Abstract
In recent years, the role of nanotechnology in drug delivery has become increasingly important, and this field of research holds many potential benefits for cancer treatment, particularly, in achieving cancer cell targeting and reducing the side effects of anticancer drugs. Biocompatible and biodegradable properties have been essential for using a novel material as a carrier molecule in drug delivery applications. Biocompatible nanocarriers are easy to synthesize, and their surface chemistry often enables them to load different types of photosensitizers (PS) to use targeted photodynamic therapy (PDT) for cancer treatment. This review article explores recent studies on the use of different biocompatible nanocarriers, their potential applications in PDT, including PS-loaded biocompatible nanocarriers, and the effective targeting therapy of PS-loaded biocompatible nanocarriers in PDT for cancer treatment. Furthermore, the review briefly recaps the global clinical trials of PDT and its applications in cancer treatment.
Keywords: photodynamic therapy, biocompatible, cancer, nanocarriers, photosensitizers
1. Introduction
Cancer is caused by the uncontrollable and abnormal proliferation of cells in the body, and is the leading cause of death worldwide [1]. Radiation and chemical carcinogens have been identified as significant causes of cancer that damage DNA and induce mutations in the cells, and different types of cancers have been identified [2]. Most types of cancer are highly resistant to conventional chemotherapy and radiotherapy, which is known for its elevated multidrug resistance and low rate of patient survival [3]. According to the World Health Organization, it is estimated that there were nearly 10 million cancer deaths in 2020, and the most common causes of cancer death in 2020 were lung, colon and rectum, liver, stomach, and breast cancer [4]. Identifying novel therapy for the successful treatment of cancer is a significant problem across the world. Chemotherapy is widely used as a conventional cancer therapy: the primary function of this therapy is to destroy cancer cells, but it often kills both cancer and normal cells [5]. Chemotherapy is often associated with severe side effects to the patient’s health, and some of the normal cells (blood-forming cells in the bone marrow, hair follicles, and cells in the mouth, digestive tract, and reproductive system) are the most likely to be damaged [6]. Hence, developing a targeted therapy approach is the best way to destroy cancer cells instead of normal cells.
In the past few decades, nanotechnology has received substantial attention amongst scientists to understand tumor-targeted nanoparticle-mediated drug delivery for cancer therapy [7]. Biocompatible nanocarriers can be successfully used as a carrier molecule for various biomedical applications, including drug delivery [8], phototherapy [9] biosensing [10], bioimaging [11], diagnosis [12], cancer therapy [13], and hyperthermia [14]. The development and employment of biocompatible nanocarriers provide various functional applications in the treatment of cancer, such as a controlled delivery of drugs, being non-immunogenic, a long shelf life, more excellent stability, efficient drug loading, functionalization of targeting ligands, and intracellular drug release into targeted cells. Biocompatible nanocarriers exhibit good cytocompatibility and hemocompatibility, are friendly to physiological conditions, they should be non-toxic when entering the body, and they contact tissues and cells directly [15,16,17]. The toxic nanoparticles are often called non-biocompatible materials. Various factors are associated with the toxic effects of nanoparticles, such as nanoparticle concentration, interaction time with living matter, stability in biological fluids, and accumulation capacity in tissues and organs. The complete understanding of the factors mentioned above and their positive outcomes help develop a safe and biocompatible nanoparticle for drug delivery applications [18]. Biocompatible nanocarriers-based photosensitizer (PS) delivery has become a promising platform for PDT, and it offers many benefits owing to its unique physicochemical properties [19].
Furthermore, nanoparticle-based delivery enables passive drug targeting by utilizing the enhanced permeability and retention effect (EPR effect) in cancerous tissues [20]. The potential role of functionalized nanomaterials in cancer photodynamic therapy (PDT) and their effective targeting efficiency have been extensively studied [21,22,23]. Photodynamic therapy is an emerging, minimally invasive therapeutic strategy for the management of a variety of cancers. Photodynamic therapy involves three principal components: PS; visible light; and oxygen—the activated PS helps the formation of ROS, and initiates the cytotoxic effects in the target cells or tissues [24]. Photodynamic therapy has been investigated for more than 25 years as an unconventional treatment for cancer [25]. The first PS introduced by Dougherty et al. (1975) was a water-soluble mixture of porphyrins named “haematoporphyrin derivatives” (HpD), and the modern term, “photofrin”. Several light-absorbing and light-activating compounds are used as PS in PDT, and it has shown significant outcomes in cancer treatment [26]. The photochemical and photophysical properties of PS-loaded biocompatible nanocarriers play a vital role in the cancer cell death mechanism. Briefly, the PS is activated and excited at a specific wavelength to induce cell death through the production of reactive oxygen species (ROS) [27,28]
In this review article, we explore the use of biocompatible nanocarriers-based PS delivered in PDT for cancer treatment. Thus, this review article is divided into six different sections. Section 1 briefly explains the introduction to the study. Section 2 studied the use of different biocompatible nanocarriers and their potential applications in PDT. In Section 3, PS-loaded with biocompatible nanocarriers in PDT for cancer are discussed in detail. Section 4 describes the effective targeting approach of PS-loaded biocompatible nanocarriers in PDT for cancer, and some of the global clinical trials of PDT in cancer treatment are given in Section 5. In Section 6, future perspectives of this work are briefly discussed.
2. The Potential Application of Biocompatible Nanocarriers in PDT
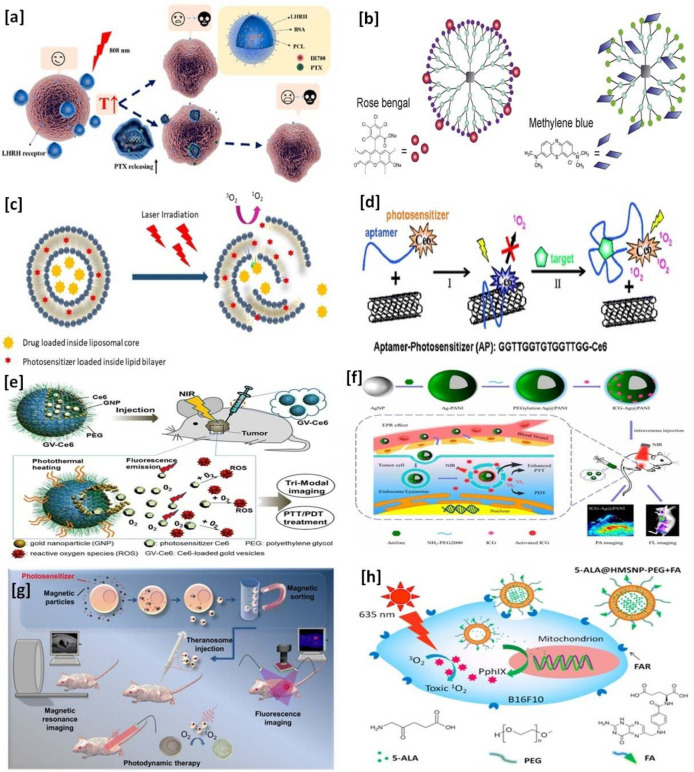
The functional role of biocompatible nanocarriers and their applications in PDT are widely reported for cancer treatment. There are different types of biocompatible nanocarriers studied in cancer PDT—some are polymer-based nanocarriers [29], dendrimers [30], liposomes [31], carbon-based nanoparticles [32], gold nanoparticles [33], silver nanoparticles [34], magnetic nanoparticles [35], and mesoporous silica nanoparticles [36]. Schematic illustrations of PS-loaded nanocarriers in PDT for the treatment of cancer are given in Figure 1.
Figure 1.
Schematic illustration of photosensitizers-loaded nanocarriers in PDT for the treatment of cancer: (a) polymeric nanoparticles—reprinted with permission from reference [84], Copyright 2020, American Chemical Society; (b) dendrimers—reprinted with permission from reference [85], Copyright 2015, Elsevier; (c) liposomes—reprinted with permission from reference [86], Copyright 2019, Elsevier; (d) carbon-based nanoparticles—reprinted with permission from reference [87], Copyright 2008, American Chemical Society; (e) gold nanoparticles—reprinted with permission from reference [70], Copyright 2013, American Chemical Society; (f) silver nanoparticles–reprinted with permission from reference [88], Copyright 2016, American Chemical Society; (g) magnetic nanoparticles—reprinted with permission from reference [89], Copyright 2013, American Chemical Society; and (h) mesoporous silica nanoparticles—reprinted with permission from reference [90], Copyright 2015, American Chemical Society.
2.1. Polymer-Based Nanocarriers
The polymer-based nanocarriers are more often considered as carrier molecules for various drug delivery applications, including PDT. Polymer-based nanocarriers can alter their surface chemistry to functionalize the specific targeting moieties (ligands or antibodies), which helps to facilitate site-specific or targeted drug delivery to the site of action [37,38]. Li et al. (2021) recently reported the use of biocompatible nanocomplex for cancer therapy—the synthesized 5,10,15,20-tetrakis (4-aminophenyl) porphyrin (TAPP) and Fe3+-loaded PEGylated polygalacturonic acid nanocomplex increased the 1O2 upon 760 nm laser irradiation, and exhibited cytotoxic effects in B16 melanoma cells [39]. Chlorin e6-loaded poly (dopamine) nanospheres showed enhanced PDT/PTT effects in tumor cells upon 670 nm and 808 nm laser irradiation. In 670 nm laser irradiation, the poly (dopamine) conjugated chlorin e6 exhibited higher PDT efficacy, cellular update, and ROS production in tumor cells compared to free chlorin e6. It was also observed that the synthesized nanospheres showed an excellent PTT effect upon 808 nm laser irradiation. The combination of 670 and 808 nm irradiation confirmed the low dark toxicity with excellent phototoxicity effects of the nanospheres in both in vitro and in vivo studies [40]. Zinc Phthalocyanine(ZnPc)-loaded carboxymethyl chitosan/ionic liquid imidazolium-based nanoparticles in an in vitro release study confirmed the sustained release of ZnPc. The synthesized nanoparticles showed great ability to generate singlet oxygen, and it is appropriate to facilitate the high PDT activity to diseased cells [41]. Light-responsive polymers have attracted considerable attention in PDT, and are designed to load and release the encapsulated drugs inside the cells. An external light triggers the light-responsive polymers to release the drugs in both in vitro and in vivo systems by inducing the local heating, leading to thermal degradation of the matrix [42]. Different light parameters, such as wavelength, power, and pulse length, play an essential role in the triggering process, and the optimized parameters may induce disruption on the chemical structures (breaks covalent bonds) of polymers [43]. Schoppa et al. (2021) recently synthesized the light-responsive polymeric nanoparticles using the emulsion diffusion method with an average hydrodynamic diameter of 200 nm, and the negative zeta potential shows excellent colloidal stability. The light-responsive property and nanoparticle degradation study showed that the reduction of the molar mass of the polymer was confirmed by size exclusion chromatography upon light irradiation. The light-depending drug release property was evaluated using the PS 5,10,15,20-tetrakis (m-hydroxyphenyl) chlorine (mTHPC), and it confirmed the improved intracellular uptake of mTHPC in the colon cancer cell line (HT-29 cells) [44].
2.2. Dendrimers
Dendrimers are three-dimensional, branched macromolecules with a low polydispersity index, and they have shown numerous advantages as carrier molecules in drug delivery due to their physicochemical and biological properties. The three-dimensional structure consists of an initial core with repeated branching and terminal groups connected to the units of repeated branching, and this dendron-like structure ensures good stability, easy surface modifications, and biocompatibility for different drug delivery applications [45,46,47]. The structural morphology of dendrimers offered more inner space to load drug molecules/PS, and it facilitated passive targeting to the cells [48]. Dendrimers can be successfully used as a stabilizer for metal-based nanoparticles, and it shows numerous advantages in PTT by enhancing the high photothermal conversion efficiency of the nanoparticle upon irradiation [49]. Rose bengal is successfully loaded on cationic phosphorous dendrimer complex, and it showed enhanced production of singlet oxygen molecules in the aqueous medium than free rose bengal [50]. Zhou et al. (2018) synthesized water-soluble monodisperse dendritic carriers by incorporating 5-Aminolevulinic acid (ALA) and iron-chelating agents. The lowest concentration of 2 µM showed efficient phototoxicity in human epithelial carcinoma cells (KB cells), and the synergistic effects of iron chelating agents and ALA efficiently increased the intracellular accumulation of protoporphyrin IX [51]. Kojima et al. (2007) synthesized PS-loaded poly (ethylene glycol) (PEG), attached poly (amidoamine), PAMAM dendrimer, and PEG attached poly (propylene imine) (PPI) dendrimers for PDT applications. The inner hydrophobicity of PS-loaded PEG-PPI dendrimers showed enhanced stability compared to PEG-PAMAM dendrimers. An in vitro study revealed that the protoporphyrin IX(PpIX)-loaded PEG-PPI showed a better cytotoxic effect than free PpIX upon light irradiation [52].
2.3. Liposomes
Liposomes are biocompatible and biodegradable colloidal vesicles, and this characteristic feature makes this material more flexible to use as a carrier molecule in drug delivery applications [53]. Liposomal formulations can accommodate PS with variable physicochemical properties, substantially protect PS safety, and improve their PDT efficacy [54]. These conventional liposomes have limitations, especially the plasma half-life and difficulty loading and delivering the drug to the targeted area. Surface-modified liposomes have often overcome those limitations, and they ensure the safety and delivery of loaded drugs to the targeted tumor site [31]. An in vivo Meth-A sarcoma-bearing mice study showed that the pegylated liposomes enhanced the accumulation of benzoporphyrin-based PS in tumor tissues. The targeting delivery of surface-modified pegylated liposomes strongly suppressed the tumor growth, and then, the pegylated liposomes upon laser irradiation. The surface-modified pegylated liposomes also show a four-fold higher delivery of benzoporphyrin-based PS than the non-modified liposomes [55] Yang et al. (2019) synthesized aggregation-induced emission PS entrapped liposomes for PDT applications. The study results confirmed that the liposomes act as the most suitable carrier for PS delivery, and greatly improved the tumor-targeting behavior of liposomes [56]. The physicochemical characteristics of liposomes, such as thermodynamic phase and self-assembling properties, allow them to load and have a site-specific delivery of both hydrophilic and lipophilic drugs [57]. Feuser et al. (2021) successfully achieved the co-encapsulation of sodium diethyldithiocarbamate (DETC) and zinc phthalocyanine (ZnPc) in liposomes above 85% through the reverse-phase evaporation method. The synthesized liposomes showed a 308 nm diameter mean size with a highly stable zeta potential of −36 mV. The cytotoxic effects of co-encapsulation were studied against mouse embryo fibroblast (NIH3T3) cells, and it showed decreased cellular effects compared to free DETC+ZnPc. Enhanced phototoxic effects of the co-encapsulated liposomes were observed against human breast cancer cells (MDA-MB231) [58]. Lee et al. (2019) confirmed that the chitosan-coated liposomes protected the stability and skin permeation of indocyanine green better than uncoated liposomes. An in vitro B16-F10 melanoma cells study demonstrated that the chitosan-coated liposomes enhanced indocyanine’s cellular uptake and photocytotoxicity effects upon 775 nm laser irradiation at a power of 250 mW for 2.5 min [59]. The liposomal formulation plays a significant role, and it helps to use a lesser concentration of PS for PDT applications. Miretti et al. (2020) synthesized dipalmitoylphosphatidylcholine cholesterol liposomes, and successfully loaded different PS (Zinc Phthalocyanines and its derivatives, Zn(II)tetraminephthalocyanine), and the PDT efficiency of PS-loaded liposomes were studied using a glioblastoma cell line (T98G cells). The results showed that the liposomal formulations with 0.05 µM concentration of PS achieved similar cellular effects to that of the 0.5 µM concentration [60].
2.4. Carbon-Based Nanoparticles
The promising chemodynamic therapy (CDT), PDT, photothermal therapy (PTT) effects of Fe-N codoped carbon nanoparticles were investigated in both in vitro and in vivo models. The photothermal effects of synthesized nanoparticles were studied by irradiating with an 808 nm (1.5 W/cm2) laser, and it showed excellent photothermal conversion efficiency (around 29.15%), enhanced OH production, and H2O2 enhanced ROS generation in in vitro. Further, the synergistic CDT/PDT/PTT effects of nanoparticles were confirmed using 4T1 tumor-bearing Balb/c mice as an in vivo model. A 21-day mice study demonstrated that the synthesized nanoparticles can control the tumor growth, and it was observed that the tumor weight was reduced approximately 53 times smaller than the PBS (-) group. The treatment approaches also ensure the low biotoxicity of nanoparticles in in vivo, and there were no noticeable weight changes and histopathological damages in all the studied groups [61]. Zheng et al. (2016) synthesized protoporphyrin-loaded and Arg-Gly-Asp (RGD) targeting motif coated carbon nitride-based multifunctional nanocomposite for enhanced PDT. It was confirmed that the synthesized nanocomposites accumulated in the tumor tissues through active RGD targeting and the passive EPR effect. Then, the nanocomposite started splitting water to generate O2, and the PS generated singlet oxygen (1O2) from the produced O2 upon 630 nm laser irradiation. An in vivo biodistribution study revealed that the targeting specificity of synthesized nanocomposite and the nanocomposite accumulation was explicitly observed in the tumor region. It was confirmed through the confocal laser scanning microscope study, by observing a strong fluorescence signal in the tumor region, and a similar signal was absent in metabolic organs, such as the lung, liver, and kidney [62]. Chan et al. (2016) synthesized noncytotoxic graphitic carbon nitride quantum dots (g-C3N4 QDs) using a solid-phase hydrothermal method as a potential PS for cancer treatment. The synthesized g-C3N4 QDs exhibit limited tissue permeability upon ultraviolet light radiation, while also having excellent cytotoxic properties. The modified form of g-C3N4 QDs nanocomposite using NaYF4:Yb/Tm and poly(L-lysine) produces ROS by entering into the cells, is responsible for the damage of mitochondrial function, and is associated with the induction of apoptosis in an oral epidermoid carcinoma cell line (OEC-M1) [63].
2.5. Gold Nanoparticles
The unique optical property and the biocompatibility of gold nanoparticles received considerable attention for cancer PDT treatments [64]. Gold nanoparticles require either covalent or non-covalent attachment approaches to deliver the therapeutic molecules in drug delivery, targeting, and imaging applications [65]. Photosensitizer-loaded gold nanoparticles can be successfully used to deliver to the tumor site via active or passive accumulation [66]. Cheng et al. (2011) performed an in vivo animal experiment to study PEGylated gold nanoparticles’ drug release mechanism and pharmacokinetics. The intravenous administration of gold nanoparticles showed an efficient PDT drug release and penetration into the tumor site without producing any adverse effects of the synthesized molecules. An in vivo fluorescence imaging study confirmed the fast drug excretion from the body by renal clearance and the hepatobiliary system [67]. Dutta et al. (2019) synthesized cationic PS methylene blue(MB)-loaded gold nanocluster embedded mucin nanoparticles by the facile green synthesis method for an imaging-guided PDT application. The synthesized nanoparticles showed an average size of 139 ± 47 nm, and the size of the gold cluster revealed an average size of 1.9 ± 0.34 nm inside the mucin nanoparticles. The synthesized nanoparticles show a sustained release pattern, with a higher MB release in acidic pH 4.5, and a lesser release in pH 7.4 (24 h), and it directly indicates the beneficial release behavior of synthesized nanoparticles in the tumor microenvironment. The cell viability study revealed the biocompatibility nature of nanoparticles against HeLa cells (human cervical carcinoma) and HEK 293T (human embryonic kidney) cells. The luminescent property of synthesized nanoparticles aids in understanding the bioimaging of PS inside the cells, and it can be successfully used for bioimaging guided cancer PDT [68]. The combined cancer PDT and PTT effects of covalently immobilized porphyrin-loaded crosslinked polyphosphazene nanospheres based on gold nanoparticles were studied by Wei et al. (2018). The synthesized nanoparticles showed low cytotoxicity against HeLa cells in the dark, and showed significant cytotoxicity upon laser irradiation with 808 nm (PTT) and 630 nm (PDT) [69]. Chlorin e6(Ce6)-loaded gold vesicles showed strong absorption in the range of 650–800 nm, and it ensures the enhanced cellular update and localization of Ce6 in human breast cancer cells (MDA-MB-435). The in vitro cell viability of laser irradiated gold vesicles, Ce6, and synthesized Ce6-loaded gold vesicles were analyzed by MTT assay. The results indicate that the cytotoxic effects of Ce6-loaded gold vesicles show a higher percentage (45–70%) than cells treated with gold vesicles (5%) and Ce6 (10%). An in vivo study performed using tumor-bearing mice shows the higher therapeutic effect of Ce6-loaded gold vesicles than gold vesicles and Ce6. An in vitro and in vivo study suggested that the synthesized Ce6-loaded gold vesicles may be suitable for image-guided synergistic PTT/PDT cancer treatment [70].
2.6. Silver Nanoparticles
Silver nanoparticles are broadly studied for their various biomedical applications, including drug delivery, PDT, antimicrobial activity, and cellular imaging. Silver nanoparticles were irradiated using a 635 nm diode laser, and it showed decreased cell viability, proliferation, and induced apoptosis (programmed cell death) in breast cancer cells (MCF-7) and lung cancer cells (A549). Although cell death was caused in both cell lines, the AgNPs exhibited enhanced cytotoxic effects in the MCF-7 compared to A549 cells [71]. This indicates that different types of cancer cells respond differently to the same NPs, and thus, studies on various cancer cell types need to be examined. Mahajan et al. (2019) synthesized porphyrin-loaded mercaptosuccinic acid capped silver nanoparticles for PDT and cell imaging applications. The average size distribution of synthesized nanoparticles shows 110 nm with excellent zeta potential (−31.1 mV), and the scanning electron microscopy study shows the uneven cube synthesized nanoparticles were studied against A375 malignant melanoma cancer cells. It shows non-toxic behavior up to the concentration of 5 µM, with excellent fluorescence imaging properties [72]. Natesan et al. (2017) synthesized hypocrellin B and nanosilver-loaded poly lactide-co-glycolide-based nanoparticles by a nanoprecipitation method for enhanced production of singlet oxygen (1O2), and it showed the time-dependent phototoxicity against A549 (human adeno lung carcinoma) cells upon irradiation [73]. Curcumin and silver nanoparticles-loaded chitosan and chondroitin sulfate-based hydrogels were synthesized by Fabiano de Freitas et al. (2020), and it was further modified with ionic liquids to enhance the solubility properties of chitosan. The cytotoxic and phototoxic behaviors of synthesized nanoparticles were analyzed using fibroblast cell lines (CCL1.3). The cytotoxic results exhibited >80% cell viability for the studied highest concentrations (1000 µg mL−1), and the phototoxicity assay showed cell death at ~60% at the highest concentrations. There was no cell death in the absence of the loaded molecules (curcumin and silver nanoparticles) [74].
2.7. Magnetic Nanoparticles
Magnetic nanoparticle-based carriers have been extensively studied for their applications in biomedicine, such as drug delivery, drug targeting, cell isolation and sorting, magnetic resonance imaging, and cancer PDT [75]. Iron oxide-based materials are considered an excellent choice to use as magnetic nanoparticles due to their already proven biocompatibility and superparamagnetic behavior [76]. Protoporphyrin IX PS-loaded multifunctional magnetic nanoparticles were synthesized using triphenylphosphine (TPP)-grafted dextran to enhance the magnetic imaging-guided PDT effect in tumor cells. The average particle size distribution of synthesized nanoparticles was found in the range of 76.91 ± 5.33 nm, with corresponding polydispersity indices of 0.223, and negatively charged zeta potential (−5.73 ± 0.65 mV). The cellular uptake and photoinduced internalization of synthesized nanoparticles were studied in 4T1 cells (mouse breast tumor cells), and it confirmed the enhanced effect compared to control, and, further, the mitochondrial damage was confirmed using a fluorescence microscopy study. An in vivo study, performed using 4T1 tumor-bearing Balb/c mice, indicates the antitumor effect upon laser irradiation [77]. Cinteza et al. (2006) synthesized the 2-[1-hexyloxyethyl]-2-devinyl pyropheophorbide-a (HPPH) PS-loaded diacyllipid micelle-based magnetic Fe3O4 nanoparticles. The synthesized nanoparticle shows excellent stability and physicochemical properties for magnetic guided PDT drug delivery and light-activated PDT. It also exhibits an enhanced in vitro cellular uptake and phototoxicity against HeLa cells [78]. Di Corato et al. (2015) synthesized dually-loaded hybrid liposomes for PDT and magnetic hyperthermia applications. They successfully loaded iron oxide nanoparticles and PS (m-Tetrahydroxyphenylchlorin (m-THPC)) within the aqueous core and lipid bilayer, respectively, by a one-pot synthesis method. An in vitro antitumoral efficacy of synthesized nanoparticles was performed using human adenocarcinoma SKOV-3 cells, and it created tumor cell death when each treatment was performed alone, and the combined treatment revealed the destruction of cells in vitro. Similarly, an in vivo study was conducted using six-week-old female NMRI nude mice, and the synthesized nanoparticles were capable of inhibiting tumor growth when each treatment was performed alone, and the combined treatment revealed the complete eradication of the tumor [79]. Superstable magnetic nanoparticles were used in conjugation with indocyanine green (IR820), a near-infrared organic dye used as a PS for PDT applications. The synthesized PS-loaded nanoparticles exhibit excellent stability in water, and an enhanced PDT efficiency was observed compared to free IR820, and it showed improved cellular uptake and fluorescence intensity of the cells [80].
2.8. Mesoporous Silica Nanoparticles
Biocompatible and biodegradable mesoporous silica-based nanoparticles have been extensively studied in drug delivery applications owing to their physicochemical properties, such as tunable size, large surface area, biosafety, and surface modification flexibility. The tunable size and large surface area properties facilitate the load of one or more drug molecules, and the surface modification flexibility helps control the drug release behavior precisely [81]. Doxorubicin and rose-bengal-loaded hollow mesoporous silica nanoparticles (HMSNs) are successfully used in chemo-photodynamic combination therapy. The drug entrapment efficiency was 76.67% for doxorubicin, and 95.85% for rose bengal, and an in vitro drug release study indicated the pH-responsive drug release from HMSNs. The synthesized HMSNs show negligible drug release in pH 7.4 due to their tightly capped surface, and offer an improved and sustained drug release behavior in acidic pH (6.0 and 5.0). The synthesized nanoparticle shows excellent physicochemical properties, and the Fourier transform infrared spectroscopy study results confirmed the coating of hyaluronic acid on the surface of HMSNs. An in vitro cellular uptake study was performed using a confocal laser scanning microscopic technique to confirm the targeting ability of hyaluronic acid-coated HMSNs against murine mammary carcinoma (4T1 cells), which are considered CD44 receptor overexpressed cells, and hyaluronic acid has a high affinity on CD44 receptor [82]. Han et al. recently synthesized the ferrocene modified multifunctional mesoporous silica nanoparticles, and successfully loaded indocyanine green PS for synergistic CDT/PDT/PTT applications. An in vitro cellular study was performed using HeLa cells to determine the cell killing rate, and it was observed that 93% of cells were killed using the synergistic CDT/PDT/PTT approach. The loaded indocyanine green facilitates the generation of hyperpyrexia upon near-infrared light irradiation, and aims to kill the cancer cells using PTT. Ferrocene modification helps initiate an intracellular Fenton reaction, and kills the cells through CDT and generated singlet oxygen. Indocyanine green kills the cancer cells by PDT [83].
3. Biocompatible Nanocarriers for Photosensitizers in PDT
The design and exploration of various PS-loaded biocompatible nanocarriers in PDT have shown minimized toxicity in cancer therapy [91]. There are several PS compounds loaded with biocompatible nanocarriers studied in PDT and listed in Table 1.
Table 1.
Different types of photosensitizers-loaded biocompatible nanocarriers in PDT for cancer.
| Biocompatible Nanocarriers | Preparation Method | Size (nm) | Photosensitizers | Outcomes |
|---|---|---|---|---|
| Albumin nanoparticles | Solvent diffusion method | 100 to 200 nm | Hematoporphyrin | The synthesized hematoporphyrin-loaded albumin nanoparticle accumulation was increased in murine lung tumor cells compared to normal lungs cells [92]. |
| Polymeric micelles (Pluronic P123 and F127 mixture) | Solvent evaporation method | 12.5 to 16.6 nm | Photofrin II® | PDT irradiation on PS loaded polymeric micelles showed an increased cytotoxic effect in the human cancer cell model [93]. |
| TmPyP-loaded PLGA nanoparticles | Evaporation method | Between 118 ± 5 and 133 ± 2 nm | 5,10,15,20-tetrakis(1-methylpyridinium-4-yl)-porphyrin tetra-iodide (TMPyP) | The formulation showed positive outcomes in laser irradiation and skin permeability studies, and it can be successfully used for topical diseases, such as melanoma [94]. |
| Chitosan nanoparticles | Ionic crosslinking method | 254.3 ± 9.42 nm | ALA | The synthesized nanoparticle shows a spherical shape, good dispersion, and stability. The PDT effect of ALA-loaded nanoparticles was studied against WSU-HN6 and CAL-27 cells—the elevated mitochondrial ROS production was observed in both cells [95]. |
| Thermoresponsive solid lipid nanoparticles | High-performance hot homogenization and ultrasonication method | from ~20 nm up to 700 nm | Temoporfin | Temoporfin-loaded solid lipid nanoparticle formulation was tested in 4T1 (murine mammary carcinoma) and MDA-MB-231 (human breast adenocarcinoma) cells. It showed faster accumulation in the cells, and induced increased phototoxicity against tumor cells [96]. |
| Poly(d,l-lactide-co-glycolide) nanoparticles | Salting-out technique | Two types 167 and 370 nm in diameter | Verteporfin | The synthesized biocompatible polymeric nanoparticle was tested against EMT-6 mammary tumor cells, and the smaller size of the nanoparticle showed very good photocytotoxicity compared to large nanoparticles. Similarly, the small nanoparticles effectively controlled the tumor growth in an in vivo mice study [97]. |
| Hyaluronic acid-based carbon nanotubes | π-π interactions | 203 ± 6.6 nm | Chlorin e6 | The synthesized single-walled carbon nanotubes confirmed the enhanced PDT effect of chlorin e6 against CACO-2 cells compared to free chlorin e6 [98]. |
| Core-shell polymeric nanoparticles | Microemulsion polymerization method | ~170 and 220 nm | HPPH | The synthesized nanoparticles help to prevent the fluorescence quenching in water. It helps to achieve fluorescence imaging-guided PDT [99]. |
| Lipid polymer hybrid nanoparticles | Self-assembly | 170 ± 20 nm | Zinc phthalocyanine | The synthesized lipid polymer hybrid nanoparticles improved the stability, cellular uptake, sustained release, and fluorescence properties of Zinc Phthalocyanine. The synthesized nanoparticle was tested both in vitro and in vivo. In vitro cytotoxic study shows increased cell death against MCF-7 cells, and an increased PDT antitumor effect in an in vivo study (Sprague Dawley rats) [100]. |
| Pluronic-based nanocomposite | Thin-film hydration method. | 121.8 nm | Methylene blue | The synthesized nanocomposite shows synergistic effects (PDT/PTT) against the human cervical cancer cell line (SiHa). Cell death occurred by following the cell apoptosis pathway, and it can effectively treat cancer via noninvasive phototherapy [101]. |
| Multifunctional mesoporous silica nanoparticle | Sol-gel method | 200 nm | Indocyanine green | The combined chemodynamic/PTT/PDT therapy shows that an increased inhibition rate of HeLa cells compared to the treatment given by chemodynamic therapy alone or dual PTT/PDT [83]. |
| Rose bengal-loaded nanostructured poly-amidoamine dendrimers | Michael addition method followed by encapsulation | 20 nm | Rose bengal | The controlled release property of Rose bengal-loaded dendrimer formulation was confirmed by the in vitro drug release study. The nanostructured formulation produced remarkable photocytotoxicity properties against DLA cells (Dalton’s Lymphoma Ascite) [102]. |
| BODIPY with mPEG-based phototheranostic nanoparticle | Freeze-drying method | 282 nm | BODIPY | The synthesized Mitomycin C-graphene BODIPY-mPEG nanoparticle possessed excellent properties for applying tumor tissue imaging-guided photo chemo synergistic therapy [103]. |
| Pluronic®-based nanoparticles | Solid dispersion method | NA | Hypericin | The synthesized micelles showed high stability and selective internalization in MCF-7 cells. The accumulated micelles were observed in mitochondria and endoplasmic reticulum, and it showed effective phototoxic cell death [104]. |
| Hypocrellin and nanosilver-loaded PLGA-TPGS copolymeric nanoparticles | Ring-opening and bulk polymerization method | 89.59 to 566.8 nm | Hypocrellin | An enhanced phototoxic effect was observed in A549 cells (human adeno lung carcinoma) irradiated by 590 nm using a mercury vapor lamp [105]. |
| Pectin-coated silver nanoparticles | Heated and stirring method | 2.3 ± 0.7 nm and 9 ± 6 nm. | Riboflavin | The synthesized pectin-based nanoparticle increases the biocompatibility of silver nanoparticles, and the loaded riboflavin emission enhanced singlet oxygen production compared to the control. Cytotoxicity study shows the increased photodamage effect when nanoparticles and riboflavin are present in the sample [106]. |
| Albumin-based nanoparticle | Self-assembly method | 36 nm | Curcumin | Enhanced antitumor activity was observed in HeLa cells through PDT. The curcumin derivative-loaded nanoparticle induced cell cycle arrest and apoptosis in HeLa cells [107]. |
4. Biocompatible Nano Carrier-Based Targeted Therapy in PDT
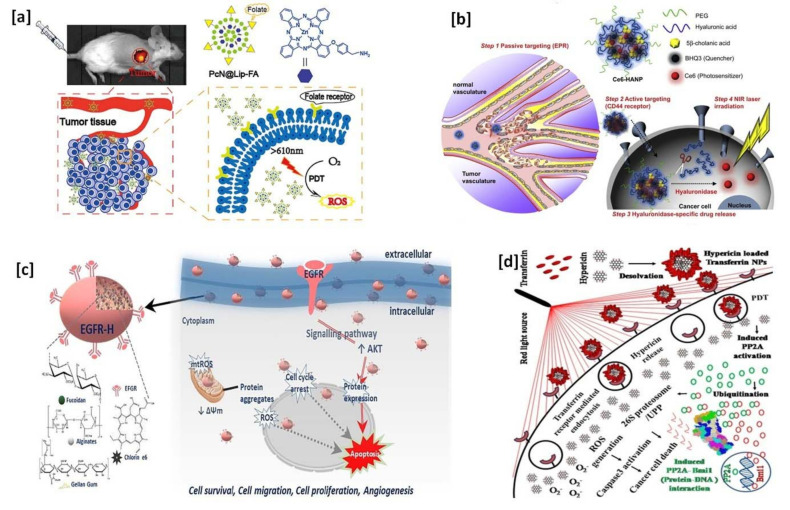
Many types of cancerous cells overexpress some specific receptors on the cell surface—some of them are the folate receptor, CD 44 receptor, avβ3 integrin receptor, EGFR receptor, transferrin receptor, and epithelial cell adhesion molecules (EpCAM), also known as the CD326 receptor. The targeting ligand-modified biocompatible nano carrier-based approaches can target the site of action in PDT cancer therapy. Biocompatible nano carrier-based targeted therapy enhances the PDT effects by targeting such receptors using specific ligands. The detail of PS-loaded and targeting ligand modified nanocarriers and their great targeting potential in cancer treatments are discussed in Table 2. A schematic illustration of PS-loaded cancer cell targeting efficiency of biocompatible nanocarriers in PDT are given in Figure 2.
Table 2.
Cancer targeting efficiency of biocompatible nanocarriers in PDT.
| Name of the Nanocarriers/Targeting Ligand/Photosensitizers/Drug Used | Target | Cancer Treatment (In Vitro/In Vivo) | Outcomes | Reference |
|---|---|---|---|---|
| Folic acid-functionalized and Poly-lactic acid (PLA) coated, Indocyanine green loaded colloidal gold nanobipyramid | Folate receptor | Murine melanoma B16-F10 cell line (in vitro) | The synthesized nanocarriers targeted the overexpressed folate receptor on the membrane of B16-F10 cells, which also showed improved photothermal and photodynamic activity when irradiated with both 785 and 808 nm lasers. | [108] |
| Iridium (III) nano-PS self-assembled with hyaluronic acid (HA) | CD 44 receptor | Mouse metastatic breast cancer cells (4T1.2) (in vitro) | Nano-PS treated cells were irradiated by 532 nm light. The CD 44 receptor targeting efficiency of HA-coated nanoparticles showed excellent cellular uptake and mitochondria accumulation abilities, and it significantly improved the phototoxicity in 4T1.2 cells. | [109] |
| Protoporphyrin IX-loaded hyaluronic acid-based polymeric micelles | CD 44 receptor | CD44 overexpressing A549 cells (in vitro) | It is observed that the synthesized micelles showed an increased cellular uptake and enhanced phototoxic activity in CD44, overexpressing A549 cells in both 2D and 3D cultures. | [110] |
| Arg-Gly-Asp (RGD) peptide-functionalized chlorin e6 (Ce6) loaded PEGylated mesoporous silica nanoparticles | avβ3 integrin | The human glioma cell line of U87 MG cells (in vitro) | Confocal laser scanning microscopy study confirmed the cellular targeting efficiency and cellular internalization of RGD functionalized nanoparticles in U87 MG cells. 660 nm laser irradiation on RGD functionalized nanoparticles resulted in improved cellular toxicity than free Ce6. | [111] |
| Curcumin-loaded Poly (D, l-lactic-co-glycolic acid) (PLGA) nanoparticles (NPs) conjugated to the anti-EGFRvIII monoclonal antibody | EGFR receptor | DKMG/EGFRvIII cells (EGFRvIII overexpressed human glioblastoma cell line) (in vitro) | Antibody conjugated PLGA NPs were incubated with cells for 1 h and irradiated with 460 nm blue LED light at a dose of 60 J/cm2. Cellular uptake percentage was significantly higher in EGFRvIII overexpress cells than DK-MGlow cells (low expressed EGFRvIII human glioblastoma cell line). | [112] |
| Transferrin and aptamer conjugated [Ru(bpy)2(tip)]2+ (RBT)-loaded mesoporous ruthenium nanoparticles | Transferrin (TfR) and nucleolin expressing gliomas | U87 cells glioma cells, 293T cells and brain capillary endothelial (HBMEC) cells (in vitro), and BALB/c nude mice (in vivo) | Aptamer AS1411 and transferrin have a high binding affinity with nucleolin and transferrin receptors, respectively. Antitumor drug, RBT, has a high-efficiency PS when irradiated with 808 nm. The study suggested that the dual functionalized RBT-loaded MRN overcomes the blood-brain barrier (c), and actively targets gliomas. | [113] |
| Antibodies conjugated, rose bengal (RB) PS-loaded upconversion nanoparticles with a silica layer | Epithelial cell adhesion molecules (EpCAM), also known as CD326 | Human colorectal adenocarcinoma HT-29 cells (in vitro) | 980 nm irradiation was used to activate RB molecules. Fluorescence imaging study revealed that the synthesized antibody conjugated nanomaterials had a high affinity, with EpCAM overexpressed in HT-29 cells, and negligible in EpCAM negative murine microglia cells (BV2 cell line). | [114] |
Figure 2.
Schematic illustration of photosensitizers loaded cancer cell targeting efficiency of biocompatible nanocarriers in PDT: (a) folate receptor targeting—reprinted with permission from reference [115], Copyright 2020, Elsevier; (b) CD 44 receptor targeting—reprinted with permission from reference [116], Copyright 2012, Elsevier; (c) EGFR receptor targeting—reprinted with permission from reference [117], Copyright 2020, Elsevier; and (d) transferrin receptor targeting—reprinted with permission from reference [118], Copyright 2020, American Chemical Society.
5. Clinical Application of PDT in Cancer Treatment
Photodynamic therapy-based cancer treatment shows several advantages, such as reduced toxicity and invasiveness, short treatment time, and being inexpensive compared to classical cancer therapies [119,120]. Biocompatible nanocarriers and several PSs are well studied in global clinical trials, and it has shown positive effects in cancer PDT. Some of the significant global clinical trial statuses, and details of the PS and PDT parameters, are given in Table 3.
Table 3.
Details of the photosensitizer and PDT parameters used in some of the global clinical trials of PDT in cancer treatment.
| ClinicalTrials.Gov Identifier | Condition or Disease | Photosensitizer | PDT | Phase | Recruitment Status |
|---|---|---|---|---|---|
| NCT03638622 | Oral cancer | Total 60 mg/kg of Aminolevulinic acid (5-ALA) administered orally via three repeated doses (20 mg/kg at 0, 1, and 2 h) |
LED light sources are used in a wavelength of 405 nm. The total fluence of 100 J/cm2 at the lesion surface in 30–45 min | 1 and 2 | Completed [121] |
| NCT00675233 | Head and neck cancer | HPPH (2-1[Hexyloxyethyl]-2-devinylpyropheophorbide-a) | 665 nm | 1 | Completed [122] |
| NCT01682746 | Recurrent pediatric brain tumors | Photofrin (Porfimer sodium) administered via intravenous (IV) route, 24 h before surgery and PDT | 630 nm photo illumination with a total energy of 240 J/cm2 | 1 | Completed [123] |
| NCT00984243 | Lung cancer | 2mm/Kg dose of Photofrin II administered via IV, 40–50 before PDT | 620–630 nm, and a total energy of 200–300 J/cm2 (Argon-dye laser) and 100–200 J/cm2 (Excimer-dye laser) |
NA | Completed [124] |
| NCT00322699 | Bladder cancer | 1.5 mg/kg of Photofrin (Porfimer sodium) administered via IV, 2 days before PDT | 630 nm with light doses of 1200 J (±100 J) | 1 and 2 | Completed [125] |
| NCT00002975 | Skin cancer | Aminolevulinic acid | 633 nm laser irradiation | 2 | Completed [126] |
| NCT00862901 | Breast cancer Skin cancer |
Photofrin (0.8 mg/kg body weight) administered via single IV injection 36–48 h before continuous low-irradiance photodynamic therapy (CLIPT) procedure | 630 nm red spectrum Diomed laser in four different experimental conditions (fluence 100, 200, 400 and 800 J/cm2 over 24 h) through a fiber optic patch | 1 | Completed [127] |
| NCT01800838 | Lymphoma | Topically applied Silicon phthalocyanine 4 | Visible light at a wavelength of 675 nm | 1 | Completed [128] |
| NCT01140178 | Oral cavity carcinoma | HPPH | 665 nm light with escalating laser doses from 100 J/cm2 to 125 and 140 J/cm2 | 1 | Completed [129] |
| NCT02872064 | Breast cancer | Single IV dose of Verteporfin (0.4 mg/kg), 60–90 min before PDT | 690 nm red laser light. A light dose from 20 to 90 J/cm of light diffuser length | NA | Completed [130] |
| NCT01875393 | Prostate cancer | Lyophilized formulation of TOOKAD® (4 mg/kg) | 753 nm with the fixed energy of 200 J/cm | 3 | Completed [131] |
| NCT03012009 | Non-melanoma skin cancer | Methyl aminolevulinate | 630 nm, 37 J/cm2 | NA | Completed [132] |
| NCT02662504 | Malignant Pleural Mesothelioma | Photofrin (2 mg/kg) | 630 nm | 2 | Completed [133] |
| NCT01682811 | Benign Dermal Neurofibromas | 5-ALA | 630 nm | 1 | Completed [134] |
| NCT04429139 | Retinoblastoma | Verteporfin (6 mg/m2) administered via IV route | 689 nm (200 s to generate 120 J/cm2) | NA | Completed [135] |
| NCT00868088 | Squamous Cell Carcinoma | Topically applied ALA | 405–420 nm at a dose of 1000 s | 4 | Completed [136] |
6. Future Perspectives and Conclusions
In this review article, we discussed the potential benefits of biocompatible nanocarriers and their enhanced cancer PDT applications. Different types of biocompatible nanocarriers are extensively studied in cancer PDT applications, and are well documented in the literature—some of them are polymer-based nanocarriers, dendrimers, liposomes, carbon-based nanoparticles, gold nanoparticles, silver nanoparticles, magnetic nanoparticles, and mesoporous silica nanoparticles. A comprehensive literature study revealed that the advancement of using biocompatible nanocarriers and their cancer PDT applications had shown numerous positive outcomes in both in vitro and in vivo studies. We strongly believe that the discussed biocompatible nanocarriers have shown numerous advantages for cancer PDT applications. Some of them include: targeted PS delivery to the site of action, ensuring the long-term stability of PS; enhanced loading efficiency; and the sustained release of PS. The successful preparation of biocompatible nanocarriers significantly avoids the limitations associated with chemo drugs and PS. We expect the use of photosensitizers loaded with biocompatible-based nanocarriers will be broader in the future, as well as more significant outcomes in clinical trials for cancer PDT applications.
Abbreviations
| µM | Micromolar |
| 1O2 | Singlet oxygen |
| 2D | Two-dimension |
| 3D | Three-dimension |
| 4T1 | Murine mammary carcinoma cells |
| 4T1 cells | Mouse breast tumor cells |
| A375 | malignant melanoma cancer cells |
| A549 | Human adeno lung carcinoma |
| ALA | 5-Aminolevulinic acid |
| Arg-Gly-Asp | Arginylglycylaspartic acid |
| B16-F10 | Murine melanoma cells |
| BODIPY | boron-dipyrromethene |
| CACO-2 cells | Human colorectal adenocarcinoma cells |
| CCL1.3 | Fibroblast cells |
| CD44 | Cell surface adhesion receptor 44 |
| CDT | Chemodynamic therapy |
| Ce6 | Chlorin e6 |
| CLIPT | Continuous low-irradiance photodynamic therapy procedure |
| DETC | Diethyldithiocarbamate |
| DLA cells | Dalton’s Lymphoma Ascite |
| DNA | Deoxyribonucleic acid |
| EGFRvIII | Epidermal growth factor receptor variant III |
| EpCAM or CD326 | Epithelial cell adhesion molecules |
| EPR effect | Enhanced permeability and retention Effect |
| Fe3O4 | Iron (II, III) oxide |
| g-C3N4 QDs | Graphitic carbon nitride quantum dots |
| h | Hour |
| H2O2 | Hydrogen peroxide |
| HBMEC | Brain capillary endothelial cells |
| HBMEC | Blood-brain barrier |
| HEK 293T | Human embryonic kidney cells |
| HeLa | Human cervical carcinoma cells |
| HMSNs | Hollow mesoporous silica nanoparticles |
| HpD | Haematoporphyrin derivatives |
| HPPH | 2-[1-hexyloxyethyl]-2-devinyl pyropheophorbide-a |
| HT-29 cells | Human colon cancer cells |
| IR820 | Indocyanine green |
| J/cm2 | Joules per square centimeter |
| Kg | Kilogram |
| LED | Light emitting diode |
| MB | Methylene blue |
| MCF-7 | Human breast cancer cells |
| MDA-MB231 | human breast cancer cells |
| MDA-MB-435 | Human breast cancer cells |
| mg | Milligram |
| mTHPC | m-Tetrahydroxyphenylchlorin |
| MTT | 2,5-diphenyl-2H-tetrazolium bromide salts |
| mV | Millivolt |
| NIH3T3 cells | Mouse embryo fibroblast cells |
| nm | Nanometer |
| NPs | Nanoparticles |
| O2 | Oxygen |
| OEC-M1 | Oral epidermoid carcinoma cells |
| OH | Hydroxide |
| PAMAM | Poly(amidoamine) |
| PBS | Phosphate bufferred saline |
| PDT | Photodynamic therapy |
| PEG | Poly(ethylene glycol) |
| PLGA | Poly(lactic-co-glycolic acid) |
| PPI | Poly(propylene imine) |
| PpIX | Protoporphyrin IX |
| PS | Photosensitizer |
| PS | Photosensitizers |
| PTT | Photothermal effect |
| RGD | Tripeptide consisting of arginine, glycine, and aspartate |
| ROS | Reactive oxygen species |
| SiHa cells | Human cervical cancer cells |
| SKOV-3 cells | Human adenocarcinoma cells |
| T98G cells | Glioblastoma cells |
| TAPP | 5,10,15,20-tetrakis (4-aminophenyl) porphyrin |
| TPP | Triphenylphosphine |
| U87 MG | Uppsala 87 malignant glioma cells |
| W/cm2 | Watt per square centimetre |
| ZnPc | Zinc phthalocyanine |
Author Contributions
S.S.D.K.: conceptualization, investigation, and writing original draft. H.A.: organizing this study, supervision, and revising critically for intellectual content. All authors have read and agreed to the published version of the manuscript.
Funding
This work is based on the research supported by the South African Research Chairs Initiative of the Department of Science and Technology and National Research Foundation of South Africa (Grant No 98337), as well as grants received from the University of Johannesburg (URC), the National Research Foundation (NRF), and the CSIR (Council for Scientific and Industrial Research)-NLC (National Laser Centre) Laser Rental Pool Programme.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors confirm that this article content has no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cooper G.M. The Cell: A Molecular Approach. 2nd ed. Sinauer Associates; Sunderland, MA, USA: 2000. [(accessed on 15 September 2021)]. The Development and Causes of Cancer. Available online: https://www.ncbi.nlm.nih.gov/books/NBK9963/ [Google Scholar]
- 2.Lodish H., Berk A., Zipursky S.L., Matsudaira P., Baltimore D., Darnell J. Molecular Cell Biology. 4th ed. W. H. Freeman; New York, NY, USA: 2000. [(accessed on 15 September 2021)]. Section 12.4, DNA Damage and Repair and Their Role in Carcinogenesis. Available online: https://www.ncbi.nlm.nih.gov/books/NBK21554/ [Google Scholar]
- 3.Mansoori B., Mohammadi A., Davudian S., Shirjang S., Baradaran B. The Different Mechanisms of Cancer Drug Resistance: A Brief Review. Adv. Pharm. Bull. 2017;7:339–348. doi: 10.15171/apb.2017.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. [(accessed on 7 May 2021)]. Available online: https://www.who.int/news-room/fact-sheets/detail/cancer.
- 5.Ravindran J., Prasad S., Aggarwal B.B. Curcumin and Cancer Cells: How Many Ways Can Curry Kill Tumor Cells Selectively? AAPS J. 2009;11:495–510. doi: 10.1208/s12248-009-9128-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sutradhar K.B., Amin M.L. Nanotechnology in cancer drug delivery and selective targeting. ISRN Nanotechnol. 2014;2014:939378. doi: 10.1155/2014/939378. [DOI] [Google Scholar]
- 7.Yao Y., Zhou Y., Liu L., Xu Y., Chen Q., Wang Y., Wu S., Deng Y., Zhang J., Shao A. Nanoparticle-Based Drug Delivery in Cancer Therapy and Its Role in Overcoming Drug Resistance. Front. Mol. Biosci. 2020;7:193. doi: 10.3389/fmolb.2020.00193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ang C.Y., Tan S.Y., Zhao Y. Recent advances in biocompatible nanocarriers for delivery of chemotherapeutic cargoes towards cancer therapy. Org. Biomol. Chem. 2014;12:4776–4806. doi: 10.1039/c4ob00164h. [DOI] [PubMed] [Google Scholar]
- 9.Li L.-Y., Zhou Y.-M., Gao R.-Y., Liu X.-C., Du H.-H., Zhang J.-L., Ai X.-C., Zhang J.-P., Fu L.-M., Skibsted L.H. Naturally occurring nanotube with surface modification as biocompatible, target-specific nanocarrier for cancer phototherapy. Biomaterials. 2019;190–191:86–96. doi: 10.1016/j.biomaterials.2018.10.046. [DOI] [PubMed] [Google Scholar]
- 10.Malekzad H., Zangabad P.S., Mirshekari H., Hamblin M.R. Noble metal nanoparticles in biosensors: Recent studies and application. Nanotechnol. Rev. 2017;6:301–329. doi: 10.1515/ntrev-2016-0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mekuria S.L., Debele T.A., Tsai H.-C. PAMAM dendrimer based targeted nano-carrier for bio-imaging and therapeutic agents. RSC Adv. 2016;6:63761–63772. doi: 10.1039/C6RA12895E. [DOI] [Google Scholar]
- 12.Bhaskar S., Tian F., Stoeger T., Kreyling W., de la Fuente J.M., Grazu V., Borm P., Estrada G., Ntziachristos V., Razansky D. Multifunctional Nanocarriers for diagnostics, drug delivery and targeted treatment across blood-brain barrier: Perspectives on tracking and neuroimaging. Part. Fibre Toxicol. 2010;7:3. doi: 10.1186/1743-8977-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tyagi N., Song Y.H., De R. Recent progress on biocompatible nanocarrier-based genistein delivery systems in cancer therapy. J. Drug Target. 2019;27:394–407. doi: 10.1080/1061186X.2018.1514040. [DOI] [PubMed] [Google Scholar]
- 14.Sharma P., Rana S., Barick K.C., Kumar C., Salunke H.G., Hassan P.A. Biocompatible phosphate anchored Fe3O4 nanocarriers for drug delivery and hyperthermia. New J. Chem. 2014;38:5500–5508. doi: 10.1039/C4NJ01431F. [DOI] [Google Scholar]
- 15.Patra J.K., Das G., Fraceto L.F., Campos E.V.R., Rodriguez-Torres M.D.P., Acosta-Torres L.S., Diaz-Torres L.A., Grillo R., Swamy M.K., Sharma S., et al. Nano based drug delivery systems: Recent developments and future prospects. J. Nanobiotechnology. 2018;16:71. doi: 10.1186/s12951-018-0392-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sathish Sundar D., Gover Antoniraj M., Senthil Kumar C., Mohapatra S.S., Houreld N.N., Ruckmani K. Recent trends of biocompatible and biodegradable nanoparticles in drug delivery. Curr. Med. Chem. 2016;23:3730–3751. doi: 10.2174/0929867323666160607103854. [DOI] [PubMed] [Google Scholar]
- 17.Li X., Wang L., Fan Y., Feng Q., Cui F.-Z. Biocompatibility and toxicity of nanoparticles and nanotubes. J. Nanomat. 2012;2012:548389. doi: 10.1155/2012/548389. [DOI] [Google Scholar]
- 18.Sukhanova A., Bozrova S., Sokolov P., Berestovoy M., Karaulov A., Nabiev I. Dependence of nanoparticle toxicity on their physical and chemical properties. Nanoscale Res. Lett. 2018;13:44. doi: 10.1186/s11671-018-2457-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park J., Lee Y.-K., Park I.-K., Hwang S.R. Current limitations and recent progress in nanomedicine for clinically available photodynamic therapy. Biomedicines. 2021;9:85. doi: 10.3390/biomedicines9010085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bazak R., Houri M., Achy S.E., Hussein W., Refaat T. Passive targeting of nanoparticles of cancer: A comprehensive review of the literature. Mol. Clin. Oncol. 2014;2:904–908. doi: 10.3892/mco.2014.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hong E.J., Choi D.G., Shim M.S. Targeted and effective photodynamic therapy for cancer using functionalized nanomaterials. Acta Pharm. Sin. B. 2016;6:297–307. doi: 10.1016/j.apsb.2016.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fakayode O.J., Tsolekile N., Songca S.P., Oluwafemi O.S. Applications of functionalized nanomaterials in photodynamic therapy. Biophys. Rev. 2018;10:49–67. doi: 10.1007/s12551-017-0383-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yang Z., Sun Z., Ren Y., Chen X., Zhang W., Zhu X., Mao Z., Shen J., Nie S. Advances in nanomaterials for use in photothermal and photodynamic therapeutics (review) Mol. Med. Rep. 2019;20:5–15. doi: 10.3892/mmr.2019.10218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Benov L. Photodynamic therapy: Current status and future directions. Med. Princ. Pract. 2014;24:14–28. doi: 10.1159/000362416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mansoori B., Mohammadi A., Amin Doustvandi M., Mohammadnejad F., Kamari F., Gjerstorff M.F., Baradaran B., Hamblin M.R. Photodynamic therapy for cancer: Role of natural products. Photodiagnosis Photodyn. Ther. 2019;26:395–404. doi: 10.1016/j.pdpdt.2019.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Abrahamse H., Hamblin M.R. New photosensitizers for photodynamic therapy. Biochem. J. 2016;473:347–364. doi: 10.1042/BJ20150942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Castano A.P., Demidova T.N., Hamblin M.R. Mechanisms in photodynamic therapy: Part one-photosensitizers, photochemistry and cellular localization. Photodiagnosis Photodyn. Ther. 2004;1:279–293. doi: 10.1016/S1572-1000(05)00007-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kwiatkowski S., Knap B., Przystupski D., Saczko J., Kędzierska E., Knap-Czop K., Kotlińska J., Michel O., Kotowski K., Kulbacka J. Photodynamic therapy—Mechanisms, photosensitizers and combinations. Biomed. Pharmacother. 2018;106:1098–1107. doi: 10.1016/j.biopha.2018.07.049. [DOI] [PubMed] [Google Scholar]
- 29.Li T., Yan L. Functional Polymer Nanocarriers for Photodynamic Therapy. Pharmaceuticals. 2018;11:133. doi: 10.3390/ph11040133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Klajnert B., Rozanek M., Bryszewska M. Dendrimers in photodynamic therapy. Curr. Med. Chem. 2012;19:4903–4912. doi: 10.2174/0929867311209024903. [DOI] [PubMed] [Google Scholar]
- 31.Derycke A.S., de Witte P.A. Liposomes for photodynamic therapy. Adv. Drug Deliv. Rev. 2004;56:17–30. doi: 10.1016/j.addr.2003.07.014. [DOI] [PubMed] [Google Scholar]
- 32.Sundaram P., Abrahamse H. Phototherapy combined with carbon nanomaterials (1D and 2D) and their applications in cancer therapy. Materials. 2020;13:4830. doi: 10.3390/ma13214830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.García Calavia P., Bruce G., Pérez-García L., Russell D.A. Photosensitiser-gold nanoparticle conjugates for photodynamic therapy of cancer. Photochem. Photobiol. Sci. 2018;17:1534–1552. doi: 10.1039/C8PP00271A. [DOI] [PubMed] [Google Scholar]
- 34.Khoza P., Ndhundhuma I., Karsten A., Nyokong T. Photodynamic therapy activity of phthalocyanine silver nanoparticles on melanoma cancer cells. J. Nanosci. Nanotechnol. 2020;20:3097–3104. doi: 10.1166/jnn.2020.17398. [DOI] [PubMed] [Google Scholar]
- 35.Choi K.H., Nam K.C., Cho G., Jung J.S., Park B.J. Enhanced Photodynamic Anticancer Activities of Multifunctional Magnetic Nanoparticles (Fe3O4) Conjugated with Chlorin e6 and Folic Acid in Prostate and Breast Cancer Cells. Nanomaterials. 2018;8:722. doi: 10.3390/nano8090722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xu C., Nam J., Hong H., Xu Y., Moon J.J. Positron Emission Tomography-Guided Photodynamic Therapy with Biodegradable Mesoporous Silica Nanoparticles for Personalized Cancer Immunotherapy. ACS Nano. 2019;13:12148–12161. doi: 10.1021/acsnano.9b06691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fernandez M., Orozco J. Advances in functionalized photosensitive polymeric nanocarriers. Polymers. 2021;13:2464. doi: 10.3390/polym13152464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Prabhu R., Patravale V., Joshi M.D. Polymeric nanoparticles for targeted treatment in oncology: Current insights. Int. J. Nanomedicine. 2015;10:1001–1018. doi: 10.2147/IJN.S56932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li J., Li J., Pu Y., Li S., Gao W., He B. PDT-Enhanced Ferroptosis by a Polymer Nanoparticle with pH-Activated Singlet Oxygen Generation and Superb Biocompatibility for Cancer Therapy. Biomacromolecules. 2021;22:1167–1176. doi: 10.1021/acs.biomac.0c01679. [DOI] [PubMed] [Google Scholar]
- 40.Zhang D., Wu M., Zeng Y., Wu L., Wang Q., Han X., Liu X., Liu J. Chlorin e6 Conjugated Poly(dopamine) Nanospheres as PDT/PTT Dual-Modal Therapeutic Agents for Enhanced Cancer Therapy. ACS Appl. Mater. Interfaces. 2015;7:8176–8187. doi: 10.1021/acsami.5b01027. [DOI] [PubMed] [Google Scholar]
- 41.Ebani P.R., Stefanello L., Kuhn B.L., Frizzo C.P., Burgo T.A.L., Kloster C.L., Villetti M.A. Carboxymethyl chitosan/ionic liquid imidazolium-based nanoparticles as nanocarriers for zinc phthalocyanine and its photodynamic activity. J. Mol. Liq. 2021;336:116874. doi: 10.1016/j.molliq.2021.116874. [DOI] [Google Scholar]
- 42.Zhu D., Roy S., Liu Z., Weller H., Parak W.J., Feliu N. Remotely controlled opening of delivery vehicles and release of cargo by external triggers. Adv. Drug Deliv. Rev. 2019;138:117–132. doi: 10.1016/j.addr.2018.10.003. [DOI] [PubMed] [Google Scholar]
- 43.Barhoumi A., Liu Q., Kohane D.S. Ultraviolet light-mediated drug delivery: Principles, applications, and challenges. J. Control. Rel. 2015;219:31–42. doi: 10.1016/j.jconrel.2015.07.018. [DOI] [PubMed] [Google Scholar]
- 44.Schoppa T., Jung D., Rust T., Mulac D., Kuckling D., Langer K. Light-responsive polymeric nanoparticles based on a novel nitropiperonal based polyester as drug delivery systems for photosensitizers in PDT. Int. J. Pharm. 2021;597:120326. doi: 10.1016/j.ijpharm.2021.120326. [DOI] [PubMed] [Google Scholar]
- 45.Madaan K., Kumar S., Poonia N., Lather V., Pandita D. Dendrimers in drug delivery and targeting: Drug-dendrimer interactions and toxicity issues. J. Pharm. Bioallied Sci. 2014;6:139–150. doi: 10.4103/0975-7406.130965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sherje A.P., Jadhav M., Dravyakar B.R., Kadam D. Dendrimers: A versatile nanocarrier for drug delivery and targeting. Int. J. Pharm. 2018;548:707–720. doi: 10.1016/j.ijpharm.2018.07.030. [DOI] [PubMed] [Google Scholar]
- 47.Patri A.K., Kukowska-Latallo J.F., Baker J.R., Jr. Targeted drug delivery with dendrimers: Comparison of the release kinetics of covalently conjugated drug and non-covalent drug inclusion complex. Adv. Drug Deliv. Rev. 2005;57:2203–2214. doi: 10.1016/j.addr.2005.09.014. [DOI] [PubMed] [Google Scholar]
- 48.Pooresmaeil M., Namazi H. Advances in development of the dendrimers having natural saccharides in their structure for efficient and controlled drug delivery applications. Eur. Polym. J. 2021;148:110356. doi: 10.1016/j.eurpolymj.2021.110356. [DOI] [Google Scholar]
- 49.Ouyang Z., Gao Y., Shen M., Shi X. Dendrimer-based nanobybrids in cancer photomedicine. Mater. Today Bio. 2021;10:100111. doi: 10.1016/j.mtbio.2021.100111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dabrzalska M., Janaszewska A., Zablocka M., Mignani S., Majoral J.P., Klajnert-Maculewicz B. Cationic phosphorus dendrimer enhances photodynamic activity of rose bengal against basal cell carcinoma cell lines. Mol. Pharm. 2017;14:1821–1830. doi: 10.1021/acs.molpharmaceut.7b00108. [DOI] [PubMed] [Google Scholar]
- 51.Zhou T., Battah S., Mazzacuva F., Hider R.C., Dobbin P., MacRobert A.J. Design of bifunctional dendritic 5-Aminolevulinic acid and hydroxypyridinone conjugates for photodynamic therapy. Bioconjugate Chem. 2018;29:3411–3428. doi: 10.1021/acs.bioconjchem.8b00574. [DOI] [PubMed] [Google Scholar]
- 52.Kojima C., Toi Y., Harada A., Kono K. Preparation of Poly (ethylene glycol)-Attached Dendrimers Encapsulating Photosensitizers for Application to Photodynamic Therapy. Bioconjugate Chem. 2007;18:663–670. doi: 10.1021/bc060244u. [DOI] [PubMed] [Google Scholar]
- 53.Guimaraes D., Cavaco-Paulo A., Nogueira E. Design of liposomes as drug delivery system for therapeutic applications. Int. J. Pharm. 2021;601:120571. doi: 10.1016/j.ijpharm.2021.120571. [DOI] [PubMed] [Google Scholar]
- 54.Jin C.S., Zheng G. Liposomal nanostructures for photosensitizer delivery. Lasers Surg. Med. 2011;43:734–748. doi: 10.1002/lsm.21101. [DOI] [PubMed] [Google Scholar]
- 55.Ichikawa K., Hikita T., Maeda N., Yonezawa S., Takeuchi Y., Asai T., Namba Y., Oku N. Antiangiogenic photodynamic therapy (PDT) by using long-circulating liposomes modified with peptide specific to angiogenic vessels. Biochim. Biophys. Acta Biomembr. 2005;1669:69–74. doi: 10.1016/j.bbamem.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 56.Yang Y., Wang L., Cao H., Li Q., Li Y., Han M., Wang H., Li J. Photodynamic Therapy with Liposomes Encapsulating Photosensitizers with Aggregation-Induced Emission. Nano Lett. 2019;19:1821–1826. doi: 10.1021/acs.nanolett.8b04875. [DOI] [PubMed] [Google Scholar]
- 57.Akbarzadeh A., Rezaei-Sadabady R., Davaran S., Joo S.W., Zarghami N., Hanifehpour Y., Samiei M., Kouhi M., Nejati-Koshki K. Liposome: Classification, preparation, and applications. Nanoscale Res. Lett. 2013;8:102. doi: 10.1186/1556-276X-8-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Feuser P.E., Cordeiro A.P., de Bem Silveira G., Correa M.E.A.B., Silveira P.C.L., Sayer C., de Araujo P.H.H., Machado-de-Avila R.A., Bo A.G.D. Co-encapsulation of sodium diethyldithiocarbamate (DETC) and zinc phthalocyanine (ZnPc) in liposomes promotes increases phototoxic activity against (MDA-MB 231) human breast cancer cells. Colloids Surf. B. 2021;197:111434. doi: 10.1016/j.colsurfb.2020.111434. [DOI] [PubMed] [Google Scholar]
- 59.Lee E.-H., Lim S.-J., Lee M.-K. Chitosan-coated liposomes to stabilize and enhance transdermal delivery of indocyanine green for photodynamic therapy of melanoma. Carbohydr. Polym. 2019;224:115143. doi: 10.1016/j.carbpol.2019.115143. [DOI] [PubMed] [Google Scholar]
- 60.Miretti M., Tempesti T.C., Prucca C.G., Baumgartner M.T. Zn phthalocyanines loaded into liposomes: Characterization and enhanced performance of photodynamic activity on glioblastoma cells. Bioorg. Med. Chem. 2020;28:115355. doi: 10.1016/j.bmc.2020.115355. [DOI] [PubMed] [Google Scholar]
- 61.Sui C., Tan R., Chen Y., Yin G., Wang Z., Xu W., Li X. MOFs-Derived Fe–N Codoped Carbon Nanoparticles as O2-Evolving Reactor and ROS Generator for CDT/PDT/PTT Synergistic Treatment of Tumors. Bioconjugate Chem. 2021;32:318–327. doi: 10.1021/acs.bioconjchem.0c00694. [DOI] [PubMed] [Google Scholar]
- 62.Zheng D.-W., Li B., Li C.-X., Fan J.-C., Lei Q., Li C., Xu Z., Zhang X.-Z. Carbon-Dot-Decorated Carbon Nitride Nanoparticles for Enhanced Photodynamic Therapy against Hypoxic Tumor via Water Splitting. ACS Nano. 2016;10:8715–8722. doi: 10.1021/acsnano.6b04156. [DOI] [PubMed] [Google Scholar]
- 63.Chan M.-H., Chen C.-W., Lee I.-J., Chan Y.-C., Tu D., Hsiao M., Chen C.-H., Chen X., Liu R.-S. Near-Infrared Light-Mediated Photodynamic Therapy Nanoplatform by the Electrostatic Assembly of Upconversion Nanoparticles with Graphitic Carbon Nitride Quantum Dots. Inorg. Chem. 2016;55:10267–10277. doi: 10.1021/acs.inorgchem.6b01522. [DOI] [PubMed] [Google Scholar]
- 64.Kang M.S., Lee S.Y., Kim K.S., Han D.W. State of the Art Biocompatible Gold Nanoparticles for Cancer Theragnosis. Pharmaceutics. 2020;12:701. doi: 10.3390/pharmaceutics12080701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kong F.Y., Zhang J.W., Li R.F., Wang Z.X., Wang W.J., Wang W. Unique Roles of Gold Nanoparticles in Drug Delivery, Targeting and Imaging Applications. Molecules. 2017;22:1445. doi: 10.3390/molecules22091445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yao C., Zhang L., Wang J., He Y., Xin J., Wang S., Xu H. Gold nanoparticles mediated phototherapy for cancer. J. Nanomat. 2016;2016:5497136. doi: 10.1155/2016/5497136. [DOI] [Google Scholar]
- 67.Cheng Y., Meyers J.D., Broome A.-M., Kenney M.C., Basilion J.P., Burda C. Deep Penetration of a PDT Drug into Tumors by Noncovalent Drug-Gold Nanoparticle Conjugates. J. Am. Chem. Soc. 2011;133:2583–2591. doi: 10.1021/ja108846h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dutta D., Sailapu S.K., Simon A.T., Ghosh S.S., Chattopadhyay A. Gold-Nanocluster-Embedded Mucin Nanoparticles for Photodynamic Therapy and Bioimaging. Langmuir. 2019;35:10475–10483. doi: 10.1021/acs.langmuir.9b00998. [DOI] [PubMed] [Google Scholar]
- 69.Wei X., Chen H., Tham H.P., Zhang N., Xing P., Zhang G., Zhao Y. Combined Photodynamic and Photothermal Therapy Using Cross-Linked Polyphosphazene Nanospheres Decorated with Gold Nanoparticles. ACS Appl. Nano Mater. 2018;1:3663–3672. doi: 10.1021/acsanm.8b00776. [DOI] [Google Scholar]
- 70.Lin J., Wang S., Huang P., Wang Z., Chen S., Niu G., Li W., He J., Cui D., Lu G., et al. Photosensitizer-Loaded Gold Vesicles with Strong Plasmonic Coupling Effect for Imaging-Guided Photothermal/Photodynamic Therapy. ACS Nano. 2013;7:5320–5329. doi: 10.1021/nn4011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mfouo-Tynga I., El-Hussein A., Abdel-Harith M., Abrahamse H. Photodynamic ability of silver nanoparticles in inducing cytotoxic effects in breast and lung cancer cell lines. Int. J. Nanomed. 2014;9:3771–3780. [Google Scholar]
- 72.Mahajan P.G., Dige N.C., Vanjare B.D., Eo S.-H., Seo S.-Y., Kim S.J., Hong S.-K., Choi C.-S., Lee K.H. A potential mediator for photodynamic therapy based on silver nanoparticles functionalized with porphyrin. J. Photochem. Photobiol. A Chem. 2019;377:26–35. doi: 10.1016/j.jphotochem.2019.03.034. [DOI] [Google Scholar]
- 73.Natesan S., Krishnaswami V., Ponnusamy C., Madiyalakan M., Woo T., Palanisamy R. Hypocrellin B and nano silver loaded polymeric nanoparticles: Enhanced generation of singlet oxygen for improved photodynamic therapy. Mater. Sci. Eng. C. 2017;77:935–946. doi: 10.1016/j.msec.2017.03.179. [DOI] [PubMed] [Google Scholar]
- 74.de Freitas C.F., Kimura E., Rubira A.F., Muniz E.C. Curcumin and silver nanoparticles carried out from polysaccharide-based hydrogels improved the photodynamic properties of curcumin through metal-enhanced singlet oxygen effect. Mater. Sci. Eng. C. 2020;112:110853. doi: 10.1016/j.msec.2020.110853. [DOI] [PubMed] [Google Scholar]
- 75.Hosu O., Tertis M., Cristea C. Implication of magnetic nanoparticles in cancer detection, screening, and treatment. Magnetochemistry. 2019;5:55. doi: 10.3390/magnetochemistry5040055. [DOI] [Google Scholar]
- 76.Arias L.S., Pessan J.P., Vieira A.P.M., Lima T.M.T., Delbem A.C.B., Monteiro D.R. Iron Oxide Nanoparticles for Biomedical Applications: A Perspective on Synthesis, Drugs, Antimicrobial Activity, and Toxicity. Antibiotics. 2018;7:46. doi: 10.3390/antibiotics7020046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hou H., Huang X., Wei G., Xu F., Wang Y., Zhou S. Fenton Reaction-Assisted Photodynamic Therapy for Cancer with Multifunctional Magnetic Nanoparticles. ACS Appl. Mater. Interfaces. 2019;11:29579–29592. doi: 10.1021/acsami.9b09671. [DOI] [PubMed] [Google Scholar]
- 78.Cinteza L.O., Ohulchanskyy T.Y., Sahoo Y., Bergey E.J., Pandey R.K., Prasad P.N. Diacyllipid Micelle-Based Nanocarrier for Magnetically Guided Delivery of Drugs in Photodynamic Therapy. Mol. Pharm. 2006;3:415–423. doi: 10.1021/mp060015p. [DOI] [PubMed] [Google Scholar]
- 79.Di Corato R., Bealle G., Kolosnjaj-Tabi J., Espinosa A., Clement O., Silva A.K.A., Menager C., Wilhelm C. Combining Magnetic Hyperthermia and Photodynamic Therapy for Tumor Ablation with Photoresponsive Magnetic Liposomes. ACS Nano. 2015;9:2904–2916. doi: 10.1021/nn506949t. [DOI] [PubMed] [Google Scholar]
- 80.Zhou H., Hou X., Liu Y., Zhao T., Shang Q., Tang J., Liu J., Wang Y., Wu Q., Luo Z., et al. Superstable Magnetic Nanoparticles in Conjugation with Near-Infrared Dye as a Multimodal Theranostic Platform. ACS Appl. Mater. Interfaces. 2016;8:4424–4433. doi: 10.1021/acsami.5b11308. [DOI] [PubMed] [Google Scholar]
- 81.Rastegari E., Hsiao Y.-J., Lai W.-Y., Lai Y.-H., Yang T.-C., Chen S.-J., Huang P.-I., Chiou S.-H., Mou C.-Y., Chien Y. An Update on Mesoporous Silica Nanoparticle Applications in Nanomedicine. Pharmaceutics. 2021;13:1067. doi: 10.3390/pharmaceutics13071067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chen K., Chang C., Zuhao L., Zhou Y., Xu Q., Li C., Huang Z., Xu H., Xu P., Lu B. Hyaluronic acid targeted and pH-responsive nanocarriers based on hollow mesoporous silica nanoparticles for chemo-photodynamic combination therapy. Colloids Surf. B. 2020;194:111166. doi: 10.1016/j.colsurfb.2020.111166. [DOI] [PubMed] [Google Scholar]
- 83.Han R., Wu S., Yan Y., Chen W., Tang K. Construction of ferrocene modified and indocyanine green loaded multifunctional mesoporous silica nanoparticle for simultaneous chemodynamic/photothermal/photodynamic therapy. Mater. Today Commun. 2021;26:101842. doi: 10.1016/j.mtcomm.2020.101842. [DOI] [Google Scholar]
- 84.Pan Q., Tian J., Zhu H., Hong L., Mao Z., Oliveira J.M., Reis R.L., Li X. Tumor-Targeting Polycaprolactone Nanoparticles with Codelivery of Paclitaxel and IR780 for Combinational Therapy of Drug-Resistant Ovarian Cancer. ACS Biomater. Sci. Eng. 2020;6:2175–2185. doi: 10.1021/acsbiomaterials.0c00163. [DOI] [PubMed] [Google Scholar]
- 85.Dabrzalska M., Zablocka M., Mignani S., Majoral J.P., Klajnert-Maculewicz B. Phosphorus dendrimers and photodynamic therapy. Spectroscopic studies on two dendrimer-photosensitizer complexes: Cationic phosphorus dendrimer with rose bengal and anionic phosphorus dendrimer with methylene blue. Int. J. Pharm. 2015;492:266–274. doi: 10.1016/j.ijpharm.2015.06.014. [DOI] [PubMed] [Google Scholar]
- 86.Ghosh S., Carter K.A., Lovell J.F. Liposomal formulations of photosensitizers. Biomaterials. 2019;218:119341. doi: 10.1016/j.biomaterials.2019.119341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zhu Z., Tang Z., Phillips J.A., Yang R., Wang H., Tan W. Regulation of singlet oxygen generation using single-walled carbon nanotubes. J. Am. Chem. Soc. 2008;130:10856–10857. doi: 10.1021/ja802913f. [DOI] [PubMed] [Google Scholar]
- 88.Tan X., Wang J., Pang X., Liu L., Sun Q., You Q., Tan F., Li N. Indocyanine Green-Loaded Silver Nanoparticle@Polyaniline Core/Shell Theranostic Nanocomposites for Photoacoustic/Near-Infrared Fluorescence Imaging-Guided and Single-Light-Triggered Photothermal and Photodynamic Therapy. ACS Appl. Mater. Interfaces. 2016;8:34991–35003. doi: 10.1021/acsami.6b11262. [DOI] [PubMed] [Google Scholar]
- 89.Silva A.K.A., Kolosnjaj-Tabi J., Bonneau S., Marangon I., Boggetto N., Aubertin K., Clement O., Bureau M.F., Luciani N., Gazeau F., et al. Magnetic and Photoresponsive Theranosomes: Translating Cell-Released Vesicles into Smart Nanovectors for Cancer Therapy. ACS Nano. 2013;7:4954–4966. doi: 10.1021/nn400269x. [DOI] [PubMed] [Google Scholar]
- 90.Ma X., Qu Q., Zhao Y. Targeted Delivery of 5-Aminolevulinic Acid by Multifunctional Hollow Mesoporous Silica Nanoparticles for Photodynamic Skin Cancer Therapy. ACS Appl. Mater. Interfaces. 2015;7:10671–10676. doi: 10.1021/acsami.5b03087. [DOI] [PubMed] [Google Scholar]
- 91.Yi G., Hong S.H., Son J., Yoo J., Park C., Choi Y., Koo H. Recent advances in nanoparticle carriers for photodynamic therapy. Quant. Imaging Med. Surg. 2018;8:433–443. doi: 10.21037/qims.2018.05.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Yang S.-G., Chang J.-E., Shin B., Na K., Shim C.-K. 99mTc-hematoporphyrin linked albumin nanoparticles for lung cancer targeted photodynamic therapy and imaging. J. Mater. Chem. 2010;20:9042–9046. doi: 10.1039/c0jm01544j. [DOI] [Google Scholar]
- 93.Lamch L., Bazylinska U., Kulbacka J., Pietkiewicz J., Bieżuńska-Kusiak K., Wilk K.A. Polymeric micelles for enhanced Photofrin II® delivery, cytotoxicity and pro-apoptotic activity in human breast and ovarian cancer cells. Photodiagnosis Photodyn. Ther. 2014;11:570–585. doi: 10.1016/j.pdpdt.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 94.Gonzalez-Delgado J.A., Castro P.M., Machado A., Araujo F., Rodrigues F., Korsak B., Ferreira M., Tome J.P., Sarmento B. Hydrogels containing porphyrin-loaded nanoparticles for topical photodynamic applications. Int. J. Pharm. 2016;510:221–231. doi: 10.1016/j.ijpharm.2016.06.037. [DOI] [PubMed] [Google Scholar]
- 95.Wang X., Li S., Liu H. Co-delivery of chitosan nanoparticles of 5-aminolevulinic acid and shGBAS for improving photodynamic therapy efficacy in oral squamous cell carcinomas. Photodiagnosis Photodyn. Ther. 2021;34:102218. doi: 10.1016/j.pdpdt.2021.102218. [DOI] [PubMed] [Google Scholar]
- 96.Brezaniova I., Hruby M., Kralova J., Kral V., Cernochova Z., Cernoch P., Slouf M., Kredatusova J., Stepanek P. Temoporfin-loaded 1-tetradecanol-based thermoresponsive solid lipid nanoparticles for photodynamic therapy. J. Control. Release. 2016;241:34–44. doi: 10.1016/j.jconrel.2016.09.009. [DOI] [PubMed] [Google Scholar]
- 97.Konan-Kouakou Y.N., Boch R., Gurny R., Allemann E. In vitro and in vivo activities of verteporfin-loaded nanoparticles. J. Control. Rel. 2005;103:83–91. doi: 10.1016/j.jconrel.2004.11.023. [DOI] [PubMed] [Google Scholar]
- 98.Sundaram P., Abrahamse H. Effective Photodynamic Therapy for Colon Cancer Cells Using Chlorin e6 Coated Hyaluronic Acid-Based Carbon Nanotubes. Int. J. Mol. Sci. 2020;21:4745. doi: 10.3390/ijms21134745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Chepurna O.M., Yakovliev A., Ziniuk R., Nikolaeva O.A., Levchenko S.M., Xu H., Losytskyy M.Y., Bricks J.L., Slominskii Y.L., Vretik L.O., et al. Core–shell polymeric nanoparticles co-loaded with photosensitizer and organic dye for photodynamic therapy guided by fluorescence imaging in near and short-wave infrared spectral regions. J. Nanobiotechnol. 2020;18:1–15. doi: 10.1186/s12951-020-0572-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Thakur N.S., Mandal N., Patel G., Kirar S., Reddy Y.N., Kushwah V., Jain S., Kalia Y.N., Bhaumik J., Banerjee U.C. Co-administration of zinc phthalocyanine and quercetin via hybrid nanoparticles for augmented photodynamic therapy. Nanomedicine Nanotechnol. 2021;33:102368. doi: 10.1016/j.nano.2021.102368. [DOI] [PubMed] [Google Scholar]
- 101.Ma M., Cheng L., Zhao A., Zhang H., Zhang A. Pluronic-based graphene oxide-methylene blue nanocomposite for photodynamic/photothermal combined therapy of cancer cells. Photodiagnosis Photodyn. Ther. 2020;29:101640. doi: 10.1016/j.pdpdt.2019.101640. [DOI] [PubMed] [Google Scholar]
- 102.Karthikeyan K., Babu A., Kim S.-J., Murugesan R., Jeyasubramanian K. Enhanced photodynamic efficacy and efficient delivery of Rose Bengal using nanostructured poly(amidoamine) dendrimers: Potential application in photodynamic therapy of cancer. Cancer Nanotechnol. 2011;2:95–103. doi: 10.1007/s12645-011-0019-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Su Y., Wang N., Liu B., Du Y., Li R., Meng Y., Feng Y., Shan Z., Meng S. A phototheranostic nanoparticle for cancer therapy fabricated by BODIPY and graphene to realize photo-chemo synergistic therapy and fluorescence/photothermal imaging. Dyes Pigm. 2020;177:177–108262. doi: 10.1016/j.dyepig.2020.108262. [DOI] [Google Scholar]
- 104.Damke G.M.Z.F., Souza R.P., Montanha M.C., Damke E., Gonçalves R.S., César G.B., Kimura E., Caetano W., Hioka N., Consolaro M.E. Selective Photodynamic Effects on Breast Cancer Cells Provided by p123 Pluronic®- Based Nanoparticles Modulating Hypericin Delivery. Anticancer Agents Med. Chem. 2020;20:1352–1367. doi: 10.2174/1871520618666181102091010. [DOI] [PubMed] [Google Scholar]
- 105.Krishnaswami V., Ponnusamy C., Sankareswaran S., Paulsamy M., Madiyalakan R., Palanichamy R., Kandasamy R., Natesan S. Development of copolymeric nanoparticles of hypocrellin B: Enhanced phototoxic effect and ocular distribution. Eur. J. Pharm. Sci. 2018;116:26–36. doi: 10.1016/j.ejps.2017.10.023. [DOI] [PubMed] [Google Scholar]
- 106.Rivas Aiello M.B., Castrogiovanni D., Parisi J., Azcarate J.C., Garcia Einschlag F.S., Gensch T., Bosio G.N., Martire D.O. Photodynamic therapy in HeLa cells incubated with Riboflavin and pectin-coated silver nanoparticles. Photochem. Photobiol. 2018;94:1159–1166. doi: 10.1111/php.12974. [DOI] [PubMed] [Google Scholar]
- 107.He C., Zhang L., Liu W., Huang Y., Hu P., Dai T., Xu J., Chen Z. Albumin-based nanoparticles combined with photodynamic therapy enhance the antitumor activity of curcumin derivative C086. Dyes Pigm. 2021;189:109258. doi: 10.1016/j.dyepig.2021.109258. [DOI] [Google Scholar]
- 108.Campu A., Focsan M., Lerouge F., Borlan R., Tie L., Rugina D., Astilean S. ICG-loaded gold nano-bipyramids with NIR activatable dual PTT-PDT therapeutic potential in melanoma cells. Colloid Surf. B. 2020;194:111213. doi: 10.1016/j.colsurfb.2020.111213. [DOI] [PubMed] [Google Scholar]
- 109.Deng Y., Pan S., Zheng J., Hong Y., Liu J., Chang H., Miao Y., Sun Y., Li Y. Electrostatic self-assembled Iridium(III) nano-photosensitizer for selectively disintegrated and mitochondria targeted photodynamic therapy. Dyes Pigm. 2020;175:108105. doi: 10.1016/j.dyepig.2019.108105. [DOI] [Google Scholar]
- 110.Wang X., Wang J., Li J., Huang H., Sun X., Lv Y. Development and evaluation of hyaluronic acid-based polymeric micelles for targeted delivery of photosensitizer for photodynamic therapy in vitro. J. Drug Deliv. Sci. Technol. 2018;48:414–421. doi: 10.1016/j.jddst.2018.10.018. [DOI] [Google Scholar]
- 111.Fu X., Sun H., Zhang G., Zhao K., Tian Y., Gao Z., Cui J., Yu Q. Targeted poly(ethylene glycol) nanoparticles for photodynamic therapy. Colloid Surf. A. 2020;606:125394. doi: 10.1016/j.colsurfa.2020.125394. [DOI] [Google Scholar]
- 112.Jamali Z., Khoobi M., Hejazi S.M., Eivazi N., Abdolahpour S., Imanparast F., Moradi-Sardareh H., Paknejad M. Evaluation of targeted curcumin (CUR) loaded PLGA nanoparticles for in vitro photodynamic therapy on human glioblastoma cell line. Photodiagnosis Photodyn. Ther. 2018;23:190–201. doi: 10.1016/j.pdpdt.2018.06.026. [DOI] [PubMed] [Google Scholar]
- 113.Zhu X., Zhou H., Liu Y., Wen Y., Wei C., Yu Q., Liu J. Transferrin/aptamer conjugated mesoporous ruthenium nanosystem for redox-controlled and targeted chemo-photodynamic therapy of glioma. Acta Biomater. 2018;82:143–157. doi: 10.1016/j.actbio.2018.10.012. [DOI] [PubMed] [Google Scholar]
- 114.Liang L., Care A., Zhang R., Lu Y., Packer N.H., Sunna A., Qian Y., Zvyagin A.V. Facile Assembly of Functional Upconversion Nanoparticles for Targeted Cancer Imaging and Photodynamic Therapy. ACS Appl. Mater. Interfaces. 2016;8:11945–11953. doi: 10.1021/acsami.6b00713. [DOI] [PubMed] [Google Scholar]
- 115.Lin A.-L., Fan P.-P., Liu S.-F., Chen J.-H., Zhao Y.-Y., Zheng B.-Y., Ke M.-R., Huang J.-D. A phthalocyanine-based liposomal nanophotosensitizer with highly efficient tumor-targeting and photodynamic activity. Dyes Pigm. 2020;180:108455. doi: 10.1016/j.dyepig.2020.108455. [DOI] [Google Scholar]
- 116.Yoon H.Y., Koo H., Choi K.Y., Lee S.J., Kim K., Kwon I.C., Leary J.F., Park K., Yuk S.H., Park J.H., et al. Tumor-targeting hyaluronic acid nanoparticles for photodynamic imaging and therapy. Biomaterials. 2012;33:3980–3989. doi: 10.1016/j.biomaterials.2012.02.016. [DOI] [PubMed] [Google Scholar]
- 117.Shanmugapriya K., Kim H., Kang H.W. Epidermal growth factor receptor conjugated fucoidan/alginates loaded hydrogel for activating EGFR/AKT signaling pathways in colon cancer cells during targeted photodynamic therapy. Int. J. Biol. Macromol. 2020;158:1163–1174. doi: 10.1016/j.ijbiomac.2020.05.008. [DOI] [PubMed] [Google Scholar]
- 118.Sardoiwala M.N., Kushwaha A.C., Dev A., Shrimali N., Guchhait P., Karmakar S., Choudhury S.R. Hypericin-Loaded Transferrin Nanoparticles Induce PP2A-Regulated BMI1 Degradation in Colorectal Cancer-Specific Chemo-Photodynamic Therapy. ACS Biomater. Sci. Eng. 2020;6:3139–3153. doi: 10.1021/acsbiomaterials.9b01844. [DOI] [PubMed] [Google Scholar]
- 119.Spring B.Q., Rizvi I., Xu N., Hasan T. The role of photodynamic therapy in overcoming cancer drug resistance. Photochem. Photobiol. Sci. 2015;14:1476–1491. doi: 10.1039/C4PP00495G. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Yoo S.W., Oh G., Ahn J.C., Chung E. Non-oncologic applications of nanomedicine-based phototherapy. Biomedicines. 2021;9:113. doi: 10.3390/biomedicines9020113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Low-cost Enabling Technology for Image-guided Photodynamic Therapy (PDT) of Oral Cancer Cancer. [(accessed on 15 September 2021)]; Available online: https://www.clinicaltrials.gov/ct2/show/study/NCT03638622.
- 122.Photodynamic Therapy Using HPPH in Treating Patients with Dysplasia, Cancer in Situ, or Invasive Cancer of the Larynx. [(accessed on 15 September 2021)]; Available online: https://www.clinicaltrials.gov/ct2/show/NCT00675233.
- 123.Photodynamic Therapy (PDT) for Recurrent Pediatric Brain Tumors. [(accessed on 15 September 2021)]; Available online: https://www.clinicaltrials.gov/ct2/show/NCT01682746.
- 124.Photodynamic Therapy (PDT) in Lung Cancer (PDT) [(accessed on 15 September 2021)]; Available online: https://www.clinicaltrials.gov/ct2/show/NCT00984243.
- 125.Sequential Whole Bladder Photodynamic Therapy (WBPDT) in the Management of Superficial Bladder Cancer. [(accessed on 15 September 2021)]; Available online: https://www.clinicaltrials.gov/ct2/show/NCT00322699.
- 126.Photodynamic Therapy in Treating Patients with Skin Cancer. [(accessed on 15 September 2021)]; Available online: https://www.clinicaltrials.gov/ct2/show/NCT00002975.
- 127.Safety Study Using Photodynamic Therapy Light Therapy for Patients With Chest Wall Progression of Breast Cancer and Satellite Metastases of Melanoma (CLIPT) [(accessed on 15 September 2021)]; Available online: https://www.clinicaltrials.gov/ct2/show/NCT00862901.
- 128.Silicon Phthalocyanine 4 and Photodynamic Therapy in Stage IA-IIA Cutaneous T-Cell Non-Hodgkin Lymphoma. [(accessed on 15 September 2021)]; Available online: https://www.clinicaltrials.gov/ct2/show/NCT01800838.
- 129.A Trial of Photodynamic Therapy with HPPH for Treatment of Dysplasia, Carcinoma in Situ and T1 Carcinoma of the Oral Cavity and/or Oropharynx. [(accessed on 15 September 2021)]; Available online: https://www.clinicaltrials.gov/ct2/show/NCT01140178.
- 130.Treatment of Primary Breast Cancer Using PDT. [(accessed on 15 September 2021)]; Available online: https://www.clinicaltrials.gov/ct2/show/NCT02872064.
- 131.Efficacy, Safety and Quality of Life after TOOKAD® Soluble VTP for Localized Prostate Cancer (PCM304) [(accessed on 15 September 2021)]; Available online: https://www.clinicaltrials.gov/ct2/show/NCT01875393.
- 132.Laser Assisted Drug Delivery in the Treatment of Superficial Non Melanoma Skin Cancer: A Randomized Controlled Trial. [(accessed on 15 September 2021)]; Available online: https://www.clinicaltrials.gov/ct2/show/NCT03012009.
- 133.Intrapleural Photodynamic Therapy in a Multimodal Treatment for Patients with Malignant Pleural Mesothelioma (MesoPDT) [(accessed on 15 September 2021)]; Available online: https://www.clinicaltrials.gov/ct2/show/NCT02662504.
- 134.Phase I Photodynamic Therapy (PDT) for Benign Dermal Neurofibromas (NF1) [(accessed on 15 September 2021)]; Available online: https://www.clinicaltrials.gov/ct2/show/NCT01682811.
- 135.Photodynamic Therapy with Visudyne for Human Retinoblastoma: A Preliminary Study. [(accessed on 15 September 2021)]; Available online: https://www.clinicaltrials.gov/ct2/show/NCT04429139.
- 136.Photodynamic Therapy to Treat Actinic Damage in Patients with Squamous Cell Carcinoma (SCC) of the Lip. [(accessed on 15 September 2021)]; Available online: https://www.clinicaltrials.gov/ct2/show/NCT00868088.