Abstract
Background and objectives: Ambulatory (outpatient) health care organizations continue to respond to the COVID-19 global pandemic using an array of initiatives to provide a continuity of care for both COVID-19 and non-COVID-19 patients. The purpose of this study is to systematically identify the facilitators and barriers experienced by outpatient health care organizations in an effort to maintain effective and efficient patient throughput during the pandemic. Materials and methods: This study systematically reviewed articles focused on initiatives taken by ambulatory care organizations to maintain optimal outpatient throughput levels while balancing pandemic precautions, published during 2020. Results: Among the 30 articles that met the inclusion criteria, three initiatives healthcare organizations have taken to maintain throughput were identified: the use (and enhanced use) of telehealth, protocol development, and health care provider training. The research team also identified three barriers to patient throughput: lack of telehealth, lack of resources, and overall lack of knowledge. Conclusions: To maintain patient throughput during the COVID-19 pandemic, healthcare organizations need to develop strategies such as the use of virtual consultation and follow-up, new guidelines to move patients along the care delivery value-chain, and ongoing training of providers. Additionally, the availability of required technology for telehealth, availability of resources, and adequate knowledge are vital for continuous patient throughput to ensure continuity of care during a pandemic.
Keywords: ambulatory care, outpatient care, patient throughput, COVID-19, pandemic
1. Introduction
1.1. Rationale
The novel coronavirus disease of 2019 (COVID-19) is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-Cov-2) and was declared a worldwide pandemic by the World Health Organization in March 2020. COVID-19 has severely affected the world and those with pre-existing conditions, with an estimated 230 million confirmed cases and over 4.7 million deaths [1]. As a result, many countries’ healthcare systems have been overwhelmed while treating COVID-19 patients. Furthermore, the operational work and patient-flow of health care delivery has been disrupted by the unprecedented surge of COVID-19 patients. Health care organizations and their providers often delay the provision of care for non-COVID-19 patients to accommodate COVID-19 patients and to help control the spread of the virus within their respective healthcare facilities. This unexpected and rapid spread of the disease has strained healthcare organizations due to the lack of necessary resources to provide adequate care for COVID-19 and non-COVID-19 patients. Such resources include strains on the availability of health care providers, health care infrastructure issues, and even medication and protective personal equipment (PPE) shortages. These factors have contributed to challenges in processing care for both COVID-19 and non-COVID-19 patients and have negatively impacted patient throughput, defined for purposes of this research study as allowing, “…for the efficient flow of patients through the hospital, ensuring timely and appropriate level of care” [2].
Beyond the simple flow of patients through a health care facility, the research team decided to investigate variables affecting the flow of patients (and/or lack thereof) with an additional, broader purpose—to assess and identify potential best practices or inhibitors of care delivery in the ambulatory care setting as compared to a non-pandemic environment of care. This initiative, while focused on throughput, was evaluated by the research team in an attempt to address questions regarding an alignment of practices and procedures to assist outpatient health care organizations work to sustain somewhat ‘normal’ patient continuity of care operations during the pandemic and required public health protocols. These intended observations were analyzed with regard to several facilitator and barrier constructs identified, including organizational reporting of:
Frequency of patients seen
Type of patients seen (example: routine vs. acute, primary care vs. specialty)
Best practices to provide continuity of care during the pandemic and public health initiatives that potentially restrict normal (non-pandemic) clinic operations
The research team focused on these throughput initiatives at this broad level in order to be as inclusive as possible due to the limited research surrounding patient throughput in the ambulatory care setting during the COVID-19 pandemic. Identified facilitators and barriers to outpatient throughput initiatives can further assist ambulatory care clinics in their ongoing challenges to continue patient care in a more efficient manner.
Several systematic reviews on patient throughput/patient flow have been conducted. Some of these reviews looked at the relationships between lean health care and patient flow [3], the impact of scribes on patient throughput [4,5], strategies used to improve patient flow [6,7], the role of computer simulation modeling on patient flow [8], and the impact of triage-related intervention to enhance patient flow [9,10,11].
Granted these prior reviews focused on patient throughput in various healthcare settings, the majority of these reviews were published before the COVID-19 pandemic and those published in 2020 and 2021 did not assess the impact of COVID-19 on patient throughput. To our knowledge, there is a dearth of systematic reviews assessing the strategies adopted by health care organizations to manage disrupted throughput due to the COVID-19 pandemic. Therefore, the purpose this systematic review is to build on extant patient throughput systematic reviews by focusing on strategies adopted to restore disrupted patient flow due to the COVID-19 pandemic, specifically in the ambulatory care setting. Since healthcare organizations are still dealing with the pandemic, despite the invention of COVID-19 vaccines, a systematic review of published articles regarding outpatient healthcare organizations’ strategies to deal with patient flow during this pandemic would be useful to all health care organizations.
1.2. Objectives
The objective of this study is to systematically review the strategies that outpatient healthcare organizations have adopted to mitigate the negative impact of the COVID-19 pandemic on patient throughput and underlying constructs related to patient throughput. Underlying constructs surrounding patient throughput facilitating occurrences/observations (such as continuity of routine care initiatives) and barriers to patient throughput (such as public health physical distancing and isolation measures) are known to exist based upon observations in the healthcare environment. Therefore, identification of best practices and prior organizational experiences for improvement (facilitators and barriers to patient throughput measures) were deemed valuable information as the COVID-19 pandemic continues at a global level.
2. Materials and Methods
2.1. Eligibility Criteria
Articles included in the review had to meet the initial research database search string criteria, therefore focusing specifically on outpatient/ambulatory care healthcare organizations with patient throughput facilitators and barriers experienced during and in response to the COVID-19 global pandemic. Only quality peer-reviewed, academic journals were utilized in the search initiative. Because only a limited (less than 5) articles identified in the initial search reported on patient outcomes, the research team decided that this was not to be a required criterion for the article to be included in the sample. Articles reporting on patient throughput initiatives during COVID-19 were identified using an aggressive publication date search criteria (1 March 2020 to 1 April 2021) to ensure findings were specifically related to organizations’ responses to the COVID-19 pandemic.
2.2. Information Sources
The research team utilized three databases to identify articles in the review: Academic Search Complete, MEDLINE Complete, and Complementary Index. Available via the Elton B. Stephens Company EBSCO library research search website, these three databases were utilized in the study based upon their overall number of results that met the study’s search string and related criteria, while also yielding the fewest number of duplicate articles between databases. All database search efforts were conducted from March 20 through 1 April 2021.
2.3. Search
A search string was developed by the research team that involved multiple iterations to generate the highest initial database results in order to be as inclusive as possible, yet also meet the investigation’s intent. Only non-hospital, outpatient (ambulatory care) healthcare organizations were included in the review. The National Library of Medicine’s Medical Subject Headings (MeSH) controlled thesaurus, used to index research articles for PubMed (MEDLINE), was utilized to identify key words for the query search string for the ambulatory care organization terminology.
‘Patient throughput’ and related terms are not included in the MeSH thesaurus. Therefore, the research team conducted various Google searches to identify terms that yielded the most results for this review variable. This initiative was conducted to specifically identify the most common terms and applicable research studies as identified on the Google.com search engine by the review team. Several internet searches were conducted at the individual level by six of the team members and a collaborative webinar was held to identify the most common terms related to ‘patient throughput’ on the web. These terms were then inserted into the search string on the library’s research database.
Multiple database searches were conducted utilizing various Boolean operators to identify the highest initial review sample. String terms were truncated were necessary in order to be as inclusive as possible for specific string vocabulary. The final search string identified by the researchers was: (“ambulatory care” OR “outpatient care” OR “outpatient service*” OR “urgent care” OR “clinic visit*”) AND (“patient flow” OR “patient throughput” OR “waiting time*” OR “wait time*” OR “overcrowding”) AND (“covid-19” OR “Coronavirus” OR “2019-ncov” OR “Sars-Cov-2” OR “cov-19”). This search string was utilized for all three research databases and information regarding the development of each search term is summarized in Table 1. The combination of search terms and their usage in the search string and database search entry fields was a result of multiple search attempts by the research team to identify the search criteria that yielded the highest number of articles identified.
Table 1.
Development and Use of Search Terms.
| Search Variable | Development Method | Database Usage |
|---|---|---|
| Ambulatory Care | MeSH (exploded) | Subject Terms (SU) |
| Patient Throughput | Google search | All Text (TX) |
| COVID-19 | EBSCO research database popular terms list | Subject Terms (SU) |
Given that our study was limited to COVID-19-related articles, all published COVID-19 articles were published in 2020–2021, therefore conducting additional search using snowballing was not effective because snowballing led to articles published before COVID-19; these articles did not meet our inclusion criteria.
2.4. Initial Study Selection
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guided the review process [12]. Six of the seven study researchers participated in the initial database search. Full text was not utilized as an initial search criteria, therefore allowing the maximum number of initial database results. After initial sample article identification, all articles were located in full-text format by the research team and saved to a MS Teams project site. Articles were numbered accordingly and reviewed by all seven members of the research team. A reference management software program was also utilized for citation and PDF storage of the sample.
During the review process, the research team met multiple times via webinar and telephone in order to identify any/all articles from the initial search that met the study criteria. A MS Excel spreadsheet was generated to collectively record underlying constructs identified by the research team (at the individual level), while also providing individual comments regarding each article’s continued inclusion in the review. In all stages of the review process, the review team experienced no disagreements regarding article inclusion decisions or the underlying themes (constructs) identified.
3. Results
3.1. Study Selection/Exclusion
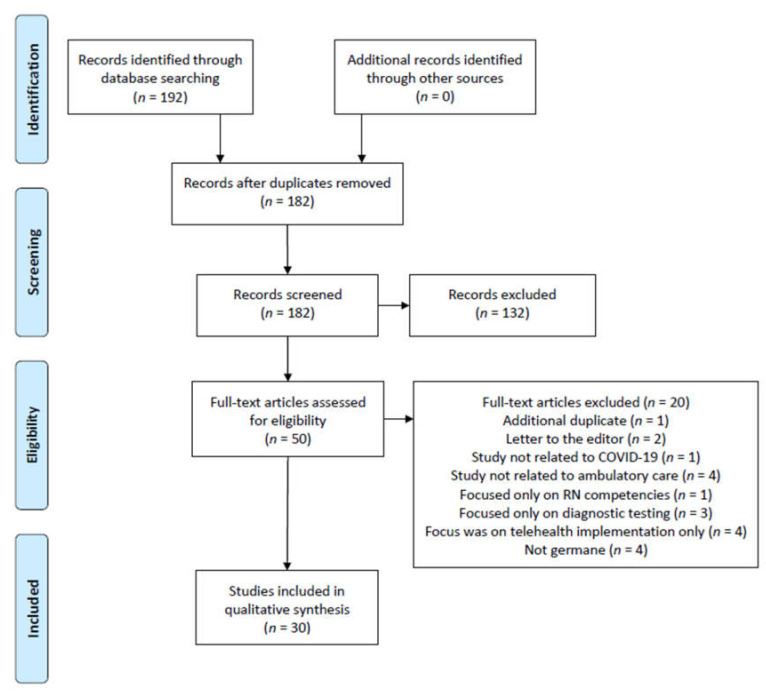
The study selection and follow-on exclusion process is demonstrated in Figure 1. The research team’s initial search resulted in identification of 192 articles from all three research databases. A by-database listing of total search results was not recorded (only total records identified through database searching) and therefore is a limitation of the study. Ten duplicate articles were identified in the initial sample and removed. The subsequent filtering process eliminated 130 articles from the initial research database query, leaving 50 articles remaining.
Figure 1.
Preferred reporting items for systematic reviews and meta-analysis (PRISMA) figure that demonstrates the study selection process.
A full-text review of the remaining 50 articles was conducted by the seven-member research team. This was accomplished by five members of the team reviewing 30 articles each. The two other members of the research team reviewed all 50 articles in the findings to assess for eligibility in the review (Table 2). This review effort ensured that each article was read/analyzed by at least four members of the researcher team (minimum).
Table 2.
Reviewer assignment of the initial database search findings (full article review).
| Article Assignment | Reviewer 1 | Reviewer 2 | Reviewer 3 | Reviewer 4 | Reviewer 5 | Reviewer 6 | Reviewer 7 |
|---|---|---|---|---|---|---|---|
| Articles 1–10 | X | X | X | X | X | X | |
| Articles 11–20 | X | X | X | X | X | X | |
| Articles 21–30 | X | X | X | X | X | ||
| Articles 31–40 | X | X | X | X | |||
| Articles 41–50 | X | X | X | X |
Upon completion of the full-text review process, an additional 20 articles were removed for the following reasons:
an additional duplicate article identified (one article)
letter to the editor (two articles)
the article was not related to COVID-19 throughput analysis (one article)
the article was not focused on ambulatory (outpatient) care (four articles)
the article was a general nursing competency summary (one article)
the article focused solely on diagnostic testing results (three articles)
the article focused specifically on implementation of telehealth resources (four articles)
the article was overall not germane to this review’s research topic (four articles)
Articles removed from the sample for not being focused on ambulatory (outpatient) care focused on overall hospital system(s), hospital emergency department(s), and/or long-term care facilities. Articles eliminated by the research team for the ‘not germane’ reason were completely unrelated to the review’s search criteria yet were somehow identified by the library database search engine. Upon completion of the review, a total of 30 articles were included in the study. Article selection bias was addressed by a series of researcher consensus meetings (via webinar) that focused on each of the 10 articles sets from Table 2. The team experienced no disagreement or difference of opinion in the exclusion of the 20 articles and consensus was established for the remaining articles in the study.
3.2. Study Characteristics
The research team’s thorough review of the 30 articles identified underlying constructs (characteristics) associated with patient throughput initiatives (facilitators and barriers) in ambulatory care organizations during the COVID-19 pandemic. The sample included peer-reviewed research articles from several countries/health systems, and the Johns Hopkins Nursing Evidence-Based Practice study design model’s criteria was used to assess study design [13]. Additionally, facilitators and barriers associated with patient throughput initiatives were identified by the research team and are summarized in Table 3.
Table 3.
Summary of findings (n = 30).
| Author(s) | Participant(s) | JHNEBP Study Design * | Facilitators Leading to an Increase in Patient Throughput in Ambulatory Care Organizations during COVID-19 | Barriers Leading to a Decrease in Patient Throughput in Ambulatory Care Organizations during COVID-19 |
|---|---|---|---|---|
| Akuamoa-Boateng et al. [14] | German University Hospital radiation oncology clinic | 3 |
|
|
| Anderson et al. [15] | Ambulatory care pharmacy preceptors in the U.S. | 3 |
|
|
| Aquilanti et al. [16] | Dental patients in Italy | 3 |
|
|
| Atchley et al. [17] | U.S. nurse practitioner outpatient clinics | 3 |
|
|
| Baughman et al. [18] | Boston post-acute care facilities and surrounding healthcare organizations | 3 |
|
|
| Beattie et al. [19] | Inner Hebrides of Scotland outpatient clinics |
3 |
|
|
| Casiraghi et al. [20] | Spedali Civili Italian hospital trauma department patients | 3 |
|
|
| Darr et al. [21] | NHS tertiary pediatric referral center | 2 |
|
|
| Das [22] | Community-based ambulatory endoscopy center in the U.S. | 3 |
|
|
| De Biase et al. [23] | Tertiary institution neurology clinic (U.S) | 2 |
|
|
| dos Santos et al. [24] | Public university service mastology outpatient clinic in Ceará |
3 |
|
|
| Fu et al. [25] | Lung Cancer patients at a health system clinic in the People’s Republic of China | 2 |
|
|
| George et al. [26] | Singapore community health pain management clinics | 3 |
|
|
| Gharaibeh et al. [27] | International orthopedic clinics | 3 |
|
|
| Hockaday et al. [28] | Federal Medical Station for COVID patients in Dallas, TX, USA | 3 |
|
|
| Janig et al. [29] | Military medical treatment facilities | 3 |
|
|
| Küçük et al. [30] | Health Ministry of Turkey EHR/EMR data from multiple healthcare organizations | 2 |
|
|
| Kyari & Watts [31] | U.S. outpatient eye clinics | 3 |
|
|
| Lou et al. [32] | Orthopedic surgery institution in Shanghai, China | 3 |
|
|
| Lynch et al. [33] | Representatives from adult pain clinics in Canada | 2 |
|
|
| Mason et al. [34] | Radiotherapy patients at the The Christie at Oldham satellite center in the UK | 3 |
|
|
| Mukerji et al. [35] | Otolaryngology clinic at a U.S. community pediatric hospital |
3 |
|
|
| Raidla et al. [36] | Hospital system in Sweden | 2 |
|
|
| Rodler et al. [37] | Patients currently being treated for genitourinary cancers at a single German hospital | 2 |
|
|
| Sacchelli et al. [38] | Psoriasis patients in ambulatory care clinics in Italy | 2 |
|
|
| Segal et al. [39] | Washington state pharmacy service for multiple ambulatory care clinics | 3 |
|
|
| Tam et al. [40] | Cardiac health system in Ontario that has outpatient clinics | 3 |
|
|
| Thorakkattil et al. [41] | Johns Hopkins Aramco Health Care (JHAH) ambulatory care pharmacy services in Saudi Arabia | 2 |
|
|
| Wang et al. [42] | Outpatient fever clinics located at the Union Medical College Hospital (China) | 3 |
|
|
| Waya et al. [43] | African healthcare organizations | 3 |
|
|
* Johns Hopkins Nursing Evidence-Based Practice (JHNEBP) levels of strength of evidence: Level 1, experimental study/randomized control trial (RCT); Level 2, quasi-experimental study; Level 3, non-experimental, qualitative, or meta-synthesis study; Level 4, opinion of nationally recognized experts based on research evidence/consensus panels; Level 5, opinions of industry experts not based on research evidence.
3.3. Risk of Bias
The research team utilized the JHNEBP quality indicator as a tool to assess the quality of each article (strength of evidence) in the sample. This review did not include any level I (experimental study/randomized control trial) articles, which has also been the experience in prior reviews by members of the research team involved in ambulatory/outpatient care organizations [44,45]. This review included nine articles (30%) classified as level II (quasi-experimental) studies and 21 articles (70%) classified as level III (non-experimental, qualitative, or meta-synthesis) studies. A common observation across many sample articles in the review demonstrates outpatient healthcare organizational leaders describing their experiences and convenience samples in attempt to disseminate information regarding best practices and protocols related to patient throughput initiatives. There were no articles identified in the study classified with JHNEBP levels IV or V.
3.4. Additional Analysis
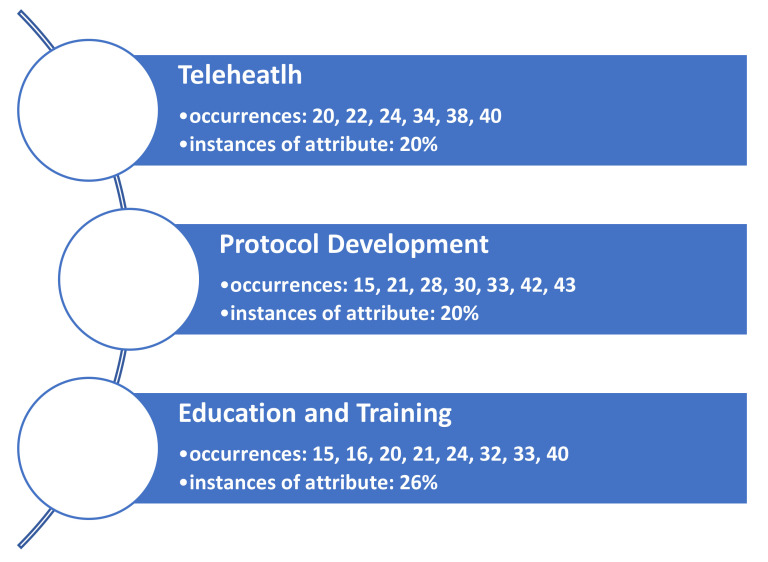
Results of the research team’s consensus meetings demonstrate three facilitator themes identified in the literature to support the adoption of telehealth resources for the ambulatory care segment of the industry during the pandemic (Figure 2).
Figure 2.
Identified themes (constructs) identified as facilitators leading to an increase in patient throughput in ambulatory care organizations during COVID-19.
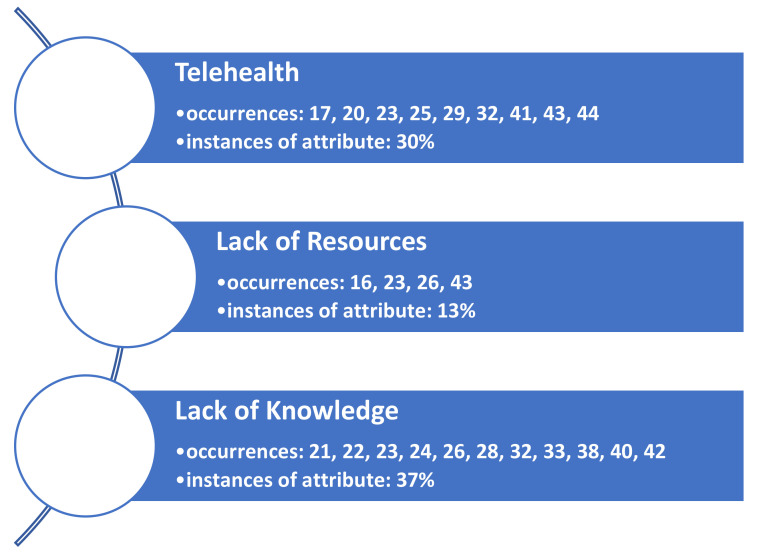
Additionally, three barrier themes were also identified. These are listed in Figure 3. Findings are not mutually exclusive only to a facilitator or a barrier theme, as several articles demonstrated both constructs upon review.
Figure 3.
Themes (constructs) identified as barriers leading to a decrease in patient throughput in ambulatory care organizations during COVID-19.
4. Discussion
4.1. Summary of Evidence
An ongoing initiative to maintain a high level of quality ambulatory/outpatient care continues to challenge the U.S. healthcare system as the COVID-19 pandemic continues. Evidence from this review suggests that enhanced safety and patient distancing protocols [20,27,41], in conjunction with appropriate provider training centered around such public health initiatives [19,23,31]. enhance outpatient providers’ ability to increase patient throughput. Contrary, a lack of both resources [22,25,42] and provider and staff knowledge surrounding updated patient flow protocols [15,22,25] serve as barriers to an enhanced throughput initiative. The review findings also suggest the implementation of additional telehealth initiatives [21,23,33], while also attributing this same identified construct as a barrier to the throughput initiative [19,22,42].
4.2. Facilitator to Patient Throughput: Telehealth
The COVID-19 pandemic came with an impact on healthcare resources, services, and budget. The biggest challenge was to evaluate how to minimize the risk of disease exposure and at the same time provide the required medical services. The idea of keeping these patients out of the clinics and hospitals in their healthy state is helping in many ways. Today’s advanced technology is assisting the healthcare industry in the process of managing patients at home. Telemedicine with emails, chat services, text messages, and video-assisted calls between patients and healthcare professionals are helpful in the early diagnosis followed by guidance if there is a need for emergency services.
Implementation of Coronavirus Preparedness and Response Supplemental Appropriations Act allowed pharmacists and other credentialed healthcare providers to offer patient care services via telehealth [39]. This was a collective effort from all the specialized clinics, such as the Uro-Oncology and Neurosurgery Clinics, to develop protocols, staff training, and education and implementation of their knowledge of telehealth regarding patients’ complaints and symptoms [33,37]. A very similar positive effect was seen in a neurosurgery clinic for preoperative and postoperative follow up visits via telehealth during the pandemic [23]. Patients have started to accept telemedicine, which offers safe and effective therapies.
4.3. Facilitator to Patient Throughput: Protocol Development
In reviewing the literature, one of the common facilitators identified was the use and development of protocols to help in patient throughput during the COVID 19 pandemic. These protocols ranged from patient check-in to deciding who is appropriate for a needed surgical procedure. The goal of these articles is to make sure patients are cared for safely and resources are used appropriately during the COVID 19 pandemic.
One major reason for protocol development was to ensure that surgical resources are allocated to the correct patient population. Seen in patients in need of orthopedic surgery during the pandemic, protocols were developed to make sure that only necessary emergency surgery were done while others were managed medically until a strain on hospital resources was reduced [27,32]. Another type of protocol that was developed during this time were safety protocols to ensure patients and staff remained safe from the COVID 19 virus. With the implementation of safety protocols for in-person visits, it was found that patients were more likely to stay on treatment regimens with the extra layer of protection these protocols provided [14,27,34,41]. Lastly a protocol theme was identified surrounding how to evaluate staffing levels to ensure that areas in high need of staff were assisted by areas with a lighter workload. Triaging staff was needed to help maintain quality care for patients and for the staff to be able to safely care for an increased patient care load [20,29,41,42]. Overall, there was a positive experience in the development of protocols during the COVID 19 pandemic.
4.4. Facilitator to Patient Throughput: Education and Training
Another common facilitator presented in the literature regarding optimizing throughput of patients in the ambulatory care during the pandemic includes education and training components. This applies to both the staff taking care of the patients, along with the patients receiving care. With the ever-changing guidelines presented by the public health authorities and other international agencies, patients need to be educated on the most up-to-date information to keep themselves and their loved one’s safe while being treated in the ambulatory setting [31].
For healthcare staff taking care of patients in the ambulatory setting, education and training pertained to learning new protocols and guidelines, providing education to patients, learning new technology platforms, and conducting research. At times, each day brought new requirements, warranting the creation of new protocols, methods and learning modules for safe patient care [14,15,20,32,39]. For those ambulatory settings conducting care virtually, new technology tools were implemented, requiring training of staff on how to use the new tools, such as Zoom and Microsoft Teams [15,23].
4.5. Barrier to Patient Throughput: Telehealth
The U.S. healthcare system was already progressing towards telehealth services intending to provide convenience and comfort for both healthcare providers and patients. The COVID-19 pandemic has helped the healthcare industry in expediting the evolvement of teleservices for medical services and medical education. A transition from physical visits to medical offices and clinics to using telemedicine services was not very smooth in several articles identified in the study. For example, in dermatology patients, about 75% were willing to adapt telehealth for their appointments. However, 25% of patients were still not ready to make the switch. This could be related to patient satisfaction when physicians see patient’s skin ailments and touch their wounds, or it could be the feeling of not getting sufficient attention from healthcare providers because they are not seeing their patients in person [34].
4.6. Barrier to Patient Throughput: Lack of Resources
Lack of resources are seen across the healthcare trajectory during the pandemic. There was a concern that patients would possibly be unable to access needed medications to treat medical conditions. Pharmacies lacked resources, patients were not coming in to fill or refill needed medications and there was a fear of medical conditions going untreated [15]. As hospitals were becoming overwhelmed with COVID-19 cases, surgical cases, except for emergency needs, were almost eliminated for a time period. This led to orthopedic ambulatory clinics having to become creative in how they care for their patient population.
Another example of lack of surgical resources was presented by a pediatric urology clinic. A lack of open surgical space and equipment in the hospital led the clinic’s leaders to rethink the way they triaged the patients for surgery. Patients who would experience a life altering effect from not having surgery were offered surgery, but patients who could be treated medically were moved further down on the surgical list [22]. Yet, as the pandemic continues and ambulatory clinics are starting to look towards to a return to somewhat normal operations, there are several concerns surrounding a lack of resources and this particular challenge. Having the proper protocols, guidelines, PPE, and staff resources will have to be considered when looking to return to normal operations [22].
4.7. Barrier to Patient Throughput: Lack of Knowledge
As healthcare faced an unprecedented worldwide pandemic, one of the biggest challenges faced was the lack of knowledge of the virus and the effects thereof. Lack of knowledge of protocols and workflow as to how to proceed with orthopedic surgical cases, due to the unprecedented burden brought by the current pandemic, halted surgical cases in healthcare facilities and outpatient clinics. More comprehensive guidelines for the orthopedic surgeon in the era of COVID-19 were needed to maintain a safe and effective practice to resume surgical cases [27].
As the challenge to care for patients in the outpatient setting continued, more data was gathered and safety guidelines and protocols were created, but healthcare providers would find out when implemented that they may not meet the needs of patients. For instance, one radiation oncology clinic surveyed their lung cancer population to see what effect the pandemic was having on their treatment schedules [25]. This provided a method to obtain patients’ point of view on how the pandemic has changed their perceived access to treatment. It was identified that there was an increase of wait times for treatments and an increase of fear of contracting the virus, which held them from seeking such treatment [25]. One of the greatest unknowns of the pandemic for the ambulatory space was the simple fact of seeing patients safely and being cognizant of the resources available for treatment [31,37,39]. This lack of knowledge of telemedicine prior to COVID-19 led to an overwhelmed healthcare industry unable to keep up with demand for outpatient, elective services, pharmacy services, neurosurgery, pediatric otolaryngology, cancer patients, and pain treatment patients [21,23,25,33]. Although much of this was remedied using telemedicine and virtual clinics, there was a large learning curve, and it was unknown at the time if these clinics would offer the same quality as an in-person visit.
The findings from this systematic review are not directly comparable with prior systematic reviews on patient throughput given our special focus on COVID-19, which has dramatically disrupted patient throughput. Since COVID-19 is the major cause of disruption, throughput strategies such as the use of telemedicine, protocol development, education and training were especially implemented to address that disruption. Therefore, these strategies and related characteristics were not found in prior systematic reviews focused specifically on patient throughput. Pre-COVID-19 strategies to improve throughput that were found in systematic reviews consisted of the use of medical scribes [4,5], the use of lean management and process improvement [2,3,6], the use of triage liaison [10], and the role of nurses [11]. Additional studies focused on the establishment of access centers, call centers, patient placement centers, ED clinical laboratory, ED self-registration kiosks, ED result waiting area, physician-assisted triage, patient flow automation, and rapid admissions units [2,7], the use of hospital staff to undertake responsibility for ED admissions [2], and admissions screening for MRSA [2]. Lastly, the expansion of nursing roles such as clinical initiative nurses and nurse practitioners and fast tracking the care of clinically stable patients are identified as constructs prior to the COVID-19 pandemic that also support initiatives to accommodate patient throughput [7].
5. Conclusions
Across the globe, patient care processes and related public health disease precautions have changed to adapt to the ongoing COVID-19 pandemic. This systematic review identified facilitators and barriers related to patient throughput initiatives in ambulatory care (outpatient) organizations. Identified constructs from this study support ongoing patient care initiatives and offer insight into additional, future efforts towards the continuity of outpatient care during the pandemic.
Telemedicine, identified as both a facilitator and barrier to patient throughput in the outpatient setting, demonstrates how increased access to medical providers for consultations and related care efforts can be improved, while high-touch, in-person care processes are lacking. Further facilitating of outpatient organization throughput concerned planning and strategic implementation of protocol development processes/procedures and related education and training initiatives as adaptive initiatives. Patient throughput barriers (in addition to telemedicine) regarding organizational needs (PPE, clinic space for physical distancing, and medical staff) and overall lack of knowledge surrounding patient care processes related to throughput initiatives were also identified. Ambulatory care providers can benefit from these patient throughput facilitators and barriers as the global pandemic continues. Future research surrounding these identified constructs include specific outpatient industry segment care lines (specialty care) and associated patient outcomes within and between care processes.
As with most systematic reviews, this study has some limitations. First, given that we reviewed published studies on COVID-19 patients throughput, and since most COVID-19 studies were published in 2020–2021, conducting additional article search using a snowballing method was not effective since snowballing leads to articles published before 2020 before the COVID-19 pandemic. Second, we did not record the number of original articles by database since by-database listing of original findings is an optional step in the PRISMA guideline.
Acknowledgments
The research team would like to acknowledge the support of Clemens Scott Kruse in his provision of resources and guidance regarding the PRISMA systematic review process.
Author Contributions
All authors contributed to this review in accordance with ICMJE standards. Conceptualization, C.L., Z.R., J.C., J.D., K.G., E.H. and A.K.; methodology, C.L.; software, C.L.; validation, C.L., Z.R., J.C., J.D., K.G., E.H. and A.K.; formal analysis, C.L., Z.R., J.C., J.D., K.G., E.H. and A.K.; investigation, C.L., Z.R., J.C., J.D., K.G., E.H. and A.K; resources, C.L., Z.R., J.C., J.D., K.G., E.H. and A.K; data curation, C.L., Z.R., J.C., J.D., K.G., E.H. and A.K; writing—original draft preparation, C.L., Z.R., J.C., J.D., K.G., E.H. and A.K.; writing—review and editing, C.L. and Z.R.; visualization, C.L. and Z.R.; supervision, C.L.; project administration, C.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization WHO Coronavirus (COVID-19) Dashboard. [(accessed on 15 July 2021)]. Available online: https://covid19.who.int/
- 2.Walker C., Kappus K., Hall N. Strategies for Improving Patient Throughput in an Acute Care Setting Resulting in Improved Outcomes: A Systematic Review. Nurs. Econ. 2016;34:277–288. [PubMed] [Google Scholar]
- 3.Tlapa D., Zepeda-Lugo C.A., Tortorella G.L., Baez-Lopez Y.A., Limon-Romero J., Alvarado-Iniesta A., Rodriguez-Borbon M.I. Effects of Lean Healthcare on Patient Flow: A Systematic Review. Value Health. 2020;23:260–273. doi: 10.1016/j.jval.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 4.Heaton H.A., Castaneda-Guarderas A., Trotter E.R., Erwin P.J., Bellolio M.F. Effect of scribes on patient throughput, revenue, and patient and provider satisfaction: A systematic review and meta-analysis. Am. J. Emerg. Med. 2016;34:2018–2028. doi: 10.1016/j.ajem.2016.07.056. [DOI] [PubMed] [Google Scholar]
- 5.Gottlieb M., Palter J., Westrick J., Peksa G.D. Effect of Medical Scribes on Throughput, Revenue, and Patient and Provider Satisfaction: A Systematic Review and Meta-analysis. Ann. Emerg. Med. 2021;77:180–189. doi: 10.1016/j.annemergmed.2020.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gualandi R., Masella C., Tartaglini D. Improving hospital patient flow: A systematic review. Bus. Process. Manag. J. 2020;26:1541–1575. doi: 10.1108/BPMJ-10-2017-0265. [DOI] [Google Scholar]
- 7.Elder E., Johnston A., Crilly J. Review article: Systematic review of three key strategies designed to improve patient flow through the emergency department. Emerg. Med. Australas. 2015;27:394–404. doi: 10.1111/1742-6723.12446. [DOI] [PubMed] [Google Scholar]
- 8.Sobolev B., Sanchez V., Vasilakis C. Systematic Review of the Use of Computer Simulation Modeling of Patient Flow in Surgical Care. J. Med Syst. 2011;35:1–16. doi: 10.1007/s10916-009-9336-z. [DOI] [PubMed] [Google Scholar]
- 9.Oredsson S., Jonsson H., Rognes J., Lind L., Göransson K.E., Ehrenberg A., Asplund K., Castrén M., Farrohknia N. A systematic review of triage-related interventions to improve patient flow in emergency departments. Scand. J. Trauma Resusc. Emerg. Med. 2011;19:43. doi: 10.1186/1757-7241-19-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benabbas R., Shah R., Zonnoor B., Mehta N., Sinert R. Impact of triage liaison provider on emergency department throughput: A systematic review and meta-analysis. Am. J. Emerg. Med. 2020;38:1662–1670. doi: 10.1016/j.ajem.2020.04.068. [DOI] [PubMed] [Google Scholar]
- 11.Sharma S., Rafferty A.M., Boiko O. The role and contribution of nurses to patient flow management in acute hospitals: A systematic review of mixed methods studies. Int. J. Nurs. Stud. 2020;110:103709. doi: 10.1016/j.ijnurstu.2020.103709. [DOI] [PubMed] [Google Scholar]
- 12.Moher D., Liberati A., Tetzlaff J., Altman D.G., The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johns Hopkins Medicine Johns Hopkins Evidence-Based Practice Model. [(accessed on 26 September 2021)]. Available online: https://www.hopkinsmedicine.org/evidence-based-practice/ijhn_2017_ebp.html.
- 14.Akuamoa-Boateng D., Wegen S., Ferdinandus J., Marksteder R., Baues C., Marnitz S. Managing patient flows in radiation oncology during the COVID-19 pandemic: Reworking existing treatment designs to prevent infections at a German hot spot area University Hospital. Strahlenther. Und Onkol. 2020;196:1080–1085. doi: 10.1007/s00066-020-01698-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anderson S.L., Bianco J., DeRemer C.E. Adapting ambulatory care learning environments in response to the COVID-19 pandemic. Am. J. Health-Syst. Pharm. 2021;78:467–471. doi: 10.1093/ajhp/zxab016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aquilanti L., Gallegati S., Temperini V., Ferrante L., Skrami E., Procaccini M., Rappelli G. Italian Response to Coronavirus Pandemic in Dental Care Access: The DeCADE Study. Int. J. Environ. Res. Public Health. 2020;17:6977. doi: 10.3390/ijerph17196977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Atchley M.D., Kroll N.P., Etcher L. Reducing the wait: When time is priceless. Nurse Pract. 2021;46:50–55. doi: 10.1097/01.NPR.0000731576.93905.48. [DOI] [PubMed] [Google Scholar]
- 18.Baughman A.W., Hirschberg R.E., Lucas L.J., Suarez E.D., Stockmann D., Hutton Johnson S., Hutter M.M., Murphy D.J., Marsh R.H., Thompson R.W., et al. Pandemic Care Through Collaboration: Lessons From a COVID-19 Field Hospital. J. Am. Med Dir. Assoc. 2020;21:1563–1567. doi: 10.1016/j.jamda.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beattie M., Morrison C., MacGilleEathain R., Gray N., Anderson J. Near Me at Home: Codesigning the use of video consultations for outpatient appointments in patients’ homes. BMJ Open Qual. 2020;9:e001035. doi: 10.1136/bmjoq-2020-001035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Casiraghi A., Domenicucci M., Cattaneo S., Maggini E., Albertini F., Avanzini S., Pansi Marini M., Galante C., Guizzi P., Milano G. Operational strategies of a trauma hub in early coronavirus disease 2019 pandemic. Int. Orthop. 2020;44:1511–1518. doi: 10.1007/s00264-020-04635-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Darr A., Senior A., Argyriou K., Limbrick J., Nie H., Kantczak A., Stephenson K., Parmar A., Grainger J. The impact of the coronavirus (COVID-19) pandemic on elective paediatric otolaryngology outpatient services—An analysis of virtual outpatient clinics in a tertiary referral centre using the modified paediatric otolaryngology telemedicine satisfaction survey (POTSS) Int. J. Pediatric Otorhinolaryngol. 2020;138:110383. doi: 10.1016/j.ijporl.2020.110383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Das A. Impact of the COVID-19 pandemic on the workflow of an ambulatory endoscopy center: An assessment by discrete event simulation. Gastrointest. Endosc. 2020;92:914–924. doi: 10.1016/j.gie.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.De Biase G., Freeman W.D., Bydon M., Smith N., Jerreld D., Pascual J., Casler J., Hasse C., Quiñones-Hinojosa A., Abode-Iyamah K. Telemedicine Utilization in Neurosurgery During the COVID-19 Pandemic: A Glimpse Into the Future? Mayo Clinic Proceedings. Innov. Qual. Outcomes. 2020;4:736–744. doi: 10.1016/j.mayocpiqo.2020.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dos Santos C.P.R.S., Fernandes A.F.C., Silva D.M.D., Castro R.C.M.B. Restructuring service at a mastology outpatient clinic during the COVID-19 pandemic. Rev. Bras. Enferm. 2021;74((Suppl. 1)):1–4. doi: 10.1590/0034-7167-2020-0571. [DOI] [PubMed] [Google Scholar]
- 25.Fu R., Wu L., Zhang C., Chu Q., Hu J., Lin G., Yang L., Li J.-S., Yang X.-N., Yang J.-J., et al. Real-World Scenario of Patients With Lung Cancer Amid the Coronavirus Disease 2019 Pandemic in the People’s Republic of China. JTO Clin. Res. Rep. 2020;1:100053. doi: 10.1016/j.jtocrr.2020.100053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.George J.M., Xu Y., Nursa’adah B.J., Lim S.F., Low L.L., Chan D.X.H. Collaboration between a tertiary pain centre and community teams during the pandemic. Br. J. Community Nurs. 2020;25:480–488. doi: 10.12968/bjcn.2020.25.10.480. [DOI] [PubMed] [Google Scholar]
- 27.Gharaibeh M.A., Al Mohammad B., Gharaibeh B., Khasawneh L., Al-Naser S. Guidelines for the orthopedic surgeon in the era of COVID-19. Orthop. Rev. 2020;12:191–195. doi: 10.4081/or.2020.8833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hockaday S., Krause K., Sobieski C., Li J.N., Hurst R., Ryan B., Leader M., Smith D., Fowler R., Tran A., et al. Protocols for Personal Protective Equipment in a COVID-19 Medical Shelter. Disaster Med. Public Health Prep. 2020;14:551–557. doi: 10.1017/dmp.2020.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jänig C., Forklage R., Gurney J.M., Groth R., Wirth C., van de Krol H., Schmidbauer W., Güsgen C. Triage Decisions in the Context of COVID-19: Old Burden, New Challenge-The Structured Approach for Intensive Care Unit Triage (SAINT) Protocol. Mil. Med. 2021;186:e300–e304. doi: 10.1093/milmed/usaa287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Küçük A., Demirci M., Kerman G., Soner Özsoy V. Evaluating of hospital appointment systems in Turkey: Challenges and opportunities. Health Policy Technol. 2021;10:69–74. doi: 10.1016/j.hlpt.2020.11.008. [DOI] [Google Scholar]
- 31.Kyari F., Watts E. How to adapt your eye service in the time of COVID-19. Community Eye Health J. 2020;33:14. [PMC free article] [PubMed] [Google Scholar]
- 32.Lou T., Ren Z., Sun Z., Wang W., Fan C. Full recovery of elective orthopedic surgery in the age of COVID-19: An 8-month retrospective cohort study. J. Orthop. Surg. Res. 2021;16:154. doi: 10.1186/s13018-021-02286-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lynch M.E., Williamson O.D., Banfield J.C. COVID-19 impact and response by Canadian pain clinics: A national survey of adult pain clinics. Can. J. Pain. 2020;4:204–209. doi: 10.1080/24740527.2020.1783218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mason T., Bennett R., White A., Rembielak A. Changing radiotherapy review practice in response to COVID-19 in a radiotherapy satellite centre. J. Radiother. Pract. 2020;19:312–314. doi: 10.1017/S1460396920000527. [DOI] [Google Scholar]
- 35.Mukerji S.S., Liu Y.-C., Musso M.F. Pediatric otolaryngology workflow changes in a community hospital setting to decrease exposure to novel coronavirus. Int. J. Pediatric Otorhinolaryngol. 2020;136:110169. doi: 10.1016/j.ijporl.2020.110169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Raidla A., Darro K., Carlson T., Khorram-Manesh A., Berlin J., Carlström E. Outcomes of Establishing an Urgent Care Centre in the Same Location as an Emergency Department. Sustainability. 2020;12:8190. doi: 10.3390/su12198190. [DOI] [Google Scholar]
- 37.Rodler S., Apfelbeck M., Stief C., Heinemann V., Casuscelli J. Lessons from the coronavirus disease 2019 pandemic: Will virtual patient management reshape uro-oncology in Germany? Eur. J. Cancer. 2020;132:136–140. doi: 10.1016/j.ejca.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sacchelli L., Evangelista V., Di Altobrando A., Lacava R., Rucci P., Rosa S., Patrizi A., Bardazzi F. How infodemic during the COVID-19 outbreak influenced common clinical practice in an Outpatient Service of Severe Psoriasis. Dermatol. Ther. 2020;33:e14065. doi: 10.1111/dth.14065. [DOI] [PubMed] [Google Scholar]
- 39.Segal E.M., Alwan L., Pitney C., Taketa C., Indorf A., Held L., Lee K.S., Son M., Chi M., Diamantides E., et al. Establishing clinical pharmacist telehealth services during the COVID-19 pandemic. Am. J. Health-Syst. Pharm. 2020;77:1403–1408. doi: 10.1093/ajhp/zxaa184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tam D.Y., Naimark D., Natarajan M.K., Woodward G., Oakes G., Rahal M., Barrett K., Khan Y.A., Ximenes R., Mac S., et al. The Use of Decision Modelling to Inform Timely Policy Decisions on Cardiac Resource Capacity During the COVID-19 Pandemic. Can. J. Cardiol. 2020;36:1308–1312. doi: 10.1016/j.cjca.2020.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Thorakkattil S.A., Nemr H.S., Al-Ghamdi F.H., Jabbour R.J., Al-Qaaneh A.M. Structural and operational redesigning of patient-centered ambulatory care pharmacy services and its effectiveness during the COVID-19 pandemic. Res. Soc. Adm. Pharm. 2021;17:1838–1844. doi: 10.1016/j.sapharm.2020.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang J., Zong L., Zhang J., Sun H., Harold Walline J., Sun P., Xu S., Li Y., Wang C., Liu J., et al. Identifying the effects of an upgraded “fever clinic” on COVID-19 control and the workload of emergency department: Retrospective study in a tertiary hospital in China. BMJ Open. 2020;10:e039177. doi: 10.1136/bmjopen-2020-039177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Waya J.L.L., Ameh D., Mogga J.L.K., Wamala J.F., Olu O.O. COVID-19 case management strategies: What are the options for Africa? Infect. Dis. Poverty. 2021;10:30. doi: 10.1186/s40249-021-00795-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lieneck C., Weaver E., Maryon T. Pandemic Pause: Systematic Review of Cost Variables for Ambulatory Care Organizations Participating in Accountable Care Organizations. Healthcare. 2021;9:198. doi: 10.3390/healthcare9020198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lieneck C., Weaver E., Maryon T. Outpatient Telehealth Implementation in the United States during the COVID-19 Global Pan-demic: A Systematic Review. Medicina. 2021;57:462. doi: 10.3390/medicina57050462. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.