Abstract
Open transosseous repair was historically considered the gold-standard surgical solution for rotator cuff tears; however, with advancements in arthroscopic surgery, this procedure was largely replaced by anchor-based techniques. Yet, the ability of anchor-based techniques to achieve similar biomechanical fixation remains uncertain.
In this article, we describe a reproducible, economical, arthroscopic anchorless transosseous rotator cuff repair technique that uses an Omega configuration. This technique involves two bone tunnels and four high-strength polyethylene sutures and is suitable for medium-to-large rotator cuff tears that would alternatively need multiple anchors. This procedure not only maximizes the tendon-footprint contact area without using any implanted device but also theoretically lowers the bone laceration rate and is cost effective. In the current Technical Note, the procedure is described in detail along with several tips and tricks.
Classifications
Level I, shoulder; Level II, rotator cuff.
Technique Video
The arthroscope is first inserted to the joint for simple intra-articular inspection and management. Then, the scope is shifted to the subacromial space to perform bursectomy and acromioplasty before the repair begin. The cuff edge is examined and trimmed to a smooth crescent shape to ease traction suture application and manipulation of the cuff. The tuberosity spur is removed, and decortication is done at the footprint area where we planned to create the bone tunnels. A 1.5-mm straight punch is used to create the anterior pilot hole. Then, a no. 5 Ethibond suture needle is introduced into the pilot hole and slowly inserted further by using a curved needle holder, which is inserted through the lateral portal, and finally piercing the lateral humeral cortex. The scope is then moved to the subdeltoid space to seek the needle tip, which is then retrieved through the lateral portal. The posterior tunnel is created with the same manner. The suture can now be used for shuttling of the cuff sutures. The whole configuration is made from four polyethylene cuff sutures. They are attached to the proximal portion of the torn cuff by tissue penetrator. The inferior limbs are brought to the lateral row through bone tunnels via the shuttle sutures, which were previously placed within the tunnels. The medial row is tightened and tied first at the inferior limb of the anterior cortex, and then the cross-link sutures, and lastly, the traction limbs. Completion of the tying knots results in the final construct of the omega-shaped configuration.
Introduction
Rotator cuff injury is a common cause of shoulder pain in people of all age groups. In 1944, McLaughlin introduced open transosseous rotator cuff repair, and this technique was considered the gold standard because of its good clinical and biomechanical results.1 For a long time, transosseous repair was only feasible by using the open approach. In pursuit of the toughness and biomechanical compression healing benefits of the transosseous suture technique, the ideal configuration of the anchors in arthroscopic rotator cuff repair has been investigated, evolving from the single-row and double-row to the transosseous-equivalent construct. A high number of anchors is needed to achieve the ideal configuration, thus increasing the surgery cost. In addition, some anchor-related complications are still unsolved, including postoperative knot impingement pain, anchor pullout, greater tuberosity bone osteolysis, and difficult revision. Therefore, some studies have explored arthroscopic transosseous rotator cuff repair techniques. The purpose of this Technical Note is to describe an economical, reproducible, standardized, arthroscopic anchorless transosseous rotator cuff repair technique that uses an Omega configuration.
Surgical Technique
Preparation
The patient is set up in a beach chair position. A standard posterior portal is created for arthroscopic visualization. After intra-articular inspection, an anterior portal is created through the rotator cuff interval lateral to the coracoid process by using the outside-in technique. Intra-articular management is first performed through the anterior portal for debridement or labral reattachment (Video 1). The scope is then shifted to the subacromial space. Bursectomy is accomplished through the anterior portal. Cuff tear dimension is determined after bursectomy. The cuff edge is trimmed to a crescent shape to ease traction suture application (Fig 1). A lateral portal is made through needle localization, directed toward the center of the cuff defect.
Fig 1.
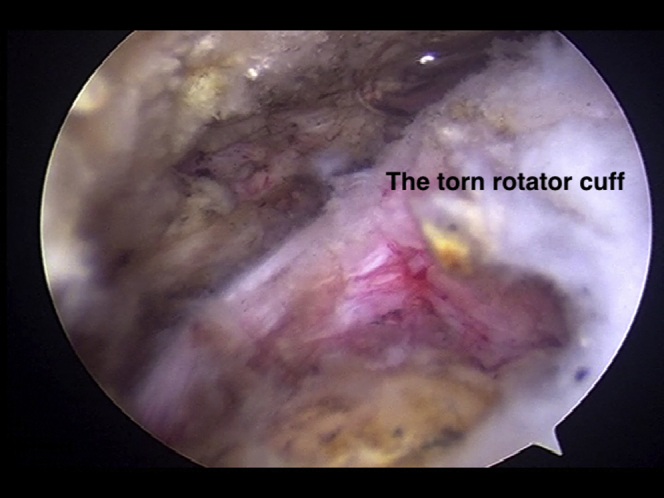
The cuff edge is trimmed to a crescent shape.
Tunnel Creation
A 1.5-mm-diameter straight punch is inserted through the lateral portal to create the medial row inlet on the medial edge of the footprint. Two pilot holes are created by tapping the punch through the bone surface. The anterior one is positioned near the bicipital groove, and the posterior one is positioned at the posterior edge of the cuff defect.
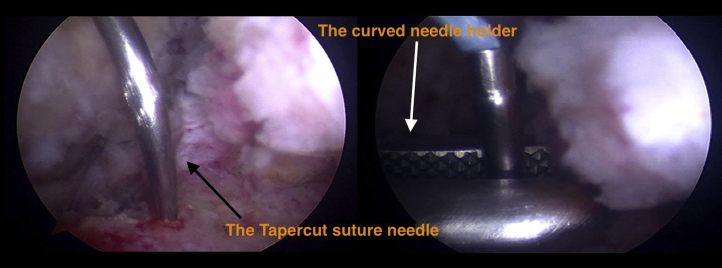
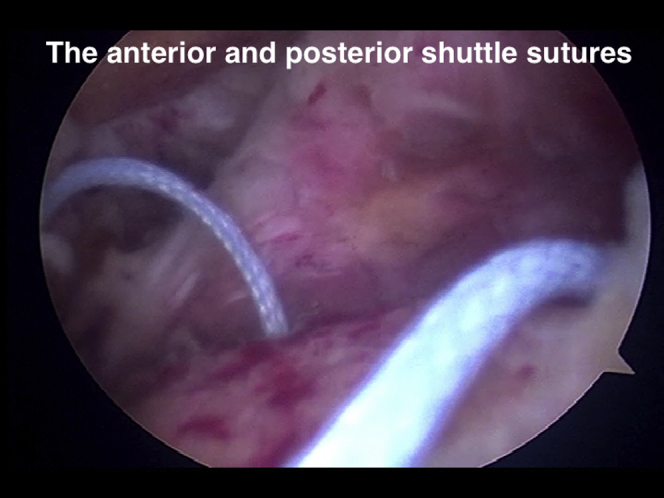
A no. 5, 1/2 circle, 48 mm, Tapercut suture needle (Ethibond Excel, Ethicon) is used to pierce though the skin at the lateral edge of the acromion. The needle tip is visible through the posterior portal and grasped by a curved needle holder introduced from the lateral portal (Fig 2). The needle tip is introduced into the posterior pilot hole and slowly inserted further by using a curved needle holder (Fig 3), finally piercing out of the lateral humeral cortex. The scope is then moved to the subdeltoid space to seek the needle tip, which is retrieved through the lateral portal also using the curved needle holder (Fig 4). The same procedure is repeated again at the anterior pilot hole with slightly external rotation of the shoulder. The sutures can now be used for shuttling (Fig 5).
Fig 2.
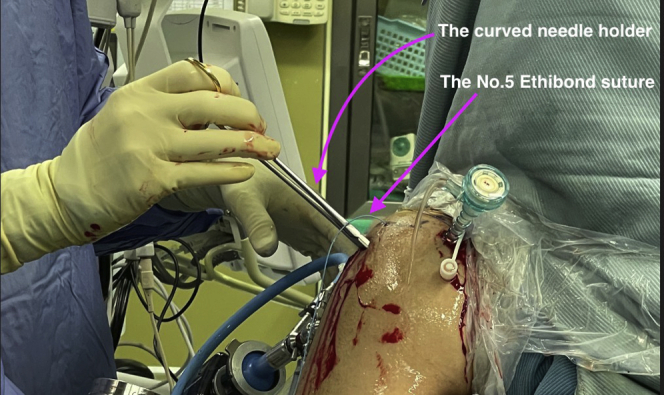
The curved needle holder is used to grasp the penetrating Ethibond suture needle from the lateral portal, and the scope is placed in the posterior portal.
Fig 3.
The needle tip is inserted further by using of curved needle holder.
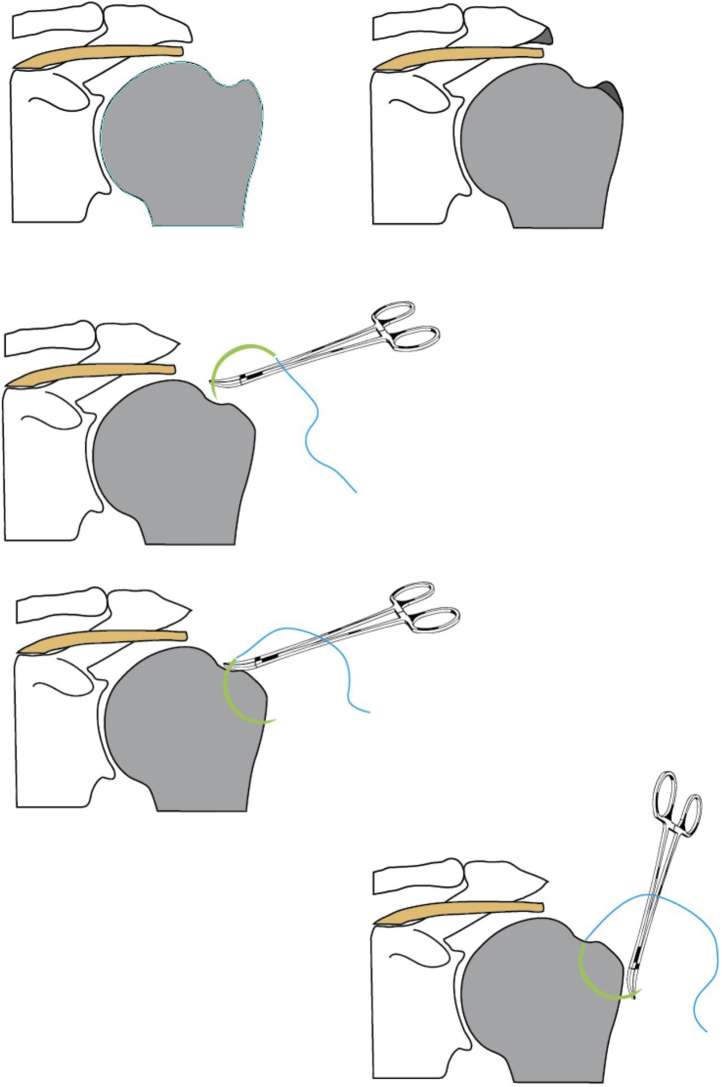
Fig. 4.
The whole bone tunnel preparation procedure in illustration.
Fig 5.
The two No. 5 Ethibond sutures used for cuff sutures’ shuttling.
Cuff Manipulation
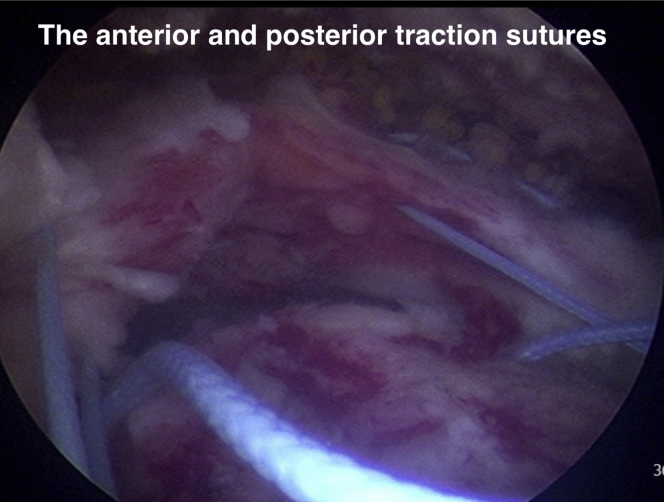
Two No. 2 polyester sutures (Ethibond Excel, Ethicon) are applied on the anterior and posterior edges of the torn cuff to serve as traction sutures (Fig 6). The traction sutures are retrieved through lateral portals. Two polyethylene sutures are applied to the medial row of the tendon. This is performed by dragging the cuff out with the traction sutures. The superior limbs of the medial row sutures are retrieved through the anterior portal. The inferior limbs of medial row sutures are passed through the anterior and posterior bone tunnels by using No. 5 Ethibond shuttle sutures and retrieved from the lateral portal. Two more polyethylene sutures are applied to the tendon both slightly anterior and posterior to the medial row sutures. All of the sutures are applied to the tendon with suture passer (TRUEPASS, Smith & Nephew). The superior limbs of the two sutures serve a cross-linking purpose, and the inferior limbs are passed through the suture tunnels in the same manner as the medial row sutures are.
Fig 6.
The two No. 2 Ethibond sutures used for traction sutures and at the end replaced by Polyethylene cuff sutures.
Sutures Configuration
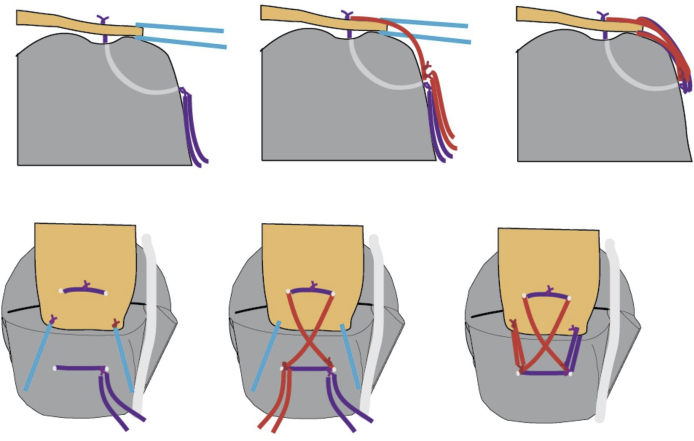
The shoulder is placed in an abduction position to facilitate rotator cuff traction. Superior limbs of the medial row are tied first, tightened through traction of the inferior limbs, and then tied on the lateral humeral cortex at the exit of suture tunnels. The superior limb of the posterior cross-link suture and inferior limb of the anterior cross-link suture are retrieved and tied together at the exit of the anterior tunnel of the lateral humeral cortex. Furthermore, the inferior limb of the posterior cross-link suture and superior limb of the anterior cross-link suture are tied at the posterior tunnel exit to finish the cross-link construct. The anterior traction suture is replaced by the remaining previously installed medial row-tying sutures, and the posterior traction suture is replaced by the remaining previously installed cross-link-tying sutures. The completion of the tying knots on the edge of the rotator cuff results in a final “W”-shaped construct (Fig 7).
Fig 7.
The cuff sutures’ arrangement in illustration. Blue denotes traction sutures, purple denotes medial row sutures, and red denotes crosslink sutures.
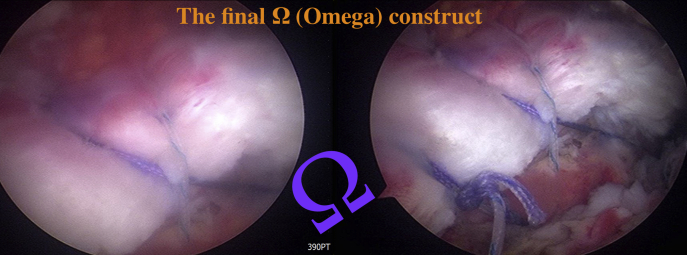
The core surgical procedure is the creation of two parallel curved suture tunnels. Two sets of sutures pass through these tunnels. One makes a horizontal row in proximal and distal regions, and the other makes a figure-eight cross-link. The final figure of the sutures appears like the final letter in the Greek alphabet: Omega (Fig 8).
Fig 8.
The final configuration of the sutures, Greek alphabet: Omega.
Rehabilitation
The patients are asked to wear a sling or abduction brace for at least 6 weeks. Passive shoulder range of motion is allowed during sling protection phase. Gentle strengthening exercises commence after sling removal.
Discussion
Although anchor-based repair became popular with the advancement of arthroscopy and even became the major technique in rotator cuff repair, biomechanical studies have demonstrated that anchor-based repair may not result in the same degree of repair site integrity as does transosseous repair.2, 3, 4
Since Cicak et al. suggested doing so in one of the first proposals of arthroscopic transosseous rotator cuff repair in 2006,5 many methods have been described that entail performing transosseous rotator cuff repair in a completely arthroscopic manner. However, most of these procedures require specific instruments for creating the tunnel or for passing sutures through the tunnel. In 2014, we have started conducting an anchorless technique for arthroscopic transosseous rotator cuff repair with an ordinary surgical instrument. This technique has several potential advantages.
First, the diameter of bone tunnels is a theoretical concern with transosseous techniques. Large bone tunnels involve more micromotion between the suture and the bone and have a higher possibility of bone laceration. The bone tunnel created using the ArthroTunneler (Wright) is 2.9 mm, and the reported intraoperative bone laceration rate by Liu et al. was 44%.6 No bone laceration cases related to bone tunnels were reported after using our procedure, which involves bone tunnels with a diameter of only 1.6 mm. Moreover, small entry maximizes the cuff-to-footprint contact area and creates a wide cuff-to-bone healing area compared with that produced with large tunnel holes.
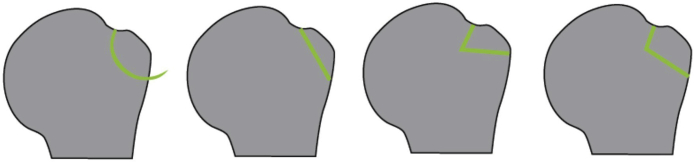
Second, the type of bone tunnel tract can influence the bone laceration rate. We categorized bone tunnels created during arthroscopic transosseous suture into four types (Fig 9). Type I is the curved tract. The tract is smooth without an angle, and it is usually created with a needle directly or an instrument such as a hooked bone penetrator. Type II is the straight linear tract. This type of tract is usually made with an anterior cruciate ligament (ACL) aiming device, directing the bone tunnel from the humeral lateral cortex to the medial side of the rotator cuff footprint. Types III and IV are sharp and blunt angle tracts composed of two intersecting bone tunnels created by a specific instrument designed for arthroscopic transosseous repair, such as the ArthroTunneler. Theoretically, the presence of an angle within the tunnel tract in types III and IV can lead to stress concentration at the angle, which might result in an intramedullary bone marrow laceration. A bone marrow laceration will loosen the construct and increase the micromotion between the bone and suture, leading to bone laceration and failure. The same rule applies to the type II linear tunnel, as it has a sharp turn at the entry and exit of the bone tunnel that can result in further bone laceration. In our technique, type I tunnels were created, with the least number of angles within the tunnel tract.
Fig 9.
Different types of bone tunnel tract in transosseous suture repair.
Lastly, the biomechanical effect of torn tendon compression on the prepared footprint makes transosseous repair superior to anchor repair. In our technique, two traction sutures are required to draw the cuff stump peripherally and apply adequate initial fixing power to the footprint. The traction sutures in the end are replaced by the remaining previously installed anterior medial row distal-tying sutures and the posterior cross-link-tying sutures, firmly securing the outer edge of the rotator cuff on the footprint. Compared with the X-Box technique described by Amir Steinitz et al.,7 our technique replaces the anterior and posterior limbs of the box, which are largely responsible for bone laceration due to the direct constriction force, with the divergent W-shaped edge traction suture to flatten the cuff.
As for the risks and limitations, there are several obstacles that one might encounter in the beginning of the learning curve, including failure to penetrate the lateral humeral cortex with the needle tip while creating the suture tunnels, inadequate span of the suture tunnels causing bone laceration, and the complicated configuration but poor visualization for the suture’s manipulation (Table 1). These factors can prompt the surgeon to give up this procedure and turn to other easier methods.
Table 1.
The Pearls and Pitfalls
| Pearls | Pitfalls | |
|---|---|---|
| Preparation | The subdeltoid bursa should be removed as far as 1 cm below the greater tuberosity to obtain good visualization of the needle exit point. The greater tuberosity should be burred to form a mild downslope morphology to ease cuff and suture manipulation. | Insufficient subdeltoid bursa resection will hinder the lateral humeral cortex needle exit point and become a time-consuming step. Without sufficient greater tuberosity removal, the subdeltoid space might be too narrow for suture manipulation and cause suture limbs to kink. |
| Tunnel creation | A perpendicular needle entrance alignment is crucial for the needle to penetrate the lateral humeral cortex. | The issues that may encounter regarding the needle exit point at the lateral humeral cortex, including needle entrapment within the humeral canal and insufficient span of the bone tunnels. Needle entrapment can occur because of acute insertion angle. Insufficient bone tunnel span is due to poor needle trajectory. |
| Cuff manipulation | The traction suture should be applied at the lateral side of the medial row suture to prevent suture tangling while engaging the medial row suture to the proximal suture tunnels. Cuff defect can be trimmed to a rectangle shape border instead of a half circle to facilitate cuff traction. | Sufficient cuff traction can be hard to achieve without adequate peripheral soft tissue release. |
| Suture fixation | Maintain adequate traction force during suture fixation to minimize tying resistance and decrease cutout of suture tunnels. | Suture fixation in a wrong sequence may cause insufficient rotator cuff tension. The fixation sequence should be as follows: the horizontal row, the cross limb, and the traction limb. |
In conclusion, arthroscopic transosseous rotator cuff repair is advantageous because it is a minimally invasive surgery and has good biomechanical healing factors. The Omega technique involves a low bone laceration rate and is cost effective, in addition to providing the aforementioned benefits (Table 2). After the coverage of National Health Insurance in Taiwan, the total surgical cost of the suture anchor method using around 4 or 5 anchors is approximately $4,000, and that of specific devices, such as the ArthroTunneler, is approximately $6,000. As we do not use disposable surgical instruments, the total surgical cost after the insurance coverage is merely $100. Regarding the limitations of this technique, new users face a long learning curve, and the technique is time-consuming.
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
|
|
|
|
|
|
|
|
|
Footnotes
Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The arthroscope is first inserted to the joint for simple intra-articular inspection and management. Then, the scope is shifted to the subacromial space to perform bursectomy and acromioplasty before the repair begin. The cuff edge is examined and trimmed to a smooth crescent shape to ease traction suture application and manipulation of the cuff. The tuberosity spur is removed, and decortication is done at the footprint area where we planned to create the bone tunnels. A 1.5-mm straight punch is used to create the anterior pilot hole. Then, a no. 5 Ethibond suture needle is introduced into the pilot hole and slowly inserted further by using a curved needle holder, which is inserted through the lateral portal, and finally piercing the lateral humeral cortex. The scope is then moved to the subdeltoid space to seek the needle tip, which is then retrieved through the lateral portal. The posterior tunnel is created with the same manner. The suture can now be used for shuttling of the cuff sutures. The whole configuration is made from four polyethylene cuff sutures. They are attached to the proximal portion of the torn cuff by tissue penetrator. The inferior limbs are brought to the lateral row through bone tunnels via the shuttle sutures, which were previously placed within the tunnels. The medial row is tightened and tied first at the inferior limb of the anterior cortex, and then the cross-link sutures, and lastly, the traction limbs. Completion of the tying knots results in the final construct of the omega-shaped configuration.
References
- 1.McLaughlin H.L. Lesions of the musculotendinous cuff of the shoulder. The exposure and treatment of tears with retraction. 1944. Clin Orthop Relat Res. 1994;(304):3–9. [PubMed] [Google Scholar]
- 2.Cole B.J., ElAttrache N.S., Anbari A. Arthroscopic rotator cuff repairs: An anatomic and biomechanical rationale for different suture-anchor repair configurations. Arthroscopy. 2007;23:662–669. doi: 10.1016/j.arthro.2007.02.018. [DOI] [PubMed] [Google Scholar]
- 3.Shi B.Y., Diaz M., Binkley M., McFarland E.G., Srikumaran U. Biomechanical strength of rotator cuff repairs: A systematic review and meta-regression analysis of cadaveric studies. Am J Sports Med. 2019;47:1984–1993. doi: 10.1177/0363546518780928. [DOI] [PubMed] [Google Scholar]
- 4.Urita A., Funakoshi T., Horie T., Nishida M., Iwasaki N. Difference in vascular patterns between transosseous-equivalent and transosseous rotator cuff repair. J Shoulder Elbow Surg. 2017;26:149–156. doi: 10.1016/j.jse.2016.06.010. [DOI] [PubMed] [Google Scholar]
- 5.Cicak N., Klobucar H., Bicanic G., Trsek D. Arthroscopic transosseous suture anchor technique for rotator cuff repairs. Arthroscopy. 2006;22:565.e1–565.e6. doi: 10.1016/j.arthro.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 6.Liu X.N., Yang C.J., Lee G.W., Kim S.H., Yoon Y.H., Noh K.C. Functional and radiographic outcomes after arthroscopic transosseous suture repair of medium sized rotator cuff tears. Arthroscopy. 2018;34:50–57. doi: 10.1016/j.arthro.2017.07.035. [DOI] [PubMed] [Google Scholar]
- 7.Steinitz A., Buxbaumer P., Hackl M., Buess E. Arthroscopic transosseous anchorless rotator cuff repair using the X-box technique. Arthrosc Tech. 2019;8:e175–e181. doi: 10.1016/j.eats.2018.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The arthroscope is first inserted to the joint for simple intra-articular inspection and management. Then, the scope is shifted to the subacromial space to perform bursectomy and acromioplasty before the repair begin. The cuff edge is examined and trimmed to a smooth crescent shape to ease traction suture application and manipulation of the cuff. The tuberosity spur is removed, and decortication is done at the footprint area where we planned to create the bone tunnels. A 1.5-mm straight punch is used to create the anterior pilot hole. Then, a no. 5 Ethibond suture needle is introduced into the pilot hole and slowly inserted further by using a curved needle holder, which is inserted through the lateral portal, and finally piercing the lateral humeral cortex. The scope is then moved to the subdeltoid space to seek the needle tip, which is then retrieved through the lateral portal. The posterior tunnel is created with the same manner. The suture can now be used for shuttling of the cuff sutures. The whole configuration is made from four polyethylene cuff sutures. They are attached to the proximal portion of the torn cuff by tissue penetrator. The inferior limbs are brought to the lateral row through bone tunnels via the shuttle sutures, which were previously placed within the tunnels. The medial row is tightened and tied first at the inferior limb of the anterior cortex, and then the cross-link sutures, and lastly, the traction limbs. Completion of the tying knots results in the final construct of the omega-shaped configuration.
The arthroscope is first inserted to the joint for simple intra-articular inspection and management. Then, the scope is shifted to the subacromial space to perform bursectomy and acromioplasty before the repair begin. The cuff edge is examined and trimmed to a smooth crescent shape to ease traction suture application and manipulation of the cuff. The tuberosity spur is removed, and decortication is done at the footprint area where we planned to create the bone tunnels. A 1.5-mm straight punch is used to create the anterior pilot hole. Then, a no. 5 Ethibond suture needle is introduced into the pilot hole and slowly inserted further by using a curved needle holder, which is inserted through the lateral portal, and finally piercing the lateral humeral cortex. The scope is then moved to the subdeltoid space to seek the needle tip, which is then retrieved through the lateral portal. The posterior tunnel is created with the same manner. The suture can now be used for shuttling of the cuff sutures. The whole configuration is made from four polyethylene cuff sutures. They are attached to the proximal portion of the torn cuff by tissue penetrator. The inferior limbs are brought to the lateral row through bone tunnels via the shuttle sutures, which were previously placed within the tunnels. The medial row is tightened and tied first at the inferior limb of the anterior cortex, and then the cross-link sutures, and lastly, the traction limbs. Completion of the tying knots results in the final construct of the omega-shaped configuration.