneumonia (UIP) [5]. Currently, there are two antifibrotic drugs used as a therapeutic strategy for IPF patients, Pirfenidone and Nintedanib, that are able to slow down the respiratory functional decline and improve survival in IPF patients [6,7,8]. Despite this, IPF still has a high mortality rate and the survival times are quite heterogenous [9,10,11]. Although IPF is idiopathic by definition and is not classified as a genetic disease, there are both environmental and genetic risk factors (or “genetic susceptibility”) that can play a fundamental role in the initiation and progression of IPF [12,13]. Among them, the most studied and validated genetic risk factor is represented by the single nucleotide polymorphism in the promoter region of the mucin 5B (MUC5B) responsible for sporadic and familial IPF [12]. Furthermore, among the environmental risks there are exposure to cigarette smoke and inhalation of wood and metal dust, which might severely affect “genetically susceptible” patients [14] with the resulting alteration in the regulation of key genes contributing to the pathogenesis of IPF. Several studies have demonstrated that viral infection, including with the recently prominent SARS-CoV-2, might be responsible for the initiation or exacerbation of pulmonary fibrosis. In particular, it has been postulated that the “cytokine storm” caused by the exaggerated inflammatory response following SARS-CoV-2 infection, as well as micro-thrombotic hypotheses, may predispose patients with COVID-19 pneumonia to aberrant mechanisms of repair and fibrosis [15] culminating in acute lung injury and interstitial lung disease [16]. Although different prospective studies aiming to investigate the long-term pulmonary consequences of COVID-19 are still ongoing, it has been observed in the study of Wu et al. that about 40% of 201 patients with COVID-19 pneumonia developed acute respiratory distress syndrome (ARDS) [17]. Indeed, like SARS-CoV-2, the other two known coronaviruses, both the severe acute respiratory syndrome coronavirus (SARS-CoV; SARS) and Middle East respiratory syndrome coronavirus (MERS-CoV; MERS), caused in some patients interstitial abnormalities and lung functional decline. [18,19].
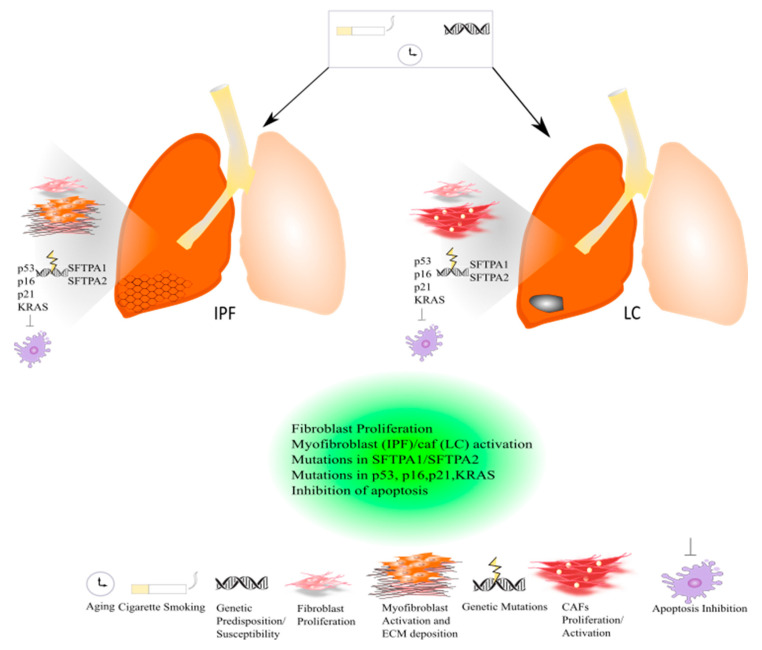
In the past few years, there has been growing interest in the role of comorbidities in IPF study. Smoking history, elderly age, male sex, and emphysema might represent strong risk factors for developing lung cancer (LC) in IPF patients; thus, besides the concomitant risk factors, IPF itself might be considered a risk factor for lung carcinogenesis [20,21,22]. Lung cancer is the most diffuse cause of cancer death worldwide. It has been estimated that about 85% of LC patients have a diagnosis of non-small cell lung cancer (NSLC). In the majority of patients, the onset of LC is related to tobacco smoking [23] (Figure 1).
Figure 1.
Common pathogenic mechanisms between lung cancer and IPF.
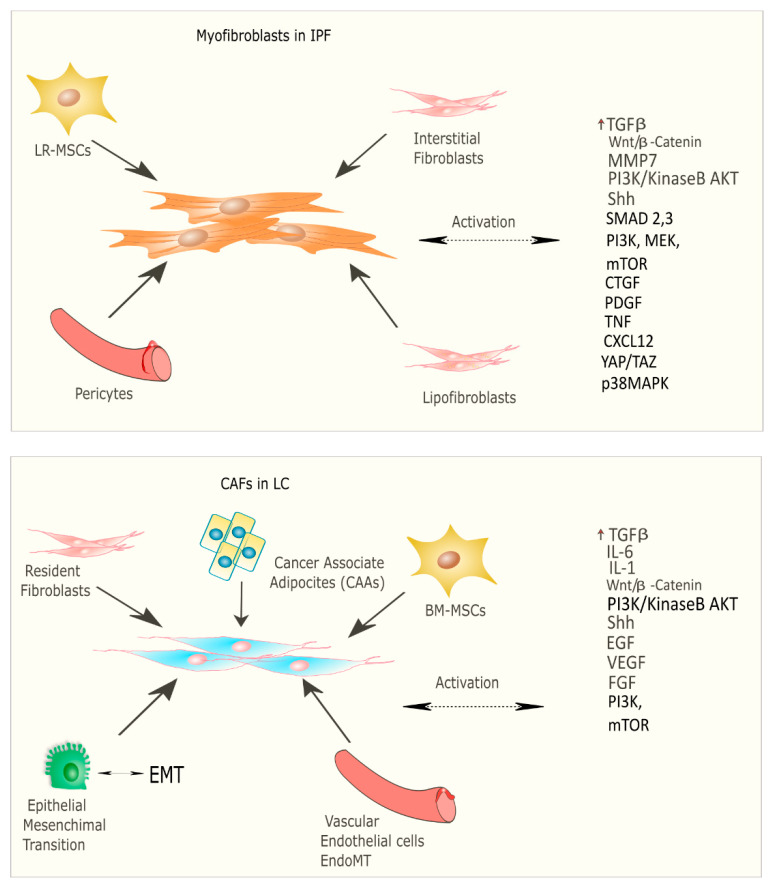
Recent studies have focused on the identification of common molecular pathways between IPF and LC for a better therapeutic strategy and optimal management of patients with both diseases. There are many common cellular and molecular mechanisms that might predispose patients to the onset and development of IPF and LC such as the activation and proliferation of both myofibroblasts (IPF) and cancer-associated fibroblasts (CAFs), and the alteration of growth factors expression level [24]. Myofibroblasts represent the cellular key players in IPF since their proliferation and activation under profibrotic stimuli lead to the secretion and deposition of extracellular matrix (ECM) proteins, which are responsible for causing fibrosis [25]. Thus, this process culminates in increased lung structural rigidity that compromises the lung’s biomechanical properties and thickens of the alveolar–capillary barrier with aberrant alveolar gas exchange function. According to recent investigations, the myofibroblasts derive from different lung resident cell populations such as the interstitial lung fibroblasts, the lipofibroblasts [26], lung resident mesenchymal stromal cells (LR-MSCs) [27,28], the perycites [29] and mesothelial cells [30], ruling out the contribution of both epithelial cells in the so-called epithelial mesenchymal transition (EMT) [31] and circulating fibrocytes [32]. In LC, cancer-associated fibroblasts (CAFs) are the cellular key players, like myofibroblasts in IPF pathogenesis [33]. Several studies have been focused on the identification of the origins, biological characteristics, and the role of CAFs as the major component of the stroma during carcinogenesis. Intriguingly, among the components of the tumour microenvironment (TME), CAFs play a fundamental role in drug resistance in NSCLC, protecting tumours from the effects of chemotherapeutic drugs [34,35]. As is the case with IPF, there are several hypotheses still under debate regarding the cellular sources of CAFs in tumours; among them are (1) the resident fibroblasts, which can differentiate to CAFs during the course of tumour progression under the orchestration of specific signalling pathways; (2) cancer associated adipocytes (CAAs) that are present in tumour stroma and might derive from circulating progenitors in the bone marrow [36]; (3) bone-marrow-derived mesenchymal stromal cells (BM-MSCs) and hematopoietic stem cells (HSCs) [37]; (4) epithelial cells through the epithelial mesenchymal transition (EMT) [38]; (5) vascular endothelial cells through the endothelial–mesenchymal transition (EndMT), crucial for tumour angiogenesis [39] (Figure 2) Thus, CAFs exhibit high heterogeneity in terms of origin as well as surface markers and resident organs. During malignancy while the tumour progresses, CAFs contribute to promote tumour growth, metastasis, and drug resistance. Here, tumor cells together with non-malignant stromal cells trigger CAF activation through inflammatory mediators such as transforming growth factor beta (TGF-β), interleukin (IL)-1, and interleukin (IL)-6 that contribute to inflammation and carcinogenesis [40,41]. To this purpose, TGF-β that can be considered as a master molecular regulator of profibrotic signaling, promoting lung cancer progression and triggering mitogenic stimuli to lung cancer cells. Furthermore, among the common signalling pathways characterizing both IPF and LC progression, there is the Wnt/β-catenin pathway that has been involved both in cancer progression and the EMT process through its target genes, cyclin-D1 and matrix metalloproteinase (MMP)-7, contributing to the pathogenesis of IPF [42]. Aberrant activation of phosphoinositide 3-kinase (PI3K)/protein kinase B (AKT) causes cancer invasion and the progression of lung fibrosis [43] with the activation of profibrotic downstream signalling mediators such as TGF-β1 and platelet-derived growth factor (PDGF). The sonic hedgehog (Shh) pathway is also activated both in bronchial epithelial cells of honeycomb cysts and in cancer fibroblasts, being responsible for resistance to fibroblast apoptosis, tumour growth, metastasis, and chemotherapy resistance [44]. (Figure 2) Furthermore, cellular senescence is associated with the progression of pulmonary fibrosis through different mechanisms and central players in the lung niche. Among them, Wiley et al. [45] demonstrated that the biologically active profibrotic lipids, namely the leukotrienes (LT), are involved in the senescence-associated secretory phenotype (SASP) which represents one of the mechanisms responsible for the progression of pulmonary fibrosis. They demonstrated that the LT-rich conditioned medium (CM) of senescent lung fibroblasts triggered profibrotic signalling in modified fibroblasts treated with inhibitors of ALOX5, the main enzyme in LT biosynthesis [45]. To this purpose, another recent study from Li et al. [46], stated that blocking the biosynthesis of leukotriene B4 (LTB4) would be an efficient therapeutic strategy in the treatment of both IPF and acute lung injury (ALI). They performed in vivo experiments, where they observed a decreased neutrophilic inflammation in an IPF mouse model at early stage, as well as decreased LPS-induced ALI through LTB4 blocking biosynthesis in vivo. Indeed, several works have been published about the role of LT in lung cancer progression. Among them, Poczobutt et al. [47] showed a selective production of leukotrienes by inflammatory cells of the microenvironment during lung cancer progression through an orthotopic model of lung cancer progression and by liquid chromatograph coupled with tandem mass spectrometry (LC/MS/MS) [47].
Figure 2.
Origin and signalling pathway leading to the activation of myofibroblasts in IPF and CAFs in LC.
Indeed, there are also common genetic mechanisms shared by both diseases based on mutations in surfactant protein genes (SFTPA2-A1) that lead to impaired protein secretion, endoplasmic reticular stress, and apoptosis, culminating in the onset and progression of IPF or adenocarcinoma [24]. (Figure 1) To date, the approved IPF therapies, Pirfenidone and Nintedanib, are also active in LC. In particular, Nintedanib is approved as a treatment in NSCLC, and Pirfenidone has shown anti-neoplastic effects in preclinical studies [24]. Hence, with this review we would like to summarize and clarify the mechanisms implicated in the development of both IPF and LC patients highlighting the similarities in the pathogenesis of both diseases. Hopefully, this would ameliorate the prognosis, opening the possibility of new therapeutic strategies and improving survival among IPF-LC patients.
2. Diagnostic Approaches for Idiopathic Pulmonary Fibrosis and Lung Cancer
Idiopathic pulmonary fibrosis (IPF) is a rare pulmonary disease with an incidence ranging from 0.09 to 0.49 in Europe [48]. Among these patients, there is an increased risk of developing lung cancer (LC), with a relative prevalence reported from 2.7% to 48% [49,50]. The correlation between IPF and lung cancer is still being debated [6], although recent studies have demonstrated possible connections [49,50]. In particular, Ozawa et al. [51] showed an increased incidence of lung cancer in a retrospective study of 103 patients with IPF. Similar results have been described by Tomassetti et al. [52], with cancer occurring in 30% of studied patients. One of the most interesting approaches was to analyze the period of onset of lung cancer in IPF-LC patients. In 2021, Alomaish H. et al. [53] reported a LC incidence of 13,5% IPF patients. Because lung cancer has a high incidence in patients with IPF having an important impact on the survival of these patients, the scientific community has focused its attention on identifying predictive factors for lung cancer in IPF patients [54,55,56]. These characteristics are mainly described in older patients with IPF at diagnosis who have a history of smoking and emphysema [51,56,57]. However, the causes inducing lung cancer in this population of patients have not been clarified yet [58,59]. One of the most interesting aspects, which seems important to consider, is a rapid annual decline of forced vital capacity (FVC) as a lung-cancer-predisposing factor [60]. In particular, it seems that tissue damage and abnormal repair is the key to the connections between IPF and LC [59]. Indeed, it has been thought that patients with a very rapid decrease in FVC and consequent IPF progression are more sensitive to lung cancer development; however, further studies will need to be conducted to clarify the common factors between cancer and IPF. A recent study demonstrated a median time from IPF to lung cancer of 38 months [53], although Tomassetti et al. [52] found the time to be around 30 months. Besides the decrease in FVC and carbon monoxide diffusion capacity (DLCO) in patients who developed both IPF and LC, another aspect to investigate are the histopathological findings. Previous studies have shown that squamous cell carcinoma is the most common histologic type encountered in IPF [51,52,53,54,55,56,57,58,59,60,61,62]. This aspect would highlight the importance of considering older patients with a diagnosis of IPF who have a long and heavy history of smoking and whose median FVC and DLCO are slightly lower than normal [63]. In particular, radiological findings are crucial to consider since round or ovoid masses are frequently observed [64,65] in correspondance to the lower lobes [64,66]. The recent guidelines recommend an annual low-dose chest CT scan in high-risk patients [67,68], but there are no recommendations for IPF patients. It is probably important to consider screening patients with IPF, especially in the first two years after diagnosis, with an annual or shorter-term chest CT scan to follow the possible presence and evolution of lung cancer nodules [69]. Since recent studies have described a worse survival rate in patients with IPF and lung cancer [70,71], it would be fundamental to establish a surveillance protocol in order to set a diagnosis and medical treatment for these patients.
The scientific community believes that multidisciplinary approaches are the diagnostic gold standard for patients with moderate IPF and IPF-LC [72,73]. In particular, in patients with IPF of mild to moderate functional impairment (FVC > 50%, DLCO > 35%) and the association of an early-stage lung cancer or metastasis, the common approaches are surgery for the early stages and stereotactic radiotherapy for the advanced stages, together with anti-fibrotic treatments used for more than 50% of patients [74,75,76]. In critical patients with advanced IPF and operable lung cancer but impaired pulmonary function, the recommended treatments are anti-fibrotics, immune checkpoint inhibitors, and targeted therapy [73,77]. Another interesting aspect for diagnostic and therapeutic approaches is the identification of biomarkers, which represents the first step toward future personalized therapies for IPF [73,77]. These approaches may have an important impact in either preventing or monitoring lung cancer in IPF patients. To this purpose, in the last decades, several potential biomarkers have been discovered [78,79].
2.1. Diagnostic Biomarkers
The most studied biomarkers able to discriminate IPF from healthy donors are the markers Krebs von den Lungen (KL)-6 [80,81,82,83], the chitinase-like protein (YKL40) [84,85], leucocytes and circulating innate immune cells [78,79,80], and surfactant proteins (SP)-A, -B, -D [86,87,88,89,90,91]. Indeed, the matrix metalloproteinase (MMP7), at higher values, seems to show a higher risk of possible interstitial lung diseases [92]. In particular, MMP7 and MMP1 are important for making a differential diagnosis between IPF and hypersensitivity pneumonitis. The recent PROFILE (Prospective Study of Fibrosis in Lung Endpoints) study that analyzed the molecular profile of more than 100 serum proteins showed a significantly higher level of MMP1, MMP7, and SP-D in IPF patients compared with healthy people. Furthermore, it showed that oncostatin M and cytokeratin 19 fragments (CYFRA-21-1) were markers for IPF patients [54,93,94,95,96,97,98]. These biomarkers may be an important aspect to investigate in the future even for lung cancer. However, the settings of serum biomarkers for clinical perspectives for IPF monitoring and further lung cancer development are still lacking and have not been considered for diagnostic purposes in IPF [99].
2.2. Prognostic Biomarkers
Functional decline and respiratory function monitoring are the best approaches at the moment for setting and monitoring IPF progression [96,97], but the possibility has recently arisen of identifying biomarkers with prognostic purposes for IPF. Although the heterogeneity of IPF patients complicates the definition of a univocal approach, a composite scoring system incorporating lung physiology, sex, and age (GAP) is more accurate at predicting mortality [98,99]. These biomarkers seem to improve prognosis for IPF patients [100,101,102,103,104,105,106,107,108,109,110,111,112,113,114]. In particular, a high concentration of MMP7 correlates with IPF severity for the decline of lung function as well as worse survival of IPF [115]. For example, in the PROFILE study, the protein MMP1/8 (CRPM) indicates pulmonary disease progression and very poor overall survival [116]. Another interesting predictor for IPF as well as lung cancer seems to be surfactant protein D and the cancer antigen (CA)19-9 [117].
2.3. Radiological Biomarkers
As previously described, several studies defined the high-resolution computed tomography (HRCT) patterns as prospective prognostic biomarkers [118,119]. In particular, a recent study claims that the employment of specific CT-associated tool such as data-driven textural analysis (DTA) [120] associated with a visual and functional changes score, might be useful in predicting IPF progression [120]. However, the definition of a unique method and score set using HRCT characteristics associated with pulmonary function test results is still lacking. Recently, Jacob et al. [121] reported that a computer score set on the quantification of parenchymal patterns including vessel-related structure was able to predict IPF mortality and functional decline, representing a potential non-invasive method for estimating gas-exchange impairment in IPF [121,122].
In summary, keeping in mind the variability and uncertainty of the approaches, the best strategies that need to be considered in asymptomatic middle-aged smokers are: (1) a chest low-dose HRCT or regular CT conducted annually; (2) optimal selection of patients for surgical lung interventions, chemotherapy, and radiotherapy; (3) the role of anti-fibrotics in preventing and treating lung cancer and reducing acute exacerbations of IPF post-operatively; (4) the settings of new molecular biomarkers that may be useful as diagnostic and predictive factors for optimal monitoring of IPF. All these aspects will be better addressed through the setting of a future consensus statement for diagnosis and management of these patients in order to standardize the diagnostic and prognostic approaches as well as also develop more focused medical treatments.
3. Common Pathogenic Mechanisms between LC and IPF: Genetic and Epigenetic Alterations in Focus
Several studies going inside the pathogenesis of IPF and LC exhibit great similarity between both diseases concerning the abnormal activation of the signalling pathway, the cellular responses, the activation of lung fibroblasts and their proliferation. To date, there is a growing interest in the epigenetic and genetic abnormalities characterizing IPF and LC that might explain the concomitant manifestation of the two diseases. Although IPF is not considered a genetic disease, genome-wide association analysis (GWA) identified different genetic variants that account for almost 30% of IPF patients that together with the environmental risks play a crucial role in both sporadic and familial IPF [13,123,124]. Among these, the most studied genetic risk factor for both familial and sporadic IPF is the single nucleotide polymorphism rs35705950 in the promoter region of the mucin 5B (MUC5B) gene [12,125]. Normally, in the alveolar epithelium, MUC5B plays a pivotal role together with mucin 5AC (MUC5AC) in the muco-ciliary clearance (MCC), removing inhaled debris and pathogens and contributing to the maintenance of the overall lung homeostasis [126]. To this purpose, it has been shown that the overexpression of full-length murine MUC5B in the AECII of two lines of C57BL/6 mice compromised the muco-ciliary clearance activity, leading to an increase in lung fibrosis of bleomycin-treated mice [1]. Moreover, other genetic variants associated with sporadic and familial IPF are represented by: genes involved in cell–cell adhesion (DSP, DPP9) fundamental in the maintenance of epithelial integrity, genes involved in innate and adaptive immune response (Toll-like receptor signalling, TOLLIP, TLR3), surfactant protein genes (SFTPA2-A1), cytokines and growth factors (IL1RN, IL8, IL4, TGF-β1), genes involved in telomere maintenance (TERT, OBFC1), and cell-cycle regulation genes (KIF15, MAD1L1, CDKN1A, TP53) [127].
Different IPF-related genetic variants have been associated with the risk to develop lung cancer. Among these, there are mutations in surfactant protein genes (SFTPA1, SFTPA2,) that have been studied in lung adenocarcinoma that compromise protein secretion and promote endoplasmic reticular stress and apoptosis [128,129]. In familial IPF, genetic variants of telomerase complex components, such as TERT (telomerase reverse transcriptase) and TERC (telomerase RNA component), lead to shortened telomeres following by genomic instability [130]. To this purpose, several studies suggest a different role of telomerase in IPF and LC since it was found that the expression level of TERT and TERC was significantly lower in the lung tissue of IPF patients compared to NSCLC tissues and controls [131]. Indeed, mutations in the p53 gene that lead to a decrease in the apoptotic process together with mutations in p16, p21, and the Kirsten rat sarcoma virus gene (KRAS) have been found both in IPF and LC [132]. (Figure 1). Furthermore, Maher et al. performed the PROFILE study of a large cohort of IPF patients, four serum biomarkers predictive of disease progression, among which are the cancer-related genes CA-19 and CA-125 [133]. In addition, Allen et al. assessed the genomic profiles of IPF-LC using targeted exome sequencing where they found several somatic mutations, among which were the TP53 and BRAF genes, which were significantly mutated in IPF-LC [134]. Intriguingly, it has been demonstrated that epidermal growth factor receptor (EGFR) and anaplastic lymphoma kinase (ALK) mutations that normally drive the therapeutic decisions in the management of LC patients are either less frequent in IPF-LC adenocarcinoma patients compared with LC adenocarcinoma patients or have not been studied, respectively [135]. The enviromental risk factors, smoking exposure and aging, that might charaterize both IPF and LC patients might induce epigenetic responses such as changes in the methylation patterns that are quite similar between both diseases according to genome-wide methylation analysis [136]. Finally, recent studies show that IPF and LC share the aberrant expression of some microRNA. Among them, miR-21 was both upregulated in patients with IPF, [137] and correlated with poor prognosis in NSCLC patients according to the meta-analysis performed [138]. Finally, miR-29, miR-200, and let-7d were found to be downregulated both in the lung tissue of IPF patients and LC tissues [139,140]. However, it is important to mention that LC is endowed with metastatic potential, disseminating around the body (especially into the brain and bone), unlike IPF, which remains still localized to the lung.
Cigarette smoking together with genetic susceptibility/predisposition and aging can lead to the onset and progression of IPF and LC. Both diseases are characterized by common and similar pathogenic mechanisms. Both in IPF and lung cancer, a massive proliferation of lung resident fibroblasts occurs that contributes to the progression of IPF and lung cancer. In IPF, activated myofibroblasts promote the deposition of ECM leading to an acute exacerbation of the disease, while in lung cancer activated cancer-associated fibroblasts (CAFs) drive the carcinogenesis. Indeed, genetic mutations in surfactant proteins such as SFTPA1 and SFTPA2 have been studied both in familial IPF and lung cancer. Genetic mutations in the p53 gene that lead to a decrease in apoptosis and p16, p21, and KRAS have been found both in IPF and LC.
4. The Onset and Progression of IPF: The Leading Role of TGF-β1
According to the most recent studies, IPF is the result of aberrant functional epithelium due to aging and exposure to alveolar injuries together with compromised regenerative capacity of lung tissue that culminate in an imbalance between profibrotic and antifibrotic factors [141,142]. In particular, when injuries occur in normal alveolar lung epithelium, there is a depletion of alveolar epithelial cells 1 (AECI) that are deputed to the alveolar gas exchange functions, being located at the interface with lung vascular endothelium. Here, the depletion of AECI that strongly affects the integrity of lung alveolar epithelium is compensated by the action of alveolar epithelial cells 2 (AECII) that normally secrete the pulmonary surfactant to maintain surface tension, while in this exceptional situation they proliferate and differentiate into AECI. Thus, the AECII are able to ripristinate the integrity of alveolar epithelium during injuries, preserving its functionality [25]. In the lungs of IPF patients the AECII fail to repopulating the alveolar epithelium after their differentiation, compromising both the integrity of alveolar epithelium and the lung’s biomechanical properties. Consequently, this aberrant reparative mechanism of alveolar epithelial cells after injuries marks the onset of IPF and its progression. From here, the AECs enable the disease’s progression through the secretion of profibrotic factors that promote fibroblast migration, proliferation, and differentiation into myofibroblasts. Here, the myofibroblasts cause the distortion of lung architecture with the deposition of exaggerated ECM that increases the stiffening of the lung alveolar epithelium that will translate into impaired elastic properties of lungs and consequent respiratory failure [143].
The profibrotic mediators that contribute to the progression of IPF are represented by transforming growth factor beta-1 (TGF-β1), platelet-derived growth factor (PDGF), tumor necrosis factor (TNF), endothelin-1 (EDN1), connective tissue growth factor (CTGF), osteopontin (OPN), and CXC chemokine ligand 12 (CXCL12). Among them, TGF-β1 represents the master regulator of fibrotic progression since it is responsible for the myofibroblasts’ activity, and the consequent remodeling of ECM [144]. Indeed, the TGF-β that is a chemotactic factor for monocytes and macrophages, and triggers in these cell populations the release of PDGF, IL-1β, basic FGF (bFGF), and TNF-α. To this purpose, an upregulation of the TGF-β expression level has been observed both in AECs and macrophages from the lung tissues of IPF patients [23] as well as in IPF induced in vivo model named the bleomycin mouse model [24]. Indeed, to this purpose the alveolar macrophages play an important role in both IPF and lung cancer progression as highlighted in the work of Jovanovic et al. [145], who found positive membrane PD-L1 expression in alveolar macrophages of IPF lung tissue samples in 9 samples out of 12. They also found elevated concentrations of soluble PD-L1 (sPD-L1) in the serum of IPF patients, significantly higher than a healthy control group. In cancer biology, checkpoint inhibitor agents targeting PD-1/PD-L1 liberate antitumor T cells allowing their activation, proliferation, and killing of tumor cells.
Moreover, the activation of TGF-β receptor complex leads to downstream canonical (SMAD2 and 3) [146] and non-canonical signaling cascades (PI3K, MEK, mTOR, etc.), which modulate the transcription of profibrotic mediators, growth factors, microRNAs, and ECM proteins [147,148]. In particular, activated TGF-β receptors trigger the phosphorylation of SMAD2 and SMAD3, which are translocated into the nucleus for the modulation of transcriptional responses. To this purpose, Zhao et al. demonstrated that knockout mice for SMAD3 reduced bleomycin-induced pulmonary fibrosis in mice [149]. Furthermore, thare are several studies that exhibit cross-talk with TGF-β1 signaling such as the Wnt/β-catenin pathway that might promote epithelial–mesenchymal transition and myofibroblast activation [150]. Recently, it has been demonstrated that the activation of Wnt/β-catenin signaling in the alveolar epithelium of IPF patients might impair lung repair increasing AECII senescence [151]. Indeed, it has been found that Yes-associated protein (YAP) and the transcriptional coactivator with PDZ-binding motif (TAZ) that belong to the Hippo pathway are activated in lung fibrosis. To this purpose, Xu et al. through single-cell RNA sequencing found that the YAP/TAZ, TGF-β, Wnt, and the PI3K axis were activated in the AECs of IPF patients [152,153]. They suggested that mTOR/PI3K/AKT signalling contributed to IPF pathogenesis, both increasing the proliferation of lung epithelial cells and lung fibroblasts. Consequently, TGF-β1 might control the hedgehog pathway (Shh) whose activation in IPF lungs promotes IPF pathogenesis with fibroblast proliferation and aberrant extracellular matrix deposition [36]. Among the other pathways involved, TGF-β1 secretion by the AECs of IPF lungs is due to the activation of αvβ6 integrin that activates the unfolded protein response (UPR), the protective cellular mechanism deputated to the accumulation of aberrant folded proteins [154].
5. The Importance of Mechanosignalling in the Progression of Idiopathic Pulmonary Fibrosis
One of the main properties of the lung is represented by the elastic capacity that allows expansion or contraction with inspiratory/expiratory breathing. This particular mechanical capacity is transduced by several mechanosensing proteins to chemical signals into the cells. It is well known that AECII can sense and traduce the breathing mechanism in the alveolar lung epithelium into surfactant secretion. Moreover, stretching might induce the differentiation of AECII to AECI and AECII apoptosis [155,156]. In a fibrotic lung this elastic property is altered due to an increased rigidity in some areas, causing a mechanical disadvantage. We know that the ability of the cell to perceive the extracellular matrix rigidity is due the expression of some proteins called mechanosensors. For example, changes in plasma membrane tension are efficiently detected by mechanosensitive ion-channels [157,158] while mechanical stress between cells is transduced by cadherin-based adhesion complexes [159]. Furthermore, pathological conditions can arise when mechanical parameters in tissues are permanently altered (e.g., tissue stiffening during fibrosis). In addition, the increased ECM stiffness correlates with tumour progression and metastasis [160,161]. Additionally, cell differentiation and migration are induced for substrate stiffness in a phenomenon called durotaxis that is critical for several biological processes like wound healing or cell invasion [162,163]. However, ECM components and rigidity are sensed by cells using a simple receptors and complex transduction machinery. The anchors of this complex machine are the integrins that can connect and transform out-side to inside signalling through the focal adhesion formation and ROCK/myosin activation that can transform the chemical energy (ATP) into mechanical force [164,165]. Integrins connect cells to a wide range of ECM proteins including fibronectin, vitronectin, collagens, and laminins [164]. Mammals express 18 α and 8 β integrin subunits, with which they form 24 distinct α/β heterodimeric integrins that bind specific ECM ligand and signal by assembling hundreds of proteins into a large signalling hub termed adhesome [165,166]. Most cell types express several different integrins, which can synergize to amplify downstream signalling [166,167]. The focal adhesion complex connects integrin signalling to the actin cytoskeleton and gene transcription [168]. This complex transmission system has been found altered in lung fibrosis diseases, while the mechano-interaction between myofibroblast and fibrotic extracellular matrix (stiff matrix) induces a positive feedback loop amplifying lung fibrosis [169]. Even in IPF, fibroblasts display a pathological pattern of several integrins in response to epithelial injury—the expression of α2β1, α3β1, α5β1, α6β4, αvβ5, and αvβ6 are upregulated in epithelial cells [170]. Chen et al. [171] explain that human myofibroblasts expressed high levels of integrin α6 in response to matrix stiffness. Moreover, a stiff matrix induced α6 integrin expression and invasion in lung myofibroblast. The latter was due to RhoA/ROCK and c-Fos/c-Jun transcription complex activation that led to upregulated α6 expression and MMP-2 proteolytical activity associated with an enhanced lung myofibroblast invasion. In addition, mice with conditional α6-gene deletion were shown to be resistant to bleomycin lung fibrosis induction [171,172]. Furthermore, fibroblast cell adhesion to collagen type I is mediated mainly for α2β1 integrin. Xia H. et al. observed that β1 integrin signalling in response to polymerized collagen led to cell proliferation and Akt activation due to low PTEN activity in IPF fibroblasts [173]. Another fibronectin binding integrin, αvβ6, was found elevated in IPF, in response to a profibrotic process that involves TGF-β activation [174,175]. Several studies indicate that inflammation or trauma may increase contractility and induce TGF-β activation, generating an autocrine loop. Whereas TGF-β1 induced αvβ6 integrin via SMAD3, myofibroblast can use αvβ8 integrin to activate TGF-β, generating ECM accumulation and fibrosis [167]. Particularly, knockout mice for αvβ6 and αvβ8 integrins display similar abnormalities to TGF-β1 and TGF-β3 null mice [176]. Furthermore, αvβ6 mice deletion as well as the pharmacological TGF-β inhibition protect from pulmonary oedema formation after bleomycin or endotoxin treatment [177]. Interestingly, it has been recently shown that in a murine bleomycin model, the inhalation of small molecule GSK3008348, an RGD-mimetic, reduced collagen deposition and serum C3M, a marker for disease progression. In particular, it has been shown that GSK3008348 binds to integrin αvβ6, inhibiting the TGF-β downstream profibrotic pathway [178]. As we described before, integrins are involved in the actin cytoskeleton dynamics though GTPases activation. Actin microfilaments exist in a dynamic equilibrium between monomeric G- and polymerized F-actin controlled by the small RhoA-GTPases. Actin cytoskeletal remodelling plays a fundamental role in myocardin-related transcription factor-A (MRTF-A/MLK1/MAL) activation [179]. Hermann et al. demonstrated that fibronectin binding integrins differentially regulate the G- and F-actin ratio though small RhoA activation and induce MRTF-SRF target genes expression [180]. To this purpose, it has been shown that lung fibroblasts in response to matrix stiffening activate nuclear factors that promote myofibroblast differentiation such as F-actin and α-SMA, both over-expressed in a stiff collagen matrix compared with soft and 2 kPa gels. Furthermore, a stiff matrix induces RhoA/ROCK/MLC activation in lung fibroblasts, inducing actin stress fibre formation and lung myofibroblast differentiation [181]. Indeed, ROCK1 and ROCK2 have been the target of studies in pulmonary fibrosis. ROCKs are serine/kinases proteins, and they are the first RhoA mechanical response effectors though myosin light chain (MLC) phosphorylation. The human protein atlas shows elevated ROCK1 protein expression in lung, bronchus, colon, kidney, placenta, spleen, lymph node, tonsil, bone marrow, gallbladder, urinary bladder, and fallopian tube, among others. Instead, ROCK2 is highly expressed in testes and has a medium expression in lungs and other organs [182]. In addition, Knipe and colleagues generated haploinsufficient mice for selective inhibition of ROCK1, ROCK2, or both isoforms. ROCK knockout mice died during embryogenesis, but haploinsufficient mice were viable into adulthood. After bleomycin treatment to induce lung injury, both single- and double-isoform haploinsufficient mice developed a significant reduction in pulmonary fibrosis. Indeed, they observed that ROCK1 significantly protected AEC cells from apoptosis. This study demonstrates that ROCK1 and ROCK2 could protect mice from bleomycin pulmonary fibrosis induction. The specific role of each ROCK isoform involved in lung fibrosis developments is poorly understood. Pharmacological treatment with fasudil in bleomycin-induced pulmonary fibrosis reduced the production of TGF-β1, α-SMA, CTGF, and plasminogen activator inhibitor-1 (PAI-1) [182]. Indeed, a stiff matrix induced the activation of focal adhesion proteins, like FAK, PI3K, RhoA-GTPases, Ras, and YAP, involved in tumour development and metastasis [183,184,185]. Finally, mechanical forces play an important role in fibrosis and cancer progression. Nevertheless, lung cell differentiation during fibrotic tissue stimuli followed by cancer cell transformation and mechanotransduction remains to be elucidated. Further works will need to explain the specific mechanosignalling between fibrotic matrix and lung cell transformation in order to find future therapeutic targets for both diseases.
6. The Key Role of Myofibroblasts in Fibrosis-Related Diseases
Myofibroblasts, first identified in granulation tissue during wound healing, are fibroblast-like cells endowed with microfilaments in their cytoplasm similar to that of smooth muscle cells [186]. These cells display contractile properties due to their microfilaments, whose main components are smooth muscle alpha actin (αSMA) and non-muscle myosin type II [187], that make them essential for the regeneration process after wounds [187]. Indeed, myofibroblasts play a pivotal role in the deposition of ECM molecules such as type I collagen, type III collagen, and fibronectin. Myofibroblasts are tightly anchored to the cytoskeleton through integrin-mediated focal adhesions and cadherin-mediated adhesion junctions. Moreover, they express several proteins and collagen cross-linking enzymes such as protein-glutamine gamma-glutamyltransferase 2 (transglutaminase 3), protein-lysine 6-oxidase (LOX), and procollagen-lysine 2-oxoglutarate 5-dioxygenase 2 (PLOD2) [188]. These enzymes reinforce the fibrillar collagen bundles enabling the post-translational modification of collagen molecules during the wound healing. The resulting crosslinks increase the strength of these collagen networks and prevent enzymatic degradation, thereby strengthening the injured tissue [186,187,188,189]. Myofibroblasts can originate in several ways, including from differentiation from fibroblasts, a key process in normal wound healing, orchestrated by growth factors such as TGF-β, WNT, fibronectin cloths, and tissue stiffness [190]. The principal growth factor for myofibroblasts formation is TGF-β, which directly induces extracellular matrix production and αSMA expression. During the fibrotic process, TGF-β modulates several downstream signalling pathways, like SMAD3, PI3K/AKT, and p38 MAPK, promoting the trans-differentiation of myofibroblasts. In particular, the overexpression of SMAD3 enhances both the production of αSMA and the extracellular matrix proteins from fibroblasts [191,192]. Furthermore, the in vivo specific deletion of SMAD3 in mice cardiac fibroblast αSMA production and myofibroblast activation has been demonstrated [193]. Next to these aforementioned stimuli, cellular mechanosensing is another crucial element in the transition of fibroblasts to myofibroblasts. The mechanosensitivity of the cells, described in the previous section, results in activation of various intracellular pathways involving FAK, PI3K/AKT, p38 MAPK, β-catenin, and the activation of transcription activators such as myocardin-like protein 1 (MKL-1), YAP1, and TAZ. Moreover, it has been demonstrated that both MKL-1 and YAP/TAZ directly regulate the myofibroblast phenotype. In particular, the knockdown of MKL-1 lowers αSMA expression in cells grown on a stiff matrix whereas overexpression of a constitutively active form of MKL-1 increases αSMA expression in cells grown on a soft matrix [194,195]. The MLK family, in particular MLK-3, activates type I collagen expression in human embryonic lung fibroblast cell line [10], and interacts with SMAD3 to bind type I collagen and αSMA promoters [196]. Nevertheless, this interplay in the cell line of lung fibroblasts between MKL-1 and SMAD3 can trigger a faster degradation of MKL-1, leading to its suppression [197]. It has been shown that β-catenin serves to counteract this effect of SMAD3 [197], indicating that MKL-1 function depends on the bundling of multiple pathways [197]. Furthermore, the YAP/TAZ pathway can influence matrix stiffness by directly inducing Serpine1 expression. Serpine1 inhibits the activation of plasmin, a protease which degrades extracellular matrix molecules such as fibrin and fibronectin and can activate collagenases, softening the extracellular matrix [195,198]. In turn, YAP/TAZ induces TGF-β and this mechanical activation of TGF-β is enhanced in stiffer matrices [199] (Figure 2). Thus, both YAP/TAZ and TGF-β activity together with matrix stiffness are involved in a sort of feed-forward loop. Finally, another process involved in the transition to myofibroblasts depends on the matrix environment, going beyond the previously described stiffness issue. During tissue repair, fibroblasts that are highly dynamic cells can acquire distinct phenotypes depending on changes in their environment [200] Modulation of the extracellular matrix critically regulates myofibroblast trans-differentiation, the key step in tissue fibrosis. To this purpose, the extradomain-A (ED-A) variant of fibronectin, non-fibrillar collagens, and hyaluronan have been implicated in myofibroblast conversion. In particular, the ED-A fibronectin splice variant is aberrantly expressed during organ fibrosis and it is essential for TGF-β1-mediated myofibroblast conversion [201]. Non-fibrillar collagens (such as collagen VI) have been reported to stimulate myofibroblast trans-differentiation, both in vitro and in vivo [201]. Moreover, the deposition of pericellular hyaluronan may also facilitate and maintain myofibroblast trans-differentiation in response to TGF-β [194], while an independent activation of CD44 signalling by hyaluronan may accentuate the TGF-β/SMAD signalling cascade [24]. Myofibroblasts are also able to modify the biological and mechanical properties of ECM through the secretion of MMPs and tissue inhibitors of metalloproteinases (TIMPs) [202]. Indeed, their contractile capacity results in the structural reorganization of ECM during wound healing and fibrotic conditions [203]. The ECM represents a reservoir of growth factors, creating a highly stimulating environment, which influences cell adhesion, migration, and proliferation [204,205]. Furthermore, the cytoskeleton can regulate trans-differentiation in myofibroblasts and modulate their response to extracellular growth factors, cytokines, and biomechanical stimuli/signals in the ECM [189] Many studies have shown the interplay between myofibroblasts and immune cells, since myofibroblasts can be activated by components of innate and adaptive immunity, and in turn they are capable of modifying immune cells’ behaviour by altering the microenvironment [206,207]. These modifications that cause aberrant ECM production could lead to non-functional fibrotic tissue in multiple organs.
The Role of CAFs in Tumor Progression
Besides the fibrotic process, the paracrine activity of myofibroblasts, which is carried out with cytokines and growth factors secretion, can affect tumour proliferation and progression, immunosuppression, angiogenesis, and vascular remodelling [208,209]. Cancer associated fibroblasts (CAFs), similarly to myofibroblasts in IPF, are key components of the tumour microenvironment, [210,211], whose recruitment and activation is mainly governed by the cytokines released by cancer cells and infiltrated immune cells. They originate from different cell populations as illustrated in Figure 2 and explained in the Introduction. CAFs which represent the predominant cellular component of the tumour stroma and strongly contribute to the biology of tumour, being essential in the mechanisms of proliferation, invasion, inflammation, angiogenesis, and metastasis that take place in the tumour microenvironment (TME). Furthermore, tumour cells and non-malignant stromal cells secrete different growth factors such as TGF-β1, EGF, vascular endothelial growth factor (VEGF), FGF, TNF-α, IL-1β, and IL-6 [212,213] that promote CAF trans-differentiation and activation, contributing to a pro-inflammatory profile and carcinogenesis. Considering this all, it is possible to note that there is a similarity between fibrosis and LC, and among the action of the different growth factors, TGF-β represents the key driver signalling for the trans-differentiation of both fibroblasts and CAFs, which are essential in tumour progression and resistance to therapies [214,215]. In recent years, many in vitro studies have shown that TGF-β induced EMT into non-tumour epithelial cells though the activation of mTOR and PI3K pathways, leading to the apoptosis resistance of cancer cells, thereby promoting the trans-differentiation of CAFs [216]. Furthermore, CAFs are characterised by high heterogeneity, probably due to the exposure to different tumour secreted factors (TSF), that make them express different molecular markers. Despite their heterogeneity, the molecular mechanisms driving the activation of CAFs and their role in carcinogenesis may be common to various cancers. To this purpose, the main molecular pathways involved besides the TGF-β are the Wnt/β-catenin, the epidermal growth factor receptor, JAK/STAT, and Hippo pathways [217]. Indeed, it has been shown that the different subgroups of CAFs can display opposite biological functions in cancer biology given the identification of some tumour-suppressive CAF populations that are characterized by activated Hedgehog signalling pathways in mouse models of colon, pancreatic, and bladder cancers. [218]. Furthermore, it has been demonstrated the depletion of CAFs in a mouse model of pancreatic ductal adenocarcinoma (PDAC) caused hypoxia, cancer cell proliferation, and cancer progression revealing the tumour-suppressing role of CAFs at this level. [219]. On the other side, Duda et al. [220] demonstrated in preclinical studies of lung cancer that the ablation of CAFs reduced the number of metastases. Indeed, the authors, after analysing human brain metastases from lung, breast, kidney, and endometrium, found high expression of activated CAFs within these metastases. These results demonstrated that the CAFs from the primary tumour might migrate in blood circulation proliferating at the metastatic site. Finally, CAFs contribute to the increased stiffness of a tumour, that leads to the impairment of the blood vessel function, resulting in hypoxia that causes the inefficient uptake of anti-cancer drugs [215,221]. In conclusion, given the pivotal role of myofibroblasts in tumorigenesis, they could represent a promising strategy both to prevent organ fibrosis and to limit tumour progression.
According to the most recent studies, the cell population that gives rise to myofibroblasts in IPF lungs are the interstitial fibroblasts localized close to the vascular endothelium, fundamental for the alveolar gas-exchange function, the lipofibroblasts that are fibroblasts unreached with lipid droplets, the lung resident mesenchymal stromal cells, and the perycites. The pro-fibrotic stimuli lead to an increase in the TGFβ expression level that crosstalks or activates many other downstream pathways (e.g., canonical SMAD3 or non-canonical pathway and growth factors, as listed in the Figure) promoting myofibroblast activation following the aberrant deposition of ECM and progression of IPF. The myofibroblasts’ counterpart in LC, the CAFs, can originate from (1) the resident fibroblasts, (2) cancer associated adipocytes (CAAs) that are present in tumour stroma that might derive from circulating progenitors in the bone marrow [36] (3) bone marrow-derived mesenchymal stromal cells (BM-MSCs) and hematopoietic stem cells [37] (HSCs), (4) epithelial cells through the epithelial mesenchymal transition (EMT) [38], (5) vascular endothelial cells through the endothelial–mesenchymal transition (EndMT). Here, cancer cells which sustain the survival of the tumour secrete different growth factors such as TGF-β1, epidermal growth factor (EGF), vascular endothelial growth factor (VEGF), fibroblast growth factor (FGF), tumour necrosis factor α (TNF-α), interleukin 1β (IL-1β), and interleukin 6 (IL-6) which allow the differentiation of these cell populations into CAFs. Similarly, to IPF, TGF-β, representing the master regulator, activates several downstream signalling pathways. Among them, it induces the epithelial–mesenchymal transition (EMT) into non-tumour epithelial cells though the activation of mTOR and PI3K pathways, leading to the apoptosis resistance of cancer cells, and thereby promoting the trans-differentiation of CAFs. Here, CAFs under the orchestration of specific signalling pathways promote tumour progression.
7. Therapeutic Agents for IPF and LC
The many studies and clinical trials related to IPF, investigating the pathogenesis of this disease, have not solved the problem of the survival rate, which is still a dilemma for clinical approaches and therapies [222,223].In this regard, we have summarized in Table 1 the approved therapeutic strategies for both IPF and LC. Concerning IPF, the two antifibrotic drugs Pirfenidone and Nintedanib can both slow down the respiratory functional decline of IPF patients and improve survival in patients according to randomized controlled trials, such as CAPACITY and ASCEND [224]. Nevertheless, IPF still has a high mortality rate. [225,226,227,228]. Pirfenidone has the capacity to inhibit TGF-β, collagen synthesis, and fibroblast proliferation mediating tissue repair [229,230,231,232]. It has been recently shown by Miura et al. [233] that the use of Pirfenidone in IPF patients decreased the incidence of lung cancer compared with IPF patients not treated with the same drug. Furthermore, the scientific community recently demonstrated that Pirfenidone may have an anti-fibrotic role through the Shh pathway [234], which may explain the lower incidence of lung cancer in IPF-treated patients. The introduction of oncological treatments for the control of IPF is not far from becoming reality. In fact, with regard to the connections between lung cancer and IPF, Mediavilla-Varela et al. showed that Pirfenidone synergizes with cisplatin in killing tumor cells and CAFs in a lung cancer preclinical model [235]. Furthermore, inhibitors of vascular receptors, such as VEGF, FGF, and PDGF receptors, namely Nintedanib, have been already approved as specific to IPF [236,237,238]. Moreover, TKIs associated with docetaxel are considered a second-line treatment in NSCLC patients with advanced disease when the patient has been previously treated with standard chemotherapy [239]. In particular, with regard to the common tyrosine-kinase inhibitors (TKIs), such as gefitinib, erlotinib, or afatinib, their role in cancer has been already shown, especially in NSCLC patients, which show mutations activating the epidermal growth factor receptor (EGFR) [138,240,241]. To this purpose, there are ongoing preliminary studies that have identified gefitinib, erlotinib, and afatinib as potential target for IPF treatment. [242]. Indeed, although Imatinib is currently in use for the treatment of NSCLC and was studied as a potential therapy for IPF, there is a strong recommendation against its use in the 2015 IPF Guidelines from ATS/ERS [236]. Indeed, nivolumab, used for lung cancer treatments, which acts on the programmed death ligand 1 (PD-1), has been used in IPF-LC patients. In this regards, Duchemann et al. reported three cases of patients with mild to moderate IPF and lung cancer treated by nivolumab. None of them developed lung toxicity or worsening of IPF on CT during follow-up, and the death was always related to lung cancer progression. They stated that for these three patients with IPF, nivolumab was well tolerated related to their pulmonary condition [237].
Table 1.
Current approved therapeutic strategies for IPF and LC treatment.
| Therapy | Approved for IPF | Approved for LC |
|---|---|---|
| Nintedanib | Yes | Yes—In combination with docetaxel (second-line treatment) for ADC-NSCLC |
| Pirfenidone | Yes | No—Preclinical studies ongoing |
| Gefitinib | No—Early phase drug discovery study | Yes |
| Erlotinib | No—Early phase drug discovery study | Yes |
| Afatinib | No—Early phase drug discovery study | Yes |
| Imatinib | No—Strong recommendation against its use for IPF patients | Yes |
| Rovalpituzumab | No—Artesunate (pre-clinical studies) | Yes |
| Everolimus | No—Not effective in IPF | Yes |
| Nivolumab | Yes—Used for IPF-LC patients | Yes |
A recent class of antifibrotic agents that do not seem to be effective in IPF is the mTOR kinase inhibitors, including everolimus, although this immunosuppressor seems to have some positive effect in advanced lung cancer patients [238,239]. Recently, a new mTOR kinase inhibitor, GSK-2126458, is in a phase I clinical trial for IPF treatment, while it has been studied as a potential therapy forrefractory solid tumours or lymphoma. [243]. A recently approved treatment is rovalpituzumab, currently used in small cell lung cancer (SCLC), although a possible role even in IPF and lung cancer-IPF patients has been noted due to its capacity to interfere and inhibit, in a rat bleomycin model, with the Notch signaling pathway, and hence the improvement of lung fibrosis [244,245,246,247,248,249,250]. Several ongoing clinical trials and preclinical studies (257–29) (Table 2) are currently investigating the role of different molecules in IPF pathogenesis to define their anti-proliferative and anti-fibrotic roles (Table 1) which might have good prospects even against lung cancer; these are the anti-IL-13 antibodies (QAX576 and Lebrikizumab), the anti-CCL2 antibodies (Carlumab and CNTO-888), the anti-TGF-β1 antibodies (Fresolimumab and GC1008), the anti-integrin αvβ6 antibodies (BG0011 and STX-100),and the integrin αvβ6 antagonist drugs (GSK3008348), etc. [251,252,253]. Another drug that is actually used and considered feasible in IPF and lung cancer-IPF patients is vantictumab, which influences Wnt signaling and is in Phase I clinical trials for the role of inhibitor of lung fibrosis [254,255] Indeed, a preclinical study demonstrated the anti-fibrotic effects of CG-745, a histone deacetylase (HDAC) inhibitor, in bleomycin mouse models. They demonstrated that CG-745 prevented collagen synthesis, inflammatory cell accumulation, and cytokine release. The anti-fibrotic effects of CG-745 may suggest a potential therapeutic effect of CG-745 on lung fibrosis [256]. Pre-clinical studies demonstrated that increased expression of HDAC-1 was associated with lung cancer progression. Consequently, treatment with HDAC inhibitors (HDACi) has shown anti-proliferative activity in non-small cell lung cancer (NSCLC) cell lines. Although these are promising results in pre-clinical studies, HDACi has shown only modest efficacy in lung cancer clinical trials [257].
Table 2.
Current phase II–III trials in idiopathic pulmonary fibrosis (IPF).
| Mechanism of Action | Clinical Trial Identifier | Phase of Development | Treatment Duration | |
|---|---|---|---|---|
| PRM-151 | Recombinant form of human SAP | NCT02550873 | II | 28 weeks |
| Simtuzumab | Anti-LOX antibody | NCT01769196 | II | 148 weeks |
| BG00011 | Anti-integrin antibody | NCT03573505 | II | 52 weeks |
| Tralokinumab | Anti IL-13 | NCT01629667 | II | 52 weeks |
| Pamrevlumab (FG-3019) | Anti-CTGF antibody | NCT01890265 | II | 48 weeks |
| Tipelukast | Leukotriene antagonists | NCT02503657 | II | 26 weeks |
| PBI-4050 | GPR84 antagonist/GPR40 agonist | NCT02538536 | II | 20 weeks |
| Lebrikizumab | Anti IL-13 antibody | NCT01872689 | II | 52 weeks |
| KD025 | Selective inhibitor of ROCK2 | NCT02688647 | II | 24 weeks |
| GLPG1690 | Autotaxin-LPA inhibitor | NCT02738801 | II | 12 weeks |
| CC-90001 | Kinase inhibitor targeting JNKs | NCT03142191 | II | 24 weeks |
| Rituximab | Antibody targeting CD20 | NCT01969409 | II | 36 weeks |
| Sirolimus | mTOR inhibitor | NCT01462006 | NA | 22 weeks |
| Saracatinib | Src family kinase inhibitor | NCT04598919 | IB/2 | 28 weeks |
SAP: serum amyloid P; LOX: lysyl oxidase; IL: interleukin; CTGF: connective tissue growth factor; GPR: G protein-coupled receptor; ROCK: ρ-associated coiled-coil containing protein kinase; JNK: Jun N-terminal kinase; mTOR: mammalian target of rapamycin.
Finally, through a computational analysis, saracatinib has emerged as a promising drug, acting on Src kinases. The clinical trial related to this study (STOP-IPF-Phases 1b/2a) [258] started in October 2020 involving 100 subjects, to explore the application of saracatinib on IPF. This molecular and omics approach allowed the identification of the basaloid cells, a novel and rare cell population detected in the lungs of IPF patients. These cells express some of the common airway basal cell markers (TP63, KRT17, and LAMB3 LAMC2) and SOX9 transcription factor, crucial for airway development and repair, but lack some lung keratins, such as KRT5 and KRT15 [259]. Thus, basaloid cells could represent a novel source of cells to direct the efforts for future target therapies. However, the new medical frontier in the treatment of IPF and lung cancer relies on the use of genomics, which through a disease-specific gene signature allows scientists to identify possible candidates for drug targeting. To date, most approaches to precision medicine have focused on the search for distinct genetic and/or molecular disease subgroups that might be crucial for the management of both familial and sporadic IPF. To this purpose, the analysis of genetic variants performed in the last two decades, together with a recent high-resolution atlas of the resident lung populations, allowed the identification of different genetic mutations that can specifically (e.g., MUC5B, SP-A, SP-d) identify different subsets of IPF patients through a genetic signature/profile [260,261].
8. Conclusions
With this review we have shown how IPF might represent a risk factor for developing lung cancer. Both diseases display great similarity concerning the cellular processes and molecular pathways involved in the onset and progression. To date, the therapeutic treament and management of patients for both diseases remains challenging. Although the two approved anti-fibrotic drugs Pirfenidone and Nintedanib increase the survival time of IPF patients and lower the incidence of LC, there is no effective therapeutic treatment preventing the progression of IPF and its related risk of the onset of lung cancer. Nevertheless, the growing interest in investigating the similarity between lung cancer biology and IPF pathogenesis is prompting scientists to test the role of specific target drugs to prevent LC in IPF patients.
Acknowledgments
We thank FIMARP (Federazione Italiana MAlattie Rare del Polmone), Modena Golf Country Club, and AMMI (Associazione Mogli di Medici Italiani) for their support of our research. We thank Massimo Borri for the help in the figures realisation.
Author Contributions
A.V.S., V.M. and B.A. equally contributed to the conception, design, writing, and editing of the manuscript and they should be considered first authors. G.P.C., R.T., A.M. (Alessandro Marchioni), G.B., F.G., D.A., I.C., L.M., A.M. (Antonio Moretti), L.T., G.G. and S.C. reviewed the literature, designed the review, and wrote the manuscript. M.D. and E.C. critically reviewed and edited the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This manuscript has been produced within the research program at Experimental Pneumology, University of Modena and Reggio Emilia) with Dipartimenti Eccellenti Fundings (Miur 2017).
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Raghu G., Remy-Jardin M., Myers J.L., Richeldi L., Ryerson C.J., Lederer D.J., Behr J., Cottin V., Danoff S.K., Morell F., et al. Diagnosis of idiopathic pulmonary fibrosis An Official ATS/ERS/JRS/ALAT Clinical practice guideline. Am. J. Respir. Crit. Care Med. 2018;198:e44–e68. doi: 10.1164/rccm.201807-1255ST. [DOI] [PubMed] [Google Scholar]
- 2.Chanda D., Otoupalova E., Smith S.R., Volckaert T., De Langhe S.P., Thannickal V.J. Developmental pathways in the pathogenesis of lung fibrosis. Mol. Asp. Med. 2019;65:56–69. doi: 10.1016/j.mam.2018.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Richeldi L., Collard H.R., Jones M.G. Idiopathic pulmonary fibrosis. Lancet. 2017;389:1941–1952. doi: 10.1016/S0140-6736(17)30866-8. [DOI] [PubMed] [Google Scholar]
- 4.Samarelli A.V., Tonelli R., Marchioni A., Bruzzi G., Gozzi F., Andrisani D., Castaniere I., Manicardi L., Moretti A., Tabbì L., et al. Fibrotic idiopathic interstitial lung disease: The molecular and cellular key players. Int. J. Mol. Sci. 2021;22:8952. doi: 10.3390/ijms22168952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Raghu G., Collard H.R., Egan J.J., Martinez F.J., Behr J., Brown K.K., Colby T.V., Cordier J.F., Flaherty K.R., Lasky J.A., et al. An Official ATS/ERS/JRS/ALAT Statement: Idiopathic pulmonary fibrosis: Evidence-based guidelines for diagnosis and management. Am. J. Respir. Crit. Care Med. 2011;183:788–824. doi: 10.1164/rccm.2009-040GL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guenther A., Krauss E., Tello S., Wagner J., Paul B., Kuhn S., Maurer O., Heinemann S., Costabel U., Barbero M.A.N., et al. The European IPF registry (eurIPFreg): Baseline characteristics and survival of patients with idiopathic pulmonary fibrosis. Respir. Res. 2018;19:1–10. doi: 10.1186/s12931-018-0845-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crestani B., Huggins J.T., Kaye M., Costabel U., Glaspole I., Ogura T., Song J.W., Stansen W., Quaresma M., Stowasser S., et al. Long-term safety and tolerability of Nintedanib in patients with idiopathic pulmonary fibrosis: Results from the open-label extension study, INPULSIS-ON. Lancet Respir. Med. 2019;7:60–68. doi: 10.1016/S2213-2600(18)30339-4. [DOI] [PubMed] [Google Scholar]
- 8.Cottin V., Koschel D., Günther A., Albera C., Azuma A., Sköld C.M., Tomassetti S., Hormel P., Stauffer J.L., Strombom I., et al. Long-term safety of Pirfenidone: Results of the prospective, observational PASSPORT study. ERJ Open Res. 2018;4:00084–02018. doi: 10.1183/23120541.00084-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Behr J., Prasse A., Kreuter M., Johow J., Rabe K.F., Bonella F., Bonnet R., Grohe C., Held M., Wilkens H., et al. Pirfenidone in patients with progressive fibrotic interstitial lung diseases other than idiopathic pulmonary fibrosis (RELIEF): A double-blind, randomised, placebo-controlled, phase 2b trial. Lancet Respir. Med. 2021;9:476–486. doi: 10.1016/S2213-2600(20)30554-3. [DOI] [PubMed] [Google Scholar]
- 10.Sanders J.L., Putman R.K., Dupuis J., Xu H., Murabito J.M., Araki T., Nishino M., Benjamin E.J., Levy D.L., Ramachandran V.S., et al. The Association of Aging Biomarkers, Interstitial Lung Abnormalities, and Mortality. Am. J. Respir. Crit. Care Med. 2021;203:1149–1157. doi: 10.1164/rccm.202007-2993OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cerri S., Monari M., Guerrieri A., Donatelli P., Bassi I., Garuti M., Luppi F., Betti S., Bandelli G., Carpano M., et al. Real-life comparison of Pirfenidone and Nintedanib in patients with idiopathic pulmonary fibrosis: A 24-month assessment. Respir. Med. 2019;159:105803. doi: 10.1016/j.rmed.2019.105803. [DOI] [PubMed] [Google Scholar]
- 12.Noth I., Zhang Y., Ma S.F., Flores C., Barber M., Huang Y., Broderick S.M., Wade M.S., Hysi P., Scuirba J., et al. Genetic variants associated with idiopathic pulmonary fibrosis susceptibility and mortality: A genome-wide association study. Lancet Respir Med. 2013;1:309–317. doi: 10.1016/S2213-2600(13)70045-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hobbs B.D., Putman R.K., Araki T., Nishino M., Gudmundsson G., Gudnason V., Eiriksdottir G., Zilhao Nogueira N.R., Dupuis J., Xu H., et al. Overlap of Genetic Risk between Interstitial Lung Abnormalities and Idiopathic Pulmonary Fibrosis. Am. J. Respir. Crit. Care Med. 2019;200:1402–1413. doi: 10.1164/rccm.201903-0511OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abramson M.J., Walters E.H. Mapping air pollution and idiopathic pulmonary fibrosis. Respirology. 2021;26:292–293. doi: 10.1111/resp.14004. [DOI] [PubMed] [Google Scholar]
- 15.Tang X., Du R.H., Wang R., Cao T.Z., Guan L.L., Yang C.Q., Zhu Q., Hu M., Li X.Y., Li Y., et al. Comparison of Hospitalized Patients With ARDS Caused by COVID-19 and H1N1. Chest. 2020;158:195–205. doi: 10.1016/j.chest.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gattinoni L., Chiumello D., Caironi P., Busana M., Romitti F., Brazzi L., Camporota L. COVID-19 pneumonia: Different respiratory treatments for different phenotypes? Intensive Care Med. 2020;46:1099–1102. doi: 10.1007/s00134-020-06033-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu C., Chen X., Cai Y., Xia J., Zhou X., Xu S., Huang H., Zhang L., Zhou X., Du C., et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Int. Med. 2020;180:934–943. doi: 10.1001/jamainternmed.2020.0994. Erratum in: JAMA Int. Med. 2020, 180, 1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang P., Li J., Liu H., Han N., Ju J., Kou Y., Chen L., Jiang M., Pan F., Zheng Y., et al. Correction: Long-term bone and lung consequences associated with hospital-acquired severe acute respiratory syndrome: A 15-year follow-up from a prospective cohort study. Bone Res. 2020;8:34. doi: 10.1038/s41413-020-00113-1. Erratum for: Bone Res. 2020, 8, 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Das K.M., Lee E.Y., Singh R., Enani M.A., Al Dossari K., Van Gorkom K., Larsson S.G., Langer R.D. Follow-up chest radiographic findings in patients with MERS-CoV after recovery. Indian J. Radiol. Imaging. 2017;27:342–349. doi: 10.4103/ijri.IJRI_469_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Karampitsakos T., Tzilas V., Tringidou R., Steiropoulos P., Aidinis V., Papiris S.A., Bouros D., Tzouvelekis A. Lung cancer in patients with idiopathic pulmonary fibrosis. Pulm. Pharmacol. Ther. 2017;45:1–10. doi: 10.1016/j.pupt.2017.03.016. [DOI] [PubMed] [Google Scholar]
- 21.Kato E., Takayanagi N., Takaku Y., Kagiyama N., Kanauchi T., Ishiguro T., Sugita Y. Incidence and predictive factors of lung cancer in patients with idiopathic pulmonary fibrosis. ERJ Open Res. 2018;4:00111–02016. doi: 10.1183/23120541.00111-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tang H., Ren Y., She Y., Dai C., Wang T., Su H., Sun W., Jiang G., Chen C. Is operation safe for lung cancer patients with interstitial lung disease on computed tomography? Ther. Adv. Respir. Dis. 2020;14:1753466620971137. doi: 10.1177/1753466620971137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Luo Y.H., Wang C., Xu W.T., Zhang Y., Zhang T., Xue H., Li Y.N., Fu Z.R., Wang Y., Jin C.H. 18β-Glycyrrhetinic Acid Has Anti-Cancer Effects via Inducing Apoptosis and G2/M Cell Cycle Arrest, and Inhibiting Migration of A549 Lung Cancer Cells. OncoTargets Ther. 2021;14:5131–5144. doi: 10.2147/OTT.S322852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pallante P., Malapelle U., Nacchio M., Sgariglia R., Galati D., Capitelli L., Zanotta S., Galgani M., Piemonte E., Sanduzzi Zamparelli A., et al. Liquid Biopsy Is a Promising Tool for Genetic Testing in Idiopathic Pulmonary Fibrosis. Diagnostics. 2021;11:1202. doi: 10.3390/diagnostics11071202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sivakumar P., Ammar R., Thompson J.R., Luo Y., Streltsov D., Porteous M., McCoubrey C., Cantu E., 3rd, Beers M.F., Jarai G., et al. Integrated plasma proteomics and lung transcriptomics reveal novel biomarkers in idiopathic pulmonary fibrosis. Respir. Res. 2021;22:273. doi: 10.1186/s12931-021-01860-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gomes R.N., Manuel F., Nascimento D.S. The bright side of fibroblasts: Molecular signature and regenerative cues in major organs. NPJ Regen. Med. 2021;6:43. doi: 10.1038/s41536-021-00153-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tan W., Wang Y., Chen Y., Chen C. Cell tracing reveals the transdifferentiation fate of mouse lung epithelial cells during pulmonary fibrosis in vivo. Exp. Ther. Med. 2021;22:1188. doi: 10.3892/etm.2021.10622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu X., Rowan S.C., Liang J., Yao C., Huang G., Deng N., Xie T., Wu D., Wang Y., Burman A., et al. Categorization of lung mesenchymal cells in development and fibrosis. iScience. 2021;24:102551. doi: 10.1016/j.isci.2021.102551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wiśniewska J., Sadowska A., Wójtowicz A., Słyszewska M., Szóstek-Mioduchowska A. Perspective on Stem Cell Therapy in Organ Fibrosis: Animal Models and Human Studies. Life. 2021;11:1068. doi: 10.3390/life11101068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Upagupta C., Shimbori C., Alsilmi R., Kolb M. Matrix abnormalities in pulmonary fibrosis. Eur. Respir. Rev. 2018;27:180033. doi: 10.1183/16000617.0033-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Phan S.H. Genesis of the myofibroblast in lung injury and fibrosis. Proc. Am. Thorac. Soc. 2012;9:148–152. doi: 10.1513/pats.201201-011AW. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kleaveland K.R., Velikoff M., Yang J., Agarwal M., Rippe R.A., Moore B.B., Kim K.K. Fibrocytes Are Not an Essential Source of Type I Collagen during Lung Fibrosis. J. Immunol. 2014;193:5229–5239. doi: 10.4049/jimmunol.1400753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhou L., Yang K., Andl T., Wickett R.R., Zhang Y. Perspective of Targeting Cancer-Associated Fibroblasts in Melanoma. J. Cancer. 2015;6:717–726. doi: 10.7150/jca.10865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jena B.C., Das C.K., Bharadwaj D., Mandal M. Cancer associated fibroblast mediated chemoresistance: A paradigm shift in understanding the mechanism of tumor progression. Biochim. Biophys. Acta Rev. Cancer. 2020;1874:188416. doi: 10.1016/j.bbcan.2020.188416. [DOI] [PubMed] [Google Scholar]
- 35.Joshi R.S., Kanugula S.S., Sudhir S., Pereira M.P., Jain S., Aghi M.K. The Role of Cancer-Associated Fibroblasts in Tumor Progression. Cancers. 2021;13:1399. doi: 10.3390/cancers13061399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bochet L., Lehuédé C., Dauvillier S., Wang Y.Y., Dirat B., Laurent V., Dray C., Guiet R., Maridonneau-Parini I., Le Gonidec S., et al. Adipocyte-derived fibroblasts promote tumor progression and contribute to the desmoplastic reaction in breast cancer. Cancer Res. 2013;73:5657–5668. doi: 10.1158/0008-5472.CAN-13-0530. [DOI] [PubMed] [Google Scholar]
- 37.Raz Y., Cohen N., Shani O., Bell R.E., Novitskiy S.V., Abramovitz L., Levy C., Milyavsky M., Leider-Trejo L., Moses H.L., et al. Bone marrow-derived fibroblasts are a functionally distinct stromal cell population in breast cancer. J. Exp. Med. 2018;215:3075–3093. doi: 10.1084/jem.20180818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Petersen O.W., Nielsen H.L., Gudjonsson T., Villadsen R., Rønnov-Jessen L., Bissell M.J. The plasticity of human breast carcinoma cells is more than epithelial to mesenchymal conversion. Breast Cancer Res. 2001;3:213–217. doi: 10.1186/bcr298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zeisberg E.M., Potenta S., Xie L., Zeisberg M., Kalluri R. Discovery of endothelial to mesenchymal transition as a source for carcinoma-associated fibroblasts. Cancer Res. 2007;67:10123–10128. doi: 10.1158/0008-5472.CAN-07-3127. [DOI] [PubMed] [Google Scholar]
- 40.Raskov H. Early mechanisms of tumor dissemination and the relation to surgery. Int. J. Cancer. 2020;3255:3244–3255. doi: 10.1002/ijc.32820. [DOI] [PubMed] [Google Scholar]
- 41.Raskov H., Orhan A., Gaggar S., Gögenur I., Roz L. Cancer-Associated Fibroblasts and Tumor-Associated Macrophages in Cancer and Cancer Immunotherapy. Front. Oncol. 2021;11:1–17. doi: 10.3389/fonc.2021.668731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chilosi M., Poletti V., Zamò A., Lestani M., Montagna L., Piccoli P., Pedron S., Bertaso M., Scarpa A., Murer B., et al. Aberrant Wnt/β-catenin pathway activation in idiopathic pulmonary fibrosis. Am. J. Pathol. 2003;162:1495–1502. doi: 10.1016/S0002-9440(10)64282-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Conte E., Gili E., Fruciano M., Korfei M., Fagone E., Iemmolo M., Lo Furno D., Giuffrida R., Crimi N., Guenther A., et al. PI3K p110γ overexpression in idiopathic pulmonary fibrosis lung tissue and fibroblast cells: In vitro effects of its inhibition. Lab. Investig. 2013;93:566–576. doi: 10.1038/labinvest.2013.6. [DOI] [PubMed] [Google Scholar]
- 44.Giroux-leprieur E., Costantini A., Ding V.W., He B. Hedgehog Signaling in Lung Cancer: From Oncogenesis to Cancer Treatment Resistance. Int. J. Mol. Sci. 2018;19:2835. doi: 10.3390/ijms19092835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wiley C.D., Brumwell A.N., Davis S.S., Jackson J.R., Valdovinos A., Calhoun C., Alimirah F., Castellanos C.A., Ruan R., Wei Y., et al. Secretion of leukotrienes by senescent lung fibroblasts promotes pulmonary fibrosis. JCI Insight. 2019;4:e130056. doi: 10.1172/jci.insight.130056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Li X., Xie M., Lu C., Mao J., Cao Y., Yang Y., Wei Y., Liu X., Cao S., Song Y., et al. Design and synthesis of Leukotriene A4 hydrolase inhibitors to alleviate idiopathic pulmonary fibrosis and acute lung injury. Eur. J. Med. Chem. 2020;203:112614. doi: 10.1016/j.ejmech.2020.112614. [DOI] [PubMed] [Google Scholar]
- 47.Poczobutt J.M., Gijon M., Amin J., Hanson D., Li H., Walker D., Weiser-Evans M., Lu X., Murphy R.C., Nemenoff R.A. Eicosanoid profiling in an orthotopic model of lung cancer progression by mass spectrometry demonstrates selective production of leukotrienes by inflammatory cells of the microenvironment. PLoS ONE. 2013;8:e79633. doi: 10.1371/journal.pone.0079633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Maher T.M., Bendstrup E., Dron L., Langley J., Smith G., Khalid J.M., Patel H., Kreuter M. Global incidence and prevalence of idiopathic pulmonary fibrosis. Respir. Res. 2021;22:197. doi: 10.1186/s12931-021-01791-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Spek C.A., Duitman J. Is idiopathic pulmonary fibrosis a cancer-like disease? Transcriptome analysis to fuel the debate. ERJ Open Res. 2019;5:00157–02018. doi: 10.1183/23120541.00157-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.JafariNezhad A., YektaKooshali M.H. Lung cancer in idiopathic pulmonary fibrosis: A systematic review and meta-analysis. PLoS ONE. 2018;13:e0202360. doi: 10.1371/journal.pone.0202360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ozawa Y., Suda T., Naito T., Enomoto N., Hashimoto D., Fujisawa T., Nakamura Y., Inui N., Nakamura H., Chida K. Cumulative incidence of and predictive factors for lung cancer in IPF. Respirology. 2009;14:723–728. doi: 10.1111/j.1440-1843.2009.01547.x. [DOI] [PubMed] [Google Scholar]
- 52.Tomassetti S., Gurioli C., Ryu J.H., Decker P.A., Ravaglia C., Tantalocco P., Buccioli M., Piciucchi S., Sverzellati N., Dubini A., et al. The impact of lung cancer on survival of idiopathic pulmonary fibrosis. Chest. 2015;147:157–164. doi: 10.1378/chest.14-0359. [DOI] [PubMed] [Google Scholar]
- 53.Alomaish H., Ung Y., Wang S., Tyrrell P.N., Zahra S.A., Oikonomou A. Survival analysis in lung cancer patients with interstitial lung disease. PLoS ONE. 2021;16:e0255375. doi: 10.1371/journal.pone.0255375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.d’Alessandro M., Bergantini L., Torricelli E., Cameli P., Lavorini F., Pieroni M., Refini R.M., Sestini P., Bargagli E. Systematic Review and Metanalysis of Oncomarkers in IPF Patients and Serial Changes of Oncomarkers in a Prospective Italian Real-Life Case Series. Cancers. 2021;13:539. doi: 10.3390/cancers13030539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Goto T. Measuring Surgery Outcomes of Lung Cancer Patients with Concomitant Pulmonary Fibrosis: A Review of the Literature. Cancers. 2018;10:223. doi: 10.3390/cancers10070223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kawai T., Yakumaru K., Suzuki M., Kageyama K. Diffuse interstitial pulmonary fibrosis and lung cancer. Acta Pathol. Jpn. 1987;37:11–19. doi: 10.1111/j.1440-1827.1987.tb03130.x. [DOI] [PubMed] [Google Scholar]
- 57.Hironaka M., Fukayama M. Pulmonary fibrosis and lung carcinoma: A comparative study of metaplastic epithelia in honeycombed areas of usual interstitial pneumonia with or without lung carcinoma. Pathol Int. 1999;49:1060–1066. doi: 10.1046/j.1440-1827.1999.00989.x. [DOI] [PubMed] [Google Scholar]
- 58.Shiratori T., Tanaka H., Tabe C., Tsuchiya J., Ishioka Y., Itoga M., Taima K., Takanashi S., Tasaka S. Effect of nintedanib on non-small cell lung cancer in a patient with idiopathic pulmonary fibrosis: A case report and literature review. Thorac. Cancer. 2020;11:1720–1723. doi: 10.1111/1759-7714.13437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Vancheri C. Common pathways in idiopathic pulmonary fibrosis and cancer. Eur. Respir. Rev. 2013;22:265–272. doi: 10.1183/09059180.00003613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Millan-Billi P., Serra C., Alonso Leon A., Castillo D. Comorbidities, Complications and Non-Pharmacologic Treatment in Idiopathic Pulmonary Fibrosis. Med. Sci. 2018;6:59. doi: 10.3390/medsci6030059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Antoniou K.M., Tomassetti S., Tsitoura E., Vancheri C. Idiopathic pulmonary fibrosis and lung cancer: A clinical and pathogenesis update. Curr. Opin. Pulm. Med. 2015;21:626–633. doi: 10.1097/MCP.0000000000000217. [DOI] [PubMed] [Google Scholar]
- 62.Yokoyama A., Kondo K., Nakajima M., Matsushima T., Takahashi T., Nishimura M., Kohno N. Prognostic value of circulating KL-6 in idiopathic pulmonary fibrosis. Respirology. 2006;11:164–168. doi: 10.1111/j.1440-1843.2006.00834.x. [DOI] [PubMed] [Google Scholar]
- 63.Leuschner G., Klotsche J., Kreuter M., Prasse A., Wirtz H., Pittrow D., Frankenberger M., Behr J., Kneidinger N., INSIGHTS-IPF Registry Group Idiopathic Pulmonary Fibrosis in Elderly Patients: Analysis of the INSIGHTS-IPF Observational Study. Front. Med. 2020;7:601279. doi: 10.3389/fmed.2020.601279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cordier J.F., Cottin V. Neglected evidence in idiopathic pulmonary fibrosis: From history to earlier diagnosis. Eur. Respir. J. 2013;42:916–923. doi: 10.1183/09031936.00027913. [DOI] [PubMed] [Google Scholar]
- 65.Spagnolo P., Ryerson C.J., Putman R., Oldham J., Salisbury M., Sverzellati N., Valenzuela C., Guler S., Jones S., Wijsenbeek M., et al. Early diagnosis of fibrotic interstitial lung disease: Challenges and opportunities. Lancet Respir. Med. 2021;9:1065–1076. doi: 10.1016/S2213-2600(21)00017-5. [DOI] [PubMed] [Google Scholar]
- 66.Park J., Kim D.S., Shim T.S., Lim C.M., Koh Y., Lee S.D., Kim W.S., Kim W.D., Lee J.S., Song K.S. Lung cancer in patients with idiopathic pulmonary fibrosis. Eur. Respir. J. 2001;17:1216–1219. doi: 10.1183/09031936.01.99055301. [DOI] [PubMed] [Google Scholar]
- 67.Wood D.E., Kazerooni E., Baum S.L., Dransfield M.T., Eapen G.A., Ettinger D.S., Hou L., Jackman D.M., Klippenstein D., Kumar R., et al. Lung cancer screening, version 1.2015: Featured updates to the NCCN guidelines. J. Natl. Compr. Canc. Netw. 2015;13:23–34. doi: 10.6004/jnccn.2015.0006. [DOI] [PubMed] [Google Scholar]
- 68.Humphrey L.L., Deffebach M., Pappas M., Baumann C., Artis K., Mitchell J.P., Zakher B., Fu R., Slatore C.G. Screening for lung cancer with low-dose computed tomography: A systematic review to update the US preventive services task force recommendation. Ann. Intern. Med. 2013;159:411–420. doi: 10.7326/0003-4819-159-6-201309170-00690. [DOI] [PubMed] [Google Scholar]
- 69.Ley S., Ley-Zaporozhan J. Novelties in imaging in pulmonary fibrosis and nodules. A narrative review. Pulmonology. 2020;26:39–44. doi: 10.1016/j.pulmoe.2019.09.009. [DOI] [PubMed] [Google Scholar]
- 70.Lee T., Park J.Y., Lee H.Y., Cho Y.J., Yoon H.I., Lee J.H., Jheon S., Lee C.T., Park J.S. Lung cancer in patients with idiopathic pulmonary fibrosis: Clinical characteristics and impact on survival. Respir. Med. 2014;108:1549–1555. doi: 10.1016/j.rmed.2014.07.020. [DOI] [PubMed] [Google Scholar]
- 71.Goto T., Maeshima A., Oyamada Y., Kato R. Idiopathic pulmonary fibrosis as a prognostic factor in non-small cell lung cancer. Int. J. Clin. Oncol. 2014;19:266–273. doi: 10.1007/s10147-013-0566-1. [DOI] [PubMed] [Google Scholar]
- 72.Spagnolo P., Tzouvelekis A., Bonella F. The Management of Patients With Idiopathic Pulmonary Fibrosis. Front. Med. 2018;5:148. doi: 10.3389/fmed.2018.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tzouvelekis A., Antoniou K., Kreuter M., Evison M., Blum T.G., Poletti V., Grigoriu B., Vancheri C., Spagnolo P., Karampitsakos T., et al. The DIAMORFOSIS (DIAgnosis and Management Of lung canceR and FibrOSIS) survey: International survey and call for consensus. ERJ Open Res. 2021;7:00529–02020. doi: 10.1183/23120541.00529-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Luppi F., Kalluri M., Faverio P., Kreuter M., Ferrara G. Idiopathic pulmonary fibrosis beyond the lung: Understanding disease mechanisms to improve diagnosis and management. Respir. Res. 2021;22:109. doi: 10.1186/s12931-021-01711-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Pastre J., Barnett S., Ksovreli I., Taylor J., Brown A.W., Shlobin O.A., Ahmad K., Khangoora V., Aryal S., King C.S., et al. Idiopathic pulmonary fibrosis patients with severe physiologic impairment: Characteristics and outcomes. Respir. Res. 2021;22:5. doi: 10.1186/s12931-020-01600-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Palma D.A., Chen H., Bahig H., Gaede S., Harrow S., Laba J.M., Ryerson C.J. Assessment of precision irradiation in early non-small cell lung cancer and interstitial lung disease (ASPIRE-ILD): Study protocol for a phase II trial. BMC Cancer. 2019;19:1206. doi: 10.1186/s12885-019-6392-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Duitman J., van den Ende T., Spek C.A. Immune Checkpoints as Promising Targets for the Treatment of Idiopathic Pulmonary Fibrosis? J. Clin. Med. 2019;8:1547. doi: 10.3390/jcm8101547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Stainer A., Faverio P., Busnelli S., Catalano M., Della Zoppa M., Marruchella A., Pesci A., Luppi F. Molecular Biomarkers in Idiopathic Pulmonary Fibrosis: State of the Art and Future Directions. Int. J. Mol. Sci. 2021;22:6255. doi: 10.3390/ijms22126255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ni S., Song M., Guo W., Guo T., Shen Q., Peng H. Biomarkers and their potential functions in idiopathic pulmonary fibrosis. Expert Rev. Respir. Med. 2020;14:593–602. doi: 10.1080/17476348.2020.1745066. [DOI] [PubMed] [Google Scholar]
- 80.Maher T.M. PROFILEing idiopathic pulmonary fibrosis: Rethinking biomarker discovery. Eur. Respir. Rev. 2013;22:148–152. doi: 10.1183/09059180.00000913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Organ L.A., Duggan AM R., Oballa E., Taggart S.C., Simpson J.K., Kang’ombe A.R., Maher T.M. Biomarkers of collagen synthesis predict progression in the PROFILE idiopathic pulmonary fibrosis cohort. Respir. Res. 2019;20:148. doi: 10.1186/s12931-019-1118-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Peng D.H., Luo Y., Huang L.J., Liao F.L., Liu Y.Y., Tang P., Hu H.N., Chen W. Correlation of Krebs von den Lungen-6 and fibronectin with pulmonary fibrosis in coronavirus disease 2019. Clin. Chim. Acta. 2021;517:48–53. doi: 10.1016/j.cca.2021.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Horimasu Y., Hattori N., Ishikawa N., Kawase S., Tanaka S., Yoshioka K., Costabel U. Different MUC1 gene polymorphisms in German and Japanese ethnicities affect serum KL-6 levels. Respir. Med. 2012;106:1756–1764. doi: 10.1016/j.rmed.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 84.Korthagen N.M., van Moorsel C.H., Zanen P., Ruven H.J., Grutters J.C. Evaluation of circulating YKL-40 levels in idiopathic interstitial pneumonias. Lung. 2014;192:975–980. doi: 10.1007/s00408-014-9647-9. [DOI] [PubMed] [Google Scholar]
- 85.Korthagen N.M., van Moorsel C.H., Barlo N.P., Ruven H.J., Kruit A., Heron M., Bosch J.M.V.D., Grutters J.C. Serum and BALF YKL-40 levels are predictors of survival in idiopathic pulmonary fibrosis. Respir. Med. 2011;105:106–113. doi: 10.1016/j.rmed.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 86.Herazo-Maya J.D., Sun J., Molyneaux P.L., Li Q., Villalba J.A., Tzouvelekis A., Lynn H., Juan-Guardela B.M., Risquez C., Osorio J.C., et al. Validation of a 52-gene risk profile for outcome prediction in patients with idiopathic pulmonary fibrosis: An international, multicentre, cohort study. Lancet Respir. Med. 2017;5:857–868. doi: 10.1016/S2213-2600(17)30349-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Huang Y., Ma S.-F., Espindola M.S., Vij R., Oldham J.M., Huffnagle G.B., Erb-Downward J.R., Flaherty K.R., Moore B., White E.S., et al. Microbes are associated with host innate immune response in idiopathic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 2017;196:208–219. doi: 10.1164/rccm.201607-1525OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Molyneaux P.L., Willis-Owen S.A., Cox M.J., James P., Cowman S., Loebinger M., Blanchard A., Edwards L.M., Stock C., Daccord C., et al. Host–microbial interactions in idiopathic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 2017;195:1640–1650. doi: 10.1164/rccm.201607-1408OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Saini G., Jenkins G., McKeever T., Simpson J., Hubbard R., Johnson S., Braybrooke R., Russell A.-M., Meakin G., Sweeney L., et al. The PROFILE study: A prospective study of fibrosis in lung endpoints to discover and qualify biomarkers for use in clinical trials. Am. J. Respir. Crit. Care Med. 2012;185:A5169. [Google Scholar]
- 90.Takahashi H., Fujishima T., Koba H., Murakami S., Kurokawa K., Shibuya Y., Shiratori M., Kuroki Y., Abe S. Serum surfactant proteins A and D as prognostic factors in idiopathic pulmonary fibrosis and their relationship to disease extent. Am. J. Respir. Crit. Care Med. 2000;162:1109–1114. doi: 10.1164/ajrccm.162.3.9910080. [DOI] [PubMed] [Google Scholar]
- 91.Kahn N., Rossler A.K., Hornemann K., Muley T., Grünig E., Schmidt W., Herth F.J., Kreuter M. C-proSP-B: A possible biomarker for pulmonary diseases? Respiration. 2018;96:117–126. doi: 10.1159/000488245. [DOI] [PubMed] [Google Scholar]
- 92.Rosas I.O., Richards T.J., Konishi K., Zhang Y., Gibson K., Lokshin A.E., Lindell K.O., Cisneros J., Macdonald S.D., Pardo A., et al. MMP1 and MMP7 as potential peripheral blood biomarkers in idiopathic pulmonary fibrosis. PLoS Med. 2008;5:e93. doi: 10.1371/journal.pmed.0050093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ebert W., Dienemann H., Fateh-Moghadam A., Scheulen M., Konietzko N., Schleich T., Bombardieri E. Cytokeratin 19 fragment CYFRA 21-1 compared with carcinoembryonic antigen, squamous cell carcinoma antigen and neuron-specific enolase in lung cancer. Results of an international multicentre study. Eur. J. Clin. Chem. Clin. Biochem. 1994;32:189–199. [PubMed] [Google Scholar]
- 94.Stieber P., Hasholzner U., Bodenmüller H., Nagel D., Sunder-Plassmann L., Dienemann H., Meier W., Fateh-Moghadam A. CYFRA 21-1. A new marker in lung cancer. Cancer. 1993;72:707–713. doi: 10.1002/1097-0142(19930801)72:3<707::AID-CNCR2820720313>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 95.Albera C., Verri G., Sciarrone F., Sitia E., Mangiapia M., Solidoro P. Progressive Fibrosing Interstitial Lung Diseases: A Current Perspective. Biomedicines. 2021;9:1237. doi: 10.3390/biomedicines9091237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Du Bois R.M., Weycker D., Albera C., Bradford W.Z., Costabel U., Kartashov A., King Jr T.E., Lancaster L., Noble P.W., Sahn S.A., et al. Forced vital capacity in patients with idiopathic pulmonary fibrosis: Test properties and minimal clinically important difference. Am. J. Respir. Crit. Care Med. 2011;184:1382–1389. doi: 10.1164/rccm.201105-0840OC. [DOI] [PubMed] [Google Scholar]
- 97.King T.E., Jr., Tooze J.A., Schwarz M.I., Brown K.R., Cherniack R.M. Predicting survival in idiopathic pulmonary fibrosis: Scoring system and survival model. Am. J. Respir. Crit. Care Med. 2001;164:1171–1181. doi: 10.1164/ajrccm.164.7.2003140. [DOI] [PubMed] [Google Scholar]
- 98.Lee S.H., Park J.S., Kim S.Y., Kim D.S., Kim Y.W., Chung M.P., Uh S.T., Park C.S., Park S.W., Jeong S.H., et al. Comparison of CPI and GAP models in patients with idiopathic pulmonary fibrosis: A nationwide cohort study. Sci. Rep. 2018;8:4784. doi: 10.1038/s41598-018-23073-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Torrisi S.E., Ley B., Kreuter M., Wijsenbeek M., Vittinghoff E., Collard H.R., Vancheri C. The added value of comorbidities in predicting survival in idiopathic pulmonary fibrosis: A multicentre observational study. Eur. Respir. J. 2019;53:1801587. doi: 10.1183/13993003.01587-2018. [DOI] [PubMed] [Google Scholar]
- 100.Prasse A., Probst C., Bargagli E., Zissel G., Toews G.B., Flaherty K.R., Olschewski M., Rottoli P., Müller-Quernheim J. Serum CC-chemokine ligand 18 concentration predicts outcome in idiopathic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 2009;179:717–723. doi: 10.1164/rccm.200808-1201OC. [DOI] [PubMed] [Google Scholar]
- 101.Richards T.J., Kaminski N., Baribaud F., Flavin S., Brodmerkel C., Horowitz D., Li K., Choi J., Vuga L.J., Lindell K.O., et al. Peripheral blood proteins predict mortality in idiopathic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 2012;185:67–76. doi: 10.1164/rccm.201101-0058OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Greene K.E., Ye S., Mason R.J. Serum surfactant protein-A levels predict development of ARDS in at-risk patients. Chest. 1999;116:90S–91S. doi: 10.1378/chest.116.suppl_1.90S. [DOI] [PubMed] [Google Scholar]
- 103.Kinder B.W., Brown K.K., McCormack F.X., Ix J.H., Kervitsky A., Schwarz M.I., King T.E., Jr. Serum surfactant protein-A is a strong predictor of early mortality in idiopathic pulmonary fibrosis. Chest. 2009;135:1557–1563. doi: 10.1378/chest.08-2209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Nagata N., Kitasato Y., Wakamatsu K., Kawabata M., Fukushima K., Kajiki A., Kitahara Y., Watanabe K. Prognostic value of immunohistochemical surfactant protein A expression in regenerative/hyperplastic alveolar epithelial cells in idiopathic interstitial pneumonias. Diagn. Pathol. 2011;6:25. doi: 10.1186/1746-1596-6-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Song J.W., Song J.K., Kim D.S. Echocardiography and brain natriuretic peptide as prognostic indicators in idiopathic pulmonary fibrosis. Respir. Med. 2009;103:180–186. doi: 10.1016/j.rmed.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 106.Ando M., Miyazaki E., Ito T., Hiroshige S., Nureki S.-I., Ueno T., Takenaka R., Fukami T., Kumamoto T. Significance of serum vascular endothelial growth factor level in patients with idiopathic pulmonary fibrosis. Lung. 2010;188:247–252. doi: 10.1007/s00408-009-9223-x. [DOI] [PubMed] [Google Scholar]
- 107.Gilani S.R., Vuga L.J., Lindell K.O., Gibson K.F., Xue J., Kaminski N., Valentine V.G., Lindsay E.K., George M.P., Steele C., et al. CD28 down-regulation on circulating CD4 T-cells is associated with poor prognoses of patients with idiopathic pulmonary fibrosis. PLoS ONE. 2010;5:e8959. doi: 10.1371/journal.pone.0008959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kahloon R.A., Xue J., Bhargava A., Csizmadia E., Otterbein L., Kass D.J., Bon J., Soejima M., Levesque M.C., Lindell K.O., et al. Patients with idiopathic pulmonary fibrosis with antibodies to heat shock protein 70 have poor prognoses. Am. J. Respir. Crit. Care Med. 2013;187:768–775. doi: 10.1164/rccm.201203-0506OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Okamoto M., Hoshino T., Kitasato Y., Sakazaki Y., Kawayama T., Fujimoto K., Ohshima K., Shiraishi H., Uchida M., Ono J., et al. Periostin, a matrix protein, is a novel biomarker for idiopathic interstitial pneumonias. Eur. Respir. J. 2011;37:1119–1127. doi: 10.1183/09031936.00059810. [DOI] [PubMed] [Google Scholar]
- 110.Tajiri M., Okamoto M., Fujimoto K., Johkoh T., Ono J., Tominaga M., Azuma K., Kawayama T., Ohta S., Izuhara K., et al. Serum level of periostin can predict long-term outcome of idiopathic pulmonary fibrosis. Respir. Investig. 2015;53:73–81. doi: 10.1016/j.resinv.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 111.Kadota J., Mizunoe S., Mito K., Mukae H., Yoshioka S., Kawakami K., Koguchi Y., Fukushima K., Kon S., Kohno S., et al. High plasma concentrations of osteopontin in patients with interstitial pneumonia. Respir. Med. 2005;99:111–117. doi: 10.1016/j.rmed.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 112.Xue J., Kass D.J., Bon J., Vuga L., Tan J., Csizmadia E., Otterbein L., Soejima M., Levesque M.C., Gibson K.F., et al. Plasma B lymphocyte stimulator and B cell differentiation in idiopathic pulmonary fibrosis patients. J. Immunol. 2013;191:2089–2095. doi: 10.4049/jimmunol.1203476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Moeller A., Gilpin S.E., Ask K., Cox G., Cook D., Gauldie J., Margetts P.J., Farkas L., Dobranowski J., Boylan C., et al. Circulating fibrocytes are an indicator of poor prognosis in idiopathic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 2009;179:588–594. doi: 10.1164/rccm.200810-1534OC. [DOI] [PubMed] [Google Scholar]
- 114.Vuga L.J., Tedrow J.R., Pandit K.V., Tan J., Kass D.J., Xue J., Chandra D., Leader J.K., Gibson K.F., Kaminski N. C-X-C motif chemokine 13 (CXCL13) is a prognostic biomarker of idiopathic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 2014;189:966–974. doi: 10.1164/rccm.201309-1592OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Armstrong H.F., Podolanczuk A.J., Barr R.G., Oelsner E.C., Kawut S.M., Hoffman E.A., Tracy R., Kaminski N., McClelland R.L., Lederer D.J. Serum matrix metalloproteinase-7, respiratory symptoms, and mortality in community-dwelling adults. MESA (Multi-Ethnic Study of Atherosclerosis) Am. J. Respir. Crit. Care Med. 2017;196:1311–1317. doi: 10.1164/rccm.201701-0254OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Jenkins R.G., Simpson J.K., Saini G., Bentley J.H., Russell A.M., Braybrooke R., Molyneaux P.L., McKeever T.M., Wells A.U., Flynn A., et al. Longitudinal change in collagen degradation biomarkers in idiopathic pulmonary fibrosis: An analysis from the prospective, multicentre PROFILE study. Lancet Respir. Med. 2015;3:462–472. doi: 10.1016/S2213-2600(15)00048-X. [DOI] [PubMed] [Google Scholar]
- 117.Maher T.M., Braybrooke R., Costa M.J., Duggan A.M., Fahy W.A., Hubbard R., Lukey P., Marshall R.P., Oballa E., Saini G., et al. The PROFILE (Prospective Observation of Fibrosis in the Lung Clinical Endpoints) study. Am. J. Respir. Crit. Care Med. 2017;195:A6790. [Google Scholar]
- 118.Maher Toby M., Susanne Stowasser Yasuhiko Nishioka Eric S. Investigating the effects of Nintedanib on biomarkers of extracellular matrix turnover in patients with IPF: Design of the randomised placebo-controlled INMARK® trial. BMJ Open Respir. Res. 2018;5:e000325. doi: 10.1136/bmjresp-2018-000325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Wu X., Kim G.H., Salisbury M.L., Barber D., Bartholmai B.J., Brown K.K., Conoscenti C.S., De Backer J., Flaherty K.R., Gruden J.F., et al. Computed tomographic biomarkers in idiopathic pulmonary fibrosis. The future of quantitative analysis. Am. J. Respir. Crit. Care Med. 2019;199:12–21. doi: 10.1164/rccm.201803-0444PP. [DOI] [PubMed] [Google Scholar]
- 120.Humphries S.M., Yagihashi K., Huckleberry J., Rho B.-H., Schroeder J.D., Strand M., Schwarz M.I., Flaherty K.R., Kazerooni E.A., Van Beek E.J.R., et al. Idiopathic pulmonary fibrosis: Data-driven textural analysis of extent of fibrosis at baseline and 15-month follow-up. Radiology. 2017;285:270–278. doi: 10.1148/radiol.2017161177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Jacob J., Bartholmai B.J., Rajagopalan S., Van Moorsel C.H.M., Van Es H.W., Van Beek F.T., Struik M.H.L., Kokosi M., Egashira R., Brun A.L., et al. Predicting outcomes in idiopathic pulmonary fibrosis using automated computed tomographic analysis. Am. J. Respir. Crit. Care Med. 2018;198:767–776. doi: 10.1164/rccm.201711-2174OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Mammarappallil J.G., Rankine L., Chan H.F., Weatherley N., Wild J., Driehuys B. New developments in imaging idiopathic pulmonary fibrosis with hyperpolarized xenon magnetic resonance imaging. J. Thorac. Imaging. 2019;34:136–150. doi: 10.1097/RTI.0000000000000392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kwon B.S., Choe J., Chae E.J., Hwang H.S., Kim Y.G., Song J.W. Progressive fibrosing interstitial lung disease: Prevalence and clinical outcome. Respir. Res. 2021;22:282. doi: 10.1186/s12931-021-01879-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Soon P.S., Kim E., Pon C.K., Gill A.J., Moore K., Spillane A.J., Benn D.E., Baxter R.C. Breast cancer-associated fibroblasts induce epithelial-to-mesenchymal transition in breast cancer cells. Endocr. Relat. Cancer. 2013;20:1–12. doi: 10.1530/ERC-12-0227. [DOI] [PubMed] [Google Scholar]
- 125.Mathai S.K., Schwartz D.A. Translational research in pulmonary fibrosis. Transl. Res. 2019;209:1–13. doi: 10.1016/j.trsl.2019.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kekevian A., Gershwin M.E., Chang C. Diagnosis and classification of idiopathic pulmonary fibrosis. Autoimmun. Rev. 2014;13:508–512. doi: 10.1016/j.autrev.2014.01.037. [DOI] [PubMed] [Google Scholar]
- 127.Cutting C.C., Bowman W.S., Dao N., Pugashetti J.V., Garcia C.K., Oldham J.M., Newton C.A. Family History of Pulmonary Fibrosis Predicts Worse Survival in Patients With Interstitial Lung Disease. Chest. 2021;159:1913–1921. doi: 10.1016/j.chest.2021.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Wang Y., Kuan P.J., Xing C., Cronkhite J.T., Torres F., Rosenblatt R.L., DiMaio J.M., Kinch L.N., Grishin N.V., Garcia C.K. Genetic Defects in Surfactant Protein A2 Are Associated with Pulmonary Fibrosis and Lung Cancer. Am. J. Hum. Genet. 2009;84:52–59. doi: 10.1016/j.ajhg.2008.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Song J.W., Ogura T., Inoue Y., Xu Z., Quaresma M., Stowasser S., Stansen W., Crestani B. Long-term treatment with nintedanib in Asian patients with idiopathic pulmonary fibrosis: Results from INPULSIS®-ON. Respirology. 2020;25:410–416. doi: 10.1111/resp.13647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Barratt S.L., Mulholland S., Al Jbour K., Steer H., Gutsche M., Foley N., Srivastava R., Sharp C., Adamali H.I. South-West of England’s Experience of the Safety and Tolerability Pirfenidone and Nintedanib for the Treatment of Idiopathic Pulmonary Fibrosis (IPF) Front. Pharmacol. 2018;9:1480. doi: 10.3389/fphar.2018.01480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Noble P.W., Albera C., Bradford W.Z., Costabel U., Glassberg M.K., Kardatzke D., King T.E., Jr., Lancaster L., Sahn S.A., Szwarcberg J., et al. Pirfenidone in patients with idiopathic pulmonary fi brosis ( CAPACITY ): Two randomised trials. Lancet. 2011;377:1760–1769. doi: 10.1016/S0140-6736(11)60405-4. [DOI] [PubMed] [Google Scholar]
- 132.Shin K.H., Shin S.W. Idiopathic Pulmonary Fibrosis. N. Engl. J. Med. 2018;379:795–796. doi: 10.1056/NEJMc1807508. [DOI] [PubMed] [Google Scholar]
- 133.Feng H., Zhao Y., Li Z., Kang J. Real-life experiences in a single center: Efficacy of pirfenidone in idiopathic pulmonary fibrosis and fibrotic idiopathic non-specific interstitial pneumonia patients. Ther. Adv. Respir. Dis. 2020;14:1753466620963015. doi: 10.1177/1753466620963015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Allen R.J., Porte J., Braybrooke R., Flores C., Fingerlin T.E., Oldham J.M., Guillen-Guio B., Ma S.F., Okamoto T., John A.E., et al. Genetic variants associated with susceptibility to idiopathic pulmonary fibrosis in people of European ancestry: A genome-wide association study. Lancet Respir. Med. 2017;5:869–880. doi: 10.1016/S2213-2600(17)30387-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Allen R.J., Guillen-Guio B., Oldham J.M., Ma S.F., Dressen A., Paynton M.L., Kraven L.M., Obeidat M., Li X., Ng M., et al. Genome-wide association study of susceptibility to idiopathic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 2020;201:564–574. doi: 10.1164/rccm.201905-1017OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Shull J.G., Pay M.T., Lara Compte C., Olid M., Bermudo G., Portillo K., Sellarés J., Balcells E., Vicens-Zygmunt V., Planas-Cerezales L., et al. Mapping IPF helps identify geographic regions at higher risk for disease development and potential triggers. Respirology. 2020:1–8. doi: 10.1111/resp.13973. [DOI] [PubMed] [Google Scholar]
- 137.Padilla M. Idiopathic pulmonary fibrosis: The role of pathobiology in making a definitive diagnosis. Am. J. Manag. Care. 2015;21((Suppl. 14)):s276–s283. [PubMed] [Google Scholar]
- 138.Lettieri S., Oggionni T., Lancia A., Bortolotto C., Stella G.M. Immune Stroma in Lung Cancer and Idiopathic Pulmonary Fibrosis: A Common Biologic Landscape? Int. J. Mol. Sci. 2021;22:2882. doi: 10.3390/ijms22062882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Song M.J., Kim S.Y., Park M.S., Kang M.J., Lee S.H., Park S.C. A nationwide population-based study of incidence and mortality of lung cancer in idiopathic pulmonary fibrosis. Sci. Rep. 2021;11:2596. doi: 10.1038/s41598-021-82182-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Herbst R.S., Morgensztern D., Boshoff C. The biology and management of non-small cell lung cancer. Nature. 2018;553:446–454. doi: 10.1038/nature25183. [DOI] [PubMed] [Google Scholar]
- 141.Tzouvelekis A., Gomatou G., Bouros E., Trigidou R., Tzilas V., Bouros D. Common Pathogenic Mechanisms between Idiopathic Pulmonary Fibrosis and Lung Cancer. Chest. 2019;156:383–391. doi: 10.1016/j.chest.2019.04.114. [DOI] [PubMed] [Google Scholar]
- 142.Selman M., Pardo A. The leading role of epithelial cells in the pathogenesis of idiopathic pulmonary fibrosis. Cell. Signal. 2020;66:109482. doi: 10.1016/j.cellsig.2019.109482. [DOI] [PubMed] [Google Scholar]
- 143.Barron L., Gharib S.A., Duffield J.S. Lung Pericytes and Resident Fibroblasts: Busy Multitaskers. Am. J. Pathol. 2016;186:2519–2531. doi: 10.1016/j.ajpath.2016.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.El Agha E., Moiseenko A., Kheirollahi V., De Langhe S., Crnkovic S., Kwapiszewska G., Kosanovic D., Schwind F., Schermuly R.T., Henneke I., et al. Two-Way Conversion between Lipogenic and Myogenic Fibroblastic Phenotypes Marks the Progression and Resolution of Lung Fibrosis. Cell Stem. Cell. 2017;20:261–273. doi: 10.1016/j.stem.2016.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Jovanovic D., Roksandic Milenkovic M., Kotur Stevuljevic J., Markovic J., Ceriman V., Kontic M., Skodric Trifunovic V. Membrane PD-L1 expression and soluble PD-L1 plasma levels in idiopathic pulmonary fibrosis-a pilot study. J. Thorac. Dis. 2018;10:6660–6669. doi: 10.21037/jtd.2018.11.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Xie T., Liang J., Liu N., Huan C., Zhang Y., Liu W., Kumar M., Xiao R., D’Armiento J., Metzger D., et al. Transcription factor TBX4 regulates myofibroblast accumulation and lung fibrosis. J. Clin. Investig. 2016;126:3063–3079. doi: 10.1172/JCI85328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Marriott S., Baskir R.S., Gaskill C., Menon S., Carrier E.J., Williams J., Talati M., Helm K., Alford C.E., Kropski J.A., et al. ABCG2pos lung mesenchymal stem cells are a novel pericyte subpopulation that contributes to fibrotic remodeling. Am. J. Physiol. Cell Physiol. 2014;307:C684–C698. doi: 10.1152/ajpcell.00114.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Karki S., Surolia R., Hock T.D., Guroji P., Zolak J.S., Duggal R., Ye T., Thannickal V.J., Antony V.B. Wilms’ tumor 1 (Wt1) regulates pleural mesothelial cell plasticity and transition into myofibroblasts in idiopathic pulmonary fibrosis. FASEB J. 2014;28:1122–1131. doi: 10.1096/fj.13-236828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Rock J.R., Barkauskas C.E., Cronce M.J., Xue Y., Harris J.R., Liang J., Noble P.W., Hogan B.L.M. Multiple stromal populations contribute to pulmonary fibrosis without evidence for epithelial to mesenchymal transition. Proc. Natl. Acad. Sci. USA. 2011:108. doi: 10.1073/pnas.1117988108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Strieter R.M., Keeley E.C., Hughes M.A., Burdick M.D., Mehrad B. The role of circulating mesenchymal progenitor cells (fibrocytes) in the pathogenesis of pulmonary fibrosis. J. Leukoc. Biol. 2009;86:1111–1118. doi: 10.1189/jlb.0309132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Shiga K., Hara M., Nagasaki T., Sato T., Takahashi H., Takeyama H. Cancer-associated fibroblasts: Their characteristics and their roles in tumor growth. Cancers. 2015;7:2443–2458. doi: 10.3390/cancers7040902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Chen C., Hou J., Yu S., Li W., Wang X., Sun H., Qin T., Claret F.X., Guo H., Liu Z. Role of cancer-associated fibroblasts in the resistance to antitumor therapy, and their potential therapeutic mechanisms in non-small cell lung cancer (Review) Oncol. Lett. 2021;21:1–12. doi: 10.3892/ol.2020.12296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Domen A., Quatannens D., Zanivan S., Deben C., Van Audenaerde J., Smits E., Wouters A., Lardon F., Roeyen G., Verhoeven Y., et al. Cancer-associated fibroblasts as a common orchestrator of therapy resistance in lung and pancreatic cancer. Cancers. 2021;13:987. doi: 10.3390/cancers13050987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.De P., Aske J., Dey N. Cancer-Associated Fibroblast Functions as a Road-Block in Cancer Therapy. Cancers. 2021;13:5246. doi: 10.3390/cancers13205246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Edwards Y.S. Stretch stimulation: Its effects on alveolar type II cell function in the lung. Comp. Biochem. Physiol. A Mol. Integr. Physiol. 2001;129:245–260. doi: 10.1016/S1095-6433(01)00321-X. [DOI] [PubMed] [Google Scholar]
- 156.Heise R.L., Stober V., Cheluvaraju C., Hollingsworth J.W., Garantziotis S. Mechanical stretch induces epithelial-mesenchymal transition in alveolar epithelia via hyaluronan activation of innate immunity. J. Biol. Chem. 2011;286:17435–17444. doi: 10.1074/jbc.M110.137273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Arnadóttir J., Chalfie M. Eukaryotic mechanosensitive channels. Annu. Rev. Biophys. 2010;39:111–137. doi: 10.1146/annurev.biophys.37.032807.125836. [DOI] [PubMed] [Google Scholar]
- 158.Anishkin A., Loukin S.H., Teng J., Kung C. Feeling the hidden mechanical forces in lipid bilayer is an original sense. Proc. Natl. Acad. Sci. USA. 2014;111:7898–7905. doi: 10.1073/pnas.1313364111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Leckband D.E., de Rooij J. Cadherin adhesion and mechanotransduction. Annu. Rev. Cell Dev. Biol. 2014;30:291–315. doi: 10.1146/annurev-cellbio-100913-013212. [DOI] [PubMed] [Google Scholar]
- 160.Even-Ram S., Artym V., Yamada K.M. Matrix control of stem cell fate. Cell. 2006;126:645–647. doi: 10.1016/j.cell.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 161.Lo C.M., Wang H.B., Dembo M., Wang Y.L. Cell movement is guided by the rigidity of the substrate. Biophys. J. 2000;79:144–152. doi: 10.1016/S0006-3495(00)76279-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Geiger B., Spatz J.P., Bershadsky A.D. Environmental sensing through focal adhesions. Nat. Rev. Mol. Cell Biol. 2009;10:21–33. doi: 10.1038/nrm2593. [DOI] [PubMed] [Google Scholar]
- 163.Ringer P., Colo G., Fässler R., Grashoff C. Sensing the mechano-chemical properties of the extracellular matrix. Matrix Biol. 2017;64:6–16. doi: 10.1016/j.matbio.2017.03.004. [DOI] [PubMed] [Google Scholar]
- 164.Hynes R.O. The extracellular matrix: Not just pretty fibrils. Science. 2009;326:1216–1219. doi: 10.1126/science.1176009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Hynes R.O. Integrins: Bidirectional, allosteric signaling machines. Cell. 2002;110:673–687. doi: 10.1016/S0092-8674(02)00971-6. [DOI] [PubMed] [Google Scholar]
- 166.Schiller H.B., Fässler R. Mechanosensitivity and compositional dynamics of cell-matrix adhesions. EMBO Rep. 2013;14:509–519. doi: 10.1038/embor.2013.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Roca-Cusachs P., Gauthier N.C., Del Rio A., Sheetz M.P. Clustering of alpha(5)beta(1) integrins determines adhesion strength whereas alpha(v)beta(3) and talin enable mechanotransduction. Proc. Natl. Acad. Sci. USA. 2009;106:16245–16250. doi: 10.1073/pnas.0902818106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Legate K.R., Wickström S.A., Fässler R. Genetic and cell biological analysis of integrin outside-in signaling. Genes Dev. 2009;23:397–418. doi: 10.1101/gad.1758709. [DOI] [PubMed] [Google Scholar]
- 169.Liu F., Mih J.D., Shea B.S., Kho A.T., Sharif A.S., Tager A.M., Tschumperlin D.J. Feedback amplification of fibrosis through matrix stiffening and COX-2 suppression. J. Cell Biol. 2010;190:693–706. doi: 10.1083/jcb.201004082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Sheppard D. Functions of pulmonary epithelial integrins: From development to disease. Physiol. Rev. 2003;83:673–686. doi: 10.1152/physrev.00033.2002. [DOI] [PubMed] [Google Scholar]
- 171.Chen Y., Yi H.T., Wu X., Haroldson R., Gartstein Y.N., Rodionov Y.I., Tikhonov K.S., Zakhidov A., Zhu X.Y., Podzorov V. Extended carrier lifetimes and diffusion in hybrid perovskites revealed by Hall effect and photoconductivity measurements. Nat. Commun. 2016;7:12253. doi: 10.1038/ncomms12253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Jokinen J., Dadu E., Nykvist P., Käpylä J., White D.J., Ivaska J., Vehviläinen P., Reunanen H., Larjava H., Häkkinen L., et al. Integrin-mediated cell adhesion to type I collagen fibrils. J. Biol. Chem. 2004;279:31956–31963. doi: 10.1074/jbc.M401409200. [DOI] [PubMed] [Google Scholar]
- 173.Xia H., Diebold D., Nho R., Perlman D., Kleidon J., Kahm J., Avdulov S., Peterson M., Nerva J., Bitterman P., et al. Pathological integrin signaling enhances proliferation of primary lung fibroblasts from patients with idiopathic pulmonary fibrosis. J. Exp. Med. 2008;205:1659–1672. doi: 10.1084/jem.20080001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Lukey P.T., Coello C., Gunn R., Parker C., Wilson F.J., Saleem A., Garman N., Costa M., Kendrick S., Onega M. Clinical quantification of the integrin αvβ6 by [18F]FB-A20FMDV2 positron emission tomography in healthy and fibrotic human lung (PETAL Study) Eur. J. Nucl. Med. Mol. Imaging. 2020;47:967–979. doi: 10.1007/s00259-019-04586-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Munger J.S., Huang X., Kawakatsu H., Griffiths M.J., Dalton S.L., Wu J., Pittet J.F., Kaminski N., Garat C., Matthay M.A., et al. The integrin alpha v beta 6 binds and activates latent TGF beta 1: A mechanism for regulating pulmonary inflammation and fibrosis. Cell. 1999;96:319–328. doi: 10.1016/S0092-8674(00)80545-0. [DOI] [PubMed] [Google Scholar]
- 176.Aluwihare P., Mu Z., Zhao Z., Yu D., Weinreb P.H., Horan G.S., Violette S.M., Munger J.S. Mice that lack activity of alphavbeta6- and alphavbeta8-integrins reproduce the abnormalities of Tgfb1- and Tgfb3-null mice. Pt 2J. Cell Sci. 2009;122:227–232. doi: 10.1242/jcs.035246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Pittet J.F., Griffiths M.J., Geiser T., Kaminski N., Dalton S.L., Huang X., Brown L.A., Gotwals P.J., Koteliansky V.E., Matthay M.A., et al. TGF-beta is a critical mediator of acute lung injury. J. Clin. Investig. 2001;107:1537–1544. doi: 10.1172/JCI11963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.John A.E., Graves R.H., Pun K.T., Vitulli G., Forty E.J., Mercer P.F., Morrell J.L., Barrett J.W., Rogers R.F., Hafeji M. Translational pharmacology of an inhaled small molecule αvβ6 integrin inhibitor for idiopathic pulmonary fibrosis. Nat. Commun. 2020;11:4659. doi: 10.1038/s41467-020-18397-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Plessner M., Melak M., Chinchilla P., Baarlink C., Grosse R. Nuclear F-actin formation and reorganization upon cell spreading. J. Biol. Chem. 2015;290:11209–11216. doi: 10.1074/jbc.M114.627166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Hermann M.R., Jakobson M., Colo G.P., Rognoni E., Jakobson M., Kupatt C., Posern G., Fässler R. Integrins synergise to induce expression of the MRTF-A-SRF target gene ISG15 for promoting cancer cell invasion. J. Cell Sci. 2016;129:1391–1403. doi: 10.1242/jcs.177592. [DOI] [PubMed] [Google Scholar]
- 181.Huang X., Yang N., Fiore V.F., Barker T.H., Sun Y., Morris S.W., Ding Q., Thannickal V.J., Zhou Y. Matrix stiffness-induced myofibroblast differentiation is mediated by intrinsic mechanotransduction. Am. J. Respir. Cell Mol. Biol. 2012;47:340–348. doi: 10.1165/rcmb.2012-0050OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Uhlén M., Fagerberg L., Hallström B.M., Lindskog C., Oksvold P., Mardinoglu A., Sivertsson Å., Kampf C., Sjöstedt E., Asplund A., et al. Proteomics. Tissue-based map of the human proteome. Science. 2015;347:1260419. doi: 10.1126/science.1260419. [DOI] [PubMed] [Google Scholar]
- 183.Levental K.R., Yu H., Kass L., Lakins J.N., Egeblad M., Erler J.T., Fong S.F., Csiszar K., Giaccia A., Weninger W., et al. Matrix crosslinking forces tumor progression by enhancing integrin signaling. Cell. 2009;139:891–906. doi: 10.1016/j.cell.2009.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Yuan Y., Zhong W., Ma G., Zhang B., Tian H. Yes-associated protein regulates the growth of human non-small cell lung cancer in response to matrix stiffness. Mol. Med. Rep. 2015;11:4267–4272. doi: 10.3892/mmr.2015.3231. [DOI] [PubMed] [Google Scholar]
- 185.Guilluy C., Osborne L.D., Van Landeghem L., Sharek L., Superfine R., Garcia-Mata R., Burridge K. Isolated nuclei adapt to force and reveal a mechanotransduction pathway in the nucleus. Nat Cell Biol. 2014;16:376–381. doi: 10.1038/ncb2927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Darby I.A., Laverdet B., Bonté F., Desmoulière A. Fibroblasts and myofibroblasts in wound healing. Clin. Cosmet. Investig. Dermatol. 2014;7:301–311. doi: 10.2147/CCID.S50046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Wang J., Zohar R., McCulloch C.A. Multiple roles of alpha-smooth muscle actin in mechanotransduction. Exp. Cell Res. 2006;312:205–214. doi: 10.1016/j.yexcr.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 188.van Caam A., Vonk M., van den Hoogen F., van Lent P., van der Kraan P. Unraveling SSc Pathophysiology; The Myofibroblast. Front Immunol. 2018;9:2452. doi: 10.3389/fimmu.2018.02452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Hinz B. Formation and function of the myofibroblast during tissue repair. J. Investig. Dermatol. 2007;127:526–537. doi: 10.1038/sj.jid.5700613. [DOI] [PubMed] [Google Scholar]
- 190.Tai Y., Woods E.L., Dally J., Kong D., Steadman R., Moseley R., Midgley A.C. Myofibroblasts: Function, Formation, and Scope of Molecular Therapies for Skin Fibrosis. Biomolecules. 2021;11:1095. doi: 10.3390/biom11081095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Biernacka A., Dobaczewski M., Frangogiannis N.G. TGF-β signaling in fibrosis. Growth Factors. 2011;29:196202. doi: 10.3109/08977194.2011.595714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.He W., Dai C. Key Fibrogenic Signaling. Curr. Pathobiol. Rep. 2015;3:183–192. doi: 10.1007/s40139-015-0077-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Umbarkar P., Ejantkar S., Tousif S., Lal H. Mechanisms of Fibroblast Activation and Myocardial Fibrosis: Lessons Learned from FB-Specific Conditional Mouse Models. Cells. 2021;10:2412. doi: 10.3390/cells10092412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Lin F., Ren X.-D., Pan Z., Macri L., Zong W.-X., Tonnesen M.G., Rafailovich M., Bar-Sagi D., Clark R.A. Fibronectin growth factor-binding domains are required for fibroblast survival. J. Investig. Dermatol. 2011;131:84–98. doi: 10.1038/jid.2010.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Simone T.M., Higgins C.E., Czekay R.P., Law B.K., Higgins S.P., Archambeault J., Kutz S.M., Higgins P.J. SERPINE1: A Molecular Switch in the Proliferation-Migration Dichotomy in Wound-"Activated" Keratinocytes. Adv. Wound Care. 2014;3:281–290. doi: 10.1089/wound.2013.0512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Lin C.H., Yu M.C., Tung W.H., Chen T.T., Yu C.C., Weng C.M., Tsai Y.J., Bai K.J., Hong C.Y., Chien M.H., et al. Connective tissue growth factor induces collagen I expression in human lung fibroblasts through the Rac1/MLK3/JNK/AP-1 pathway. Biochim. Biophys. Acta. 2013;1833:2823–2833. doi: 10.1016/j.bbamcr.2013.07.016. [DOI] [PubMed] [Google Scholar]
- 197.Midgley A.C., Rogers M., Hallett M.B., Clayton A., Bowen T., Phillips A.O., Steadman R. Transforming growth factor-β1 (TGF-β1)-stimulated fibroblast to myofibroblast differentiation is mediated by hyaluronan (HA)-facilitated epidermal growth factor receptor (EGFR) and CD44 co-localization in lipid rafts. J. Biol. Chem. 2013;288:14824–14838. doi: 10.1074/jbc.M113.451336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Kim C.L., Choi S.H., Mo J.S. Role of the Hippo Pathway in Fibrosis and Cancer. Cells. 2019;8:468. doi: 10.3390/cells8050468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Szeto S.G., Narimatsu M., Lu M., He X., Sidiqi A.M., Tolosa M.F., Chan L., De Freitas K., Bialik J.F., Majumder S., et al. YAP/TAZ Are Mechanoregulators of TGF-β-Smad Signaling and Renal Fibrogenesis. J. Am. Soc. Nephrol. 2016;27:3117–3128. doi: 10.1681/ASN.2015050499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Frangogiannis N.G. Fibroblast-Extracellular Matrix Interactions in Tissue Fibrosis. Curr Pathobiol. Rep. 2016;4:11–18. doi: 10.1007/s40139-016-0099-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Klingberg F., Chau G., Walraven M., Boo S., Koehler A., Chow M.L., Olsen A.L., Im M., Lodyga M., Wells R.G., et al. The fibronectin ED-A domain enhances recruitment of latent TGF-β-binding protein-1 to the fibroblast matrix. J. Cell Sci. 2018;131:jcs201293. doi: 10.1242/jcs.201293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Micallef L., Vedrenne N., Billet F., Coulomb B., Darby I.A., Desmoulière A. The myofibroblast, multiple origins for major roles in normal and pathological tissue repair. Fibrogenesis Tissue Repair. 2012;5((Suppl. 1)) doi: 10.1186/1755-1536-5-S1-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Marchioni A., Tonelli R., Cerri S., Castaniere I., Andrisani D., Gozzi F., Bruzzi G., Manicardi L., Moretti A., Demurtas J., et al. Pulmonary Stretch and Lung Mechanotransduction: Implications for Progression in the Fibrotic Lung. Int. J. Mol. Sci. 2021;22:6443. doi: 10.3390/ijms22126443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Bonnans C., Chou J., Werb Z. Remodelling the extracellular matrix in development and disease. Nat. Rev. Mol. Cell Biol. 2014;15:786–801. doi: 10.1038/nrm3904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Poltavets V., Kochetkova M., Pitson S.M., Samuel M.S. The Role of the Extracellular Matrix and Its Molecular and Cellular Regulators in Cancer Cell Plasticity. Front. Oncol. 2018;8:431. doi: 10.3389/fonc.2018.00431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Winkler J., Abisoye-Ogunniyan A., Metcalf K.J., Werb Z. Concepts of extracellular matrix remodelling in tumour progression and metastasis. Nat. Commun. 2020;11:5120. doi: 10.1038/s41467-020-18794-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Davidson S., Coles M., Thomas T., Kollias G., Ludewig B., Turley S., Brenner M., Buckley C.D. Fibroblasts as immune regulators in infection, inflammation and cancer. Nat. Rev. Immunol. 2021 doi: 10.1038/s41577-021-00540-z. [DOI] [PubMed] [Google Scholar]
- 208.Wei K., Nguyen H.N., Brenner M.B. Fibroblast pathology in inflammatory diseases. J. Clin. Investig. 2021;131:e149538. doi: 10.1172/JCI149538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Du H., Chen D., Zhou Y., Han Z., Che G. Fibroblast phenotypes in different lung diseases. J. Cardiothorac. Surg. 2014;9:147. doi: 10.1186/s13019-014-0147-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Monteran L., Erez N. The Dark Side of Fibroblasts: Cancer-Associated Fibroblasts as Mediators of Immunosuppression in the Tumor Microenvironment. Front. Immunol. 2019;10:1835. doi: 10.3389/fimmu.2019.01835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.De Jaeghere E.A., Denys H.G., De Wever O. Fibroblasts Fuel Immune Escape in the Tumor Microenvironment. Trends Cancer. 2019;5:704–723. doi: 10.1016/j.trecan.2019.09.009. [DOI] [PubMed] [Google Scholar]
- 212.Yazdani S., Bansal R., Prakash J. Drug targeting to myofibroblasts: Implications for fibrosis and cancer. Adv. Drug Deliv. Rev. 2017;121:101–116. doi: 10.1016/j.addr.2017.07.010. [DOI] [PubMed] [Google Scholar]
- 213.Aja L., Dituri F., Mancarella S., Caballero-Diaz D., Moustakas A., Giannelli G., Fabregat I. TGF-β and the Tissue Microenvironment: Relevance in Fibrosis and Cancer. Int. J. Mol. Sci. 2018;19:1294. doi: 10.3390/ijms19051294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Chen P.Y., Wei W.F., Wu H.Z., Fan L.S., Wang W. Cancer-Associated Fibroblast Heterogeneity: A Factor That Cannot Be Ignored in Immune Microenvironment Remodeling. Front Immunol. 2021;12:671595. doi: 10.3389/fimmu.2021.671595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Ji X., Ji J., Shan F., Zhang Y., Chen Y., Lu X. Cancer-associated fibroblasts from NSCLC promote the radioresistance in lung cancer cell lines. Int. J. Clin. Exp. Med. 2015;8:7002–7008. [PMC free article] [PubMed] [Google Scholar]
- 216.Hua W., Ten Dijke P., Kostidis S., Giera M., Hornsveld M. TGF-β-induced metabolic reprogramming during epithelial-to-mesenchymal transition in cancer. Cell Mol. Life Sci. 2020;77:2103–2123. doi: 10.1007/s00018-019-03398-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Pereira B.A., Vennin C., Papanicolaou M., Chambers C.R., Herrmann D., Morton J.P., Cox T.R., Timpson P. CAF Subpopulations: A New Reservoir of Stromal Targets in Pancreatic Cancer. Trends Cancer. 2019;5:724–741. doi: 10.1016/j.trecan.2019.09.010. [DOI] [PubMed] [Google Scholar]
- 218.Chen K., Wang Q., Li M., Guo H., Liu W., Wang F., Tian X., Yang Y. Single-cell RNA-seq reveals dynamic change in tumor microenvironment during pancreatic ductal adenocarcinoma malignant progression. EBioMedicine. 2021;66:103315. doi: 10.1016/j.ebiom.2021.103315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Özdemir B.C., Pentcheva-Hoang T., Carstens J.L., Zheng X., Wu C.C., Simpson T.R., Laklai H., Sugimoto H., Kahlert C., Novitskiy S.V., et al. Depletion of carcinoma-associated fibroblasts and fibrosis induces immunosuppression and accelerates pancreas cancer with reduced survival. Cancer Cell. 2014;25:719–734. doi: 10.1016/j.ccr.2014.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Duda D.G., Duyverman A.M., Kohno M., Snuderl M., Steller E.J., Fukumura D., Jain R.K. Malignant cells facilitate lung metastasis by bringing their own soil. Proc. Natl. Acad. Sci. USA. 2010;107:21677–21682. doi: 10.1073/pnas.1016234107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Kugeratski F.G., Atkinson S.J., Neilson L.J., Lilla S., Knight J.R.P., Serneels J., Juin A., Ismail S., Bryant D.M., Markert E.K., et al. Hypoxic cancer-associated fibroblasts increase NCBP2-AS2/HIAR to promote endothelial sprouting through enhanced VEGF signaling. Sci. Signal. 2019;12:eaan8247. doi: 10.1126/scisignal.aan8247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Loomis-King H., Flaherty K.R., Moore B.B. Pathogenesis, current treatments and future directions for idiopathic pulmonary fibrosis. Curr. Opin. Pharmacol. 2013;13:377–385. doi: 10.1016/j.coph.2013.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Sgalla G., Cocconcelli E., Tonelli R., Richeldi L. Novel drug targets for idiopathic pulmonary fibrosis. Expert Rev. Respir. Med. 2016;10:393–405. doi: 10.1586/17476348.2016.1152186. [DOI] [PubMed] [Google Scholar]
- 224.Krauss E., Gehrken G., Drakopanagiotakis F., Tello S., Dartsch R.C., Maurer O., Windhorst A., von der Beck D., Griese M., Seeger W., et al. Clinical characteristics of patients with familial idiopathic pulmonary fibrosis (f-IPF) BMC Pulm. Med. 2019;19:130. doi: 10.1186/s12890-019-0895-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Glaspole I.N., Chapman S.A., Cooper W.A., Ellis S.J., Goh N.S., Hopkins P.M., Macansh S., Mahar A., Moodley Y.P., Paul E., et al. Health-related quality of life in idiopathic pulmonary fibrosis: Data from the Australian IPF Registry. Respirology. 2017;22:950–956. doi: 10.1111/resp.12989. [DOI] [PubMed] [Google Scholar]
- 226.Sgalla G., Biffi A., Richeldi L. Idiopathic pulmonary fibrosis: Diagnosis, epidemiology and natural history. Respirology. 2016:427–437. doi: 10.1111/resp.12683. [DOI] [PubMed] [Google Scholar]
- 227.King T.E., Jr., Pardo A., Selman M. Idiopathic pulmonary fibrosis. Lancet. 2011;378:1949–1961. doi: 10.1016/S0140-6736(11)60052-4. [DOI] [PubMed] [Google Scholar]
- 228.Rogliani P., Calzetta L., Cavalli F., Matera M.G., Cazzola M. Pirfenidone, nintedanib and N-acetylcysteine for the treatment of idiopathic pulmonary fibrosis: A systematic review and meta-analysis. Pulm. Pharmacol. Ther. 2016;40:95–103. doi: 10.1016/j.pupt.2016.07.009. [DOI] [PubMed] [Google Scholar]
- 229.Hisatomi K., Mukae H., Sakamoto N., Ishimatsu Y., Kakugawa T., Hara S., Fujita H., Nakamichi S., Oku H., Urata Y., et al. Pirfenidone inhibits TGF-beta1-induced over-expression of collagen type I and heat shock protein 47 in A549 cells. BMC Pulm. Med. 2012;12:24. doi: 10.1186/1471-2466-12-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Nakayama S., Mukae H., Sakamoto N., Kakugawa T., Yoshioka S., Soda H., Oku H., Urata Y., Kondo T., Kubota H., et al. Pirfenidone inhibits the expression of HSP47 in TGF-beta1-stimulated human lung fibroblasts. Life Sci. 2008;82:210–217. doi: 10.1016/j.lfs.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 231.Oku H., Shimizu T., Kawabata T., Nagira M., Hikita I., Ueyama A., Matsushima S., Torii M., Arimura A. Antifibrotic action of Pirfenidone and prednisolone: Different effects on pulmonary cytokines and growth factors in bleomycin-induced murine pulmonary fibrosis. Eur. J. Pharmacol. 2008;590:400–408. doi: 10.1016/j.ejphar.2008.06.046. [DOI] [PubMed] [Google Scholar]
- 232.Choi K., Lee K., Ryu S.W., Im M., Kook K.H., Choi C. Pirfenidone inhibits transforming growth factor-beta1-induced fibrogenesis by blocking nuclear translocation of Smads in human retinal pigment epithelial cell line ARPE-19. Mol. Vis. 2012;18:1010–1020. [PMC free article] [PubMed] [Google Scholar]
- 233.Miura Y., Saito T., Tanaka T., Takoi H., Yatagai Y., Inomata M., Nei T., Saito Y., Gemma A., Azuma A. Reduced incidence of lung cancer in patients with idiopathic pulmonary fibrosis treated with Pirfenidone. Respir. Investig. 2018;56:72–79. doi: 10.1016/j.resinv.2017.09.007. [DOI] [PubMed] [Google Scholar]
- 234.Xiao H., Zhang G.F., Liao X.P., Li X.J., Zhang J., Lin H., Chen Z., Zhang X. Anti-fibrotic effects of Pirfenidone by interference with the hedgehog signaling pathway in patients with systemic sclerosis-associated interstitial lung disease. Int. J. Rheum. Dis. 2018;21:477–486. doi: 10.1111/1756-185X.13247. [DOI] [PubMed] [Google Scholar]
- 235.Mediavilla-Varela M., Boateng K., Noyes D., Antonia S.J. The anti-fibrotic agent Pirfenidone synergizes with cisplatin in killing tumor cells and cancer-associated fibroblasts. BMC Cancer. 2016;16:176. doi: 10.1186/s12885-016-2162-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Raghu G., Rochwerg B., Zhang Y., Garcia C.A., Azuma A., Behr J., Brozek J.L., Collard H.R., Cunningham W., Homma S., et al. An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline: Treatment of Idiopathic Pulmonary Fibrosis. An Update of the 2011 Clinical Practice Guideline. Am. J. Respir. Crit. Care Med. 2015;192:e3–e19. doi: 10.1164/rccm.201506-1063ST. [DOI] [PubMed] [Google Scholar]
- 237.Duchemann B., Didier M., Pailler M.C., Brillet P.Y., Kambouchner M., Uzunhan Y., Freynet O., Chouahnia K., Zelek L., Nunes H. Le nivolumab peut-il être utilisé dans les fibroses pulmonaires idiopathiques ? [Can nivolumab be used safely in idiopathic pulmonary fibrosis?] Rev. Mal. Respir. 2019;36:209–213. doi: 10.1016/j.rmr.2018.11.001. [DOI] [PubMed] [Google Scholar]
- 238.Wollin L., Wex E., Pautsch A., Schnapp G., Hostettler K.E., Stowasser S., Kolb M. Mode of action of Nintedanib in the treatment of idiopathic pulmonary fibrosis. Eur. Respir. J. 2015;45:1434–1445. doi: 10.1183/09031936.00174914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Amano H., Matsui Y., Hatanaka K., Hosono K., Ito Y. VEGFR1-tyrosine kinase signaling in pulmonary fibrosis. Inflamm. Regen. 2021;41:16. doi: 10.1186/s41232-021-00166-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Grimminger F., Günther A., Vancheri C. The role of tyrosine kinases in the pathogenesis of idiopathic pulmonary fibrosis. Eur. Respir. J. 2015;45:1426–1433. doi: 10.1183/09031936.00149614. [DOI] [PubMed] [Google Scholar]
- 241.Song Y., Wu Y.L., Cao L.J., Chen J.H., Ma Z.Y., Cui J.W., Wang J., Liu H.B., Ding J.Y., Hu M. Efficacy and Safety of Gefitinib as Third-line Treatment in NSCLC Patients With Activating EGFR Mutations Treated With First-line Gefitinib Followed by Second-line Chemotherapy: A Single-Arm, Prospective, Multicenter Phase II Study (RE-CHALLENGE, CTONG1304) Am. J. Clin. Oncol. 2019;42:432–439. doi: 10.1097/COC.0000000000000538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Wang Y., Yella J.K., Ghandikota S., Cherukuri T.C., Ediga H.H., Madala S.K., Jegga A.G. Pan-transcriptome-based candidate therapeutic discovery for idiopathic pulmonary fibrosis. Ther. Adv. Respir. Dis. 2020;14:1753466620971143. doi: 10.1177/1753466620971143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Reck M., Kaiser R., Mellemgaard A., Douillard J.Y., Orlov S., Krzakowski M., von Pawel J., Gottfried M., Bondarenko I., Liao M., et al. Docetaxel plus Nintedanib versus docetaxel plus placebo in patients with previously treated non-small-cell lung cancer (LUME-Lung 1): A phase 3, double-blind, randomised controlled trial. Lancet Oncol. 2014;15:143–155. doi: 10.1016/S1470-2045(13)70586-2. [DOI] [PubMed] [Google Scholar]
- 244.Soria J.C., Shepherd F.A., Douillard J.Y., Wolf J., Giaccone G., Crino L., Cappuzzo F., Sharma S., Gross S.H., Dimitrijevic S., et al. Efficacy of everolimus (RAD001) in patients with advanced NSCLC previously treated with chemotherapy alone or with chemotherapy and EGFR inhibitors. Ann. Oncol. 2009;20:1674–1681. doi: 10.1093/annonc/mdp060. [DOI] [PubMed] [Google Scholar]
- 245.Narov K., Yang J., Samsel P., Jones A., Sampson J.R., Shen M.H. The dual PI3K/mTOR inhibitor GSK2126458 is effective for treating solid renal tumours in Tsc2+/- mice through suppression of cell proliferation and induction of apoptosis. Oncotarget. 2017;8:58504–58512. doi: 10.18632/oncotarget.17215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Ahluwalia N., Shea B.S., Tager A.M. New therapeutic targets in idiopathic pulmonary fibrosis. Aiming to rein in runaway wound-healing responses. Am. J. Respir. Crit. Care Med. 2014;190:867–878. doi: 10.1164/rccm.201403-0509PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Ballester B., Milara J., Cortijo J. Idiopathic Pulmonary Fibrosis and Lung Cancer: Mechanisms and Molecular Targets. Int. J. Mol. Sci. 2019;20:593. doi: 10.3390/ijms20030593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Wuyts W.A., Antoniou K.M., Borensztajn K., Costabel U., Cottin V., Crestani B., Grutters J.C., Maher T.M., Poletti V., Richeldi L., et al. Combination therapy: The future of management for idiopathic pulmonary fibrosis? Lancet Respir. Med. 2014;2:933–942. doi: 10.1016/S2213-2600(14)70232-2. [DOI] [PubMed] [Google Scholar]
- 249.Ide M., Tanaka K., Sunami S., Asoh T., Maeyama T., Tsuruta N., Nakanishi Y., Okamoto I. Durable response to nivolumab in a lung adenocarcinoma patient with idiopathic pulmonary fibrosis. Thorac. Cancer. 2018;9:1519–1521. doi: 10.1111/1759-7714.12853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Malouf M.A., Hopkins P., Snell G., Glanville A.R., Everolimus in IPF Study Investigators An investigator-driven study of everolimus in surgical lung biopsy confirmed idiopathic pulmonary fibrosis. Respirology. 2011;16:776–783. doi: 10.1111/j.1440-1843.2011.01955.x. [DOI] [PubMed] [Google Scholar]
- 251.Yuan R., Kay A., Berg W.J., Lebwohl D. Targeting tumorigenesis: Development and use of mTOR inhibitors in cancer therapy. J. Hematol. Oncol. 2009;2:45. doi: 10.1186/1756-8722-2-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Singh P., Kumar V., Gupta S.K., Kumari G., Verma M. Combating TKI resistance in CML by inhibiting the PI3K/Akt/mTOR pathway in combination with TKIs: A review. Med. Oncol. 2021;38:10. doi: 10.1007/s12032-021-01462-5. [DOI] [PubMed] [Google Scholar]
- 253.Graney B.A., Lee J.S. Impact of novel antifibrotic therapy on patient outcomes in idiopathic pulmonary fibrosis: Patient selection and perspectives. Patient Relat. Outcome Meas. 2018;9:321–328. doi: 10.2147/PROM.S144425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Chen X., Shi C., Meng X., Zhang K., Li X., Wang C., Xiang Z., Hu K., Han X. Inhibition of Wnt/β-catenin signaling suppresses bleomycin-induced pulmonary fibrosis by attenuating the expression of TGF-β1 and FGF-2. Exp. Mol. Pathol. 2016;101:22–30. doi: 10.1016/j.yexmp.2016.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Cao H., Wang C., Chen X., Hou J., Xiang Z., Shen Y., Han X. Inhibition of Wnt/β-catenin signaling suppresses myofibroblast differentiation of lung resident mesenchymal stem cells and pulmonary fibrosis. Sci. Rep. 2018;8:13644. doi: 10.1038/s41598-018-28968-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Kim Y.S., Cha H., Kim H.J., Cho J.M., Kim H.R. The Anti-Fibrotic Effects of CG-745, an HDAC Inhibitor, in Bleomycin and PHMG-Induced Mouse Models. Molecules. 2019;24:2792. doi: 10.3390/molecules24152792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Mamdani H., Jalal S.I. Histone Deacetylase Inhibition in Non-small Cell Lung Cancer: Hype or Hope? Front. Cell Dev. Biol. 2020;8:582370. doi: 10.3389/fcell.2020.582370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Saracatinib in the Treatment of Idiopathic Pulmonary Fibrosis (STOP-IPF) [(accessed on 1 November 2021)]; Available online: https://clinicaltrials.gov/ct2/show/NCT04598919.
- 259.Bilodeau C., Shojaie S., Goltsis O., Wang J., Luo D., Ackerley C., MRogers I., Cox B., Post M. TP63 basal cells are indispensable during endoderm differentiation into proximal airway cells on acellular lung scaffolds. NPJ Regen. Med. 2021;6:12. doi: 10.1038/s41536-021-00124-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Peljto A.L., Zhang Y., Fingerlin T.E., Ma S.F., Garcia J.G., Richards T.J., Silveira L.J., Lindell K.O., Steele M.P., Loyd J.E., et al. Association between the MUC5B promoter polymorphism and survival in patients with idiopathic pulmonary fibrosis. JAMA. 2013;309:2232–2239. doi: 10.1001/jama.2013.5827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Liu Y., Huang G., Mo B., Wang C. Artesunate ameliorates lung fibrosis via inhibiting the Notch signaling pathway. Exp. Ther. Med. 2017;14:561–566. doi: 10.3892/etm.2017.4573. [DOI] [PMC free article] [PubMed] [Google Scholar]