Abstract
To address the issue of obesity, the World Health Organization (WHO) recommends a set of comprehensive programmes aimed at changing the obesogenic environments to provide opportunities for healthy food options and increased physical activity in the school, home, and at the population level. The objectives of this study were to examine the nature and range of policies related to overweight and obesity prevention in Africa, and to assess how they align with international guidelines. An existing methodological framework was adapted for this scoping review. A search of publicly available national documents on overweight/obesity, general health, and non-communicable diseases (NCDs) was undertaken from relevant websites, including WHO, ministries, and Google Scholar. Additional requests were sent to key contacts at relevant ministries about existing policy documents. The documents were reviewed, and the policies were categorised, using the Analysis Grid for Environments Linked to Obesity (ANGELO) framework. The framework categorises the environmental drivers of obesity into four domains (physical, economic, legislative, and socio-cultural) and two scales: macro (national, regional, sectors, food industries, media, etc.) and micro (household, institutional, and community). This review included documents from 41 African countries. The policy initiatives to prevent overweight/obesity target the school, family and community settings, and macro environments, and broadly align with global recommendations. The NCD documents were in the majority, with only two on obesity. The majority of the documents detailed strategies and key interventions on unhealthy diets and physical inactivity. The physical, legislative, and sociocultural domains were largely featured, with less emphasis on the economic domain. Additionally, nutrition- and diet-related policies were in the majority. Overlaps and interactions of policies were observed in the application of the ANGELO framework. This study has provided information on national policies and programmes in Africa and can be useful as a first point of call for policymakers. The overlapping and interaction in the initiatives demonstrate the importance of multi-sectoral partnerships in providing supportive environments for healthy behaviours.
Keywords: policy, programmes, NCDs, overweight/obesity, ANGELO framework, unhealthy diets, physical inactivity, Africa
1. Introduction
Globally, an estimated 18% of children and adolescents aged 5–19 years and 39% of adults were overweight or obese in 2016 [1]. The available statistics show increasing trends of body mass index and obesity in Africa. For example, between 1984 and 2014, the age-standardised mean BMI increased in adult men from 21.0 kg/m2 to 23.0 kg/m2, and from 21.9 kg/m2 to 24.9 kg/m2 in women [2]. Similarly, recent estimates from the Global Burden of Disease, Injuries, and Risk Factors Study revealed that obesity more than doubled in Southern African populations, from 12.0% to 18.5% in adult females and 4.5% to 8.8% in adult males between 1990 and 2019. Moreover, among children and adolescents aged 2–19 years, the prevalence rates increased from 2.4% to 5.5% in boys and from 2.8% to 6.0% in girls over the period [3].
The focus has been on unhealthy diets and physical inactivity as the main determinants of the growing obesity crisis [4,5]. However, with the moderate success of individual lifestyle interventions to prevent and control overweight/obesity [6,7,8,9,10], recent attention has been shifted to the wider structural, global and national systems as significant drivers of the obesity crisis [11]. A considerable number of research has linked changes in the food system resulting from global and international food trade to the nutrition transition observed in low-to-middle income countries [12,13,14]. At the same time, structures and national policies on urban planning and design impact neighbourhood walkability, public transport, and public amenities for recreation [11].
To address the issue of obesity, the World Health Organization (WHO) [15,16,17] proposes comprehensive population-wide policy actions and plans for member states, aimed at changing obesogenic environments to provide opportunities for healthy food choices and increased physical activity at the school, home, workplace, healthcare facilities, community, and population levels. It is the responsibility of governments to provide political leadership and commitment by developing multi-sectoral policies and programmes, given that no single intervention is adequate to meet the prevention and control objectives. This scoping review therefore aimed to examine the nature and range of policies related to overweight/obesity prevention in Africa, and to assess how they align with international guidelines for the prevention of obesity.
2. Materials and Methods
The methodological framework for scoping review proposed by Arksey [18] was adapted to develop the protocol for this review, the details of which are provided elsewhere [19].
2.1. Stage 1: Identifying the Research Questions
Based on the literature, the WHO documents, and in the context of this review, key research questions were derived. These covered investigating policy actions undertaken by African countries to reduce unhealthy diets and physical inactivity to prevent overweight/obesity.
2.2. Stage 2: Identification and Collection of Policy Documents
Briefly, a search of relevant, publicly available national documents on overweight/obesity, health, nutrition, and or non-communicable diseases (NCDs) was undertaken from Google Scholar, WHO websites, and relevant ministries in countries in Africa, using the key words ‘nutrition’, ‘food’, ‘physical activity’ in combination with ‘policy’, guideline’, ‘action plan’, ‘programmes’, ‘strategy,’ ‘regulation’, ‘law’, relating to ‘overweight’, ‘obesity’, and ‘non-communicable diseases’. Additionally, requests were sent to key contacts at the health and education ministries of the countries about existing policy documents. The last search date was 29 April 2019 and covered the period of 2003 to 2019.
2.3. Stage 3: Screening and Selection of Policy Documents
This was done following pre-determined inclusion and exclusion criteria. Documents were included if they were national policies, either adopted and/or at the draft stage; initiatives were being implemented or actions and strategies were proposed, targeted at unhealthy diets and physical inactivity; they formed part of a larger chronic disease prevention strategy to prevent and control overweight/obesity; and were post 2000. No language restrictions were set. Documents that were not national in coverage and reviews of policies were excluded. Where updated duplicate documents were found, the most recent, in terms of the year of production, was included.
2.4. Stage 4: Charting the Data
The documents were reviewed, and a standardised form was used to extract data on the nature of policies, e.g., title of document, type (policies, programmes, strategic plans or strategies, and action plans), year of publication or production and status (whether documents had official signatories, or at the draft stage), and coverage, such as policies to increase fruit and vegetable intake, limit the intake of fat and sugar, and promote physical activity.
2.5. Stage 5: Collating, Summarising, and Reporting the Results
For the purposes of this review, policy refers to all documents regardless of the type, and includes policies, programmes, strategic plans or strategies, and action plans. The policies were categorised using the Analysis Grid for Environments Linked to Obesity (ANGELO) framework [20], commonly used for understanding the obesogenic environment. The ANGELO framework was first applied by Swinburn et al. [20] to study the environmental determinants of obesity in some Pacific Island communities with the highest rates of overweight and obesity globally. The framework categorises the environmental drivers of obesity into four domains (physical, economic, legislative, and socio-cultural). The drivers are further divided into two scales: macro (national, regional, sectors, food industries, media, etc.) and micro (households, institutions, and community). While policies at the micro level are context specific, the macro-level policies are necessary to ensure effectiveness and sustainability at the population level.
The physical environment refers to the availability of facilities, built environment, training opportunities, nutrition and exercise expertise, and information. Economic environment relates to monetary considerations associated with diet and physical activity, including taxes and incentives. Legislative environment comprises rules and regulations, guidelines, and policy messages on diet and physical activity. Socio-cultural refers to attitudes, beliefs, culture, and social norms relating to diet and physical activity; Table 1. Based on the contents of these documents, the policy actions on diet and physical activity were manually mapped. Those policy actions that were context specific were assigned to one of the four domains under micro scale. Likewise, all policies that were targeted at the general population were categorised as macro. The results are presented by the settings, key policy interventions, policy domains, scale, and by country.
Table 1.
Analysis grid for environments linked to obesity (ANGELO).
| Macro-Environment, Diet-Related and Physical Activity-Related (National, Regional, Sectors, Food Industries, Media, etc.) |
Micro-Environment, Diet-Related and Physical Activity (Homes, Schools, Community Groups, Food Retailers, etc.) |
|
|---|---|---|
| Physical | What is available? Example: facilities, built environment, training opportunities, nutrition and exercise expertise, information. | |
| Economic | What are the monetary cost/factor influences and consequences? Example: taxes and subsidies. | |
| Legislative | What are the statutory provisions, rules and legal guidance, policy messages? | |
| Socio-cultural | What are the attitudes, beliefs, perceptions, and values? | |
Adapted from Swinburn et al. (1999) [20].
2.6. Ethics Consideration
Ethics approval was not required since the study did not involve the collection of primary data. The results are based on data from publicly available documents.
3. Results
3.1. Description of Policy Documents
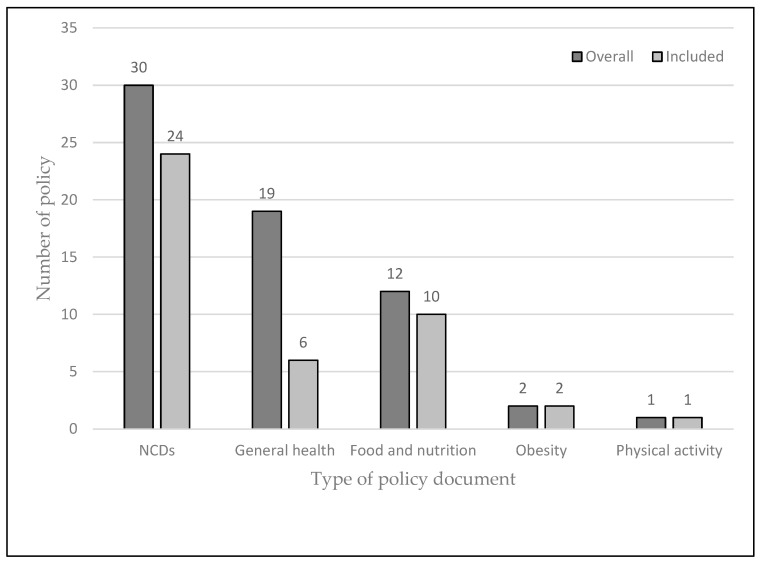
The searches resulted in 87 documents from 54 African countries. Out of this, 64 documents were reviewed, and 43 documents from 41 countries were included in this study (Figure 1, Supplementary Table S1). After initial searches, it became apparent that many countries did not have standalone policies on obesity prevention, so the searches were modified to focus on NCDs. Thirty (46.9%) of the retrieved documents were on NCDs [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50], 19 (29.7%) on general health [51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69], 12 (18.8%) on nutrition [42,70,71,72,73,74,75,76,77,78,79,80], 2 (3.1%) on obesity [81,82], and 1 (1.5%) on physical activity [83]. In addition to the obesity and physical activity policies, 24 on NCDs, 6 on general health, and 10 on food and nutrition were included. Furthermore, these documents were described as policies, strategies, strategic plans, or action plans. Thirteen countries, namely, Burundi, Cape Verde, Comoros Island, Democratic Republic of Congo, Djibouti, Eritrea, Mali, Sao Tome et Principe, Senegal, Somali, South Sudan, Sudan, and Uganda [27,32,38,50,54,55,61,62,63,64,67,69,73], did not detail policy measures to address unhealthy diets and physical inactivity, although the policies underscored the importance of these risk factors. Table 2 summarises the key policy actions identified in the reviewed documents.
Figure 1.
National policies reviewed, overall and included.
Table 2.
Categorisation of key policy interventions related to unhealthy diets, physical inactivity, and overweight/obesity prevention.
| Policy intervention | Environment | Country | |
|---|---|---|---|
| Micro-scale | |||
| School | |||
| Nutrition and diet-related | Provision of healthy school meals (provision of, and access to like fruits and vegetables) | Physical/ Legislative |
Algeria, Benin, Botswana, Chad, Egypt, Gabon, Ghana, Guinea-Bissau, Kenya, Liberia, Mauritius, Morocco, Mozambique, Seychelles, South Africa, Tanzania, Tunisia, Zambia |
| Promotion of school vegetable gardens | Legislative | Algeria, Burkina Faso, Gabon, Guinea-Bissau, Rwanda, Tunisia. | |
| Restricting marketing of unhealthy foods and beverages | Legislative | Algeria, Ghana, Mauritius, South Africa, Tunisia | |
| Food supply near schools (limits on refined sugars, fats, and salt | Legislative | Algeria, South Africa | |
| Strengthen nutrition education | Legislative/Sociocultural | Algeria, Angola, Botswana, Burkina Faso, Cameroon, Egypt, Gabon, Gambia, Ghana, Guinea-Bissau, Guinea, Kenya, Liberia, Madagascar, Mauritius, Morocco, Rwanda, Seychelles, Sierra Leone, South Africa, Tanzania, Tunisia | |
| Professional development for teachers and school canteen staff, etc. | Physical/ Sociocultural |
Algeria, Burkina Faso, Guinea-Bissau, Tanzania |
|
| Monitoring of BMI | Legislative | Algeria, Botswana, Zambia | |
| Physical activity | Mandatory/strengthen physical education and activity in the curriculum | Legislative/Sociocultural | Algeria, Angola, Botswana, Chad, Egypt, Ghana, Guinea-Bissau, Kenya, Lesotho, Liberia, Madagascar, Mauritius, Morocco, Sierra Leone, Seychelles, South Africa, Togo, Tunisia, Zambia |
| After-school physical activity programmes | Physical/ Legislative |
Mauritius, Seychelles | |
| Provision of, and access to adequate recreational facilities | Physical | Angola, Algeria, Benin, Botswana, Chad, Egypt, Ethiopia, Mauritius, Nigeria, Seychelles, South Africa, Tanzania, Tunisia | |
| Promote and support active transport | Physical/ Legislative |
Algeria, Ethiopia, Mauritius, Seychelles, South Africa | |
| Professional development/trained instructors for school staff including PE teachers and school doctors | Physical/ Sociocultural |
Algeria, Liberia, Mauritius | |
| Family | Educational materials/programmes/sensitisation to promote healthy lifestyles | Physical/ Sociocultural |
Algeria, Burkina Faso, Ghana, Guinea-Bissau, Liberia, Tunisia |
| Promotion of breastfeeding | Physical/ Legislative/Sociocultural |
Algeria, Botswana, Cameroon, Chad, Egypt, Gabon, Gambia, Guinea-Bissau, Kenya, Liberia, Malawi, Mauritania, Mauritius, Morocco, Namibia, Nigeria, Rwanda, Seychelles, South Africa, Togo, Zambia, Zimbabwe | |
| Promotion of vegetable gardens | Physical/ Sociocultural |
Lesotho, Mauritius, South Africa | |
| Community | Provision of, and access to adequate recreational facilities | Physical/Legislative | Algeria, Benin, Cameroon, Cote d’Ivoire, Gambia, Ghana, Guinea, Madagascar, Mauritius, Nigeria, Sierra Leone, South Africa, Togo, Tunisia, Zambia |
| Provision of, and access to safe walking paths, cycling lanes, public transport, etc. | Physical/ Legislative |
Angola, Algeria, Botswana, Congo, Chad, Egypt, Ghana, Madagascar, Mauritius, Morocco, Nigeria, Seychelles, Sierra Leone, South Africa, Togo, Zambia | |
| Physical activity clubs/organisation of games and sports | Sociocultural | Algeria, Botswana, Egypt, Chad, Ghana, Guinea-Bissau, Mauritius, South Africa, Togo, Tunisia | |
| Health promotion/awareness campaigns of healthy lifestyles (healthy foods/physical activity) | Legislative/ Sociocultural |
Angola, Algeria, Benin, Burkina Faso, Cote d’Ivoire, Chad, Central African Republic, Egypt, Ethiopia, Gabon, Gambia, Ghana, Guinea-Bissau, Guinea, Kenya, Lesotho, Liberia, Madagascar, Malawi, Mauritania, Mauritius, Morocco, Namibia, Niger, Nigeria, Seychelles, Sierra Leone, South Africa, Swaziland, Tanzania, Togo, Zambia, Zimbabwe | |
| Financial incentives for healthy lifestyle (rewards for active transport) | Economic | Botswana, Ghana, Tunisia, | |
| Production, provision of, and access to healthy foods like fruits and vegetables | Physical/ Sociocultural/ Legislative |
Benin, Chad, Congo, Cote d’Ivoire, Ethiopia, Guinea-Bissau, Guinea, Liberia, Madagascar, Mauritius, Seychelles, South Africa, Togo | |
| Role models for physical activity | Sociocultural | Ghana, Mauritius, South Africa, Tunisia | |
| Macro-scale | |||
| Health promotion/awareness campaigns of healthy lifestyles (healthy foods/physical activity) | Legislative/ Sociocultural |
Angola, Algeria, Benin, Burkina Faso, Cote d’Ivoire, Chad, Central African Republic, Egypt, Ethiopia, Gabon, Gambia, Ghana, Guinea-Bissau, Guinea, Kenya, Lesotho, Liberia, Madagascar, Malawi, Mauritania, Mauritius, Morocco, Namibia, Niger, Nigeria, Seychelles, Sierra Leone, South Africa, Swaziland, Tanzania, Togo, Zambia, Zimbabwe | |
| Educational material/training relevant stakeholders for healthy lifestyles e.g., consumers, food manufacturers, NGO, etc. | Physical/ Sociocultural |
Algeria, Cameroon, Chad, Egypt, Gabon, Ghana, Mauritius, Morocco, Seychelles, South Africa, Tunisia | |
| Financial incentives for healthy lifestyle (e.g., subsidies on sports equipment and bicycles | Economic | Botswana, Ghana, Tunisia | |
| National physical activity guidelines/plans | Legislative | Cote d’Ivoire, Egypt, Ethiopia, Ghana, Mauritius, Nigeria, Seychelles, South Africa, Zambia | |
| Provision of, and access to adequate recreational facilities | Physical/Legislative | Benin, Chad, Congo, Cote d’Ivoire, Ethiopia, Guinea-Bissau, Guinea, Liberia, Madagascar, Mauritius, Seychelles, South Africa, Togo | |
| Food taxes and subsidies to promote healthier diets | Economic | Botswana, Chad, Egypt, Ethiopia, Ghana, Guinea, Kenya, Lesotho, Liberia, Mauritius, Morocco, Seychelles, South Africa | |
| Marketing of unhealthy foods and beverages especially to children | Legislative | Algeria, Botswana, Egypt, Ghana, Guinea-Bissau, Kenya, Mauritius, Morocco, Nigeria, Seychelles, South Africa | |
| Food and nutrition labelling | Sociocultural/ Legislative |
Algeria, Egypt, Ethiopia, Ghana, Kenya, Mauritius, Morocco, Namibia, Nigeria, Seychelles, South Africa, Tunisia, Zambia | |
| Production, provision of, and access to healthy foods like fruits and vegetables | Physical/ Sociocultural/ Legislative |
Benin, Chad, Congo, Cote d’Ivoire, Ethiopia, Guinea-Bissau, Guinea, Liberia, Madagascar, Mauritius, Seychelles, South Africa, Togo | |
| Regulation of sugars, fats, and salt in processed foods | Legislative/ Sociocultural |
Benin, Botswana, Congo, Cote d’Ivoire, Chad, Egypt, Ghana, Kenya, Madagascar, Morocco, Nigeria, Seychelles, South Africa, Zambia |
3.2. Key Policy Interventions at the Micro Scale (School, Family and Community)
These included the provision of healthy school meals, promotion of school vegetable gardens, marketing of unhealthy food and beverages in and around the school, integration of the concepts of nutrition and heathy eating in the curricula, professional development for teachers, canteen staff and school doctors, and monitoring of body mass index (BMI).
The majority (51.2%) of the documents outlined actions to strengthen nutrition education of children. The provision of healthy school meals was addressed in 18 countries. For example, Botswana, Kenya, Nigeria, Guinea-Bissau, and Liberia targeted healthy school meals as a component of the school health programme [22,35,40,74,84]; Algeria and Seychelles specified the free distribution of fruits and drinking water fountains [21,43]; and others, including Benin and Ghana, proposed the mandatory inclusion of fruits and vegetables in the school menu [23,33]. The promotion of vegetable gardens was specified by six countries [21,42,74,75,76,81], while Algeria [21], and South Africa [82] targeted regulations on the sugar, fat, and salt content of food sold near schools. Monitoring the BMI of children [21,22,48], professional development for staff [21,46,74,76], and marketing of unhealthy foods [21,33,70,81,82] were addressed in three, four and five country documents, respectively.
The promotion and strengthening of mandatory physical education and or physical activity in the curriculum as strategies to promote physical activity was mentioned by 19 countries, including Algeria [21], Botswana [22], Chad [26], Ghana [33], Seychelles [43], Nigeria [40], and South Africa [82]. Two countries, Mauritius [83] and Seychelles [43], stated the organising of after-school physical activity programmes by setting up health clubs, among other measures. Again, about a third [21,22,23,26,30,31,40,43,46,51,81,82,83] outlined the provision and access to adequate recreational facilities to promote active play. Algeria [21], Ethiopia [31], Mauritius [83], Seychelles [43], and South Africa [82] proposed strategies to promote and support active transport. Professional development and or trained instructors for school staff, including physical education teachers and school doctors was the focus of Algeria [21], Liberia [78], and Mauritius [83].
3.2.1. Family
The key policy actions at the family level were the provision of educational materials and programmes, sensitisation to promote healthy lifestyles, promotion of breastfeeding, and home vegetable gardens. Nearly one-half of the countries, including Liberia, Mauritius, Morocco, Namibia, Seychelles, and South Africa, addressed the promotion of adequate infant and young child feeding, including exclusive breastfeeding with continued breastfeeding and adequate complementary feeding. Lesotho [36], Mauritius [70] and South Africa [82] addressed the promotion of home vegetable gardens, while Algeria [21], Burkina Faso [76], Ghana [33], Guinea-Bissau [74], Liberia [78], and Tunisia [81] targeted the sensitisation of parents to healthy diets and the importance of physical activity for health.
3.2.2. Community
The majority targeted health promotion and awareness campaigns for healthy lifestyles. Botswana [22], Ghana [33] and Tunisia [81] proposed financial incentives for healthy lifestyles, such as rewards for active transport. Ghana, Mauritius, South Africa, Tunisia proposed the role models for physical activity. Ten countries proposed policy measures on the formation of private and public physical activity clubs, organisation of games and sports, and development of physical activity programmes. Thirteen countries proposed the production of and access to healthy foods, such as fruits and vegetables, through community initiatives.
3.3. Key Policy Interventions at the Macro-Scale
The policy measures at the macro-level included the production, provision, and access to healthy foods, such as fruits and vegetables; health promotion; regulation of processed foods; regulation of marketing of unhealthy foods and beverages; fiscal policies; development, implementation and strengthening of transport policies to improve the built and natural environments; and national physical activity guidelines. By targeting the food industry, 14 countries, including Benin, Botswana, Cote d’Ivoire, Egypt, Kenya, Morocco, Nigeria, Seychelles, and South Africa, outlined policy actions on the regulation of sugars, fats, and salt in processed foods. Furthermore, regulation of the marketing of unhealthy foods and beverages, especially to children, was addressed in 11 countries [21,22,30,33,35,40,43,49,70,74,82].
Thirteen countries [22,26,30,31,33,34,35,36,43,49,59,82,84] stated fiscal policies to promote healthier diets and discourage unhealthy diets. For instance, the sugar tax was one such strategy by South Africa [82] and Mauritius [59], while Liberia [84] and Egypt [30] mentioned the taxation of sugar-sweetened beverages in general. Other countries stated that subsidies would be introduced to promote the production and accessibility of fruits and vegetables. For example, Lesotho [36] specified the exemption of fruits and vegetables from taxation, while Guinea [34] proposed subsidies on local production of fruits and vegetables. Additionally, 13 countries [21,30,31,33,35,40,43,48,49,70,72,81,82] highlighted food and nutrition labelling through point of sale, product package, and front of pack labelling to provide adequate nutrition information to the consumer.
Several strategies were outlined to promote physical activity. The strengthening and implementation of transport policies to improve the built and natural environments were the main strategies outlined in 31 countries. The provision of and access to adequate recreational facilities to promote active play was addressed in 15 countries, including Algeria [21], Benin [23], Cote d’Ivoire [29], Ghana [33], Madagascar [37], South Africa [82] Togo [47], and Zambia [48]. Furthermore, the availability of safe walking paths, cycling lanes, and public transport were outlined in 16 countries, including Angola, Botswana, Congo, Egypt, Madagascar, Morocco, Nigeria, Seychelles, and Togo. In addition, other countries, including Cote d’Ivoire, Egypt, Ethiopia, Mauritius, Seychelles, and South Africa, outlined the development, strengthening or implementation of national physical activity guidelines and plans. Financial incentives for healthy lifestyles, such as subsidies on sports equipment, was the focus of Botswana [22], Ghana [33] and Tunisia [81].
3.4. Policy Domains
Majority of the policy interventions were legislative, sociocultural, and physical domains at both scales, with only two under the economic domain at the macro level.
4. Discussion
This scoping study was conducted to assess the nature and extent of policies related to overweight/obesity prevention in Africa and to assess how they align with the international guidelines. Despite the absence of standalone policies on obesity prevention—only two—the results highlight the availability of national policies targeted at promoting healthy diets and physical activity on the micro and macro scales. The evidence-based recommended population-based strategies for obesity and NCDs prevention [15,16,17] include interventions to reduce the main shared modifiable risk factors for NCDs. For example, objective 3 of the WHO Action Plan for the Global Strategy for the Prevention and Control of Non-communicable Diseases 2008–2013) proposed actions for Member States include: “promote interventions to reduce the main shared modifiable risk factors including unhealthy diets and physical inactivity”. The strategies involve the provision and promotion of healthy choices, which in the context of this review include policy actions to increase the intake of fruits and vegetables, decrease the intake of sugar-sweetened beverages, and promote physical activity for all through multi-sectoral actions that target multiple settings.
In the current review, the policy measures are generally in alignment with global strategies and recommendations. These documents underscore the importance of multi-sectoral collaborations in creating supportive environments. Many countries have proposed policy initiatives to address unhealthy diets and physical inactivity. The findings from the present review demonstrate a significant improvement relative to the 2013 findings by Lachat and colleagues [85], who observed a low coverage of diet and physical activity policies in African countries. Moreover, there are overlaps and interactions in the application of the framework. Except for the economic domain, the physical, legislative, and sociocultural domains were largely featured.
At the macro level, diet-related economic or fiscal policy initiatives by many governments have had strong opposition, mainly by the food and beverage industry [86,87]. Nonetheless, the evidence from high and low-to-middle income countries demonstrates the feasibility and effectiveness of these initiatives in providing supportive environments. There is considerable evidence that food taxes and subsidies encourage healthy food choices, food preferences and consumption, and subsequent reduction in BMI, obesity, and chronic diseases [13,86,88,89].
In their systematic review of high-income countries, Thow and colleagues [89] found that subsidies on healthy foods increased the purchase and consumption of these foods, particularly fruits and vegetables, by a lower margin relative to the subsidy; however, the overall effect on energy intake was inconsistent [89]. In the same analysis, the taxation of sugar-sweetened beverages reduced the consumption as well as the energy intake of these beverages proportional to the tax component [89]. In another meta-analysis involving France, Brazil, Mexico and the U.S.A. [88], the taxation of sugar-sweetened beverages increased the demand for healthier alternatives, such as milk, and also led to a reduction in the prevalence of overweight and obesity [88]. Limited evidence from Africa indicates that the implementation of the sugar tax, the Health Promotion Levy in 2018 in South Africa, has impacted product reformation, price increase, and reduction in the purchases of sugar-sweetened beverages, especially by low socioeconomic households [90,91].
Nutrition labelling is key to product reformation and provides adequate information to consumers at the point of sale, thereby encouraging healthy food choices. Nutrition labelling comes in variant forms, including front-of-package labelling and the traffic light system. The traffic light system, where the contents of sugar, salt, and total fats of packaged foods are indicated using colours, is recommended as one of the effective strategies in the prevention of obesity. Nutrition labelling may result in increased purchases of healthy food options, which may influence dietary quality [92,93].
Food advertising and marketing, especially to children, may influence their preferences and dietary intake and subsequently their weight status [94,95]. For example, evidence from a systematic review and meta-analysis [95] suggests that acute advertising exposure to unhealthy foods is significantly associated with greater food intake in children, but not in adults.
At the micro-level, food-based guidelines are relevant to ensure appropriate food standards. African countries have explicitly stated policy measures to ensure appropriate food standards in settings such as schools, restaurants, and fast food outlets. Comprehensive school-based health and nutrition policies are related to healthier eating habits, improved physical activity, and decreased rates of obesity. For example, limiting children’s access to foods that are high in fat and sugars and increasing access to healthy alternatives at the school are associated with improved dietary intake [96,97]. Furthermore, menu labelling at restaurants and fast food outlets informs consumers of the energy contents of menu items to make an informed decision at the point of purchase and is related to the purchase of low-calorie food [98].
The main policy interventions to promote physical activity are the provision of and access to adequate recreational facilities to promote active play, and the availability of safe walking paths, cycling lanes, and public transport, among others. Policy interventions at the macro level target the built and natural environments, public transport, access to parks and recreational facilities, and mass media campaigns for attitude and behaviour changes. Mass media campaigns and large-scale public participation events, for example, can be effective when linked to specific programmes, such as urban design and infrastructure, and land use to promote walking and cycling for exercise [99].
At the micro scale, these include recreational facilities at schools, and design features in institutions, communities, and buildings, such as stairways. Point-of-decision prompts, such as health and motivational messages at the base of stairways or the elevator, have shown moderate results, as they serve as reminders [99]. Unless the population is educated about the importance of active living, the availability of these alone might not produce the expected impact.
Addressing the global obesity pandemic through effective implementation of the proposed national policies and programmes is critical in meeting the United Nations Sustainable Development Goals (SDGs) 3 of “good health and well-being to ensure healthy lives and promote well-being at all ages”. It is not adequate to have these policies, as the presence of the documents is not indicative of implementation. The reported impact of obesity on global health, especially in light of the COVID-19 pandemic [100], calls for proactive and concerted actions by all relevant stakeholders, including governments, international partners, civil society, private sector involvement, and non-governmental organisations.
There are strengths of the present study. This is the only study on national policies in African countries that provides information on the available national documents outlining key policy interventions to address unhealthy diets, physical inactivity, and obesity. Other policy analyses have focused on a few selected African countries [101] or implementations of NCD policies [102]. Additionally, an attempt was made to include nearly all African countries, regardless of language. A source of limitation was the limited number of standalone policies on obesity prevention. Another potential limitation could be the categorisation of the key policy interventions at the domains and scales, as some of the initiatives tended to overlap and interact within the framework. Moreover, due to the anticipated volume of available documents, the searches were limited to national documents. Finally, language was another challenge that was addressed by resorting to online language translation services.
5. Conclusions
This study has provided information on the extent and nature of policies and programmes related to overweight and obesity prevention in Africa; it can be useful as a first point of call for policymakers on unhealthy diets, physical inactivity, and obesity policy documents. We found that the policy initiatives broadly align with global strategies and recommendations. The overlapping and interactions in the initiatives demonstrate the importance of multi-sectoral partnerships in providing supportive environments for healthy behaviours. It is recommended that a comprehensive systematic review and impact study of available national policies be conducted; this should include implementation, monitoring and evaluation, where applicable. The results should be made available in a regional repository.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/nu13114028/s1, Table S1: National policy, actions, programmes, and strategies on diet and physical activity to prevent obesity/non-communicable diseases in African countries.
Author Contributions
Conceptualization, T.A., A.P.K.; data curation, T.A., A.P.K.; formal analysis, T.A.; investigation, T.A.; methodology, T.A., A.D.V., A.P.K.; resources, T.A.; supervision, A.P.K., A.D.V., T.P.; writing—original draft preparation, T.A.; writing—review and editing, T.A., A.D.V., T.P., A.P.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO . WHO (2021)–Fact Sheet–Obesity and Overweight. WHO; Geneva, Switzerland: 2021. [Google Scholar]
- 2.Kengne A.P., Bentham J., Zhou B., Peer N., Matsha T.E., Bixby H., Di Cesare M., Hajifathalian K., Lu Y., Taddei C., et al. Trends in obesity and diabetes across Africa from 1980 to 2014: An analysis of pooled population-based studies. Int. J. Epidemiol. 2017;46:1421–1432. doi: 10.1093/ije/dyx078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gona P.N., Kimokoti R.W., Gona C.M., Ballout S., Rao S.R., Mapoma C.C., Lo J., Mokdad A.H. Changes in body mass index, obesity, and overweight in Southern Africa development countries, 1990 to 2019: Findings from the Global Burden of Disease, Injuries, and Risk Factors Study. Obes. Sci. Pract. 2021;7:509–524. doi: 10.1002/osp4.519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Newby P.K. Are dietary intakes and eating behaviors related to childhood obesity? A comprehensive review of the evidence. J. Law. Med. Ethics. 2007;35:35–60. doi: 10.1111/j.1748-720X.2007.00112.x. [DOI] [PubMed] [Google Scholar]
- 5.Hills A.P., Andersen L.B., Byrne N.M. Physical activity and obesity in children. Br. J. Sports Med. 2011;45:866–870. doi: 10.1136/bjsports-2011-090199. [DOI] [PubMed] [Google Scholar]
- 6.Kamath C.C., Vickers K.S., Ehrlich A., McGovern L., Johnson J., Singhal V., Paulo R., Hettinger A., Erwin P.J., Montori V.M. Behavioral interventions to prevent childhood obesity: A systematic review and metaanalyses of randomized trials. J. Clin. Endocrinol. Metab. 2008;93:4606–4615. doi: 10.1210/jc.2006-2411. [DOI] [PubMed] [Google Scholar]
- 7.Harris K.C., Kuramoto L.K., Schulzer M., Retallack J.E. Effect of school-based physical activity interventions on body mass index in children: A meta-analysis. CMAJ. 2009;180:719–726. doi: 10.1503/cmaj.080966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dobbins M., Husson H., Decorby K., Rl L. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst. Rev. 2013:CD007651. doi: 10.1002/14651858.CD007651.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hooper L., Abdelhamid A., Moore H.J., Douthwaite W., Skeaff C.M., Summerbell C.D. Effect of reducing total fat intake on body weight: Systematic review and meta-analysis of randomised controlled trials and cohort studies. BMJ. 2012;345:e7666. doi: 10.1136/bmj.e7666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ledoux T.A., Hingle M.D., Baranowski T. Relationship of fruit and vegetable intake with adiposity: A systematic review. Obes. Rev. 2011;12:143–150. doi: 10.1111/j.1467-789X.2010.00786.x. [DOI] [PubMed] [Google Scholar]
- 11.Friel S., Chopra M., Satcher D. Unequal weight: Equity oriented policy responses to the global obesity epidemic. BMJ. 2007;335:1241–1243. doi: 10.1136/bmj.39377.622882.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thow A.M., Sanders D., Drury E., Puoane T., Chowdhury S.N., Tsolekile L., Negin J. Regional trade and the nutrition transition: Opportunities to strengthen NCD prevention policy in the Southern African Development Community. Glob. Heal. Action. 2015;8:28338. doi: 10.3402/gha.v8.28338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thow A.M., Jan S., Swinburn B. The effect of fiscal policy on diet, obesity and chronic disease: A systematic review. Bull. World Health Organ. 2010;88:609–614. doi: 10.2471/BLT.09.070987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Friel S., Hattersley L., Snowdon W., Thow A.M., Lobstein T., Sanders D., Barquera S., Mohan S., Hawkes C., Kelly B., et al. Monitoring the impacts of trade agreements on food environments. Obes. Rev. 2013;14:120–134. doi: 10.1111/obr.12081. [DOI] [PubMed] [Google Scholar]
- 15.WHO . Report of the Commission on Ending Childhood Obesity. WHO; Geneva, Switzerland: 2016. [Google Scholar]
- 16.WHO . Global Strategy on Diet, Physical Activity and Health. Volume 8. WHO; Geneva, Switzerland: 2004. pp. 1–21. [Google Scholar]
- 17.WHO . Action Plan for the Global Strategy for the Prevention and Control of Noncommunicable Diseases 2008–2013. WHO; Geneva, Switzerland: 2008. p. 35. [Google Scholar]
- 18.Arksey H., O’Malley L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. Theory Pract. 2005;8:19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 19.Adom T., Puoane T., De Villiers A., Kengne A.P. Protocol for a scoping review of existing policies on the prevention and control of obesity across countries in Africa. BMJ Open. 2017;7:e013541. doi: 10.1136/bmjopen-2016-013541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Swinburn B., Egger G., Raza F. Dissecting Obesogenic Environments: The Development and Application of a Framework for Identifying and Prioritizing Environmental Interventions for Obesity 1. Prev. Med. (Baltim) 1999;29:563–570. doi: 10.1006/pmed.1999.0585. [DOI] [PubMed] [Google Scholar]
- 21.Algeria . Plan Strategique National Multisectoriel de Lutte Integree Contre les Facteurs de Risque des Maladies Non Transmissibles 2015–2019. Ministere de la Sante, de la Population et de la Reforme Hospitaliere; El Madania, Algeria: 2015. [Google Scholar]
- 22.Botswana . Botswana National Multisectoral Strategy for the Prevention and Control. of Non-Communicable Diseases. Ministry of Health and Wellness; Gaborone, Botswana: 2017. [Google Scholar]
- 23.Benin . Plan Strategique Integre de Lutte Contre les Maladies Non Transmissibles 2014–2018. Ministère de la Santé; Porto-Novo, Benin: 2014. [Google Scholar]
- 24.Burkina Faso . Plan Strategique Integre de Lutte Contre les Maladies Non Transmissibles Plan Strategique Integre de Lutte Contre les Maladies Non Transmissibles 2016–2020. Ministère de la Santé; Ouagadougou, Burkina Faso: 2016. [Google Scholar]
- 25.Central African Republic . Document de Politique Nationale de Prevention et de Lutte Contre les Maladies Non Transmissibles. Ministere de la Sante Publique, des Affaires Sociale, de la Promotion du Genre et de L’action Humanitaire; Bangui, Central African Republic: 2014. [Google Scholar]
- 26.Tchad . Plan Multisectoriel de Maladies Non Transmissibles 2017–2021. Ministère de la Santé; N’Djamena, Tchad: 2017. [Google Scholar]
- 27.Des Comores U. Document de Stratégie Nationale de Prévention et de Lutte Contre les Maladies Non Transmissibles. Ministere de Santé, de la Cohésion Ministère de la Santé, de la Solidarité, de la Cohésion Sociale et de la Promotion du Genre; Moroni, Comoros: 2013. [Google Scholar]
- 28.Congo . Plan National Integré de Lutte Contre les Maladies Non Transmissibles au Congo 2013–2017. Ministere de la Sante et de la Population; Goma, Congo: 2013. [Google Scholar]
- 29.Côte d’Ivoire . Plan Stratégique Intégré de Prévention et de Prise en Charge des Maladies Non Transmissibles en Côte d’Ivoire 2015–2019. Ministère de la Santé et de la Lutte contre le Sida; Yamoussoukro, Côte D’ivoire: 2014. [Google Scholar]
- 30.Egypt. WHO . Egypt Multisectoral Action Plan for Noncommunicable Diseases Prevention and Control 2018–2022. Ministry of Health and Population; Cairo, Egypt: 2018. [Google Scholar]
- 31.Ethiopia . Ethiopia_National Strategic Action Plan. (NSAP) for Prevention and Control of Non-Communicable Diseases-Final 2014–2016. Ministry of Health; Ababa, Ethiopia: 2014. [Google Scholar]
- 32.Eritrea . Non-Communicable Diseases Policy. Ministry of Health; Asmara, Eritrea: 2008. [Google Scholar]
- 33.Ghana . Strategy for the Management, Prevention and Control of Chronic Non-Communicable Diseases in Ghana. Ministry of Health; Accra, Ghana: 2016. [Google Scholar]
- 34.Guinée . Programme National Intégré de Prévention et de Contrôle des Maladies Non Transmissibles. Ministère de la Santé et de l’hygiène Publique; Conakry, Guinée: 2010. [Google Scholar]
- 35.Kenya . Kenya National Strategy for the Prevention and Control of Non-Communicable Diseases 2015–2020. Ministry of Health; Nairobi, Kenya: 2015. [Google Scholar]
- 36.Lesotho . National Multi-Sectoral Integrated Strategic Plan for the Prevention and Control of Non-Communicable Diseases (NCDS): 2014–2020. Ministry of Health; Maseru, Lesotho: 2017. [Google Scholar]
- 37.Madagascar . Politique Nationale de Prévention et Lutte Intégrées contre les Maladies Chroniques Non Transmissibles. World Health Organization (WHO); Geneva, Switzerland: Ministère de la Santé Publique; Antananarivo, Madagascar: 2013. [Google Scholar]
- 38.Mali . Politique Nationale de Lutte Contre les Maladies Non Transmissibles. Ministère de la Santé; Bamako, Mali: 2013. [Google Scholar]
- 39.Moçambique . Plano Estratégico Nacional de Prevenção e Controlo das Doenças não Transmissíveis para Período de 2008–2014. Ministry of Health National Directorate of Public Health Department of Non-Communicable Diseases; Maputo, Mozambique: 2008. [Google Scholar]
- 40.Nigeria . National Policy and Strategic Plan of Action on Non-Communicable Diseases. Federal Ministry of Health; Abuja, Nigeria: 2013. [Google Scholar]
- 41.Niger . Politique et Plan Strategique Integre de Lutte Contre les Maladies Non Transmissibles (Psimnt) 2012–2015. Ministère de la Santé Publique; Niamey, Niger: 2012. [Google Scholar]
- 42.Rwanda . National Food and Nutrition Policy 2013–2018. Social Cluster Ministries; Kigali, Rwanda: 2013. [Google Scholar]
- 43.Seychelles . Strategy for the Prevention and Control of Non-Communicable Diseases, 2016–2025. Ministry of Health; Victoria, Seychelles: 2016. [Google Scholar]
- 44.Sierra Leone . National Non-Communicable Diseases Strategic Plan. Ministry of Health and Sanitation; Freetown, Sierra Leone: 2013. [Google Scholar]
- 45.Swaziland . National Non Communicable Diseases Prevention and Control. Ministry of Health; Geneva, Swaziland: WHO; Geneva, Swaziland: 2016. [Google Scholar]
- 46.Tanzania . Strategic Action Plan for Prevention and Control of Non communicable Diseases in Tanzania 2016–2020. Ministry of Health, Community Development, Gender, Elderly and Children; Dodoma, Tanzania: 2016. [Google Scholar]
- 47.Togo . Politique et Plan Strategique Integre de Lutte Contre les Maladies Non Transmissibles (PSIMNT) 2012–2015. Ministere de la Sante; Lome, Togo: 2012. [Google Scholar]
- 48.Zambia . Zambian Strategic Plan 2013–2016 Non-Communicable Diseases and Their Risk Factors Version 1. Ministry of Health; Lusaka, Zambia: 2016. [Google Scholar]
- 49.Maroc . Stratégie Multisectorielle de Prévention et de Contrôle des Maladies Non Transmissibles 2016–2025. Ministre de la Santé, l’Organisation Mondiale de la Santé; Rabat, Maroc: 2016. [Google Scholar]
- 50.Burundi . Plan Strategique Multisectoriel de Securite Alimentaire et Nutritionnelle (PSMSAN) 2014–2017. 2ève Vice-Presidence de la Republique; Gitega, Burundi: 2014. [Google Scholar]
- 51.Angola . Plano Nacional de Desenvolvimento Sanitário 2012–2025 (PNDS) Volume 1 Ministério da Saúde; Luanda, Angola: 2014. [Google Scholar]
- 52.Burundi . National Health Development Plan. Volume 151 Ministry of Public Health and Fighting AIDS; Gitega, Burundi: 2015. [Google Scholar]
- 53.Cameroun . Plan National de Développement Sanitaire, PNDS 2016–2020. Ministere de Santé, de la Cohésion Ministère de la Santé Publique; Yaounde, Cameroun: 2016. [Google Scholar]
- 54.Cabo Verde . Plano Nacional de Desenvolvimento Sanitário 2012–2016. Ministério da Saúde; Praia, Cabo Verde: 2012. [Google Scholar]
- 55.Djibouti . Plan National de Developpment 2013–2015. Ministere de la Sante; Djibouti-Ville, Djibouti: 2013. [Google Scholar]
- 56.Gambia . The Gambia National Health Sector Strategic Plan. Ministry of Health and Social Welfare; Banjul, Gambia: 2014. [Google Scholar]
- 57.Malawi . Health Sector Strategic Plan. II (2017–2022) Ministry of Health; Lilongwe, Malawi: 2017. [Google Scholar]
- 58.Mauritanie . Plan National de Developpement Sanitaire 2012–2020. Ministere de Santé; Nouakchott, Mauritanie: 2012. [Google Scholar]
- 59.East Africa . Mauritius Draft Health Sector Strategy 2017–2021. Ministry of Health and Quality of Life; Port Louis, Mauritius: 2017. [Google Scholar]
- 60.Namibia . Namibian National Health Policy Framework. Ministry of Health and Social National Services; Windhoek, Namibia: 2010. [Google Scholar]
- 61.São Tomé et Príncipe . Plano Nacional do Desenvolvimento da Saúde 2017–2021. Ministério da Saúde; São Tomé, São Tomé et Príncipe: 2017. [Google Scholar]
- 62.Senegal . Plan National de Developpement Sanitaire PNDS 2009–2018. Ministere de la Sante et de la Prevention; Dakar, Senegal: 2009. pp. 1–86. [Google Scholar]
- 63.Somali . Health Sector Strategic Plan January 2013–December 2016. Ministry of Human Development and Public Services; Hargeysa, Somali: 2013. [Google Scholar]
- 64.Sudan . 25 Years Strategic Plan for Health Sector. Ministry of Health; Khartoum, Sudan: 2003. [Google Scholar]
- 65.Uganda . Health Sector Development Plan 2015/16–2019/20. Ministry of Health; Kampala, Uganda: 2015. [Google Scholar]
- 66.Zimbabwe . The National Health Strategy for Zimbabwe 2016–2020. Ministry of Health and Child Care; Harare, Zimbabwe: 2016. [Google Scholar]
- 67.South Sudan . The Republic of South Sudan Policy Framework 2013–2016. Ministry of Health; Juba, South Sudan: 2013. [Google Scholar]
- 68.Somaliland . Somaliland National Health Policy. Ministry of Health; Hargeisa, Somaliland: 2011. pp. 1–48. [Google Scholar]
- 69.Democratic Republic of the Congo . Plan National de Developpement Sanitaire 2016–2020. Ministere de la Sante Publique; Goma, Democratic Republic of the Congo: 2016. [Google Scholar]
- 70.Mauritius . Plan of Action for Nutrition 2009–2010. Ministry of Health and Quality of Life; Port Louis, Mauritius: 2009. [Google Scholar]
- 71.Sierra Leone . National Food and Nutrition Security Policy 2012–2016. Ministry of Health and Sanitation; Freetown, Sierra Leone: 2012. [Google Scholar]
- 72.Namibia . Strategic Plan for Nutrition 2011–2015. Ministry of Health and Social Services; Windhoek, Namibia: 2014. [Google Scholar]
- 73.Uganda . Nutrition Action Plan 2011–2016. Government of Uganda; Kampala, Uganda: 2011. [Google Scholar]
- 74.Guinee-Bissau . Politique Nationale de Nutrition 2015–2019. Ministère de la Santé Publique; Bissau, Guinee-Bissau: 2014. [Google Scholar]
- 75.Gabon . Politique Nationale de Securite Alimentaire et Nutritionnelle (PNSAN) 2017–2025. Ministère de l’Agriculture, de l’elevage, Chargé de la Mise en œuvre du Programme Graine; Libreville, Gabon: 2017. [Google Scholar]
- 76.Burkina Faso . National Nutrition Policy (Politique Nationale de Nutrition) Ministère de la Santé; Ouagadougou, Burkina Faso: 2016. [Google Scholar]
- 77.Cameroun . Politique Nationale de Nutrition 2012–2021. Ministère de la Santé Publique; Yaounde, Cameroun: 2006. [Google Scholar]
- 78.Liberia . National Food Security and Nutrition Strategy Government of Liberia. Ministry of Agriculture; Monrovia, Liberia: 2008. [Google Scholar]
- 79.Republique de Madagascar . Plan National d’Action Pour la Nutrition (PNAN III 2017–2021) Ministere de Sante; Antananarivo, Madagascar: 2017. [Google Scholar]
- 80.Malawi . National Multi-Sector Nutrition Policy 2018–2022. Department of Nutrition HIV and AIDS; Lilongwe, Malawi: 2018. [Google Scholar]
- 81.Tunisia . Stratégie de Prévention et de lutte Contre L’obésité 2013–2017. Ministère de la Santé; Tunis, Tunisia: 2014. [Google Scholar]
- 82.South Africa . Strategy for the Prevention and Control of Obesity. Department of Health; Pretoria, South Africa: 2015. [Google Scholar]
- 83.Mauritius . National Action Plan on Physical Activity 2011–2014. Ministry of Health and Quality of Life; Port Louis, Mauritius: 2011. [Google Scholar]
- 84.Liberia . National Policy and Strategic Plan on Health Promotion. Ministry of Health; Monrovia, Liberia: WHO; Geneva, Switzerland: 2016. [Google Scholar]
- 85.Lachat C., Otchere S., Roberfroid D., Abdulai A., Maria F., Seret A., Milesevic J., Xuereb G., Candeias V., Kolsteren P. Diet and Physical Activity for the Prevention of Noncommunicable Diseases in Low- and Middle-Income Countries: A Systematic Policy Review. PLoS Med. 2013;10:e1001465. doi: 10.1371/journal.pmed.1001465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Pérez-Escamilla R., Lutter C., Rabadan-Diehl C., Rubinstein A., Calvillo A., Corvalán C. Prevention of childhood obesity and food policies in Latin America: From research to practice. Obes. Rev. 2017;18:28–38. doi: 10.1111/obr.12574. [DOI] [PubMed] [Google Scholar]
- 87.Margetts B. Editorial. Public Health Nutr. 2004;7:361–363. doi: 10.1079/PHN2004622. [DOI] [PubMed] [Google Scholar]
- 88.Thow A.M., Downs S., Jan S. A systematic review of the effectiveness of food taxes and subsidies to improve diets: Understanding the recent evidence. Nutr. Rev. 2014;72:551–565. doi: 10.1111/nure.12123. [DOI] [PubMed] [Google Scholar]
- 89.Escobar M.A.C., Veerman J.L., Tollman S.M., Bertram M.Y., Hofman K.J. Evidence that a tax on sugar sweetened beverages reduces the obesity rate: A meta-analysis. BMC Public Health. 2013;13:1–10. doi: 10.1186/1471-2458-13-1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Stacey N., Mudara C., Ng S.W., van Walbeek C., Hofman K., Edoka I. Sugar-based beverage taxes and beverage prices: Evidence from South Africa’s Health Promotion Levy. Soc. Sci. Med. 2019;238:112465. doi: 10.1016/j.socscimed.2019.112465. [DOI] [PubMed] [Google Scholar]
- 91.Stacey N., Edoka I., Hofman K., Swart E.C., Popkin B., Ng S.W. Changes in beverage purchases following the announcement and implementation of South Africa’s Health Promotion Levy: An observational study. Lancet Planet. Health. 2021;5:e200–e208. doi: 10.1016/S2542-5196(20)30304-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Miller S.L.M., Cassady D.L., Applegate E.A., Beckett L.A., Wilson M.D., Gibson T.N., Ellwood K. Relationships among Food Label Use, Motivation, and Dietary Quality. Nutrients. 2015;7:1068–1080. doi: 10.3390/nu7021068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Cecchini M., Warin L. Impact of food labelling systems on food choices and eating behaviours: A systematic review and meta-analysis of randomized studies. Obes. Rev. 2016;17:201. doi: 10.1111/obr.12364. [DOI] [PubMed] [Google Scholar]
- 94.Sadeghirad B., Duhaney T., Motaghipisheh S., Campbell N.R.C., Johnston B.C. Influence of unhealthy food and beverage marketing on children’s dietary intake and preference: A systematic review and meta-analysis of randomized trials. Obes. Rev. 2016;17:945–959. doi: 10.1111/obr.12445. [DOI] [PubMed] [Google Scholar]
- 95.Boyland E.J., Nolan S., Kelly B., Tudur-Smith C., Jones A., Halford J.C.G., Robinson E. Advertising as a cue to consume: A systematic review and meta-analysis of the effects of acute exposure to unhealthy food and nonalcoholic beverage advertising on intake in children and adults. Am. J. Clin. Nutr. 2016;103:519–533. doi: 10.3945/ajcn.115.120022. [DOI] [PubMed] [Google Scholar]
- 96.Mansfield J.L., Savaiano D.A. Effect of school wellness policies and the Healthy, Hunger-Free Kids Act on food-consumption behaviors of students, 2006–2016: A systematic review. Nutr. Rev. 2017;75:533–552. doi: 10.1093/nutrit/nux020. [DOI] [PubMed] [Google Scholar]
- 97.Micha R., Karageorgou D., Bakogianni I., Trichia E., Whitsel L.P., Story M., Peñalvo J.L., Mozaffarian D. Effectiveness of school food environment policies on children’s dietary behaviors: A systematic review and meta-analysis. PLoS ONE. 2018;13:1–27. doi: 10.1371/journal.pone.0194555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Littlewood J.A., Lourenço S., Iversen C.L., Hansen G.L. Menu labelling is effective in reducing energy ordered and consumed: A systematic review and meta-analysis of recent studies. Public Health Nutr. 2016;19:2106–2121. doi: 10.1017/S1368980015003468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Heath G.W., Parra D.C., Sarmiento O.L., Andersen L.B., Owen N., Goenka S., Montes F., Brownson R.C., Alkandari J.R., Bauman A.E., et al. Evidence-based intervention in physical activity: Lessons from around the world. Lancet. 2012;380:272–281. doi: 10.1016/S0140-6736(12)60816-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Helvaci N., Eyupoglu N.D., Karabulut E., Yildiz B.O. Prevalence of Obesity and Its Impact on Outcome in Patients With COVID-19: A Systematic Review and Meta-Analysis. Front. Endocrinol. (Lausanne) 2021;12:598249. doi: 10.3389/fendo.2021.598249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Juma P.A., Mohamed S.F., Mwagomba B.L.M., Ndinda C., Mapa-tassou C., Oluwasanu M., Oladepo O., Abiona O., Nkhata M.J., Wisdom J.P., et al. Non-communicable disease prevention policy process in five African countries. BMC Public Health. 2018;18:961. doi: 10.1186/s12889-018-5825-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Nyaaba G.N., Stronks K., Aikins A.D.-G., Kengne A.P., Agyemang C. Tracing Africa’s progress towards implementing the Non-Communicable Diseases Global action plan 2013–2020: A synthesis of WHO country profile reports. BMC Public Health. 2017;17:1–13. doi: 10.1186/s12889-017-4199-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.