In the initial months of the coronavirus disease 2019 (COVID-19) pandemic because of the lack of effective treatments and unavailability of a vaccine, governments worldwide developed a variety of safety measures to control the spread of virus among their populations. Heterogeneous strategies variously implemented during the first year of the pandemic were often maintained after COVID-19 vaccines were made available.1, 2
Public health and social measures of containment, and nonpharmaceutical interventions (NPIs) that were developed and enforced at local level worldwide proved to be effective in limiting the spread of the disease and reducing the number of deaths.3 Safety measures adopted to minimize possible viral contamination included frequent hand washing, wearing facemasks, and social distancing policies taken on by communities to limit the spread of a disease. To further reduce person to person transmission of the virus, most countries have introduced a combination of school and workplace closures; public event cancellations, restrictions on public gatherings, closures of public transport, and stay-at-home orders.4
The implementation of strict public health NPIs targeting COVID-19 has been credited for a reduction of many viral and bacterial infectious diseases in children.5 , 6 For instance, global rates of respiratory syncytial virus (RSV), the most common cause of admission to hospital for infants in high-income countries, accounting for 60%-80% of bronchiolitis hospitalizations, have been significantly low since early 2020.6 , 7
However, the substantial decrease of protective immunity because of the extended period of low exposure to pathogens seems to have left a large part of the pediatric population susceptible to infections.6 For instance, the interseasonal circulation of RSV has been reported in different areas, including Australia during late 2020, South Africa in early 2021, southern US in June 2021, and in Europe after summer 2021.8
This commentary, authored by the working group on social pediatrics of the European Pediatric Association/Union of National European Pediatric Societies and Associations, briefly discusses the insurgence of infectious diseases because of the immune debt associated to the public health NPIs established to control the COVID-19 pandemic. Our aim is to raise awareness of pediatricians and public health authorities on the importance vaccination programs in children to contrast the immune debt associated to the pandemic.6 , 9
Effect of COVID-19 NPIs on Pediatric Infectious Diseases
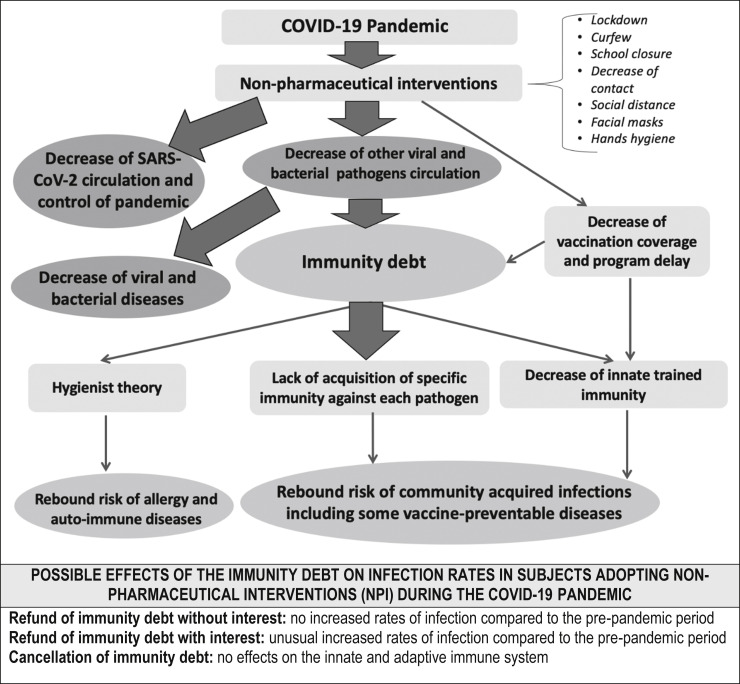
Since the beginning of the COVID-19 pandemic, children and adolescents have shown low rates of infection, as well as relatively low rates of severe or critical forms of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).10 , 11 NPIs have limited the spread of COVID-19 in Europe.6 , 12 NPIs imposed to reduce the SARS-CoV-2 spread are also credited for the decrease of viral and bacterial infections observed, particularly in pediatric population5 (Figure; available at www.jpeds.com).
Figure.
Immunity debt in children following the adoption of COVID-19 NPIs.
Studies performed in the European Union have shown that lockdown measures have led to a rapid decline in the infectious respiratory diseases, specifically, a sharper decrease in influenza and RSV infections in 2020 and 2021, compared with previous years.12 However, the implementation of NPIs among the various European countries was different with a negative correlation between the severity of the NPI imposed and the decline of the infectious diseases. For instance, the decline of influenza and RSV was stronger in Italy, compared with other European countries such as Sweden and Germany, where the NPIs were less stringent and the population less compliant.12 The efficacy of the measures established to control of COVID-19 transmission is a consolidated evidence,13 and their effectiveness is also recognized as a key factor in containing the spread of other respiratory infectious diseases.3 However, the long-term impact of an extensive adoption of useful NPI safety measures is currently unknown.6 In particular, it is unclear whether and to what extent infectious diseases that significantly declined during the pandemic will re-emerge after COVID-19 mitigation measures are lifted. Data on increasing numbers of RSV cases after the summer 2021 seems to suggest an imminent risk for children's health.6
Immunity Debt following Extended Periods of COVID-19 Mitigation Measures
Because of the NPIs enforced during the pandemic, children have experienced extended periods of low exposure to pathogens.7 , 14 Immune memory is a defining feature of the acquired immune system.15 Concerns have been raised about the lack of exposure to common infections and the possibility that prolonged periods of reduced contacts with pathogens may reduce protective immunity6 , 7 , 16 and influence the development of adaptive immunity against infectious agents.6 , 16 , 17 Activation of the innate immune system can also result in enhanced responsiveness to triggers.15 In the absence of exposure to seasonal infectious diseases, immunity may decrease while the susceptibility to infections increases.6 Therefore, the immunity debt caused by the NPIs adopted during the pandemic (Figure) could expose children to a greater potential for an increase in outbreaks and possible epidemics because of new or re-emerging infectious agents.6 , 7
Unusual Surge of RSV Infections in Children Amid the Ongoing Pandemic
A significant decline in infection rates was reported for pneumococcal diseases,18 , 19 Neisseria meningitidis infections,19 , 20 pertussis,21 , 22 varicella,21 , 23 measles,21 enterovirus infections,23 influenza,5 , 23, 24, 25 and RSV infections.5 , 24 , 26, 27, 28
In Australia, RSV infections29 began to increase during the spring months and peaked in late September 2021 with the number of cases significantly greater than in previous years.24 , 25 In Japan, a significant outbreak of RSV infections was reported starting in spring 2021,30 while in the US, RSV started to rise in some areas of the southern states before summer 2021.30 , 31 In Texas, where the trend began at the end of June, nearly one-half of pediatric patients hospitalized in local hospitals in August 2021 were diagnosed with RSV.32 , 33 In Europe, respiratory infections in young children have begun to rise in England following low infection rates in response to COVID-19 restrictions and positivity of samples tested for RSV rapidly increased over 5 consecutive weeks by the end of July 2021, well before the typical winter season.34 In France, a delayed bronchiolitis epidemic driven by RSV was reported in March 2021.27 In autumn 2021, epidemiology indicators showed an earlier and more rapid onset of bronchiolitis virus circulation compared to previous years.34, 35, 36
Israel has experienced a large outbreak of RSV bronchiolitis during the summer of 2021 following the decline of the COVID-19 third wave and the lifting of NPI. This outbreak resulted in a significant increase of hospitalizations and overloaded pediatric wards and pediatric intensive care units throughout the country.37 In response to the RSV outbreak, the Israeli Ministry of Health recommended routine prophylaxis programs from the month of November.38 In Italy, the Italian Society of Pediatrics reports that RSV infection rose earlier than the usual peak observed in December-January.39 , 40 In some areas of Southern Italy, in October 2021 there was a 30% increase of RSV cases compared to previous years39 and similar data are reported from the Northern regions, where in Veneto, in the month of October 2021 alone, the hospitalizations related to RSV were one-half of those recorded throughout the entire 2020-2021 winter season.39
Conclusions
COVID-19 mitigation measures led to shifts in typical annual respiratory virus patterns.6 It is unclear whether this global trend will continue and how co-infection of RSV and other respiratory viruses with SARS-CoV-2 will affect disease severity in children during the winter season. Appropriate monitoring of the ongoing RSV epidemic and adequate interventional measures41 , 42 should be continued and regular vaccination programs for infectious diseases maintained to protect children against respiratory viruses and other infectious agents and to prevent community transmission of diseases.32 , 43
Footnotes
The authors declare no conflict of interest.
References available at www.jpeds.com.
Appendix
References
- 1.Ferrara P., Franceschini G., Corsello G., Mestrovic J., Giardino I., Vural M., et al. Effects of coronavirus disease 2019 (COVID-19) on family functioning. J Pediatr. 2021;237:322–323.e2. doi: 10.1016/j.jpeds.2021.06.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shen Y., Powell G., Ganser I., Zheng Q., Grundy C., Okhmatovskaia A., et al. Monitoring nonpharmaceutical public health interventions during the COVID-19 pandemic. Sci Data. 2021;8:225. doi: 10.1038/s41597-021-01001-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Müller O., Razum O., Jahn A. Effects of nonpharmaceutical interventions against COVID-19 on the incidence of other diseases. Lancet Reg Health Eur. 2021;6:100139. doi: 10.1016/j.lanepe.2021.100139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Perra N. Nonpharmaceutical interventions during the COVID-19 pandemic: a review. Phys Rep. 2021;913:1–52. doi: 10.1016/j.physrep.2021.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baker R.E., Park S.W., Yang W., Vecchi G.A., Metcalf C.J.E., Grenfell B.T. The impact of COVID-19 nonpharmaceutical interventions on the future dynamics of endemic infections. Proc Natl Acad Sci U S A. 2020;117:30547–30553. doi: 10.1073/pnas.2013182117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cohen R., Ashman M., Taha M.K., e Varon E., Angoulvant F., Levy C., et al. Pediatric Infectious Disease Group (GPIP) position paper on the immune debt of the COVID-19 pandemic in childhood, how can we fill the immunity gap? Infect Dis Now. 2021;51:418–423. doi: 10.1016/j.idnow.2021.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hatter L., Eathorne A., Hills T., Bruce P., Beasley R. Respiratory syncytial virus: paying the immunity debt with interest. Lancet Child Adolesc Health. 2021;5:e44–e45. doi: 10.1016/S2352-4642(21)00333-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Center for Diseaes Control and Prevention (CDC) Emergency Preparedness and Response. Increased Interseasonal Respiratory Syncytial Virus (RSV) Activity in Parts of the Southern United States. https://emergency.cdc.gov/han/2021/han00443.asp
- 9.Campbell J.D. When can children get the COVID-19 vaccine? HealthyChildren Magazine. https://www.healthychildren.org/English/tips-tools/ask-the-pediatrician/Pages/when-can-children-get-the-COVID-19-vaccine.aspx
- 10.Njonnou S.R.S., Anangmo N.C.N., Lekpa F.K., Njinkui D.N., Enyama D., Ouankou C.N., et al. The COVID-19 prevalence among children: hypotheses for low infection rate and few severe forms among this age group in Sub-Saharan Africa. Interdisciplinary Perspectives on Infectious Diseases. 2021. Article ID 4258414. [DOI] [PMC free article] [PubMed]
- 11.Williams J., Namazova-Baranova L., Weber M., Vural M., Mestrovic J., Carrasco-Sanz A., et al. The importance of continuing breastfeeding during coronavirus disease-2019: in support of the World Health Organization statement on breastfeeding during the pandemic. J Pediatr. 2020;223:234–236. doi: 10.1016/j.jpeds.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Micha Kaiser M., Otterbach S., Sousa-Poza A., Bloom D.E. 2020. Interventions with positive side-effects: COVID-19 nonpharmaceutical interventions and infectious diseases in Europe. Institute of Labor Economics. Deutche Post Foundation. IZA DP No. 13927. [Google Scholar]
- 13.Tempia S., Walaza S., Bhiman J.N., McMorrow M.L., Moyes J., Mkhencele T., et al. Decline of influenza and respiratory syncytial virus detection in facility-based surveillance during the COVID-19 pandemic, South Africa, January to October 2020. Euro Surveill. 2021;26:2001600. doi: 10.2807/1560-7917.ES.2021.26.29.2001600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huss G., Magendie C., Pettoello-Mantovani M., Jaeger-Roman E. Implications of the COVID-19 Pandemic for Pediatric Primary Care Practice in Europe. J Pediatr. 2021;233:290–291.e2. doi: 10.1016/j.jpeds.2021.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Netea M.G., Domínguez-Andrés J., Barreiro L.B., Chavakis T., Divangahi M., Fuchs E., et al. Defining trained immunity and its role in health and disease. Nat Rev Immunol. 2020;20:375–388. doi: 10.1038/s41577-020-0285-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mak T.W., Saunders M.E., Jett B.D. Primer to the immune response (second edition). Chapter 1-Introduction to the immune response. 2014. pp. 3–20. Editor: Academic Cell. [Google Scholar]
- 17.Agha R., Avner J.R. Delayed seasonal RSV surge observed during the COVID-19 pandemic. Pediatrics. 2021;148 doi: 10.1542/peds.2021-052089. e2021052089. [DOI] [PubMed] [Google Scholar]
- 18.Amin-Chowdhury Z., Aiano F., Mensah A. Impact of the coronavirus disease 2019 (COVID-19) pandemic on invasive pneumococcal disease and risk of pneumococcal coinfection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): prospective national cohort study, England. Clin Infect Dis. 2021;72:e65–e75. doi: 10.1093/cid/ciaa1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brueggemann A.B., Jansen van Rensburg M.J., Shaw D. Changes in the incidence of invasive disease due to Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis during the COVID-19 pandemic in 26 countries and territories in the Invasive Respiratory Infection Surveillance Initiative: a prospective analysis of surveillance data. Lancet Digit Health. 2021;3:e360–e370. doi: 10.1016/S2589-7500(21)00077-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Taha M.K., Deghmane A.E. Impact of COVID-19 pandemic and the lockdown on invasive meningococcal disease. BMC Res Notes. 2020;13:399. doi: 10.1186/s13104-020-05241-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Belingheri M., Paladino M.E., Piacenti S., Riva M.A. Effects of COVID-19 lockdown on epidemic diseases of childhood. J Med Virol. 2021;93:153–154. doi: 10.1002/jmv.26253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Matczak S., Levy C., Fortas C. Association between COVID-19 pandemic and pertussis in France using multiple nationwide data sources. https://wwwmedrxivorg/content/101101/2021071621260367v1 2021 [DOI] [PMC free article] [PubMed]
- 23.Cohen R., Bechet S., Gelbert N. New approach to the surveillance of pediatric infectious diseases from ambulatory pediatricians in the digital era. Pediatr Infect Dis J. 2021;40:674–680. doi: 10.1097/INF.0000000000003116. [DOI] [PubMed] [Google Scholar]
- 24.Yeoh D.K., Foley D.A., Minney-Smith C.A. The impact of COVID-19 public health measures on detections of influenza and respiratory syncytial virus in children during the 2020 Australian winter. Clin Infect Dis. 2021;72:2199–2202. doi: 10.1093/cid/ciaa1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Foley D.A., Yeoh D.K., Minney-Smith C.A. The interseasonal resurgence of respiratory syncytial virus in Australian children following the reduction of coronavirus disease 2019-related public health measures. Clin Infect Dis. 2021;73:e2829–e2830. doi: 10.1093/cid/ciaa1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Casalegno J.S., Ploin D., Cantais A., Masson E., Bard E., Valette M., et al. Characteristics of the delayed respiratory syncytial virus epidemic, 2020/2021, Rhone Loire, France. Euro Surveill. 2021;26:2100630. doi: 10.2807/1560-7917.ES.2021.26.29.2100630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rybak A., Levy C., Jung C., Béchet S., Batard C., Hassid F., et al. Delayed bronchiolitis epidemic in french primary care setting driven by respiratory syncytial virus: preliminary data from the Oursyn study, March 2021. Pediatr Infect Dis J. 2021;40:e511–e514. doi: 10.1097/INF.0000000000003270. [DOI] [PubMed] [Google Scholar]
- 28.Skurnik D., Rybak A., Yang D.D. Unexpected lessons from the COVID-19 lockdowns in France: low impact of school opening on common communicable pediatric airborne diseases. Clin Infect Dis. 2021;73:e2830–e2832. doi: 10.1093/cid/ciaa1899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Miller E.K., Gebretsadik T., Carroll K.N., Dupont W.D., Mohamed Y.A., Morin L.L., et al. Viral etiologies of infant bronchiolitis, croup and upper respiratory illness during 4 consecutive years. Pediatr Infect Dis J. 2013;32:950–955. doi: 10.1097/INF.0b013e31829b7e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Center for Disease Control and Prevention (CDC) Increased Interseasonal Respiratory Syncytial Virus (RSV) Activity in Parts of the Southern United States. https://emergency.cdc.gov/han/2021/han00443.asp
- 31.Pan American Health Organization Regional update, influenza. https://www.paho.org/en/documents/regional-update-influenza-epidemiological-week-25-july-6-2021 Epidemiological week 25—July 6, 2021.
- 32.Global Virus Network Perspectives. Unusual surge of respiratory syncytial virus in children. September 24, 2021. https://gvn.org/unusual-surge-of-respiratory-syncytial-virus-in-children/
- 33.Romo V. As children's COVID cases surge, there's another virus on the rise. NPR Health. https://www.npr.org/2021/08/14/1027663917/rsv-covid-children
- 34.UK Health Security Agency and Office for Health Improvement and Disparities Health chiefs issue warning as childhood respiratory infections rise ahead of winter. https://www.gov.uk/government/news/health-chiefs-issue-warning-as-childhood-respiratory-infections-rise-ahead-of-winter
- 35.INFOVC-France Information Platform on Vaccinations. https://www.infovac.fr/reseau-pari?layout=list&types[0]=1
- 36.Public Health France Impact of COVID-19 social distancing on viral infection in France: A delayed outbreak of RSV. https://www.santepubliquefrance.fr/docs/impact-of-covid-19-social-distancing-on-viral-infection-in-france-a-delayed-outbreak-of-rsv [DOI] [PMC free article] [PubMed]
- 37.Weinberger Opek M., Yeshayahu Y., Glatman-Freedman A. Delayed respiratory syncytial virus epidemic in children after relaxation of COVID-19 physical distancing measures, Ashdod, Israel, 2021. Euro Surveill. 2021;26:2100706. doi: 10.2807/1560-7917.ES.2021.26.29.2100706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Respiratory viruses in Israel Surveillance Report, The Israeli Center for Disease Control. October 2021. https://www.gov.il/BlobFolder/reports/corona-flu-10072021/en/files_weekly-flu-corona_EN-2021_corona-flu-week-27-EN.pdf
- 39.AdnKronos Health Virus respiratorio neonati, nel 2021 più casi e più gravi. https://www.adnkronos.com/virus-respiratorio-neonati-nel-2021-piu-casi-e-piu-gravi_33oWiaHyt5JQRukwtwk9kB?refresh_ce
- 40.European Centre for Disease Prevention and Control. COVID-19 surveillance guidance‒transition from COVID-19 emergency surveillance to routine surveillance of respiratory pathogens. Accessed November 6, 2021.
- 41.Somekh I., Somech R., Pettoello-Mantovani M., Somekh E. Changes in routine pediatric practice in light of coronavirus 2019 (COVID-19) J Pediatr. 2020;224:190–193. doi: 10.1016/j.jpeds.2020.05.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pettoello-Mantovani M., Pop T.L., Mestrovic J., Ferrara P., Giardino I., Carrasco-Sanz A., et al. Fostering resilience in children: the essential role of healthcare professionals and families. J Pediatr. 2019;205:298–299.e1. doi: 10.1016/j.jpeds.2018.10.069. [DOI] [PubMed] [Google Scholar]
- 43.Pettoello-Mantovani M., Carrasco-SanzHuss A.G., Mestrovic J., Vural M., Pop T.L., et al. Viewpoint of the European pediatric societies over severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccination in children younger than age 12 years amid return to school and the surging virus variants. J Pediatric. 2021;239:250–251.e2. doi: 10.1016/j.jpeds.2021.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]